ABSTRACT
Passive heat therapy is characterized by exposure to a high environmental temperature for a brief period. There are several types of passive heat therapy which include hot tubs, Waon therapy, hydrotherapy, sanarium, steam baths, infrared saunas and Finnish saunas. The most commonly used and widely studied till date are the Finnish saunas, which are characterized by high temperatures (ranging from 80–100°C) and dry air with relative humidity varying from 10–20%. The goal of this review is to provide a summary of the current evidence on the impact of passive heat therapies particularly Finnish saunas on various health outcomes, while acknowledging the potential of these therapies to contribute to the extension of healthspan, based on their demonstrated health benefits and disease prevention capabilities. The Finnish saunas have the most consistent and robust evidence regarding health benefits and they have been shown to decrease the risk of health outcomes such as hypertension, cardiovascular disease, thromboembolism, dementia, and respiratory conditions; may improve the severity of musculoskeletal disorders, COVID-19, headache and flu, while also improving mental well-being, sleep, and longevity. Finnish saunas may also augment the beneficial effects of other protective lifestyle factors such as physical activity. The beneficial effects of passive heat therapies may be linked to their anti-inflammatory, cytoprotective and anti-oxidant properties and synergistic effects on neuroendocrine, circulatory, cardiovascular and immune function. Passive heat therapies, notably Finnish saunas, are emerging as potentially powerful and holistic strategies to promoting health and extending the healthspan in all populations.
KEYWORDS: Passive heat therapy, hot tub, Waon therapy, hydroptherapy, steam bath, Finnish sauna, cardiovascular disease, mortality, lifespan
Introduction
Passive heat therapy, also known as thermotherapy, is characterized by exposure to a high environmental temperature for a brief period. There are several types of passive heat therapy which include hot tubs, Waon therapy, hydrotherapy, sanarium, steam baths, infrared saunas and Finnish saunas. These passive heat therapies vary by relative humidity and temperature (Table 1). The most commonly used and widely studied till date are the Finnish saunas, which are characterized by high temperatures (ranging from 80–100°C) and dry air with relative humidity varying from 10–20%. The majority of these passive heat therapies have been initially used for the purposes of leisure and relaxation, without research-based knowledge on their potential health effects. In recent times, there is an emerging body of robust research evidence showing that a number of these passive heat therapies are linked with substantial health benefits and may help to increase the lifespan and extend healthspan [1–4].
Table 1.
Types of passive heat therapies by temperature and humidity levels.
| Type | Temperature,°C | Humidity, % |
|---|---|---|
| Hot tub | 37–40 | Varies |
| Russian sauna/sanarium | 50–60 | 40–70 |
| Waon therapy | 40–60 | 50–70 |
| Balneotherapy | 34–38 | Varies |
| Hamman/steam room | 40–50 | 100 |
| Infrared sauna | 30–40 | 0 |
| Sauna (wet) | 40–60 | 100 |
| Finnish sauna | 70–110 | 10–20 |
The exact temperatures and humidity levels can vary depending on personal preferences, location, and specific equipment.
Healthspan refers to the phase of an individual’s life characterized by optimal health and functionality, where they experience minimal physical or mental limitations. It denotes the duration of time when a person enjoys a high quality of life, maintaining independence, engaging in daily activities, and pursuing personal aspirations, without the burden of chronic ailments or disabilities [5]. Distinguishing it from lifespan, which measures the overall length of an individual’s existence, healthspan emphasizes the quality of those years by prioritizing well-being and vigor. It encompasses multiple dimensions of health, including physical fitness, mental wellness, and emotional equilibrium, encompassing the absence of diseases, sustained cognitive abilities, sound mental health, and active social engagement.
The objective of extending healthspan is to prolong the period of vitality and productivity while minimizing the years spent in ill health or disability. Strategies to enhance healthspan commonly involve adopting a wholesome lifestyle, encompassing regular physical exercise, a balanced diet, sufficient sleep, stress management, recovery and relaxation, and avoiding detrimental habits like smoking or excessive alcohol consumption.
Based on compelling data from observational, interventional and mechanistic studies, passive heat therapies are emerging as potential strategies that could be used to extend the healthspan and improve the quality of life. For instance, having hot tub baths almost daily or every day have been shown to reduce the risk of adverse cardiovascular outcomes by about 23–46% [6]. Repeated sessions of Waon therapy have been shown to reduce blood pressure (BP) in patients with hypertension [7,8] and relieve symptoms of peripheral arterial disease (PAD), chronic obstructive pulmonary disease (COPD), fibromyalgia, chronic pain, mild depression, and chronic fatigue syndrome [9,10]. In heart failure (HF) patients, Waon therapy improves clinical symptoms and the quality of life [8–11]. Hydrotherapy (e.g. steam baths) produces significant reductions in BP and has been shown to improve pain and used for the management of HF, myocardial infarction, COPD, asthma, Parkinson’s disease, ankylosing spondylitis, osteoarthritis, rheumatoid arthritis, fibromyalgia, anorectal disorders, fatigue, anxiety, obesity, hypercholesterolemia, hyperthermia, and labor [12,13]. Regular or frequent Finnish sauna baths have been reported to (i) reduce the risk of diseases such as hypertension [14], cardiovascular disease (CVD) mortality [15], sudden cardiac death (SCD) [15], stroke [16], dementia [17], venous thromboembolism (VTE) [18], all-cause mortality [15], lung diseases [19–21], and psychotic disorders [22]; and (ii) improve the severity of musculoskeletal disorders such as osteoarthritis, rheumatoid arthritis, and fibromyalgia [23,24], COVID-19 [25], and lung disease conditions such as asthma, chronic bronchitis, and COPD [26,27]. The beneficial effects of passive heat therapies may be linked to their anti-inflammatory, cytoprotective and anti-oxidant properties and synergistic effects on neuroendocrine, circulatory, cardiovascular and immune function [1].
Given the extensive literature on the health benefits of passive heat therapies especially Finnish saunas, it is necessary to provide a comprehensive summary which will enable patients, practitioners, researchers and policy makers to make appropriate interpretations, which can optimally impact on public health and clinical practice. Hence, the goal of this review is to provide a summary of the substantial evidence on the impact of passive heat therapies on various health outcomes. We aim to accurately represent the scope and findings of the reviewed evidence while acknowledging the potential of these therapies to contribute to the extension of healthspan, based on their demonstrated health benefits and disease prevention capabilities. Furthermore, the current review will provide insights into the underlying biological mechanisms through which passive heat therapies exert their beneficial health effects and potentially extend the healthspan; health, clinical and policy implications of the findings; gaps in the existing evidence base and future directions. This review will mostly focus on evidence from the traditional Finnish saunas since they are the most widely studied to date. While the emphasis remains on Finnish sauna, other modalities are given due consideration, especially in sections where they have been rigorously studied.
Types of passive heat therapy
Finnish sauna
Sauna bathing is a form of passive heat therapy which is characterized by exposure to a high environmental temperature for a brief period. Sauna bathing is a tradition embedded in the Finnish culture and has been used for thousands of years for leisure, relaxation, and wellness; it is accessible to most people in Finland [28,29]. It is also commonly used in other Nordic countries. The sauna is usually made up of logs or wood with wooden benches well above the floor for bathers to sit on. The recommended temperature for a dry sauna bath is from 80°C to 100°C at the level of the bather’s head, but it is significantly lower at the floor-level which ensures efficient ventilation and makes sure the conditions are comfortable for sauna bathers [30]. The relative humidity of sauna usually varies from 10 to 20%. Temperature and humidity can be temporarily increased by throwing water on the hot rocks of the sauna heater. Typical sauna sessions consist of short stays in the sauna room which are interspersed with cooling-off periods (swim, shower, jumping in ice cold water, rolling on the snow, or a period at room temperature and sauna bather’s rehydration) [31]. The duration of stay in the sauna room depends on the comfort and temperature of the sauna bather, but it usually ranges from 5–20 minutes, although longer sauna bathing sessions may be used depending on the individual [32]. Sauna bathing habits may have changed over time, but still a typical Finnish person has a sauna bath at least once per week, with the average habitual frequency being 2–3 times per week [15,33,34].
Hot tub
Hot tub bathing which involves sitting in a hot tub with water up to the shoulders at temperatures ranging from 37.8–41.0°C, is ingrained in the culture of Japan.
Waon therapy
Waon therapy (which means “soothing warm therapy”) is a form of thermal treatment in a far-infrared dry sauna maintained at a uniform temperature of 60°C; it is the predominant passive therapy that is used for the treatment of HF in Japan. Patients usually remain in the sauna for 15 min, and after the sauna, patients are then placed in a supine position on a bed outside the sauna room where they are covered with blankets for 30 min [9,10].
Hydrotherapy
Hydrotherapy (also known as water therapy, aquatic therapy, pool therapy, and balneotherapy) which was widely used in ancient cultures including Egypt, China and India, involves the use of water in any form (liquid, ice, steam) at varying temperatures and pressure, to promote health and/or treat diseases [12,35].
Steam baths
They are a form of hydrotherapy, which operate at temperatures around 43°C with a humidity level of 100%.
Balneotherapy
Also known as spa therapy or hydrotherapy, balneotherapy is a traditional therapeutic practice that involves treating health conditions by bathing or immersion in thermal springs and mineral waters at 40°C for 10 minutes [36]. This form of therapy has been used for centuries, particularly for its benefits in improving mobility in arthritic and neuromuscular disorders, as well as in managing low-grade inflammation and stress-related pathologies.
Sanarium
A sanarium or Russian sauna (also known as banya) is a type of sauna that combines features of both traditional saunas and steam rooms. It typically offers a milder and more humid heat compared to traditional dry saunas.
Leg thermal therapy
The patient’s lower limbs are heated by infrared radiation at 45°C for 20 min [37].
Methods
We conducted a thorough search for observational studies, including prospective cohort, nested case-control, case-cohort or retrospective cohort studies, randomized controlled trials (RCTs), and non-RCTs from MEDLINE and EMBASE up to November 2023. Our search focused on the cardiovascular and other health benefits of passive heat therapies, with a particular emphasis on robust systematic reviews and meta-analyses of these study designs when available, according to the hierarchy of evidence [38]. We combined search terms or keywords related to passive heat therapy (“Finnish Sauna,” “Waon therapy,” “hot tub,” “hot bath,” “hydrotherapy,” “samarium,” “steam bath,” “hammam,” “Russian steam bath” and “banya”) and cardiovascular and other health outcomes (“cardiovascular disease,” “coronary heart disease,” “sudden cardiac death,” “heart failure,” “hypertension,” “blood pressure,” “dementia,” “depression,” “anxiety,” “pulmonary disease,” “sleep,” “fracture,” “mortality,” “lipids,” “inflammation,” “oxidative stress,” “arterial stiffness,” “arterial compliance,” and “intima media thickness”). We restricted our review to studies conducted in human populations, reported in English, and in adults. We focused particularly on studies with follow-up given that they address temporality; however, results of some cross-sectional studies were discussed where relevant.
Health benefits of passive heat therapies
Cardiovascular outcomes
Blood pressure and hypertension
Finnish sauna - Several studies, both experimental and epidemiological, suggest that sauna bathing can positively influence BP regulation. However, it’s noteworthy that most of these investigations targeted individuals with preexisting vascular conditions and predominantly assessed the immediate impact of sauna on BP [39,40]. In studies by Laukkanen et al and Lee et al involving 100 participants (56% male, ages ranging from 32–75) with at least one cardiovascular risk marker, there was a notable decline in both systolic and diastolic blood pressure (SBP and DBP) post a 30-minute sauna session [34,41]. The average SBP dropped from 137 (16) to 130 (14) mmHg and DBP from 82 (10) to 75 (9) mmHg post-sauna, with both showing statistically significant decreases (p < 0.0001) [34,41]. Even after 30 minutes of recovery, the SBP was still lower than its initial level. Gayda et al [42] explored the benefits of just sauna bathing versus combining exercise with sauna on daily BP monitoring and primary hemodynamic metrics in 16 individuals with mildly elevated BP. Of these, 8 were prehypertensive individuals (SBP between 120 and 139 mmHg) and 8 had stage I hypertension (SBP between 140 and 159 mmHg) [42]. The results from a single sauna session showed promising reductions in overall BP as gauged by 24-hour recordings. Drawing from the results of this study, the researchers suggested that both exercise and sauna sessions can be effective non-drug approaches for mitigating elevated SBP and average BP in patients not yet on hypertension medications [42].
The long-term effects of regular sauna bathing on BP and the potential risk of hypertension in the broader population remain less explored. Zaccardi et al. carried out a unique long-term prospective evaluation of the Kuopio Ischemic Heart Disease (KIHD) cohort study involving 1,621 males aged 42–60 years recruited from the general population. The study discovered that Caucasian men who engaged in regular sauna sessions (4–7 times weekly) experienced a remarkable 47% relative decrease in the likelihood of developing hypertension over an extensive follow-up period of 24.7 years [14]. At the study’s outset, participants exhibited BP values within the normal range and were not on any antihypertensive treatments [14]. After accounting for known risk factors and other potential confounders, such as alcohol intake, socioeconomic factors, and cardiorespiratory fitness (CRF) levels, the findings remained consistent.
Other passive heat therapies – Several studies based on experimental designs have reported BP lowering effects of other passive heat therapies [43,44]. Brunt and colleagues investigated the effects of 8 weeks of repeated hot water immersion on various cardiovascular biomarkers in young, sedentary humans; their results demonstrated that relative to a sham group, heat therapy reduced mean arterial pressure (MAP) and DBP [43]. An experimental study compared symptoms, heart rate, and SBP and DBP responses to 10 minutes of hot-tub immersion in a group of patients with treated hypertension and in a control group of normotensive subjects [44]. Systolic blood pressure fell in both groups, from a mean of 144 to 122 mmHg in the hypertensive group and from 130 to 110 mmHg in the control group [44]. In a RCT that investigated the hemodynamic changes by a single steam bath session on cardiovascular functions among healthy volunteers, findings showed significant reduction in BP immediately after taking steam bath and this was sustained for at least 30 min, whereas a control intervention did not achieve this sustained change [13]. In a recent systematic review of 15 studies to assess the effect of heat therapy on BP and vascular function, usual heat exposure for 30–90 min, over 10–36 sessions vs control conditions reduced MAP (mean difference (MD): −5.86 mmHg), SBP (MD: −3.94 mmHg) and DBP (MD: −3.88 mmHg), respectively [45].
