Abstract
Objectives:
To evaluate the utility and diagnostic performance of portable handheld ultrasound for evaluating fibular rotation at the distal tibiofibular articulation after syndesmotic disruption.
Methods:
Four above-the-knee cadaveric specimens were included. Syndesmotic disruption was precipitated by transecting the Anterior Inferior Tibiofibular Ligament, Interosseous Ligament, and Posterior Inferior Tibiofibular Ligament. Thereafter, a proximal fibular osteotomy was performed, and three conditions were modeled at the distal syndesmosis: 1) reduced, 2) 5 degree internal rotation malreduction, and 3) 5 degree external rotation malreduction. Two blinded observers performed separate ultrasonographic examinations for each condition at the level of both the anterior and posterior distal tibiofibular articular surfaces. Syndesmotic gap penetrance, defined as the ability of the P-US to generate signal between the distal fibula and tibia at the level of the incisura, was graded positive if the sonographic waves penetrated between the distal tibiofibular joint and negative if no penetrating waves were detected. The accuracy measures of the anterior and posterior gap penetrance were evaluated individually.
Results:
Our preliminary results showed that posterior gap penetrance showed good performance when detecting either internal or external rotational malreduction of the fibula with very good specificity (87.5%) and PPV (90.0%). On the other hand, the anterior gap penetrance showed limited performance when detecting either form of rotational malreduction.
Conclusion:
We introduced a novel sign, the “gap penetrance sign”, best measured from the posterior ankle, which can accurately detect syndesmotic malreduction using P-US in a manner that does not require specific quantitative measurements and is readily accessible to early P-US users.
Key Words: Ankle instability, Ankle malreduction, Syndesmotic instability, Tibiofibular joint, Trauma
Introduction
Ankle syndesmotic injuries affect almost 15 per 100,000 individuals in the general population and are more common among athletes.1 It is estimated that between 1% and 11% of all ankle sprains and 10% of all ankle fractures involve injury to the ankle syndesmosis.2,3 Among fractures that require surgical intervention, rates are much higher, with an estimated 39% of Weber B fractures displaying syndesmotic instability intraoperatively.4 Among the inherent challenges of operative treatment of such instability is achieving anatomic reduction of the distal tibiofibular joint.5 Current methods of assessment of the accuracy of reduction and detection of malreduction include direct inspection, arthroscopic visualization, radiographic and CT imaging, and range of motion testing.6 However, previous reports have shown that up to 52% of cases of syndesmosis instability treated surgically were malreduced on postoperative CT scans.7–10
In light of the shortcomings of current methods and techniques used to evaluate for syndesmotic malreduction intraoperatively, researchers have attempted to develop newer approaches. Tornetta et al. have described ‘the articular surface method’ that evaluates the relationship between the articular cartilage of the distal anteromedial fibula and the anterolateral plafond as superior to evaluation at the level of the incisura.11 They showed that this technique is highly accurate and reliable for assessing syndesmotic reduction in a cadaveric model but focused primarily on the sagittal plane. Rotational plane malreduction may be more challenging to determine intraoperatively. Therefore, considering the unreliability of current techniques for intraoperative detection of malreduction, it is important to explore the capacity of other modalities in order to mitigate the postoperative functional complications of malreduced syndesmoses and, therefore, improve functional outcomes – more specifically, in inconspicuous rotationally malreduced syndesmoses.12–14 Portable handheld ultrasound (P-US) is a low-cost, easily accessible, accurate, and radiation-free imaging tool that has previously been used to evaluate syndesmotic instability.15–19 Ultrasonic waves cannot penetrate bone; therefore, any penetrance at the distal tibiofibular articulation may signify malreduction at the distal tibiofibular joint, given the subtle incongruence of the articular surface. We aimed to assess the feasibility and accuracy of detecting syndesmotic rotational malreduction using portable ultrasound (P-US) in a cadaveric model. We hypothesize that penetration of the sonographic waves between the articular surfaces of the syndesmosis will allow us to detect rotational syndesmotic malreduction when using this diagnostic technique.
Materials and Methods
For the ultrasound examination, we utilized a P-US device (Fujifilm iViz air, Tokyo, Japan) to evaluate the distal tibiofibular joint from both the anterior and posterior aspects. The general framework of the methodology is presented [Figure 1].
Figure 1.
