Abstract
The current study examined racial and ethnic differences in psychological, behavioral, and metabolic risk factors for cardiovascular disease (CVD) and CVD conditions among family caregivers (FCGs) of persons with dementia. We used the 2015–2020 Behavioral Risk Factor Surveillance System data. The sample included a total of 6,132 FCGs of persons with dementia. Compared to non-Hispanic White FCGs, non-Hispanic Black and non-Hispanic Asian FCGs were less likely to have depression. The Other racial/ethnic FCG group were more likely to currently smoke. Non-Hispanic Black FCGs were less likely to have exercised, more likely to be obese, and more likely to have been diagnosed with diabetes. No differences in CVD conditions (angina/coronary heart disease, stroke, myocardial infarction) were detected between racial/ethnic minority FCGs and non-Hispanic White FCGs. Future studies should investigate relationships between racial/ethnic minority-specific caregiving and CVD by including a larger, racially and ethnically diverse population of FCGs.
Introduction
More than 16 million family caregivers (FCGs) in the United States provide care for persons living with Alzheimer’s disease and related dementias (Alzheimer’s Association, 2022). Alzheimer’s disease is the most common type of dementia, with an estimated 5.8 million people in the U.S., including 5.6 million aged 65 and older (Alzheimer’s Association, 2019; CDC, 2019). Alzheimer’s disease is characterized by an irreversible, progressive decline in cognitive and functional abilities. Associated symptoms include disorientation, mood and behavior changes, and memory loss (National Institute on Aging, 2021). Due to the health care demands, FCGs of persons living with dementia experience higher caregiving burden than FCGs of persons with other chronic diseases (Chen et al., 2020; Xu et al., 2021).
Racially and ethnically diverse FCGs face more challenges in providing care to their family members as well as managing their own health (Cohen et al., 2019; Rote & Moon, 2018). When compared to non-Hispanic White counterparts, racial/ethnic minority FCGs reported worse health status and negative physical health (Rote et al., 2019). The latter are also less likely to use professional support services such as the use of paid services (e.g., in-home or community-based respite care) (Rote et al., 2019). Cohen and colleagues (2019) reported that non-Hispanic Black FCGs are more likely to manage multiple tasks while fulfilling caregiving duties and experience more financial burdens than non-Hispanic White FCGs. Hispanic and non-Hispanic Asian FCGs are more likely to have depression than non-Hispanic White FCGs (Haley et al., 2004).
Recent studies have reported that FCGs have a higher risk of developing cardiovascular disease (CVD) than non-caregivers (Xu et al., 2020). Stressors and distress related to caregiving have been linked to key mechanisms of developing atherothrombotic diseases (von Känel et al., 2012), and changes in physiological and emotional responses can impact CVD outcomes (Xu et al., 2020). Mausbach and colleagues (2007) reported that FCGs’ depression is a significant predictor of incident CVD diagnoses. Caregiving stress is significantly associated with more alcohol use (Gottschalk et al., 2020; Rospenda et al., 2010), and caregiver burden is associated with increased odds of smoking (Gottschalk et al., 2020). Moreover, studies reported that physical inactivity is significantly associated with providing care (Gottschalk et al., 2020; von Känel et al., 2012), with higher caregiving intensity increasing the odds of being overweight and obese (Gottschalk et al., 2020; Lakka & Bouchard, 2005).
The CVD risk associated with caregiving varies by race (Capistrant et al., 2012); however, racial and ethnic disparities in cardiovascular health among FCGs are understudied and poorly understood (Capistrant et al., 2012; Xu et al., 2020). In order to develop culturally appropriate CVD prevention strategies, it is important to identify how CVD risk factors and CVD conditions in FCGs of persons with dementia differ by race/ethnicity. In this study, we evaluated racial/ethnic differences in psychological, behavioral, and metabolic risk factors for CVD and CVD conditions among FCGs of persons with dementia in the U.S. using the national Behavioral Risk Factor Surveillance System database (CDC, 2022a). We hypothesized that racial/ethnic minority FCGs of persons living with dementia will have a higher psychological, behavioral, and metabolic risk for CVD and CVD conditions than non-Hispanic White FCGs.
Methods
This is a secondary analysis of data from the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System (BRFSS). The purpose was to assess racial and ethnic differences in psychological (depression), behavioral (tobacco use, binge drinking, physical activity), and metabolic (body mass index, diabetes) risk factors and CVD conditions (angina/coronary heart disease, stroke, myocardial infarction) among FCGs of persons living with dementia (CDC, 2022a).
Data sources
The BRFSS is a nationally representative landline and cell phone survey initiated in 1984 to assess the health of adults over the age of 18 in the U.S. (CDC, 2022a). The BRFSS is the largest continuously conducted health-related survey using random digit dialing techniques. It collects data on demographic characteristics, health-related behaviors, chronic health conditions, caregivers, health care access, and the use of preventive health services from more than 400,000 individuals every year. We used the 2015–2020 BRFSS data to (a) include indicators related to caregivers, risk factors for CVD, and CVD conditions and (b) maximize the sample size of non-White FCGs of persons living with dementia to increase power to detect differences across race/ethnicity groups. The median response rate for the 2015–2020 BRFSS survey was 47.6% (CDC, 2022a).
Measures
Demographic characteristics
Age in years, sex (male, female), race/ethnicity (non-Hispanic White, Hispanic, non-Hispanic Black or African American, non-Hispanic Asian, Other [American Indian and Alaska Native, Native Hawaiian and Pacific Islander, or Multi-racial]), highest education, income, participants’ self-rated general health (excellent, very good, good, fair, poor), caregiver relationship to persons with dementia, and caregiving duration and intensity were assessed.
Psychological risk factor
Depression was included to assess psychological risk for CVD. Participants were asked the question, “Has a doctor, nurse, or other health professional ever told you have a depressive disorder (including depression, major depression, dysthymia, or minor depression)?” (yes/no).
Behavioral risk factors
Smoking, binge drinking, and physical activity were included to assess behavioral risk. Participants were asked whether they have smoked at least 100 cigarettes in their entire life (yes/no), and whether they currently smoke cigarettes (yes/no). Participants were asked how many days per week or per month they had at least one drink of any alcoholic beverage and how many times during the past 30 days they had five or more drinks for men or four or more drinks for women on an occasion. Binge drinkers were calculated and defined in the BRFSS data codebook as males having five or more drinks and females having four or more drinks on one occasion and modeled as a binary variable (yes/no). For physical activity, respondents were asked whether they participated in physical activities or exercised in the past 30 days (yes/no).
Metabolic risk factors
Overweight was defined as a body mass index (BMI) of 25.0 to < 30.0 kg/m2, and obesity, a BMI of ≥ 30.0 kg/m2. The overweight and obesity variables were assessed based on self-reported height and weight and dichotomized based on the CDC guidelines (CDC, 2022b). For diabetes, participants were asked if they had ever been told that they had diabetes (yes/no).
