Abstract
Background
The present study aims to investigate the prognostic role of systematic inflammatory and nutritional indexes in extensive-stage small-cell lung cancer (ES-SCLC) treated with first-line chemotherapy and atezolizumab.
Materials and methods
Prospective cohort population involving 53 patients were identified from NCT03041311 trial. The following peripheral blood-derived inflammatory and nutritional indexes, including neutrophil–lymphocyte ratio (NLR), platelet lymphocyte ratio (PLR), lymphocyte–monocyte ratio (LMR), systemic immune-inflammation index (SII), systemic inflammation response index (SIRI), prognostic nutrition index (PNI), advanced lung cancer inflammation index (ALI), and lung immune prognostic index (LIPI) were evaluated.
Results
The optimal cut-off values of the ALI, LMR, NLR, PLR, PNI, SII and SIRI were 323.23, 2.73, 2.57, 119.23, 48, 533.28 and 2.32, respectively. With a median follow-up of 17.1 months, the 1-year OS and PFS were 56% and 8%, respectively. Multivariate analysis showed that PLR was the only independent prognostic factors for OS among ES-SCLC patients treated with chemotherapy and atezolizumab (HR 4.63, 95%CI: 1.00–21.46, p = 0.05). K-M analysis showed that the OS and PFS for patients with high PLR (> 119.23) were significantly poorer than these with low PLR (≤ 119.23) (p = 0.0004 for OS and p = 0.014 for PFS). In external validation set, prognosis of patients with high PLR was also significantly poorer than these with low PLR in terms of OS (p = 0.038) and PFS (p = 0.028).
Conclusion
Pre-treatment PLR could serve as a valuable independent prognostic factor for ES-SCLC who receive chemotherapy and immune checkpoint inhibitors. Further, prospective studies are still needed to confirm our findings.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00262-021-02926-3.
Keywords: Small-cell lung cancer, Platelet lymphocyte ratio, Atezolizumab, Prognosis
Introduction
Lung cancer is the most commonly diagnosed cancer worldwide and the leading cause of cancer-related deaths, with 2.1 million new lung cancer cases and 1.8 million deaths predicted in 2018 [1]. Among them, small-cell lung cancer (SCLC) represents 15% of all lung cases. In general, SCLC is a highly aggressive and fatal disease, which is characterized by rapid tumor growth and early distant metastasis [2, 3]. Prior to the era of immunotherapy, limited improvements have been achieved in the treatment of SCLC, and the standard first-line treatment for extensive-stage(ES)-SCLC remains platinum-based doublet chemotherapy [4, 5]. In addition, early detection of SCLC is very challenging due to lack of specific symptoms. Therefore, approximately 70% of cases present with ES- SCLC at diagnosis [6]. The prognosis of ES-SCLC is very poor, with 5-year survival of 1–2% [7]. Therefore, novel treatment strategy for ES-SCLC is urgently needed.
As we all known, SCLC is characterized by multiple genetic alterations, reflecting its genomic instability [8]. Therefore, SCLC could be an candidate for immunotherapy by triggering an adaptive immune response that is capable of detecting and eradicating tumor cells. Indeed, several clinical trials have been performed to investigate the efficacy and toxicity of combining chemotherapy with immunotherapies, including anti-CTLA4, anti-PD-1 or anti-PD-L1, for the treatment of ES-SCLC [9–11]. Excepting for anti-CTLA4, adding immune checkpoint inhibitors (ICIs) to standard first-line chemotherapy provided a better survival benefit for newly diagnosed ES-SCLC. A more recent meta-analysis also showed that chemotherapy plus nivolumab, atezolizumab or durvalumab had significantly improved patient outcomes in terms of OS (hazard ratio HR, 0.67; 95% CI: 0.46–0.98 for nivolumab, HR, 0.70, 95%CI: 0.54–0.91 for atezolizumab, HR0.73; 95%CI: 0.59–0.90 for durvalumab), but not for pembrolizumab or ipilimumab [12]. Based on these findings, ICIs [13] have been approved by the US FDA as first-line and third-line settings for patients with extensive-stage or relapsed small-cell lung cancer (SCLC), respectively.
Generally, although most of ES-SCLC could benefit from ICIs, a number of patients may not respond to ICIs therapy and exhibit a shorter lifetime with ICIs treatment or suffer major life-threatening immunotoxicities [14]. In addition, the American Joint Committee on cancer tumor-node-metastasis (TNM) classification and staging system is a significant prognostic factor for SCLC patients, but it could not further stratify the same TNM stage SCLC patients with a high risk of recurrence. Therefore, it is crucial to identify effective prognostic factors to predict prognosis and to precisely stratify ES-SCLC who might benefit from chemo-immunotherapy. Systemic inflammation plays an important role in tumor promotion and progression. Therefore, it is not surprising that different markers of systemic inflammation have been related to poor outcome in multiple solid neoplasms, including SCLC. Recently, a variety of novel parameters have emerged as independent prognostic factors with an interesting role in clinical practice such as advanced lung cancer inflammation index (ALI) [15, 16], neutrophil–lymphocyte ratio (NLR) [17–19], platelet lymphocyte ratio (PLR) [17], lymphocyte–monocyte ratio (LMR) [20], systemic immune-inflammation index (SII) [21, 22], systemic inflammation response index (SIRI) [23–25], prognostic nutrition index (PNI) [26, 27], and lung immune prognostic index (LIPI) [28–30]. However, the prognosis of these inflammatory and nutritional indexes in ES-SCLC treated with chemotherapy and immunotherapy remains undetermined. As a result, we perform the present study to investigate prognostic role of systematic inflammatory and nutritional indexes in extensive-stage small-cell lung cancer (ES-SCLC) treated with first-line chemotherapy and atezolizumab.
