Abstract
BACKGROUND
Isolated unilateral alar ligament injury (IUALI) is a rare and likely underreported occurrence after upper cervical trauma, with only 16 cases documented in the literature to date. Patients generally present with neck pain, and definitive diagnosis is typically made by magnetic resonance imaging (MRI). Unfortunately, likely due in part to its rarity, there are no formal guidelines for the treatment of an IUALI. Furthermore, there is a limited understanding of the long-term consequences associated with its inadequate treatment.
OBSERVATIONS
Here, the authors report on three pediatric patients, each found to have an IUALI after significant trauma. All patients presented with neck tenderness, and two of the three had associated pain-limited range of neck motion. Imaging revealed either a laterally deviated odontoid process on cervical radiographs and/or MRI evidence of ligamentous strain or discontinuity. Each patient was placed in a hard cervical collar for 1 to 2 months with excellent resolution of symptoms. A comprehensive review of the literature showed that all patients with IUALI who had undergone external immobilization with either rigid cervical collar or halo fixation had favorable outcomes at follow-up.
LESSONS
For patients with IUALI, a moderate course of nonsurgical management with rigid external immobilization appears to be an adequate first-line treatment.
Keywords: alar ligament, pediatric, spine trauma, craniocervical junction injury
ABBREVIATIONS: AP = anteroposterior, CCJ = craniocervical junction, CT = computed tomography, ED = emergency department, IUALI = isolated unilateral alar ligament injury, LDAS = lateral dens atlas space, LOC = loss of consciousness, MRI = magnetic resonance imaging, STIR = short tau inversion recovery
The alar ligaments, with help from the transverse ligament and tectorial membrane, are responsible for the bulk of craniocervical junction (CCJ) stability.1 Strain or rupture of the alar ligaments is often seen following upper cervical trauma, most commonly alongside concomitant injuries such as condylar fracture, atlantooccipital dislocation, atlantoaxial subluxation, or other ligamentous disruption.2–6 Such injuries can result in high cervical instability and often warrant urgent surgical intervention to prevent or abate severe spinal cord damage.
Isolated unilateral alar ligament injury (IUALI) is seemingly rare, however, with only 16 cases documented in the literature to date.7–14 Due in part to the rarity of this injury, there is limited understanding of the long-term outcomes associated with IUALI. Therefore, consensus on the best treatment strategy has been lacking in the literature.
Herein, we describe the cases of three pediatric patients who presented after trauma with an IUALI, each treated via rigid collar immobilization with excellent resolution of symptoms. Aided by a systematic review of the literature, our report is the first to propose a gold-standard treatment paradigm for IUALI.
Illustrative Cases
Case 1
A 11-year-old male with no relevant past medical history presented to the emergency department (ED) after being involved in an accident between a scooter with an unhelmeted rider and a car. He reported head trauma without loss of consciousness (LOC) and neck pain exacerbated by lateral rotation of the head. The patient was neurologically intact, and the remainder of his examination was notable only for neck tenderness, scattered abrasions, and pain-limited range of motion of the neck. Cervical radiographs revealed rightward lateral deviation of the odontoid process on an anteroposterior (AP) “fish-mouth” view (Fig. 1A). Computed tomography (CT) scanning ruled out any associated fracture, atlantoaxial subluxation, or atlantooccipital dislocation. Magnetic resonance imaging (MRI) of the cervical spine demonstrated isolated T2 and short tau inversion recovery (STIR) signal intensity within the left alar ligament (Fig. 1B–D). The patient was maintained in a hard cervical collar and discharged the following day. At the 1-month follow-up, his neck pain and tenderness had resolved, and flexion/extension radiographs revealed no evidence of dynamic instability (Fig. 1E and F). His cervical collar was subsequently cleared. At the 2-month follow-up, the patient remained asymptomatic with full cervical range of motion.
FIG. 1.
