Abstract
Objectives:
The medial collateral ligament (MCL) injury is one of the possible complications of primary total knee arthroplasty (TKA), which can lead to coronal-plane instability that requires surgical revision. Injured MCL can result in joint instability and polyethylene wear. Different strategies have been proposed for MCL reconstruction based on the location of the injury. However, there is a lack of clarity regarding the optimal method for handling an iatrogenic MCL injury throughout a TKA.
Methods:
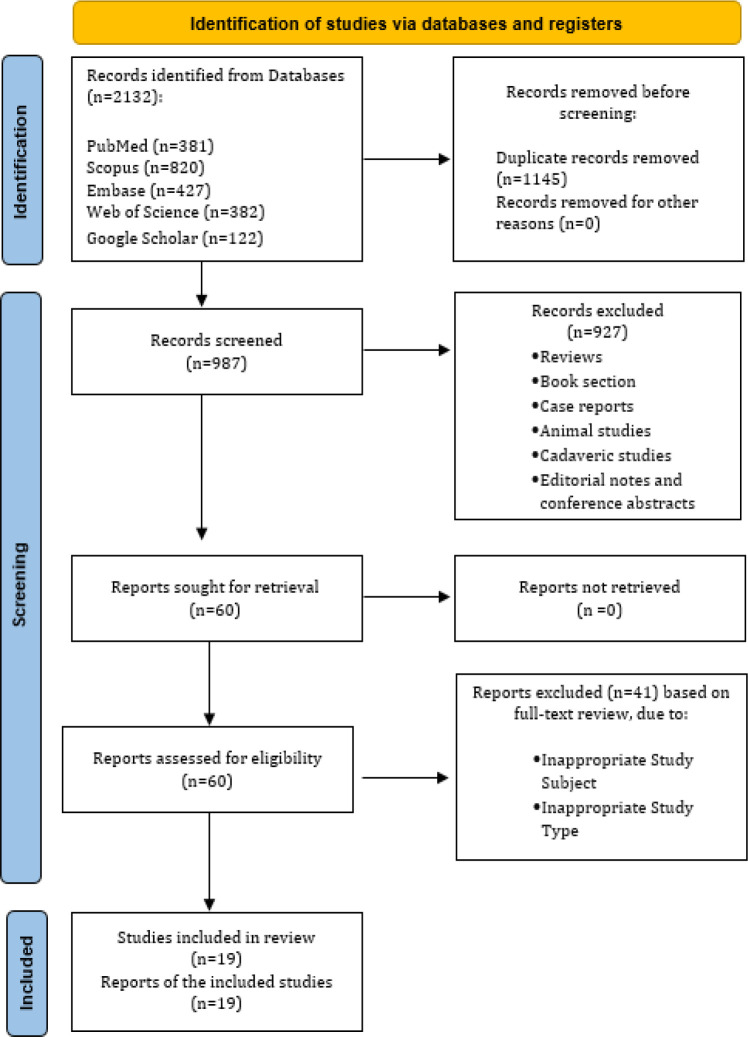
A PRISMA flow diagram was used to guide the systematic literature review. An extensive search was conducted in PubMed, Embase, Scopus, Web of Science, and Google Scholar. Newcastle Ottawa scale checklist was used to assess the methodological quality of the articles.
Results:
A total of 19 qualitative studies, including non-cadaveric patients with MCL injury during TKA, were identified after analyzing the full text of the articles. All included studies were either retrospective, observational cohort or case series. A total of 486 patients were studied to gather information on the methods used to repair the MCL and their results. Most injuries arose in the tibial attachment, which surgeons mostly realized during the final stages of surgery. Used techniques can be categorized into three main groups: Primary repair, Repair with augmentation, and changing prosthesis characteristics.
Conclusion:
This systematic review demonstrated that the most popular management of iatrogenic MCL injury was using suture anchors, staples, screws and washers, and more constrained prostheses. The proper method should be decided considering the site of the MCL injury.
