Abstract
Introduction
Disability and HIV are intricately linked, as people with disabilities are at higher risk of contracting HIV, and living with HIV can lead to impairments and disability. Despite this well‐established relationship, there remains limited internationally comparable evidence on HIV knowledge and access to testing for people with disabilities.
Methods
We used cross‐sectional data from 37 Multiple Indicator Cluster Surveys. Surveys were from six UNICEF regions, including East Asia and Pacific (n = 6), East and Central Asia (n = 7), Latin America and the Caribbean (n = 6), Middle East and North Africa (n = 4), South Asia (n = 2) and sub‐Saharan Africa (n = 12). A total of 513,252 people were eligible for inclusion, including 24,695 (4.8%) people with disabilities. We examined risk ratios and 95% confidence intervals for key indicators on HIV knowledge and access to testing for people with disabilities by sex and country. We also conducted a meta‐analysis to get a pooled estimate for each sex and indicator.
Results
Men and women with disabilities were less likely to have comprehensive knowledge about HIV prevention (aRR: 0.74 [0.67, 0.81] and 0.75 [0.69, 0.83], respectively) and to know of a place to be tested for HIV (aRR: 0.95 [0.92, 0.99] and 0.94 [0.92, 0.97], respectively) compared to men and women without disabilities. Women with disabilities were also less likely to know how to prevent mother‐to‐child transmission (aRR: 0.87 [0.81, 0.93]) and ever have been tested for HIV (aRR: 0.90 [0.85, 0.94]).
Conclusions
Men and women with disabilities have lower overall HIV knowledge and in particular women with disabilities also indicate lower testing rates. Governments must include people with disabilities in HIV programmes by improving disability‐inclusion and accessibility to HIV‐related information, education and healthcare services.
Keywords: HIV testing, HIV knowledge, disability, health equity, accessibility, people with disabilities
1. INTRODUCTION
Globally, there are 1.3 billion people with disabilities [1]. There is a close relationship between HIV and disability, as research suggests that people with disabilities are at higher risk of contracting HIV (e.g. due to poverty, exclusion and discrimination) and HIV can lead to impairments and disability (e.g. due to direct effect of the virus, opportunistic infections or exclusion, and discrimination) [2, 3, 4]. While HIV control efforts have centred around expanding access to prevention, testing and treatment, these programmes often fail to consider accessibility for people with disabilities and people living with HIV who develop disabling conditions [4, 5]. People with disabilities experience poorer health, on average, including a higher prevalence of communicable diseases, such as acute respiratory infection, sexually transmitted infections, diarrhoeal disease and tuberculosis [6, 7, 8, 9]. People with disabilities also face barriers in accessing healthcare, and these are amplified for HIV care by a lack of knowledge and accessible information about HIV, lack of access to sexuality education; cultural beliefs around disability and HIV; lack of affordable, accessible, acceptable and quality HIV care; and health workers’ beliefs that people with disabilities are asexual [10, 11, 12, 13, 14].
Data on HIV knowledge among people with disabilities vary across surveys [15, 16, 17, 18]. While early disability‐focused studies suggested that people with disabilities had lower knowledge about HIV [2, 19, 20, 21, 22], recent studies using population‐based surveys show more diverse result. For instance, the 2017 HIV Impact Survey in Tanzania suggests that women with disabilities are more likely to know their HIV status [23]. In South Africa, the 2012 National HIV Prevalence, Incidence and Behavior surveys found that people with disabilities had less knowledge about HIV and were less likely to find testing sites [24]. Analysis of the 2011 Demographic Health Survey in Uganda showed equal knowledge of transmission for delivery and breastfeeding, but wide gaps in knowledge about HIV acquisition or transmission risk and misconceptions about HIV [18].
Beyond these data, indicators on HIV prevention, testing and treatment are rarely disaggregated by disability status in large‐scale household surveys and country surveillance data and internationally comparable data on disability and HIV data are lacking. Hence, the UNICEF‐supported Multiple Indicator Cluster Surveys (MICS) conducted across a large number of low‐ and middle‐income countries (LMICs) is an opportunity to assess the HIV knowledge and testing practices among people with disabilities. While the Disability Data Initiative reports suggest some differences in HIV knowledge or testing among women with disabilities, these reports only discuss descriptive statistics for women [25]. More country‐specific and sex‐disaggregated analysis is needed to further understand inequities.
This paper presents sex‐disaggregated, internationally comparable evidence on HIV knowledge and testing among adults 15−49 from the MICS conducted in 37 LMICs. The aim is to compare in access to knowledge about prevention between people with disabilities and those without disabilities in access to knowledge about prevention and testing for HIV by disability status. Efforts to improve access to knowledge, testing and treatment are central to UNAIDS 95‐95‐95 targets by 2030 and so these data provide evidence on how these efforts are reaching people with disabilities [3].
2. METHODS
This study is a secondary analysis of the MICS. We describe the methods used to conduct the MICS, as well as our methods to analyse the published datasets.
2.1. MICS programme methods
The MICS are cross‐sectional, population‐based survey conducted in LMICs. The MICS use a multi‐stage sampling approach to sample clusters of households selected from a previous national sample frame (i.e. census, national survey) to generate nationally representative data on indicators for tracking the Sustainable Development Goals, health and development [26, 27].
Trained data collectors conducted interviews with adults aged 15−49 living in the randomly selected households. All men and women aged 18−49 were eligible, while participants aged 15−17 may have been one of the children aged 5−17 randomly selected from the household roster. Data were collected for both individual women and men, where countries have opted‐in to including the individual men's questionnaire. Questions were standardized across countries, allowing comparisons across all the countries where MICS6 has been completed. We selected countries that had anonymized individual data on all variables of interest and were publicly available as of March 2023, though data were collected between 2017 and 2021.
2.2. Secondary analysis methods
This analysis focuses on the 37 countries where HIV and disability data were available for women (and a subset of 29 countries that had men's disability and the HIV questionnaire). Countries included in this study were geographically diverse, with 12 in sub‐Saharan Africa, 7 in East and Central Asia, 6 in Latin and Central America, 6 in East Asia and Pacific, 4 in Middle East and North Africa, and 2 in South Asia.
2.3. Exposure
Disability was measured in the child and adult functioning modules for adults 15−17 and 18−49, respectively. Both modules use the standardized definition of disability, as assessed by Washington Group Questions, which have been validated for use in the MICS across settings [28]. These questions assess the participants’ impairments based on their self‐reported level of functional difficulty in functional domains (Table 1). We defined disability as the highest two thresholds of impairment, including only those who answered “cannot do at all” or a “lot of difficulty” in at least one functional domain as disabled. However, it does mean our comparison group includes individuals who have reported “some” functional difficulty in one or more functional domains. This threshold of disability was selected in accordance with the Washington Group syntax, so that the indicators aligned with the UNICEF reports, and to preserve the specificity of the disability measure. Individuals without fully completed functioning modules were excluded from analysis, unless they had met the threshold for disability in one or more domains, since the missing data would not have impacted their disability status.
Table 1.