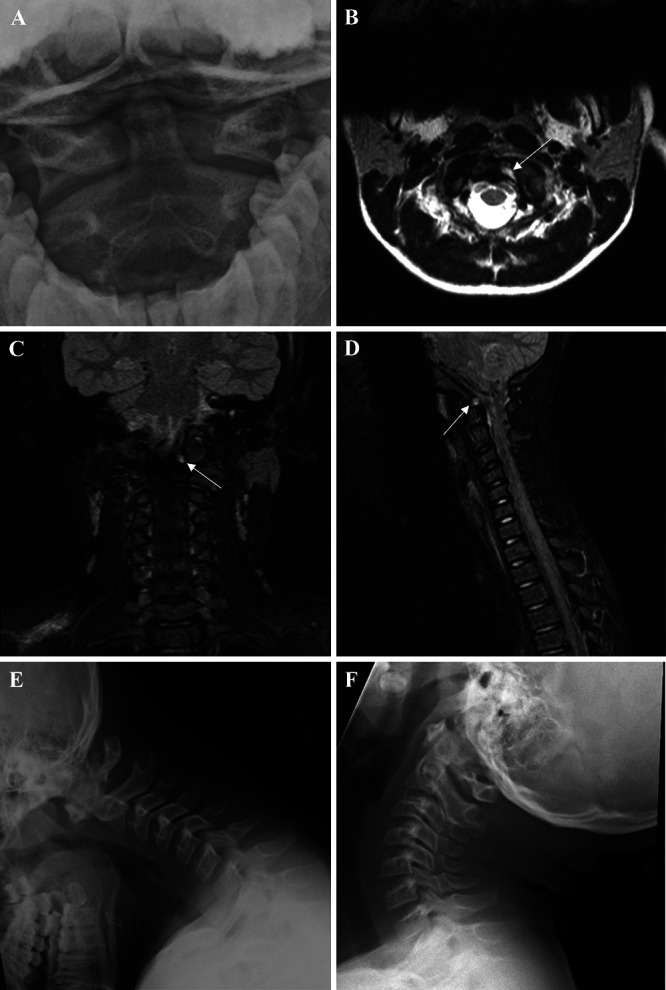
Case 1. Cervical radiograph (A) obtained on presentation, demonstrating lateral deviation of the odontoid process with no associated cervical spine fractures. Axial T2-weighted MRI (B), coronal STIR (C), and sagittal STIR (D) sequences obtained on the day of patient presentation, showing signal intensity within the left alar ligament (white arrows). Flexion (E) and extension (F) cervical radiographs obtained at the 1-month follow-up, demonstrating no signs of dynamic cervical instability.
Case 2
A 11-year-old male with no relevant past medical history presented to the ED with neck pain after a fall from a trampoline. The patient reported that the neck pain was exacerbated by lateral rotation of the head and by flexion or extension of the neck. Physical examination was only notable for diffuse cervical tenderness and pain-limited range of motion of the neck. MRI of the cervical spine revealed T2 signal intensity within the left alar ligament and widening of the left lateral dens atlas space (LDAS), with rightward odontoid deviation (Fig. 2A and B). The patient was placed in a hard collar and sent home, scheduled to follow-up in 2 months. At the follow-up, the patient had full painless range of motion of the neck. Repeat MRI demonstrated reduced signal in the left alar ligament and medialization of the odontoid, although some mild asymmetry remained (Fig. 2C and D). The collar was subsequently cleared.
FIG. 2.
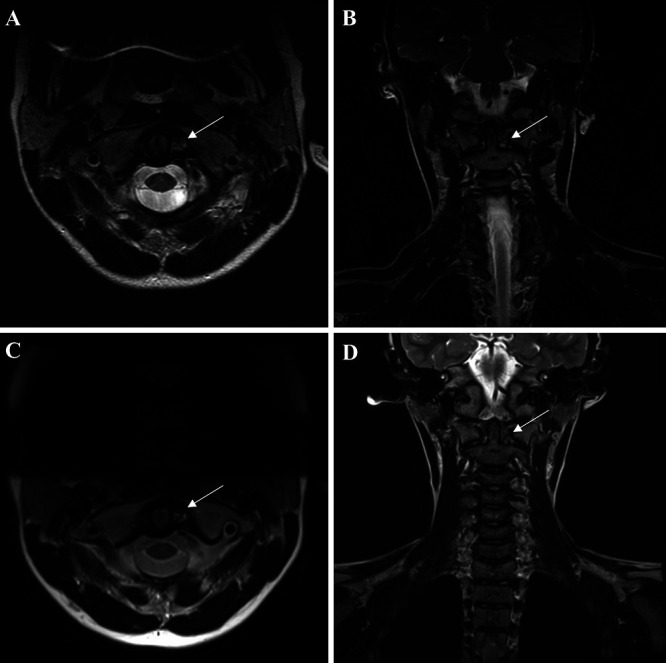
Case 2. Axial (A) and coronal (B) T2-weighted MRI of the cervical spine performed on the day of presentation, with signal intensity observed within the left alar ligament and widening of the left LDAS (white arrows). Follow-up axial (C) and coronal (D) T2-weighted MRI performed 2 months later, demonstrating resolved signal intensity and medialization of the odontoid.
