Abstract
Objective
This study aimed to determine the usability of the EMPOWER-SUSTAIN Self-Management Mobile App© and evaluate the factors associated with its usability among patients with cardiovascular risk factors in primary care.
Methodology
This was a cross-sectional study, conducted among patients aged ≥ 18 years with cardiovascular risk factors attending a university primary care clinic. Patients were given the app to use for at least three months. Those who fulfilled the eligibility criteria were recruited. Data gathered were on sociodemographic, clinical characteristics, self-management support by doctors, utilisation of the app at home and social support in using the app. The previously translated and validated Malay version of the mHealth App Usability Questionnaire was used to measure usability. The mean usability score was calculated and linear regressions analysis was conducted to determine the factors associated with the usability of the app.
Results
A total of 247 patients with at least one cardiovascular risk factor(s) were recruited. The mean age was 60.2 (±8.2). The majority were Malays (86.2%) and half of them were males (52.2%). The total mean (±SD) usability score was 5.26 (±0.67) indicating a high usability of the app. Usability of the app declined with increasing age in the simple linear regressions analysis. The multiple linear regressions yielded that being Malay (b = 0.31, 95% CI 0.08,0.54), using the app at home to understand their medications (b = 0.33, 95% CI 0.12,0.53) and having social support from family members and friends (b = 0.28, 95% CI 0.07,0.49) were significantly associated with higher usability of the app.
Conclusion
The usability of the EMPOWER-SUSTAIN Self-Management Mobile App© was high among patients with cardiovascular risk factors in our primary care clinic. This finding supports the widespread use of this app among our patients. Involvement of family members and friends should be encouraged to improve the usability of the app.
Keywords: Digital health, mHealth app, usability, Malay version of the mHealth App Usability Questionnaire, cardiovascular risk factors, primary care
Introduction
Background
Cardiovascular disease (CVD) is the principal cause of death and disability worldwide, with 366 million disability-adjusted life years attributed to CVD in 2017. 1 Four major cardiovascular (CV) risk factors i.e., hypertension, type 2 diabetes mellitus (T2DM), dyslipidaemia and obesity have been identified to cause CVD. 1 In Malaysia, the clustering of multiple CV risk factors has undoubtedly contributed towards CVD being the number one cause of death over the last three decades.2,3 The National Health and Morbidity Survey (NHMS) 2019 found that a staggering 3.4 million people lived with two major risk factors while another 1.7 million people lived with three major risk factors. 2 Out of all deaths, CVD was responsible for 35%, with coronary artery disease contributing 15% and stroke 8%. 3 Meanwhile, 18% of CVD deaths in 2020 were premature, occurring in the age group of 41–59 years old. 3
In Malaysia, most patients with CV risk factors are managed in primary care. 4 However, the majority of them do not achieve control targets.4–8 Suboptimal management of long-term conditions such as those with CV risk factors leads to CVD complications.4–8 In order to improve outcomes, the Chronic Care Model (CCM) provides a conceptual framework for healthcare system change in managing long-term conditions. 9 This model describes six integrated elements i.e., health system structure, self-management support, delivery system architecture, decision support, clinical information system and community resources.9,10 Among the elements of CCM, self-management support has been acknowledged as one of the key elements to improve outcomes, especially for those with CV risk factors. 11
Traditionally, self-management support tools for patients with multiple CV risk factors were developed using paper-based materials e.g., the EMPOWER-SUSTAIN Global Cardiovascular Risks Self-Management Booklet©.12,13 The exponential use of mobile phones in the last two decades unlocks the potential to digitise paper-based self-management tools into an app using mobile health (mHealth) technology. 13 With this in mind, the booklet was transformed into the EMPOWER-SUSTAIN Self-Management Mobile App©.13,14 This app consists of eight sections, namely ‘My Profile’, ‘My Cardiovascular Risks’, ‘My Treatment Targets’, ‘My Check-Up’, ‘My Weight Management’, ‘My Smoking Habit’, ‘My Self-Management’ and ‘My Medication’.13,14 The design, development, testing and refinement of the mobile app, including its specific features and functionalities to support CV risk factor self-management have been elaborated in great details in a recent publication. 14 The section on ‘My Self-Management’ consists of subsections on ‘My Home Blood Pressure’, ‘My Home Blood Sugar’, ‘My Daily Food Plan’, ‘My Exercise’ and ‘My Achievement’ where patients can use the app to record and monitor their blood pressure (BP), blood sugar, daily food intake and exercise at home. 14 This mobile app is currently being used in the EMPOWER-SUSTAIN Clinic at our primary care centre among patients with CV risk factors. However, the usability of this app among these patients was not known.
Objectives
Therefore, the objectives of this study were to determine the usability of the EMPOWER-SUSTAIN Self-Management Mobile App© and to evaluate the factors associated with its usability among patients with CV risk factors in primary care.
Methods
Study design, setting and population
This was a cross-sectional study conducted at the EMPOWER-SUSTAIN Clinic, which is located at a university primary care centre in Klang Valley, Malaysia from June 2021 to June 2023. The study population was patients with at least one CV risk factor attending the EMPOWER-SUSTAIN Clinic who fulfilled the inclusion and exclusion criteria.
Inclusion and exclusion criteria
This study included patients aged 18–80 years who fulfilled the following criteria:
Have at least one CV risk factor(s) i.e., clinician's diagnosis of hypertension, and/or T2DM, and/or dyslipidaemia, and/or obesity.
Were able to read and understand the Malay language.
Have an Android smartphone for installation of the app.
Have the EMPOWER-SUSTAIN Self-Management Mobile App© installed for at least 3 months.
Attended the EMPOWER-SUSTAIN Clinic at least twice within 6 months.
Patients who fulfilled any of the following criteria were excluded from the study:
Diagnosed with circulatory disorders requiring secondary care over the past 1 year (e.g., acute coronary syndrome, stroke, transient ischaemic attacks, peripheral vascular disease).
On renal dialysis.
Presented with severe hypertension (systolic BP > 180 mmHg and/or diastolic BP > 110 mmHg).
On radiotherapy/chemotherapy or palliative care.
Had any form of mental disorder or cognitive impairment that would affect the ability to answer the questionnaire, for example, dementia or mental retardation.
Pregnant.
