Abstract
BACKGROUND
Eagle syndrome, an uncommon condition, causes symptoms due to neural and/or vascular compression from an elongated styloid process or calcified stylohyoid ligament and can also complicate other planned surgical procedures.
OBSERVATIONS
A 42-year-old female with loss of balance, dizziness, and ataxic gait underwent cranial magnetic resonance imaging (MRI), revealing a right-sided Koos grade IV vestibular schwannoma. Initially, a retrosigmoid craniotomy for tumor resection was planned. However, preoperative MRI and computed tomography (CT) showed a dilated right-sided mastoid emissary vein, tortuous scalp and paraspinal veins, and bilateral elongated styloid processes. CT angiography and digital subtraction angiography indicated Eagle syndrome–related compression of both internal jugular veins and concurrent occlusion of the left internal jugular vein at the jugular foramen. Consequently, given the risk of damaging venous structures, Gamma Knife radiosurgery was chosen over resection.
LESSONS
This case highlights the importance of adapting treatment plans based on patient-specific anatomical and pathological factors. In situations in which traditional surgery poses risks to sensitive structures such as the venous system, alternative approaches like radiosurgery offer safer yet effective options. Comprehensive risk-benefit evaluations are crucial for such decisions.
Keywords: digital subtraction angiography, Eagle syndrome, Gamma Knife radiosurgery, radiosurgery, vestibular schwannoma
ABBREVIATIONS: CT = computed tomography, MRI = magnetic resonance imaging, SRS = stereotactic radiosurgery
Eagle syndrome is a relatively rare condition that arises due to an elongated styloid process or calcification of the stylohyoid ligament. The most common symptom is a dull and persistent pain in the throat. Patients can also experience odynophagia, globus sensation, facial and cervical pain, hoarseness, and, in rare cases, symptoms related to vascular compression such as stroke or transient ischemic attack. Eagle syndrome occurs in approximately 4% of the population, but only a small fraction (approximately 0.16%) actually experience symptoms.1
Eagle syndrome is often diagnosed through patient history and physical examination, but imaging studies such as panoramic radiography, computed tomography (CT), and three-dimensional reconstruction can confirm the diagnosis.2 Initial management usually involves conservative measures such as analgesics, local anesthetic injections, and corticosteroid injections. If these are not effective, surgical shortening of the styloid process can be considered. The importance of early detection and intervention in Eagle syndrome cannot be overstated, as delayed treatment can lead to serious complications such as stroke or pseudoaneurysms, which can be life-threatening.3 For effective management, clinicians must possess a thorough understanding of the condition’s diverse presentations, including the rare and subtle ones.
This paper enhances existing knowledge by documenting a patient’s experience with jugular compression, an exceedingly uncommon symptom of Eagle syndrome, who was treated with Gamma Knife radiosurgery for a vestibular schwannoma due to the manifestations of vascular Eagle syndrome.
Illustrative Case
A 42-year-old female with no significant medical or family history presented to our clinic with symptoms of loss of balance and dizziness. Neurological examination revealed an ataxic gait but no other significant findings. The patient had no history of trauma or substance abuse. Laboratory results were within normal limits.
Brain magnetic resonance imaging (MRI) showed an enhancing 3.5 × 4 cm mass originating from the internal acoustic canal, projecting into the pontocerebellar corner cistern and compressing the middle cerebellar peduncle and pons The lesion was regarded as a Koos grade IV vestibular schwannoma, and a retrosigmoid craniotomy was planned for resection; however, a dilated right-sided mastoid emissary vein, tortuous scalp and paraspinal veins, and bilateral elongated styloid processes were observed on preoperative MRI and CT (Fig. 1). CT angiography and digital subtraction angiography were ordered. CT angiography showed impingement of the internal jugular vein between the styloid process and the arch of C1 on the right side. Catheter angiography showed narrowing of the right internal jugular vein and reconstitution of flow to the right internal jugular vein immediately downstream to the presumed impingement point. The absence of blood flow through the left internal jugular vein was also noted (Fig. 2).
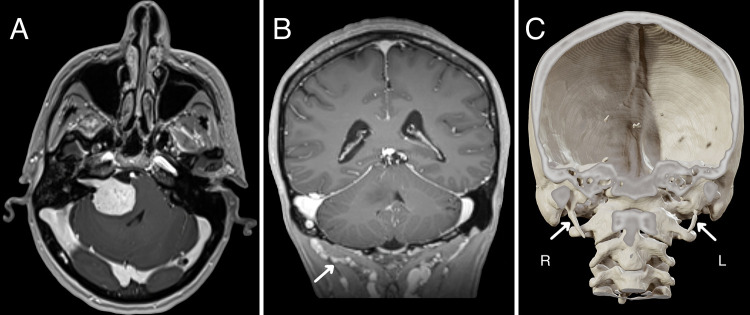
FIG. 1.