Case 3
A 17-year-old female with no relevant past medical history presented to the ED with neck and shoulder pain after a motorcycle accident in which she was unhelmeted and ejected off the bike, hit her head, and experienced LOC. On examination, the patient was found to have right clavicular and pan-spine tenderness, worse in the neck. She was otherwise neurologically intact, with no new numbness, tingling, or weakness. A radiograph of the shoulder revealed a right clavicular fracture for which she was placed in a sling. Total spine CT was without fracture or bony displacement. A STIR sequence of the cervical spine showed isolated signal within the right alar ligament, indicative of an IUALI (Fig. 3A). The patient was placed in a hard cervical collar. At the 1-month follow-up, the patient demonstrated full painless range of motion of the neck and dynamic and AP radiographs were normal (Fig. 3B-D). The collar was subsequently cleared.
FIG. 3.
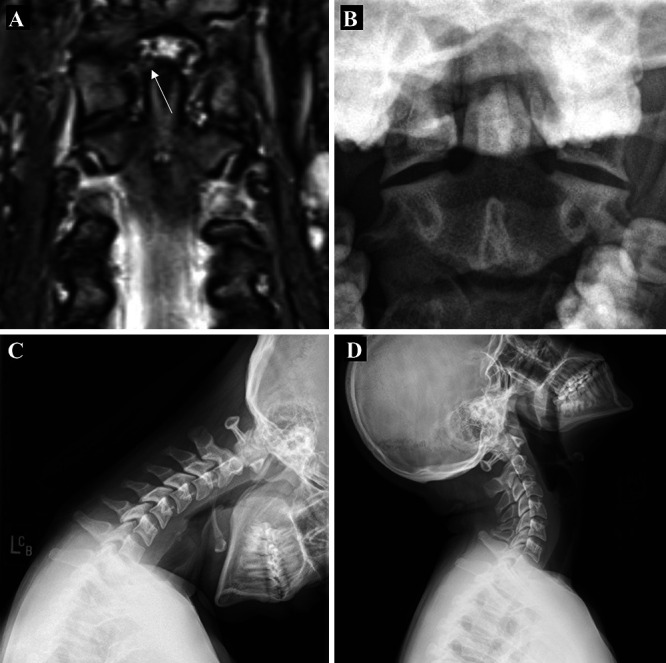
Case 3. Coronal STIR image of the cervical spine on the day of presentation (A), demonstrating signal intensity within the right alar ligament (white arrow). Follow-up odontoid (B), flexion (C), and extension (D) cervical radiographs without evidence of bony asymmetry or instability.
Literature Review
This comprehensive review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines with the aim of supplementing our cases with the literature’s current understanding of the presentation, management, and outcomes of patients with an IUALI. PubMed was queried for any report involving patients with an IUALI that had been published between database inception and November 2023. The following search terms were utilized to achieve this goal: “isolated unilateral alar rupture,” “isolated unilateral alar injury,” “isolated alar injury,” “isolated alar rupture,” “alar rupture,” “alar injury,” “alar strain,” and “upper cervical spine trauma.”
Any original article that investigated adult or pediatric human patients with a traumatic alar injury was considered. Exclusion criteria were as follows: 1) studies with patients who had multiple other upper cervical injuries alongside the alar injury, 2) studies in which there was not ample clinical information (e.g., lack of details regarding patient presentation or management), and 3) studies in which the alar injury was ambiguous.