Definition of terms and study variables
Usability was defined as ‘the extent to which a product can be used by specified users to achieve specified goals with effectiveness, efficiency, and satisfaction in a specified context of use’.15,16 Household income groups were categorised into Bottom 40%; B40 (<RM4850), Middle 40%; M40 (RM4850–RM10959), and Top 20%; T20 (>RM10959) based on the Report of Household Income and Basic Amenities Survey 2019 by the Department of Statistics, Malaysia. 17 CV risk factors were defined as having any of the following conditions i.e., clinician's diagnosis of hypertension and/or T2DM and/or dyslipidaemia and/or obesity; body mass index (BMI) which were categorised into obese class I (27.5–34.9 kg/m²), obese class II (35.0–39.9 kg/m²) and extreme obesity class III (≥ 40 kg/m²). 18 A current smoker was defined as patients who were smoking any kind of tobacco product at the time of data collection. Ex-smokers were defined as those who had stopped smoking for more than a year, and non-smokers were defined as those who never smoked any tobacco product. Self-rated health status was defined as the patients’ perception of their own health condition based on the 2002 World Health Survey. 19 Treatment targets were defined according to the Malaysian Clinical Practice Guidelines (CPG) on the Management of Primary and Secondary Prevention of Cardiovascular Diseases 2017 20 and the CPG on the Management of Type 2 Diabetes Mellitus (6th Edition) 2020. 21 According to these guidelines, HbA1c of <7%, fasting plasma glucose (FPG) of <6.1 mmol/L, BP of <140/80 mmHg for diabetes and <140/90 mmHg for non-diabetes, total cholesterol (TC) < 5 mmol/L, high-density lipoprotein cholesterol (HDL-c) of > 1.0 in males and > 1.2 mmol/L in females, triglyceride (TG) of ≤1.7 mmol/L, and low-density lipoprotein cholesterol (LDL-c) of ≤2.6 mmol/L were defined as achieving the treatment targets.20,21 Optimum BMI was defined as 18.5–22.9 kg/m². 18 Social support was defined as ‘patients receiving support from family members/neighbours/friends to use the mobile app at home, which is inclusive of technical support’.
Study tool
The usability of the app was measured using the mHealth App Usability Questionnaire (MAUQ) 22 which has been translated and validated in the Malay language (M-MAUQ). 23 This questionnaire has excellent internal consistency reliability, with an overall Cronbach's value of 0.914. 23 The kappa statistic revealed excellent agreement between expert and user raters for both the content and face validities (>0.77). 23 Permission to use the M-MAUQ was obtained from the authors. This questionnaire consists of 18 items framed within three subscale domains which is summarised in Table 1.
Table 1.
Summary of the subscale domains of the Malay version of the mHealth App Usability Questionnaire (M-MAUQ) and the related items.
| Subscale domains | Item number | Statement |
|---|---|---|
| Ease of use | 1–5 |
|
| Interface and satisfaction | 6–12 |
|
| Usefulness | 13–18 |
|
Each item was rated using a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). The mean and standard deviation (±SD) for the individual items in the M-MAUQ were calculated. Subsequently, the total mean score and the mean scores of the three subscale domains were calculated. A higher mean score indicates better usability, where a mean score of ≥4 gives an indication of a high usability of a mHealth app.22,23
Recruitment and data collection procedures
Patients with at least one CV risk factors (hypertension and/or T2DM and/or dyslipidaemia and/or obesity) who were already using the EMPOWER-SUSTAIN Global Cardiovascular Risks Self-Management Booklet© were approached in the nurse's assessment room. They were invited to use the EMPOWER-SUSTAIN Self-Management Mobile App©. Once they agreed, this app was installed into the patients’ Android smartphone. They were given a username and password to access the app. A brief explanation on how to use the app was given. The above steps were conducted between June 2021 and December 2022 to ensure that the patients had the app for at least three months prior to their recruitment into the cross-sectional study. These patients were then given an appointment to be seen at the EMPOWER-SUSTAIN Clinic. This specialised service clinic was set up under the university primary care centre for patients who are using the EMPOWER-SUSTAIN Self-Management Mobile App©.
Recruitment and data collection were conducted from November 2021 to April 2023. Patients were recruited during their second visit to the EMPOWER-SUSTAIN Clinic. A universal sampling method was used in this study whereby all patients attending the EMPOWER-SUSTAIN Clinic were invited to participate. Four research assistants were trained to recruit patients and collect the data in order to maintain a standardised method. Patients were approached in the nurse's assessment room and invited to participate. They were given the study information sheet containing background, purpose, benefit, procedure, confidentiality status, and contact information for the study. The patient was then screened for eligibility according to the inclusion and exclusion criteria. Those who fulfilled the eligibility criteria and agreed to participate were recruited. Written informed consent was obtained from all participants involved in the study.
Socio-demographic data, which included age, gender, marital status, education level, employment status and household income were collected. Data on clinical factors i.e., self-reported health status and smoking status were also collected. Weight in kilogram were measured using Seca® weighing scale and standing height in centimetre were measured using Seca® stadiometer. BMI was calculated as weight in kilograms divided by the square of the height in meter. BP in mmHg was measured twice using a Welch Allyn® automated digital BP monitor, taken two minutes apart on the right arm in a sitting position. The average of the two BP readings were used for analysis. Patients’ blood investigation results i.e., HbA1c and fasting serum lipid i.e., TC, TG, HDL-c and LDL-c done within the last 1 year, were retrieved from the electronic medical record.
Questionnaire administration
The M-MAUQ was given to the participants to be self-administered. Prior to the questionnaire administration, a clear verbal instruction on how to fill out the questionnaire was given. Participants were reminded to complete the questionnaire in approximately 30 minutes without referring to notes or family members. They were free to ask for clarification from the research assistants at any time should any query arise. Once the questionnaire was completed, participants returned them directly to the research assistants, who then checked for completeness.
Sample size determination
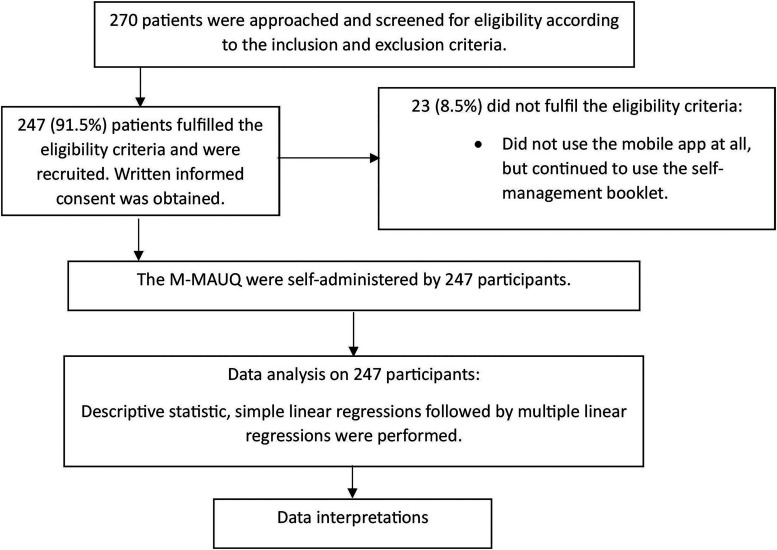
A single mean formula [n = (z σ/Δ)², z = 1.96 (95% confidence interval); σ = mean (SD) of the population and Δ = precision (0.05)] was used to calculate the sample size in this study. The assumption for the mean (±SD) was based on the usability of the Cora Health app, a self-management programme for hypertension, using the MAUQ. 24 This study found that the mean score (±SD) for the usefulness domain was 6.3 (±0.4). 24 Therefore, by taking α = 0.05, 80% power of study, SD of 0.4 and precision of 0.05, the minimum sample size needed for this study was 246. Considering a non-responder/non-eligibility rate of 10%, the study aimed to approach 270 patients.