Materials and methods
About PDS and study cohorts
Individual patient-level data were obtained from project data sphere, which was an independent, not-for-profit data-sharing platform (https://www.projectdatasphere.org/). In the present study, we used the raw individual data from one phase II randomized trial evaluating efficacy and toxicities of platinum plus etoposide chemotherapy and atezolizumab with or without trilaciclib for ES-SCLC patients (NCT03041311). The primary results of the trial were analyzed and published [31]. Patients were ineligible for inclusion if they presented with symptomatic brain metastases or had received prior systemic therapy for limited-stage or ES-SCLC. (The detailed inclusion and exclusion criteria had been presented in supplemental 1) Finally, a total of 53 patients with ES-SCLC in the controlled group treated with platinum plus etoposide chemotherapy and atezolizumab were included for analysis. In addition, a total of 31 ES-SCLC patients treated with chemotherapy and immunotherapy were used as a externally validated cohort in the present study.
Data collection
The available data of the phase II trial contain data about age at diagnosis, baseline ECOG performance status, sex, race, baseline neutrophil, lymphocytes, monocytes, platelets and leukocytes, baseline lactate dehydrogenase(LDH), albumin (g/L), baseline weight and height and smoking history. Moreover, data about progression-free survival (PFS) status and overall survival (OS) status were recorded. Based on the inclusion criteria for clinical trials, all included patients in the present study should have adequate organ function and acceptable performance status.
Definition of inflammatory markers
All hematological examinations were tested before chemotherapy and atezolizumab. Inflammatory markers were defined as follows: NLR = (the ratio of neutrophil count to lymphocyte count); LMR = (the ratio of lymphocyte count to monocyte count); PLR = (the ratio of platelet count to lymphocyte count); The PNI was the sum of albumin value (g/L) and 5 times lymphocyte count (109/L)[32]; SII = (platelet count) × NLR; SIRI = neutrophils × monocytes/lymphocytes[33]; ALI, advanced lung cancer inflammation index = BMI × (Albumin/NLR), BMI is the weight(kg)/height(m)2, and NLR is the ratio of neutrophil count to lymphocyte count [33]. The LIPI composite scores were calculated based on the dNLR (absolute neutrophil count/[white blood cell count—absolute neutrophil count]) and the baseline LDH level according to Mezquita et al. report[28]. The ALI,PLR, LMR, PLR, PNI,SII and SIRI cut-offs were utilized to select the optimal cut-off value using the receiver operating characteristic curve (ROC).
Statistical consideration
The baseline characteristics of included patients were simply described by using frequencies and percentages. Univariate and multivariate Cox-regression analyses were performed to investigate predictors for overall survival and progression-free survival. Factors significantly associated with risk of OS and PFS in the univariate analysis (p < 0.055) were then included for analysis in the multivariate Cox-regression analysis. OS and PFS were assessed according to PLR through Kaplan–Meier analysis. A two-tailed p value < 0.05 was considered statistically significant. Statistical analyses were conducted through NCSS version 11.0 statistical software.
Results
Patients characteristics
Baseline characteristics of the included 53 patients are shown in Table 1. All of the chemotherapy-naïve ES-SCLC patients received platinum plus etoposide chemotherapy and atezolizumab. Of them, 27 (50.9%) patients aged less than 65, while 26 (49.1%) patients older than 65; among these patients, and 46 (86.8%) had performance status of 1 or less. 34 were male and 19 were female patients; In addition, 14 patients presented with brain metastasis at initial diagnosis. As for smoking histology, 35 patients had never or former smoking status, while 18 patients were currently smoking (Table 1).
Table 1.