CVD conditions
In the BRFSS surveys, participants were asked whether a doctor, nurse, or other health professional had ever told them that they had any of the following CVD conditions: angina/coronary heart disease, stroke, or myocardial infarction (yes/no).
Statistical analysis
All analysis were conducted in SAS Version 9.4. Descriptive statistics were calculated for the demographic characteristics, CVD risk factors, and CVD conditions grouped by race/ethnicity and all combined. Frequencies and/or percentages were used as the variables were all categorical. Chi-square tests were used for pairwise comparisons between each racial/ethnic minority FCG group and the non-Hispanic White group across the demographic characteristics. Logistic regression models were used to estimate unadjusted (OR) and adjusted odds ratios (AOR) with 95% confidence intervals (CI) for the association of race/ethnicity with psychological, behavioral, and metabolic risk factors for CVD, and CVD conditions. The non-Hispanic White group was the reference group for all racial/ethnic minority FCG group odds ratios. All models were adjusted with the following covariates: age group, sex, education, income, self-rated health status, relationship to persons with dementia, and caregiver duration and intensity. CVD risk factors were not included as covariates in models for specific CVD conditions, as an examination of these relationships was not an aim of this study. A two-sided p < 0.05 was considered statistically significant. Figures displaying the odds ratio and 95% confidence interval for each racial/ethnic minority group relative to the non-Hispanic White group were created for each of the outcomes related to the psychological, behavioral, and metabolic risk factors and CVD conditions.
Results
The analytic sample included a total of 6,132 FCGs of persons living with dementia (Table 1). FCGs (36%) were ≥ 65 years old, 49% female, and 77% non-Hispanic White. Many (41%) were college graduates, and 34% rated their health as good. FCGs provided care to persons with dementia from 2–5 years (29%) and 46% provided care up to 8 hours per week.
Table 1.
Demographic Characteristics by Race and Ethnicity
| n(%) | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| All Race/Ethnicity (N = 6,132) | Non-Hispanic White (N= 4,665) | Hispanic (N=326) | Non-Hispanic Black (N=534) | Non-Hispanic Asian (N=199) | Other* (N=318) | |
| Demographic Characteristics | ||||||
|
| ||||||
| Age a, b, d | ||||||
| 18 to 24 | 161 (2.7) | 96 (2.1) | 23 (7.1) | 19 (3.6) | 6 (3.0) | 17 (5.3) |
| 25 to 34 | 281 (4.6) | 187 (4.0) | 29 (8.9) | 26 (4.9) | 9 (4.5) | 30 (9.4) |
| 35 to 44 | 422 (7.0) | 283 (6.1) | 48 (14.7) | 48 (9.0) | 14 (7.0) | 29 (9.2) |
| 45 to 54 | 980 (16.2) | 719 (15.4) | 65 (19.9) | 106 (19.9) | 33 (16.6) | 57 (17.9) |
| 55 to 64 | 1,950 (32.2) | 1,532 (32.8) | 85 (26.1) | 181 (33.9) | 62 (31.2) | 90 (28.3) |
| ≥ 65 | 2,196 (36.3) | 1,808 (38.8) | 73 (22.4) | 151 (28.3) | 72 (36.2) | 92 (28.9) |
| Missing | 52 (1.0) | 40 (0.9) | 3 (0.9) | 3 (0.6) | 3 (1.5) | 3 (0.9) |
|
| ||||||
| Sex a, b | ||||||
| Male | 1,491(24.8) | 1,194 (25.6) | 63 (19.3) | 103 (19.3) | 46 (23.1) | 85 (26.7) |
| Female | 2,958 (48.8) | 2,227 (47.8) | 183 (56.1) | 315 (59.0) | 95 (47.7) | 138 (43.4) |
| Missing | 1,593 (26.5) | 1,244 (26.7) | 80 (24.5) | 116 (21.7) | 58 (29.1) | 95 (29.9) |
|
| ||||||
| Highest Education a, b, c, d | ||||||
| Never attended school | 3 (0.1) | 2 (0.1) | 1 (0.3) | 0 (0) | 0 (0) | 0 (0) |
| Elementary school | 75 (1.2) | 46 (1.0) | 19 (5.8) | 5 (0.9) | 2 (1.0) | 3 (0.9) |
| Some high school | 192 (3.2) | 130 (2.8) | 15 (4.6) | 29 (5.4) | 1 (0.5) | 17 (5.3) |
| High school graduate | 1,471 (24.4) | 1,122 (24.1) | 78 (23.9) | 150 (28.1) | 30 (15.1) | 91 (28.6) |
| Some college | 1,812 (30.1) | 1,363 (29.2) | 99 (30.4) | 182 (34.1) | 57 (28.6) | 111 (34.9) |
| College graduate | 2,481 (40.9) | 1,998 (42.8) | 113 (34.7) | 167 (31.3) | 108 (54.3) | 95 (29.9) |
| Missing | 8 (0.2) | 4 (0.1) | 1 (0.3) | 1 (0.2) | 1 (0.5) | 1 (0.3) |
|
| ||||||
| Income a, b, d | ||||||
| Less than $25,000 | 1,013 (19.6) | 811 (16.7) | 119 (36.5) | 166 (31.1) | 28 (14.1) | 94 (29.6) |
| $25,000 – $49,999 | 1,350 (22.4) | 1019 (21.8) | 68 (20.9) | 147 (27.5) | 38 (19.1) | 78 (24.5) |
| $50,000 – $74,999 | 933 (15.4) | 735 (15.8) | 51 (15.6) | 65 (12.2) | 34 (17.1) | 48 (15.1) |
| $75,000 or more | 1,752 (28.9) | 1,451 (31.1) | 55 (16.9) | 94 (17.6) | 84 (42.2) | 68 (21.4) |
| Missing | 819 (13.8) | 679 (14.6) | 33 (10.1) | 62 (13.0) | 15 (7.5) | 30 (9.4) |
|
| ||||||