Statistical analysis
Data was entered and analysed using the IBM SPSS version 28. 25 Continuous data was expressed as mean with ± SD for normally distributed data or median with interquartile range for non-normally distributed data. Categorical variables were described in numbers and percentages. Simple linear regression analysis was initially performed on 46 variables to determine the factors associated with usability scores. These included the sociodemographic and clinical factors of participants, self-management support given to patients by doctors, utilisation of the app at home by patients and social support they received in using the app. Variables with a p value of <0.25 from the simple linear regressions were included in the multiple linear regressions to determine the associated factors. The stepwise method was used for the analysis. The model assumptions of the linearity of the numerical independent variables and the normality and equal variance of the residuals were checked. Statistical significance was taken at a p value of <0.05.
Results
A total of 270 patients were approached and invited to participate. Out of this, 247 (91.5%) patients were eligible and recruited into the study. The flowchart of the conduct of the study is shown in Figure 1.
Figure 1.
The flowchart of the conduct of the study.
Table 2 summarises the demographic and clinical characteristics of the participants. The mean age was 60.2 (±8.2), with the highest age group being the middle age range of 55–64 years (45%). Out of 247 participants, the majority were Malays (86.2%), married (93.9%), never smoked (86.6%) and reported to have good health status (78.5%). More than half were males (52.2%), had tertiary education level (65.5%) and came from the B40 income group (59.1%).
Table 2.
Sociodemographic and clinical characteristics of participants (n = 247).
| Characteristic of participants | Frequency, n (%) | Mean(±SD) |
|---|---|---|
| Gender | ||
| Male | 129 (52.2) | |
| Female | 118 (47.8) | |
| Age | 60.2 (±8.2) | |
| Age group | ||
| 18–24 (Young adult) | 0 (0) | |
| 25–54 (Adult) | 51 (20.6) | |
| 55–64 (Middle age) | 111 (45.0) | |
| 65–80 (Elderly) | 85 (34.4) | |
| Ethnicity | ||
| Malay | 213 (86.2) | |
| Chinese | 11 (4.5) | |
| Indian | 22 (8.9) | |
| Others | 1 (0.4) | |
| Marital status | ||
| Single | 4 (1.6) | |
| Married | 232 (93.9) | |
| Widow/widower | 11 (4.5) | |
| Divorced | 0 (0) | |
| Education level | ||
| No education | 0 (0) | |
| Primary school | 12 (4.9) | |
| Secondary school | 73 (29.6) | |
| Tertiary education (College/University) | 162 (65.5) | |
| Employment status | ||
| Employed | 91 (36.8) | |
| Unemployed | 33 (13.4) | |
| Pensioner | 123 (49.8) | |
| Household income | ||
| B40 (<RM4850) | 146 (59.1) | |
| M40 (RM 4850–10959) | 77 (31.2) | |
| T20 (>RM 10959) | 24 (9.7) | |
| Smoking status | ||
| Non-smoker | 214 (86.6) | |
| Current smoker | 11 (4.5) | |
| Ex-smoker | 22 (8.9) | |
| Self-rated health status | ||
| Very good | 12 (4.9) | |
| Good | 194 (78.5) | |
| Moderate | 35 (14.2) | |
| Not good | 6 (2.4) | |
| Very bad | 0 (0) | |
| No. of CV risk factors | ||
| 1 | 24 (9.7) | |
| 2 | 84 (34) | |
| 3 | 89 (36) | |
| 4 | 50 (20.3) | |
| Diabetes mellitus | ||
| No | 124 (50.2) | |
| Yes | 123 (49.8) | |
| BMI target achieved (18.5-22.9 kg/m²) | ||
| No | 225 (91.1) | |
| Yes | 22 (8.9) | |
| BP target achieved (<140/80 for DM, < 140/90 for non-DM) | ||
| No | 101 (40.9) | |
| Yes | 146 (59.1) | |
| FPG/HbA1c target achieved (FPG <6.1 mmol/L or HbA1c < 7%) | ||
| No | 93 (37.7) | |
| Yes | 154 (62.3) | |
| TC target achieved (<5 mmol/L) | ||
| No | 66 (26.7) | |
| Yes | 181 (73.3) | |
| HDL-c target achieved (Male > 1.0 mmol/L/Female > 1.2 mmol/L) | ||
| No | 53 (21.5) | |
| Yes | 194 (78.5) | |
| TG target achieved (≤ 1.7 mmol/L) | ||
| No | 62 (25.1) | |
| Yes | 185 (74.9) | |
| LDL-c target achieved (≤ 2.6 mmol/L) | ||
| No | 82 (33.2) | |
| Yes | 165 (66.8) |
BMI: body mass index; FPG: fasting plasma glucose; BP: blood pressure; TC: total cholesterol; HDL-c: high-density lipoprotein cholesterol; TG: triglyceride; LDL-c: low-density lipoprotein cholesterol.
Table 3 shows self-management support given to patients by doctors. Majority of the patients had one treating doctor (92.7%) and they reported that their doctors used various sections of the mobile app during consultation, particularly to explain regarding treatment targets (98.8%) and investigation results (98.0%).
Table 3.
Self-management support given to patients by doctors (n = 247).
| Variables | Frequency, n (%) |
|---|---|
| Number of treating primary doctor/s | |
| 1 treating doctor | 229 (92.7) |
| >1 treating doctors | 18 (7.3) |
| Doctors used the mobile app with patients during consultation to explain regarding cardiovascular risk | |
| No | 16 (6.4) |
| Yes | 231 (93.6) |
| Doctors used the mobile app with patients during consultation to explain regarding treatment targets | |
| No | 3 (1.2) |
| Yes | 244 (98.8) |
| Doctors used the mobile app with patients during consultation to explain regarding investigation results | |
| No | 5 (2.0) |
| Yes | 242 (98.0) |
| Doctors used the mobile app with patients during consultation to explain regarding healthy diet | |
| No | 12 (4.9) |
| Yes | 235 (95.1) |
| Doctors used the mobile app with patients during consultation to explain regarding physical activities | |
| No | 11 (4.5) |
| Yes | 236 (95.5) |
| Doctors used the mobile app with patients during consultation to explain regarding blood pressure monitoring at home | |
| No | 14 (5.7) |
| Yes | 233 (94.3) |
| Doctors used the mobile app with patients during consultation to explain regarding blood glucose monitoring at home | |
| No | 24 (9.7) |
| Yes | 223 (90.3) |
| Doctors used the mobile app with patients during consultation to explain regarding medications | |
| No | 18 (7.3) |
| Yes | 229 (92.7) |
Table 4 shows the utilisation of the app at home by patients and social support that they received from their family members and friends. Patients reported that they used the app at home on average of <5 times per month (78.5%), particularly to understand their CV risks (87.4%), treatment targets (91.5%), investigation results (92.7%) and medications (78.9%). Regarding self-management at home, the majority of patients used the app to understand healthy diet (87.9%), physical activities (82.2%) and to monitor their BP (71.3%). The majority of patients also received social support in using the app from their family members and friends (80.2%).