Adverse cardiovascular outcomes
Finnish sauna - In a longitudinal evaluation of the KIHD study spanning 20.7 years conducted by Laukkanen et al., they assessed 2,315 Finnish men and discovered noteworthy associations between the frequency and duration of sauna sessions and a decline in the risk of SCD, fatal coronary heart disease (CHD) and CVD, and overall mortality [15]. These associations were independent of several potential confounding factors, such as age, body mass index (BMI), SBP, serum low density lipoprotein cholesterol (LDL-C) levels, smoking habits, alcohol intake, prior history of myocardial infarction, presence of type 2 diabetes (T2D), CRF, resting heart rate, levels of physical activity, and socioeconomic standing. A follow-up study showed that higher frequency and duration of sauna bathing were each strongly, inversely, and independently associated with fatal CVD events in middle-aged to older males and females [46]. The relationship of duration of sauna bathing with CVD mortality was consistent with a dose-response association (Figure 1). Furthermore, adding information on frequency of sauna bathing to established cardiovascular risk factors was shown to improve the prediction of the long-term risk for CVD mortality [46]. Despite some scarce findings suggesting a link between frequent sauna use and an elevated risk of SCDs [30], which are unexpected devastating but preventable events, evaluation of the KIHD study showed that an increase in the frequency and duration of sauna sessions was consistently tied to a lower risk of SCD [15,47]. In a related vein, Kunutsor et al. presented results from a separate cohort of the KIHD study of 1,628 participants, including both males and females, tracked for over 15 years. Their findings indicated that regular sauna use (4–7 times a week) in comparison to a singular weekly session led to a 62% decline in the risk of stroke [48]. This association held true for both ischemic and hemorrhagic stroke types. In 2242 men without a history of VTE in the KIHD prospective cohort, having 2–3 sauna sessions per week was associated with a 33% reduced risk of VTE compared with participants who had ≤ 1 sauna session per week. This association was independent of several established risk factors including lifestyle factors [18].
Figure 1.
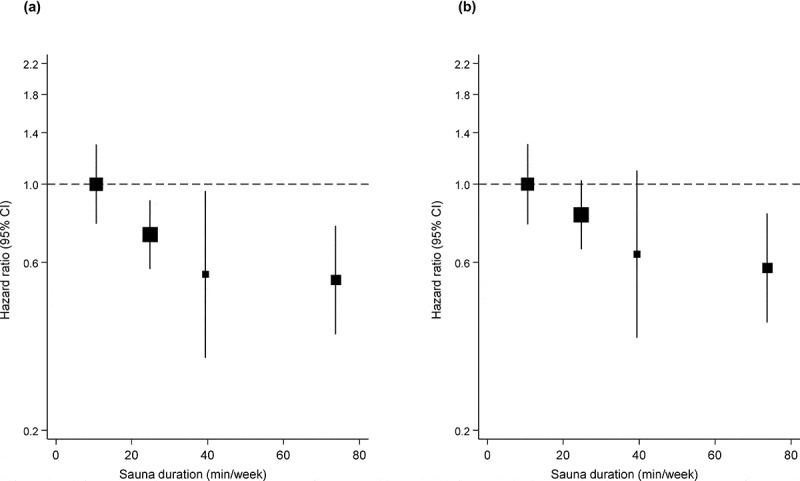
Dose-response relationship between duration of sauna bathing and cardiovascular mortality. a, adjusted for age and gender; b, adjusted for age, gender, body mass index, smoking, systolic blood pressure, serum low-density lipoprotein cholesterol, alcohol consumption, previous myocardial infarction and type 2 diabetes; CI, confidence interval. Reproduced from Laukkanen T, et al. [17].
Other passive heat therapies - In a recent prospective study based on 30,076 participants aged 40–59 years with no baseline history of CVD or cancer followed up from 1990 to 2009, having hot tub baths almost daily or every day versus zero to two times/week were associated with risk reductions in cardiovascular outcomes ranging from 23–46% [6].
There is a growing body of evidence on the use of passive heat therapies to treat and improve the prognosis of patients with HF. To synthesize the existing evidence, a recent systematic review evaluated the clinical outcomes of heat therapies in patients with HF. In their qualitative and quantitative analysis of 64 eligible studies, heat therapy was observed to improve several parameters of HF which included the New York Heart Association (NYHA) class (which reflects the severity of HF), BP, cardiac geometry, left ventricular diastolic volume and atrial diameter [49]. Another review specifically evaluated the effect of Waon therapy on left ventricular ejection fraction (LVEF), BP, natriuretic peptides (NPs), and noradrenaline in patients with HF [8]. Their synthesis of 10 studies demonstrated favorable effects of Waon therapy on NP andBP (mean reduction of 6.0 mmHg for SBP and 4.7 mmHg for DBP) in patients with HF [8]. Waon therapy has been shown to improve the following in patients with PAD: pain score, ankle brachial pressure index and blood flow, and the formation of new collateral vessels [50,51]. Studies of patients with HF who were treated with regular infrared-ray sauna therapy have reported reductions in concentrations of brain NPs (BNPs) [52,53].
Mortality
Finnish sauna - Based on the KIHD prospective study, increased frequency and duration of sauna bathing have been shown to be inversely and independently associated with a reduced risk of all-cause mortality and some cause-specific mortality events [15,46,54].
Type 2 diabetes
Finnish sauna – Though there are no specific studies that have assessed the relationship between Finnish saunas and the risk of T2D, research indicates some links between sauna use and diabetes. A study published in 1980 investigated the effect of the Finnish sauna on insulin absorption from a subcutaneous injection site [55]. This study involved eight insulin-dependent diabetic patients and focused on the disappearance rate of 125I-labeled rapid-acting insulin. The results of the study showed that exposure to the sauna (twice for 25 minutes at 85°C) led to an acceleration in insulin absorption by 110% in comparison to room temperature [55]. Following the sauna session, blood glucose concentrations dropped by 3.0–3.3 mmol/1 (54.1–59.5 mg/100 ml) in comparison to the control day without sauna. It’s inferred that the hypoglycemic effect of the sauna on insulin-treated diabetics is largely due to enhanced insulin absorption from the injection site.
Other passive heat therapies – An experimental study involving eight patients with T2D who sat in a hot tub with water up to their shoulders (temperature range of 37.8–41.0°C) for 30 minutes a day, six days a week, for three weeks, their mean fasting plasma glucose level decreased from 182 mg/dl (10.1 mmol/l) to 159 mg/dl (8.8 mmol/l) (p = 0.02), and their mean HbA1c levels decreased from 11.3% to 10.3% (p = 0.004) [56]. In a study that investigated the effects of heat therapy on metabolic function in obese women with polycystic ovary syndrome, 30 one-hour hot tub sessions spread across 8–10 weeks compared with no heat therapy led to decrease in fasting glucose from 105 to 89 mg/dl, reduction in glucose area under the curve (AUC) and decline in insulin AUC [57]. In a recent qualitative and quantitative synthesis of five studies to assess the efficacy of passive heat therapy on glycemic and cardiovascular parameters, and body weight among patients with T2D, no significant differences were observed in levels of HbA1c, fast glucose and triglycerides pre- and post-intervention [58].
Kidney disease and renal function
Finnish sauna - In 2,071 middle-aged and older men aged 42–61 years with normal kidney function who were recruited into the KIHD prospective study, cross-sectional and longitudinal analysis showed that frequent sauna bathing (4–7 sauna sessions per week) was not associated with impaired renal function (as measured using estimated glomerular filtration rate and serum levels of creatinine, potassium and sodium) or the future risk of chronic kidney disease [59] (Figure 2). Although intensive sweating, induced by sauna with dry or wet heat, usually increases losses of water, urea, sodium, potassium, and chloride, a sauna bath session does not cause significant longer-term changes in serum electrolyte or creatinine levels.
Figure 2.
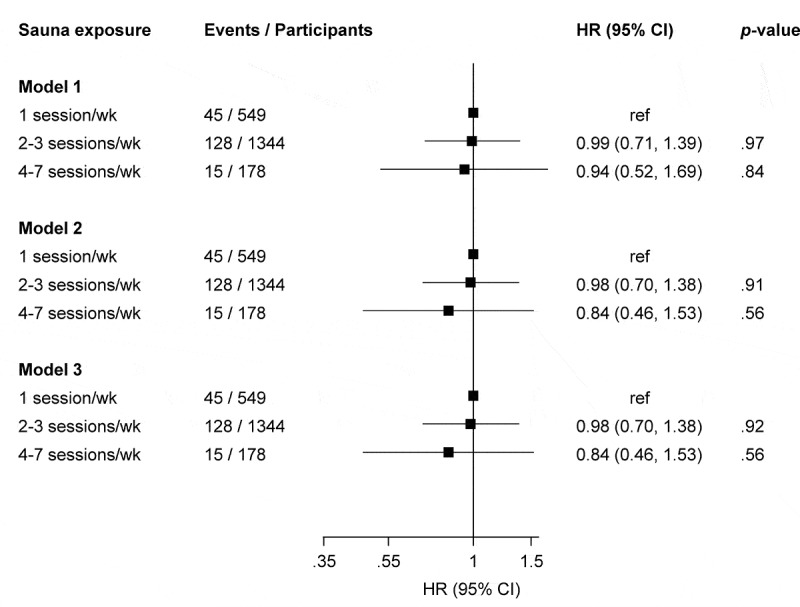
Association of frequency of sauna with risk of chronic kidney disease. CI, confidence interval; HR, hazard ratio; ref, reference. Model 1: adjusted for age. Model 2: Model 1 plus body mass index, smoking status, systolic blood pressure, total cholesterol, history of type 2 diabetes, history of hypertension, history of coronary heart disease, alcohol consumption, socioeconomic status, and physical activity. Model 3: Model 2 plus estimated glomerular filtration rate. Reproduced from Kunutsor SK, et al. [59].
Other passive heat therapies - Twelve healthy adults underwent passive heating (using a water-perfused suit model) before and after a 7-day controlled hyperthermia heat acclimation protocol and the impact of passive heat exposure on urine and serum markers of kidney function was evaluated before and after heat acclimation [60]. The results showed that passive heating did not acutely alter glomerular filtration rate, and it did not change the reduction in urine-concentrating ability that occurs acutely after passive heat stress. Also, regular passive heat acclimation reduced the incidence of microalbuminuria that occurs after acute passive heat exposure [60].
Cognitive function and neurodegenerative disease
Finnish sauna – Emerging research indicates potential protective benefits of sauna use against common neurocognitive disorders. In a study by Laukkanen et al. involving 2,315 Finnish men aged 42–60 who were generally healthy at the start, those participating in 4–7 sauna sessions weekly had their risk of developing dementia and Alzheimer’s disease decreased by 66% and 65%, respectively, when compared to those with only one session per week [17]. In 13,994 men and women aged 30–69 years at baseline and free from dementia diagnosis who were followed up for 39 years, Knekt and colleagues [61] showed that frequent sauna bathing (9–12 times/month) vs non-frequent sauna bathing (<4 times/month) was associated with a 53% reduced risk of dementia during the first 20 years of follow-up and 19% reduced risk during the entire follow-up.
Other passive heat therapies – No specific studies have evaluated the effect of other potential heat therapies on cognitive function and neurodegenerative diseases. However, given that heat therapy increases the expression heat shock proteins (HSPs), which have a protective effect against protein aggregation common to neurodegenerative diseases, there have been calls to investigate the potential benefits of passive heat therapy for neurodegenerative diseases [62].
Cancer
Finnish sauna – In 2,173 men aged 42–61 years with no history of cancer who were recruited into the KIHD prospective study and followed up for a median duration of 24.3 years, frequent Finnish sauna bathing (defined as ≥ 4 sauna sessions per week) was not associated with the risk of all-cause cancer as well as prostate and gastrointestinal cancers. There was, however, modest evidence that frequent sauna bathing may reduce the risk of lung cancer.
Other heat therapies – Therapeutic hyperthermia is a procedure that involves heating tissues to a higher temperature level, typically ranging from 41 to 45°C. The use of therapeutic hyperthermia for the treatment of cancer has been in existence for many centuries and has commonly been used as a complementary treatment to established cancer treatments such as radiotherapy and chemotherapy [63–65]. This is based on the rationale that temperatures ranging from 41 to 45°C are cytotoxic for cells in an environment with a low pO2 and low pH, which are the conditions that specifically exist within the tumor environment, due to insufficient blood perfusion [65]. Treatment with hyperthermia can be local, regional or whole-body and this depends on the extent of the area being treated [65]. In local hyperthermia, the primary goal is to increase the tumor temperature and involves heat being applied to a small area such as a brain tumor or tumors below the skin or within body cavities such as the esophagus or rectum. Regional hyperthermia is employed for large body areas such as a limb, organ or a body cavity and it involves perfusion with heated fluids [65]. Whole-body hyperthermia involves introduction of energy into the body, while energy losses are minimized at the same time; the temperature increase is usually limited to 41.8–42°C [65]. This method is commonly used to treat metastatic cancer that has spread throughout the body [63]. Several clinical trials have reported high response rates and significant reduction in tumor sizes when hyperthermia is used in conjunction with other treatments [65,66]. However, the use of hyperthermia alone has resulted in lower complete overall response rates of about 13% [65].