Flowchart illustrating the process of creating the syndesmosis models and evaluation by two blinded observers
GPS, Gap Penetrance Sign
Specimens
Two blinded observers separately performed the evaluation on four cadaveric specimens amputated above the knee and thawed for 24 hours prior to experimentation. The cadavers did not have any previous foot or ankle injuries. Institutional Review Board (IRB) approval for this study was obtained.
In order to create the cadaveric models of syndesmotic instability, each specimen underwent a high fibular osteotomy at the level of the fibular neck followed by the dissection of the posterior inferior tibiofibular ligament (PITFL), interosseous ligament (IOL), and anterior inferior tibiofibular ligament (AITFL) via a small posterolateral incision as performed in previous studies.20,21 Three different conditions were simulated for each specimen: 1) reduced, 2) 5 degrees external rotation malreduced, and 3) 5 degrees internal rotation malreduced in a random sequential fashion. Anatomic alignment at the fibular osteotomy site was used to confirm anatomic reduction or a 5 malrotation using a goniometer. In order to ensure that the syndesmosis was aligned in the sagittal plane and to control for other types of malreduction, an anterolateral incision was used to guide and ascertain whether the anteromedial fibular cartilage was aligned with the anterolateral plafond using the articular surface method by Tornetta III et al [Figure 2].11 Once achieved, the model simulation was stabilized proximally using a quadricortical K-wire from fibula to tibia.22 The anterior incision was then sutured to perform the ultrasound examination and prevent observer bias. A fellowship-trained foot and ankle surgeon created the syndesmosis models, and another independent observer recorded the results of the ultrasonographic evaluation.
Figure 2.
Anterior view of the cadaveric syndesmotic models via a longitudinal anterolateral incision. (a) External rotation malreduced syndesmotic model. (b) Reduced syndesmotic model
Imaging
To eliminate bias during ultrasonographic evaluation by the two blinded observers, the order of the models for each cadaver was randomized in each assessment. This randomization order was determined a priori via another independent researcher who dictated to the surgeon creating the simulation models the order by which each simulation for each cadaver was performed before the two blinded observers conducted their ultrasound examination. A water-soluble ultrasound coupling medium was applied, and the examiner adjusted the probe to achieve optimal visualization of the tibiofibular joint with the ankle held in dorsiflexion, ensuring that the probe was perpendicular to the joint line. For the anterior examination, the observer placed the probe plane along the extent of the AITFL [Figure 2]. For the posterior examination, the observer placed the probe along the extent of the PITFL [Figure 3a & 3b] and [Figure 3c & 3d].
Figure 3.

Demonstration of probe placement during GPS evaluation. (a, b) demonstrate the P-US probe placement while evaluating the anterior GPS. (c, d) demonstrate the P-US probe placement while evaluating the posterior GPS
Image analysis
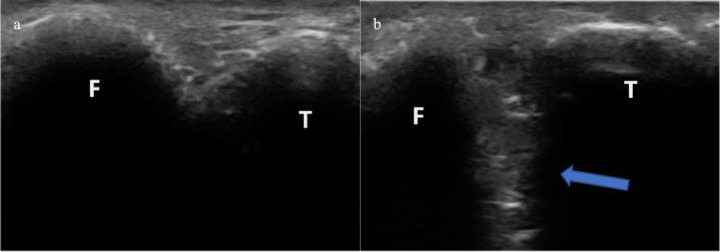
In a reduced syndesmosis, the distal articular surfaces of the tibia and fibula coapt, preventing any ultrasonographic waves from ‘penetrating’ in between. Prior to ligament transection and creation of the malreduced syndesmotic models, ultrasonographic examination was performed anteriorly and posteriorly and showed no sonographic penetrance between the articular surfaces in their native, uninjured forms [Figure 4a & 5a]. This occurs due to the inherent trait of acoustic impedance displayed by bones. The adjoined anatomic nature is altered in a malreduced syndesmosis, which allows sonographic waves to ‘penetrate’ between the malreduced articular surfaces and be readily detectable by the observer [Figure 4b & 5b]. We referred to this ultrasonographic phenomenon as the “Gap Penetrance Sign” (GPS), which was graded positive if sonographic waves penetrated between the distal articular surfaces of the tibia and fibula and negative if no penetrating sonographic waves were detected.
Figure 4.
The anterior examination of the GPS. (a) Reduced ‘native’ syndesmotic model showing no acoustic signal penetrance between the distal tibiofibular articulations. (b) The same ultrasonographic view of the distal tibiofibular articulation but in an externally rotated malreduced model. T, distal anterolateral Tibia. F, distal anteromedial Fibula
Figure 5.