Table 4.
Utilisation of the app at home by patients and social support they received (n = 247).
| Variables | Frequency, n (%) |
|---|---|
| Frequency of using the app/month | |
| <5 | 194 (78.5) |
| 5–15 | 31 (12.6) |
| >15 | 22 (8.9) |
| Patients used the mobile app at home to understand their cardiovascular risk | |
| No | 31 (12.6) |
| Yes | 216 (87.4) |
| Patients used the mobile app at home to understand their treatment targets | |
| No | 21 (8.5) |
| Yes | 226 (91.5) |
| Patients used the mobile app at home to understand their investigation results | |
| No | 18 (7.3) |
| Yes | 229 (92.7) |
| Patients used the mobile app at home to understand healthy diet | |
| No | 30 (12.1) |
| Yes | 217 (87.9) |
| Patients used the mobile app at home to understand physical activities | |
| No | 44 (17.8) |
| Yes | 203 (82.2) |
| Patients used the mobile app to monitor their blood pressure (BP) at home | |
| No | 71 (28.7) |
| Yes | 176 (71.3) |
| Patients used the mobile app to monitor their blood glucose at home | |
| No | 127 (51.4) |
| Yes | 120 (48.6) |
| Patients used the mobile app at home to understand their medications | |
| No | 52 (21.1) |
| Yes | 195 (78.9) |
| Received social support in using the app from family members and friends | |
| No | 49 (19.8) |
| Yes | 198 (80.2) |
Table 5 summarises the total mean usability score of the EMPOWER-SUSTAIN Self-Management Mobile App© and the mean score of each subscale domain, as measured by M-MAUQ. The total mean score was 5.26 (SD ±0.67). With regards to the subscale domains, the mean scores for ‘ease of use’, ‘interface and satisfaction’ and ‘usefulness’ were 5.89 (SD ± 0.79), 5.91 (SD ± 0.79) and 5.49 (SD ±0.78), respectively.
Table 5.
The Malay version of the mHealth App Usability Questionnaire (M-MAUQ) total mean score and the mean scores of the subscale domains.
| Subscale domains | Subscale item | Mean (±SD) | Min score | Max score |
|---|---|---|---|---|
| Ease of use | 1. The app was easy to use. | 6.03 (0.05) | 3.00 | 7.00 |
| 2. It was easy for me to learn to use the app. | 5.96 (0.85) | 2.00 | 7.00 | |
| 3. The navigation was consistent when moving between screens. | 5.95 (0.84) | 2.00 | 7.00 | |
| 4. The interface of the app allowed me to use all the functions (such as entering information, responding to reminders, viewing information) offered by the app. | 5.89 (0.88) | 2.00 | 7.00 | |
| 5. Whenever I made a mistake using the app, I could recover easily and quickly. | 5.62 (1.09) | 2.00 | 7.00 | |
| Mean score for subscale domain | 5.89 (0.79) | 2.60 | 7.00 | |
| Interface and satisfaction | 6. I like the interface of the app. | 5.95 (0.79) | 4.00 | 7.00 |
| 7. The information in the app was well organised, so I could easily find the information I needed. | 5.97 (0.87) | 2.00 | 7.00 | |
| 8. The app adequately acknowledged and provided information to let me know the progress of my action. | 5.85 (0.98) | 2.00 | 7.00 | |
| 9. I feel comfortable using this app in social settings. | 5.95 (0.89) | 2.00 | 7.00 | |
| 10. The amount of time involved in using this app has been fitting for me. | 5.80 (0.92) | 2.00 | 7.00 | |
| 11. I would use this app again. | 5.92 (0.86) | 1.00 | 7.00 | |
| 12. Overall, I am satisfied with this app. | 5.94 (0.83) | 2.00 | 7.00 | |
| Mean score for subscale domain | 5.91 (0.79) | 2.57 | 7.00 | |
| Usefulness | 13. The app would be useful for my health and well-being. | 6.00 (0.78) | 3.00 | 7.00 |
| 14. The app improved my access to health care services. | 6.04 (0.77) | 4.00 | 7.00 | |
| 15. The app helped me manage my health effectively. | 5.94 (0.85) | 2.00 | 7.00 | |
| 16. This app has all the functions and capabilities I expected it to have. | 5.83 (0.91) | 2.00 | 7.00 | |
| 17. I could use the app even when the Internet connection was poor or not available. | 3.29 (2.21) | 1.00 | 7.00 | |
| 18. This mHealth app provided an acceptable way to receive health care services, such as accessing educational materials, tracking my own activities, and performing self-assessment. | 5.88 (0.86) | 3.00 | 7.00 | |
| Mean score for subscale domain | 5.49 (0.78) | 3.50 | 7.00 | |
| Total mean score | 5.26 (0.67) | 2.83 | 6.22 |
Bold font = mean scores for the subscale domains and the total mean score.
Table 6 shows the factors associated with the usability of the mobile app generated from the linear regressions analysis. Out of 46 variables, the simple linear regressions yielded 24 factors with a p value of <0.25. These 24 factors were then included in the multiple linear regressions, where three factors were found to be significantly associated with a higher M-MAUQ usability score, explaining 10.9% of the variation (adjusted R² = 0.109). The three factors were Malay ethnicity (b = 0.31, 95% CI 0.08,0.54), used the app at home to understand their medications (b = 0.33, 95% CI 0.12,0.53), and received social support from family members and friends in using the app (b = 0.28, 95% CI 0.07,0.49). The regression analysis results for each of the usability domains are provided in Appendices 1, 2 and 3.
Table 6.