Axial contrast-enhanced T1-weighted MRI demonstrating a right cerebellopontine angle mass compatible with Koos grade IV vestibular schwannoma (A). Note the tortuous scalp and paraspinal veins on coronal contrast-enhanced T1-weighted MRI (arrow, B). Bilateral elongated styloid processes are also observed on CT with three-dimensional reconstruction (arrows, C). L = left; R = right.
FIG. 2.
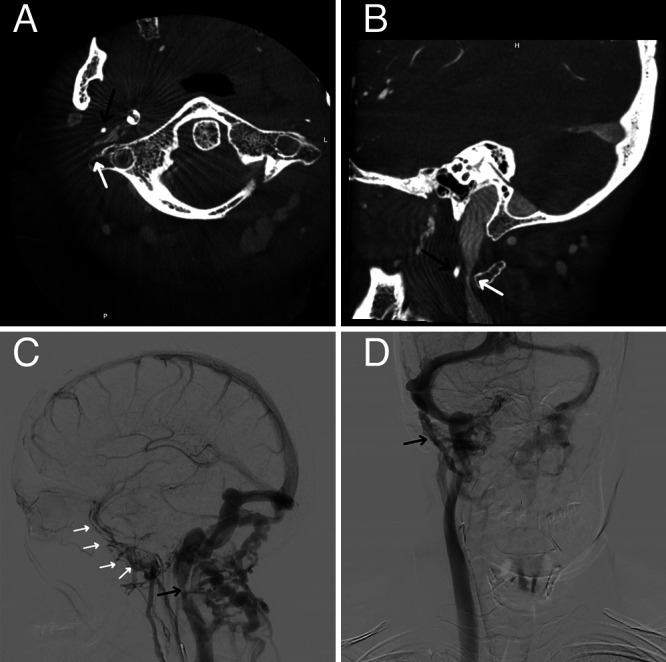
Axial (A) and sagittal (B) CT angiography showing impingement of the internal jugular vein between the styloid process (black arrows) and the arch of C1 (white arrows). Catheter angiography shows narrowing of the right internal jugular vein (black arrow, C) and reconstitution of flow to the right internal jugular vein immediately downstream to the presumed impingement point (white arrows, C) and dilated right-sided mastoid emissary vein (black arrow, D) and absence of blood flow on the left side.
Initially, retrosigmoidal resection of the vestibular schwannoma was planned. A translabyrinthine approach was not preferred, as the patient’s hearing was intact. Considering the potential risk to venous structures during surgical incision and craniotomy, Gamma Knife radiosurgery was proposed as a safer alternative. The patient underwent frameless hypofractionated Gamma Knife radiosurgery, receiving a margin dose of 30 Gy in 10 fractions (40% isodose line). Follow-up MRI 6 months after radiosurgery showed a stable lesion without adverse radiation effects, and subsequent annual follow-up MRI studies were planned.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
In this unique case, we encountered a clinical scenario that required a deviation from our standard surgical approach for treating a vestibular schwannoma. The patient, diagnosed with vascular Eagle syndrome, presented a significant challenge: the elongated styloid process caused jugular vein occlusion and raised concerns about the potential for collateral vascular damage during a conventional scalp incision and craniotomy. This necessitated a shift from our initially planned resection to a radiosurgical treatment, because Gamma Knife radiosurgery is a reliable and efficient approach for achieving tumor control in patients with Koos grade IV vestibular schwannomas who have symptoms that are not life-threatening or severely debilitating and especially those who have surgical comorbidities that make resection inadvisable.4
The decision to perform radiosurgery was driven by the need to mitigate the risks of vascular injury, which were heightened given the patient’s underlying Eagle syndrome. This condition, characterized by an elongated styloid process or calcified stylohyoid ligament, can lead to the compression of neurovascular structures. In surgical settings, this compression significantly increases the risk of intraoperative and postoperative vascular complications, which could be catastrophic.
Observations
The main observation in this case is the critical impact of vascular Eagle syndrome on surgical decision-making for a patient with vestibular schwannoma. This is important for several reasons. First, it highlights the complexity of managing patients with concurrent conditions that can complicate standard treatment protocols. Second, it underscores the importance of thorough preoperative evaluation and planning, particularly in recognizing anatomical variations or pathologies that may necessitate an alternative treatment approach.