Respiratory function and diseases
Finnish sauna - Sauna bathing appears to offer benefits to lung function, including enhancing vital capacity, ventilation, and forced expiratory volume [26,27]. In a study by Cox et al. on 12 male participants with obstructive pulmonary disease, sauna sessions resulted in a short-term improvement in their lung function [27]. Meanwhile, Laitinen et al.‘s review highlighted research demonstrating that sauna exposure could aid in improving respiratory issues in individuals with asthma or chronic bronchitis [26]. A trial by Ernst et al. on 50 volunteers, with half being exposed to saunas, found that the incidence of common colds in the sauna group was halved during the final three months of the investigation [67]. Kunutsor et al., in the first prospective evaluation of the long-term effects of sauna use on the risk of pulmonary conditions, discovered that frequent sauna sessions (2–3 times weekly or 4–7 times weekly) lowered the risk of respiratory diseases like COPD, asthma, or pneumonia [19]. Additionally, specific research has shown that frequent sauna use is linked to a decreased risk of future incidence of pneumonia [20,21,68,69] and COPD [70,71].
Other passive heat therapies – There is some evidence linking other heat therapies for the prevention and treatment of lung conditions including respiratory infections. In a RCT that aimed to determine whether inhaling fully humidified air at 43°C (nasal hyperthermia) gave more benefit to cold sufferers than inhaling air at 30°C, nasal hyperthermia was shown to improve the course of a common cold and also give immediate relief of symptoms [72]. In a review involving six trials from five publications with a total of 387 participants to assess the effects of inhaling heated water vapor (steam) in the treatment of the common cold, the evidence was mixed and did not show any benefits or harms [73]. Four weeks of Waon therapy has been shown to improve pulmonary hypertension during exercise, exercise tolerance, and the quality of life in patients with severe COPD [74].
Bone and musculoskeletal health
Finnish sauna - Sauna bathing has been linked with an improvement in the pain and symptoms associated with musculoskeletal disorders such as osteoarthritis, rheumatoid arthritis, and fibromyalgia [23,24].
Other passive heat therapies – In 13 female patients with fibromyalgia syndrome who received Waon therapy, they all experienced a significant reduction in pain after the first session of Waon therapy. The effects of Waon therapy became stable after 10 treatments and persisted throughout the observation period of a mean duration of 14 months [75]. Balneotherapy is a common practice and has been used for centuries for the treatment of musculoskeletal complaints and rheumatic diseases. In a comprehensive review to summarize RCT data on the effect of balneotherapy on chronic inflammatory rheumatic diseases, Cozzi and colleagues identified a number of RCTs which showed that balneotherapy improved the clinical course of conditions such as ankylosing and enteropathic spondylitis and psoriatic arthritis [76]. In obese patients with knee osteoarthritis, thermal balneotherapy was shown to improve pain relief, joint function, and walking speed until 6 months of follow-up [77].
Skin diseases
Finnish sauna - Though there is no robust evidence to suggest that sauna bathing can be used to treat or prevent skin disease; a study has suggested that sauna bathing may be of benefit to patients with psoriasis as it facilitates the removal of the hyperkeratotic scales [78]. Indeed, a previous study has suggested a protective effect of regular Finnish sauna on skin physiology as evidenced by stability of the epidermal barrier function, increase in hydration of the stratum corneum, and faster recovery of elevated water loss and skin pH [79].
Other passive heat therapies - While there aren’t any specific studies on the use of passive heat therapy to prevent or treat skin diseases, there is data that points to its benefits for the skin. In 18 young, sedentary, otherwise healthy subjects who participated in 8 weeks of heat therapy (hot water immersion to maintain rectal temperature ≥ 38.5°C for 60 min per session) or thermoneutral water immersion, passive heat therapy was shown to improve cutaneous microvascular function by improving nitric oxide (NO)-dependent dilation [80]. Further research needs to investigate if this observation has clinical significance for skin diseases.
Sleep health
Finnish sauna – To our knowledge, only one study has so far investigated the effects of Finnish sauna bathing on sleep patterns. Putkonen and Elomaa monitored the sleep patterns of five test subjects following a sauna bathing session and again after no time spent in the sauna [81]. It was observed that the sauna session increased the amount of deep sleep significantly; during the first two hours, the amount of deep sleep increased by over 70%, while during the first six hours the figure was 45%. The amount of time spent awake after the sauna reduced significantly.
Other passive heat therapies – Passive body heating such as warm bath immersion with temperature 40–41°C for 30 min has been shown to promote sleep and improve sleep quality in older people with insomnia [82,83].
Infections including COVID-19
Finnish sauna – Some individuals have tended to treat common cold symptoms using hot and dry sauna. Indeed, sauna exposure has been shown to reduce the risk of infections such as common colds and pneumonia [20,21,67,69]. Though there are no specific studies that show that passive heat therapies are effective for treating and preventing COVID-19, a review of the existing evidence suggests that heat therapy including Finnish saunas can prevent or reduce the severity of COVID-19 [25]. This is based on the rationale that (i) the COVID-19 virus (SARS-CoV-2) is very sensitive to heat and its infectivity is reduced at higher temperatures. These observations are consistent with reports which show that warmer weather and higher temperatures might reduce the transmission of COVID-19 [84–86]; (ii) frequent sauna sessions have been shown to boost the immune system and reduce the risk of infection [1,20,21,67,69]; and (iii) sauna exposure reduces systemic inflammation [87,88] which may have a role in predicting severe COVID-19 [89]. It has been suggested that sauna bathing might be linked to lower urinary tract symptoms (LUTS). The proposed mechanisms underlying the potential beneficial effects of sauna bathing on LUTS include relaxation of certain type of muscles and increased blood flow in the pelvic region, a general relaxing effect, reduced urine production and increased NO bioactivity. However, studies so far have not found a significant association between sauna bathing frequency and prevalence of LUTS [90,91].
Mental health and quality of life
Finnish sauna – Exposure to Finnish sauna has been linked to a reduction in the risk of mental disorders and improved quality of life. In a RCT by Kanji et al., 37 people with chronic tension-type headache were randomized to regular sauna bathing or advice and education for a period of 8 weeks and sauna therapy was demonstrated to substantially and significantly improve headache intensity [92]. Using the KIHD prospective study, we have shown that men who had 4–7 sauna sessions per week had a 78% reduced risk of developing psychosis in the future compared to men who only had one sauna session per week [22]. Having regular sauna baths has also been reported to be associated with a better health-related quality of life. In a cross-sectional analysis of 524 octogenarians followed up in a longitudinal cohort study by Strandberg et al., physical function, vitality, social functioning, and general health were reported to be significantly better among those who were sauna users compared with non-users [93].
Other passive heat therapies – Passive heat therapies including Waon therapy and far-infrared sauna treatments have been shown to improve the mental symptoms and the quality of life in patients with chronic conditions such as chronic pain, chronic fatigue syndrome, depression, T2D and congestive HF [94,95]. In a study that examined the effect of Waon therapy on mildly depressed patients with general fatigue, appetite loss, and somatic and mental complaints, 4 weeks of Waon therapy decreased somatic and mental complaints, and produced a relaxation effect [95]. In a RCT that randomly assigned 28 mildly depressed inpatients with general fatigue, appetite loss, and somatic and mental complaints to thermal therapy group or nonthermal therapy group, patients in the thermal therapy group were treated with 60°C far-infrared ray dry sauna for 15 minutes and were then kept at bed rest with a blanket for 30 minutes once a day, 5 days a week for a total of 20 sessions in 4 weeks. Following the treatment period, symptoms improved in the thermal therapy group compared with the nonthermal therapy group [95].
Combined effects of passive heat therapy and physical activity and/or exercise training
Finnish sauna
Intermediate cardiovascular phenotypes
Several intervention-based investigations have elucidated the synergistic impact of sauna therapy coupled with exercise regimen or kinetic activities on intermediary cardiovascular outcomes. Utilizing a pre-post intervention design, 77 subjects presenting with at least one cardiovascular risk factor underwent a 15-minute aerobic regimen on a cycle ergometer, subsequently transitioning to a 15-minute sauna session. This regime yielded beneficial modulations in parameters such as MAP, pulse pressure, and augmentation index, with these modifications being sustained during the post 30-minute recovery period [96]. Another study, adopting a cross-over design with equivalent durations, sought to evaluate the hemodynamic changes of sauna exposure when compared with the combination of aerobic exercise and sauna exposure in middle-aged individuals with at least one cardiovascular risk factor. Both interventions were observed to elicit comparable acute hemodynamic alterations, notably the decrement in BP and MAP [97]. In a cohort of 16 patients with untreated hypertension who were exposed to sauna alone vs exercise and sauna, Gayda et al. showed that exercise and sauna had positive effects on 24-hour systolic and mean blood pressure; furthermore, both interventions reduced total vascular resistance, with positive effects lasting up to 120 minutes after heat exposure [42]. In a separate study involving seven well-trained male cyclists, subsequent to their routine training, a 30-minute immersion in a sauna environment (87°C, 11% relative humidity) over a span of 10 sequential days manifested a pronounced augmentation in plasma volume post the fourth session [98]. An experiment encompassing 27 healthy prehypertensive males subjected to varied combinations of sauna and exercise modalities demonstrated that the combination of endurance training followed by sauna immersion was the most efficacious in attenuating BP levels [99]. In a contemporary RCT engaging 47 middle-aged subjects with at least one conventional cardiovascular risk factor, an 8-week regimen of systematic sauna sessions combined with guideline-based regular exercise produced substantial beneficial effects on CRF, SBP, and total cholesterol indices than the standalone exercise regimen; the mean reduction in SBP was 8 mmHg [100].
It is believed that the success of Finnish athletes in the early to mid-20th century can be partly attributed to regular sauna bathing. Finnish athletes made it a practice to bring saunas to sporting events, including the 1948 Olympics in London. These saunas were designed as comprehensive recovery facilities, equipped with hot sauna rooms, cold showers, and massage tables. They were used to ensure optimal recovery from intense competition and training. Over the decades, both active individuals and elite athletes have made it a routine to use saunas post-exercise. Saunas offer a healthy means of recovery, relaxing the body, muscles, and mind after strenuous physical activity. However, it has been observed that extremely high temperatures can lead to temporary neuromuscular fatigue. This acts as a short-term stressor for the body and circulatory system. Studies have shown that prolonged exposure to sauna temperatures exceeding 70°C for 30 minutes can be particularly taxing on the neuromuscular performance of active individuals [101]. Intense strength training followed by a sauna session is more draining on neuromuscular performance than aerobic endurance exercise followed by a sauna. Research has shown that strength exercises, when combined with a sauna session – which demands exhaustive muscle work and contraction – are more fatiguing than pairing aerobic exercise with a sauna for neuromuscular performance [99]. As a result, a relatively extended recovery period might be necessary before the next training session to achieve peak performance after combining strength training with a sauna session.
Maintaining an adequate plasma volume is crucial for an effective circulatory system, both at rest and during exercise. Sauna bathing has been known to cause fluctuations in blood plasma volume [102]. There are typically minor to moderate decreases in blood plasma volume immediately after sauna bathing. However, this is followed by a return to baseline levels or even a slight increase. Generally, plasma levels return to normal within 30–60 minutes of recovery [99], provided there is adequate fluid intake during and after the sauna session. A study among healthy individuals suggested that the regular combination of endurance exercise training followed by sauna sessions might consistently increase blood volume levels. This could potentially have positive effects on cardiovascular performance during endurance exercises [99].
Adverse cardiovascular outcomes
Observational epidemiological research has suggested a synergistic cardioprotective effect of regular sauna bathing combined with measures of physical activity, as opposed to the singular impact of each modality. Evaluation of the KIHD prospective study – which monitored 2,277 middle-aged to older Finnish men over an average span of 26.1 years – it was shown that the combination of optimal CRF levels with regular sauna sessions offered substantial protection against cardiovascular and all-cause mortality than either elevated CRF or frequent sauna exposure in isolation [33]. Another supplementary examination of the KIHD dataset established that the synergistic relationship of increased CRF with regular sauna exposure substantially reduced the subsequent likelihood of SCDs, over and above the protective effects of each individual modality [103].
Other outcomes
In a follow-up evaluation of the KIHD study, a combination of high CRF levels and frequent sauna baths was demonstrated to be associated with a substantially lowered risk of incident pneumonia compared with each modality alone [69].
Other passive heat therapies
In a study that evaluated the effectiveness of the combination of Waon therapy with exercise training vs Waon therapy alone in 28 patients with HF, the combined group of Waon therapy and exercise training produced marked attenuations in BNP concentrations and augmented exercise endurance [104]. In a study that investigated the combined effects of repeated infrared-ray sauna and exercise training vs sauna alone on subjective symptoms, cardiac function, daily activities and ambulation capacity in 54 patients with chronic HF, the combined group showed marked improvements in outcomes than the monotherapy group [53]. In a clinical investigation targeting overweight, community-residing individuals of middle to advanced age, subjects were randomized into four distinct cohorts: (A) those receiving a tripartite intervention comprising exercise, dietary modifications, and hot bathing; (B) those subjected to dual modalities of exercise and dietary modifications; (C) participants solely benefiting from the hot-bathing intervention; and (D) a control group devoid of the aforementioned interventions. Upon biweekly interventions spanning 3 months, it was observed that the cohort experiencing the combined regimen of exercise, dietary alterations, and hot bathing demonstrated substantial improvements in anthropometric indices (weight, abdominal circumference, BMI and body fat percentage), markedly surpassing the improvements noted in either the exclusive hot-bathing group or the control cohort [105].