The following data were extracted from each included article: first author, year of publication, age and sex of reported patients, mechanism of trauma, clinical presentation, relevant imaging findings (e.g., radiography, CT, MRI), type and duration of treatment, and clinical and radiological outcome. Some of the extracted data were shown as a fraction or percentage for presentation purposes. No comparisons between studies or statistical analyses were performed. Of note, data were limited by what was reported within original texts, which accounts for some discrepancies in the level of detail provided herein.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
The alar ligaments extend bilaterally from the lateral or posterolateral upper third of the dens to the medial surface of the ipsilateral occipital condyle, with additional extension of the ligament to the medial aspect of the C1 lateral mass in some patients.10,15 The paired ligaments work to maintain the atlas in a midline position as well as to limit axial rotation and lateral flexion at the C0–1 and C1–2 joints.15,16 Thus, IUALI likely occurs with abrupt contralateral rotation or hyperflexion of the neck at forces that are not great enough to compromise bone or the sturdier transverse ligament and tectorial membrane.10 Presumably because of its rarity and the sometimes subtle symptom presentation associated with the injury, diagnosis of an IUALI is thought to often be missed when clinical suspicion is lacking, which has uncertain long-term consequences.11,12
Each patient included in our report presented with neck pain and tenderness after a significant trauma. Notably, no patient in our cohort presented with torticollis, painful neck spasms, or neurological deficit. Although IUALI was suspected on the cervical radiograph of the patient in case 1, which demonstrated lateral odontoid deviation, all diagnoses were ultimately made on MRI. In all patients, the condyle–C1 interval, powers ratio, basion-dens interval, and anterior atlantodental interval were within normal limits, suggesting stability across the occiput–C1 and atlantoaxial joints. Each patient was treated with rigid collar immobilization for 1 to 2 months with good resolution of symptoms. Postimmobilization imaging in each case showed resolution of ligamentous injury and stability of the CCJ.
Lessons
Eight prior studies have reported on a total of 16 patients with IUALI. Among the cases of IUALI that have been previously described (Table 1), the most common presenting symptom, affecting >30% of patients, was motion-aggravated neck pain, particularly when rotating contralateral to the injury.7–14 Most often, the neck pain localized to the side of the rupture, although midline or diffuse pain was also commonly seen.11 Neck tenderness and restricted neck range of motion, presumably secondary to pain, have also been frequently described.8,10,12,13 Additional presenting symptoms attributable to the ligamentous injury were infrequently seen. Ipsilateral torticollis was the next most common chief compliant, with only 2 of 16 patients affected (12.5%).9,10 Interestingly, in the report by Unal et al.,11 multiple patients were discharged from the hospital after normal CT scans and were only discovered to have an IUALI after they re-presented with persistent unilateral motion-aggravated neck pain. Together, this underscores two important principles when managing cervical trauma patients. First, all trauma patients should be assessed for rotational neck pain to ensure bony integrity and cervical stability. Second, persistent isolated rotational neck pain after trauma should raise concern for alar ligament injury.
TABLE 1.
Summary of isolated alar ligament injury literature review
| Authors & Year | Age (yrs)/Sex | Mechanism | Clinical Presentation | Radiograph | CT | MRI | Management | Clinical Outcome | Radiographic Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Briem et al., 200213 |
15/M |
Gymnastics-related hyperflexion |
Neck pain w/ restricted ROM |
Lt deviated dens |
Lt deviated dens |
T1–2 hyperintensity in widened LDAS |
Hard collar for 4 wks |
Full painless ROM w/in 1 mo |
No FU imaging obtained |
| 10/F |
2-m fall w/ hyperflexion |
Neck pain |
Rt deviated dens |
Rt deviated dens |
T2 hyperintensity in widened lt LDAS |
Hard collar for 4 wks |
Full painless ROM w/in 1 mo |
No FU imaging obtained |
|
| Demetrious, 20078 |
21/F |
MVA |
Neck pain w/ restricted ROM |
Normal |
Normal |
T2 hyperintensity in widened lt LDAS & disruption of lt alar ligament |
6 wks of chiropractic readjustment |
Asymptomatic at 6-mo FU |
No FU imaging obtained |
| Caird et al., 20099 |
17/F |
Pedestrian vs vehicle |
