Abstract
Bone cement leakage from the femoral medullary cavity is a rare complication following hip replacement. Currently, there are no reports of bone cement leakage into the heart. Here, we report an 81-year-old female patient with right femoral neck fracture. A thorough preoperative examination showed that bone cement had leaked into the heart during right femoral head replacement, leading to the death of the patient that night. Postoperative cardiac ultrasound showed that bone cement entered the vascular system through the femoral medullary cavity and subsequently entered the heart. Extreme deterioration in the patient’s condition resulted in death that night. Unfortunately, the patient’s family abandoned the idea of surgical removal of foreign bodies, leading to inevitable death. This case emphasizes the risk of clinical manifestations of cardiac embolism of bone cement after artificial femoral head replacement, suggesting that the risk of such embolism might be underestimated. We propose routine real-time C-arm X-ray guidance and injection of an appropriate amount of bone cement to prevent serious cardiopulmonary failure.
Keywords: Femoral neck fracture, hip hemiarthroplasty, bone cement leakage, intracardiac embolism
Introduction
In an aging society, femoral neck fractures are becoming more common in the elderly [1]. Artificial femoral head replacement is the most effective treatment for femoral neck fractures [2]. Bone cement plays an important role in hemiarthroplasty [3-5], but complications, such as cement leakage into the blood vessels reaching the heart, lungs, and cerebral circulation, are common. However, it is exceptionally rare for bone cement to leak into the heart [6,7]. We encountered the following case of bone cement leakage into the heart.
Case report
An 81-year-old female patient fell two days prior, and the pain worsened during home recuperation, prompting her to come to our hospital. An X-ray revealed a right femoral neck fracture. She had a history of hypertension, chronic emphysema, and heart disease for 5, 10, and 8 years, respectively. No specific diagnosis or treatment had been provided, and other examinations did not reveal any notable abnormalities. The surgical operation was performed 3 days after admission. At 14:00, the patient received oxygen inhalation after entering the room. Right internal jugular vein puncture and catheterization were performed, and L2-3 combined spinal and epidural anesthesia was administered in the left lateral position. After lying down, the patient reported no obvious discomfort, and vital signs remained stable. The anesthesia was effective, and the left lateral (surgical) position was assumed. The surgery commenced at 15:00. Throughout the procedure, the patient’s vital signs remained stable, with blood pressure (BP) ranging from 125-140/65-75 mmHg, heart rate (HR) at 75-90 beats/min, and oxygen saturation (SPO2) at 99-100%. During the operation, about 1 minute after bone cement implantation at 15:31, the patient suddenly experienced a loss of consciousness, accompanied by a significant decrease in BP to 64/34 mmHg, HR to 49 beats/min, and SPO2 to 81%. Despite intravenous administration of 10 mg ephedrine and 20 µg epinephrine, the response was unsatisfactory. The patient was immediately placed in the supine position, chest compressions were initiated, and tracheal intubation was performed as the patient’s heartbeat had ceased. At 15:46, skin suturing was completed. The maintenance of the norepinephrine micropump (8 mg/36 ml NS, 3 mg/h), adrenaline administration at specific intervals (a total of 5 mg), and intravenous infusion of 150 mL sodium bicarbonate were performed. The patient’s heartbeat continuously recovered until 16:17. She was sent to the ICU at 16:50, and continued to receive sedation, ventilator support, mild hypothermia treatment to reduce oxygen consumption and protect brain cells, nutritional support for myocardial treatment of ischemia and hypoxia injury, and symptomatic support treatment, including sodium bicarbonate correction for acid imbalance. Simultaneously, the patient’s bedside echocardiography showed a large foreign body in the right atrium, with some clumps crossing the tricuspid valve and entering the right ventricle (Figure 1 and Supplementary Video, IMG_2677). The electrocardiogram indicated: 1. atrial fibrillation with a rapid ventricular rate, 2. complete right bundle branch block, 3. ST segment changes, and 4. QT interval prolongation (Figure 2). Therefore, we suspected that the patient might have had a cardiac embolism. The patient’s family refused any invasive treatment techniques. At 19:30, the patient was in a deep coma and needed large doses of vasoactive drugs to maintain stability. After 21:00, the patient’s BP was 55-60/35-38 mmHg, and SPO2 levels could not be detected. The patient was in a state of shock that was difficult to improve, and her condition was critical. The family chose to discharge the patient after a medical consultation, and she passed away on the night she returned home.