Baseline characteristics of included 53 patients
| Characteristics | N | % |
|---|---|---|
| Age | ||
| < 65 years | 27 | 50.9 |
| ≥ 65 years | 26 | 49.1 |
| Gender | ||
| Male | 34 | 64.2 |
| Female | 19 | 35.8 |
| Brain metastasis at diagnosis | ||
| Yes | 14 | 26.4 |
| No | 39 | 73.6 |
| Race | ||
| Caucasian | 51 | 96.2 |
| Non-Caucasian | 2 | 3.8 |
| ECOG status | ||
| 0–1 | 46 | 86.8 |
| 2 | 7 | 13.2 |
| Smoking status | ||
| Never or former | 35 | 66.0 |
| Current | 18 | 44.0 |
| Baseline index | ||
| PNI, median (range) | 48.69 (36–60.54) | |
| NLR, median (range) | 3.28 (1.09–15.6) | |
| PLR, median (range) | 152.2 (48.8–680) | |
| LMR, median (range) | 2.72 (0.75–20) | |
| ALI, median (range) | 296.37 (64.64–1048.48) | |
| SII, median (range) | 900.6 (155.25–5304) | |
| SIRI, median (range) | 2.04 (0.13–9.25) |
N number, PNI prognostic nutrition index, SIRI systemic inflammation response index, NLR neutrophil-to-lymphocyte ratio, LMR lymphocyte to monocyte ratio, PLR, platelet to lymphocyte ratio, SII systemic immune-inflammation index, ALI advanced lung cancer inflammation index
Optimal cut-off analysis
We performed ROC curve analysis to evaluate the predictive capability of these inflammatory response markers for OS. The optimal cut-off values of the ALI, LMR, NLR, PLR, PNI, SII and SIRI were 323.23, 2.73, 2.57, 119.23, 48, 533.28 and 2.32 based on the maximum principle of the Youden index, respectively (Fig. 1).
Fig. 1.
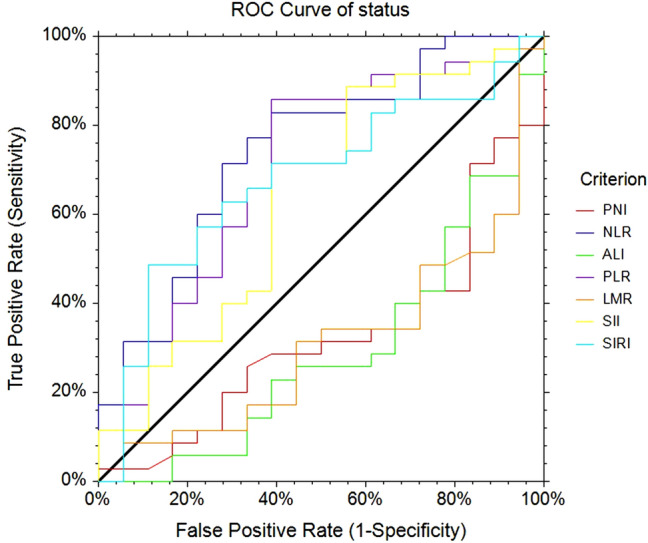
ROC curve of the preoperative inflammation markers for OS. OS = overall survival, ROC = receiver operating characteristic
Cox regression analysis for factors associated with OS
Data regarding age, race, BM at diagnosis, ECOG status, smoking status, NLR, PLR, LMR, SII, SIRI, PNI, ALI and LIPI score were included in univariate Cox regression analysis (Table 2). Our results indicated that ECOG status (HR 2.06 and 3.09, p = 0.12 and p = 0.054, respectively), NLR (HR 3.19, p = 0.01), PLR (HR 4.83, p = 0.0012), LMR (HR 0.44, p = 0.023), SII (HR 3.18, p = 0.03); PNI (HR 0.38, p = 0.0055) and LIPI (HR 1.50 and 3.43, p = 0.37 and p = 0.054, respectively) were significantly related to OS of ES-SCLC. Given the limitations of univariate analysis, multivariable Cox analysis was performed to investigate the independent factors associated with OS (Table 2). Our findings showed that PLR (HR 4.63, p = 0.05, Table 2) was the only independent predictor for OS among ES-SCLC treated with chemotherapy and atezolizumab.
Table 2.
Univariate and multivariate analysis of factors associated with OS for ES-SCLC treated with chemotherapy and atezolizumab
| Factors | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR, 95%CI | P value | HR, 95%CI | P value | |
| Age | ||||
| < 65 years | 1 | – | ||
| ≥ 65 years | 1.60 (0.82–3.13) | 0.17 | – | – |
| Gender | ||||
| Male | 1 | – | ||
| Female | 1.08(0.54–2.14) | 0.83 | – | – |
| BM at diagnosis | ||||
| No | 1 | – | ||
| Yes | 1.08 (0.54–2.15) | 0.83 | – | – |
| ECOG status | ||||
| 0 | 1 | 1 | ||
| 1 | 2.06(0.84–5.06) | 0.12 | 1.77 (0.63–4.95) | 0.27 |
| 2 | 3.09(0.98–9.71) | 0.054 | 2.29(0.64–8.19) | 0.20 |
| Smoking status | ||||
| Never or former | 1 | – | ||
| Current | 1.22 (0.59–2.49) | 0.59 | – | – |
| NLR | ||||
| ≤ 2.57 | 1 | 1 | ||
| > 2.57 | 3.19(1.32–7.74) | 0.01 | 1.46(0.24–9.04) | 0.69 |
| PLR | ||||
| ≤ 119.23 | 1 | 1 | ||
| > 119.23 | 4.83 (1.86–12.56) | 0.0012 | 4.63(1.00–21.46) | 0.05 |
| LMR | ||||
| ≤ 2.73 | 1 | 1 | ||
| > 2.73 | 0.44(0.22–0.90) | 0.023 | 0.78(0.29–2.07) | 0.61 |
| SII | ||||