The posterior examination of the GPS. (a) Reduced ‘native’ syndesmotic model showing no acoustic signal penetrance between the posterior distal tibiofibular articulations. (b) The same ultrasonographic view of the posterior distal tibiofibular articulation but in an internally rotated malreduced model. T, distal anterolateral Tibia. F, distal anteromedial Fibula
Statistical analysis
The performance of the ultrasonographic examination was assessed by means of accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).23 the diagnostic performance of the anterior and posterior GPS was evaluated individually for the detection of external rotation malreduction, internal rotation malreduction, or either.
Results
The overall measures of performance of the anterior GPS and posterior GPS are illustrated [Table 1]. The anterior GPS showed 75% sensitivity and 12.5% specificity when used alone to evaluate any type of rotational malreduction. The posterior GPS showed 56.3% sensitivity and 87.5% specificity, along with a PPV of 90% for the same evaluation. An analysis of the anterior GPS’s performance for evaluating either form of rotational malreduction did not yield significant performance. However, the posterior GPS showed excellent performance when used to evaluate either internal rotation malreduction (75% sensitivity, 87.5% specificity) or external rotation malreduction (87.5% sensitivity, 87.5% specificity).
Table 1.
Measures of accuracy of GPS signs during evaluation for syndesmotic rotational malreduction models compared to reduced ‘native’ models
| Approach | Syndesmotic malreduction | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|---|
| Anterior GPS only | ERM model | 87.5 | 12.5 | 50.0 | 50.0 | 50.0 |
| Anterior GPS only | IRM model | 62.5 | 12.5 | 41.6 | 25.0 | 33.3 |
| Posterior GPS only | ERM model | 87.5 | 87.5 | 87.5 | 87.5 | 87.5 |
| Posterior GPS only | IRM model | 75.0 | 87.5 | 87.5 | 77.5 | 81.3 |
| Anterior GPS only | either ERM or IRM model | 75.0 | 12.5 | 63.5 | 20.0 | 54.2 |
| Posterior GPS only | either ERM or IRM model | 56.30 | 87.50 | 90.0 | 50.0 | 66.7 |
ERM, external rotation malreduced
IRM, internal rotation malreduced
Discussion
Syndesmotic malreduction following surgical fixation can occur in the coronal, sagittal, and rotational planes. While its clinical implications may be less clear, rotational malreduction is difficult to detect, especially using conventional intra-operative techniques.24 More recent evidence shows that syndesmosis malreduction may better be visualized using 3-D imaging techniques, such as intra-operative CT, but such technology is not widely available, does not generally afford a contralateral comparison when used intraoperatively, and remains relatively cumbersome to use in practice.9,17,24–29
The advent of modern, P-US probes attached to tablet screens represents an advancement in the accessibility of imaging in multiple settings, including the operating room. Despite technological advancements, however, the widespread use of ultrasound is limited by its user dependence and learning curve. The advantage of using simpler, categorical evaluation methods such as the GPS that do not require any quantitative measurement or complex interpretation is that it makes ultrasound more accessible for the average practitioner while nonetheless empowering surgeons to make decisions intraoperatively. Our preliminary results show a promising ability to use P-US to diagnose rotational malreduction of the fibula at the syndesmosis in a manner that is readily adoptable by most practitioners while overcoming the limits of other methods that may primarily focus on the coronal or sagittal plane.
Refining P-US probe placement and positioning may improve the anterior GPS’s performance. The posterior GPS’s very good specificity for malreduction allows surgeons to rule in suspected malreduction easily and on the spot intra-operatively. Its excellent PPV, on the other hand, may prove to be a useful diagnostic tool for malreduction in real-time following surgical syndesmotic reduction or even post-operatively upon follow-up at the clinic. Considering its remarkably superior performance compared to that of the anterior GPS, the posterior GPS exhibits great potential for intra-operative use to detect syndesmotic malreduction and can be a valuable diagnostic tool at the point of care.
Open visualization of the distal tibiofibular articulation via an anterior incision, assessment of the relationship between the anterior distal fibula and anterior incisura through the lateral incision, or arthroscopic evaluation are currently considered among the most reliable methods of assessing syndesmotic reduction intraoperatively.11,30 However, these techniques are invasive and require expensive arthroscopic equipment and tools that may not be readily available intraoperatively everywhere and anytime. The posterior GPS may supplement any of these approaches when attempting to evaluate rotational reduction of the fibula without resorting to intraoperative CT. Moreover, P-US examination may be compared with the contralateral side to ascertain and confirm any assessment findings. However, since this is a cadaveric study using unmatched cadavers, we were unable to do so.