Neck pain |
NA |
Rt deviated dens |
T2 hyperintensity in widened lt LDAS |
Halo brace for 12 wks |
Returned to baseline activity in 12 wks |
Normal dynamic radiographs at 7- & 19-mo FU |
| 15/F |
MVA |
Neck pain |
Normal |
Rt deviated dens |
Hyperintensity in widened lt LDAS |
Halo brace for 12 wks |
Full painless ROM at 6 mos |
Normal dynamic radiographs at 6-mo FU |
|
| 5/F |
MVA |
Torticollis |
Normal |
Lt deviated dens |
T1 hyperintensity in widened rt LDAS w/ disruption of rt alar ligament |
Hard collar for 4 mos, soft collar for 2 mos |
Full painless ROM at 1 yr |
MRI at 4-mo FU showed disruption of alar ligament & hyperintensity in rt LDAS; normal dynamic radiographs at 18 mos |
|
| Wong et al., 201410 |
9/F |
5-ft fall w/ hyperflexion |
Neck pain w/ restricted ROM & torticollis |
Rt deviated dens |
Rt deviated dens |
T1/2 hyperintensity in widened lt LDAS w/ disruption of lt alar ligament |
Guilford brace for 12 wks |
Full painless ROM at 4 mos |
MRI at 3-mo FU showed improved deviation of dens & resolved lt LDAS T2 hyperintensity |
| Kaufmann et al., 201512 |
25/M |
Blunt fist trauma to lt side of head |
Neck stiffness, dysphagia, fasciculation in lt arm, paraesthesias in thoracic spine, & cervical hypermobility |
NA |
Rt deviated dens |
T1 hyperintensity w/in widened lt LDAS & disruption of lt alar ligament |
Hard collar for 3 mos, soft collar for 2 mos, 3 more mos of hard collar |
Near painless ROM at 13 mos |
MRI at 3-mo FU showed improved dens deviation & lt LDAS T2 hyperintensity; MRI at 5-mo FU showed worsening T2 hyperintensity; MRI at 8-mo FU showed improvement in T2 hyperintensity |
| Santin et al., 20177 |
19/M |
MVA |
Headaches, gait instability, & weakness of rt UE |
NA |
Lat atlantoaxial subluxation w/ rt deviated dens |
Rt displacement of odontoid & disruption of lt alar ligament |
Hard collar for 6 mos |
Full painless ROM |
MRI at 6-mo & 1-yr FU showed complete resolution of tear; normal dynamic CT scan at 2-yr FU |
| Unal et al., 201911 |
8/M |
Backward fall |
Rt-sided neck pain aggravated by lt rotation |
NA |
LAD interval asymmetry |
Hyperintensity in rt LDAS |
Hard collar |
Full painless ROM w/in 2 mos |
MRI & dynamic CT scan at 3- mo FU showed normal LDAS space w/ no hyperintensity or signs of cervical instability |
| 14/M |
Fight (headlock) |
Rt-sided neck pain aggravated by bilat rotation |
NA |
LAD interval asymmetry |
Hyperintensity in rt LDAS |
Hard collar |
Full painless ROM w/in 1 mo |
Normal dynamic CT scan FU |
|
| 30/M |
Backward fall |
Midline neck pain aggravated by rt rotation |
NA |
LAD interval asymmetry |
Hyperintensity in lt LDAS & apical ligament |
Hard collar |
Full painless ROM w/in 4 mos |
MRI & dynamic CT scan at 3-mo FU showed normalized LDAS space, minimal hyperintensity, & no signs of instability |
|
| 81/M |
Backward fall |
Lt-sided neck pain aggravated by bilat rotation |
NA |
LAD interval asymmetry |
Hyperintensity in lt LDAS & transverse ligament |
Hard collar |
Full painless ROM w/in 2 mos |
Normal dynamic CT scan at FU |
|
| 58/F |
Backward fall |
Rt-sided neck pain aggravated by bilat rotation |
NA |
LAD interval asymmetry |
Hyperintensity in rt LDAS & apical ligament |
Hard collar |
Full painless ROM w/in 3 mos |
MRI & dynamic CT at 3-mo FU showed normalized LDAS space, no hyperintensity, & no signs of instability |
|
| 23/F |
Fall on rt side of face |
Diffuse neck tenderness |
NA |
LAD interval asymmetry |
Hyperintensity in lt LDAS |
Hard collar |
Full painless ROM w/in 1 mo |
Normal dynamic CT scan at FU |
|
| Keskil et al., 202114 |
36/F |
Fall |
NA |
Normal |
Lt deviated dens |
Disruption of rt alar ligament |
Halo brace for 3 mos |
Full painless ROM w/in 3 mos |
MRI at 3- mo FU showed healed alar ligament |
| Reeves et al., 2024 | 11/M |
Unhelmeted scooter vs vehicle |
Motion-aggravated neck pain w/ restricted ROM |
Rt deviated dens |
No Fx or subluxation |
T2/STIR hyperintensity in lt alar ligament |
Hard collar for 1 mo |
Full painless ROM w/in 1 mo |
Normal dynamic radiographs at 1-mo FU |
| 11/M |
Fall from trampoline |
Motion-aggravated neck pain w/ restricted ROM |
NA |
NA |
T2/STIR hyperintensity in lt alar ligament |
Hard collar for 2 mos |
Full painless ROM w/in 2 mos |
MRI at 2-mo FU showed resolved signal intensity of lt alar ligament & mild continued rt deviation of odontoid |
|
| 17/F | Motorcycle accident | Neck pain & tenderness | NA | Normal | T2/STIR hyperintensity w/in rt alar ligament | Hard collar for 1 mo | Full painless ROM w/in 1 mo | Normal dynamic radiographs at 1-mo FU |
FU = follow-up; Fx = fracture; LAD = lateral atlantodental; MVA = motor vehicle accident; NA = not applicable; ROM = range of motion; UE = upper extremity.
