Abstract
Background
The Planetary Health Diet Index (PHDI) measures adherence to the dietary pattern presented by the EAT-Lancet Commission, which aligns health and sustainability targets. There is a need to understand how PHDI scores correlate with dietary greenhouse gas emissions (GHGE) and how this differs from the carbon footprints of scores on established dietary recommendations. The objectives of this study were to compare how the PHDI, Healthy Eating Index-2015 (HEI-2015) and Dietary Approaches to Stop Hypertension (DASH) relate to (a) dietary GHGE and (b) to examine the influence of PHDI food components on dietary GHGE.
Methods
We used life cycle assessment data from the Database of Food Recall Impacts on the Environment for Nutrition and Dietary Studies to calculate the mean dietary GHGE of 8,128 adult participants in the 2015–2016 and 2017–2018 cycles of the National Health and Nutrition Examination Survey (NHANES). Poisson regression was used to estimate the association of (a) quintiles of diet score and (b) standardized dietary index Z-scores with dietary GHGE for PHDI, HEI-2015, and DASH scores. In secondary analyses, we used Poisson regression to assess the influence of individual PHDI component scores on dietary GHGE.
Results
We found that higher dietary quality on all three indices was correlated with lower dietary GHGE. The magnitude of the dietary quality-dietary GHGE relationship was larger for PHDI [-0.4, 95% CI (-0.5, -0.3) kg CO2 equivalents per one standard deviation change] and for DASH [-0.5, (-0.4, -0.6) kg CO2-equivalents] than for HEI-2015 [-0.2, (-0.2, -0.3) kg CO2-equivalents]. When examining PHDI component scores, we found that diet-related GHGE were driven largely by red and processed meat intake.
Conclusions
Improved dietary quality has the potential to lower the emissions impacts of US diets. Future efforts to promote healthy, sustainable diets could apply the recommendations of the established DASH guidelines as well as the new guidance provided by the PHDI to increase their environmental benefits.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12966-024-01581-y.
Keywords: EAT-Lancet Commission, Dietary patterns, Planetary Health Diet, Healthy eating index, Dietary approaches to stop hypertension, Dietary greenhouse gas emissions, NHANES, 24-hour recalls
Background
Over the past 50 years, global dietary shifts and accompanying changes in food production have played a significant role in environmental degradation [1, 2]. Specifically, increased consumption of ruminant meats has led to increased diet-related greenhouse gas emissions (GHGE) [3, 4], as has increasing intake of ultra-processed foods high in refined starches, added sugars, fats and oils that provide little nutritional value to the diet but demand significant environmental resources that could otherwise be used for healthy food production [2, 5]. Food production makes up 16% of all GHGE in the US, a country for which per-capita emissions are more than three times the global average [6, 7]. Beyond environmental impact, these dietary shifts are also a key part of the nutrition transition and are a major contributor to the burden of non-communicable disease in the US [8, 9].
In this context, dietary guidelines are one strategy to alter consumer behavior and the composition of federal food policies, with the potential for food production to shift in response to changing dietary preferences [10]. One such set of dietary recommendations is those released by the EAT-Lancet Commission on Food, Planet, Health, which are unique in their explicit aim to jointly promote sustainability and human health. Their recommendations are an omnivorous diet that consists mostly of plant-based foods and allows for small amount of animal products [1]. The Planetary Health Diet Index (PHDI) is a dietary quality tool designed to measure adherence to these recommendations [11].
Previous research in the US has consistently found that healthy plant-based diets are associated with lower diet-related GHGE, while unhealthy plant-based diets do not necessarily have the same environmental benefits [12–14]. In this context, the PHDI can fill an important gap, as it is a novel a priori measure that considers both environmental sustainability and health outcomes. But to date, no study has examined how American diets align with the recommendations of the PHDI and how PHDI scores in the US correlate with dietary GHGE. Other commonly used dietary indices in the US primarily exist to inform health outcomes. For example, the Healthy Eating Index (HEI) quantifies adherence to the Dietary Guidelines for Americans (DGAs), which are designed to promote nutrient adequacy and prevent disease in the American population [15]. Results on the associations between diet quality as measured by the DGAs and diet-related GHGE have been mixed [13, 16–18]. Another example is the Dietary Approaches to Stop Hypertension (DASH), which is designed to prevent cardiovascular disease [19]. To justify incorporating more climate-focused dietary recommendations into US food policies—such as those recommended by the EAT-Lancet Commission and captured by the PHDI—there is a need to assess how current dietary patterns in the US align with this guidance and compare how diet-related GHGEs of individuals adhering to PHDI differ from adherence to dietary recommendations already in use.
Additionally, certain foods—such as red meat—are known to have much higher emissions impacts than others [4]. Therefore, it is important to understand whether the associations with indices such as PHDI and dietary GHGE are driven by overall differences in dietary quality, or if individual components are driving these differences.
The primary objective of this study was to compare the performance of PHDI with the Healthy Eating Index-2015 (HEI-2015) and Dietary Approaches to Stop Hypertension (DASH) with respect to diet-related GHGE. We further examine the influence of individual PHDI food components on diet-related GHGE.