Pathways underlying the beneficial effects of passive heat therapies
Metabolic and endocrine pathways
The therapeutic efficacy of passive heat modalities, notably Finnish saunas, cuts across several physiological systems, with a significant impact on the cardiovascular system. The benefits can be attributed to several mechanisms (Figure 3): 1) attenuation of BP [14]; (2) decrease in oxidative burden [87,106,107] and systemic inflammation [87,88]; (3) advancements in arterial pliability and enhanced compliance [43,106,108–110]; (4) augmentation of endothelial function [111–114]; (5) improvement in levels of circulating vascular risk indicators like lipids, fatty acids, glycemic metrics, NPs, cardiac troponin T, interleukins, and C-reactive protein [87,88,100,108,115,116]; (6) enhancement of the cardiorespiratory system [117] and cardiovascular function [30,32,118]; (7) induction of analgesic responses via increased beta-endorphin levels [119]; (8) enhancement of immunological defenses [25,102]; (9) favorable modulation of the autonomic nervous system [40], leading to heightened norepinephrine synthesis and parasympathetic orchestration [120–122]; (10) facilitated excretion of metals like aluminum, cobalt, and lead through perspiration [123]; (11) improvement in cutaneous microvascular function, especially by enhancing NO-dependent dilation [80]; (12) elevated induction of HSPs, integral for cellular activities such as immunoregulation and protein fidelity, thereby fortifying against chronic diseases [124]; and (13) promotion of neurogenesis via surges in brain-derived neurotrophic factor expression [125].
Figure 3.
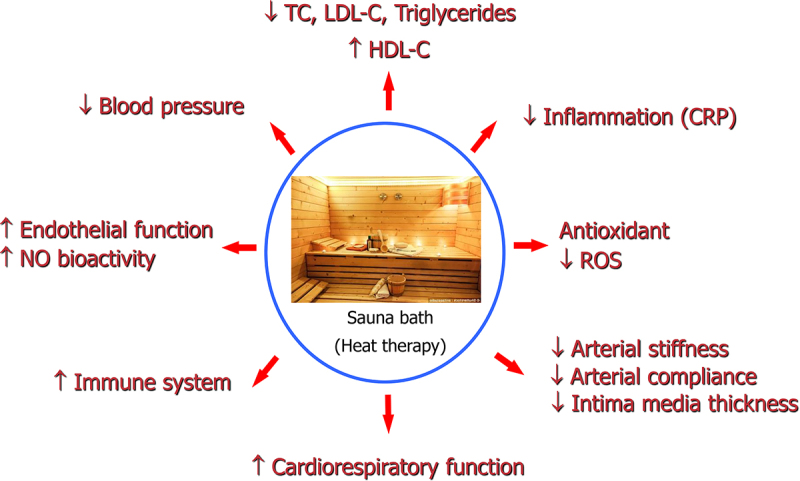
Proposed mechanistic pathways underlying Finnish sauna baths and health outcomes.
CRP, C-reactive protein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; NO, nitric oxide; ROS, reactive oxygen species; TC, Total cholesterol. Reproduced with permission from Laukkanen JA, et al. [1].
Passive heat therapy significantly impacts the hormonal system, leading to increased concentrations of hormones such as plasma renin, cortisol, and growth hormone (GH) [126].
While high-intensity exercises result in elevated serum cortisol, testosterone, and GH concentrations, no significant additional changes in these hormone concentrations are noted after adding post-exercise sauna bathing. Similarly, sauna sessions following exercise do not alter the hormonal responses in the same way as exercise training alone [127]. Sauna bathing induces various hormonal responses, which are mostly temporary and diminish by the day following heat exposure [128]. These responses tend to vary between individuals accustomed to saunas and those without prior experience. For the latter, the sauna acts as a stronger stress stimulus due to their lack of regular exposure to hot and dry sauna conditions. The cortisol response to sauna bathing can largely depend on the duration and temperature, with higher humidity and temperature typically leading to increased cortisol levels. Factors influencing different hormonal reactions include the temperature and duration of heat exposure, time of day for the sauna session, and individual characteristics like age, sex, and body composition. Neuroendocrine responses to saunas have primarily focused on stress-related hormones such as beta-endorphin and ACTH. These hormones show variable responses, ranging from a decrease, no change, to an increase. When heat exposure reaches a level of subjective discomfort, the increase in ACTH/beta-endorphin is more pronounced [129]. The rise in beta-endorphin contributes to the feeling of well-being and relaxation post-sauna.
Rissanen and colleagues [99] investigated the effects of various physical exercises (endurance, strength, combined) followed by sauna bathing on serum hormone levels (GH, testosterone, cortisol) in men. This combination of exercise and sauna is prevalent among active individuals and athletes in Finland. Interestingly, hormone level increases were observed after afternoon sauna sessions compared to morning sessions, which did not induce significant hormonal changes. There was an indication that afternoon sauna bathing following strength exercise might elevate testosterone levels the next day due to the combined effects of exercise and sauna [127]. Hyperthermia elevates the levels of several glucose-regulating hormones. In a study on men in a hot bath, glucose, GH, b-endorphin, and glucagon levels increased, while insulin levels remained unchanged [130]. Both sauna and hot baths also raise leptin levels, a hormone associated with the feeling of fullness [131]. The increased energy expenditure from sauna sessions suggests that its regular use might offer potential benefits for weight reduction as a lifestyle modification. There is compelling evidence that acute exposure to hyperthermia, such as in saunas, has a reversible negative effect on spermatogenesis in men. However, the effects of chronic hyperthermia (including sauna) are less clear-cut. In all studies, changes in sperm induced by saunas were reversible within weeks after discontinuing exposure [128].
Potential avenues that might explain sauna therapy’s beneficial effects on psychotic symptoms may hinge on its ability to improve mental function and mood. The beneficial effects of sauna on pulmonary conditions might be attributed to its direct effect on the respiratory tract, leading to optimized ventilation, increased pulmonary efficiency, and alleviated pulmonary congestion [26]. The analgesic pathways activated by sauna sessions for musculoskeletal conditions may be channeled through dermal sensory nerve terminals [32]. Intermittent thermal stresses coupled with profound cooling intervals appear to potentiate analgesic manifestations, as evidenced by increased concentrations of beta-endorphin [119]. The ensuing tranquility and euphoria following sauna exposure might be correlated to surges in endorphin levels [132]. Considering that stress is an etiological factor in the development of several diseases [133], the health promoting effects of sauna might partly be attributed to its stress relieving properties. The ability of frequent sauna bathing to augment the beneficial effects of physical activity and CRF, suggests a synergistic effect. This is backed by evidence showing that (i) the physiological responses and adaptations stimulated by a sauna bath are similar to those produced by moderate or high intensity physical activity [134,135] and (ii) the protective effects of sauna bathing on adverse outcomes are independent of physical activity and fitness levels [18,68,69].
Effects of passive heat therapy on cellular and molecular mechanisms of aging
Passive heat therapy, such as sauna bathing or other forms of controlled thermal exposure, has been gaining attention for its influence on the cellular and molecular dynamics associated with aging (Figure 4). At the cellular forefront, heat therapy fosters the release of HSPs [136,137]. These molecular chaperones are essential in preserving protein homeostasis and mitigating the accrual of misfolded proteins, a recognized hallmark of cellular aging [138]. Moreover, passive heat therapy can amplify autophagy, the cell’s intrinsic recycling mechanism which declines with age [139]. By revitalizing this process, old and potentially detrimental cellular components are degraded and repurposed, bolstering cellular vitality and function. At the molecular stratum, heat therapy has the potential to counteract oxidative stress by enhancing antioxidant defense mechanisms [140]. Given that cumulative oxidative damage is inextricably linked with the aging trajectory and the emergence of age-related conditions, this facet is of prime importance. Passive heat therapy reduces systemic inflammation [87,88], which is a hallmark of aging. Passive heat therapy also exerts beneficial effects on the mitochondria by increasing mitochondrial enzyme content and respiratory capacity of muscle cells [141]. Aging is known to be associated with a decline in mitochondrial function [142,143], which can promote various age-related conditions, including sarcopenia and CVDs [142,144]. Additionally, thermal interventions have demonstrated modulation of salient signaling pathways, notably the sirtuin pathway, renowned for their ability to delay multiple diseases of aging and implications in longevity and metabolic orchestration [145]. In summation, while this is a topic for further investigation, initial insights show that passive heat therapy might be a potential tool in influencing the cellular and molecular processes inherent to the aging paradigm.
Figure 4.
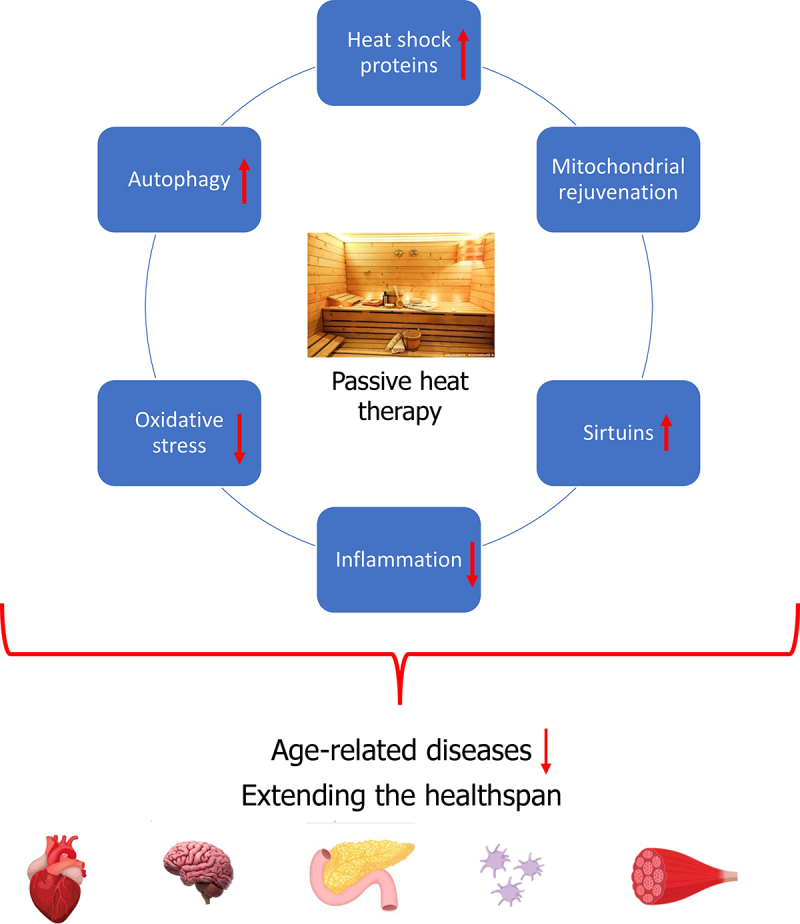
Mechanisms mediating the anti-aging health benefits of passive heat therapy.
This figure illustrates how passive heat therapies contribute to healthy aging by potentially reversing or attenuating underlying cellular and molecular mechanisms of aging as well as preventing or delaying the onset of age-related diseases in multiple organ systems
Adverse effects of passive heat therapies
Finnish sauna
Finnish sauna is a cherished recreational activity celebrated for its wellness and relaxation benefits. In general, those in good health find the hot and dry environment of a Finnish sauna, with temperatures ranging between 80–100°C and humidity levels of 10–20%, both tolerable and pleasurable [30,146]. While there were initial reservations – primarily based on anecdotal evidence – about its suitability for individuals with cardiovascular conditions due to the sauna’s demand on the cardiovascular system [32,147], current research indicates that those with stable cardiovascular conditions can safely engage in sauna bathing [30,148]. Benefits such as increased cardiac output, improved ventricular arrhythmias, and overall symptomatic improvement have been documented, especially among patients with HF [108,113,120,149]. Despite its advantages, it’s necessary to engage in sauna bathing with caution, particularly concerning alcohol consumption. There have been instances linking saunas to sudden deaths, largely influenced by alcohol, which magnifies risks of hypotension, cardiac complications, and potential accidents [148,150,151]. For those with specific symptomatic or unstable conditions like unstable coronary artery disease, sauna bathing could be detrimental [32]. It’s generally advised that individuals with conditions such as recent myocardial infarction, severe aortic stenosis, uncontrolled hypertension, or severe valvular disease exercise caution or avoid saunas entirely due to potential BP fluctuations and other risks [30,148,152]. Other conditions warranting caution include fever, skin abrasions, urticaria, and certain infections [24,78]. Sauna-related burns represent a tangible concern. A retrospective study over seven years found that a significant 26% of burn cases were linked to sauna sessions, often resulting from contact with the hot stove or steam. Notably, alcohol played a role in 40% of these incidents [153]. The tradition of interspersing short sauna sessions with quick cool-offs in cold water, while popular and seemingly beneficial to athletes [154], may be associated with adverse reactions, particularly in individuals with cardiovascular conditions [155,156]. This rapid transition from hot to cold stimulates cold receptors, leading to a cascade of physiological responses that could be dangerous for those with preexisting cardiovascular conditions [157,158].
Interestingly, a study with young Finnish participants highlighted that the combination of sauna and cold immersion, while causing significant hormonal changes, was generally well tolerated by those without HF [40]. Yet, caution is necessary, especially for those with unstable cardiovascular conditions. The profound physiological shifts between heat exposure and cold immersion can trigger rapid hemodynamic changes and a heightened risk of arrhythmias, particularly in patients with recent acute myocardial infarction or other underlying cardiac diseases [146]. Indeed, there have been fatal instances where individuals plunged headfirst into cold water post-sauna, leading to coronary artery constriction and reduced heart oxygen supply [134,159]. The associated risks, heightened by the secretion of adrenocorticotropic hormone, cortisol, and catecholamines, emphasize the need for thorough research to provide clearer guidelines on sauna bathing combined with varying cooling-down procedures, especially for patients with preexisting cardiovascular issues.