Definitions of HIV and disability indicators
| Indicators | MICS indicator | Definition |
|---|---|---|
| Comprehensive knowledge about HIV prevention | TM.29 | % of people who know of the two ways of HIV prevention (having only one monogamous, uninfected partner and using a condom every time), who know that a healthy‐looking person can be HIV positive and who reject the country‐specific two most common misconceptions about HIV transmission. |
| Knowledge of mother‐to‐child‐transmission (MTCT) | TM.30 | % of people who can identify that HIV can be transmitted from mother to child (during pregnancy, during delivery and by breastfeeding). |
| People who know where to get tested for HIV | TM.32 | % of people who know where they can get tested for HIV. |
| People who have ever been tested for HIV and know the results | TM.33 | % of people who report ever being tested for HIV and know the results of the most recent test. |
| People who have been tested for HIV in the last year and know the results | − | % of people who report being tested for HIV in the last 12 months and know the results of the most recent test. |
| Disability | − | % of adults aged 18−49 with functional difficulty as assessed by the Washington Group Short Set (“cannot do at all” or “a lot of difficulty” in at least one of the following domains: 1) seeing, 2) hearing, 3) walking, 4) remembering/concentrating, 5) self‐care, 6) communication) and adults 15−17 with functional difficulty as assessed by the Child Functioning Module (“cannot do at all” or “a lot of difficulty” in at least one of the following domains: 1) seeing, 2) hearing, 3) walking, 4) remembering, 5) concentrating, 6) self‐care, 7) making friends, 8) controlling behaviour, 9) accepting change, 10) learning, 11) communication or “daily” in either 12) anxiety, and 13) depression. |
2.4. Outcomes and co‐variates
Outcomes related to HIV knowledge and testing behaviour were measured through five indicators. We used the standard MICS definitions to calculate each outcome (Table 1 and Appendix S1). Responses were reported by the individual participants, and those unable to participate independently were recorded as “incapacitated” [29]. Not all countries included had all HIV indicators or data on both sexes, which is why we did not conduct an “overall” result that included both sexes. We adjusted the analysis by age (years), wealth quintile and residence area (urban vs. rural).
2.5. Statistical analysis
All analyses were completed using R 4.2.2. We described all outcomes, exposures, and covariates by country and overall. Continuous data were reported as mean (standard deviation [SD]), and categorical data were reported as numbers (percentage).
To estimate the relative inequities of each outcome between people with and without disabilities, we first modelled the probability of each outcome by sex and by country, using a modified Poisson model [30]. Results were reported as (adjusted) risk ratio (RR or aRR) and its 95% confidence interval (CI). The complex survey design and sample weights were also accounted for using the “survey” package in R [31]. We then pooled the country‐specific estimations by meta‐analysis with the inverted standard error as the weight. The heterogeneity of estimates across countries was assessed by Cochran's Q test [32]. For the presence of significant heterogeneity (p < 0.1), a random‐effect meta‐analysis was performed to pool the estimates, and for those where p > 0.1, a fixed‐effects meta‐analysis was conducted. We excluded cases with missing values instead of any imputation when we fitted the data for each outcome. To reduce the bias due to the small sample size, we excluded countries with fewer than 25 respondents with disabilities when we pooled the country‐specific estimations.
2.6. Ethical approval
The London School of Hygiene and Tropical Medicine Research Ethics Committee approved this project on the 9th of November 2020 (reference number: 22719). Before data collection begins, UNICEF also obtains ethical approval from each country's national Ethics Committee. Consent was obtained by MICS interviewers at the time of the survey and only participants who consent to have their data shared anonymously are made publicly available on the MICS website. We accessed the anonymized data from the MICS website in January 2023.
3. RESULTS
3.1. Overall sample
Our sample included 513,252 people across 37 countries, with sample sizes ranging from 1031 in Tuvalu to 57,585 in Bangladesh (Table 2). The overall prevalence of disability in the sample was 4.8% (n = 24,695), but the prevalence ranged from 0.8% of the sample in Turkmenistan (n = 58) to 10.8% in Central African Republic (n = 1235) and Costa Rica (n = 743). The overall sample was predominantly female (82.5%, n = 423,615) and there was a slightly larger proportion of rural participants (55.6%, n = 285,454).
Table 2.
Summary statistics of adults 15−49 included in the analysis overall and by country
| Country | Sample size | Prevalence of disability, n (%) | Urban, n (%) | Age, mean (SD) | Male, n (%) | Female, n (%) | Knowledge about HIV, n (%) | Knowledge about MTCT, n (%) | Know of a place to be tested for HIV, n (%) | Ever tested for HIV and know the results, n (%) | Tested for HIV in the last 12 months and know the results, n (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total sample | 513,252 | 24,695 (4.8) | 227,798 (44.4) | 31.46 (8.96) | 89,637 (17.5) | 423,615 (82.5) | 98,876 (20.0) | 132,846 (26.7) | 281,168 (56.5) | 175,159 (37.9) | 71,772 (26.0) |
| East Asia and Pacific | |||||||||||
| Fiji | 6827 | 206 (3.0) | 3849 (56.4) | 33.16 (8.87) | 2261 (33.1) | 4566 (66.9) | 2527 (37.0) | 1326 (19.4) | 4861 (71.3) | 2068 (30.5) | 439 (16.4) |