Methods
Study population
The US National Health and Nutrition Examination Survey (NHANES) is a repeated cross-sectional survey that obtains a nationally-representative sample of the civilian, non-institutionalized population of the United States [20]. Two cycles of NHANES are recommended to obtain reliable estimates of population-level means [21, 22], so we included data from the two most recently available NHANES cycles unaffected by the COVID-19 pandemic. Eligible participants were non-pregnant or lactating individuals aged 20 years or older who participated in the 2015–2016 or 2017–2018 NHANES cycle and for whom two days of valid dietary intake data were available. Participants whose mean total energy intake was < 500 kcal or > 8000 kcal/day were excluded [23].
Assessment of dietary intake
Trained NCHS interviewers used the Automated Multiple Pass Method to gather 24-hour dietary recall data on all foods and beverages consumed by participants on the previous day [24]. The second dietary interview was conducted via an unannounced phone call three to ten days after the initial face-to-face interview.
Twenty-four hour dietary recall data were merged to the Food Patterns Equivalent Database (FPED), which uses the USDA Food Composition Table to categorize foods into the 37 USDA Food Pattern Components. For single-ingredient food items, FPED assigns foods directly to the corresponding component. For multi-ingredient foods with ingredients from more than one component, FPED disaggregates these items into their component ingredients using standard recipe files [25]. We converted the food pattern equivalents measurements (e.g., cups, ounces, teaspoons) to grams via a method described elsewhere [26]. Because cow’s milk is approximately 90% water, we used FPED’s cup-equivalents of dairy rather than grams of dairy to better represent the nutrient density and environmental impact of the various dairy foods (e.g., milk vs. cheese) [14].
Dietary recall data also provided estimates of participants’ total energy intake.
Dietary indices
To validate the PHDI’s recommendations with respect to emissions, we compared the PHDI with two other commonly used dietary indices, the Healthy Eating Index-2015 (HEI-2015) [15] and the Dietary Approaches to Stop Hypertension (DASH) [19].
The PHDI measures adherence to the recommendations of the EAT-Lancet Commission Scientific Report [1]. Its purpose is to provide evidence-based recommendations that promote human health and operate within planetary boundaries. PHDI consists of fourteen components scored from 0 to 10 points each, six of which are adequacy components and eight of which are moderation components. Therefore, the theoretical range of the PHDI is 0 to 140. Additional details on the derivation of the PHDI are available elsewhere [11, 26].
The HEI-2015 is a quantitative measure of adherence to the US Dietary Guidelines for Americans (DGAs), which are dietary recommendations published by the federal government to help the American population meet nutritional requirements, prevent chronic disease, and promote health. They are used as the basis for federal food and nutrition policy [15, 27]. HEI-2015 consists of thirteen components, nine of which are adequacy components (three scored from 0 to 10 points, six scored from 0 to 5 points) and four of which are moderation components (all scored from 0 to 10 points). The theoretical range of the HEI-2015 is 0-100 points, and the minimum and maximum scoring criteria for each food group are described in detail elsewhere [28, 29].
For both PHDI and HEI-2015, the scoring for components is assigned based on a priori quantities and participant intakes between the minimum and maximum were scored proportionately.
DASH is specifically designed to maintain a healthy blood pressure and has been adapted in settings throughout the globe. It consists of eight components, five of which are adequacy components and three of which are moderation components. Scores for each category range from 1 to 5, as described by Fung et al. [30]. Unlike PHDI or HEI-2015, DASH scores are defined by the underlying distribution of component intake in the study population, rather than by a priori quantities. DASH values range from 8 to 40 [29, 31].
For all three indices, component scores were summed to create a total index value, with a higher value indicating better adherence to the dietary recommendations and higher dietary quality. A summary table of the components of the three indices is available in Supplemental Table 1.
Calculation of diet-related GHGE
We used data from the database of Food Recall Impacts on the Environment for Nutrition and Dietary Studies (dataFRIENDS) to obtain diet-related GHGE estimates. The methodology of dataFRIENDS is described in detail elsewhere [32]. Briefly, dataFRIENDS relies on the linkage between the Food Commodities Intake Database (FCID) with individual dietary data from NHANES. FCID was a database developed by the US Environmental Protection Agency to enable a diet-level analysis of food commodities. The FCID database contains a recipe file that links foods reported in NHANES to ingredients in the form of 332 commodities. To create dataFRIENDS, Heller and colleagues conducted a literature review and calculated the greenhouse gas emissions associated with each of the 332 commodities in FCID from seed to farm gate [17, 32]. Additionally, proxy assignments were made when direct matches were unavailable, and adjustments were made to account for differences in mass basis (for example, excluding inedible portions) [17, 32]. A team of three trained research assistants, led by a member of the original dataFRIENDS (version 1.0) team, applied the same methodology used to derive the publicly-available version of dataFRIENDS to obtain estimates for the 2015–2016 (v2.0) [33] and 2017–2018 (v3.0) cycles of NHANES.
GHGE data are reported in kilogram CO2-equivalents (CO2-eq) per edible kilogram (kg) of food, which reflect global warming potential. Using the dataFRIENDS linkage described above, the total GHG can be calculated for each NHANES participant by summing over all food items reported in the 24-hour recalls. Because we used the mean of two days of dietary recall to derive the dietary index exposure variable, we calculated mean emissions from two days of dietary recall as the outcome.