Figure 1.

Bedside echocardiography showed the cardiac dynamic results. A. A large foreign body was visible in the right atrium (red arrow); B. Emboli caused ineffective contractions of the right atrium; C. Some clumps could cross the tricuspid valve and enter the right ventricle.
Figure 2.
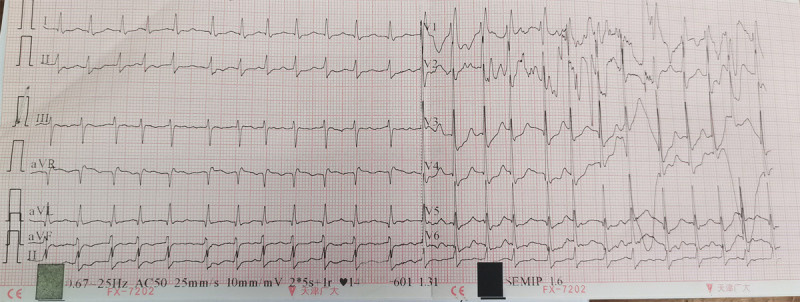
Electrocardiogram showed the cardiac results: 1. atrial fibrillation with a rapid ventricular rate, 2. complete right bundle branch block, 3. ST segment changes, and 4. QT interval prolongation.
Discussion
Intracardiac bone cement embolization is a rare complication associated with hip replacement surgery. Cement leakage can occur through small veins into the venous system, further migrating to the right side of the heart and pulmonary artery. In most cases, cement leakage is considered to be a subclinical problem. However, in some cases, cement leaks can be fatal. We reviewed the literature and found 26 cases of intracardiac bone cement embolization (Table 1). The main manifestations of cardiac embolism are perforation, pericardial tamponade, or pericardial perforation, which can cause chest pain and dyspnea [8-12] and occur during or after surgery. Pannirselvam et al. [13] reported that one patient presented with syncope in the ninth month after vertebroplasty. Transesophageal echocardiography revealed a mass with a size of 2.8 cm at the outlet of the inferior vena cava in the right atrium. The patient was treated with prophylactic anticoagulants for the emboli, and symptoms improved.
Table 1.
Patients’ characteristics of the cement embolus, method of the treatment and the outcome
| Case no. | Age/sex | Surgery | Embolus | Symptoms | Treatment | Outcome | Paper |
|---|---|---|---|---|---|---|---|
| 1 | 62/f | Kyphoplasty | Right ventricle | Chest pain | Thoracotomy | Recovery | Prokop et al. [8] |
| 2 | 84/f | Vertebroplasty | Cement leakage from t10 to l2 | Weakness, numbness, and pain in both legs | Removed intradural cement completely | Recovery | Baek et al. [25] |
| 3 | 52/f | Vertebroplasty | Right atrium | Syncope | Anticoagulation | Recovery | Pannirselvam et al. [13] |
| 4 | 73/f | Vertebroplasty | Right atrium, right ventricle, right pulmonary artery | Asymptomatic | Thoracotomy | Recovery | Dash et al. [26] |
| 5 | 55/f | Vertebroplasty | Right atrium, right ventricle | Dyspnea and edema | Thoracotomy | Recovery | Lim et al. [18] |
| 6 | 71/f | Vertebroplasty | Right ventricle, right pulmonary artery | Acute respiratory distress | Thoracotomy | Recovery | Arnaiz-garcia et al. [27] |
| 7 | 64/f | Vertebroplasty | Right atrium, right pulmonary artery, left pulmonary artery | Progressive dyspnea | Thoracotomy | Recovery | Caynak et al. [28] |
| 8 | -/f | Vertebroplasty | Right ventricle | Worsening dyspnea | Thoracotomy | Death | Lee et al. [14] |
| 9 | 71/m | Vertebroplasty | Right atrium | Chest pain, epigastric pain, diaphoresis, syncope | Percutaneous retrieval | Recovery | Mattis et al. [9] |
| 10 | 66/f | Vertebroplasty | Right atrium, right ventricle | Pleuritic chest pain | Thoracotomy | Recovery | Park et al. [15] |
| 11 | 65/f | Vertebroplasty | Right atrium, right ventricle | Chest pain and collapse | Thoracotomy | Recovery | Son et al. [10] |
| 12 | 71/m | Vertebroplasty | Right atrium | Chest pain | Percutaneous retrieval | Recovery | Grifka et al. [11] |
| 13 | 74/f | Kyphoplasty | Right ventricle, right pulmonary artery | Right-sided chest pain, nausea | Thoracotomy | Recovery | Farahvar et al. [16] |
| 14 | 58/f | Kyphoplasty | Right ventricle, right pulmonary artery | Chest pain, shortness of breath | Thoracotomy | Recovery | Gosev et al. [29] |
| 15 | 75/f | Vertebroplasty | Right atrium, right ventricle | Dyspnea | Thoracotomy | Recovery | Kim et al. [12] |
| 16 | 66/f | Vertebroplasty | Right atrium, right ventricle | Chest pain | Thoracotomy | Recovery | Kim et al. [17] |