A notable limitation of our study was the small sample size and cadaveric design. However, with that in mind, the primary purpose of this technical tip is to introduce this diagnostic method and its technique, inspired by Tornetta et al.’s articular surface method’, to the literature for further substantiation with more robust sample sizes. A larger human sample size may better capture the sign’s true potential and reliability. It is also worth noting that P-US is observer-dependent, and its interpretation may vary with experience. Furthermore, we only investigated rotational malreduction. The impact of sagittal or coronal plane malreduction and its impact on the GPS still needs to be evaluated.
Conclusion
In conclusion, we have described a novel ultrasonographic technique, the GPS, for detecting syndesmotic rotational malreduction intra-operatively. Our preliminary results indicate that the posterior GPS is accurate, easy to perform, and has the potential to reduce the need for invasive visual inspection or intra-operative CT.
Acknowledgment
Not applicable
Conflict of interest:
None
Funding:
None
References
- 1.Porter DA. Evaluation and treatment of ankle syndesmosis injuries. Instr Course Lect. 2009;58:575–581. [PubMed] [Google Scholar]
- 2.Mulligan EP. Evaluation and management of ankle syndesmosis injuries. Phys Ther Sport off J Assoc Chart Physiother Sports Med. 2011;12(2):57–69. doi: 10.1016/j.ptsp.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 3.van Zuuren WJ, Schepers T, Beumer A, Sierevelt I, van Noort A, van den Bekerom MPJ. Acute syndesmotic instability in ankle fractures: A review. Foot Ankle Surg. 2017;23(3):135–141. doi: 10.1016/j.fas.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Stark E, Tornetta PI, Creevy WR. Syndesmotic Instability in Weber B Ankle Fractures: A Clinical Evaluation. J Orthop Trauma. 2007;21(9):643. doi: 10.1097/BOT.0b013e318157a63a. [DOI] [PubMed] [Google Scholar]
- 5.Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014;5:173–182. doi: 10.2147/OAJSM.S41564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gardner MJ, Graves ML, Higgins TF, Nork SE. Technical Considerations in the Treatment of Syndesmotic Injuries Associated With Ankle Fractures. J Am Acad Orthop Surg. 2015;23(8):510 . doi: 10.5435/JAAOS-D-14-00233. [DOI] [PubMed] [Google Scholar]
- 7.Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the Tibiofibular Syndesmosis in Ankle Fractures. Foot Ankle Int. 2006;27(10):788–792. doi: 10.1177/107110070602701005. [DOI] [PubMed] [Google Scholar]
- 8.Loizou CL, Sudlow A, Collins R, Loveday D, Loveday D, Smith G. Radiological assessment of ankle syndesmotic reduction. The Foot. 2017;32:39–43. doi: 10.1016/j.foot.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Franke J, von Recum J, Suda AJ, Grützner PA, Wendl K. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am. 2012;94(15):1386–1390. doi: 10.2106/JBJS.K.01122. [DOI] [PubMed] [Google Scholar]
- 10.Schwarz N, Köfer E. Postoperative Computed Tomography–Based Control of Syndesmotic Screws. Eur J Trauma. 2005;31(3):266–270. [Google Scholar]
- 11.Tornetta P, Tornetta P rd, Yakavonis M, Veltre DR, Veltre DR, Shah AR. Reducing the Syndesmosis Under Direct Vision: Where Should I Look? J Orthop Trauma. 2019;33(9):450–454. doi: 10.1097/BOT.0000000000001552. [DOI] [PubMed] [Google Scholar]
- 12.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19(2):102–108. doi: 10.1097/00005131-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Sagi HC, Shah AR, Sanders RW. The Functional Consequence of Syndesmotic Joint Malreduction at a Minimum 2-Year Follow-Up. J Orthop Trauma. 2012;26(7):439–443. doi: 10.1097/BOT.0b013e31822a526a. [DOI] [PubMed] [Google Scholar]
- 14.van den Heuvel SB, Dingemans SA, Gardenbroek TJ, Schepers T. Assessing Quality of Syndesmotic Reduction in Surgically Treated Acute Syndesmotic Injuries: A Systematic Review. J Foot Ankle Surg. 2019;58(1):144–150. doi: 10.1053/j.jfas.2018.08.038. [DOI] [PubMed] [Google Scholar]