Sociodemographic characteristics
All sociodemographic information was self-reported as part of a standardized questionnaire. Age data were modeled in continuous years. Income data were classified using the Poverty Income Ratio (PIR), a measure of family income relative to the Federal Poverty Level that accounts for household size. Income was categorized as PIR 0–185%, PIR 186–399%, PIR ≥ 400%, and Missing (due to high missingness in self-reported income, 8.1%) [34]. Education was reported in continuous years and classified as high school equivalent or lower, some college, and college degree or higher [35]. Race/ethnicity data were self-reported via categorical selection and classified as Non-Hispanic white, Non-Hispanic Black, Hispanic, and Other race/ethnicity (including Multiracial) [34, 36].
Analyses
In descriptive analyses, participants were classified into quintile of dietary GHGE and we compared the scores for each component in the highest vs. lowest quintile of GHGE.
Participants were classified into quintiles for each diet index (PHDI, HEI-2015, and DASH) and for dietary GHGE. Because of the skew in the diet-related GHGE outcome, Poisson regression models [37] were used to estimate the association between quintile of diet score and dietary GHGE. To directly compare the dietary indices, we created a standardized variable (Z-score) for each index and included this variable as a continuous exposure in Poisson regression. We compared the results from the continuous analysis using adjusted Wald tests. All models were adjusted for total energy intake.
To assess the influence of individual PHDI components on dietary GHGE, we conducted exploratory data analysis in which we regressed continuous dietary GHGE on each component score, both alone and controlling for overall PHDI score. To assess whether any individual PHDI components drove the observed associations of PHDI with dietary GHGE, we created 14 modified versions of the PHDI that was total PHDI score minus each respective component [38]. We then repeated our main analyses and regressed continuous GHGE on each of these modified scores. As in the main analyses, in these exploratory analyses all models were adjusted for total energy intake.
All analyses were conducted in Stata 17.0. We used a statistical significance level of p < 0.05 and applied the Bonferroni correction for multiple testing where appropriate. We accounted for the multistage sampling design of NHANES using the primary sampling unit and stratum variables and applied complex survey weights.
Results
The final sample included 8,128 eligible participants (Table 1, Supplemental Fig. 1). The range of PHDI values was 18–125 on a scale from 0 to 140, whereas HEI-2015 values ranged from 15 to 99 on a scale of 0-100, and DASH spanned the theoretical range of 8 to 40.
Table 1.
Characteristics of eligible participants with two days of dietary recall data, National Health and Nutrition Examination Survey 2015–2018*
| Sex | |
| Male | 49.1 (3954) |
| Female | 50.9 (4174) |
| Mean age (SD), years | 48.6 (15.6) |
| Educational attainment | |
| High school equivalent or lower | 35.5 (3425) |
| Some college | 32.1 (2575) |
| College degree or greater | 32.4 (2121) |
| Income | |
| Poverty-to-Income Ratio < 185% | 28.6 (3212) |
| Poverty-to-Income Ratio 185–399% | 28.3 (2217) |
| Poverty-to-Income Ratio ≥ 400% | 35.0 (1874) |
| Missing income information | 8.1 (825) |
| Race/ethnicity | |
| Non-Hispanic white | 64.1 (2949) |
| Non-Hispanic Black | 11.1 (1873) |
| Hispanic | 14.8 (2054) |
| Asian, Multiracial, and Other Non-Hispanic race/ethnicities | 10.0 (1252) |
| Median (IQR) Planetary Health Diet Index score | 68 (59, 77) |
| Median (IQR) Healthy Eating Index-2015 score | 53 (44, 63) |
| Median (IQR) Dietary Approaches to Stop Hypertension score | 24 (19, 28) |
| Median (IQR) diet-related greenhouse gas emissions | 3.9 (2.6, 5.8) |
* Values are weighted % (unweighted N) unless otherwise noted. Weighted % accounts for complex survey weights
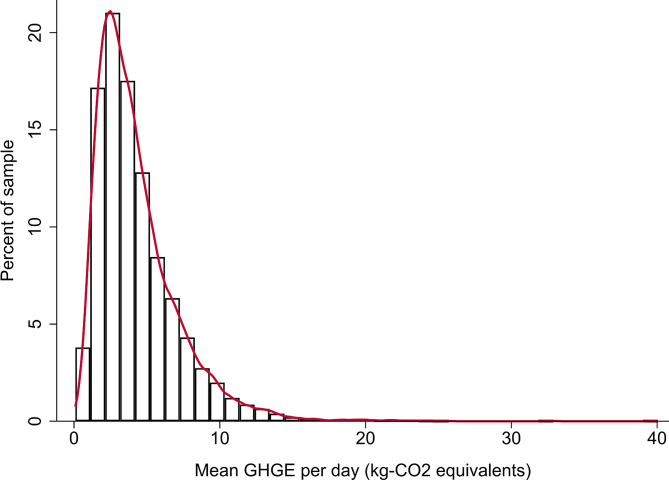
The distribution of per-capita dietary GHGE was skewed right, and median GHGE was 3.8 (IQR: 2.5–5.7) kg CO2-equivalents per person per day (Fig. 1).
Fig. 1.