| 17 | 86/f | Vertebroplasty | Right atrium, right ventricle | Chest pain and fever | Thoracotomy | Recovery | Moon et al. [30] |
| 18 | 68/f | Kyphoplasty | Right ventricle | Chest pain and dyspnea, cardiac shock | Thoracotomy and percutaneous retrieval | Recovery | Tran et al. [31] |
| 19 | 85/f | Vertebroplasty | Right atrium | Hypotension | Percutaneous retrieval | Recovery | Bose et al. [32] |
| 20 | 51/f | Vertebroplasty | Right atrium, right ventricle | Chest pain and palpitation | Percutaneous retrieval | Recovery | Braiteh et al. [33] |
| 21 | 70/f | Kyphoplasty and vertebroplasty | Right atrium, right ventricle | Chest tightness | Thoracotomy | Recovery | Sun et al. [19] |
| 22 | 61/f | Vertebroplasty | Right ventricle | Chest pain and dyspnea | Thoracotomy | Recovery | Krithika et al. [20] |
| 23 | -/f | Vertebroplasty | Right atrium, right ventricle | Unconscious | Thoracotomy | Recovery | Yin et al. [34] |
| 24 | 56/m | Kyphoplasty | Right atrium | Dyspnea and right-sided chest pain | Thoracotomy | Recovery | Weininger et al. [35] |
| 25 | 57/f | Vertebroplasty | Right atrium | Left-sided chest pain | Anticoagulation | Recovery | Hatzantonis et al. [24] |
| 26 | 28/m | Kyphoplasty and vertebroplasty | Right ventricle | Chest pain | Thoracotomy | Recovery | Audat et al. [36] |
The occurrence of cement emboli at different locations has different effects on the cardiac function of patients. For example, case studies of echocardiography in patients with embolus-related right ventricular complications revealed moderate to severe pericardial effusion [14-16] or hemopericardium [9,10,17]. Park et al. [15] hypothesized that cement deposits in the right atrium and ventricle of a 66-year-old female patient were attributable to the injection of very low-viscosity acrylic cement into the vertebral body that subsequently flowed into the right ventricle, resulting in acute pericarditis. Kim et al. reported on an embolus in a patient undergoing vertebroplasty of the right atrium and ventricle. The echocardiogram showed an overall decline in cardiac function, poor systolic function (27%), impaired diastolic functioning in the left ventricle, and moderate to severe tricuspid reflux [12]. One case reported difficulty in breathing and heart-related problems more than 5 years later; it was revealed that bone cement leakage had occurred from the mouth into the right atrium and right ventricle [18]. Two patients experienced left and right pulmonary trunk and right ventricular embolism. Though the patients reported no discomfort and stable vital signs, conservative treatment was chosen [19,20]. Most of the remaining patients needed open heart surgery. Intracardiac cement embolism mostly occurred during or after percutaneous vertebroplasty, and the incidence of intracardiac cement embolism after percutaneous vertebroplasty was only 3.9% [11].
All the leakage of cement into the inferior vena cava resulted in a pulmonary embolism [21]. Reducing bone cement leakage, especially towards the inferior vena cava, can reduce the incidence of bone cement cardiac embolism. Unclear display screens in C-shaped arm line machines, use of low-viscosity cement, and excessive injection of bone cement increase the risk of bone cement leakage [14,22]. Bone cement injection under the fluoroscopic guidance of a C-arm machine with real-time and clear display screen is very helpful for reducing bone cement leakage. Immediate cessation of bone cement injection is crucial in the event of a leakage. Alternatively, a gelatin sponge can be placed through the working sleeve, and prompt repositioning of the sleeve can be considered [23]. In this case, bone cement injection occurred without real-time guidance from the C-arm X-ray machine, resulting in bone cement leakage, an essential factor in this complication. In addition, the injection of a total of about 50 mL of bone cement was a secondary complicating factor.