Key Words: Arthroplasty, Iatrogenic mcl injury, Intraoperative complications, Intraoperative repair, Knee, Medial collateral ligament
Introduction
Iatrogenic injury of the medial collateral ligament (MCL) during primary total knee arthroplasty (TKA) can lead to coronal-plane instability, which may require revision TKA if left untreated.1-5 The incidence of iatrogenic MCL injuries ranges from 0.77 to 2.7% in TKA patients (2.4), and it may reach 8% among obese patients.5 An injured MCL can result in knee instability, which can accelerate the polyethylene wear. Additionally, a lack of MCL leads to pain and decreased postoperative function of the knee.3,6,7
Iatrogenic MCL injury occurs at various sites, such as mid-substance,6 tibial insertion,8,9 and femoral insertion.10 There are two main categories of risk factors for iatrogenic MCL injury during TKA: patient-related factors and surgeon-related factors. The patient-related factors such as severe varus deformities, associated sagittal deformities such as fixed flexion deformities, knee stiffness, osteoporosis, and obesity are associated with an increased risk of MCL injuries.11 There are also surgeon-related factors such as hyper-flexing the knees during the exposure, failing to remove tenting medial osteophytes beneath the MCL, not protecting the MCL while handling the oscillating sawblade, incorrectly balanced MCLs, insertion of thick trial meniscus components, retraction in hyperflexion, and forceful extension increase the risk of intraoperative MCL injury.4,12
There is still ongoing debate surrounding the most effective approach for handling intraoperative MCL injury. The treatment options could be categorized into three main groups ranging from 1) primary repair, including using suture or staple only,2,13,14 fixing with screws and washer construct,13 or using suture anchors,12 2) repair with augmentation using autograft6 or synthetic ligament,15 or meniscus transfer,16 3) changing prosthesis characteristic such as thicker polyethylene insert,12,17 or conversion to the constrained prosthesis.3,12 Although various approaches exist for managing iatrogenic MCL injuries in TKA, there is still no agreement on the best approach when it comes to the site of injury. As such, this study aimed to assess all possible techniques that can be utilized in this context.
Materials and Methods
In accordance with PRISMA (18), articles were screened against eligibility criteria prior to performing the systematic review. In this study, the researchers identified patients who experienced an intraoperative iatrogenic MCL injury while undergoing primary TKA using data obtained from the existing literature. During these primary TKA, the MCL was injured intraoperatively as an inadvertent intraoperative event. Observational studies were considered retrospectively and prospectively since randomized trials were not anticipated. To find non-cadaveric original articles across a wide range of databases without limiting language, a search strategy was developed. An assessment of the quality scores of included studies was done using the Newcastle-Ottawa Scale.
Search Strategy
The following keywords were used during the period from conception to March 2023 by an independent investigator (AM) to search PubMed, Embase, Scopus, Web of Science, and Google Scholar: ("knee arthroplasty" OR "knee replacement" OR "TKA") AND ("MCL" OR "medial collateral ligament" OR "collateral ligament") as well as MeSH terms.
Eligibility and Study Selection
We included all studies investigating the iatrogenic MCL injury during TKA in any language. Exclusion criteria were 1) case reports, 2) reviews (narrative, systematic, or meta-analyses), 3) cadaveric studies, 4) animal studies, 5) consensus statements and guidelines, 6) editorial notes, letters, and conference abstracts, 7) studies with insufficient data. Two independent authors (AP and SA) reviewed every report.
Results
The flowchart for this systematic review can be found in [Figure 1]. We used PubMed, Scopus, Embase, Web of Science, and Google Scholar in the initial search. A total of 2,132 articles were found during the initial search, including 381 articles from PubMed, 820 from Scopus, 427 from Embase, 382 from Web of Science, and 122 from Google Scholar. A total of 1,145 articles were removed by Endnote software as duplicate articles. Due to inappropriate study types and inappropriate study participants, 927 out of 987 reports were excluded as a result of the title and abstract screening and application of the exclusion criteria. Upon evaluating the full text of the studies, 19 qualitative studies were identified. A summary of the study and patients' characteristics is shown in [Table 1]. An evaluation was conducted on 19 retrospective studies, including 486 patients. [Table 2] contains more details about the information that we went over and selected from the articles. Iatrogenic MCL injuries occur at three sites: tibial insertion, femoral insertion, and mid-substance. As shown in [Table 3], in most studies, most injuries arise in the tibial attachment, which surgeons may realize during the final stages of surgery. The most popular techniques were primary repair and augmentation, suture anchors, staples, screws and washers, and more constrained prostheses.