Other passive heat therapies
Exposure to heat during passive heat therapies, including Finnish saunas, can elevate body tissue temperatures, stimulating sweating and vasodilation, which in turn can lead to dehydration if fluid loss is not adequately replenished [160]. Dehydration can exacerbate the effects of heat stress, affecting thermoregulation and increasing the risk of heat-related illnesses like heat exhaustion or heat stroke [161]. Dehydration risks due to prolonged immersion can lead to dizziness or fainting. Factors such as individual heat tolerance, which can vary due to infections, electrolyte disturbances, or physical condition, play a crucial role in susceptibility to heat stress [162]. Additionally, certain demographic groups, like older adults or those with preexisting medical conditions, may be more vulnerable to the adverse effects of heat and dehydration [163].
Hot tubs - Prolonged exposure can also result in heat rashes or folliculitis, influenced by bacterial infections. Poorly maintained hot tubs may harbor Mycobacterium avium, resulting in “hot tub lung” [164]. Furthermore, soaking in a hot tub can lead to dangerous drops in BP [165].
Waon therapy - Generally considered safe but can lead to mild heat-related discomfort in those unaccustomed to thermal therapies. Overexposure might cause dehydration or heat stress.
Hydrotherapy - Risks include water-borne infections if cleanliness is not maintained and potential slipping hazards. Sudden shifts from hot to cold water can stress the cardiovascular system [12].
Sanarium - Respiratory discomfort can arise due to the increased humidity, especially in individuals with preexisting respiratory conditions.
Steam baths - High humidity can exacerbate respiratory issues especially in individuals with conditions like asthma or COPD. There’s also a risk of steam burns and overheating from prolonged sessions [166]. The heat and humidity of a steam bath can put stress on the cardiovascular system.
Infrared saunas - Overexposure or improper use can lead to burns or heat-induced conditions, and light-sensitive individuals may experience flare-ups.
As with any therapy, it’s essential to monitor individual reactions and consult healthcare professionals before initiation. Proper hydration and adherence to session guidelines can help reduce adverse effects.
Optimizing passive heat therapy: Clinical and public health implications
The potential of passive heat therapy, particularly Finnish saunas, to positively impact on health and well-being has implications for public health and clinical care. Finnish saunas, characterized by high temperatures in a low humidity environment, are emerging as prominent therapeutic tools, with the most consistent evidence backing their beneficial health effects. The overall evidence suggests that reaping the optimal benefits from sauna sessions requires a frequency of 3–7 sessions per week, with each session lasting approximately 15–20 minutes. Given the range of passive heat therapies available, choosing the most suitable modality based on an individual’s specific health requirements becomes paramount. Therapeutic protocols need to be tailored to individual health needs and contraindications. Finnish saunas can act as an adjunct to existing therapeutic strategies, especially for conditions such as hypertension, CVDs, and musculoskeletal disorders. When combined with regular physical activity, this dual approach can lead to optimized health outcomes and enhanced quality of life. Beyond the physical, the role of saunas in promoting mental well-being and improved sleep quality further enhances their potential as a holistic health tool.
From a public health perspective, the widespread benefits of passive heat therapies suggest a need for increased accessibility. Advocacy for more sauna facilities in community centers, gyms, and public health clinics could ensure that a broader section of society avails of these benefits. Raising awareness is key. Public health campaigns can highlight the several advantages of passive heat therapies and underscore the benefits of combining them with regular physical activity. To achieve maximal cardiovascular and overall health benefits, combining sauna sessions (3–7 sessions per week, with each session lasting approximately 15–20 minutes) with the physical activity guideline recommendations of at least 150–300 minutes of moderate-intensity or 75–150 minutes of vigorous-intensity physical activity per week could be a game-changer. This synergistic approach could pave the way for substantial improvements in cardiovascular health, overall well-being, and longevity. As we navigate the evolving landscape of health and wellness, refining recommendations based on new evidence, and integrating passive heat therapy into wellness and preventive health programs can yield dividends for population health. In essence, passive heat therapies, especially Finnish saunas, represent a promising nexus of tradition and science.
Future directions
The increasing interest in passive heat therapies, especially Finnish saunas, and their potential to ameliorate a plethora of health conditions and potentially extend the healthspan, sets the stage for a promising future of research and application. As we move forward, several areas merit attention:
Expanding the scope of research: While Finnish saunas have been studied extensively, other forms of passive heat therapies remain relatively underexplored. Future studies should delve deeper into the specific health benefits of hydrotherapy, Waon therapy, infrared saunas, and other modalities to identify their unique advantages and optimal conditions for use. Previous RCTs of these passive heat therapies had shortcomings with regards to design and methodological quality, such as randomization procedures and low statistical power. Hence, large, definitive, and rigorous RCTs are needed going forward. Further studies on the mechanistic pathways underlying the health benefits of passive heat therapies are also warranted.
Future studies: To truly understand the longevity benefits and potential side effects, longitudinal studies spanning decades will be essential. Such studies can elucidate the lasting impact of regular passive heat therapy on lifespan, healthspan, and potential risks. The majority of longitudinal studies of Finnish sauna have been based on the KIHD cohort (Figure 5), which increases the likelihood of type 1 error due to multiplicity [167], given the use of the KIHD study to test for associations of sauna bathing with multiple outcomes. Furthermore, given the well-established health benefits of Finnish sauna, definitive trials that randomize patients to Finnish sauna and other passive heat therapies would help address gaps in the evidence base. Head-to-head comparisons of passive heat therapies and physical activity/exercise are also urgently warranted. Finally, RCTs of passive heat therapies that measure biomarkers of healthspan across months to a few years could provide extensive insight on the impact of passive heat therapies on the healthspan.
Figure 5.
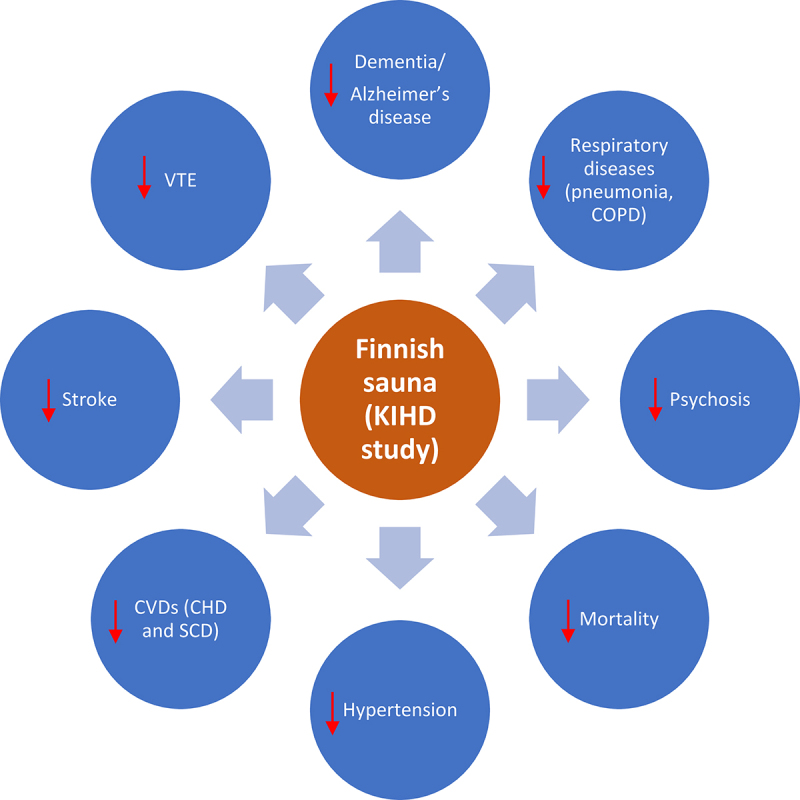
Health benefits of Finnish sauna bathing: insights from the KIHD study.
CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; KIHD, Kuopio Ischemic Heart Disease; SCD, sudden cardiac death; VTE, venous thromboembolism
Personalized approaches: - Given the variability in individual responses to passive heat therapies, research that investigates personalized protocols based on genetics, preexisting health conditions, and individual preferences could provide more tailored and effective therapeutic solutions.
Integration with other therapies - Exploring how passive heat therapies can be synergistically combined with other interventions, such as diet, cognitive training, or novel pharmaceuticals, can provide insights into holistic wellness strategies.
Technological innovations - Leveraging technology to enhance the efficacy of passive heat therapies can be a frontier of innovation. For instance, integrating sensors to monitor vital signs during sauna sessions or creating AI-driven personalized heat therapy protocols based on real-time data can optimize therapeutic outcomes.
Public awareness and accessibility - While the health community is becoming increasingly cognizant of the benefits, more extensive public awareness campaigns are essential. Collaborating with medical schools to include sauna therapy in the curriculum could be a starting point. This could involve presenting current research findings on sauna use and its health benefits, as well as exploring potential risks and contraindications. Organizing community events, wellness programs, and educational seminars can raise awareness among the general public. Collaborating with wellness influencers and leveraging social media platforms can also be effective. Partnering with health and wellness centers, spas, and gyms to offer sauna facilities and education about its benefits can help integrate sauna use into regular health and wellness routines. Such initiatives can be complemented by efforts to make passive heat therapy facilities more accessible, especially in regions where they aren’t traditionally popular.
Policy implications - As evidence increases regarding the health benefits of passive heat therapies, there is a compelling case for policymakers to consider subsidizing access to such facilities, integrating them into healthcare recommendations, and supporting further research through grants and other funding mechanisms. For instance, guidelines of the Osteoarthritis Research Society International (OARSI) recommend balneotherapy as a management strategy for patients with multi-joint osteoarthritis and comorbidities [168].
Environmental and sustainable considerations - With the rising popularity of saunas and other heat therapies, it will be crucial to consider their environmental footprint. Future directions should include designing sustainable sauna systems, ensuring energy efficiency, and promoting practices that are ecologically responsible, such as the reuse of heated sauna energy for housewarming.
Safety protocols - With increasing usage, the establishment of clear safety and operational guidelines for passive heat therapies will be paramount. This would include precautions for specific populations, such as older people, pregnant women, or those with certain medical conditions.
Conclusions
Passive heat therapies, notably Finnish saunas, are emerging as potentially powerful and holistic strategies to promoting health and longevity. The compelling evidence underscores their potential in mitigating various health conditions, augmenting the benefits of established lifestyle interventions like physical activity, and enhancing overall well-being. Considering the public health burden of CVD risk related to hypertension, the blood pressure-lowering effect of regular sauna use is a very welcome lifestyle intervention to prevent CVDs.
As the scientific community delves deeper into optimizing these therapies and integrating them into routine healthcare, individuals worldwide stand to reap the myriad benefits. Moving forward, it is essential to continue rigorous research, raise public awareness, and ensure accessibility, ensuring that passive heat therapies remain a cornerstone in the quest for a healthier and longer life.
Biographies
Jari A. Laukkanen is a cardiologist and researcher hailing from Jyväskylä, Finland, and holds the position of Professor of Internal Medicine at the University of Eastern Finland. His research focuses on the of lifestyle factors in cardiovascular disease prevention. His research interests prominently feature the health benefits of sauna bathing, a topic he has extensively studied. Dr. Laukkanen's research has shed light on the positive impacts of regular sauna use on cardiovascular health, including improved endothelium-dependent dilatation, reduced arterial stiffness, and a decreased risk of fatal cardiovascular events. His work has been instrumental in highlighting the potential preventive benefits of saunas in reducing the risk of various health conditions, such as Alzheimer's disease and cardiovascular diseases. Through his pioneering research, Dr. Laukkanen has significantly contributed to the emerging science of saunas and their potential therapeutic applications for improving overall health and well-being.
Setor K. Kunutsor received his doctoral degree in Cardiovascular Epidemiology from the University of Cambridge. He is currently an Associate Professor in Cardiometabolic Epidemiology in the Leicester Diabetes Research Centre in the University of Leicester. His research interests include investigating the health benefits associated with lifestyle factors such as physical activity, nutrition, cold water therapy and sauna bathing. He has conducted studies that explore the combined effects of Finnish sauna bathing with lifestyle factors such as physical activity or exercise. His research has contributed valuable insights into how these lifestyle factors may interact to improve health outcomes. His work has added to the growing body of evidence supporting the positive impacts of sauna bathing on overall health and well-being.
Funding Statement
This work received no specific funding. SKK is supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration East Midlands (ARC EM) and Leicester NIHR Biomedical Research Centre (BRC). The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(S).