- 15.Roberts CS, Beck DJJ, Heinsen J, Seligson D. Review Article Diagnostic Ultrasonography: Applications in Orthopaedic Surgery. Clin Orthop Relat Res. 2002;(401):248–64. doi: 10.1097/00003086-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 16.Apard T. Ultrasonography for the orthopaedic surgeon. Orthop Traumatol Surg Res. 2019;105(1):S7–S14. doi: 10.1016/j.otsr.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 17.Ghandour S, Ashkani-Esfahani S, Kwon JY. The Emerging Role of Automation, Measurement Standardization, and Artificial Intelligence in Foot and Ankle Imaging: An Update. Foot Ankle Clin. 2023;28(3):667–680. doi: 10.1016/j.fcl.2023.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Hagemeijer NC, Lubberts B, Saengsin J, et al. Portable dynamic ultrasonography is a useful tool for the evaluation of suspected syndesmotic instability: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2023;31(5):1986–1993. doi: 10.1007/s00167-022-07058-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jirawat S, Noortje H, Rohan B, et al. Using Portable Ultrasound to Measure the Effect of Lateral Ankle Ligament Injury on Syndesmotic Stability: A Cadaveric Study. Foot Ankle Orthop. 2020;5:4. [Google Scholar]
- 20.Westermann RW, Rungprai C, Goetz JE, Femino J, Amendola A, Phisitkul P. The Effect of Suture-Button Fixation on Simulated Syndesmotic Malreduction: A Cadaveric Study. JBJS. 2014;96(20):1732. doi: 10.2106/JBJS.N.00198. [DOI] [PubMed] [Google Scholar]
- 21.Krähenbühl N, Bailey TL, Weinberg MW, et al. Impact of torque on assessment of syndesmotic injuries using weightbearing computed tomography scans. Foot Ankle Int. 2019;40(6):710–719. doi: 10.1177/1071100719829720. [DOI] [PubMed] [Google Scholar]
- 22.Schepers T, Dingemans SA, Rammelt S. Recent developments in the treatment of acute syndesmotic injuries. Fuß Sprunggelenk. 2016;14(2):66–78. [Google Scholar]
- 23.Trevethan R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front Public Health. 2017;5:307. doi: 10.3389/fpubh.2017.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of Standard Fluoroscopy in Detecting Rotational Malreduction of the Syndesmosis in an Ankle Fracture Model. Foot Ankle Int. 2011;32(6):616–622. doi: 10.3113/FAI.2011.0616. [DOI] [PubMed] [Google Scholar]
- 25.Vasarhelyi A, Lubitz J, Gierer P, et al. Detection of Fibular Torsional Deformities after Surgery for Ankle Fractures with a Novel CT Method. Foot Ankle Int. 2006;27(12):1115–1121. doi: 10.1177/107110070602701219. [DOI] [PubMed] [Google Scholar]
- 26.Dikos GD, Heisler J, Choplin RH, Weber TG. Normal Tibiofibular Relationships at the Syndesmosis on Axial CT Imaging. J Orthop Trauma. 2012;26(7):433–438. doi: 10.1097/BOT.0b013e3182535f30. [DOI] [PubMed] [Google Scholar]
- 27.Knops S, Kohn MA, Kohn M, Hansen EN, Matityahu A, Marmor M. Rotational malreduction of the syndesmosis: reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. 2013;34(10):1403–10. doi: 10.1177/1071100713489286. [DOI] [PubMed] [Google Scholar]
- 28.Nault ML, Hébert-Davies J, Laflamme GY, Leduc S. CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma. 2013;27(11):638–641. doi: 10.1097/BOT.0b013e318284785a. [DOI] [PubMed] [Google Scholar]
- 29.Yildirim H, Mavi A, Büyükbebeci O, Gümüşlburun E. Evaluation of the Fibular Incisura of the Tibia with Magnetic Resonance Imaging. Foot Ankle Int. 2003;24(5):387–391. doi: 10.1177/107110070302400502. [DOI] [PubMed] [Google Scholar]
- 30.Sanders D, Schneider P, Taylor M, Tieszer C, Lawendy AR. Improved Reduction of the Tibiofibular Syndesmosis With TightRope Compared With Screw Fixation: Results of a Randomized Controlled Study. J Orthop Trauma. 2019;33(11):531–537. doi: 10.1097/BOT.0000000000001559. [DOI] [PubMed] [Google Scholar]