Figure 1.
Study selection based on the Preferred Reporting Items for Systematic Reviews (PRISMA) 2018 statement
Table 1.
Characteristics of the included studies
| Male/Female, % | Age (y),Mean or Range | Follow-up Period (months) |
No.
of Cases |
Study Design, Patient Enrollment |
Study
Period |
Country | Year | Lead Author |
|---|---|---|---|---|---|---|---|---|
| 4/96 | 67 (59–74) | 24 | 43 | Prospective, consecutive | January 2003 to December 2015 | China | 2022 | Jin et al.9 |
| 14.28/85.75 | 67.3±6.6 | 24 | 14 | Prospective, consecutive | January 2016 to 2018 | China | 2021 | Liu et al.21 |
| 21.42/78.58 | 72.6±3.9 | 24 | 14 | Prospective, consecutive | January 2009 to December 2016 | China | 2021 | Li et al.22 |
| 18/82 | 64.2 ± 5.64 | 24 | 11 | Prospective, consecutive | January 2014 to November 2019 | China | 2020 | Sun et al.16 |
| 17.1/82.9 | 65.22 ± 7.97 | 24 | 41 | Prospective, consecutive | January 2011 to December 2015 | India | 2020 | Rajkumar et al.10 |
| 5.6/94.4 | 68±5 | 24 | 35 | Prospective, consecutive | 2007 to 2017 | Iran | 2020 | Motiffard et al.23 |
| 14.28/85.75 | 63.6 (49–79) | 15.6 | 14 | Prospective, consecutive | March 2018 and March 2019 | China | 2020 | Ni et al.25 |
| 30.3/69.7 | 63.6 (8.95) | 24 | 33 | Prospective, consecutive | 2005 to 2015 | USA | 2019 | White et al.20 |
| NA | 71.4±7.8 | 24 | 65 | Prospective, consecutive | January 2003 to June 2014 | South Korea | 2019 | Jin et al.24 |
| 0/100 | 67.4 ± 6.0 | 24 | 53 | Prospective, consecutive | January 2001 to February 2006 | South Korea | 2018 | Choi et al.8 |
| 23.52/76.48 | 63.0±4.2 | 24 | 17 | Prospective, consecutive | 2007 to 2013 | China | 2017 | Wang et al.26 |
| 13/87 | 66.5 ± 9.7 | 24 | 23 | Prospective, consecutive | January 2003 and December 2009 | USA | 2016 | Siqueira et al.4 |
| 18.18/81.82 | 64.3 (55-77) | 24 | 11 | Prospective, consecutive | March 2009 to May 2014 | China | 2016 | Cao et al.27 |
| 15.55/84.45 | 85.22 | 24 | 45 | Prospective, consecutive | 1991 to 2009 | USA | 2016 | Bohl et al.13 |
| NA | 64 (43-85) | 12 ± 5 | 11 | Prospective, consecutive | January 2003 and November 2012 a | USA | 2014 | Shahi et al.15 |
| NA | 64.8 | 12 | 10 | Prospective, consecutive | 2005 to 2012 | Romania | 2013 | Dragosloveanu et al.12 |
| NA | 58 | NA | 9 | NA | 5 years | USA | 2012 | Stephens et al.14 |
| 48.64/51.36 | 60 | 24 | 37 | Prospective, consecutive | 1998 to 2004 | USA | 2010 | Lee et al.3 |
| 28.57/71.43 | 63 (47-86) | 45 | 14 | Prospective, consecutive | June 1991 to June 1997 | USA | 2001 | Leopold et al.2 |
Table 2.