Factors associated with the usability of the mobile app among the study population using simple and multiple linear regressions (n = 247).
| Variables | Simple linear regressions | Multiple linear regressions | |||
|---|---|---|---|---|---|
| b (95% CI) | p value | b a (95% CI) | t-stat | p value | |
|
Gender Female, n = 118 Male, n = 129 |
0 −0.01(−0.19,0.15) |
0.842 |
- |
- |
- |
|
Age (years) Adult (25–54), n = 51 Middle age (55–64), n = 111 Elderly (65–80), n = 85 |
0 −0.13 (−0.35,0.09) −0.25 (−0.49, −0.02) |
0.254 0.034 |
- |
- |
- |
|
Ethnicity Non-Malay, n = 44 Malay, n = 213 |
0 0.34 (0.10,0.58) |
0.006 |
0 0.31 (0.08,0.54) |
2.65 |
0.009 |
|
Marital status Single, n = 4 Married, n = 232 Widow, n = 11 |
0 −0.64 (−1.30,0.03) −0.70 (−1.47,0.07) |
0.060 0.076 |
- |
- |
- |
|
Education level Primary school, n = 12 Secondary school, n = 73 Tertiary education (College/University), n = 162 |
0 0.21 (−0.62,0.20) 0.20 (−0.38,0.40) |
0.305 0.962 |
- |
- |
- |
|
Employment status Unemployed, n = 33 Employed, n = 91 Pensioner, n = 123 |
0 0.14 (−0.17,0.37) 0.13 (−0.18,0.34) |
0.470 0.547 |
- |
- |
- |
|
Household income T20 (>RM 10959), n = 24 M40 (RM 4850-10959), n = 77 B40 (<RM4850), n = 146 |
0 0.15 (−0.38,0.20) 0.16 (−0.16,0.46) |
0.523 0.331 |
- |
- |
- |
|
Smoking status Ex-smoker, n = 22 Non-smoker, n = 214 Current smoker, n = 11 |
0 0.51 (−0.18,0.42) 0.25 (−0.31,0.67) |
0.418 0.472 |
- |
- |
- |
|
Self-rated health status Not good, n = 6 Moderate, n = 35 Good, n = 194 Very good, n = 12 |
0 0.02 (−0.57,0.60) 0.26 (−0.28,0.81) 0.42 (−0.24,1.08) |
0.955 0.341 0.208 |
- |
- |
- |
|
Number of CV risk factors ≤2, n = 108 >2, n = 139 |
0 0.20 (0.04,0.37) |
0.018 |
- |
- |
- |
|
Diabetes mellitus No, n = 124 Yes, n = 123 |
0 0.12 (−0.05, 0.29) |
0.153 |
- |
- |
- |
|
BMI target achieved (18.5–22.9 kg/m²) No, n = 225 Yes, n = 22 |
0 0.18 (−0.11,048) |
0.225 |
- |
- |
- |
|
BP target achieved (<140/80 for DM, < 140/90 for non-DM) No, n = 101 Yes, n = 146 |
0 0.09 (−0.20,015) |
0.757 |
- |
- |
- |
|
TC target achieved (<5 mmol/L) No, n = 66 Yes, n = 181 |
0 0.16 (−0.03,0.35) |
0.097 |
- |
- |
- |
|
FPG/HbA1c target achieved (FPG <6.1 mmol/L or HbA1c < 7%) No, n = 93 Yes, n = 154 |
0 −0.23 (−0.21,014) |
0.720 |
- |
- |
- |
| HDL-c target achieved (Male >1.0 mmol/L/Female >1.2 mmol/L) No, n = 53 Yes, n = 194 |
0 0.10 (−0.26,015) |
0.575 |
- |
- |
- |
| TG target achieved (≤1.7 mmol/L) No, n = 62 Yes, n = 185 |
0 0.04 (−0.13,026) |
0.491 |
- |
- |
- |
|
LDL-c target achieved (≤2.6 mmol/L) No, n = 82 Yes, n = 165 |
0 0.14 (−0.04,0.32) |
0.129 |
- |
- |
- |
|
Number of treating primary doctor/s >1 treating doctor, n = 18 1 treating doctor, n = 229 |
0 0.14 (−0.35,0.21) |
0.615 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding cardiovascular risk No, n = 16 Yes, n = 231 |
0 0.17 (-0.19,0.49) |
0.390 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding treatment targets No, n = 3 Yes, n = 244 |
0 0.39 (−0.66,0.88) |
0.776 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding investigation results No, n = 5 Yes, n = 242 |
0 0.48 (−0.12, 1.08) |
0.115 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding healthy diet No, n = 12 Yes, n = 235 |
0 0.20 (−0.31,0.48) |
0.433 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding physical activities No, n = 11 Yes, n = 236 |
0 0.48 (0.07, 0.88) |
0.021 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding BP monitoring at home No, n = 14 Yes, n = 233 |
0 0.27 (−0.09, 0.64) |
0.139 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding blood glucose monitoring at home No, n = 24 Yes, n = 223 |
0 0.25 (−0.04, 0.53) |
0.087 |
- |
- |
- |
|
Doctors used the mobile app with patients during consultation to explain regarding medications No, n = 18 Yes, n = 229 |
0 0.45 (0.13, 0.76) |
0.007 |
- |
- |
- |
|
Frequency of using the app/month >15, n = 22 5-15, n = 31 <5, n = 194 |
0 0.18 (−0.35,0.37) 0.15 (−0.14,0.18) |
0.949 0.439 |
- |
- |
- |
|
Patients used the mobile app at home to understand their cardiovascular risk No, n = 31 Yes, n = 216 |
0 0.43 (0.18, 0.68) |
<0.001 |
- |
- |
- |
|
Patients used the mobile app at home to understand their treatment targets No, n = 21 Yes, n = 226 |
0 0.61 (0.32, 0.90) |
<0.001 |
- |
- |
- |
|
Patients used the mobile app at home to understand their investigation results No, n = 18 Yes, n = 229 |
0 0.50 (0.18, 0.82) |
0.002 |
- |
- |
- |
|
Patients used the mobile app at home to understand healthy diet No, n = 30 Yes, n = 217 |
0 0.28 (0.03, 054) |
0.031 |
- |
- |
- |
|
Patients used the mobile app at home to understand physical activities No, n = 44 Yes, n = 203 |
0 0.44 (0.22, 0.65) |
<0.001 |
- |
- |
- |
|
Patients used the mobile app to monitor their BP at home No, n = 71 Yes, n = 176 |
0 0.29 (0.11, 0.48) |
0.002 |
- |
- |
- |
|
Patients used the mobile app to monitor their blood glucose at home No, n = 127 Yes, n = 120 |
0 0.28 (0.12,0.45) |
<0.001 |
- |
- |
- |
|
Patients used the mobile app at home to understand their medications No, n = 52 Yes, n = 195 |
0 0.43 (0.23, 0.63) |
<0.001 |
0 0.33 (0.12,0.53) |
3.09 |
0.002 |
|
Received social support in using the app from family and friends No, n = 49 Yes, n = 198 |
0 0.40 (0.20, 0.61) |
<0.001 |
0 0.28 (0.07,0.49) |
2.59 |
0.010 |
For multiple linear regressions, bold font = variables with a p value of <0.05.