| Self-rated Health Status a, b, c, d | ||||||
| Excellent | 888 (14.9) | 707 (15.2) | 43 (13.2) | 60 (11.2) | 24 (12.1) | 54 (17.0) |
| Very good | 1,984 (32.9) | 1,655 (35.5) | 68 (20.9) | 121 (22.7) | 61 (30.7) | 79 (24.8) |
| Good | 2.050 (33.9) | 1,496 (32.1) | 126 (38.7) | 237 (44.4) | 87 (43.7) | 104 (32.7) |
| Fair | 847 (14.0) | 607 (13.0) | 67 (20.6) | 90 (16.9) | 22 (11.1) | 61 (19.2) |
| Poor | 266 (4.4) | 194 (4.2) | 21 (6.4) | 26 (4.9) | 5 (2.5) | 20 (6.3) |
| Missing | 7 (0.1) | 6 (0.1) | 1 (0.3) | 0 (0) | 0 (0) | 0 (0) |
|
| ||||||
| Relationship to Persons with Dementia a, b, c, d | ||||||
| Spouse | 947 (15.4) | 817 (17.5) | 35 (10.7) | 42 (7.9) | 17 (8.5) | 36 (11.3) |
| Child | 3,159 (51.5) | 2,441 (52.3) | 175 (53.7) | 271 (50.7) | 115 (57.8) | 157 (49.4) |
| Parent | 96 (1.6) | 77 (1.7) | 6 (1.8) | 8 (1.5) | 0 (0) | 5 (1.6) |
| Other | 1,122 (18.3) | 760 (16.3) | 80 (24.5) | 149 (27.9) | 49 (24.6) | 84 (26.4) |
| Missing | 808 (13.1) | 570 (12.2) | 30 (9.2) | 64 (12.0) | 18 (9.0) | 36 (11.3) |
|
| ||||||
| Caregiving Duration a, b | ||||||
| < 6 months | 1,120 (18.6) | 812 (17.4) | 77 (23.6) | 122 (22.8) | 39 (19.6) | 70 (22.0) |
| 6 months to less than 2 years | 1,404 (23.2) | 1,114 (23.9) | 63 (19.3) | 100 (18.7) | 54 (27.1) | 73 (23.0) |
| 2 years to less than 5 years | 1,775 (29.4) | 1,419 (30.4) | 79 (24.2) | 142 (26.6) | 56 (28.1) | 79 (24.8) |
| ≥ 5 years | 1,681 (27.7) | 1,274 (27.3) | 103 (31.6) | 164 (30.7) | 48 (24.1) | 92 (28.9) |
| Missing | 152 (1.1) | 46 (1.0) | 4, (1.2) | 6 (1.1) | 2 (1.0) | 4 (1.3) |
|
| ||||||
| Caregiving Intensity a, b, d | ||||||
| Up to 8 hours/week | 2,769 (45.8) | 2,231 (47.8) | 111 (34.0) | 214 (40.1) | 93 (46.7) | 120 (37.7) |
| 9 to 19 hours/week | 864 (14.2) | 646 (13.8) | 53 (16.3) | 79 (14.8) | 29 (14.6) | 57 (17.9) |
| 20 to 39 hours/week | 694 (11.5) | 519 (11.1) | 43 (13.2) | 67 (12.5) | 22 (11.1) | 43 (13.5) |
| 40 hours or more | 1,413 (23.5) | 1,026 (22.0) | 109 (33.4) | 150 (28.1) | 46 (23.1) | 82 (25.8) |
| Missing | 302 (5.0) | 243 (5.2) | 10 (3.1) | 24 (4.5) | 9 (4.5) | 16 (5.0) |
The “Other” race/ethnicity includes the following race/ethnicities: American Indian and Alaska Native, Native Hawaiian and Pacific Islander, or Multi-racial.
Statistical significance p < 0.05
Statistically significant difference between non-Hispanic White FCGs and Hispanic FCGs
Statistically significant difference between non-Hispanic White FCGs and non-Hispanic Black FCGs
Statistically significant difference between non-Hispanic White FCGs and non-Hispanic Asian FCGs
Statistically significant difference between non-Hispanic White FCGs and other race/ethnicity FCGs
Table 1 also shows demographic characteristics of FCGs of persons with dementia by racial/ethnic groups. The significant associations indicate that there is a difference in the distribution of the demographic variable between the non-Hispanic White FCGs and the specific minority FCG to which it is being compared. The sample consisted of 4,665 non-Hispanic White FCGs (77%), 326 Hispanic FCGs (5%), 534 non-Hispanic Black FCGs (9%), 199 non-Hispanic Asian (3%), and 318 Other racial/ethnic FCGs (5%). Hispanic, Black, and Other racial/ethnic FCGs were younger, had lower incomes, and were more likely to have lower educational attainment than non-Hispanic White FCGs. Hispanic and non-Hispanic Black FCGs had a slightly lower percentage of males and slightly higher percentage of females compared to non-Hispanic White FCGs. Non-Hispanic Asian FCGs were more likely to have higher education compared to non-Hispanic White FCGs. Overall, all racial/ethnic minority FCG groups were more likely to have a lower health status (self-rated) compared to non-Hispanic White counterparts. Hispanic and non-Hispanic Black FCGs were more likely to provide care to their loved one for a shorter duration of time. Hispanic, non-Hispanic Black, and Other racial/ethnic groups are more likely to have higher caregiving intensity per week compared to non-Hispanic White counterparts (Table 1).
Table 2 shows CVD risk factors and conditions across all FCGs. 23% of the FCGs experienced depression. When looking at the behavioral risk factors, 44% had smoked at least 100 cigarettes in their life, 34% currently smoke, 10% binge drink, and 76% exercise. For the metabolic risk factors, 36% of the FCGs were overweight, 32% were obese, and 16% had diabetes. Lastly, for the CVD conditions, 6% of the FCGs experienced angina/coronary heart disease, 5% experienced stroke, and 6% experienced myocardial infarction (Table 2).
Table 2.