| ≤ 533.28 | 1 | 1 | ||
| > 533.28 | 3.18(1.12–9.07) | 0.03 | 0.61(0.09–4.09) | 0.61 |
| SIRI | ||||
| ≤ 2.32 | 1 | – | ||
| > 2.32 | 1.83(0.94–3.58) | 0.076 | – | – |
| PNI | ||||
| ≤ 48 | 1 | 1 | ||
| > 48 | 0.38(0.19–0.75) | 0.0055 | 1.13(0.38–3.36) | 0.82 |
| ALI | ||||
| ≤ 323.23 | 1 | 1 | ||
| > 323.23 | 0.41 (0.19–0.85) | 0.016 | 1.43 (0.42–4.95) | 0.57 |
| LIPI | ||||
| 0 | 1 | 1 | ||
| 1 | 1.50(0.61–3.69) | 0.37 | 0.78(0.22–2.72) | 0.70 |
| 2 | 3.43 (1.44–8.15) | 0.0054 | 1.53(0.37–6.36) | 0.56 |
HR hazard ratio, OS overall survival, PNI prognostic nutrition index, SIRI, systemic inflammation response index, NLR neutrophil-to-lymphocyte ratio, LMR, lymphocyte to monocyte ratio, PLR platelet to lymphocyte ratio, SII systemic immune-inflammation index, ALI advanced lung cancer inflammation index, LIPI lung immune prognostic index
Survival analysis according to PLR
With a median follow-up of 17.1 months (range 0.33–21.67 months), the 1-year OS was 56% and the 6-months PFS was 30%. We also performed Kaplan–Meier analysis according to baseline PLR status. Our results showed that the OS and PFS of ES-SCLC with low PLR value (≤ 119.23) were significantly higher than these with high PLR value (1-year OS: 87% vs 42%, p = 0.0004 Fig. 2; 6 months PFS: 50% vs. 22%, p = 0.014, Fig. 3).
Fig. 2.
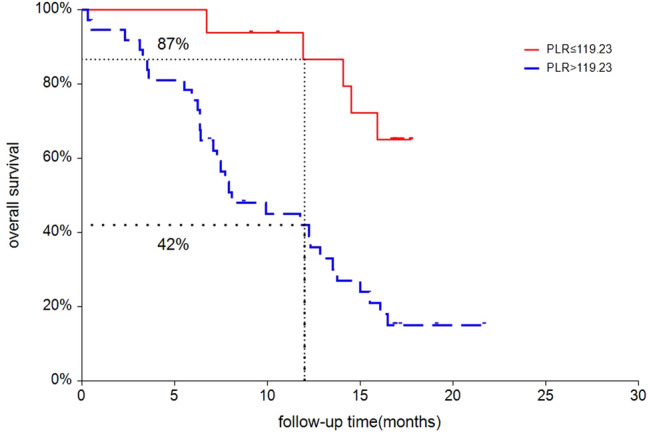
Overall survival according to PLR status (≤ 119.23 vs. > 119.23)
Fig. 3.

Progression-free survival according to PLR status (≤ 119.23 vs. 119.23)
Role of PLR in external validation set
The prognostic role of PLR was externally validated in an independent cohort of 31 ES-SCLC treated with chemotherapy and immune checkpoint inhibitors (ICIs) from our institute between November 2015 and September 2020. Of them, 20 patients treated with first-line chemotherapy and ICIs, and the other 11 patients treated with second- or third-line chemotherapy and ICIs. Until the last followed-up in January 2021, six patients had died. In consistent with our previous findings, our results also showed that prognosis of patients with high PLR was also significantly poorer than these with low PLR in terms of OS (p = 0.038, Fig. 3) and PFS (p = 0.028, Fig. 4).
Fig. 4.

Overall survival according to PLR status in external cohort
Discussion
During the past decade, the introduction of ICIs for the treatment of cancer has significantly changed the clinical treatment practice of solid tumors, including SCLC. ICIs constitute a novel class of agents that block inhibitory receptors and thus harness the immune system to mount effective antitumor responses. Atezolizumab is a humanized, engineered monoclonal antibody that targeting PD-1/PD-L1 pathways. The IMpower133 study [9], a randomized phase 3 trial, demonstrated that the atezolizumab combined with chemotherapy group had a median overall survival of 12.3 months, which was substantially higher than the 10.3 months observed in placebo combined chemotherapy group (HR, 0.70; 95%CI, 0.54 to 0.91; p = 0.007). In addition, KEYNOTE-028 study [34] also showed that the objective response rate (ORR) of pembrolizumab was 33% (95%CI: 16–55%) with acceptable toxicity profile. Therefore, it is anticipating that the usage of ICIs as a standard of care treatment for various types of cancers including SCLC could be increasing. However, the clinical benefit obtaining from ICIs therapy is not universal for all cancer patients. Therefore, it has become a priority for the oncology community to identify the optimal candidate patients for ICIs treatment by using prognostic biomarkers (Fig. 5).