Imaging findings among patients with IUALI can be variable, but initial CT is important to rule out fractures, subluxation, or dislocation. The most consistent finding, reported in 15 of the 16 documented patients, as well as in our first patient, was lateral deviation of the odontoid to the side opposite that of the alar injury.7–14 Odontoid deviation is best visualized on CT but can often be seen on radiographs as well, particularly in the AP fish-mouth view. As is the case with all trauma, patients with concerning CT findings or those with persistent neck pain or midline tenderness should be assessed with MRI to better visualize the ligaments of the upper cervical spine.11 True alar rupture can be confirmed by visualizing ligamentous discontinuity, which was explicitly seen in 5 (31.3%) of 16 cases. However, current limitations in MRI often make it difficult to identify such disruption, particularly when there is inflammation within the ligament itself or surrounding structures. Therefore, our ability to distinguish between a rupture or an injury (e.g., strain) is limited on imaging alone. In the majority of IUALI cases, diagnosis has been confirmed by visualizing the T2 or STIR signal within the alar ligament and widening of the LDAS.7–14 Although such findings are strongly suggestive of edema and/or hemorrhage related to ligamentous strain or rupture,10 they must be interpreted alongside the clinical context, as signal intensity within the alar ligament can sometimes be observed in healthy patients.17,18 Once the diagnosis of alar injury or rupture has been made, some authors have opted to examine stability with a cervical flexion/extension CT scan11 or radiograph.9 This is especially relevant when there is ambiguous signal intensity within the transverse or apical ligament that is of undetermined significance, which could represent an increased risk for dangerous instability, as was the case in three of the patients reported by Unal et al.11
The long-term consequences of an unrecognized IUALI are not well understood. It is hypothesized that untreated damage can increase the risk of later instability and neurological involvement, especially in the case of a second traumatic event. Kaufmann et al.12 reported on a case in which a patient with an initially undiagnosed IUALI re-presented 6 months after the alar injury was presumably sustained with dangerous cervical hypermobility, thoracic paraesthesias, fasciculations, and dysphagia. Thus, it is important to establish a gold-standard treatment modality. In 14 of the 16 cases currently reported in the literature, cervical orthosis for a duration of 1 to 6 months led to the resolution of presenting symptoms and full painless range of motion of the neck.7–14 Of these patients, 10 were treated with a rigid cervical collar, 3 with a halo brace, and 1 with a Guilford brace.7–14 Given the lack of deformity or neurological injury observed in our patients, conservative management until symptoms abated was also chosen as our first-line treatment modality. Although we considered halo bracing and cervical orthosis via a hard or soft collar, we ultimately opted for hard collar fixation, as it provided adequate immobilization without subjecting the patient to the morbidity of halo bracing. Thus, with our cases included, 17 of 19 total patients attained full symptomatic recovery with cervical immobilization alone; 13 of them were managed using only a collar. This suggests that rigid collar immobilization until symptoms have resolved is adequate for the treatment of IUALIs, although halo bracing can lead to a faster recovery and be a better option for patients who are unlikely to comply with collar recommendations.9 Other therapies reported to have aided in recovery included benzodiazepines, physical therapy, chiropractic readjustment, and trigger point injections; however, these interventions have scarce documentation, and further studies are needed before they are routinely recommended to patients.8,9,14
Follow-up imaging can be used to help guide the duration of cervical orthosis or to assess the need for additional management; however, some patients have been cleared on a clinical basis alone (3 [18.8%] of 16). Most commonly, patients were cleared with symptomatic recovery alongside a normal dynamic CT scan (7 [43.8%] of 16) or radiograph (2 [12.5%] of 16),9 as was the case for 2 of our patients, and/or MRI demonstrating resolved alar hyperintensity and improved asymmetry between the odontoid and C1 lateral masses (8 [50%] of 16), as was the case for 1 of our patients.7,9–11 Overall, although MRI is more sensitive for detecting ligament health, the utility of treating MRI findings alone is currently unknown. Although we opted to forgo follow-up MRI in 2 of our 3 patients, in the literature there were multiple cases of asymptomatic patients who had received extended treatment based solely on continued signal hyperintensity or poor bony symmetry on MRI.7,9,12 Larger studies are needed to better understand the relationship between MRI findings and the need for further treatment.