Descriptive Statistics on CVD Risk Factors and CVD Conditions
| n (%) | |
|---|---|
| Psychological Risk Factor | |
| Depression | |
| Yes | 1,413 (23.1) |
|
| |
| Behavioral Risk Factors | |
| Smoked in Life | |
| Yes | 2,676 (43.8) |
| Currently Smoke | |
| Yes | 911 (34.1) |
| Binge Drinking | |
| Yes | 577 (9.5) |
| Exercise | |
| Yes | 4,675 (76.3) |
|
| |
| Metabolic Risk Factors | |
| Overweight | |
| Yes | 2,081 (35.8) |
| Obese | |
| Yes | 1,872 (32.2) |
| Diabetes | |
| Yes | 965 (15.8) |
|
| |
| CVD Conditions | |
| Angina/Coronary Heart Disease | |
| Yes | 392 (6.4) |
| Stroke | |
| Yes | 291 (4.8) |
| Myocardial Infarction | |
| Yes | 373 (6.1) |
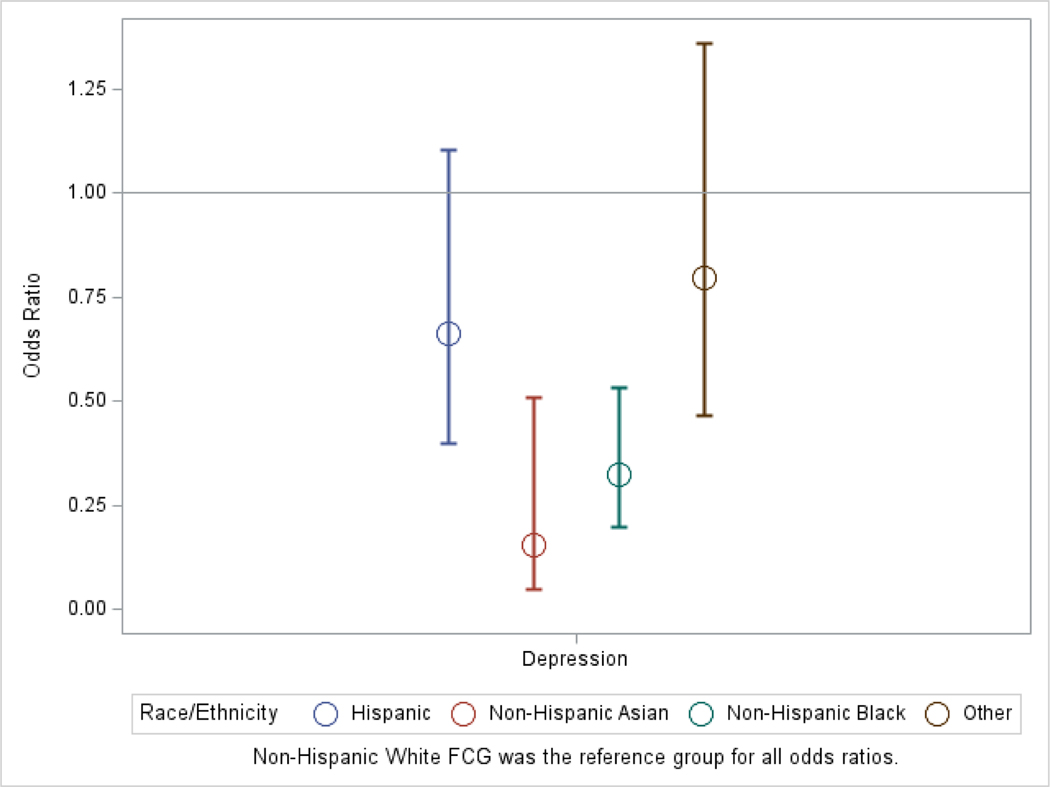
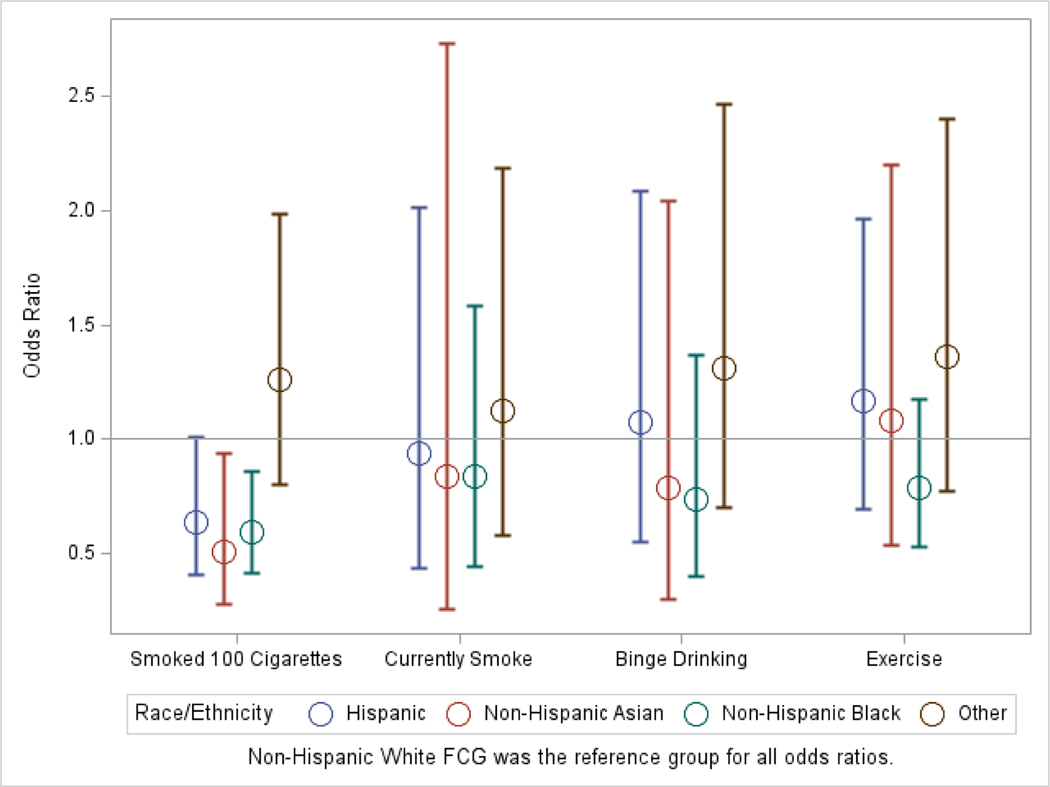
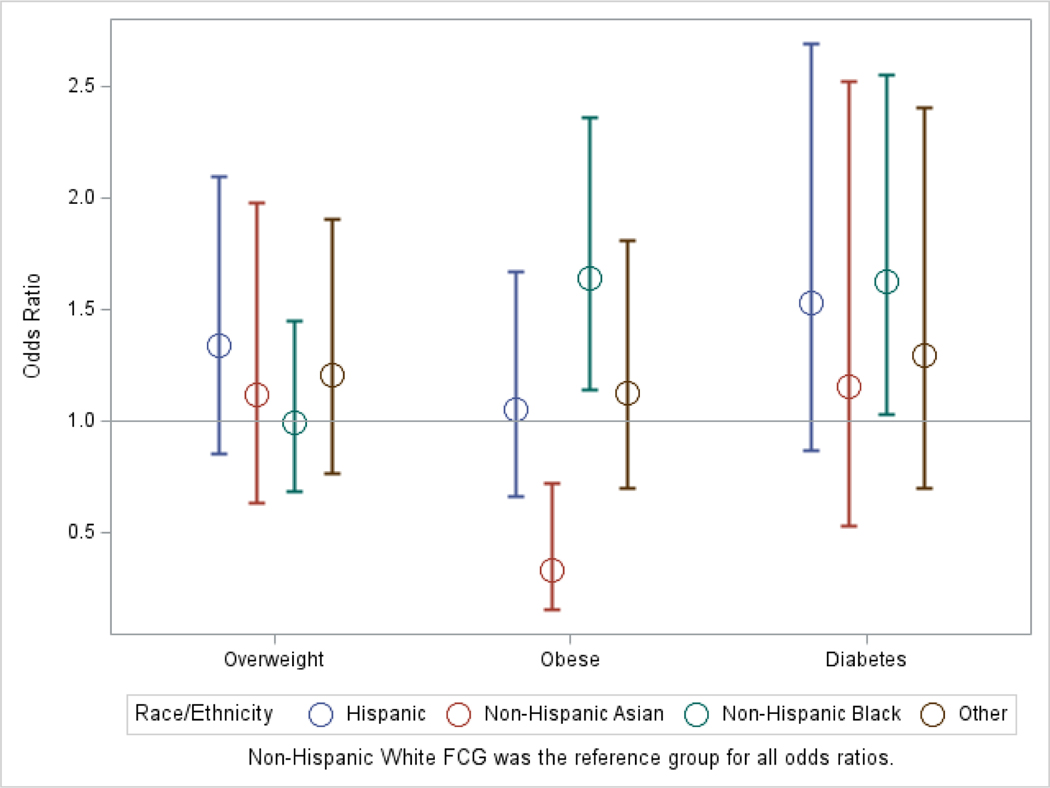
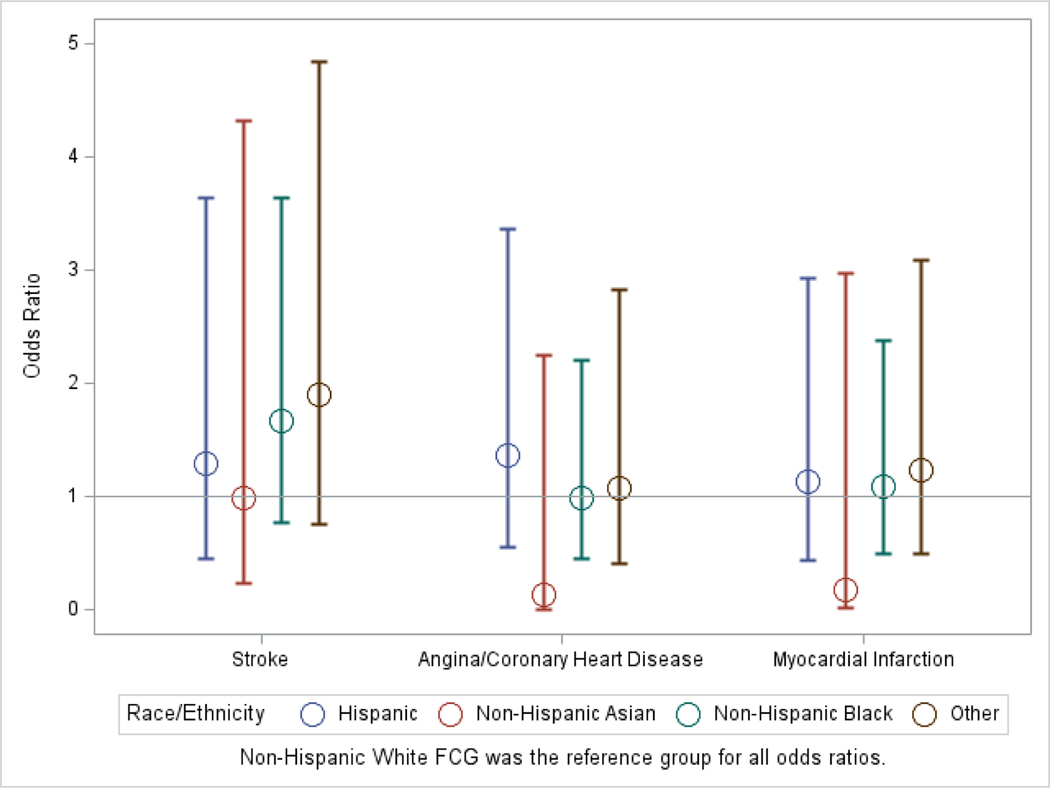
Differences in psychological, behavioral, and metabolic risk factors and CVD conditions, for racial/ethnic minority FCGs compared to non-Hispanic White FCGs are presented in Table 3 and Figures A, B, C, and D (available in the online version of this