| Kiribati | 5669 | 297 (5.2) | 2402 (42.4) | 31.24 (8.86) | 1865 (32.9) | 3804 (67.1) | 2296 (40.5) | 1709 (30.2) | 4672 (82.4) | 557 (9.8) | 220 (9.7) |
| Mongolia | 13,898 | 1198 (8.6) | 7118 (51.2) | 34.31 (8.41) | 4032 (29.0) | 9866 (71.0) | a | 742 (5.3) | 8974 (64.6) | 7042 (50.9) | 3078 (29.1) |
| Samoa | 4696 | 77 (1.6) | 1478 (31.5) | 31.82 (9.49) | 1047 (22.3) | 3649 (77.7) | 409 (8.7) | 1118 (23.8) | 1368 (29.1) | 237 (5.1) | 87 (5.6) |
| Tonga | 3525 | 79 (2.2) | 991 (28.1) | 31.78 (9.37) | 1047 (29.7) | 2478 (70.3) | a | 897 (25.5) | 2030 (57.6) | 394 (11.2) | 136 (11.7) |
| Tuvalu | 1031 | 56 (5.4) | 663 (64.3) | 30.56 (8.39) | 270 (26.2) | 761 (73.8) | 248 (24.1) | 233 (22.6) | 669 (65.0) | 294 (28.6) | 82 (13.4) |
| East and Central Asia | |||||||||||
| Belarus | 7428 | 78 (1.1) | 5516 (74.3) | 33.91 (7.66) | 2167 (29.2) | 5261 (70.8) | 4103 (55.3) | 1541 (20.8) | 7313 (98.5) | 6592 (89.0) | 2440 (36.5) |
| Georgia | 8894 | 807 (9.1) | 4254 (47.8) | 34.47 (8.61) | 2467 (27.7) | 6427 (72.3) | 1220 (13.7) | 1859 (20.9) | 3974 (44.7) | 2031 (22.9) | 651 (22.2) |
| Kosovo | 8400 | 587 (7.0) | 3910 (46.5) | 32.49 (9.52) | 2383 (28.4) | 6017 (71.6) | 768 (9.1) | 1264 (15.1) | a | a | a |
| Kyrgyzstan | 5162 | 134 (2.6) | 2355 (45.6) | 33.07 (8.90) | a | 5162 (100.0) | a | 2434 (47.2) | 4506 (87.3) | 3929 (76.6) | 1104 (25.5) |
| Montenegro | 2848 | 36 (1.3) | 1720 (60.4) | 33.90 (8.57) | 751 (26.4) | 2097 (73.6) | 918 (32.3) | 692 (24.3) | 1731 (60.8) | 191 (6.7) | 37 (10.7) |
| Turkmenistan | 6959 | 58 (0.8) | 3631 (52.2) | 32.21 (8.74) | a | 6959 (100.0) | 2166 (31.1) | 1709 (24.6) | 4546 (65.4) | 1996 (29.1) | 677 (14.6) |
| Uzbekistan | 4385 | 289 (6.6) | 2146 (48.9) | 32.76 (8.63) | a | 4385 (100.0) | 726 (16.6) | 745 (17.0) | 2800 (63.9) | 2062 (47.6) | 807 (27.5) |
| Latin America and the Caribbean | |||||||||||
| Costa Rica | 6894 | 743 (10.8) | 4316 (62.6) | 31.99 (8.63) | a | 6894 (100.0) | 2098 (30.4) | 1250 (18.1) | 5743 (83.3) | 4234 (61.8) | 879 (19.1) |
| Cuba | 11,847 | 151 (1.3) | 8392 (70.8) | 33.17 (8.76) | 3453 (29.1) | 8394 (70.9) | 6708 (56.7) | 4213 (35.6) | 11,304 (95.4) | 10,014 (84.9) | 3510 (32.8) |
| Dominican Republic | 19,992 | 803 (4.0) | 13,905 (69.6) | 32.11 (9.16) | a | 19,992 (100.0) | 7616 (38.1) | 8846 (44.3) | 19,106 (95.6) | 16,778 (84.1) | 6361 (36.7) |
| Guyana | 7209 | 233 (3.2) | 2016 (28.0) | 31.77 (9.31) | 1962 (27.2) | 5247 (72.8) | 2679 (37.2) | 2419 (33.6) | 6465 (89.8) | 5021 (70.0) | 1973 (35.9) |
| Honduras | 23,893 | 1983 (8.3) | 9680 (40.5) | 31.28 (9.14) | 6776 (28.4) | 17,117 (71.6) | 4861 (20.3) | 8217 (34.4) | 17,272 (72.3) | 11,733 (49.3) | 3008 (21.3) |
| Suriname | 8649 | 459 (5.3) | 5966 (69.0) | 32.25 (9.01) | 2420 (28.0) | 6229 (72.0) | 3327 (38.5) | 2926 (33.9) | 7357 (85.1) | 5454 (63.3) | 1984 (31.9) |
| Middle East and North Africa | |||||||||||
| Algeria | 31,368 | 1444 (4.6) | 21,152 (67.4) | 32.62 (8.95) | a | 31,368 (100.0) | a | 5255 (16.8) | 8037 (25.7) | 3035 (9.7) | 915 (8.7) |
| Iraq | 26,724 | 1338 (5.0) | 17912 (67.0) | 31.20 (9.07) | a | 26,724 (100.0) | 1314 (4.9) | 2257 (8.4) | 3854 (14.4) | 1218 (4.6) | 358 (2.5) |
| Palestine | 9777 | 221 (2.3) | 5800 (59.3) | 30.73 (8.93) | a | 9777 (100.0) | 631 (6.5) | 1286 (13.2) | a | a | a |
| Tunisia | 11,993 | 908 (7.6) | 7949 (66.3) | 33.31 (9.04) | 2232 (18.6) | 9761 (81.4) | 1695 (14.1) | 1989 (16.6) | 3421 (28.5) | 336 (2.8) | 96 (4.6) |
| South Asia | |||||||||||
| Bangladesh | 57,585 | 1773 (3.1) | 11,791 (20.5) | 31.59 (8.87) | a | 57,585 (100.0) | 5067 (8.8) | 5912 (10.3) | 9443 (16.4) | a | a |
| Nepal | 18,166 | 362 (2.0) | 10,716 (59.0) | 31.04 (8.74) | 4853 (26.7) | 13,313 (73.3) | 3781 (20.8) | 2371 (13.1) | 10,467 (57.6) | 2676 (14.8) | 640 (9.5) |
| Sub‐Saharan Africa | |||||||||||
| Central African Republic | 11,462 | 1235 (10.8) | 5052 (44.1) | 30.05 (8.64) | 3357 (29.3) | 8105 (70.7) | 1717 (15.0) | 3880 (33.9) | 6761 (59.0) | 4721 (41.3) | 2143 (28.5) |
| Chad | 24,931 | 1294 (5.2) | 5502 (22.1) | 29.96 (8.66) | 5661 (22.7) | 19,270 (77.3) | 4783 (19.2) | 8387 (39.8) | 13,265 (53.3) | 6244 (25.2) | 2771 (25.5) |
| Democratic Republic of Congo | 24,160 | 953 (3.9) | 7836 (32.4) | 30.17 (8.70) | 5187 (21.5) | 18,973 (78.5) | 4209 (17.4) | 4971 (20.6) | 11,455 (47.4) | 5033 (20.9) | 2122 (22.5) |
| Gambia | 15,520 | 470 (3.0) | 7929 (51.1) | 30.06 (8.53) | 3743 (24.1) | 11,777 (75.9) | 3678 (23.7) | 6502 (41.9) | 11,228 (72.4) | 6439 (41.6) | 2165 (31.3) |
| Ghana | 16,821 | 1355 (8.1) | 8111 (48.2) | 31.17 (9.31) | 4305 (25.6) | 12,516 (74.4) | 2792 (16.6) | 6894 (41.0) | 11,862 (70.5) | 6832 (40.7) | 2340 (26.7) |
| Guinea Bissau | 11,992 | 252 (2.1) | 4078 (34.0) | 30.03 (8.62) | 2391 (19.9) | 9601 (80.1) | 1606 (13.4) | 5022 (41.9) | 6299 (52.5) | 3824 (31.9) | 1256 (23.4) |
| Madagascar | 21,333 | 1608 (7.5) | 6029 (28.3) | 30.27 (9.08) | 6467 (30.3) | 14,866 (69.7) | 4754 (22.3) | 4459 (20.9) | 7236 (33.9) | 2512 (11.8) | 665 (6.9) |
| Malawi | 26,724 | 1523 (5.7) | 4428 (16.6) | 30.21 (8.89) | 5610 (21.0) | 21,114 (79.0) | 11,366 (42.6) | 16,159 (60.5) | 26,236 (98.2) | 24,555 (91.9) | 15,565 (62.3) |
| Sao Tome and Principe | 3794 | 268 (7.1) | 2177 (57.4) | 31.23 (8.98) | 1159 (30.5) | 2635 (69.5) | 1448 (38.2) | 914 (24.1) | 3560 (93.9) | 3043 (80.7) | 1651 (50.9) |
| Sierra Leone | 21,999 | 286 (1.3) | 8678 (39.4) | 30.33 (8.75) | 6371 (29.0) | 15,628 (71.0) | 5298 (24.1) | 8458 (38.5) | 14,509 (66.0) | 8060 (36.8) | 2262 (17.0) |
| Togo | 8367 | 629 (7.5) | 3478 (41.6) | 31.37 (8.74) | 1959 (23.4) | 6408 (76.6) | 2067 (24.7) | 3990 (47.7) | 6719 (80.3) | 4925 (58.9) | 1730 (30.6) |
| Zimbabwe | 12,330 | 502 (4.1) | 4872 (39.5) | 31.27 (8.96) | 3441 (27.9) | 8889 (72.1) | a | a | 12,125 (98.3) | 11,079 (89.9) | 7620 (67.7) |
Country did not have data available.