It is interesting to note that IUALI appears to have a predilection for children, with 11 of the now 19 reported cases occurring in pediatric patients.7–14 The pediatric cervical spine has greater elastic properties than the adult spine due to several factors, including its relatively more shallow facet joints, increased laxity within the ligaments, and underdeveloped supporting musculature.19 This is likely responsible, in part, for the increased likelihood of ligamentous injury in the absence of osseous injury.19 Thus, clinical suspicion for an alar injury should be higher in pediatric trauma patients who present with rotational neck pain. Possible age-specific changes in management, however, do not appear to apply in the case of alar rupture or injury.
We have offered three additional case studies of IUALI in pediatric patients who were each treated with rigid collar immobilization and shown to have a good clinical result. While this aligns well with the current limited body of literature, it is possible that conservative management is less beneficial for true alar ruptures, in which ligamentous continuity is no longer preserved. Despite this, for any suspected isolated alar injury (e.g., rupture, strain), we still advocate for an initial trial of rigid collar immobilization for multiple reasons: 1) in most cases, imaging cannot clearly classify a rupture versus a strain; 2) collar immobilization, via an unexplained underlying process, has proven successful even in cases in which ligamentous discontinuity can reportedly be appreciated; and 3) isolated alar injury has not been reported to present with dangerous high cervical instability or neurological deficit in any case, which complicates justification of a highly invasive surgical procedure or halo bracing. Thus, we recommend that surgical correction/fusion or more invasive orthosis (e.g., halo bracing) be pursued only in cases in which the patient has a high risk for collar noncompliance or when there is persistent pain, the development of neurological symptoms, or worsening deformity or instability even with collar immobilization. It is important to emphasize, however, that these recommendations rely on an extremely limited body of literature as well as a currently unexplained healing phenomenon. Thus, additional studies on the mechanism by which external immobilization may lead to ligamentous recovery in cases of complete rupture and those that further compare outcomes depending on treatment methodology are important to validate these findings.
Author Contributions
Conception and design: Kundishora, Reeves, DiLuna. Acquisition of data: Kundishora, Valcarce-Aspegren, DiLuna. Analysis and interpretation of data: Kundishora, Valcarce-Aspegren, Robert, Elsamadicy, DiLuna. Drafting the article: Kundishora, Reeves, Valcarce-Aspegren, DiLuna. Critically revising the article: Kundishora, Reeves, Robert, Elsamadicy, Tucker, Storm, DiLuna. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Kundishora. Administrative/technical/material support: Kundishora, DiLuna. Study supervision: Kundishora, Tucker, DiLuna.