References
- [1].Laukkanen JA, Laukkanen T, Kunutsor SK.. Cardiovascular and other health benefits of sauna bathing: a review of the evidence. Mayo Clin Proc. 2018;93(8):1111–1121. DOI: 10.1016/j.mayocp.2018.04.008 [DOI] [PubMed] [Google Scholar]
- [2].Kunutsor SK, Laukkanen JA. Does the combination of Finnish sauna bathing and other lifestyle factors confer additional health benefits? A review of the evidence. Mayo Clin Proc. 2023;98(6):915–926. DOI: 10.1016/j.mayocp.2023.01.008 [DOI] [PubMed] [Google Scholar]
- [3].Scanu A, Tognolo L, Maccarone MC, et al. Immunological events, emerging pharmaceutical treatments and therapeutic potential of balneotherapy on osteoarthritis. Front Pharmacol. 2021;12:681871. DOI: 10.3389/fphar.2021.681871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Maccarone MC, Scanu A, Coraci D, et al. The potential role of spa therapy in managing frailty in rheumatic patients: a scoping review. Healthcare (Basel). 2023;11(13):11. DOI: 10.3390/healthcare11131899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kaeberlein M. How healthy is the healthspan concept? Geroscience. 2018;40(4):361–364. DOI: 10.1007/s11357-018-0036-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ukai T, Iso H, Yamagishi K, et al. Habitual tub bathing and risks of incident coronary heart disease and stroke. Heart. 2020;106(10):732–737. DOI: 10.1136/heartjnl-2019-315752 [DOI] [PubMed] [Google Scholar]
- [7].Kominami K, Takahiza E, Tabuchi M, et al. Blood pressure-lowering effect of repeated waon therapy in non-smokers with hypertension. Med. 2021;100(23):e26266. DOI: 10.1097/MD.0000000000026266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rocha Conceicao LS, de Queiroz JG, Neto MG, et al. Effect of waon therapy in individuals with heart failure: a systematic review. J Card Fail. 2018;24:204–206. [DOI] [PubMed] [Google Scholar]
- [9].Miyata M, Tei C. Waon therapy for cardiovascular disease: - innovative therapy for the 21st Century -. Circ J. 2010;74(4):617–621. DOI: 10.1253/circj.CJ-09-0939 [DOI] [PubMed] [Google Scholar]
- [10].Miyata M, Tei C. Pleiotropic effect of waon therapy. JMAJ. 2009;52:191–193. [Google Scholar]
- [11].Sobajima M, Nozawa T, Fukui Y, et al. Waon therapy improves quality of life as well as cardiac function and exercise capacity in patients with chronic heart failure. Int Heart J. 2015;56(2):203–208. DOI: 10.1536/ihj.14-266 [DOI] [PubMed] [Google Scholar]
- [12].Mooventhan A, Nivethitha L. Scientific evidence-based effects of hydrotherapy on various systems of the body. N Am J Med Sci. 2014;6(5):199–209. DOI: 10.4103/1947-2714.132935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Pandiaraja M, Vanitha A, Maheshkumar K, et al. Effect of the steam bath on resting cardiovascular parameters in healthy volunteers. Advances In Integrative Medicine. 2021;8(3):199–202. DOI: 10.1016/j.aimed.2020.06.001 [DOI] [Google Scholar]
- [14].Zaccardi F, Laukkanen T, Willeit P, et al. Sauna bathing and incident hypertension: a prospective cohort study. Am J Hypertens. 2017;30(11):1120–1125. DOI: 10.1093/ajh/hpx102 [DOI] [PubMed] [Google Scholar]
- [15].Laukkanen T, Khan H, Zaccardi F, et al. Association between sauna bathing and fatal cardiovascular and all-cause mortality events. JAMA Intern Med. 2015;175(4):542–548. DOI: 10.1001/jamainternmed.2014.8187 [DOI] [PubMed] [Google Scholar]
- [16].Kunutsor SK, Khan H, Zaccardi F, et al. Sauna bathing reduces the risk of stroke in Finnish men and women: a prospective cohort study. Neurology. 2018;90(22):e1937–e. 1944. DOI: 10.1212/WNL.0000000000005606. [DOI] [PubMed] [Google Scholar]
- [17].Laukkanen T, Kunutsor S, Kauhanen J, Laukkanen, J A., et al. Sauna bathing is inversely associated with dementia and Alzheimer’s disease in middle-aged Finnish men. Age And Ageing. 2016;46:245–249. DOI: 10.1093/ageing/afw212 2 [DOI] [PubMed] [Google Scholar]
- [18].Kunutsor SK, Makikallio TH, Khan H, et al. Sauna bathing reduces the risk of venous thromboembolism: a prospective cohort study. Eur J Epidemiol. 2019;34(10):983–986. DOI: 10.1007/s10654-019-00544-z [DOI] [PubMed] [Google Scholar]
- [19].Kunutsor SK, Laukkanen T, Laukkanen JA. Sauna bathing reduces the risk of respiratory diseases: a long-term prospective cohort study. Eur J Epidemiol. 2017;32(12):1107–1111. DOI: 10.1007/s10654-017-0311-6 [DOI] [PubMed] [Google Scholar]
- [20].Kunutsor SK, Jae SY, Laukkanen JA. Impact of sauna bathing on risk of pneumonia in men with low socioeconomic status: a cohort study. J Cardiopulm Rehabil Prev. 2021;41(4):289–291. DOI: 10.1097/HCR.0000000000000611 [DOI] [PubMed] [Google Scholar]
- [21].Kunutsor SK, Laukkanen T, Laukkanen JA. Frequent sauna bathing may reduce the risk of pneumonia in middle-aged Caucasian men: the KIHD prospective cohort study. Respir Med. 2017;132:161–163. DOI: 10.1016/j.rmed.2017.10.018 [DOI] [PubMed] [Google Scholar]
- [22].Laukkanen T, Laukkanen JA, Kunutsor SK. Sauna bathing and risk of psychotic disorders: a prospective cohort study. Med Princ Pract. 2018;27(6):562–569. DOI: 10.1159/000493392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Nurmikko T, Hietaharju A. Effect of exposure to sauna heat on neuropathic and rheumatoid pain. Pain. 1992;49(1):43–51. DOI: 10.1016/0304-3959(92)90186-F [DOI] [PubMed] [Google Scholar]
- [24].Isomaki H. The sauna and rheumatic diseases. Ann Clin Res. 1988;20(4):271–275. [PubMed] [Google Scholar]
- [25].Kunutsor SK, Lavie CJ, Laukkanen J. Finnish sauna and COVID-19. Infez Med. 2021;29:160–162. [PubMed] [Google Scholar]
- [26].Laitinen LA, Lindqvist A, Heino M. Lungs and ventilation in sauna. Ann Clin Res. 1988;20(4):244–248. [PubMed] [Google Scholar]
- [27].Cox NJ, Oostendorp GM, Folgering HT, et al. Sauna to transiently improve pulmonary function in patients with obstructive lung disease. Arch Phys Med Rehabil. 1989;70(13):911–913. [PubMed] [Google Scholar]
- [28].Perasalo J. Traditional use of the sauna for hygiene and health in Finland. Ann Clin Res. 1988;20:220–223. [PubMed] [Google Scholar]
- [29].Valtakari P. The sauna and bathing in different countries. Ann Clin Res. 1988;20(4):230–235. [PubMed] [Google Scholar]
- [30].Hannuksela ML, Ellahham S. Benefits and risks of sauna bathing. Am J Med. 2001;110(2):118–126. DOI: 10.1016/S0002-9343(00)00671-9 [DOI] [PubMed] [Google Scholar]
- [31].Laukkanen T, Laukkanen J. Sauna, body & mind. Jyvaskyla: Docendo; 2020. [Google Scholar]
- [32].Kukkonen-Harjula K, Kauppinen K. Health effects and risks of sauna bathing. Int J Circumpolar Health. 2006;65(3):195–205. DOI: 10.3402/ijch.v65i3.18102 [DOI] [PubMed] [Google Scholar]
- [33].Kunutsor SK, Khan H, Laukkanen T, et al. Joint associations of sauna bathing and cardiorespiratory fitness on cardiovascular and all-cause mortality risk: a long-term prospective cohort study. Ann Med. 2018;50(2):139–146. DOI: 10.1080/07853890.2017.1387927 [DOI] [PubMed] [Google Scholar]
- [34].Lee E, Laukkanen T, Kunutsor SK, et al. Sauna exposure leads to improved arterial compliance: Findings from a non-randomised experimental study. Eur J Prev Cardiol. 2017;25(2):130–138. DOI: 10.1177/2047487317737629 [DOI] [PubMed] [Google Scholar]
- [35].Fleming SA, Gutknecht NC. Naturopathy and the primary care practice. Prim Care. 2010;37(1):119–136. DOI: 10.1016/j.pop.2009.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Oyama J, Kudo Y, Maeda T, et al. Hyperthermia by bathing in a hot spring improves cardiovascular functions and reduces the production of inflammatory cytokines in patients with chronic heart failure. Heart Vessels. 2013;28(2):173–178. DOI: 10.1007/s00380-011-0220-7 [DOI] [PubMed] [Google Scholar]
- [37].Inoue S, Takemoto M, Chishaki A, et al. Leg heating using far infra-red radiation in patients with chronic heart failure acutely improves the hemodynamics, vascular endothelial function, and oxidative stress. Intern Med. 2012;51(17):2263–2270. DOI: 10.2169/internalmedicine.51.7115 [DOI] [PubMed] [Google Scholar]
- [38].OCEBM Levels of Evidence Working Group . The oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Accessed on 8 October 2020. [Google Scholar]
- [39].Gayda M, Bosquet L, Paillard F, et al. Effects of sauna alone versus postexercise sauna baths on short-term heart rate variability in patients with untreated hypertension. J Cardiopulm Rehabil Prev. 2012;32(3):147–154. DOI: 10.1097/HCR.0b013e318251ffeb [DOI] [PubMed] [Google Scholar]
- [40].Radtke T, Poerschke D, Wilhelm M, et al. Acute effects of Finnish sauna and cold-water immersion on haemodynamic variables and autonomic nervous system activity in patients with heart failure. Eur J Prev Cardiol. 2016;23(6):593–601. DOI: 10.1177/2047487315594506 [DOI] [PubMed] [Google Scholar]
- [41].Laukkanen T, Kunutsor SK, Zaccardi F, et al. Acute effects of sauna bathing on cardiovascular function. J Hum Hypertens. 2017;32(2):129–138. DOI: 10.1038/s41371-017-0008-z. [DOI] [PubMed] [Google Scholar]
- [42].Gayda M, Paillard F, Sosner P, et al. Effects of sauna alone and postexercise sauna baths on blood pressure and hemodynamic variables in patients with untreated hypertension. J Clin Hypertens. 2012;14(8):553–560. DOI: 10.1111/j.1751-7176.2012.00637.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Brunt VE, Howard MJ, Francisco MA, et al. Passive heat therapy improves endothelial function, arterial stiffness and blood pressure in sedentary humans. J Physiol. 2016;594(18):5329–5342. DOI: 10.1113/JP272453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Shin TW, Wilson M, Wilson TW. Are hot tubs safe for people with treated hypertension? CMAJ. 2003;169(12):1265–1268. [PMC free article] [PubMed] [Google Scholar]
- [45].Pizzey FK, Smith EC, Ruediger SL, et al. The effect of heat therapy on blood pressure and peripheral vascular function: a systematic review and meta-analysis. Exp Physiol. 2021;106(6):1317–1334. DOI: 10.1113/EP089424 [DOI] [PubMed] [Google Scholar]
- [46].Laukkanen T, Kunutsor SK, Khan H, et al. Sauna bathing is associated with reduced cardiovascular mortality and improves risk prediction in men and women: a prospective cohort study. BMC Med. 2018;16(1):219. DOI: 10.1186/s12916-018-1198-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Laukkanen JA, Kunutsor SK. Is sauna bathing protective of sudden cardiac death? A review of the evidence. Prog Cardiovasc Dis. 2019;62(3):288–293. DOI: 10.1016/j.pcad.2019.05.001 [DOI] [PubMed] [Google Scholar]
- [48].Kunutsor SK, Khan H, Zaccardi F, et al. Sauna bathing reduces the risk of stroke in Finnish men and women: a prospective cohort study. Neurology. 2018;90(22). In Press. DOI: 10.1212/WNL.0000000000005606. [DOI] [PubMed] [Google Scholar]
- [49].Ye WN, Thipse M, Mahdi MB, et al. Can heat therapy help patients with heart failure? Artif Organs. 2020;44(7):680–692. DOI: 10.1111/aor.13659 [DOI] [PubMed] [Google Scholar]
- [50].Tei C, Shinsato T, Kihara T, et al. Successful thermal therapy for end-stage peripheral artery disease. J Cardiol. 2006;47(4):163–164. [PubMed] [Google Scholar]
- [51].Tei C, Shinsato T, Miyata M, et al. Waon therapy improves peripheral arterial disease. J Am Coll Cardiol. 2007;50(22):2169–2171. DOI: 10.1016/j.jacc.2007.08.025 [DOI] [PubMed] [Google Scholar]
- [52].Miyamoto H, Kai H, Nakaura H, et al. Safety and efficacy of repeated sauna bathing in patients with chronic systolic heart failure: a preliminary report. J Card Fail. 2005;11(6):432–436. DOI: 10.1016/j.cardfail.2005.03.004 [DOI] [PubMed] [Google Scholar]
- [53].Haseba S, Sakakima H, Kubozono T, et al. Combined effects of repeated sauna therapy and exercise training on cardiac function and physical activity in patients with chronic heart failure. Disabil Rehabil. 2016;38(5):409–415. DOI: 10.3109/09638288.2015.1044032 [DOI] [PubMed] [Google Scholar]
- [54].Kunutsor SK, Jae SY, Kurl S, et al. Frequent sauna bathing may mitigate the increased risk of mortality in men with elevated systolic blood pressure: a prospective cohort study. 2022. (Unpublished). [Google Scholar]
- [55].Koivisto VA. Sauna-induced acceleration in insulin absorption from subcutaneous injection site. British Med J. 1980;280(6229):1411–1413. DOI: 10.1136/bmj.280.6229.1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Hooper PL. Hot-tub therapy for type 2 diabetes mellitus. N Engl J Med. 1999;341(12):924–925. DOI: 10.1056/NEJM199909163411216 [DOI] [PubMed] [Google Scholar]