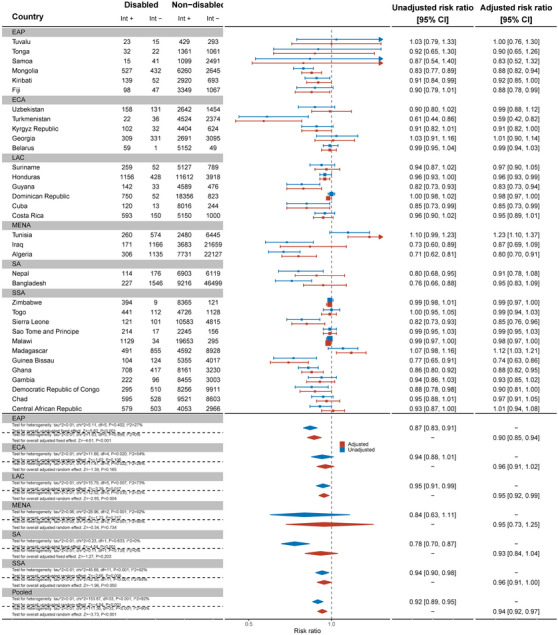
3.2. Comprehensive knowledge about HIV prevention
Thirty‐two countries reported data on comprehensive knowledge about HIV prevention in women (Figure 1). Overall, the pooled showed that women with disabilities have significantly lower knowledge about HIV prevention than women without disabilities (aRR: 0.75, 95% C.I.: 0.69, 0.93). For example, no women with disabilities in Samoa had comprehensive knowledge of HIV prevention and, in Sierra Leone, women with disabilities were less likely to have comprehensive HIV knowledge than women without disabilities (aRR: 0.33, 95% C.I.: 0.20, 0.57). Bangladesh (aRR: 0.55, 95% C.I.: 0.42, 0.72), Belarus (aRR: 0.51, 95% C.I.: 0.31, 0.84), Chad (aRR: 0.61, 95% C.I.: 0.50, 0.75), Democratic Republic of Congo (aRR: 0.47, 95% C.I.: 0.34, 0.66) and Kosovo (aRR: 0.47, 95% C.I.: 0.28, 0.79) also had evidence of substantial relative inequities for women with disabilities. In Tuvalu, however, women with disabilities had more knowledge about HIV prevention than women without disabilities (aRR: 1.62, 95% C.I.: 1.05, 2.49).
Figure 1.
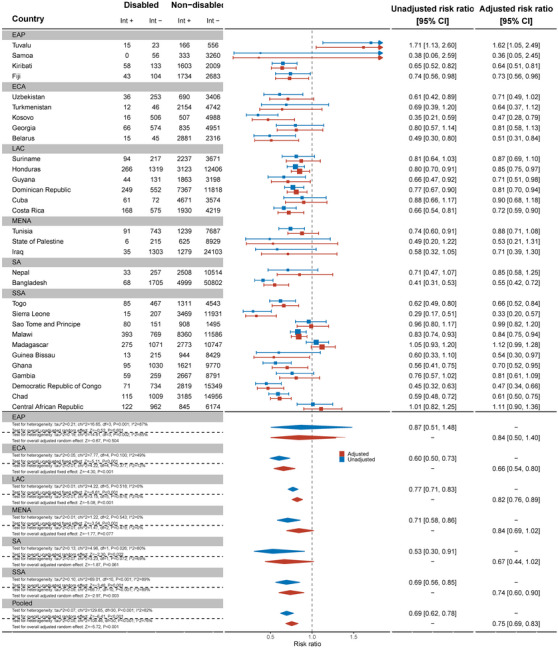
Meta‐analysis comparing comprehensive knowledge about HIV prevention among women with disabilities compared to women without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
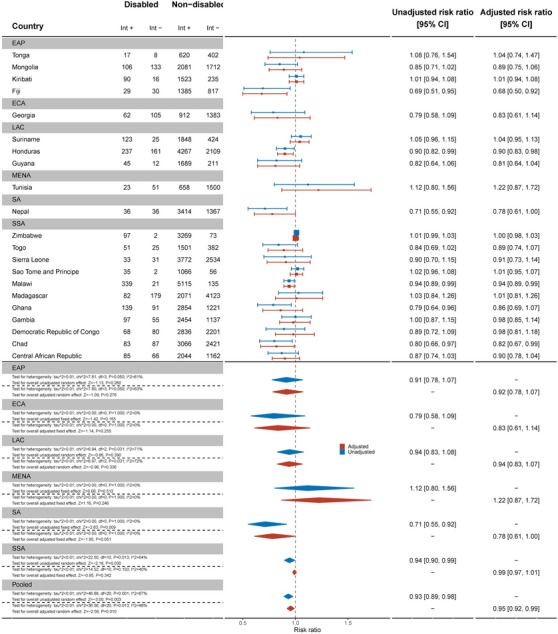
Nineteen countries reported data on comprehensive HIV knowledge for men (Figure 2). Men with disabilities were significantly less likely to have comprehensive knowledge of HIV prevention than men without disabilities (aRR: 0.74, 95% C.I.: 0.67, 0.81). This difference was most pronounced in Ghana (aRR: 0.46, 95% C.I.: 0.27, 0.78) and Chad (aRR: 0.53, 95% C.I.: 0.33, 0.84). Most countries had smaller sample sizes and wider confidence intervals.
Figure 2.