For simple linear regressions, bold font = variables with a p value of <0.25.
Dependent variable: Usability of the app (total mean score of M-MAUQ). Enter method is used for simple linear regressions. Stepwise multiple linear regressions method applied. Model assumptions were fulfilled. Statistically significant at p < 0.05. No multicollinearity detected. VIF < 5. There were no significant interactions amongst independent variables. Coefficients of determination (adjusted R²) = 0.109. 0 = reference group. CV: cardiovascular; VIF: variance inflation factor; M-MAUQ: Malay version of the mHealth App Usability Questionnaire; BMI: body mass index; FPG: fasting plasma glucose; BP: blood pressure; TC: total cholesterol; HDL-c: high-density lipoprotein cholesterol; TG: triglyceride; LDLD-c: low-density lipoprotein cholesterol.
Adjusted regression coefficient.
Therefore, the final linear regressions equation model for the usability of the app derived from the multiple linear regressions analysis is as below:
Total mean usability score = 4.51 + (0.31*Malay ethnicity) + (0.33*used the apps at home to understand their medications) + (0.28*social support in using the apps at home)
Being Malay is associated with higher usability of the app compared to the non-Malays. Meanwhile, patients who used the mobile app at home to understand their medications were associated with higher usability of the app compared to patients who did not use. Lastly, receiving social support in using the app from family members and friends were associated with higher usability of the app compared to those who did not receive social support.
Discussion
To the best of our knowledge, this is the first study to evaluate the usability of a self-management mobile app using the M-MAUQ among patients with CV risk factors in primary care. Our study shows that the total mean M-MAUQ score was 5.26 (SD ±0.67), indicating high usability of the EMPOWER-SUSTAIN Self-Management Mobile App© among our study population. Similarly, the mean usability scores for each of the subscale domains were also high [‘ease of use’: 5.89 (SD ±0.79), ‘interface and satisfaction’: 5.91 (SD ±0.79) and ‘usefulness’: 5.49 (SD ±0.78)]. Other studies using the MAUQ to measure usability of self-management apps are limited, making direct comparison difficult. 26 There was only one similar study by Alessa et al. 24 in 2021, which evaluated the usability of the Cora Health app, a self-management programme for hypertension, using the MAUQ among patients with hypertension in Saudi Arabia. Our finding is comparable to the finding of their study with regards to the subscale domain mean scores [‘ease of use’: 6.0 (SD ±0.20), ‘interface and satisfaction’: 6.2 (SD ±0.25) and ‘usefulness’: 6.3 (SD ±0.40). 24 This finding is supported by a qualitative study on patients’ perspectives on using a smartphone app to support home-based exercise which showed that patients used the app when it is easy to use, when it benefits them, and when the healthcare providers support the patients in its use. 27
With regards to the mobile app utilisation at home, we found that all of the participants used the app at home on average of <5 times per month, particularly to understand their CV risks, treatment targets, blood investigation results, healthy diet, physical activities, medications and also to monitor their BP. In general, this finding is comparable to a usability study of a disease management mobile app where patients with diabetes mellitus perceived the app as useful for disease management at home. 28
The simple linear regression analysis shows that the usability of the mobile app declined with age. However, the mean age of our study population was 60.2 (±8.2), and this is much older compared to the mean age of health app users among the general population in Malaysia which was 29.8 (±11.7) years old. 29 Those with >2 risk factors were found to be significantly associated with a higher usability of the app in the simple linear regressions analysis. This could be due to the possibility that patients with multiple CVD risk factors appreciate the app better, as this app was comprehensively designed for patients with multiple risk factors. However, these factors were not found to be significant in the final multiple linear regressions model.
With regards to the factors associated with high usability of the EMPOWER-SUSTAIN Self-Management Mobile App©, three factors were found to be significant from the multiple linear regressions i.e., Malay ethnicity, used the app to understand their medications, and received social support from family members and friends in using the app. With regards to ethnicity, the majority of the participants in our study were Malays (86.2%) and they were found to have a higher mean usability score compared with the non-Malay ethnic groups. Other studies revealed mixed outcomes when it comes to whether ethnicity influenced the use of mHealth in people with chronic diseases. 30
Using the app at home to understand their medications was another significant factor associated with a higher usability of the app found in our study. This finding is enlightening as various other studies have proven that patients using mHealth apps had better adherence to medications and better outcomes in their disease control compared to those who did not use mHealth apps.31,32 Therefore, primary care physicians should motivate their patients to use self-management mobile apps, especially to understand their medications, in order to improve adherence and outcomes.
Our study also shows that receiving social support from family members and friends was significantly associated with a higher usability of the app. Several other studies have also found a positive correlation between social support and usability of mHealth apps. A study on diabetes telemonitoring showed that incorporation of a support person (relative or friend) improved self-management and medication adherence. 33 A family-focused diabetes self-care support using mHealth intervention among low-income adults also showed that this intervention was usable and feasible in helping patients manage self-care support. 34 Interestingly, in contrast to the findings of our study, another study found that the use of diabetes apps increased in the absence of social support by family or friends due to compensation for lack of support, and decreased when such support is high due to no perceived need to use the technology. 35 However, evidence supporting the involvement of family members or friends in supporting the use of mHealth apps is far more robust. 36 Therefore, primary care physicians should encourage patients to involve their family and friends to support them in using a self-management app. Such initiatives will also empower everyone around them in the self-management of long-term conditions.
Strengths and limitations
One of the major strengths of this study is it addresses the gap in the literature where research evidence on the usability of a self-management mobile app in primary care among patients with CV risk factors is not well established. Additionally, studies using the MAUQ as a measure of usability of mHealth apps is also sparse, as this questionnaire was recently developed in 2019 22 and subsequently translated into the Malay language in 2021. 23 This poses a limitation for our study, as a direct comparison of our findings with other studies using the same usability measure was limited. Another limitation includes the use of a single primary care centre for sampling in our study where the majority of the participants were Malays. Other ethnic groups such as Chinese and Indians were underrepresented, rendering the findings inapplicable to other primary care clinics serving a multi-ethnic population in Malaysia. With regard to the factors that may influence the usability of an mHealth app, several factors e.g., health literacy, doctor-patient relationship, illness severity and mental health status were not included, as these were beyond the scope of our study. Therefore, the interpretation of the results in the multiple linear regression is limited only to the variables included in the analysis.