- [57].Ely BR, Clayton ZS, McCurdy CE, et al. Heat therapy improves glucose tolerance and adipose tissue insulin signaling in polycystic ovary syndrome. Am J Physiol Endocrinol Metab. 2019;317(1):E172–E182. DOI: 10.1152/ajpendo.00549.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Sebok J, Edel Z, Vancsa S, et al. Heat therapy shows benefit in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Int J Hyperthermia. 2021;38(1):1650–1659. DOI: 10.1080/02656736.2021.2003445 [DOI] [PubMed] [Google Scholar]
- [59].Kunutsor SK, Kauhanen J, Laukkanen JA. Sauna bathing, renal function and chronic kidney disease: cross-sectional and longitudinal findings from the KIHD study. Eur J Clin Invest. 2023;53(8):e14001. DOI: 10.1111/eci.14001 [DOI] [PubMed] [Google Scholar]
- [60].Ravanelli N, Barry H, Schlader ZJ, et al. Impact of passive heat acclimation on markers of kidney function during heat stress. Exp Physiol. 2021;106(1):269–281. DOI: 10.1113/EP088637 [DOI] [PubMed] [Google Scholar]
- [61].Knekt P, Jarvinen R, Rissanen H, et al. Does sauna bathing protect against dementia? Prev Med Rep. 2020;20:101221. DOI: 10.1016/j.pmedr.2020.101221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Hunt AP, Minett GM, Gibson OR, et al. Could heat therapy be an effective treatment for Alzheimer’s and Parkinson’s diseases? A narrative review. Front Physiol. 2019;10:1556. DOI: 10.3389/fphys.2019.01556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Wust P, Hildebrandt B, Sreenivasa G, et al. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002;3(8):487–497. DOI: 10.1016/S1470-2045(02)00818-5 [DOI] [PubMed] [Google Scholar]
- [64].Rao W, Deng ZS, Liu J. A review of hyperthermia combined with radiotherapy/chemotherapy on malignant tumors. Crit Rev Biomed Eng. 2010;38(1):101–116. DOI: 10.1615/CritRevBiomedEng.v38.i1.80 [DOI] [PubMed] [Google Scholar]
- [65].van der Zee J. Heating the patient: a promising approach? Ann Oncol. 2002;13:1173–1184. [DOI] [PubMed] [Google Scholar]
- [66].Yi GY, Kim MJ, Kim HI, et al. Hyperthermia treatment as a promising anti-cancer strategy: therapeutic targets, perspective mechanisms and synergistic combinations in experimental approaches. Antioxid (Basel). 2022;11(4):11. DOI: 10.3390/antiox11040625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Ernst E, Pecho E, Wirz P, et al. Regular sauna bathing and the incidence of common colds. Ann Med. 1990;22(4):225–227. DOI: 10.3109/07853899009148930 [DOI] [PubMed] [Google Scholar]
- [68].Kunutsor SK, Jae SY, Laukkanen JA. Attenuated risk of pneumonia due to inflammation by frequent sauna baths: a PROSPECTIVE COHORT STUDY. J Cardiopulm Rehabil Prev. 2022;42(1):59–63. DOI: 10.1097/HCR.0000000000000598 [DOI] [PubMed] [Google Scholar]
- [69].Kunutsor SK, Laukkanen JA. High fitness levels, frequent sauna bathing and risk of pneumonia in a cohort study: are there potential implications for COVID-19? Eur J Clin Invest. 2021;51(3):e13490. DOI: 10.1111/eci.13490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Kunutsor SK, Jae SY, Laukkanen JA. The interplay between socioeconomic status, sauna bathing and chronic obstructive pulmonary disease: a longitudinal study. J Cardiopulm Rehabil Prev. 2022;43(2):148–150. In Press. DOI: 10.1097/HCR.0000000000000759. [DOI] [PubMed] [Google Scholar]
- [71].Kunutsor SK, Laukkanen JA. Frequent sauna bathing may reduce chronic obstructive pulmonary disease risk: a prospective study. Eur J Clin Invest. 2023;53(5):e13940. DOI: 10.1111/eci.13940 [DOI] [PubMed] [Google Scholar]
- [72].Tyrrell D, Barrow I, Arthur J. Local hyperthermia benefits natural and experimental common colds. BMJ. 1989;298(6683):1280–1283. DOI: 10.1136/bmj.298.6683.1280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Singh M, Singh M, Jaiswal N, et al.Heated, humidified air for the common cold Cochrane Database Syst Rev 8CD00172820178 DOI: 10.1002/14651858.CD001728.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Umehara M, Yamaguchi A, Itakura S, et al. Repeated waon therapy improves pulmonary hypertension during exercise in patients with severe chronic obstructive pulmonary disease. J Cardiol. 2008;51(2):106–113. DOI: 10.1016/j.jjcc.2008.01.004 [DOI] [PubMed] [Google Scholar]
- [75].Matsushita K, Masuda A, Tei C. Efficacy of waon therapy for fibromyalgia. Intern Med. 2008;47(16):1473–1476. DOI: 10.2169/internalmedicine.47.1054 [DOI] [PubMed] [Google Scholar]
- [76].Cozzi F, Ciprian L, Carrara M, et al. Balneotherapy in chronic inflammatory rheumatic diseases—a narrative review. Int J Biometeorol. 2018;62(12):2065–2071. DOI: 10.1007/s00484-018-1618-z [DOI] [PubMed] [Google Scholar]
- [77].Masiero S, Vittadini F, Ferroni C, et al. The role of thermal balneotherapy in the treatment of obese patient with knee osteoarthritis. Int J Biometeorol. 2018;62(2):243–252. DOI: 10.1007/s00484-017-1445-7 [DOI] [PubMed] [Google Scholar]
- [78].Hannuksela M, Vaananen A. The sauna, skin and skin diseases. Ann Clin Res. 1988;20(4):276–278. [PubMed] [Google Scholar]
- [79].Kowatzki D, Macholdt C, Krull K, et al. Effect of regular sauna on epidermal barrier function and stratum corneum water-holding capacity in vivo in humans: a controlled study. Dermatology. 2008;217(2):173–180. DOI: 10.1159/000137283 [DOI] [PubMed] [Google Scholar]
- [80].Brunt VE, Eymann TM, Francisco MA, et al.Passive heat therapy improves cutaneous microvascular function in sedentary humans via improved nitric oxide-dependent dilation J Appl Physiol 19852016121716–723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Putkonen PT, Elomaa E. Sauna and physiological sleep: increased slow-wave sleep after heat exposure. In: Valtakari H, Collan Y.P, editors. Sauna studies. Helsinki: The Finnish Sauna Society; 1976. [Google Scholar]
- [82].Mishima Y, Hozumi S, Shimizu T, et al. Passive body heating ameliorates sleep disturbances in patients with vascular dementia without circadian phase-shifting. Am J Geriatr Psychiatry. 2005;13(5):369–376. DOI: 10.1097/00019442-200505000-00005 [DOI] [PubMed] [Google Scholar]
- [83].Liao WC. Effects of passive body heating on body temperature and sleep regulation in the elderly: a systematic review. Int J Nurs Stud. 2002;39(8):803–810. DOI: 10.1016/S0020-7489(02)00023-8 [DOI] [PubMed] [Google Scholar]
- [84].Liu J, Zhou J, Yao J, et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci Total Environ. 2020;726:138513. DOI: 10.1016/j.scitotenv.2020.138513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Jaakkola K, Saukkoriipi A, Jokelainen J, et al. Decline in temperature and humidity increases the occurrence of influenza in cold climate. Environ Health. 2014;13(1):22. DOI: 10.1186/1476-069X-13-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Chan KH, Peiris JS, Lam SY, et al.The effects of temperature and relative humidity on the viability of the SARS Coronavirus Adv Virol 201120111–72011 DOI: 10.1155/2011/734690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Kunutsor SK, Laukkanen T, Laukkanen J. Longitudinal associations of sauna bathing with inflammation and oxidative stress: the KIHD prospective cohort study. Ann Med. 2018;50(5):437–442. DOI: 10.1080/07853890.2018.1489143 [DOI] [PubMed] [Google Scholar]
- [88].Laukkanen JA, Laukkanen T. Sauna bathing and systemic inflammation. Eur J Epidemiol. 2018;33(3):351–353. DOI: 10.1007/s10654-017-0335-y [DOI] [PubMed] [Google Scholar]
- [89].Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. DOI: 10.1016/S0140-6736(20)30628-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Hagglund H. Sauna bathing and lower urinary tract symptoms- the heat is on? Scand J Urol. 2022;56(2):168. DOI: 10.1080/21681805.2022.2028898 [DOI] [PubMed] [Google Scholar]
- [91].Poyhonen A, Akerla J, Koskimaki J, et al. Sauna habits/bathing and changes in lower urinary tract symptoms – Tampere ageing male urologic study (TAMUS). Scand J Urol. 2022;56(1):77–82. DOI: 10.1080/21681805.2021.2002403 [DOI] [PubMed] [Google Scholar]
- [92].Kanji G, Weatherall M, Peter R, et al. Efficacy of regular sauna bathing for chronic tension-type headache: a randomized controlled study. J Altern Complement Med. 2015;21(2):103–109. DOI: 10.1089/acm.2013.0466 [DOI] [PubMed] [Google Scholar]
- [93].Strandberg TE, Strandberg A, Pitkala K, et al. Sauna bathing, health, and quality of life among octogenarian men: the Helsinki Businessmen Study. Aging Clin Exp Res. 2017;30(9):1053–1057. DOI: 10.1007/s40520-017-0855-z [DOI] [PubMed] [Google Scholar]
- [94].Beever R. The effects of repeated thermal therapy on quality of life in patients with type II diabetes mellitus. J Altern Complement Med. 2010;16(6):677–681. DOI: 10.1089/acm.2009.0358 [DOI] [PubMed] [Google Scholar]
- [95].Masuda A, Nakazato M, Kihara T, et al. Repeated thermal therapy diminishes appetite loss and subjective complaints in mildly depressed patients. Psychosom Med. 2005;67(4):643–647. DOI: 10.1097/01.psy.0000171812.67767.8f [DOI] [PubMed] [Google Scholar]
- [96].Lee E, Willeit P, Laukkanen T, et al. Acute effects of exercise and sauna as a single intervention on arterial compliance. Eur J Prev Cardiol. 2020;27(10):1104–1107. DOI: 10.1177/2047487319855454 [DOI] [PubMed] [Google Scholar]
- [97].Lee E, Kostensalo J, Willeit P, et al. Standalone sauna vs exercise followed by sauna on cardiovascular function in non-naïve sauna users: A comparison of acute effects. Health Sci Rep. 2021;4(4):e393. DOI: 10.1002/hsr2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Stanley J, Halliday A, D’Auria S, et al. Effect of sauna-based heat acclimation on plasma volume and heart rate variability. Eur J Appl Physiol. 2015;115(4):785–794. DOI: 10.1007/s00421-014-3060-1 [DOI] [PubMed] [Google Scholar]
- [99].Rissanen JA, Hakkinen K, Laukkanen JA, et al. Acute hemodynamic responses to combined exercise and sauna. Int J Sports Med. 2020;41(12):824–831. DOI: 10.1055/a-1186-1716 [DOI] [PubMed] [Google Scholar]
- [100].Lee E, Kolunsarka IA, Kostensalo J, et al. Effects of regular sauna bathing in conjunction with exercise on cardiovascular function: A multi-arm randomized controlled trial. Am J Physiol Regul Integr Comp Physiol. 2022;323(3):R289–R299. DOI: 10.1152/ajpregu.00076.2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Mero A, Tornberg J, Mantykoski M, et al. Effects of far-infrared sauna bathing on recovery from strength and endurance training sessions in men. Springerplus. 2015;4(1):321. DOI: 10.1186/s40064-015-1093-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Pilch W, Pokora I, Szygula Z, et al. Effect of a single Finnish sauna session on white blood cell profile and cortisol levels in athletes and non-athletes. J Hum Kinet. 2013;39(1):127–135. DOI: 10.2478/hukin-2013-0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Laukkanen J, Laukkanen T, Khan H, et al. Combined effect of sauna bathing and cardiorespiratory fitness on the risk of sudden cardiac deaths in Caucasian men: a long-term prospective cohort study. Prog Cardiovasc Dis. 2018;60(6):635–641. DOI: 10.1016/j.pcad.2018.03.005 [DOI] [PubMed] [Google Scholar]
- [104].Kubozono T, Miyata M, Haseba J, et al. Effect and safety of combination of waon therapy and exercise training in patients with chronic heart failure. J Card Fail. 2011;17(9):S135. DOI: 10.1016/j.cardfail.2011.06.632 [DOI] [Google Scholar]
- [105].Sakurai R, Fujiwara Y, Saito K, et al. Effects of a comprehensive intervention program, including hot bathing, on overweight adults: a randomized controlled trial. Geriatr Gerontol Int. 2013;13(3):638–645. DOI: 10.1111/j.1447-0594.2012.00955.x [DOI] [PubMed] [Google Scholar]
- [106].Sutkowy P, Woźniak A, Boraczyński T, et al. The effect of a single Finnish sauna bath after aerobic exercise on the oxidative status in healthy men. Scand J Clin Lab Invest. 2014;74(2):89–94. DOI: 10.3109/00365513.2013.860616 [DOI] [PubMed] [Google Scholar]
- [107].Masuda A, Miyata M, Kihara T, et al. Repeated sauna therapy reduces urinary 8-epi-prostaglandin F2.ALPHA. Jpn Heart J. 2004;45(2):297–303. DOI: 10.1536/jhj.45.297 [DOI] [PubMed] [Google Scholar]
- [108].Miyata M, Kihara T, Kubozono T, et al. Beneficial effects of waon therapy on patients with chronic heart failure: results of a prospective multicenter study. J Cardiol. 2008;52(2):79–85. DOI: 10.1016/j.jjcc.2008.07.009 [DOI] [PubMed] [Google Scholar]
- [109].Lee E, Laukkanen T, Kunutsor SK, et al. Sauna exposure leads to improved arterial compliance: findings from a non-randomised experimental study. Eur J Prev Cardiol. 2018;25(2):130–138. DOI: 10.1177/2047487317737629 [DOI] [PubMed] [Google Scholar]