Meta‐analysis comparing comprehensive knowledge about HIV prevention among men with disabilities compared to men without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
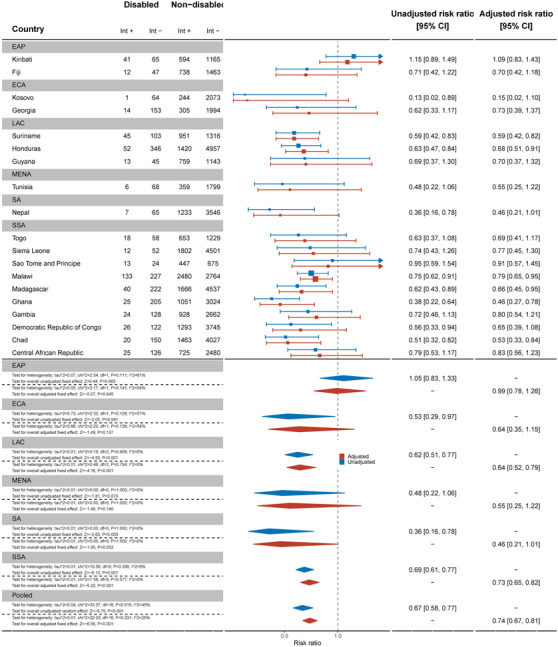
3.3. Knowledge of mother‐to‐child transmission
Women with disabilities were less likely to have knowledge of mother‐to‐child transmission (MTCT) than women without disabilities for the pooled sample of 37 countries (aRR: 0.87, 95% C.I.: 0.81, 0.93) (Figure 3). Palestine (aRR: 0.39, 95% C.I.: 0.21, 0.72), Kyrgyzstan (aRR: 0.60, 95% C.I.: 0.44, 0.82) and Sierra Leone (aRR: 0.59, 95% C.I.: 0.46, 0.77) had the most marked differences between women with and without disabilities, while most other countries had wide confidence intervals and uncertain results. Conversely, women with disabilities were more likely to have knowledge of MTCT in Madagascar (aRR: 1.31, 95% C.I.: 1.16, 1.47).
Figure 3.
Meta‐analysis comparing knowledge of mother‐to‐child transmission among women with disabilities compared to women without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
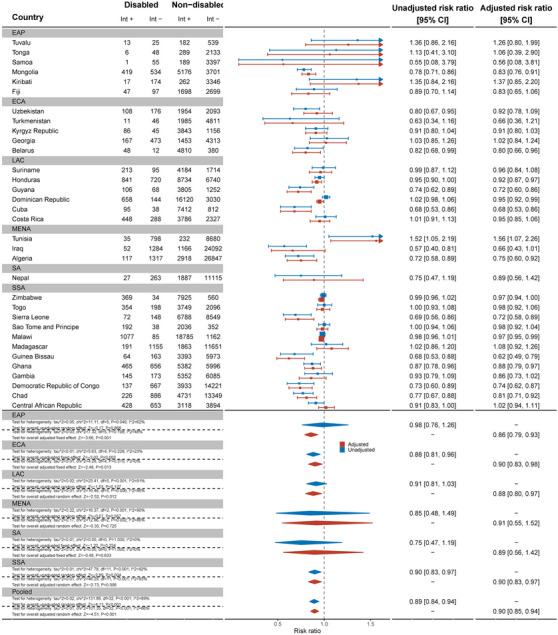
By contrast, across 21 countries, there was no evidence that men with disabilities had less knowledge about MTCT than men without disabilities (Figure 4). Exceptions were Malawi (aRR: 0.77, 95% C.I.: 0.65, 0.93) and Suriname (aRR: 0.62, 95% C.I.: 0.40, 0.96), where men with disabilities were less likely to have MTCT knowledge.
Figure 4.
Meta‐analysis comparing knowledge of mother‐to‐child transmission among men with disabilities compared to men without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
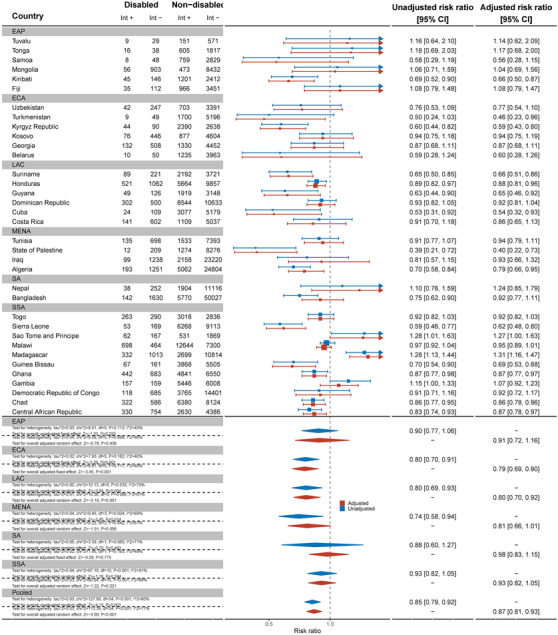
3.4. People who know where to be tested for HIV
Data from 32 countries suggested that women with disabilities were less likely to know where to be tested for HIV than women without disabilities (aRR: 0.94, 95% C.I.: 0.92, 0.97) (Figure 5). This difference was most substantial in Turkmenistan (aRR: 0.59, 95% C.I.: 0.42, 0.82). In contrast, in Tunisia (aRR: 1.23, 95% C.I.: 1.10, 1.37) and Madagascar (aRR: 1.12, 95% C.I.: 1.03, 1.21), women with disabilities were more likely to know where to be tested for HIV than women without disabilities. Results for men, across 21 countries, also showed men with disabilities were less likely to know where to get tested for HIV than men without disabilities (aRR: 0.95, 95% C.I.: 0.92, 0.99) (Figure 6).
Figure 5.
Meta‐analysis of women with disabilities who know of a place to be tested for HIV compared to women without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
Figure 6.
Meta‐analysis of men with disabilities who know of a place to be tested for HIV compared to men without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
3.5. People who have ever been tested for HIV and know the results
Across 32 countries, women with disabilities were less likely to have ever been tested and know their results for HIV than women without disabilities (aRR: 0.90, 95% C.I.: 0.85, 0.94) (Figure 7). This difference was most pronounced in Guinea‐Bissau (aRR: 0.62, 95% C.I.: 0.49, 0.79). Most countries showed strong evidence of relative inequities. However, in Tunisia, women with disabilities were more likely to have ever been tested for HIV than women without disabilities (aRR: 1.57, 95% C.I.: 1.07, 2.26).
Figure 7.
Meta‐analysis of women with disabilities who have ever been tested for HIV and know the results compared to women without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
Men with disabilities were not less likely to have ever been tested for HIV and know their results (aRR: 0.94, 95% C.I.: 0.86, 1.03) (Figure 8). Most countries showed no difference between men with and without disabilities, except in Fiji (aRR: 0.20, 95% C.I.: 0.06, 0.65) and Georgia (aRR: 0.57, 95% C.I.: 0.34, 0.95). As for women, men with disabilities in Tunisia were found to be more likely to have ever been tested for HIV and know their results (aRR: 2.81, 95% C.I.: 1.17, 6.72).
Figure 8.