Histogram of mean daily greenhouse gas emissions (GHGE) in kilograms-CO2 equivalents, National Health and Nutrition Examination Survey 2015–2018
We observed several differences in emissions by sociodemographic characteristics (Table 2). Mean dietary GHGE were higher for men than for women and for people with the highest levels of income, relative to those with the lowest income. Black individuals had lower dietary GHGE than any other racial/ethnic group. We did not observe any differences in diet-related GHGE by age or educational attainment.
Table 2.
Mean diet-related greenhouse gas emissions by sociodemographic characteristic, National Health and Nutrition Examination Survey 2015–2018*
| Estimated Emissions (kg CO2-eq person− 1 day− 1) (95% CI) |
p† | |
|---|---|---|
| Age | ||
| 20–29 | 4.3 (4.1, 4.5) | -- |
| 30–39 | 4.4 (4.2, 4.6) | 0.49 |
| 40–49 | 4.5 (4.3, 4.6) | 0.15 |
| 50–59 | 4.5 (4.3, 4.7) | 0.07 |
| 60–69 | 4.5 (4.2, 4.8) | 0.11 |
| 70–79 | 4.3 (4.1, 4.5) | 0.98 |
| 80 or older | 4.1 (3.9, 4.2) | 0.10 |
| Sex | ||
| Male | 4.7 (4.5, 4.9) | -- |
| Female | 4.1 (4.1, 4.2) | < 0.001 |
| Income | ||
| PIR≤1.30 | 4.3 (4.1, 4.4) | -- |
| PIR > 1.30–3.50 | 4.4 (4.2, 4.6) | 0.04 |
| PIR > 3.50 | 4.5 (4.3, 4.6) | 0.002 |
| Missing | 4.5 (4.3, 4.7) | 0.04 |
| Education | ||
| High school equivalent or lower | 4.6 (4.5, 4.8) | -- |
| Some college | 4.6 (4.4, 4.7) | 0.60 |
| College graduate or above | 4.4 (4.3, 4.6) | 0.06 |
| Race/Ethnicity | ||
| Non-Hispanic White | 4.4 (4.3, 4.6) | -- |
| Non-Hispanic Black | 4.1 (4.0, 4.3) | < 0.001 |
| Hispanic | 4.5 (4.4, 4.6) | 0.39 |
| Other race/ethnicity (including Multiracial) | 4.3 (4.1, 4.5) | 0.15 |
* Poisson regression models adjusted for total energy intake
† p-value for the contrast with the reference category
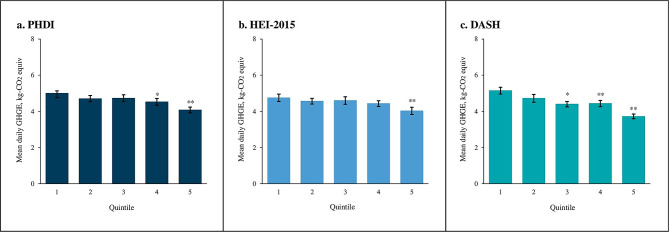
Being in a higher quintile of diet quality was associated with lower dietary GHGE for PHDI [5.0 (4.8, 5.2) in quintile 1 vs. 4.1 (3.9, 4.2) in quintile 5, p < 0.001, ptrend<0.001], HEI-2015 [4.8 (4.6, 5.0) in quintile 1 vs. 4.1 (3.9, 4.3) in quintile 5, p < 0.001, ptrend<0.001], and DASH [5.2 (5.0, 5.4) in quintile 1 vs. 3.8 (3.7, 3.9) in quintile 5, p < 0.001, ptrend<0.001] (Fig. 2, Supplemental Table 2). In analyses with standardized scores as the continuous exposure variable, a higher dietary score was similarly associated with lower dietary GHGE for all three indices. However, the magnitude of the association for standardized DASH [-0.51, (-0.60, -0.42) kg CO2-equivalents lower] was stronger than that observed for PHDI [-0.37 (-0.45, 0.28) kg CO2-equivalents lower, p < 0.001]. Both DASH and PHDI had a larger inverse association with diet-related GHGE than HEI-2015 [-0.25, (-0.33, -0.16) kg CO2-equivalents lower, all p < 0.001].
Fig. 2.
Predicted greenhouse gas emissions by quintile of Planetary Health Diet Index (PHDI), Healthy Eating Index-2015 (HEI-2015), and Dietary Approaches to Stop Hypertension (DASH), National Health and Nutrition Examination Survey 2015–2018*
* Poisson regression models adjusted for total energy intake
† *p < 0.01, **p < 0.001 for the difference from Quintile 1. With the application of the Bonferroni correction statistical significance is defined as p < 0.0125 (0.05/4 comparisons = 0.0125)
Several PHDI components were also associated with GHGE. For the adequacy components whose intake is encouraged, higher non-starchy vegetables score was associated with higher diet-related GHGE [0.05 (95% CI: 0.02, 0.08) kg CO2-equivalents increase per one-unit increase in non-starchy vegetable score], while higher scores for all other adequacy components were associated with lower diet-related GHGE (Table 3). For the moderation components for which limited intakes are recommended, higher scores for poultry [0.07 (0.05, 0.08) kg CO2 equivalents], for saturated oils and trans fats [0.05 (0.03, 0.07) kg CO2 equivalents] and for added sugar and fruit juice [0.09 (0.07, 0.11) kg CO2 equivalents] were associated with an increase in diet-related GHGE. Higher scores for red and processed meat [-0.43 (-0.46, -0.40) kg CO2 equivalents] and for dairy [-0.04 (-0.07, -0.01) kg CO2 equivalents] were associated with lower diet-related GHGE (Table 3). Because of the inverse relationship between intake and dietary score for the moderation components, this means that a lower intake of poultry, saturated oils and trans fats and of added sugar and fruit juice is correlated with higher GHGE, and lower intake of red and processed meat and of dairy is associated with lower GHGE. The magnitude and direction of the results were robust when including overall PHDI score as an additional predictor variable in the models. When the component score for red and processed meat was subtracted from the calculation of PHDI score, the association between PHDI score and mean GHGE was no longer statistically significant.