Fig. 5.

Progression-free survival according to PLR status in external cohort
Recently, increasing evidence suggests that cancer-related inflammation plays an important role in cancer development and disease progression [35]. Indeed, biomarkers of inflammation deriving from peripheral blood are significantly associated with survival for various tumors including lung cancer [36–42]. Moreover, several inflammatory indexes, such as the NLR [43, 44], nutritional index [45], LMR [46], and LIPI [47], have also been reported as potential predictors of the effectiveness of anti-PD-1 antibody therapy. However, the prognostic of inflammatory and nutritional indexes in ES-SCLC treated with ICIs remains unknown. To our best knowledge, our study is the first to comprehensively investigate the prognostic role of systematic inflammatory and nutritional indexes in ES-SCLC treated with ICIs. Our results showed that baseline ECOG status, NLR, PLR, LMR, SII, PNI and LIPI are significantly related to OS of ES-SCLC. In the multivariate analysis, PLR is the only independent predictors for OS of ES-SCLC patients who treated with chemotherapy and atezolizumab. Additionally, an externally validation of an independent cohort of 31 patients from our institute also demonstrates that baseline PLR value is a prognostic factor for ES-SCLC treated with chemotherapy and ICIs. Prior to the present study, multiple retrospective studies, mainly focusing on non-small-cell lung cancer, have been conducted to investigate the prognostic role of PLR in cancer patients treated with immunotherapy. Bilen M. et al. [48] found that baseline and early changes in PLR were strongly associated with clinical outcomes in cancer patients immunotherapy. Subsequently, Diem S. et al. demonstrated that elevated pre-treatment NLR and PLR were significantly associated with shorter OS and PFS in NSCLC treated with nivolumab. In 2019, Xu. H. et al. [49]. performed a meta-analysis indicated that PLR could be a routinely potential prognostic factor for ICIs. And low PLR might be associated with better survival for cancer patients when treated with immunotherapy. More recently, a meta-analysis of 21 studies conducted by Zhang N. et al. also demonstrated that pre-treatment PLR could serve as prognostic biomarkers in NSCLC patients treated with ICIs [17]. Based on our findings from a second-analysis of prospective clinical trial, pre-treatment PLR could be considered as a supplement in distinguishing higher risk group of ES-SCLC treated with ICIs and predicting treatment outcomes.
However, there are several potential limitations of our study needed to be concerned. First of all, despite of the randomized, prospective nature of the included studies, our study is a retrospective analysis of the prospective trial and might have potentially selection bias. In addition, the patient population in the present study have adequate organ function and acceptable performance status thus could not represent the entire SCLC population. Secondly, the standard optimal cut-off value for these markers is yet to be established; some studies choose the median of each inflammatory marker as the cut-off value, while others determine the cut-off value based on previous studies. Therefore, how to identify the optimal value for grouping patients into high versus low PLR is one of the most challenging questions. The cut-off values of defining high versus low PLR ranged from 45 to 400 among published studies. In the present study, we use receiver operating characteristic curve to select the optimal cut-off. The optimal cut-off value of the PLR is 119.23.
Conclusion
In conclusion, the present study confirms that pre-treatment PLR could serve as a valuable independent prognostic factor of ES-SCLC who receiving chemotherapy combined with atezolizumab. In addition, pre-treatment PLR could assist physicians to perform an individualized therapeutic scheme to improve the unfavorable survival in advanced. However, multi-center and large clinical trials should be performed to confirm our findings.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgement
This publication was based on research using information obtained from www.projectdatasphere.org, which was maintained by Project Data Sphere, LLC. Neither Project Data Sphere, LLC nor the owner(s) of any information from the website had contributed to, approved or were in any way responsible for the contents of this publication.
Funding
None.
Declarations
Conflict of interest
The author declares that they have no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shengguang Zhao, Email: qwx12055@rjh.com.cn.