Meta‐analysis of men with disabilities who have ever been tested for HIV and know the results compared to men without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
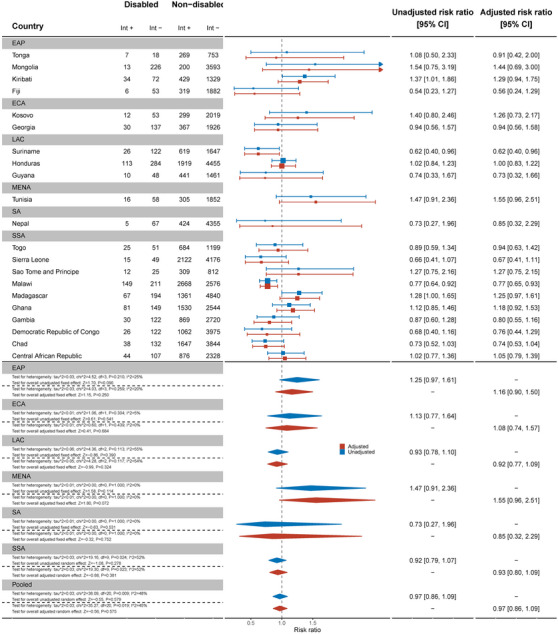
3.6. People who have been tested for HIV in the past 12 months and know the results
There was some evidence women with disabilities were less likely to have been tested for HIV in the past 12 months and know the results compared to women without disabilities (aRR: 0.95, 95% C.I.: 0.90, 1.02) (Figure 9). There was evidence that women with disabilities were less likely to be tested and know the results in the past 12 months in Algeria (aRR: 0.51, 95% C.I.: 0.32, 0.83), Chad (aRR: 0.72, 95% C.I.: 0.57, 0.90) and Mongolia (aRR: 0.76, 95% C.I.: 0.62, 0.93).
Figure 9.
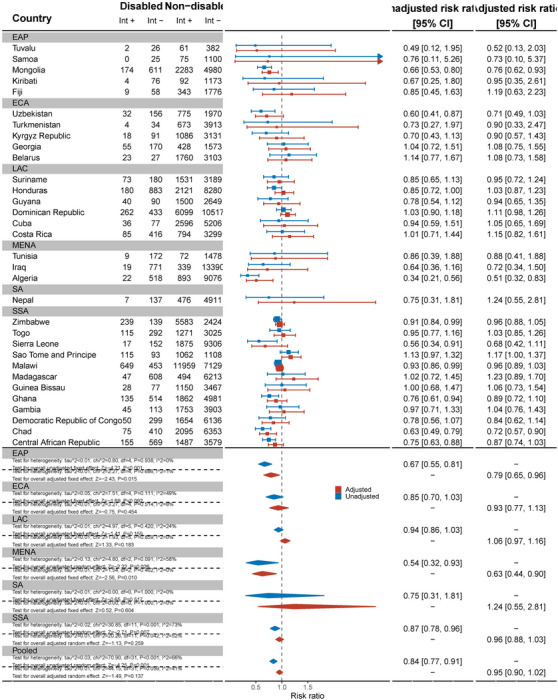
Meta‐analysis of women with disabilities who have been tested for HIV in the last 12 months and know the results compared to women without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
Across 17 countries, men with disabilities were no less likely to have been tested and know the results of the test in the last 12 months than men without disabilities (aRR: 1.02, 95% C.I.: 0.87, 1.20) (Figure 10). This differed in Mongolia, where men with disabilities were less likely to have been tested (aRR: 0.51, 95% C.I.: 0.27, 0.96), while in Suriname (aRR: 1.74, 95% C.I.: 1.28, 2.36) and Togo (aRR: 1.59, 95% C.I.: 1.02, 2.47), men with disabilities were more likely to have been tested in the past 12 months and know the results.
Figure 10.
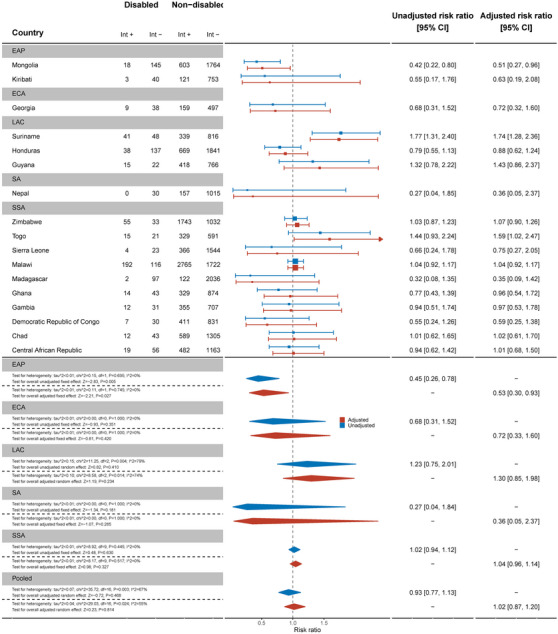
Meta‐analysis of men with disabilities who have been tested for HIV in the last 12 months and know the results compared to men without disabilities. Int +, number of people with the indicator; Int−, number of people without the indicator; EAP, East Asia Pacific; ECA, East and Central Asia; LAC, Latin America and Caribbean; MENA, Middle East and North Africa; SA, South Asia; SSA, sub‐Saharan Africa.
4. DISCUSSION
This study is the largest body of evidence on the HIV knowledge and testing gap for people with disabilities in 37 countries to date. Our findings suggest that women with disabilities are less likely to have comprehensive knowledge about HIV prevention, knowledge of MTCT, know where to be tested for HIV, and have ever been tested for HIV and know the results compared to women without disabilities. Men with disabilities were less likely to have comprehensive knowledge about HIV prevention and know of a place to be tested. There was limited evidence that men with disabilities were less likely to have ever been tested for HIV and that women with disabilities had been tested for HIV in the past 12 months and know the results. By contrast, our overall estimates found no differences in having been tested for HIV in the past 12 months and know the result and knowledge of MTCT for men. However, this estimate varied substantially by country and was impacted by small sample sizes, which may explain the result, rather than improved knowledge or access to testing.
These findings are largely consistent with the existing literature that highlight the gaps in HIV knowledge and testing for people with disabilities. For example, these results are similar to studies in South Africa that showed people with disabilities have less knowledge about HIV and testing sites [24], as well as Demographic and Health Survey data from Uganda that showed gaps in transmission [18]. However, these results present an overall picture for people with disabilities, rather than the sex‐disaggregated results included in this study. Therefore, this novel analysis suggests a gap between men and women with disabilities and showcases the “double disadvantage” women with disabilities experience based on gender and disability. Across all five indicators, women had at least some evidence they were less likely to have knowledge about HIV and access to testing than women without disabilities, whereas this was only the case for two indicators for men. Importantly, this difference was most pronounced for knowledge about MTCT, since there was significantly less knowledge among women with disabilities compared to women without, but no differences among men with and without disabilities. This information is important for all women of childbearing age, but particularly populations where there is a higher prevalence of HIV, including among those with disabilities. This knowledge gap will not only hamper women with disabilities ability to prevent MTCT among their children, but also make the global goal of eliminating MTCT impossible. These gaps are significant, but unsurprising, due to people with disabilities’ exclusion from HIV policies and programmes, comprehensive sexuality education and inaccessible information about HIV [4, 13].