There is no consensus on the best treatment for cement leakage-induced cardiac embolism. Non-surgical treatment includes symptomatic treatment and oral anticoagulant therapy for 3 to 6 months, and surgical treatment includes percutaneous embolectomy (especially for right atrial emboli) and open cardiac embolectomy [22]. Asymptomatic patients are often treated with anticoagulants such as warfarin or low-molecular-weight heparin [24]. In symptomatic patients, the emboli in the right atrium are usually removed using a percutaneous catheter. In patients with right ventricular involvement or perforation, surgical removal is required, while open surgery is required to remove large right ventricular emboli, even in the absence of symptoms.
During surgery, our patient experienced an immediate decrease in blood oxygen saturation, unclear consciousness, a significant decrease in BP and heart rate, and cessation of spontaneous breathing, after which the heartbeat stopped. In addition, the cardiac ultrasound showed a huge foreign body in the right ventricle, and our patient’s vital signs were extremely unstable. Therefore, we should have performed a thoracotomy as soon as possible. Unfortunately, the patient’s family opted not to pursue the surgical removal of foreign bodies, leading to the inevitable outcome of death.
This represents the first reported case of cardiogenic embolism resulting as a complication of hemiarthroplasty. Thus, cement can lead to cardiac embolism after solidifying from a paste during injection.
Conclusions
This case emphasizes the risk of clinical manifestations of cardiac embolism of bone cement after artificial femoral head replacement, suggesting that the risk of such embolism might be underestimated. We propose routine real-time C-arm X-ray guidance and inject an appropriate amount of bone cement to prevent serious cardiopulmonary failures. When bone cement is used, symptoms such as dyspnea, chest pain, and decreased oxygen saturation should raise suspicion of cardiac embolism, prompting immediate bedside echocardiography. A suspected cardiac embolism is a serious condition that demands prompt intervention, including open heart surgery, to save the patient’s life.
Acknowledgements
We are thankful to the patient, her families, and clinicians participating in this study.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Ballas ER, Nguyen VT, Wolin EA. Femoral neck fracture with avascular necrosis. J Nucl Med Technol. 2023;51:78–79. doi: 10.2967/jnmt.122.264354. [DOI] [PubMed] [Google Scholar]
- 2.Wu X, Shen Y, Chen Y, Zhang H, Jiang M. Comparison of clinical efficacy of artificial femoral head replacement and total hip replacement in the treatment of femoral neck fracture in the elderly. Minerva Surg. 2021;76:484–485. doi: 10.23736/S2724-5691.21.08868-7. [DOI] [PubMed] [Google Scholar]
- 3.Lewis SR, Macey R, Parker MJ, Cook JA, Griffin XL. Arthroplasties for hip fracture in adults. Cochrane Database Syst Rev. 2022;2:CD013410. doi: 10.1002/14651858.CD013410.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varnum C, Pedersen AB, Rolfson O, Rogmark C, Furnes O, Hallan G, Mäkelä K, de Steiger R, Porter M, Overgaard S. Impact of hip arthroplasty registers on orthopaedic practice and perspectives for the future. EFORT Open Rev. 2019;4:368–376. doi: 10.1302/2058-5241.4.180091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khanuja HS, Mekkawy KL, MacMahon A, McDaniel CM, Allen DA, Moskal JT. Revisiting cemented femoral fixation in hip arthroplasty. J Bone Joint Surg Am. 2022;104:1024–1033. doi: 10.2106/JBJS.21.00853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hines CB. Understanding bone cement implantation syndrome. AANA J. 2018;86:433–441. [PubMed] [Google Scholar]