Implications to clinical practice and future research
The high usability of the EMPOWER-SUSTAIN Self-Management Mobile App© among patients with CV risk factors in our primary care clinic is established in this study, supporting its widespread utilisation as an empowerment tool to aid productive interaction between doctors, nurses and patients. This shared decision-making process will empower patients to improve their health outcomes, which would eventually prevent CVD complications. Primary care physicians should also address social support from patients’ family members and friends to improve usability of this app for self-management at home. It is encouraging to discover that patients were using this app at home, particularly to understand their medications. Usability of the app in relation to other areas of self-management i.e., home BP and blood sugar monitoring, as well as diet and exercise, still needs to be improved. Primary care physicians should encourage patients to use the ‘My Self-Management’ section at home. Their home BP readings and home blood sugar readings should be checked by primary care physicians during consultation in order to encourage self-management at home. Our study population i.e., patients who attended the EMPOWER-SUSTAIN Clinic were more educated, where 65.5% had tertiary education compared to the general population in Malaysia where 42.6% enrolled in tertiary education institutions in 2020. 37 This suggests that the EMPOWER-SUSTAIN Clinic tends to attract patients with higher education level, although education level was not found to be significant in the regressions analysis. Efforts should be made to attract patients with lower education level to attend this clinic and use the app.
With regards to future research, further studies should include patients from various ethnic groups from several primary care clinics in Malaysia, in order to improve the generalisability of the findings. Future studies should also include other important factors that may influence usability of mHealth apps. These include health literacy, doctor-patient relationships, illness severity and mental health status. Ultimately, a randomised controlled trial to evaluate the effectiveness of this mHealth app in improving self-management behaviours and clinical outcomes should be conducted. 13 Although current evidence indicated that mHealth interventions for patients with multiple CV risks were beneficial for improving some anthropometric indicators, the evidence that these interventions improved biochemical outcomes or long-term health outcomes is still inconclusive. 38
Conclusions
In conclusion, this study found that the usability of the EMPOWER-SUSTAIN Self-Management Mobile App© was high among patients with CV risk factors in our primary care clinic. Belonging to the Malay ethnicity, using the app at home to understand their medications and having social support from family members and friends in using the app were identified as significant factors of high usability. Despite its limitations, this study adds to the body of evidence as published literature on the usability of a self-management mHealth app in primary care is sparse. The findings of this study also support the widespread use of this app as an empowerment tool to aid the process of shared decision-making through productive interaction between primary care physicians and patients. Further research to evaluate the effectiveness of this mHealth app in improving self-management behaviours and clinical outcomes among patients with CV risk factors should be conducted.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-3-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-4-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-5-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Acknowledgments
The authors would like to thank the research assistants, graphic designers and also computer programmers who have contributed towards the EMPOWER-SUSTAIN project. We confirmed that we have obtained the necessary permission to use the questionnaires in this study from the respective copyright holders, provided as Appendix 4. The data collection form including the M-MAUQ is provided as Appendix 5.
Footnotes
Authors’ contributions: ASR conceptualised and designed the study, acquired the funding and coordinated the study. MHD and FHY designed and developed the mobile app. SMAH collected the data and conducted the statistical analysis, supervised by HNM, NAS and ASR. SMAH and ASR drafted the manuscript and revised it critically for important intellectual content. MSMY, NHB, SFBS, NMNMN, KNK, LLK, SAR, HAH, MHD and FHY provided critical revision of the manuscript. All authors have read and given approval of the final version of this manuscript.
Authors' note: Fakhrul H Yusoff is also affiliated with Faculty of Computing and Information Technology, Sohar University, Oman.
Data availability: The datasets generated and analysed during the current study are available from the corresponding author on reasonable request and are subject to data protection laws and regulations.
Declaration of conflicting interest: The authors declare that there is no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study protocol was approved by the Research Ethics Committee (REC) of Universiti Teknologi MARA [600-TNCPI(5/1/6)/REC/10/2021]. This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice requirements (Ministry of Health, 2011).
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the MYRA Road to HICoE Research Grant, code: 600-RMC/GPM CoE 5/3 (051/2021).
Guarantor: Anis Safura Ramli (ASR)
Informed consent: Written informed consent was obtained from all participants involved in the study.
ORCID iDs: Hayatul N Miptah https://orcid.org/0000-0001-9756-2621
Nur A Shibraumalisi https://orcid.org/0000-0002-5331-1326
Mohamed-Syarif Mohamed-Yassin https://orcid.org/0000-0003-3654-2146
Nik M Nik Mohd Nasir https://orcid.org/0000-0002-3381-1390
Khairatul N Kamaruddin https://orcid.org/0000-0002-3946-8423
Lina L Kanoo https://orcid.org/0000-0001-6999-9586
Maryam H Daud https://orcid.org/0000-0002-7928-8056
Anis S Ramli https://orcid.org/0000-0002-9517-1413
Supplemental material: Supplementary material for this article is available online.
References
- 1.Kyu HH, Abate D, Abate KH, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2018; 392: 1859–922. 10.1016/S0140-6736(18)32335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Health and Morbidity Survey (NHMS) 2019. Volume I: NCD – Non-Communicable Diseases: Risk Factors and other Health Problems. Institute for Public Health, Ministry of Health, Malaysia.
- 3.Department of Statistics Malaysia. Press Release Statistics on Causes of Death, Malaysia, 2020. Department of Statistics Malaysia.
- 4.Ramli AS, Taher SW. Managing chronic diseases in the Malaysian primary health care – a need for change. Malays Fam Physician 2008; 3: 7–13. [PMC free article] [PubMed] [Google Scholar]
- 5.Teh XR, Lim MT, Tong SF, et al. Quality of hypertension management in public primary care clinics in Malaysia: an update. PLoS One 2020; 15: e0237083. 10.1371/journal.pone.0237083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malaysia Diabetes Care Performance Report 2016. Malaysian Healthcare Performance Unit, Ministry of Health Malaysia; Kuala Lumpur, 2017.
- 7.Chia YC, Lim HM, Ching SM. Does use of pooled cohort risk score overestimate the use of statin?: a retrospective cohort study in a primary care setting. BMC Family Pract 2014; 15: 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaki M, Robaayah Z, Chan SP, et al. Malaysia Shape of the Nation (MySoN): a primary care based study of abdominal obesity in Malaysia. Med J Malaysia 2010; 65: 143–9. [PubMed] [Google Scholar]
- 9.Bodenheimer T, Lorig K, Holman Het al. et al. Patient self-management of chronic disease in primary care. JAMA 2002; 288: 2469–75. doi: 10.1001/jama.288.19.2469 [DOI] [PubMed] [Google Scholar]
- 10.Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract 1998; 1: 2–4. [PubMed] [Google Scholar]
- 11.Reynolds R, Dennis S, Hasan I, et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 2018; 19: 11. doi: 10.1186/s12875-017-0692-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramli AS, Selvarajah S, Daud MH, et al. Effectiveness of the EMPOWER-PAR intervention in improving clinical outcomes of type 2 diabetes mellitus in primary care: A pragmatic cluster randomised controlled trial. BMC Fam Pract 2016; 17: 157. doi: 10.1186/s12875-016-0557-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daud MH, Ramli AS, Abdul-Razak S, et al. The EMPOWER-SUSTAIN e-Health Intervention to improve patient activation and self-management behaviours among individuals with Metabolic Syndrome in primary care: Study protocol for a pilot randomised controlled trial. Trials 2020; 21: 311. 10.1186/s13063-020-04237-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daud MH, Yusoff FH, Abdul-Razak S, et al. Design, development, utility and usability testing of the EMPOWER-SUSTAIN self-management mobile app© among primary care physicians and patients with metabolic syndrome. Digit Health 2023; 9: 20552076231176645. 10.1177/20552076231176645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ISO 9241-11:1998. Ergonomic Requirements for Office Work with Visual Display Terminals, Geneva.