Table 3.
Association of Planetary Health Diet Index (PHDI) components with dietary greenhouse gas emissions (GHGE), National Health and Nutrition Examination Survey 2015–2018*†
| Component alone | Component controlling for total PHDI | PHDI score - component | |
|---|---|---|---|
| Adequacy components | |||
| Whole grains | -0.05*** (-0.06, -0.03) | -0.01 (-0.03, 0.01) | -0.03*** (-0.03, -0.02) |
| Whole fruits | -0.04** (-0.06, -0.01) | 0.01 (-0.01, 0.03) | -0.03*** (-0.03, -0.02) |
| Non-starchy vegetables | 0.05** (0.02, 0.08) | 0.13*** (0.09, 0.16) | -0.04*** (-0.05, -0.03) |
| Nuts and seeds | -0.08*** (-0.11, -0.06) | -0.05*** (-0.07, -0.02) | -0.02*** (-0.03, -0.02) |
| Total legumes | -0.08*** (-0.12, -0.04) | -0.02 (-0.06, 0.01) | -0.03** (-0.03, -0.02) |
| Unsaturated oils | -0.08*** (-0.11, -0.06) | -0.06** (-0.09, -0.02) | -0.02*** (-0.03, -0.02) |
| Moderation components | |||
| Starchy vegetables | -0.02 (-0.04, 0.01) | -0.01 (-0.04, 0.01) | -0.03** (-0.03, -0.02) |
| Dairy | -0.04* (-0.07, -0.01) | -0.03* (-0.06. -0.01) | -0.03*** (-0.03, -0.02) |
| Red and processed meat | -0.43*** (-0.46, -0.40) | -0.42*** (-0.45, -0.39) | 0.00 (-0.01, 0.01) |
| Poultry | 0.07*** (0.05, 0.08) | 0.09*** (0.07, 0.10) | -0.03*** (-0.04, -0.03) |
| Eggs | -0.02 (-0.05, 0.00) | 0.00 (-0.03, 0.02) | -0.03*** (-0.03, -0.02) |
| Fish | -0.04 (-0.07, 0.01) | -0.02 (-0.05, 0.00) | -0.03*** (-0.03, -0.02) |
| Saturated oils and trans fats | 0.05*** (0.03, 0.07) | 0.10*** (0.08, 0.13) | -0.04*** (-0.04, -0.03) |
| Added sugar and fruit juice | 0.09*** (0.07, 0.11) | 0.15*** (0.13, 0.18) | -0.04*** (-0.05, -0.03) |
* Values are coefficients from energy-adjusted Poisson regression and represent the predicted change in GHGE per a one-point increase in component or in modified PHDI score
† * p < 0.05, ** p < 0.01, *** p < 0.001 for the difference from 0
Discussion
We found that, in this nationally-representative survey of adults living in the US, improved dietary quality across the three dietary indices we examined was associated with lower GHGE. The inverse relationship between dietary quality and lower diet-related GHGE is consistent with several recent studies published in the US [12, 17]. Another NHANES study found that vegan, vegetarian, and pescetarian diets had higher dietary quality and lower diet-related GHGE than omnivorous, keto, or paleo diets [13]. Additionally, among participants who consumed omnivorous diets, an increase in DASH-score was associated with a decrease in diet-related GHGE [13]. Results from the Nurses’ Health Study similarly found that higher diet quality measured by the Alternative Healthy Eating Index and the Plant-based Diet Index were associated with lower diet-related GHGE [14]. Outside the US, diet quality has similarly been associated with lower GHGE in other high-income settings [39, 40].
However, not all studies have found that diets lower in GHGE necessarily have higher dietary quality [16, 41, 42]. The components analysis in our study reflects the inherent complexity of diet and the nuanced ways in which components influence estimates of nutritional quality and diet-related GHGE. Similar to our results, other studies have found that healthy plant-based foods such as whole grains, fruits, nuts, and legumes are associated with lower diet-related GHGE [17, 39, 41], but so are added sugars [17, 41] and ultra-processed foods [43–45]. At the same time, non-starchy vegetable intake has been associated with higher diet-related GHGE in other studies as well [17]. As outlined in the EAT-Lancet Commission report, policy actions to improve the environmental sustainability diet therefore cannot target only diet-related GHGE, but must consider trade-offs with nutrition as well [1].