- 7.Weingärtner K, Störmann P, Schramm D, Wutzler S, Zacharowski K, Marzi I, Lustenberger T. Bone cement implantation syndrome in cemented hip hemiarthroplasty-a persistent risk. Eur J Trauma Emerg Surg. 2022;48:721–729. doi: 10.1007/s00068-020-01587-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prokop A, Hägele M, Pfeilsticker U, Koll S, Chmielnicki M. Pericardial perforation 2.5 years after kyphoplasty. A rare complication after cement extravasation. Unfallchirurg. 2013;116:80–84. doi: 10.1007/s00113-011-2136-1. [DOI] [PubMed] [Google Scholar]
- 9.Mattis T, Knox M, Mammen L. Intracardiac methylmethacrylate embolism resulting in right atrial wall perforation and pericarditis following percutaneous vertebroplasty. J Vasc Interv Radiol. 2012;23:719–720. doi: 10.1016/j.jvir.2011.12.027. [DOI] [PubMed] [Google Scholar]
- 10.Son KH, Chung JH, Sun K, Son HS. Cardiac perforation and tricuspid regurgitation as a complication of percutaneous vertebroplasty. Eur J Cardiothorac Surg. 2008;33:508–509. doi: 10.1016/j.ejcts.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 11.Grifka RG, Tapio J, Lee KJ. Transcatheter retrieval of an embolized methylmethacrylate glue fragment adherent to the right atrium using bidirectional snares. Catheter Cardiovasc Interv. 2013;81:648–650. doi: 10.1002/ccd.24333. [DOI] [PubMed] [Google Scholar]
- 12.Kim HT, Kim YN, Shin HW, Kim IC, Kim H, Park NH, Choi SY. Intracardiac foreign body caused by cement leakage as a late complication of percutaneous vertebroplasty. Korean J Intern Med. 2013;28:247–250. doi: 10.3904/kjim.2013.28.2.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pannirselvam V, Hee HT. Asymptomatic cement embolism in the right atrium after vertebroplasty using high-viscosity cement: a case report. J Orthop Surg (Hong Kong) 2014;22:244–247. doi: 10.1177/230949901402200228. [DOI] [PubMed] [Google Scholar]
- 14.Lee V, Patel R, Meier P, Lawrence D, Roberts N. Conservative management of inferior vena cava cement spike after percutaneous vertebroplasty causes fatal cardiac tamponade. J Rheumatol. 2014;41:141–142. doi: 10.3899/jrheum.130570. [DOI] [PubMed] [Google Scholar]
- 15.Park JH, Choo SJ, Park SW. Images in cardiovascular medicine. Acute pericarditis caused by acrylic bone cement after percutaneous vertebroplasty. Circulation. 2005;111:e98. doi: 10.1161/01.CIR.0000155502.90653.A5. [DOI] [PubMed] [Google Scholar]
- 16.Farahvar A, Dubensky D, Bakos R. Perforation of the right cardiac ventricular wall by polymethylmethacrylate after lumbar kyphoplasty. J Neurosurg Spine. 2009;11:487–491. doi: 10.3171/2009.5.SPINE08517. [DOI] [PubMed] [Google Scholar]
- 17.Kim SY, Seo JB, Do KH, Lee JS, Song KS, Lim TH. Cardiac perforation caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJR Am J Roentgenol. 2005;185:1245–1247. doi: 10.2214/AJR.04.1443. [DOI] [PubMed] [Google Scholar]
- 18.Lim KJ, Yoon SZ, Jeon YS, Bahk JH, Kim CS, Lee JH, Ha JW. An intraatrial thrombus and pulmonary thromboembolism as a late complication of percutaneous vertebroplasty. Anesth Analg. 2007;104:924–926. doi: 10.1213/01.ane.0000256974.84535.7a. [DOI] [PubMed] [Google Scholar]
- 19.Sun K, Huang F, Liang B. A case report of intracardiac bone cement embolization after posterior decompression and cement-enhanced pedicle screw fixation for osteoporosis and lumbar degeneration. Medicine (Baltimore) 2022;101:e28826. doi: 10.1097/MD.0000000000028826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krithika R, Geske JB, Villarraga HR, Crestanello J. Concrete proof of Murphy’s law: a case report of intracardiac cement embolization. Eur Heart J Case Rep. 2022;6:ytac386. doi: 10.1093/ehjcr/ytac386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim YJ, Lee JW, Park KW, Yeom JS, Jeong HS, Park JM, Kang HS. Pulmonary cement embolism after percutaneous vertebroplasty in osteoporotic vertebral compression fractures: incidence, characteristics, and risk factors. Radiology. 2009;251:250–259. doi: 10.1148/radiol.2511080854. [DOI] [PubMed] [Google Scholar]