Jiayi Chen, Email: chenjiayi0188@aliyun.com.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Wang S, Zimmermann S, Parikh K, Mansfield AS, Adjei AA. Current diagnosis and management of small-cell lung cancer. Mayo Clin Proc. 2019;94(8):1599–1622. doi: 10.1016/j.mayocp.2019.01.034. [DOI] [PubMed] [Google Scholar]
- 3.Byers LA, Rudin CM. Small cell lung cancer: where do we go from here? Cancer. 2015;121(5):664–672. doi: 10.1002/cncr.29098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth BJ, Johnson DH, Einhorn LH, Schacter LP, Cherng NC, Cohen HJ, Crawford J, Randolph JA, Goodlow JL, Broun GO, et al. Randomized study of cyclophosphamide, doxorubicin, and vincristine versus etoposide and cisplatin versus alternation of these two regimens in extensive small-cell lung cancer: a phase III trial of the Southeastern Cancer study group. J Clin Oncol Off J Am Soc Clin Oncol. 1992;10(2):282–291. doi: 10.1200/JCO.1992.10.2.282. [DOI] [PubMed] [Google Scholar]
- 5.Sundstrom S, Bremnes RM, Kaasa S, Aasebo U, Hatlevoll R, Dahle R, Boye N, Wang M, Vigander T, Vilsvik J, et al. Cisplatin and etoposide regimen is superior to cyclophosphamide, epirubicin, and vincristine regimen in small-cell lung cancer: results from a randomized phase III trial with 5 years' follow-up. J Clin Oncol Off J Am Soc Clin Oncol. 2002;20(24):4665–4672. doi: 10.1200/JCO.2002.12.111. [DOI] [PubMed] [Google Scholar]
- 6.Horn L, Reck M, Spigel DR. The future of immunotherapy in the treatment of small cell lung cancer. Oncologist. 2016;21(8):910–921. doi: 10.1634/theoncologist.2015-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudin CM, Ismaila N, Hann CL, Malhotra N, Movsas B, Norris K, Pietanza MC, Ramalingam SS, Turrisi AT, 3rd, Giaccone G. Treatment of small-cell lung cancer: American society of clinical oncology endorsement of the American college of chest physicians guideline. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33(34):4106–4111. doi: 10.1200/JCO.2015.63.7918. [DOI] [PubMed] [Google Scholar]
- 8.George J, Lim JS, Jang SJ, Cun Y, Ozretic L, Kong G, Leenders F, Lu X, Fernandez-Cuesta L, Bosco G, et al. Comprehensive genomic profiles of small cell lung cancer. Nature. 2015;524(7563):47–53. doi: 10.1038/nature14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horn L, Mansfield AS, Szczesna A, Havel L, Krzakowski M, Hochmair MJ, Huemer F, Losonczy G, Johnson ML, Nishio M, et al. First-line Atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220–2229. doi: 10.1056/NEJMoa1809064. [DOI] [PubMed] [Google Scholar]
- 10.Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, Statsenko G, Hochmair MJ, Ozguroglu M, Ji JH, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394(10212):1929–1939. doi: 10.1016/S0140-6736(19)32222-6. [DOI] [PubMed] [Google Scholar]
- 11.Reck M, Bondarenko I, Luft A, Serwatowski P, Barlesi F, Chacko R, Sebastian M, Lu H, Cuillerot JM, Lynch TJ. Ipilimumab in combination with paclitaxel and carboplatin as first-line therapy in extensive-disease-small-cell lung cancer: results from a randomized, double-blind, multicenter phase 2 trial. Annal Oncol Off J Eur Soc Med Oncol ESMO. 2013;24(1):75–83. doi: 10.1093/annonc/mds213. [DOI] [PubMed] [Google Scholar]
- 12.Chen HL, Tu YK, Chang HM, Lee TH, Wu KL, Tsai YC, Lee MH, Yang CJ, Hung JY, Chong IW. Systematic review and network meta-analysis of immune checkpoint inhibitors in combination with chemotherapy as a first-line therapy for extensive-stage small cell carcinoma. Cancers. 2020 doi: 10.3390/cancers12123629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iams WT, Porter J, Horn L. Immunotherapeutic approaches for small-cell lung cancer. Nat Rev Clin Oncol. 2020;17(5):300–312. doi: 10.1038/s41571-019-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suresh K, Naidoo J, Lin CT, Danoff S. Immune checkpoint immunotherapy for non-small cell lung cancer: benefits and pulmonary toxicities. Chest. 2018;154(6):1416–1423. doi: 10.1016/j.chest.2018.08.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mandaliya H, Jones M, Oldmeadow C, Nordman II. Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI) Transl Lung Cancer Res. 2019;8(6):886–894. doi: 10.21037/tlcr.2019.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobayashi S, Karube Y, Inoue T, Araki O, Maeda S, Matsumura Y, Chida M. Advanced lung cancer inflammation index predicts outcomes of patients with pathological stage IA lung adenocarcinoma following surgical resection. Annal Thorac Cardiovasc Surg Off J Assoc Thorac Cardiovasc Surg Asia. 2019;25(2):87–94. doi: 10.5761/atcs.oa.18-00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang N, Jiang J, Tang S, Sun G. Predictive value of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in non-small cell lung cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Int Immunopharmacol. 2020;85:106677. doi: 10.1016/j.intimp.2020.106677. [DOI] [PubMed] [Google Scholar]