article). Compared to non-Hispanic White FCGs, non-Hispanic Black (AOR 0.33, 95% CI 0.2–0.53) and non-Hispanic Asian FCGs (AOR 0.16, 95% CI 0.05–0.51) were less likely to have depression. Hispanic (OR 0.69, 95% CI 0.5–0.95), non-Hispanic Black (AOR 0.6, 95% CI 0.41–0.86), and non-Hispanic Asian FCGs (AOR 0.51, 95% CI 0.28–0.94) were less likely to have smoked in their life. The Other racial/ethnic FCGs (OR 1.81, 95% CI 1.16–2.83) were more likely to currently smoke compared to non-Hispanic White counterparts. Non-Hispanic Black FCGs (OR 0.69, 95% CI 0.52 −0.91) were less likely to have exercised in the past 30 days. While non-Hispanic Black FCGs (AOR 1.64, 95% CI 1.14–2.36) were more likely to be obese. Non-Hispanic Black FCGs (AOR 1.77, 95% CI 1.27–2.47) were more likely to have been diagnosed with diabetes compared to non-Hispanic White counterparts. No differences in two risk factors (binge drinking, overweight) and CVD conditions (angina/coronary heart disease, stroke, myocardial infarction) were found between racial/ethnic minority FCGs and non-Hispanic White FCGs.
Table 3.