However, one component—red and processed meat—had a much larger impact on diet-related GHGE than any other PHDI component. Red and processed meat have high production-associated GHGE [4], and diets high in this component are consistently found to have higher diet-related GHGE [46, 47]. The high emissions of red and processed meat could also explain why the associations of GHGE with PHDI and for DASH were stronger than those with HEI: PHDI and DASH both consider red meat as a moderation component to limit, whereas HEI does not. While red meat is a source of nutrients such iron and vitamin B12, at high intakes such as those observed in the US, it is also correlated with cardiovascular disease [48], type II diabetes [49], and certain cancers [50]. Moreover, in the US and other high-income contexts with high intake of animal-sourced foods, substituting red and processed meat in favor of more plant-based foods is estimated to have benefits for nutrient adequacy [51]. For the US context, dietary guidelines that recommend limited intake red and processed meat could reduce diet-related GHGE and improve population health.
The present study has several limitations. First, the life cycle assessment data are only for cradle-to-farm gate for the vast majority of foods [17, 32]. They generally do not include GHGE associated with packaging or transportation and are therefore an underestimate of the total GHGE footprint of the included foods. Additionally, we use two days 24-hour dietary recall data, which does not capture usual intake for individuals. However, the use of NHANES survey weights allow us to obtain nationally-representative, population-level estimates for the three dietary quality indices and for the PHDI component scores. Furthermore, we did not do a components-level analysis for HEI-2015 or for DASH. However, the focus of this manuscript is to validate the PHDI, and to see how its recommendations may be applied in a US context. We also do not examine how dietary patterns correlate other environmental indicators, such as water use, land use, or biodiversity loss. Future research should examine the relationship of these environmental indicators with dietary quality in the US.
Conclusions
Better dietary quality is associated with lower diet-related GHGE, with stronger associations for both PHDI and DASH than for HEI-2015. Red and processed meat—which is a moderation component for both PHDI and DASH—had the strongest influence on dietary GHGE. Future efforts to promote healthy, sustainable diets should reframe red and processed meat as a moderation component and could look to the established DASH guidelines as well as the new guidance provided by the PHDI.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to acknowledge Dr. Amelia Willits-Smith for her assistance with data preparation.
Abbreviations
- dataFRIENDS
database of Food Recall Impacts on the Environment for Nutrition and Dietary Studies
- DASH
Dietary Approaches to Stop Hypertension
- DGAs
Dietary Guidelines for Americans
- FPED
Food Patterns Equivalents Database
- GHGE
Greenhouse gas emissions
- HEI
Healthy Eating Index
- NHANES
National Health and Nutrition Examination Survey
- PHDI
Planetary Health Diet Index
- TEI
Total Energy Intake
- USDA
US Department of Agriculture
Authors’ contributions
SMF and LST designed research; DR acquired the data; SMF analyzed data; SMF and KM interpreted data; SMF drafted the paper; SMF, LMJ CLA, LSA, KM, DR, and LST substantively revised the paper; SMF had primary responsibility for final content. All authors read approved the final manuscript.
Funding
Funding from Wellcome Trust. The funders had no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Data availability
The datasets generated and/or analysed during the current study are available in the NHANES repository [https://www.cdc.gov/nchs/nhanes/index.htm].
Declarations
Ethical approval and consent to participate
Not applicable. Because the deidentified data are publicly available for download from the NHANES website, this study received a determination of “Not Human Subjects Research” from the Institutional Review Board at [institution redacted for blind peer review].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447–92. doi: 10.1016/S0140-6736(18)31788-4. [DOI] [PubMed] [Google Scholar]
- 2.Tilman D, Clark M. Global diets link environmental sustainability and human health. Nature. 2014;515(7528):518–22. doi: 10.1038/nature13959. [DOI] [PubMed] [Google Scholar]
- 3.Caro D, Davis SJ, Bastianoni S, Caldeira K. Greenhouse gas emissions due to meat production in the last fifty years. Quantification of climate variability, adaptation and mitigation for agricultural sustainability. 2017:27–37.
- 4.Poore J, Nemecek T. Reducing food’s environmental impacts through producers and consumers. Science. 2018;360(6392):987–92. doi: 10.1126/science.aaq0216. [DOI] [PubMed] [Google Scholar]
- 5.Anastasiou K, Baker P, Hadjikakou M, Hendrie G, Lawrence M. A conceptual framework for understanding the environmental impacts of ultra-processed foods and implications for sustainable food systems. J Clean Prod. 2022:133155.
- 6.Boehm R, Wilde PE, Ver Ploeg M, Costello C, Cash SB. A Comprehensive Life Cycle Assessment of Greenhouse Gas Emissions from U.S. Household Food choices. Food Policy. 2018;79:67–76. doi: 10.1016/j.foodpol.2018.05.004. [DOI] [Google Scholar]
- 7.Ritchie H, Roser M. CO2 and Greenhouse Gas Emissions: Our World in Data. https://ourworldindata.org/co2-emissions (2020). Accessed 21 March 2023.
- 8.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute for Health Metrics and Evaluation. GBD Compare. http://vizhub.healthdata.org/gbd-compare (2022). Accessed 21 March 2023.