- 18.Mirili C, Guney IB, Paydas S, Seydaoglu G, Kapukaya TK, Ogul A, Gokcay S, Buyuksimsek M, Yetisir AE, Karaalioglu B, et al. Prognostic significance of neutrophil/lymphocyte ratio (NLR) and correlation with PET-CT metabolic parameters in small cell lung cancer (SCLC) Int J Clin Oncol. 2019;24(2):168–178. doi: 10.1007/s10147-018-1338-8. [DOI] [PubMed] [Google Scholar]
- 19.Sebastian NT, Raj R, Prasad R, Barney C, Brownstein J, Grecula J, Haglund K, Xu-Welliver M, Williams TM, Bazan JG. Association of Pre- and Posttreatment Neutrophil-Lymphocyte Ratio With Recurrence and Mortality in Locally Advanced Non-Small Cell Lung Cancer. Front Oncol. 2020;10:598873. doi: 10.3389/fonc.2020.598873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luo H, Ge H, Cui Y, Zhang J, Fan R, Zheng A, Zheng X, Sun Y. Systemic Inflammation Biomarkers Predict Survival in Patients of Early Stage Non-Small Cell Lung Cancer Treated With Stereotactic Ablative Radiotherapy - A Single Center Experience. J Cancer. 2018;9(1):182–188. doi: 10.7150/jca.21703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang R, Chang Q, Meng X, Gao N, Wang W. Prognostic value of Systemic immune-inflammation index in cancer: A meta-analysis. J Cancer. 2018;9(18):3295–3302. doi: 10.7150/jca.25691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li X, Hu P, Liu J, Zhang J, Liu Q. Systemic immune-inflammation index predicted overall survival and radiosensitivity in advanced non-small-cell lung cancer. Future Oncol. 2020;16(5):103–115. doi: 10.2217/fon-2019-0761. [DOI] [PubMed] [Google Scholar]
- 23.Chen L, Kong X, Wang Z, Wang X, Fang Y, Wang J. Pretreatment Systemic Inflammation Response Index in Patients with Breast Cancer Treated with Neoadjuvant Chemotherapy as a Useful Prognostic Indicator. Cancer Manag Res. 2020;12:1543–1567. doi: 10.2147/CMAR.S235519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valero C, Pardo L, Sansa A, Garcia Lorenzo J, Lopez M, Quer M, Leon X. Prognostic capacity of Systemic Inflammation Response Index (SIRI) in patients with head and neck squamous cell carcinoma. Head Neck. 2020;42(2):336–343. doi: 10.1002/hed.26010. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Liu F, Wang Y. Evidence of the Prognostic Value of Pretreatment Systemic Inflammation Response Index in Cancer Patients: A Pooled Analysis of 19 Cohort Studies. Dis Markers. 2020;2020:8854267. doi: 10.1155/2020/8854267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin S, Cao S, Xu S, Wang C, Meng Q, Yu Y. Clinical impact of pretreatment prognostic nutritional index (PNI) in small cell lung cancer patients treated with platinum-based chemotherapy. Clin Respir J. 2018;12(9):2433–2440. doi: 10.1111/crj.12925. [DOI] [PubMed] [Google Scholar]
- 27.Jiang AM, Zhao R, Liu N, Ma YY, Ren MD, Tian T, Yao Y. The prognostic value of pretreatment prognostic nutritional index in patients with small cell lung cancer and it's influencing factors: a meta-analysis of observational studies. J Thorac Dis. 2020;12(10):5718–5728. doi: 10.21037/jtd-20-1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mezquita L, Auclin E, Ferrara R, Charrier M, Remon J, Planchard D, Ponce S, Ares LP, Leroy L, Audigier-Valette C, et al. Association of the lung immune prognostic index with immune checkpoint inhibitor outcomes in patients with advanced non-small cell lung cancer. JAMA Oncol. 2018;4(3):351–357. doi: 10.1001/jamaoncol.2017.4771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aldea M, Benitez JC, Mezquita L. The lung immune prognostic index (LIPI) stratifies prognostic groups in advanced non-small cell lung cancer (NSCLC) patients. Transl Lung Cancer Res. 2020;9(4):967–970. doi: 10.21037/tlcr.2020.04.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang W, Huang Z, Yu Z, Zhuang W, Zheng W, Cai Z, Shi L, Yu X, Lou G, Hong W, et al. Prognostic value of the lung immune prognostic index may differ in patients treated with immune checkpoint inhibitor monotherapy or combined with chemotherapy for non-small cell lung cancer. Front Oncol. 2020;10:572853. doi: 10.3389/fonc.2020.572853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daniel D, Kuchava V, Bondarenko I, Ivashchuk O, Reddy S, Jaal J, Kudaba I, Hart L, Matitashvili A, Pritchett Y, et al. Trilaciclib prior to chemotherapy and atezolizumab in patients with newly diagnosed extensive-stage small cell lung cancer: a multicentre randomised double-blind placebo-controlled phase II trial. Int J Cancer. 2020 doi: 10.1002/ijc.33453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gao J, Wang Y, Li F, Zhu Z, Han B, Wang R, Xie R, Xue Y. Prognostic nutritional index and neutrophil-to-lymphocyte ratio are respectively associated with prognosis of gastric cancer with liver metatasis undergoing and without hepatectomy. Biomed Res Int. 2019;2019:4213623. doi: 10.1155/2019/4213623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galvano A, Peri M, Guarini AA, Castiglia M, Grassadonia A, De Tursi M, Irtelli L, Rizzo S, Bertani A, Gristina V, et al. Analysis of systemic inflammatory biomarkers in neuroendocrine carcinomas of the lung: prognostic and predictive significance of NLR, LDH, ALI, and LIPI score. Ther Adv Med Oncol. 2020;12:1758835920942378. doi: 10.1177/1758835920942378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ott PA, Elez E, Hiret S, Kim DW, Morosky A, Saraf S, Piperdi B, Mehnert JM. Pembrolizumab in patients with extensive-stage small-cell lung cancer: results from the phase Ib KEYNOTE-028 Study. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35(34):3823–3829. doi: 10.1200/JCO.2017.72.5069. [DOI] [PubMed] [Google Scholar]