Newcastle-Ottawa scale of the included studies
| Total | Exposure | Comparability | Selection | ||
|---|---|---|---|---|---|
| 7 | ★★ | ★★ | ★★★ | Sun et al.16 | |
| 7 | ★★ | ★★ | ★★★ | Jin et al.9 | |
| 7 | ★★ | ★★ | ★★★ | Rajkumar et al.10 | |
| 7 | ★★ | ★★ | ★★★ | Motiffard et al.23 | |
| 7 | ★★ | ★★ | ★★★ | Liu et al.21 | |
| 7 | ★★ | ★★ | ★★★ | Li et al.22 | |
| 7 | ★★ | ★★ | ★★★ | Ni et al.25 | |
| 7 | ★★ | ★★ | ★★★ | White et al.20 | |
| 7 | ★★ | ★★ | ★★★ | Jin et al.24 | |
| 7 | ★★ | ★★ | ★★★ | Choi et al.8 | |
| 7 | ★★ | ★★ | ★★★ | Wang et al.26 | |
| 7 | ★★ | ★★ | ★★★ | Siqueira et al.4 | |
| 7 | ★★ | ★★ | ★★★ | Cao et al.27 | |
| 7 | ★★ | ★★ | ★★★ | Bohl et al.13 | |
| 7 | ★★ | ★★ | ★★★ | Shahi et al.15 | |
| 7 | ★★ | ★★ | ★★★ | Dragosloveanu et al.12 | |
| 7 | ★★ | ★★ | ★★★ | Stephens et al.14 | |
| 7 | ★★ | ★★ | ★★★ | Lee et al.3 | |
| 6 | ★★ | ★ | ★★★ | Leopold et al.2 | |
Table 3.
Details of the included studies
| Lead author | Year |
Method of
repair |
No. of patients |
Site of
injury |
Phase of
injury |
KSS** | KSF*** | No. of revisions |
|---|---|---|---|---|---|---|---|---|
| Jin9 | 2022 | Suture anchor | 43 | tibial attachment | final stage of surgery | NA* | 86_3 ± 8.1 | 0 |
| Liu21 | 2021 | Suture anchor | 14 | tibial attachment | final stage of surgery | 87.6 ± 2.7 | NA* | 1 |
| Li | 2021 | Suture anchor | 14 | 9 mid-substance 5 femoral attachment | NA* | 93.3±4.7 | NA* | NA* |
| Sum.16 | 2020 | Aaugmentation of medial meniscus transfer_ | 11 | tibial attachment | final stage of surgery | 95 ± 4.47 | 91.8± 7.5 | 0 |
| Rajkumar10 | 2020 | Screw and washer construct | 41 | femoral attachment | final stage of surgery | 80 to 90 | 80 to 95 | 0 |
| Motiffard23 | 2020 | Suture | 35 | mid-substance | trial reduction or in the final stages of surgery | 81 ± 17 | 61 ± 13 | 3 |
| Ni25 | 2020 | Screw and rectangular spiked washer | 14 | femoral attachment | final stage of surgery | NA* | NA* | 0 |
| White20 | 2019 | Staple | 33 | tibial attachment | NA* | NA* | NA* | 0 |
| Jin (a)24 | 2019 | Suture anchor | 36 | tibial attachment | final stage of surgery | 86.4 ± 7.2 | NA* | 0 |
| Jin(b)24 | 2019 | Staple | 29 | tibial attachment | final stage of surgery | 88.3 ± 7.5 | NA* | 0 |
| Choi8 | 2017 | Suture anchor | 40 | tibial attachment | final stage of surgery | 23.3 to 92.7 | 69.9± 8.4 | 3 |
| Wang26 | 2017 | MCL reconstruction without a constrained | 17 | 12 mid-substance, 5 femoral attachment | final stage of surgery | NA* | 84.7± 5.9 | 0 |
| Siqueira4 | 2016 | Unconstrained with repair | 10 | NA* | NA* | 79.2 ± 21.6 | 78.1 ± 22 | 0 |
| Siqueira4 | 2016 | Constrained with repair | 3 | NA* | NA* | 50 ± 36 | 51.7 ± 20.8 | 0 |
| Siqueira4 | 2016 | Constrained | 8 | NA* | NA* | 91.1 ± 10.5 | 59.3 ± 20.3 | 0 |
| Cao27 | 2016 | Semitendinosus and gracilis tendon | 11 | tibial attachment | final stage of surgery | 89.82 ± 3.76 | 89.54 ± 3.50 | 0 |
| Bohl13 | 2016 | Femur avulsion was repaired using suture with a screw-and-washer construct of the avulsions tibia avulsion, 4 with suture alone, 9 with suture anchors, and 7 with suture with a screw-and-washer construct A cruciate-retaining prosthesis was used in 35 total knee arthroplasties, and a posterior stabilized prosthesis was used in 10 |
45 | 24 mid-substance, 20 tibial attachment 1 femoral attachment |