- 10.Fanzo J, Davis C. Policies affecting Food environments and consumer behavior. Global Food Systems, diets, and Nutrition: linking Science, Economics, and policy. Cham: Springer International Publishing; 2021. pp. 131–52. [Google Scholar]
- 11.Bui LP, Pham TT, Wang F, Guasch-Ferre M, Willett WC. Planetary Health Diet Index and Risk of Total and cause-specific mortality in two prospective cohort studies. Curr Dev Nutr. 2023;7:100704. doi: 10.1016/j.cdnut.2023.100704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conrad Z, Drewnowski A, Love DC. Greater adherence to the Dietary guidelines for americans is associated with lower diet-related greenhouse gas emissions but higher costs. Front Nutr. 2023;10:1220016. doi: 10.3389/fnut.2023.1220016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Malley K, Willits-Smith A, Rose D. Popular diets as selected by adults in the United States show wide variation in carbon footprints and diet quality. Am J Clin Nutr. 2023;117(7):701–8. doi: 10.1016/j.ajcnut.2023.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Musicus AA, Wang DD, Janiszewski M, Eshel G, Blondin SA, Willett W, et al. Health and environmental impacts of plant-rich dietary patterns: a US prospective cohort study. Lancet Planet Health. 2022;6(11):e892–900. doi: 10.1016/S2542-5196(22)00243-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dietary Gudelines for Americans. 2015–2020. 8th ed. U.S Department of Agriculture and U.S. Department of Health and Human Services; 2020.
- 16.Conrad Z, Drewnowski A, Belury MA, Love DC. Greenhouse gas emissions, cost, and diet quality of specific diet patterns in the United States. Am J Clin Nutr. 2023;117(6):1186–94. doi: 10.1016/j.ajcnut.2023.04.018. [DOI] [PubMed] [Google Scholar]
- 17.Rose D, Heller MC, Willits-Smith AM, Meyer RJ. Carbon footprint of self-selected US diets: nutritional, demographic, and behavioral correlates. Am J Clin Nutr. 2019;109(3):526–34. doi: 10.1093/ajcn/nqy327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blackstone NT, Conrad Z. Comparing the recommended eating patterns of the EAT-Lancet Commission and Dietary guidelines for americans: implications for Sustainable Nutrition. Curr Dev Nutr. 2020;4(3). [DOI] [PMC free article] [PubMed]
- 19.Sacks FM, Obarzanek E, Windhauser MM, Svetkey LP, Vollmer WM, McCullough M, et al. Rationale and design of the Dietary approaches to stop hypertension trial (DASH): a multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann Epidemiol. 1995;5(2):108–18. doi: 10.1016/1047-2797(94)00055-X. [DOI] [PubMed] [Google Scholar]
- 20.National Health and Nutrition Examination Survey (NHANES) MEC In-Person dietary interviewers procedures manual. Hyattsville, MD: Centers for Disease Control, National Center for Health Statistics; 2017. [Google Scholar]
- 21.National Health and Nutrition Examination Survey - Module 5 . Reliability of estimates. Hyattsville, MD: Centers for Disease Control, National Center for Health Statistics; 2023. [Google Scholar]
- 22.Parker J, Talih M, Malec DJ, Beresovsky V, Carroll MD, Gonzalez JF et al. National Center for Health Statistics Data presentation: Standards for proportions. 2017. [PubMed]
- 23.Willett W. Nutritional epidemiology. Oxford University Press; 2012.
- 24.Steinfeldt L, Anand J, Murayi T. Food reporting patterns in the USDA automated multiple-pass method. Procedia Food Sci. 2013;2:145–56. doi: 10.1016/j.profoo.2013.04.022. [DOI] [Google Scholar]
- 25.Food Patterns Equivalents Database 2017–2018: methodology and user guide. Beltsville, Maryland: Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture; 2020.
- 26.Frank SM, Jaacks LM, Adair LS, Avery CL, Meyer K, Rose D, Taillie LS. Adherence to the Planetary Health Diet Index and Correlation with Nutrients of Public Health Concern: An analysis of NHANES 2003–2018. Am J Clin Nutr. 2024. In press [DOI] [PMC free article] [PubMed]
- 27.Dietary Gudelines for Americans. 2020–2025. 9th ed. U.S Department of Agriculture and U.S. Department of Health and Human Services; 2020.
- 28.Frank SM, Webster J, McKenzie B, Geldsetzer P, Manne-Goehler J, Andall-Brereton G, et al. Consumption of fruits and vegetables among individuals 15 years and older in 28 low- and Middle-Income Countries. J Nutr. 2019;149(7):1252–9. doi: 10.1093/jn/nxz040. [DOI] [PubMed] [Google Scholar]
- 29.Struijk EA, Hagan KA, Fung TT, Hu FB, Rodríguez-Artalejo F, Lopez-Garcia E. Diet quality and risk of frailty among older women in the nurses’ Health Study. Am J Clin Nutr. 2020;111(4):877–83. doi: 10.1093/ajcn/nqaa028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 31.Hu EA, Steffen LM, Coresh J, Appel LJ, Rebholz CM. Adherence to the healthy eating Index–2015 and other dietary patterns may reduce risk of Cardiovascular Disease, Cardiovascular Mortality, and all-cause mortality. J Nutr. 2020;150(2):312–21. doi: 10.1093/jn/nxz218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heller MC, Willits-Smith A, Meyer R, Keoleian GA, Rose D. Greenhouse gas emissions and energy use associated with production of individual self-selected US diets. Environ Res Lett. 2018;13(4):044004. doi: 10.1088/1748-9326/aab0ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Willits-Smith A. Food choices in the United States: Opportunities for health and sustainability co-benefits. Doctoral dissertation, Tulane University; ProQuest Dissertations & Theses Global. 2022: Document ID 2777133816.