- 35.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 36.Hu H, Yao X, Xie X, Wu X, Zheng C, Xia W, Ma S. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J Urol. 2017;35(2):261–270. doi: 10.1007/s00345-016-1864-9. [DOI] [PubMed] [Google Scholar]
- 37.Wang K, Diao F, Ye Z, Zhang X, Zhai E, Ren H, Li T, Wu H, He Y, Cai S, et al. Prognostic value of systemic immune-inflammation index in patients with gastric cancer. Chin J Cancer. 2017;36(1):75. doi: 10.1186/s40880-017-0243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dolan RD, Laird BJA, Horgan PG, McMillan DC. The prognostic value of the systemic inflammatory response in randomised clinical trials in cancer: a systematic review. Crit Rev Oncol Hematol. 2018;132:130–137. doi: 10.1016/j.critrevonc.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 39.Duan J, Pan L, Yang M. Preoperative elevated neutrophil-to-lymphocyte ratio (NLR) and derived NLR are associated with poor prognosis in patients with breast cancer: a meta-analysis. Medicine. 2018;97(49):e13340. doi: 10.1097/MD.0000000000013340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee GW, Park SW, Go SI, Kim HG, Kim MK, Min CK, Kwak JY, Bae SB, Yoon SS, Lee JJ, et al. The derived neutrophil-to-lymphocyte ratio is an independent prognostic factor in transplantation ineligible patients with multiple myeloma. Acta Haematol. 2018;140(3):146–156. doi: 10.1159/000490488. [DOI] [PubMed] [Google Scholar]
- 41.Liu JX, Li A, Zhou LY, Liu XF, Wei ZH, Wang XZ, Ying HQ. Significance of combined preoperative serum Alb and dNLR for diagnosis of pancreatic cancer. Future Oncol. 2018;14(3):229–239. doi: 10.2217/fon-2017-0339. [DOI] [PubMed] [Google Scholar]
- 42.Liu XF, Zhou LY, Wei ZH, Liu JX, Li A, Wang XZ, Ying HQ. The diagnostic role of circulating inflammation-based biomarker in gallbladder carcinoma. Biomark Med. 2018;12(10):1095–1103. doi: 10.2217/bmm-2018-0049. [DOI] [PubMed] [Google Scholar]
- 43.Petrova MP, Eneva MI, Arabadjiev JI, Conev NV, Dimitrova EG, Koynov KD, Karanikolova TS, Valev SS, Gencheva RB, Zhbantov GA, et al. Neutrophil to lymphocyte ratio as a potential predictive marker for treatment with pembrolizumab as a second line treatment in patients with non-small cell lung cancer. Biosci Trends. 2020;14(1):48–55. doi: 10.5582/bst.2019.01279. [DOI] [PubMed] [Google Scholar]
- 44.Matsubara T, Takamori S, Haratake N, Toyozawa R, Miura N, Shimokawa M, Yamaguchi M, Seto T, Takenoyama M. The impact of immune-inflammation-nutritional parameters on the prognosis of non-small cell lung cancer patients treated with atezolizumab. J Thorac Dis. 2020;12(4):1520–1528. doi: 10.21037/jtd.2020.02.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ohba T, Takamori S, Toyozawa R, Nosaki K, Umeyama Y, Haratake N, Miura N, Yamaguchi M, Taguchi K, Seto T, et al. Prognostic impact of the controlling nutritional status score in patients with non-small cell lung cancer treated with pembrolizumab. J Thorac Dis. 2019;11(9):3757–3768. doi: 10.21037/jtd.2019.09.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Failing JJ, Yan Y, Porrata LF, Markovic SN. Lymphocyte-to-monocyte ratio is associated with survival in pembrolizumab-treated metastatic melanoma patients. Melanoma Res. 2017;27(6):596–600. doi: 10.1097/CMR.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 47.Kazandjian D, Gong Y, Keegan P, Pazdur R, Blumenthal GM. Prognostic value of the lung immune prognostic index for patients treated for metastatic non-small cell lung cancer. JAMA Oncol. 2019 doi: 10.1001/jamaoncol.2019.1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bilen MA, Martini DJ, Liu Y, Lewis C, Collins HH, Shabto JM, Akce M, Kissick HT, Carthon BC, Shaib WL, et al. The prognostic and predictive impact of inflammatory biomarkers in patients who have advanced-stage cancer treated with immunotherapy. Cancer. 2019;125(1):127–134. doi: 10.1002/cncr.31778. [DOI] [PubMed] [Google Scholar]
- 49.Xu H, He A, Liu A, Tong W, Cao D. Evaluation of the prognostic role of platelet-lymphocyte ratio in cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis. Int Immunopharmacol. 2019;77:105957. doi: 10.1016/j.intimp.2019.105957. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