Differences in psychological, behavioral, and metabolic risk factors and CVD conditions between racial and ethnic FCG minorities and non-Hispanic White FCGs
| Hispanic (n =
326) Reference: Non-Hispanic White |
Non-Hispanic Black (n =
534) Reference: Non-Hispanic White |
Non-Hispanic Asian (n =
199) Reference: Non-Hispanic White |
Other (n =
318) Reference: Non-Hispanic White |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| OR (95% CI) |
AOR (95% CI) |
OR (95% CI) |
AOR (95% CI) |
OR (95% CI) |
AOR (95% CI) |
OR (95% CI) |
AOR (95% CI) |
|
| Psychological Risk Factor | ||||||||
| Depression | 1.06 (0.74, 1.53) |
0.66 (0.4, 1.1) |
0.54
(0.38, 0.76) |
0.33
(0.2, 0.53) |
0.31
(0.16, 0.61) |
0.16
(0.05, 0.51) |
1.15 (0.81, 1.64) |
0.8 (0.47, 1.36) |
|
| ||||||||
| Behavioral Risk Factors | ||||||||
| Smoked in Life |
0.69
(0.5, 0.95) |
0.64 (0.4, 1.01) |
0.76
(0.59, 0.98) |
0.6
(0.41, 0.86) |
0.43
(0.28, 0.68) |
0.51
(0.28, 0.94) |
1.3 (0.94, 1.78) |
1.26 (0.8, 1.99) |
| Currently Smoke | 1.19 (0.69, 2.03) |
0.94 (0.44, 2.01) |
1.41 (0.94, 2.12) |
0.84 (0.44, 1.58) |
1.1 (0.49, 2.45) |
0.83 (0.25, 2.73) |
1.81
(1.16, 2.83) |
1.13 (0.58, 2.18) |
| Binge Drinking | 1.2 (0.72, 1.97) |
1.07 (0.55, 2.09) |
0.85 (0.54, 1.34) |
0.74 (0.4, 1.37) |
0.61 (0.27, 1.39) |
0.78 (0.3, 2.04) |
1.42 (0.88, 2.28) |
1.31 (0.7, 2.46) |
| Exercise | 0.8 (0.56, 1.14) |
1.16 (0.69, 1.96) |
0.69
(0.52, 0.91) |
0.79 (0.53, 1.17) |
1.06 (0.66, 1.71) |
1.08 (0.53, 2.2) |
0.87 (0.6, 1.25) |
1.36 (0.77, 2.4) |
|
| ||||||||
| Metabolic Risk Factors | ||||||||
| Overweight | 1.09 (0.79, 1.51) |
1.34 (0.85, 2.1) |
0.82 (0.63, 1.08) |
1 (0.69, 1.45) |
0.95 (0.63, 1.46) |
1.12 (0.63, 1.98) |
1.01 (0.72, 1.41) |
1.21 (0.77, 1.91) |
| Obese | 1.3 (0.94, 1.81) |
1.05 (0.66, 1.67) |
2.06
(1.59, 2.67) |
1.64
(1.14, 2.36) |
0.46
(0.27, 0.78) |
0.34
(0.16, 0.73) |
1.34 (0.96, 1.87) |
1.13 (0.7, 1.81) |
| Diabetes | 1.60 (1.20, 2.11) |
1.62 (0.31, 1.14) |
1.80
(1.45, 2.24) |
1.77
(1.27, 2.47) |
1.32 (0.91, 1.92) |
1.06 (0.58, 1.91) |
1.31 (0.97, 1.77) |
1.14 (0.71, 1.85) |
|
| ||||||||
| CVD Conditions | ||||||||
| Angina/Coronary Heart Disease | 1.07 (0.58, 1.97) |
1.37 (0.56, 3.36) |
0.84 (0.49, 1.43) |
0.99 (0.45, 2.21) |
0.29 (0.07, 1.15) |
0.14 (0.01, 2.25) |
0.95 (0.49, 1.81) |
1.07 (0.41, 2.83) |
| Stroke | 0.95 (0.44, 2.06) |
1.29 (0.46, 3.63) |
1.45 (0.86, 2.44) |
1.68 (0.77, 3.64) |
0.77 (0.27, 2.25) |
0.99 (0.23, 4.32) |
1.66 (0.89, 3.1) |
1.91 (0.75, 4.85) |
| Myocardial Infarction | 0.81 (0.4, 1.63) |
1.13 (0.44, 2.93) |
0.87 (0.51, 1.5) |
1.09 (0.5, 2.38) |
0.22 (0.05, 1.11) |
0.18 (0.01, 2.97) |
1.04 (0.55, 1.97) |
1.24 (0.5, 3.09) |
Bolded estimates are statistically significant.
Figure A.
Psychological Risk factor among Family Caregivers by Race/Ethnicity
Figure B.
Behavioral Risk factors among Family Caregivers by Race/Ethnicity
Figure C.
Metabolic Risk Factors among Family Caregivers by Race/Ethnicity
Figure D.
Cardiovascular Disease Conditions among Family Caregivers by Race/Ethnicity
Discussion
Using a nationally representative sample of the US adults who care for persons living with dementia, we examined racial and ethnic differences in psychological, behavioral, and metabolic risk factors for CVD and CVD conditions. While CVD risk factors such as depression, smoking, physical inactivity, obesity, and diabetes differed by race and ethnicity in FCGs of persons with dementia, CVD conditions did not. Managing FCGs’ health and wellness is important to prevent FCGs from becoming care recipients themselves. It is helpful for FCGs to identify and resolve health issues of persons with dementia to provide the best possible care. Given that this study analyzed cardiovascular health of FCGs of older adults with dementia by race and ethnicity using the national data, the findings from this study will help inform gerontological nurses and allow researchers to begin to identify CVD risk factors for FCGs in persons living with dementia. Nurses can then develop and implement culturally appropriate preventive care strategies of CVD in the family caregiver population.
Both non-Hispanic Black and non-Hispanic Asian FCGs had less depression compared to non-Hispanic White counterparts. This finding is supported by the 2015 caregiving report in the U.S. that non-Hispanic White FCGs (42%) are more likely to report emotional stress than Hispanic FCGs (32%), non-Hispanic Black FCGs (31%), and non-Hispanic Asian FCGs (34%) (National Alliance for Caregiving & AARP Public Policy Institute, 2015). Moreover, previous research supports the finding of this study in that non-Hispanic Black FCGs experienced less depression and garnered greater rewards from caregiving than non-Hispanic White counterparts (Cuellar, 2002; Haley et al., 2004). Similarly, other studies described that Hispanic and non-Hispanic Black FCGs had lower levels of depression and higher levels of caregiving satisfaction compared to non-Hispanic White FCGs (Rote et al., 2019; Roth et al., 2015), which has been attributed to family-centered cultural values with emphasis on family ties and support (Rote et al., 2019). On the other hand, there have been reports that Asian American FCGs were more depressed than non-Hispanic White counterparts. This higher rate of depression has been attributed to: lower utilization of formal support services due to cultural and language barriers; discrepancy between cultural healthcare needs and available services; and shortage of healthcare providers from the same cultural background (Heo & Koeske 2013; Pinquart & Sörensen, 2005; Whitney et al., 2023).
Racial/ethnic minority FCG groups were more vulnerable in socioeconomic status and health status than non-Hispanic White counterparts. Hispanic, non-Hispanic Black, and Other racial/ethnic FCG groups had lower incomes and educational attainment and were more likely to have higher caregiving intensity per week. These findings are supported by previous studies (National Alliance for Caregiving, 2009; Cohen et al., 2019; Rote & Moon, 2018). Moreover, we found that all racial/ethnic minority groups in this current study reported lower levels of health status than non-Hispanic White FCGs. This is supported by previous studies where racial/ethnic minority FCGs were more likely to have worse self-rated health and negative physical health (Pinquart & Sörensen, 2005; Rote et al., 2019). Caregiving duration and intensity, FCG-care recipient relationship type and quality, formal and informal support, demographic characteristics such as education and insurance type might be significant predictors influencing FCGs’ self-rated health (Rote et al., 2019). Possible factors in understanding FCGs’ self-rated health may differ by their race and ethnicity. This current study showed a significant relationship between racial/ethnic groups and several variables (socioeconomic variables- age, sex, education, income; relationship to persons with dementia; caregiving duration and caregiving intensity). These factors should be considered when examining the relationship between FCGs’ self-rated health and race/ethnicity. Thus, future studies are needed to test and quantify the effects of socioeconomic variables on the relationships between FCGs’ self-rated health status and race/ethnicity. Being aware of possible clinical issues can guide gerontological researchers to design more culturally and linguistically appropriate interventions to enhance health and wellness.