final stage of surgery | NA* | NA* | 5 |
| Shahi15 | 2014 | Synthetic ligament | 11 | tibial attachment | final stage of surgery | 76to 100 | NA* | 0 |
| Dragosloveanu12 | 2013 | 7 suture anchor 3 constrained tibial |
10 | 7 mid-substance 3 tibial attachment | final stage of surgery | 87.71 | NA* | 1 |
| Stephens14 | 2012 | Primary repair | 9 | mid-substance | NA* | NA* | 73.3 | 0 |
| Lee3 | 2010 | Increased constraint | 37 | 28 mid-substance, 9 tibial attachment | final stage of surgery |
NA* | 83 | 3 |
| Leopold2 | 2001 | Primary repair | 14 | mid-substance | NA* | 93 | NA* | 0 |
*Not applicable, **Knee Society Score (KSS), ***Knee Functional Score (KFS)
Discussion
Injury to MCL during TKA is often unrecognized and rarely discussed. Due to its iatrogenic nature, prospective controlled studies were not found in the search. Based on the included studies site of injury and phase of detection could be possible influential factors for choosing the best repair techniques. Although sex, age, body mass index, and being a professional athlete may be influential factors, they were not mentioned in studies. Knee instability, accelerated wear, loosening, and revision surgery may result from unrecognized MCL injury.18,19
1) Primary Repair:
Mid-substance disruption of the MCL can be treated with primary repair and postoperative bracing.2
A.Staple or Suture Only
A study conducted by White et al.20 found that using staples to repair iatrogenic MCL injuries in tibial insertion had better functional outcomes and satisfaction compared to those who underwent revision TKA for instability and those who underwent TKA without MCl injury. However, 19.2% of patients with the staple repair were found to have instability.
B. Suture Anchor
For repairing iatrogenic injuries, Jin et al.9, Liu et al.21, Li et al.22 and Motififard et al.23 used suture anchors. The study conducted by Jin et al. involved an injury to the tibial attachment site, whereas Motififard's involved an injury to the mid-substance. As reported in the study by Jin et al., the results after two years of follow-up in the injury group were similar to those in the control group without iatrogenic injury of MCL.
In the study carried out by Motififard et al., however, results were not satisfactory, and 15% of the repairing group had instability. Choi et al. also reported an identical survival rate for the patient and control groups after 13 years.8
Nevertheless, in the research by Jin et al. (2019)24 which the suture anchor and staple groups were compared in MCL injury at tibial insertion, no difference was observed regarding the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Knee Society Score (KSS). Furthermore, no statistically significant difference in stability was found between the suture anchor and staple groups.
C) Screw and Washer
In studies by Ni et al.25 and Rajkumar et al.,10 it was demonstrated that femoral bony MCL avulsions during TKA could be repaired using screw and washer constructs. As a result, the excellent clinical and radiological outcomes achieved through this approach obviated the necessity for augmenting constraints. One or two K-wires were used to hold the avulsed fragment and attach the MCL in place. Depending on the fragment size, a cancellous screw with a washer of 3.5 mm was inserted when the knee was in 30 degrees of flexion.