While some of our results showed small relative differences and, therefore, suggest it may be possible to reduce these inequities, these results still emphasize and reinforce the concern that Global AIDS targets will not be met without more efforts to include people with disabilities in HIV programmes [3]. Efforts are, therefore, needed to reach people with disabilities who may be left behind in existing HIV programmes. Health systems can address these gaps by going beyond mentioning disability in their HIV policies, and, instead, integrating specific considerations into their programmes and national plans [4], and across each building block of the health system. To develop these plans fully, governments should look at their leadership, governance and financing structures to ensure people with disabilities involved in the development of HIV plans and specific budget item lines to address disability inclusion. Efforts should focus on improving the accessibility of sexuality education and HIV services for people with disabilities through ensuring physical and communication access of the facility and information material. Training health workers about disability (including destigmatizing disability and sexual activity) and ensuring public helath and patient information about HIV are available in accessible formats can further improve the quality of these services.
Finally, there needs to have more comparable data on disability within routine HIV surveys as well as other national and household surveys that look at HIV prevalence, knowledge and testing. Routine data on the prevalence of HIV among this population will help to monitor efforts to close gaps, as well as further elucidate the relationship between HIV and disability, and disaggregate further by other vulnerabilities (e.g. education, violence and social isolation). Indeed, analysis of the Demographic Health Survey in South Africa shows that women with disabilities, who were also living with HIV, were four times as likely to experience intimate partner violence than those without disabilities and HIV [33]. Together, these efforts will improve knowledge and testing among people with disabilities and so close the gaps. Good practice examples exist already of disability‐inclusion in HIV services, such as in Jamacia, where HIV‐focused civil society organizations are collaborating with organizations of persons with disabilities to reach people with disabilities [34], and South Africa, where health workers are being trained about disability and HIV [35], but these need to be scaled further.
4.1. Strengths and limitations
This analysis is the largest examining HIV knowledge and testing by disability status. It allows cross‐country comparison, providing new evidence from countries outside of sub‐Saharan Africa, while also furthering the breadth of evidence in disability‐based HIV knowledge and testing inequities in this region. Disaggregation of data by sex also allows us to examine the inequities by disability and sex, which revealed greater absolute inequities for women with disabilities. Given the global focus on improving gender‐based inequities, this analysis provides important evidence on these gaps and how women with disabilities need to be further included in gender‐targeted programmes. Combining this information with other studies also calls for more nuanced research to understand which people with disabilities are left behind and how this intersects with gender, age and mitigating factors (poverty, isolation, education and exposure to violence).
However, this analysis was limited by the definition of disability used in the MICS, which results in a lower prevalence than is estimated globally, and our analysis which focused only on people with at least a lot of difficulties in one domain. In addition, the Washington Group Short Set used for people aged 18−49 omit the full experience of disability, particularly those with psychosocial, intellectual, neurological, developmental and upper limb‐based disabilities [36]. As these are cross‐sectional surveys that do not test the onset of functional limitations, we also cannot understand if the individuals identified as having “disabilities” are those with preexisting disabilities or acquired because of HIV disease progression. Additionally, since the interview guide recommends only including people who can respond for themselves, it limits the level of functional difficulty captured in the survey. In particular, people with hearing or intellectual impairments may have been excluded. This bias may limit the applicability of our findings to those with only moderate functional limitations, rather than all people with disabilities, particularly those most likely to be excluded from HIV information and testing. Furthermore, the men's dataset is not only run in fewer countries, but also has a lower response rate (70−80% compared to the women's 90−95%). This, on top of the possible accessibility barriers to participating, introduces some non‐response bias. Finally, we were limited by the covariates and outcomes we examined, particularly since there was no MICS estimate of HIV prevalence, a limited definition of HIV prevention knowledge (i.e. excluding other important prevention tools, such as pre‐exposure prophylaxis) and small sample sizes for some indicators.
5. CONCLUSIONS
Overall, this study provides new data on the lower HIV knowledge and testing for people with disabilities. Without concerted efforts to reach people with disabilities in HIV programmes, we will not be able to achieve the global goals for HIV [3], and will leave those at most risk behind. With more data revealing these inequities, the gaps for people with disabilities are now well‐understood and require urgent action to address.
COMPETING INTERESTS
The authors declare no competing interests.
AUTHORS’ CONTRIBUTIONS
SR conceived the study and wrote the first draft, SC conducted the analysis, JH‐H, LMB, CD and HK edited the manuscript and provided crucial feedback on drafts.
FUNDING
This study was funded by the Programme for Evidence to Inform Disability Action (PENDA) grant from the UK Foreign, Commonwealth and Development Office. SR is funded by the Rhodes Trust. HK is funded by an NIHR Global Research Professorship. LMB is funded by the Arts and Humanities Research Council (AHRC, AH/X009580/1). Funders were not involved in the study design, data collection, analysis, decision to publish or preparation of the manuscript.
Supporting information
Supporting Information
ACKNOWLEDGEMENTS
We thank the participants who participated in the MICS surveys and the survey teams in each country.
DATA AVAILABILITY STATEMENT
MICS data are publicly available on the UNICEF website.
REFERENCES
- 1. World Health Organization . Global report on health equity for persons with disabilities. Geneva: World Health Organization; 2022. [Google Scholar]
- 2. De Beaudrap P, Mac‐Seing M, Pasquier E. Disability and HIV: a systematic review and a meta‐analysis of the risk of HIV infection among adults with disabilities in sub‐Saharan Africa. AIDS Care. 2014;. 26(12):1467–1476. [DOI] [PubMed] [Google Scholar]
- 3. Kuper H, Heydt P, Davey C. A focus on disability is necessary to achieve HIV epidemic control. Lancet HIV. 2022;. 9(4):e293–e298. 10.1016/S2352-3018(21)00345-3 [DOI] [PubMed] [Google Scholar]
- 4. Ward E, Hanass‐Hancock J, Amon JJ. Left behind: persons with disabilities in HIV prevalence research and national strategic plans in east and Southern Africa. Disabil Rehabil. 2022;. 44(1):114–123. 10.1080/09638288.2020.1762124 [DOI] [PubMed] [Google Scholar]
- 5. UNFPA . The right to access. Regional strategic guidance to increase access to sexual and reproductive health and rights (SRHR) for young persons with disabilities in east and southern Africa. Pretoria: UNFPA; 2018. [Google Scholar]
- 6. The Missing Billion Initiative, Clinton Health Access Initiative . Reimagining health systems that expect, accept and connect 1 billion people with disabilities. 2022.