References
- 1.Offiah CE. Craniocervical junction and cervical spine anatomy. Neuroimaging Clin N Am. 2022;32(4):875–888. doi: 10.1016/j.nic.2022.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Alves OL, Pereira L, Kim SH, et al. Upper cervical spine trauma: WFNS Spine Committee Recommendations. Neurospine. 2020;17(4):723–736. doi: 10.14245/ns.2040226.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karray M, M’nif N, Mestiri M, Kooli M, Ezzaouia K, Zlitni M. Concomitant alar and apical ligament avulsion in atlanto-axial rotatory fixation. Case report and review of the literature. Acta Orthop Belg. 2004;70(2):189–192. [PubMed] [Google Scholar]
- 4. Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation—part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery. 2007;61(5):995–1015. doi: 10.1227/01.neu.0000303196.87672.78. [DOI] [PubMed] [Google Scholar]
- 5. Adams VI. Neck injuries: I. Occipitoatlantal dislocation—a pathologic study of twelve traffic fatalities. J Forensic Sci. 1992;37(2):556–564. [PubMed] [Google Scholar]
- 6. Bloom AI, Neeman Z, Floman Y, Gomori J, Bar-Ziv J. Occipital condyle fracture and ligament injury: imaging by CT. Pediatr Radiol. 1996;26(11):786–790. doi: 10.1007/BF01396202. [DOI] [PubMed] [Google Scholar]
- 7.Santin MD, Cebula H, Ollivier I, Todeschi J, Baloglu S, Proust F. Diagnosis and suggested treatment against an isolated unilateral rupture of the alar ligament: concerning one case. Neurochirurgie. 2017;63(6):478–482. doi: 10.1016/j.neuchi.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 8. Demetrious J. Post-traumatic upper cervical subluxation visualized by MRI: a case report. Chiropr Osteopat. 2007;15:20. doi: 10.1186/1746-1340-15-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Caird MS, Hensinger RN, Vander Have KL, Gelbke MK, Farley FA. Isolated alar ligament disruption in children and adolescents as a cause of persistent torticollis and neck pain after injury. A report of three cases. J Bone Joint Surg Am. 2009;91(11):2713–2718. doi: 10.2106/JBJS.H.01405. [DOI] [PubMed] [Google Scholar]
- 10. Wong ST, Ernest K, Fan G, Zovickian J, Pang D. Isolated unilateral rupture of the alar ligament. J Neurosurg Pediatr. 2014;13(5):541–547. doi: 10.3171/2014.2.PEDS13527. [DOI] [PubMed] [Google Scholar]
- 11.Unal TC, Dolas I, Unal OF. Unilateral alar ligament injury: diagnostic, clinical, and biomechanical features. World Neurosurg. 2019;132:e878–e884. doi: 10.1016/j.wneu.2019.07.198. [DOI] [PubMed] [Google Scholar]
- 12. Kaufmann RA, Marzi I, Vogl TJ. Delayed diagnosis of isolated alar ligament rupture: A case report. World J Radiol. 2015;7(10):357–360. doi: 10.4329/wjr.v7.i10.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Briem D, Linhart W, Dickmann C, Rueger JM. Injuries of the alar ligaments in children and adolescents. Unfallchirurg. 2002;105(6):555–559. doi: 10.1007/s00113-001-0367-2. [DOI] [PubMed] [Google Scholar]
- 14.Keskil S, Yuksel U, Karadeniz Bilgili Y, Babacan A. Unilateral isolated alar ligament rupture in an adult female patient. Agri. 2021;33(4):265–267. doi: 10.14744/agri.2019.73555. [DOI] [PubMed] [Google Scholar]
- 15. Dvorak J, Panjabi MM. Functional anatomy of the alar ligaments. Spine (Phila Pa 1976) 1987;12(2):183–189. doi: 10.1097/00007632-198703000-00016. [DOI] [PubMed] [Google Scholar]
- 16. Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452–461. doi: 10.1002/jor.1100060317. [DOI] [PubMed] [Google Scholar]
- 17. Pfirrmann CW, Binkert CA, Zanetti M, Boos N, Hodler J. MR morphology of alar ligaments and occipitoatlantoaxial joints: study in 50 asymptomatic subjects. Radiology. 2001;218(1):133–137. doi: 10.1148/radiology.218.1.r01ja36133. [DOI] [PubMed] [Google Scholar]
- 18.Lummel N, Schöpf V, Bitterling H, et al. Effect of magnetic resonance imaging field strength on delineation and signal intensity of alar ligaments in healthy volunteers. Spine (Phila Pa 1976) 2012;37(17):E1062–E1067. doi: 10.1097/BRS.0b013e31825831ca. [DOI] [PubMed] [Google Scholar]
- 19. Junewick JJ. Pediatric craniocervical junction injuries. AJR Am J Roentgenol. 2011;196(5):1003–1010. doi: 10.2214/AJR.10.6051. [DOI] [PubMed] [Google Scholar]