2) Augmentation with Autograft
a. Autograft (Semitendinosus or Gracilis)
An augmentation with autograft of the semitendinosus tendon was used in the study by Wang et al.26 for primary double-bundle MCL reconstruction without constrained components. In 12 cases, the MCL injury was midsection, while in five cases, it was avulsed from the femur metaphysis. The authors demonstrated that TKA without a constrained implant produces excellent results when repairing MCL injuries. In the study by Cao et al.,27 which used both semitendinosus and gracilis tendon in MCL injuries at the joint level, the same result was shown. According to their latest follow-up, both groups had comparable KSS and functional scores.
b. Synthetic Grafts
The mid-substance MCL injuries in the study by Shahi et al.15 occurred due to direct injury from either an oscillating saw blade or sharp instruments used for medial subperiosteal lifting. The MCL was exposed during the procedure, and a synthetic ligament (NeoligamentsTM, Xiros Company, Leeds, UK) was utilized. This synthetic ligament is constructed with parallel longitudinal polyester fibers, forming an open mesh scaffold structure that facilitates tissue growth. To secure the synthetic ligament to the tibia, nonabsorbable sutures were employed to suture the graft onto the medial aspect, commencing proximally from the medial epicondyle. Additionally, the femoral and tibial attachments were sutured using deep interrupted sutures to the periosteum.
c. Meniscus Transfer
A medial meniscus transfer is another effective method. In the study by Sun,16 this method was used for the first time for iatrogenic MCL injury in tibial attachment, and it showed excellent results in clinical outcomes of the injury group and the KSS and knee functional score (KSF).
3) Changing Prosthesis Characteristics
a. Thicker Polyethylene
During the study by Koo,17 thicker polyethylene was inserted to achieve balance and stability in the mediolateral soft tissue at 0°, 30°, and 90° of knee flexion following the detection of the intraoperative MCL injury from the tibial attachment site. It was generally recommended to use a 2-mm to 4-mm thicker polyethylene insert compared to the initial one to stabilize the knee joint and allow some degree of lateral tightness. Standing anteroposterior radiography showed almost 4° more valgus in the tibiofemoral angle in the MCL-off knees than the MCL-intact side. However, there were no complaints of knee instability in daily activities.
b. Conversion to the Constrained Prosthesis
Conversion into constrained prostheses is the most popular strategy. As this method was used in a study performed by Lee,3 patients with increased constraint (TCIII; DePuy) had similar scores to those without ligament injuries during TKA. Among the MCL disruptions observed, 28 cases were characterized by transection of the ligament, while nine cases involved avulsion of the collateral ligament from the tibial metaphysis. Four patients were revised for instability among the seven who did not receive more constrained prostheses.
Otherwise, in a study conducted by Siqueira,4 treatment of the MCL injury was determined by the surgeon and consisted of using an unconstrained implant with (n=10) or without (n=2) primary ligament repair, a constrained implant with (n=3) or without (n=8) ligament repair. One patient had an avulsion from the tibial metaphysis, while the other 22 patients had mid-substance injuries. Baseline KSS varied among the four treatment groups, but postoperative KSS
scores showed no significant differences. Preoperative and postoperative KFS did not differ among the treatment groups. The difference between preoperative and postoperative KSS scores was significant, but not for KFS scores. When comparing preoperative KSS scores and the difference between pre-and postoperative KSS scores, pairwise comparisons between the groups revealed no statistically significant differences.
The mentioned techniques demonstrated various outcomes in different studies. These variations could be due to different patient demographics, surgeons, and follow-up methods. However, one of the main determinants was the site of injury. As mentioned, most of the studies evaluate MCL avulsion from tibial insertion. Primary repairs, staples, suture anchors, augmentation with autograft, and changing prosthesis characteristics were used for these patients. In contrast to tibial insertion injuries, fewer studies reported femoral insertion injuries, but the Screw and washer technique has shown a proper outcome for these patients. In addition, primary repair and augmentation with autografts are preferred in mid-substance injuries.