- 22.Fadili Hassani S, Cormier E, Shotar E, Drir M, Spano JP, Morardet L, Collet JP, Chiras J, Clarençon F. Intracardiac cement embolism during percutaneous vertebroplasty: incidence, risk factors and clinical management. Eur Radiol. 2019;29:663–673. doi: 10.1007/s00330-018-5647-0. [DOI] [PubMed] [Google Scholar]
- 23.Zhang L, Wang J, Feng X, Tao Y, Yang J, Wang Y, Zhang S, Cai J, Huang J. A comparison of high viscosity bone cement and low viscosity bone cement vertebroplasty for severe osteoporotic vertebral compression fractures. Clin Neurol Neurosurg. 2015;129:10–16. doi: 10.1016/j.clineuro.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 24.Hatzantonis C, Czyz M, Pyzik R, Boszczyk BM. Intracardiac bone cement embolism as a complication of vertebroplasty: management strategy. Eur Spine J. 2017;26:3199–3205. doi: 10.1007/s00586-016-4695-x. [DOI] [PubMed] [Google Scholar]
- 25.Baek IH, Park HY, Kim KW, Jang TY, Lee JS. Paraplegia due to intradural cement leakage after vertebroplasty: a case report and literature review. BMC Musculoskelet Disord. 2021;22:741. doi: 10.1186/s12891-021-04625-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dash A, Brinster DR. Open heart surgery for removal of polymethylmethacrylate after percutaneous vertebroplasty. Ann Thorac Surg. 2011;91:276–278. doi: 10.1016/j.athoracsur.2010.06.106. [DOI] [PubMed] [Google Scholar]
- 27.Arnáiz-García ME, Dalmau-Sorlí MJ, González-Santos JM. Massive cement pulmonary embolism during percutaneous vertebroplasty. Heart. 2014;100:600. doi: 10.1136/heartjnl-2013-304583. [DOI] [PubMed] [Google Scholar]
- 28.Caynak B, Onan B, Sagbas E, Duran C, Akpinar B. Cardiac tamponade and pulmonary embolism as a complication of percutaneous vertebroplasty. Ann Thorac Surg. 2009;87:299–301. doi: 10.1016/j.athoracsur.2008.05.074. [DOI] [PubMed] [Google Scholar]
- 29.Gosev I, Nascimben L, Huang PH, Mauri L, Steigner M, Mizuguchi A, Shah AM, Aranki SF. Right ventricular perforation and pulmonary embolism with polymethylmethacrylate cement after percutaneous kyphoplasty. Circulation. 2013;127:1251–1253. doi: 10.1161/CIRCULATIONAHA.112.144535. [DOI] [PubMed] [Google Scholar]
- 30.Moon MH, Jo KH, Kim HW. Cardiac perforation caused by bone cement embolism. Arch Cardiovasc Dis. 2013;106:413–414. doi: 10.1016/j.acvd.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 31.Tran I, Gerckens U, Remig J, Zintl G, Textor J. First report of a life-threatening cardiac complication after percutaneous balloon kyphoplasty. Spine (Phila Pa 1976) 2013;38:E316–318. doi: 10.1097/BRS.0b013e318281507a. [DOI] [PubMed] [Google Scholar]
- 32.Bose R, Choi JW. Successful percutaneous retrieval of methyl methacrylate orthopedic cement embolism from the pulmonary artery. Catheter Cardiovasc Interv. 2010;76:198–201. doi: 10.1002/ccd.22496. [DOI] [PubMed] [Google Scholar]
- 33.Braiteh F, Row M. Right ventricular acrylic cement embolism: late complication of percutaneous vertebroplasty. Heart. 2009;95:275. doi: 10.1136/hrt.2008.158790. [DOI] [PubMed] [Google Scholar]
- 34.Yin P, Hu J, Wang S, Sui G, Yuan G, Fan D. Bedside echocardiography for diagnosis of intracardiac cement embolism after percutaneous vertebroplasty: a case report. J Card Surg. 2021;36:3929–3932. doi: 10.1111/jocs.15830. [DOI] [PubMed] [Google Scholar]
- 35.Weininger G, Sekar RB, Elefteriades JA. Intracardiac polymethylmethacrylate cement embolism. JTCVS Tech. 2021;10:358–360. doi: 10.1016/j.xjtc.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Audat ZA, Alfawareh MD, Darwish FT, Alomari AA. Intracardiac leakage of cement during kyphoplasty and vertebroplasty: a case report. Am J Case Rep. 2016;17:326–330. doi: 10.12659/AJCR.897719. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