- 7. Parekh T, Gimm G, Kitsantas P. Sexually transmitted infections in women of reproductive age by disability type. Am J Prev Med. 2023;. 64(3):393–404. 10.1016/j.amepre.2022.10.013 [DOI] [PubMed] [Google Scholar]
- 8. Rotenberg S, Davey C, McFadden E. Association between disability status and health care utilisation for common childhood illnesses in 10 countries in sub‐Saharan Africa: a cross‐sectional study in the Multiple Indicator Cluster Survey. eClinicalMedicine. 2023;. 57:101870. 10.1016/j.eclinm.2023.101870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Min J, Kim SY, Park JE, Kim YY, Park JH. Nationwide trends in the incidence of tuberculosis among people with disabilities in Korea: a nationwide serial cross‐sectional study. Epidemiol Health. 2022;. 44:e2022098. 10.4178/epih.e2022098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schenk KD, Tun W, Sheehy M, Okal J, Kuffour E, Moono G, et al. “Even the fowl has feelings”: access to HIV information and services among persons with disabilities in Ghana, Uganda, and Zambia. Disabil Rehabil. 2020;. 42(3):335–348. 10.1080/09638288.2018.1498138 [DOI] [PubMed] [Google Scholar]
- 11. Banks LM, Zuurmond M, Ferrand R, Kuper H. Knowledge of HIV‐related disabilities and challenges in accessing care: qualitative research from Zimbabwe. PLoS One. 2017;. 12(8):e0181144. 10.1371/journal.pone.0181144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aderemi TJ, Mac‐Seing M, Woreta SA, Mati KA. Predictors of voluntary HIV counselling and testing services utilization among people with disabilities in Addis Ababa, Ethiopia. AIDS Care. 2014;. 26(12):1461–1466. 10.1080/09540121.2014.923811 [DOI] [PubMed] [Google Scholar]
- 13. Tun W, Okal J, Schenk K, Esantsi S, Mutale F, Kyeremaa RK, et al. Limited accessibility to HIV services for persons with disabilities living with HIV in Ghana, Uganda and Zambia. J Int AIDS Soc. 2016;. 19(5 Suppl 4):20829. 10.7448/ias.19.5.20829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. UNESCO . Needs assessment on the current state of CSE for young people with disabilities in the east and southern African region. Harare: UNESCO; 2021. [Google Scholar]
- 15. Aderemi TJ, Pillay BJ. Sexual abstinence and HIV knowledge in school‐going adolescents with intellectual disabilities and non‐disabled adolescents in Nigeria. J Child Adolesc Ment Health. 2013;. 25(2):161–174. 10.2989/17280583.2013.823867 [DOI] [PubMed] [Google Scholar]
- 16. Aderemi TJ, Pillay BJ, Esterhuizen TM. Differences in HIV knowledge and sexual practices of learners with intellectual disabilities and non‐disabled learners in Nigeria. J Int AIDS Soc. 2013;. 16(1):17331. 10.7448/ias.16.1.17331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mekonnen AG, Bayleyegn AD, Aynalem YA, Adane TD, Muluneh MA, Zeru AB. Determinants of knowledge, attitudes, and practices in relation to HIV/AIDS and other STIs among people with disabilities in North‐Shewa zone, Ethiopia. PLoS One. 2020;. 15(10):e0241312. 10.1371/journal.pone.0241312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abimanyi‐Ochom J, Mannan H, Groce NE, McVeigh J. HIV/AIDS knowledge, attitudes and behaviour of persons with and without disabilities from the Uganda Demographic and Health Survey 2011: differential access to HIV/AIDS information and services. PLoS One. 2017;. 12(4):e0174877. 10.1371/journal.pone.0174877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yousafzai AK, Edwards K, D'Allesandro C, Lindstrom L. HIV/AIDS information and services. Disabil Rehabil. 2005;. 27:1357–1363. [DOI] [PubMed] [Google Scholar]
- 20. Yousafzai A, Edwards K. Double burden: a situation analysis of HIV/AIDS and young people with disabilities in Rwanda and Uganda. London: Save the Children; 2004. [Google Scholar]
- 21. Yousafzai A, Aisha K, Dlamini PJ, Groce N, Wirz S. Knowledge, personal risk and experiences of HIV/AIDS among people with disabilities in Swaziland. Int J Rehabil Res. 2005;. 27(3):247–251. [DOI] [PubMed] [Google Scholar]
- 22. Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Pillay‐van‐Wyk V, et al. South African national HIV prevalence, incidence, behaviour and communication survey 2008: a turning tide among teenagers? Cape Town: HSRC Press; 2009. [Google Scholar]
- 23. Chipanta D, Mitra S, Amo‐Agyei S, Velarde MR, Amekudzi K, Osborne C, et al. Differences between persons with and without disability in HIV prevalence, testing, treatment, and care cascade in Tanzania: a cross‐sectional study using population‐based data. Research Square; 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pengpid S, Peltzer K. HIV status, knowledge, attitudes and behaviour of persons with and without disability in South Africa: evidence from a national population‐based survey. Pan Afr Med J. 2019;. 33:302. 10.11604/pamj.2019.33.302.17215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mitra S, Yap J. The disability data report 2022. New York: Disability Data Initiative and Fordham Research Consortium on Disability; 2022. [Google Scholar]
- 26. UNICEF . Disability Data: 6th Round of the Multiple Indicator Cluster Survey Programme. MICS; 2017. [Google Scholar]
- 27. Khan S, Hancioglu A. Multiple Indicator Cluster Surveys: delivering robust data on children and women across the globe. Stud Fam Plann. 2019;. 50(3):279–286. 10.1111/sifp.12103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cappa C, Mont D, Loeb M, Misunas C, Madans J, Comic T, et al. The development and testing of a module on child functioning for identifying children with disabilities on surveys. III: Field testing. Disabil Health J. 2018;. 11(4):510–518. 10.1016/j.dhjo.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. UNICEF . Multiple Indicator Cluster Surveys Instructions for Interviewers. New York: UNICEF; 2021. [Google Scholar]
- 30. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;. 159(7):702–706. 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 31. Lumley T. Survey: analysis of complex survey samples. R package version 4.0. 2020.
- 32. Hoaglin DC. Misunderstandings about Q and ‘Cochran's Q test’ in meta‐analysis. Stat Med. 2016;. 35(4):485–495. [DOI] [PubMed] [Google Scholar]
- 33. Akobirshoev I, Valentine A, Zandam H, Nandakumar A, Jewkes R, Blecher M, et al. Disparities in intimate partner violence among women at the intersection of disability and HIV status in South Africa: a cross‐sectional study. BMJ Open. 2022;. 12(9):e054782. 10.1136/bmjopen-2021-054782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. The Global Fund . Midterm Assessment Summary Report. Global Fund Breaking Down Barriers Initiative. Geneva: The Global Fund; 2022. [Google Scholar]
- 35. Hanass‐Hancock J, Alli F. Closing the gap: training for healthcare workers and people with disabilities on the interrelationship of HIV and disability. Disabil Rehabil. 2015;. 37(21):2012–2021. 10.3109/09638288.2014.991455 [DOI] [PubMed] [Google Scholar]
- 36. Mactaggart I, Hasan Bek A, Banks LM, Bright T, Dionicio C, Hameed S, et al. Interrogating and reflecting on disability prevalence data collected using the Washington Group Tools: results from population‐based surveys in Cameroon, Guatemala, India, Maldives, Nepal, Turkey and Vanuatu. Int J Environ Res Public Health. 2021;. 18(17):9213. 10.3390/ijerph18179213 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Data Availability Statement
MICS data are publicly available on the UNICEF website.