Conclusion
Suture anchors, staples, screws and washers, and more constrained prostheses were the most common techniques of iatrogenic MCL injury management reported in the literature. However, the decision over the optimal strategy to manage the MCL injury during TKA should be made considering the site of the MCL injury.
Acknowledgment
The authors would like to thank their colleague in department of orthopedic surgery for their assistance in data gathering.
Conflict of interest:
None
Funding:
None
References
- 1.Chang MJ, Lim H, Lee NR, Moon YW. Diagnosis, causes and treatments of instability following total knee arthroplasty. Knee Surg Relat Res. 2014;26(2):61–7. doi: 10.5792/ksrr.2014.26.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leopold SS, McStay C, Klafeta K, Jacobs JJ, Berger RA, Rosenberg AG. Primary repair of intraoperative disruption of the medical collateral ligament during total knee arthroplasty. J Bone Joint Surg Am. 2001;83(1):86–91. doi: 10.2106/00004623-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Lee GC, Lotke PA. Management of intraoperative medial collateral ligament injury during TKA. Clin Orthop Relat Res. 2011;469(1):64–8. doi: 10.1007/s11999-010-1502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siqueira MB, Haller K, Mulder A, Goldblum AS, Klika AK, Barsoum WK. Outcomes of Medial Collateral Ligament Injuries during Total Knee Arthroplasty. J Knee Surg. 2016;29(1):68–73. doi: 10.1055/s-0034-1394166. [DOI] [PubMed] [Google Scholar]
- 5.Le DH, Goodman SB, Maloney WJ, Huddleston JI. Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop Relat Res. 2014;472(7):2197–200. doi: 10.1007/s11999-014-3540-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jung KA, Lee SC, Hwang SH, Jung SH. Quadriceps tendon free graft augmentation for a midsubstance tear of the medial collateral ligament during total knee arthroplasty. Knee. 2009;16(6):479–83. doi: 10.1016/j.knee.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 7.Li J, Yan Z, Lv Y, et al. Impact of intraoperative medial collateral ligament injury on outcomes after total knee arthroplasty: a meta-analysis and systematic review. J Orthop Surg Res. 2021;16(1):686 . doi: 10.1186/s13018-021-02824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi YJ, Lee KW, Seo DK, Lee SK, Kim SB, Lee HI. Conservative Management after Intraoperative Over-Release of the Medial Collateral Ligament from its Tibial Insertion Site in Patients Undergoing Total Knee Arthroplasty. J Knee Surg. 2018;31(8):786–791. doi: 10.1055/s-0037-1608848. [DOI] [PubMed] [Google Scholar]
- 9.Jin C, Song EK, Jin QH, Seon JK, Sun SM. Clinical Outcomes of Repair of Complete Detachment of Medial Collateral Ligament at the Tibial Insertion in Bilateral Total Knee Arthroplasty. Evid Based Complement Alternat Med. 2022;2022:7266233. doi: 10.1155/2022/7266233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajkumar N, Soundarrajan D, Dhanasekararaja P, Rajasekaran S. Influence of Intraoperative Medial Collateral Ligament Bony Avulsion Injury on the Outcome of Primary Total Knee Arthroplasty. J Arthroplasty. 2021;36(4):1284–1294. doi: 10.1016/j.arth.2020.10.051. [DOI] [PubMed] [Google Scholar]
- 11.Debette C, Lustig S, Servien E, et al. Total knee arthroplasty of the stiff knee: three hundred and four cases. Int Orthop. 2014;38(2):285–9. doi: 10.1007/s00264-013-2252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dragosloveanu S, Cristea S, Stoica C, Dragosloveanu C. Outcome of iatrogenic collateral ligaments injuries during total knee arthroplasty. Eur J Orthop Surg Traumatol. 2014;24(8):1499–503. doi: 10.1007/s00590-013-1330-y. [DOI] [PubMed] [Google Scholar]