To our knowledge, such direct interference of Eagle syndrome in the surgical management of vestibular schwannoma, necessitating a shift to radiosurgery, has not been widely reported in the literature. This case adds a novel dimension to the understanding of the interplay between these two conditions and their management.
Lessons
The most important lesson from this case is the need for adaptability and comprehensive assessment in surgical planning. Upon diagnosing Eagle syndrome in this case, our multidisciplinary team conducted a thorough assessment of the patient’s overall health, focusing on how Eagle syndrome might affect venous outflow and its possible effects on the outcomes of the planned vestibular schwannoma surgery. However, the decision to pursue or forego styloid process resection before addressing the vestibular schwannoma was influenced by several key considerations. First, in this case, the symptoms attributed to the vestibular schwannoma were more prominent and directly impacting the patient’s quality of life, guiding our priority for intervention. Given the complexity of the patient’s condition, our team was cautious about introducing additional surgical risks without clear evidence that styloid process resection would significantly impact the outcomes of the vestibular schwannoma resection. The consensus was that while styloid process resection could theoretically improve venous outflow, the evidence supporting its impact on the surgical management of vestibular schwannoma was limited. After discussing the potential options and their associated risks and benefits with the patient, the first decision was made to proceed directly with treatment of the vestibular schwannoma. This approach was aligned with the patient’s preferences and the immediate goal of addressing the most symptomatic and potentially life-altering tumor. Our experience demonstrates that even with well-established surgical protocols, patient-specific anatomical or pathological conditions can necessitate a significant change in the treatment approach. In this case, recognizing the risks associated with Eagle syndrome allowed for a timely shift to a safer, noninvasive treatment modality, thus avoiding potential complications. However, because Eagle syndrome is not treated, further growth of the tumor may necessitate reevaluation of the patient’s health and ability to undergo additional treatments. Options for further treatments may include repeat stereotactic radiosurgery (SRS) or resection. Undergoing repeat SRS after an initial failure shows high rates of control in vestibular schwannomas.5 The incidence of facial nerve palsy or hearing loss seems to be comparable to that associated with the initial SRS. Another option may be surgical removal via a translabyrinthine approach, which was not preferred before, as the patient’s hearing was intact.
A limitation of our findings is the rarity of this scenario, which may not be widely applicable or encountered frequently in clinical practice. However, the relevance of this observation lies in its contribution to the broader understanding of complex surgical decision-making, particularly in neurosurgery, where anatomical variations can have significant implications.
In conclusion, this case underscores the importance of flexibility in surgical planning, the need for detailed preoperative evaluations, and the value of radiosurgery as a safe alternative in complex neurosurgical cases. Our experience with this patient serves as a valuable lesson in the management of similar challenging scenarios in the future.
Acknowledgments
The authors gratefully acknowledge the use of the services and facilities of the Koç University Research Center for Translational Medicine (KUTTAM), funded by the Presidency of Turkey, Head of Strategy and Budget.
Author Contributions
Conception and design: Peker, Karaman, Samanci. Acquisition of data: Peker, Askeroglu. Analysis and interpretation of data: Peker, Düzkalir. Drafting the article: Peker, Karaman, Düzkalir, Samanci. Critically revising the article: Peker, Düzkalir, Samanci. Reviewed submitted version of manuscript: Peker, Karaman, Samanci. Approved the final version of the manuscript on behalf of all authors: Peker. Administrative/technical/material support: Düzkalir, Senturk. Study supervision: Peker.
References
- 1. Pagano S, Ricciuti V, Mancini F, et al. Eagle syndrome: an updated review. Surg Neurol Int. 2023;14:389. doi: 10.25259/SNI_666_2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: a comprehensive review. Clin Neurol Neurosurg. 2017;159:34–38. doi: 10.1016/j.clineuro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 3. Lakner K, Savšek L. Carotid artery type of Eagle syndrome: an uncommon cause of ischemic stroke. Wien Klin Wochenschr. 2023;135(5-6):158–161. doi: 10.1007/s00508-022-02072-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pikis S, Mantziaris G, Kormath Anand R, et al. Stereotactic radiosurgery for Koos grade IV vestibular schwannoma: a multi-institutional study. J Neurosurg. 2022;138(2):405–412. doi: 10.3171/2022.4.JNS22203. [DOI] [PubMed] [Google Scholar]
- 5. Balossier A, Régis J, Reyns N, et al. Repeat stereotactic radiosurgery for progressive vestibular schwannomas after previous radiosurgery: a systematic review and meta-analysis. Neurosurg Rev. 2021;44(6):3177–3188. doi: 10.1007/s10143-021-01528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]