All racial/ethnic minority FCG groups, with the exception of Other racial/ethnic FCGs, were less likely to have smoked in their life, and Other racial/ethnic FCGs were more likely to currently smoke cigarettes than non-Hispanic White FCGs. This finding is supported by the 2020 CDC statistics about current cigarette smoking among U.S. adults, which reported that American Indian/Alaska Native, non-Hispanic adults were the racial/ethnic group having the highest smoking rates (27.1%) (CDC, 2022c). On the other hand, Salgado-García and colleagues (2015) described that Hispanic or non-Hispanic Black FCGs of persons with dementia were more likely to currently smoke than non-Hispanic White counterparts (Salgado-García et al., 2015). Given that caring for a family member living with dementia can be stressful and challenging (Chen et al., 2020; Xu et al., 2021), FCGs’ smoking behaviors have been attributed to caregiving stress and burden (Gottschalk et al., 2020; Salgado-García et al., 2015). Caregiving stress and burden might be worsened by high levels of caregiving intensity and duration which differ by race and ethnicity (Cohen et al., 2019; Rote & Moon, 2018). Future studies on how caregiving intensity and duration affect CVD risk factors, and how the relationships differ by race and ethnicity should be investigated.
While our findings found that race and ethnicity have a relationship to CVD risk factors, there were no statistically significant differences in CVD conditions (i.e., coronary heart disease, stroke, and myocardial infarction). However, by looking at the magnitude of the odds ratios and interpreting their confidence intervals, we can rule out large effects in one direction but not in the other. For instance, the odds of stroke for the non-Hispanic Black FCGs were 68% greater than in the non-Hispanic White FCGs (OR=1.68). The lower bound to the 95% confidence interval of 0.77 means that we can rule out the odds of stroke for the non-Hispanic Black group being more than 23% below the odds of stroke in the non-Hispanic White group in the population. However, the upper bound to the confidence interval of 3.64 suggests that it is possible that the odds of stroke in the non-Hispanic Black FCGs could be up to 264% greater than in the non-Hispanic White FCGs in the population. Thus, we can rule out large effects in direction but not the other. Something similar can be said when comparing the Other group to the non-Hispanic White group, as the odds of stroke for the Other group in the population could be anywhere from 25% less to 385% greater than the odds of stroke in the non-Hispanic White group. Using different variables than this study, Haley and colleagues (2010) reported that spouse caregivers’ race was not found to be significantly associated with coronary heart disease (CHD) risk scores that predict 10-year risk of onset of CHD using relevant variables (i.e., age, total cholesterol, HDL cholesterol, systolic blood pressure, diabetes, and current cigarette smoking) (Haley et al., 2010). On the other hand, they found that non-Hispanic Black caregivers had a higher stroke risk than non-Hispanic White caregivers (Haley et al., 2010). The measure of stroke risk in this study included relevant variables such as age, systolic blood pressure, antihypertensive medication, current cigarette smoking, diabetes, history of cardiovascular disease, atrial fibrillation, and left ventricular hypertrophy. There has been limited evidence on the relationships between race/ethnicity and CVD onset/conditions among a racially and ethnically diverse FCG population (Xu et al., 2020); thus, further studies should be warranted. Future work should examine what racial/ethnic FCG groups are more vulnerable to CVD conditions and develop racially and ethnically specific, preventive cardiovascular healthcare by tailoring FCGs’ needs and requirements.
Limitations
This study has several limitations. First, the BRFSS uses a cross-sectional study design; thus, it limits the ability to deduce causal relationships between variables included in this study. Second, the BRFSS data are based on participants’ self-report; thus, there is a possibility of recall bias. Moreover, the number of racial/ethnic minority FCGs included in this study, especially non-Hispanic Asian, were much smaller than non-Hispanic White FCGs; thus, the findings from this study should be interpreted with caution. Third, we measured caregiving intensity as the number of hours of care provided per week, which is a rough estimate of caregiving intensity because FCGs are likely to provide types of care requiring varying amounts of energy expenditure. Moreover, survey questions in the BRFSS might have limitations on obtaining accurate responses; thus, the findings must be interpreted cautiously. For example, in the question about physical activity, participants were asked whether they participated in physical activities or exercised in the past 30 days (yes/no). Both respondents who exercised once and respondents who worked out daily in the past 30 days might have answered “Yes”. Regarding the depression survey question, FCGs who had a depression diagnosis may not have been reported due to its stigma. Stigma may particularly be acute in certain racial and ethnic groups. That is, FCGs who had depression in some racial and ethnic groups might report the diagnosis less frequently if there is stigma related to depression. Finally, we were unable to analyze all relevant CVD risk factors (e.g., anxiety, sleep disturbance, hypertension, high cholesterol, diet) because they were not included across BRFSS datasets used in this study. Future studies should comprehensively investigate FCGs’ racial and ethnic differences in CVD by including established CVD risk factors such as diet, hypertension, and high cholesterol.
Conclusion
This study adds to the growing body of research that investigates racial and ethnic disparities in cardiovascular health among FCGs of persons living with dementia. Our study was limited by the available data because some variables related to CVD risk factors were not available across the BRFSS annual data. Nevertheless, we found that there were statistically significant racial and ethnic differences in CVD risk factors by analyzing specific psychological, behavioral, and metabolic factors. Future studies should examine racial/ethnic minority-specific caregiving conditions and CVD by including a larger, racially and ethnically diverse population of FCGs.
Acknowledgements.
We would like to thank Suzanne C. Lareau who is a senior instructor and professional editor in the Office of Research & Scholarship at the University of Colorado College of Nursing and provided constructive edits and comments on the manuscript.
Funding.
This work was supported by the National Institute on Aging of the National Institutes of Health [grant number K23AG073471] and the Intramural funding from the University of Colorado College of Nursing.
Contributor Information
Dawon Baik, University of Colorado College of Nursing, 13120 E. 19th Ave. Aurora, CO 80045, USA.
Sophia Centi, University of Colorado College of Nursing, 13120 E. 19th Ave. Aurora, CO 80045, USA.
Bryan McNair, Department of Biostatistics and Informatics, Colorado School of Public Health, University of Colorado Anschutz Medical Campus.