- 13.Bohl DD, Wetters NG, Del Gaizo DJ, Jacobs JJ, Rosenberg AG, Della Valle CJ. Repair of Intraoperative Injury to the Medial Collateral Ligament during Primary Total Knee Arthroplasty. J Bone Joint Surg Am. 2016;98(1):35–9. doi: 10.2106/JBJS.O.00721. [DOI] [PubMed] [Google Scholar]
- 14.Stephens S, Politi J, Backes J, Czaplicki T. Repair of medial collateral ligament injury during total knee arthoplasty. Orthopedics. 2012;35(2):e154–9. doi: 10.3928/01477447-20120123-01. [DOI] [PubMed] [Google Scholar]
- 15.Shahi A, Tan TL, Tarabichi S, Maher A, Della Valle C, Saleh UH. Primary Repair of Iatrogenic Medial Collateral Ligament Injury during TKA: A Modified Technique. J Arthroplasty. 2015;30(5):854–7. doi: 10.1016/j.arth.2014.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Sun C, Rong W, Du R, et al. Meniscus Graft Augmentation for a Midsubstance Tear of the Medial Collateral Ligament during Total Knee Arthroplasty. J Knee Surg. 2022;35(4):449–455. doi: 10.1055/s-0040-1715115. [DOI] [PubMed] [Google Scholar]
- 17.Koo MH, Choi CH. Conservative treatment for the intraoperative detachment of medial collateral ligament from the tibial attachment site during primary total knee arthroplasty. J Arthroplasty. 2009;24(8):1249–53. doi: 10.1016/j.arth.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Naudie DD, Rorabeck CH. Managing instability in total knee arthroplasty with constrained and linked implants. Instr Course Lect. 2004;53:207–15. [PubMed] [Google Scholar]
- 19.Lachiewicz PF, Soileau ES. Ten-year survival and clinical results of constrained components in primary total knee arthroplasty. J Arthroplasty. 2006;21(6):803–8. doi: 10.1016/j.arth.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 20.White KT, Fleischman A, Ackerman CT, Chen AF, Rothman RH. Managing Superficial Distal Medial Collateral Ligament Insufficiency in Primary Total Knee Arthroplasty Using Bone Staples. J Knee Surg. 2019;32(9):900–905. doi: 10.1055/s-0038-1669954. [DOI] [PubMed] [Google Scholar]
- 21.Liu K, Xu H, Wang Y, et al. Direct repair of medial collateral ligament injury combined with brace in total knee arthroplasty. Chin J Tissue Eng Res. 2021;25(15):2352–2357. [Google Scholar]
- 22.Li Z, Wang S, Wang A, et al. Treatment of iatrogenic injury to medial collateral ligament in total knee arthroplasty. Article. Chinese J Orthop Trauma. 2021;23(6):530–534. [Google Scholar]
- 23.Motififard M, Sheikhbahaei E, Piri Ardakani M, Cheraghsahar H, Shahzamani A. Intraoperative repair for iatrogenic MCL tear due to medial pie-crusting in TKA yields satisfactory mid-term outcomes. Knee Surg Sports Traumatol Arthrosc. 2021;29(10):3246–3253. doi: 10.1007/s00167-020-06126-x. [DOI] [PubMed] [Google Scholar]
- 24.Jin C, Zhao JY, Santoso A, et al. Primary repair for injury of medial collateral ligament during total-knee arthroplasty. Medicine (Baltimore). 2019;98(39):e17134. doi: 10.1097/MD.0000000000017134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ni M, Sun JY, Fu J, et al. Management of Medial Collateral Ligament Insufficiency during Total Knee Arthroplasty with a Screw and Rectangular Spiked Washer: A Case Series of 14 Patients. Orthop Surg. 2020;12(6):1784–1791. doi: 10.1111/os.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Liu H, Cao P, et al. Clinical outcomes of medial collateral ligament injury in total knee arthroplasty. Medicine (Baltimore). 2017;96(30):e7617. doi: 10.1097/MD.0000000000007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cao JG, Wang L, Zhao HW, Liu J. Semitendinosus and gracilis transfer for treatment of medial collateral ligament injury of total knee arthroplasty. Eur Rev Med Pharmacol Sci. 2016;20(18):3738–3742. [PubMed] [Google Scholar]