- 34.Lacko AM, Maselko J, Popkin B, Ng SW. Socio-economic and racial/ethnic disparities in the nutritional quality of packaged food purchases in the USA, 2008–2018. Public Health Nutr. 2021:1–13. [DOI] [PMC free article] [PubMed]
- 35.Frank SM, Jaacks LM, Batis C, Vanderlee L, Taillie LS. Patterns of Red and processed meat consumption across North America: a nationally Representative Cross-sectional comparison of Dietary recalls from Canada, Mexico, and the United States. Int J Environ Res Public Health. 2021;18(1):357. doi: 10.3390/ijerph18010357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Health and Nutrition Examination Survey (NHANES) Interviewer procedures manual. Hyattsville, MD: Centers for Disease Control, National Center for Health Statistics; 2017. [Google Scholar]
- 37.Gould W. The Stata Blog. https://blog.stata.com/2011/08/22/use-poisson-rather-than-regress-tell-a-friend/ (2011). Accessed 9 February 2023.
- 38.Shannon OM, Ranson JM, Gregory S, Macpherson H, Milte C, Lentjes M, et al. Mediterranean diet adherence is associated with lower dementia risk, independent of genetic predisposition: findings from the UK Biobank prospective cohort study. BMC Med. 2023;21(1):1–13. doi: 10.1186/s12916-023-02772-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Auclair O, Burgos SA. Carbon footprint of Canadian self-selected diets: comparing intake of foods, nutrients, and diet quality between low-and high-greenhouse gas emission diets. J Clean Prod. 2021;316:128245. doi: 10.1016/j.jclepro.2021.128245. [DOI] [Google Scholar]
- 40.Cobiac LJ, Scarborough P. Modelling the health co-benefits of sustainable diets in the UK, France, Finland, Italy and Sweden. Eur J Clin Nutr. 2019;73(4):624–33. doi: 10.1038/s41430-019-0401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vieux F, Soler L-G, Touazi D, Darmon N. High nutritional quality is not associated with low greenhouse gas emissions in self-selected diets of French adults. Am J Clin Nutr. 2013;97(3):569–83. doi: 10.3945/ajcn.112.035105. [DOI] [PubMed] [Google Scholar]
- 42.Payne CL, Scarborough P, Cobiac L. Do low-carbon-emission diets lead to higher nutritional quality and positive health outcomes? A systematic review of the literature. Public Health Nutr. 2016;19(14):2654–61. doi: 10.1017/S1368980016000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jayaswal R, Frank SM, Martinez-Steele E, Rose D, Taillie LS. Ultra-processed food consumption and dietary greenhouse gas emissions among US adults from 2007–2010. Am J Clin Nutr. 2023;Under review.
- 44.Vellinga RE, van Bakel M, Biesbroek S, Toxopeus IB, de Valk E, Hollander A, et al. Evaluation of foods, drinks and diets in the Netherlands according to the degree of processing for nutritional quality, environmental impact and food costs. BMC Public Health. 2022;22(1):877. doi: 10.1186/s12889-022-13282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garzillo JMF, Poli VFS, Leite FHM, Steele EM, Machado PP, Louzada MLC, et al. Ultra-processed food intake and diet carbon and water footprints: a national study in Brazil. Rev Saude Publica. 2022;56:6. doi: 10.11606/s1518-8787.2022056004551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Springmann M, Clark M, Mason-D’Croz D, Wiebe K, Bodirsky BL, Lassaletta L, et al. Options for keeping the food system within environmental limits. Nature. 2018;562(7728):519–25. doi: 10.1038/s41586-018-0594-0. [DOI] [PubMed] [Google Scholar]
- 47.Boehm R, Ver Ploeg M, Wilde PE, Cash SB. Greenhouse gas emissions, total food spending and diet quality by share of household food spending on red meat: results from a nationally representative sample of US households. Public Health Nutr. 2019;22(10):1794–806. doi: 10.1017/S136898001800407X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhong VW, Van Horn L, Greenland P, Carnethon MR, Ning H, Wilkins JT, et al. Associations of processed meat, unprocessed red meat, poultry, or fish intake with incident cardiovascular disease and all-cause mortality. JAMA Intern Med. 2020;180(4):503–12. doi: 10.1001/jamainternmed.2019.6969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94(4):1088–96. doi: 10.3945/ajcn.111.018978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16(16):1599–600. doi: 10.1016/S1470-2045(15)00444-1. [DOI] [PubMed] [Google Scholar]
- 51.Springmann M, Wiebe K, Mason-D’Croz D, Sulser TB, Rayner M, Scarborough P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet Health. 2018;2(10):e451–61. doi: 10.1016/S2542-5196(18)30206-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are available in the NHANES repository [https://www.cdc.gov/nchs/nhanes/index.htm].