References
- Alzheimer’s Association. (2019). 2019 Alzheimer’s disease facts and figures. Retrieved December 5 from https://www.alz.org/media/Documents/alzheimers-facts-and-figures-2019-r.pdf
- Alzheimer’s Association. (2022). Alzheimer’s Disease Facts and Figures. Retrieved December 1 from https://www.alz.org/alzheimers-dementia/facts-figures
- Capistrant BD, Moon JR, Berkman LF, & Glymour MM (2012). Current and long-term spousal caregiving and onset of cardiovascular disease. J Epidemiol Community Health, 66(10), 951–956. 10.1136/jech-2011-200040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2019). Minorities and Women Are at Greater Risk for Alzheimer’s Disease. Retrieved December 3 from https://www.cdc.gov/aging/publications/features/Alz-Greater-Risk.html
- CDC. (2022a). Behavioral risk factor surveillance system. Retrieved September 5 from https://www.cdc.gov/brfss/annual_data/annual_data.htm
- CDC. (2022b). Defining adult overweight and obesity. Retrieved September 3 from https://www.cdc.gov/obesity/adult/defining.html
- CDC. (2022c). Burden of Cigarette Use in the U.S. Retrieved November 20 from https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html
- Chen C, Thunell J, & Zissimopoulos J (2020). Changes in physical and mental health of Black, Hispanic, and White caregivers and non-caregivers associated with onset of spousal dementia. Alzheimers Dement (N Y), 6(1), e12082. 10.1002/trc2.12082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen SA, Sabik NJ, Cook SK, Azzoli AB, & Mendez-Luck CA (2019). Differences within Differences: Gender Inequalities in Caregiving Intensity Vary by Race and Ethnicity in Informal Caregivers. J Cross Cult Gerontol, 34(3), 245–263. 10.1007/s10823-019-09381-9 [DOI] [PubMed] [Google Scholar]
- Cuellar NG (2002). A comparison of African American & Caucasian American female caregivers of rural, post-stroke, bedbound older adults. J Gerontol Nurs, 28(1), 36–45. 10.3928/0098-9134-20020101-08 [DOI] [PubMed] [Google Scholar]
- Gottschalk S, König HH, & Brettschneider C (2020). The association between informal caregiving and behavioral risk factors: a cross-sectional study. Int J Public Health, 65(6), 911–921. 10.1007/s00038-020-01402-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley WE, Gitlin LN, Wisniewski SR, Mahoney DF, Coon DW, Winter L, Corcoran M, Schinfeld S, & Ory M (2004). Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: findings from the REACH study. Aging Ment Health, 8(4), 316–329. 10.1080/13607860410001728998 [DOI] [PubMed] [Google Scholar]
- Haley WE, Roth DL, Howard G, & Safford MM (2010). Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers: differential effects by race and sex. Stroke, 41(2), 331–336. 10.1161/strokeaha.109.568279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heo GJ, & Koeske G (2013). The role of religious coping and race in Alzheimer’s disease caregiving. Journal of applied gerontology: the official journal of the Southern Gerontological Society, 32(5), 582–604. 10.1177/0733464811433484 [DOI] [PubMed] [Google Scholar]
- Lakka TA, & Bouchard C (2005). Physical activity, obesity and cardiovascular diseases. Handb Exp Pharmacol(170), 137–163. 10.1007/3-540-27661-0_4 [DOI] [PubMed]
- Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, & Schulz R (2007). Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychol, 26(5), 539–544. 10.1037/0278-6133.26.5.539 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016). Families caring for an aging America. National Academies Press. 10.17226/23606 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving. (2009). Caregiving in the US: A focused look at the ethnicity of those caring for someone age 50 or older executive summary. Retrieved November 19 from http://assets.aarp.org/rgcenter/il/caregiving_09_es50ethnic.pdf
- National Alliance for Caregiving & AARP Public Policy Institute. (2015). Caregiving in the U.S. Retrieved November 10 from https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf
- National Institute on Aging. (2021). Alzheimer’s disease fact sheet. Retrieved December 2 from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Pinquart M, & Sörensen S (2005). Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist, 45(1), 90–106. 10.1093/geront/45.1.90 [DOI] [PubMed] [Google Scholar]
- Rospenda KM, Minich LM, Milner LA, & Richman JA (2010). Caregiver burden and alcohol use in a community sample. J Addict Dis, 29(3), 314–324. 10.1080/10550887.2010.489450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rote SM, Angel JL, Moon H, & Markides K (2019). Caregiving Across Diverse Populations: New Evidence From the National Study of Caregiving and Hispanic EPESE. Innov Aging, 3(2), igz033. 10.1093/geroni/igz033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rote SM, & Moon H (2018). Racial/Ethnic Differences in Caregiving Frequency: Does Immigrant Status Matter? J Gerontol B Psychol Sci Soc Sci, 73(6), 1088–1098. 10.1093/geronb/gbw106 [DOI] [PubMed] [Google Scholar]
- Roth DL, Dilworth-Anderson P, Huang J, Gross AL, & Gitlin LN (2015). Positive Aspects of Family Caregiving for Dementia: Differential Item Functioning by Race. J Gerontol B Psychol Sci Soc Sci, 70(6), 813–819. 10.1093/geronb/gbv034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado-García FI, Zuber JK, Graney MJ, Nichols LO, Martindale-Adams JL, & Andrasik F (2015). Smoking and Smoking Increase in Caregivers of Alzheimer’s Patients. Gerontologist, 55(5), 780–792. 10.1093/geront/gnt149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Känel R, Mills PJ, Mausbach BT, Dimsdale JE, Patterson TL, Ziegler MG, Ancoli-Israel S, Allison M, Chattillion EA, & Grant I (2012). Effect of Alzheimer caregiving on circulating levels of C-reactive protein and other biomarkers relevant to cardiovascular disease risk: a longitudinal study. Gerontology, 58(4), 354–365. 10.1159/000334219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitney RL, Bell JF, Kilaberia TR, Link BM, Choula RB, Reinhard SC, & Young HM (2023). Diverse demands and resources among racially/ethnically diverse caregivers. Ethnicity & health, 1–20. 10.1080/13557858.2023.2179022 [DOI] [PubMed]
- Xu L, Lee Y, Kim BJ, & Chen L (2021). Determinants of Discretionary and Non-Discretionary Service Utilization among Caregivers of People with Dementia: Focusing on the Race/Ethnic Differences. Home Health Care Serv Q, 40(1), 75–92. 10.1080/01621424.2020.1805083 [DOI] [PubMed] [Google Scholar]
- Xu XY, Kwan RYC, & Leung AYM (2020). Factors associated with the risk of cardiovascular disease in family caregivers of people with dementia: a systematic review. J Int Med Res, 48(1), 300060519845472. 10.1177/0300060519845472 [DOI] [PMC free article] [PubMed] [Google Scholar]