- 16.Nielsen J. Usability 101: “Introduction to Usability”. Nielsen Norman Group, 2012. https://www.nngroup.com/articles/usability-101-introduction-to-usability/ [accessed Jan 2022].
- 17.Report of Household Income and Basic Amenities Survey 2019. Department of Statistics, Malaysia, 2019.
- 18.Ministry of Health Malaysia. Clinical Practice Guidelines on the Management of Obesity. Ministry of Health Malaysia; Putrajaya, 2023.
- 19.World Health Survey 2002. Self-rated health is defined as how patients perceive their own health condition. Geneva: World Health Organization, 2002. [Google Scholar]
- 20.Ministry of Health Malaysia. Clinical Practice Guidelines on the Management of Primary and Secondary Prevention of Cardiovascular Diseases. Putrajaya: Ministry of Health Malaysia, 2017. [Google Scholar]
- 21.Ministry of Health Malaysia. Clinical Practice Guidelines on the Management of Type 2 Diabetes Mellitus. 6th Edition. Putrajaya: Ministry of Health Malaysia, 2020. [Google Scholar]
- 22.Zhou L, Bao J, Setiawan I, et al. The mHealth app usability questionnaire (MAUQ): development and validation study. JMIR Mhealth Uhealth 2019; 7: e11500. doi: 10.2196/11500. https://mhealth.jmir.org/2019/4/e11500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustafa N, Safii NS, Jaffar A, et al. Malay version of the mHealth app usability questionnaire (M-MAUQ): translation, adaptation, and validation study. JMIR Mhealth Uhealth 2021; 9: e24457. 10.2196/24457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alessa T, Hawley MS, Alsulamy Net al. et al. Using a commercially available app for the self-management of hypertension: acceptance and usability study in Saudi Arabia. JMIR Mhealth Uhealth 2021; 9: e24177. 10.2196/24177. https://mhealth.jmir.org/2021/2/e24177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.IBM SPSS Statistics for Windows. Version 28.0. IBM Corp.; 2021.
- 26.Hajesmaeel-Gohari S, Khordastan F, Fatehi F, et al. The most used questionnaires for evaluating satisfaction, usability, acceptance, and quality outcomes of mobile health. BMC Med Inform Decis Mak 2022; 22: 22. 10.1186/s12911-022-01764-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arensman R, Kloek C, Pisters M, et al. Patient perspectives on using a smartphone app to support home-based exercise during physical therapy treatment: Qualitative study. JMIR Hum Factors 2022; 9: e35316. 10.2196/35316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Janatkhah R, Tabari-Khomeiran R, Asadi-Louyeh Aet al. et al. Usability of a disease management mobile application as perceived by patients with diabetes. Comput Inform Nurs 2019; 37: 413–419. 10.1097/CIN.0000000000000532 [DOI] [PubMed] [Google Scholar]
- 29.Kc B, Alrasheedy AA, Hing Goh B, et al. The types and pattern of use of mobile health applications among the general population: A cross-sectional study from Selangor, Malaysia. Patient Prefer Adherence 2021; 15: 1755–1762. 10.2147/PPA.S325851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reiners F, Sturm J, Bouw LJWet al. et al. Sociodemographic factors influencing the use of ehealth in people with chronic diseases. Int J Environ Res Public Health 2019; 16: 645. 10.3390/ijerph16040645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Volpi SS, Biduski D, Bellei EA, et al. Using a mobile health app to improve patients’ adherence to hypertension treatment: a non-randomized clinical trial. PeerJ 2021; 9: e11491. 10.7717/peerj.11491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Armitage LC, Kassavou A, Sutton S. Do mobile device apps designed to support medication adherence demonstrate efficacy? A systematic review of randomised controlled trials, with meta-analysis. BMJ Open 2020; 10: e032045. 10.1136/bmjopen-2019-032045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aikens JE, Trivedi R, Aron DCet al. et al. Integrating support persons into diabetes telemonitoring to improve self-management and medication adherence. J Gen Intern Med 2015; 30: 319–26. 10.1007/s11606-014-3101-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayberry LS, Berg CA, Harper KJet al. et al. The design, usability, and feasibility of a family-focused diabetes self-care support mhealth intervention for diverse, low-income adults with type 2 diabetes. J Diabetes Res 2016: 7586385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brew-Sam N, Chib A, Rossmann C. Differential influences of social support on app use for diabetes self-management - a mixed methods approach. BMC Med Inform Decis Mak 2020; 20: 151. 10.1186/s12911-020-01173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abu Seman RA, Haryati A, Shameem RG, et al. Mhealth in cardiovascular diseases (CVD) self-care: a systematic review of advantages and challenges. Malays J Med Health Sci 2021; 17: 129–157. [Google Scholar]
- 37.Policy Planning and Research Division, Ministry of Higher Education, Malaysia. Higher Education Report: MALAYSIA. UNESCO National Commission in Alliance with Higher Education Institutions; 2022. https://whec2022.net/resources/Country%20report%20-%20Malaysia.pdf.
- 38.Chen D, Ye Z, Shao J, et al. Effect of electronic health interventions on metabolic syndrome: a systematic review and meta-analysis. BMJ Open 2020; 10: e036927. 10.1136/bmjopen-2020-036927 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-3-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-4-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH
Supplemental material, sj-docx-5-dhj-10.1177_20552076241242795 for Factors associated with usability of the EMPOWER-SUSTAIN Self-management mobile app© among individuals with cardiovascular risk factors in primary care by Siti M Abu Hussain, Hayatul N Miptah, Nur A Shibraumalisi, Mohamed-Syarif Mohamed-Yassin, Noorhida Baharudin and Siti F Badlishah-Sham, Nik M Nik Mohd Nasir, Khairatul N Kamaruddin, Lina L Kanoo, Suraya Abdul-Razak, Hasidah Abdul-Hamid, Maryam H Daud, Fakhrul H Yusoff, Anis S Ramli in DIGITAL HEALTH