- [110].Ganio MS, Brothers RM, Shibata S, et al. Effect of passive heat stress on arterial stiffness. Exp Physiol. 2011;96(9):919–926. DOI: 10.1113/expphysiol.2011.057091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Ohori T, Nozawa T, Ihori H, et al. Effect of repeated sauna treatment on exercise tolerance and endothelial function in patients with chronic heart failure. Am J Cardiol. 2012;109(1):100–104. DOI: 10.1016/j.amjcard.2011.08.014 [DOI] [PubMed] [Google Scholar]
- [112].Imamura M, Biro S, Kihara T, et al. Repeated thermal therapy improves impaired vascular endothelial function in patients with coronary risk factors. J Am Coll Cardiol. 2001;38(4):1083–1088. DOI: 10.1016/S0735-1097(01)01467-X [DOI] [PubMed] [Google Scholar]
- [113].Kihara T, Biro S, Imamura M, et al. Repeated sauna treatment improves vascular endothelial and cardiac function in patients with chronic heart failure. J Am Coll Cardiol. 2002;39(5):754–759. DOI: 10.1016/S0735-1097(01)01824-1 [DOI] [PubMed] [Google Scholar]
- [114].Brunt VE, Weidenfeld-Needham KM, Comrada LN, et al. Serum from young, sedentary adults who underwent passive heat therapy improves endothelial cell angiogenesis via improved nitric oxide bioavailability. Temperature. 2019;6(2):169–178. DOI: 10.1080/23328940.2019.1614851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Gryka D, Pilch W, Szarek M, et al. The effect of sauna bathing on lipid profile in young, physically active, male subjects. Int J Occup Med Environ Health. 2014;27(4):608–618. DOI: 10.2478/s13382-014-0281-9 [DOI] [PubMed] [Google Scholar]
- [116].Pilch W, Szygula Z, Klimek AT, et al. Changes in the lipid profile of blood serum in women taking sauna baths of various duration. Int J Occup Med Environ Health. 2010;23(2):167–174. DOI: 10.2478/v10001-010-0020-9 [DOI] [PubMed] [Google Scholar]
- [117].Scoon GS, Hopkins WG, Mayhew S, et al. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners. J Sci Med Sport. 2007;10(4):259–262. DOI: 10.1016/j.jsams.2006.06.009 [DOI] [PubMed] [Google Scholar]
- [118].Crandall CG, González-Alonso J. Cardiovascular function in the heat-stressed human. Acta Physiol (Oxf). 2010;199(4):407–423. DOI: 10.1111/j.1748-1716.2010.02119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Kukkonen-Harjula K, Kauppinen K. How the sauna affects the endocrine system. Ann Clin Res. 1988;20(4):262–266. [PubMed] [Google Scholar]
- [120].Tei C, Horikiri Y, Park JC, et al. Acute hemodynamic improvement by thermal vasodilation in congestive heart failure. Circulation. 1995;91(10):2582–2590. DOI: 10.1161/01.CIR.91.10.2582 [DOI] [PubMed] [Google Scholar]
- [121].Von E. Quantitation of stress by Catecholamine Analysis. Clin Pharmacol Ther. 1964;5(4):398–404. DOI: 10.1002/cpt196454398 [DOI] [PubMed] [Google Scholar]
- [122].Laukkanen T, Lipponen J, Kunutsor SK, et al. Recovery from sauna bathing favorably modulates cardiac autonomic nervous system. Complement Ther Med. 2019;45:190–197. DOI: 10.1016/j.ctim.2019.06.011 [DOI] [PubMed] [Google Scholar]
- [123].Genuis SJ, Birkholz D, Rodushkin I, et al. Blood, urine, and sweat (BUS) study: monitoring and elimination of bioaccumulated toxic elements. Arch Environ Contam Toxicol. 2011;61(2):344–357. DOI: 10.1007/s00244-010-9611-5 [DOI] [PubMed] [Google Scholar]
- [124].Patrick RP, Johnson TL. Sauna use as a lifestyle practice to extend healthspan. Exp Gerontol. 2021;154:111509. DOI: 10.1016/j.exger.2021.111509 [DOI] [PubMed] [Google Scholar]
- [125].Kojima D, Nakamura T, Banno M, et al. Head-out immersion in hot water increases serum BDNF in healthy males. Int J Hyperthermia. 2018;34(6):834–839. DOI: 10.1080/02656736.2017.1394502 [DOI] [PubMed] [Google Scholar]
- [126].Kauppinen K, Vuori I. Man in the sauna. Ann Clin Res. 1986;18(4):173–185. [PubMed] [Google Scholar]
- [127].Rissanen JA, Hakkinen A, Laukkanen J, et al. Acute neuromuscular and hormonal responses to different exercise loadings followed by a sauna. J Strength Cond Res. 2020;34(2):313–322. DOI: 10.1519/JSC.0000000000003371 [DOI] [PubMed] [Google Scholar]
- [128].Huhtaniemi IT, Laukkanen JA. Endocrine effects of sauna bath. Current Opinion In Endocrine And Metabolic Research. 2020;11:15–20. DOI: 10.1016/j.coemr.2019.12.004 [DOI] [Google Scholar]
- [129].Vescovi PP, DiGennaro C, Hormonal CV. (ACTH, cortisol, beta-endorphin, and met-enkephalin) and cardiovascular responses to hyperthermic stress in chronic alcoholics. Alcohol Clin Exp Res. 1997;21:1195–1198. [PubMed] [Google Scholar]
- [130].Kappel M, Gyhrs A, Galbo H, et al. The response on glucoregulatory hormones of in vivo whole body hyperthermia. Int J Hyperthermia. 1997;13(4):413–421. DOI: 10.3109/02656739709046542 [DOI] [PubMed] [Google Scholar]
- [131].Rivas E, Newmire DE, Crandall CG, et al. An acute bout of whole body passive hyperthermia increases plasma leptin, but does not alter glucose or insulin responses in obese type 2 diabetics and healthy adults. J Therm Biol. 2016;59:26–33. DOI: 10.1016/j.jtherbio.2016.04.010 [DOI] [PubMed] [Google Scholar]
- [132].Laatikainen T, Salminen K, Kohvakka A, et al. Response of plasma endorphins, prolactin and catecholamines in women to intense heat in a sauna. Eur J Appl Physiol Occup Physiol. 1988;57(1):98–102. DOI: 10.1007/BF00691246 [DOI] [PubMed] [Google Scholar]
- [133].Salleh MR. Life event, stress and illness. Malays J Med Sci. 2008;15:9–18. [PMC free article] [PubMed] [Google Scholar]
- [134].Vuori I. Sauna bather’s circulation. Ann Clin Res. 1988;20:249–256. 4 [PubMed] [Google Scholar]
- [135].Ketelhut S, Ketelhut RG. The blood pressure and heart rate during sauna bath correspond to cardiac responses during submaximal dynamic exercise. Complement Ther Med. 2019;44:218–222. DOI: 10.1016/j.ctim.2019.05.002 [DOI] [PubMed] [Google Scholar]
- [136].Morimoto RI. Cells in stress: transcriptional activation of heat shock genes. Sci. 1993;259(5100):1409–1410. DOI: 10.1126/science.8451637 [DOI] [PubMed] [Google Scholar]
- [137].Faulkner SH, Jackson S, Fatania G, et al. The effect of passive heating on heat shock protein 70 and interleukin-6: a possible treatment tool for metabolic diseases? Temperature. 2017;4(3):292–304. DOI: 10.1080/23328940.2017.1288688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Calderwood SK, Murshid A, Prince T. The shock of aging: molecular chaperones and the heat shock response in longevity and aging–a mini-review. Gerontology. 2009;55(5):550–558. DOI: 10.1159/000225957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139].Madeo F, Zimmermann A, Maiuri MC, et al. Essential role for autophagy in life span extension. J Clin Invest. 2015;125(1):85–93. DOI: 10.1172/JCI73946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Sies H. Oxidative stress: a concept in redox biology and medicine. Redox Biol. 2015;4:180–183. DOI: 10.1016/j.redox.2015.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Marchant ED, Nelson WB, Hyldahl RD, et al. Passive heat stress induces mitochondrial adaptations in skeletal muscle. Int J Hyperthermia. 2023;40(1):2205066. DOI: 10.1080/02656736.2023.2205066 [DOI] [PubMed] [Google Scholar]
- [142].Gonzalez-Freire M, de Cabo R, Bernier M, et al. Reconsidering the role of mitochondria in aging. J Gerontol A Biol Sci Med Sci. 2015;70(11):1334–1342. DOI: 10.1093/gerona/glv070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Dai DF, Chiao YA, Marcinek DJ, et al. Mitochondrial oxidative stress in aging and healthspan. Longev Healthspan. 2014;3(1):6. DOI: 10.1186/2046-2395-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Dai DF, Rabinovitch PS, Ungvari Z, et al. Mitochondria and cardiovascular aging. Circ Res. 2012;110(8):1109–1124. DOI: 10.1161/CIRCRESAHA.111.246140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Hubbard BP, Sinclair DA. Small molecule SIRT1 activators for the treatment of aging and age-related diseases. Trends Pharmacol Sci. 2014;35(3):146–154. DOI: 10.1016/j.tips.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Schmid JP. Some like it hot: cardiovascular health benefits of Finnish sauna. Eur J Prev Cardiol. 2018;25(2):127–129. DOI: 10.1177/2047487317742501 [DOI] [PubMed] [Google Scholar]
- [147].Shoenfeld Y, Sohar E, Ohry A, et al. Heat stress: comparison of short exposure to severe dry and wet heat in saunas. Arch Phys Med Rehabil. 1976;57(3):126–129. [PubMed] [Google Scholar]
- [148].Luurila OJ. The sauna and the heart. J Intern Med. 1992;231(4):319–320. DOI: 10.1111/j.1365-2796.1992.tb00938.x [DOI] [PubMed] [Google Scholar]
- [149].Kihara T, Biro S, Ikeda Y, et al. Effects of repeated sauna treatment on ventricular arrhythmias in patients with chronic heart failure. Circ J. 2004;68(12):1146–1151. DOI: 10.1253/circj.68.1146 [DOI] [PubMed] [Google Scholar]
- [150].Ylikahri R, Heikkonen E, Soukas A. The sauna and alcohol. Ann Clin Res. 1988;20(4):287–291. [PubMed] [Google Scholar]
- [151].Roine R, Luurila OJ, Suokas A, et al. Alcohol and sauna bathing: effects on cardiac rhythm, blood pressure, and serum electrolyte and cortisol concentrations. J Intern Med. 1992;231(4):333–338. DOI: 10.1111/j.1365-2796.1992.tb00941.x [DOI] [PubMed] [Google Scholar]
- [152].Eisalo A, Luurila OJ. The Finnish sauna and cardiovascular diseases. Ann Clin Res. 1988;20(4):267–270. [PubMed] [Google Scholar]
- [153].Papp A. Sauna-related burns: a review of 154 cases treated in Kuopio University Hospital burn center 1994–2000. Burns. 2002;28(1):57–59. DOI: 10.1016/S0305-4179(01)00073-0 [DOI] [PubMed] [Google Scholar]
- [154].Lateef F. Post exercise ice water immersion: is it a form of active recovery? J Emerg Trauma Shock. 2010;3(3):302. DOI: 10.4103/0974-2700.66570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Keatinge WR, Evans M. The respiratory and cardiovascular response to immersion in cold and warm water. Q J Exp Physiol Cogn Med Sci. 1961;46(1):83–94. DOI: 10.1113/expphysiol.1961.sp001519 [DOI] [PubMed] [Google Scholar]
- [156].Schmid JP, Morger C, Noveanu M, et al. Haemodynamic and arrhythmic effects of moderately cold (22°C) water immersion and swimming in patients with stable coronary artery disease and heart failure. Eur J Heart Fail. 2009;11(9):903–909. DOI: 10.1093/eurjhf/hfp114 [DOI] [PubMed] [Google Scholar]
- [157].Keast ML, Adamo KB. The Finnish sauna bath and its use in patients with cardiovascular disease. J Cardiopulm Rehabil. 2000;20(4):225–230. DOI: 10.1097/00008483-200007000-00002 [DOI] [PubMed] [Google Scholar]
- [158].Vuori I. The heart and the cold. Ann Clin Res. 1987;19(3):156–162. [PubMed] [Google Scholar]
- [159].Vuori I. Healthy and unhealthy sauna bathing. Ann Clin Res. 1988;20:217–219. [PubMed] [Google Scholar]
- [160].Akerman AP, Tipton M, Minson CT, et al. Heat stress and dehydration in adapting for performance: good, bad, both, or neither? Temperature. 2016;3(3):412–436. DOI: 10.1080/23328940.2016.1216255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [161].Leyk D. Health risks and interventions in exertional heat stress. Dtsch Arztebl Int. 2019;116:537–544. DOI: 10.3238/arztebl.2019.0537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162].Garcia CK, Renteria LI, Leite-Santos G, et al. Exertional heat stroke: pathophysiology and risk factors. BMJ Med. 2022;1(1):e000239. DOI: 10.1136/bmjmed-2022-000239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Meade RD, Akerman AP, Notley SR, et al. Physiological factors characterizing heat-vulnerable older adults: a narrative review. Environ Int. 2020;144:105909. DOI: 10.1016/j.envint.2020.105909 [DOI] [PubMed] [Google Scholar]
- [164].Fjallbrant H, Akerstrom M, Svensson E, et al. Hot tub lung: an occupational hazard. Eur Respir Rev. 2013;22(127):88–90. DOI: 10.1183/09059180.00002312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [165].Turner B, Pennefather J, Edmonds C. Cardiovascular effects of hot water immersion (suicide soup). Med J Aust. 1980;2(1):39–40. DOI: 10.5694/j.1326-5377.1980.tb131813.x [DOI] [PubMed] [Google Scholar]
- [166].Baartmans M, Kerkhof E, Vloemans J, et al. Steam inhalation therapy: severe scalds as an adverse side effect. Br J Gen Pract. 2012;62(600):e473–477. DOI: 10.3399/bjgp12X652337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Patel CJ, Ioannidis JP. Placing epidemiological results in the context of multiplicity and typical correlations of exposures. J Epidemiol Community Health. 2014;68(11):1096–1100. DOI: 10.1136/jech-2014-204195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil. 2014;22(3):363–388. DOI: 10.1016/j.joca.2014.01.003 [DOI] [PubMed] [Google Scholar]


