Abstract
Objective:
Our study was conducted with an attempt to investigate the diagnostic analysis of abnormal increase of fetal pulmonary artery systolic pressure (PASP) in middle and late pregnancy by color Doppler echocardiography.
Methods:
From August 2017 to January 2019, 52 fetuses with moderate or greater tricuspid high-speed regurgitation were retrospectively analyzed and selected as Group A. 88 fetuses with full-color blood flow of the two ventricles and symmetrical sizes of the cardiac cavities on both sides harboring tricuspid valve and mild regurgitation or a small amount of regurgitation were selected as Group B. The pulmonary artery blood flow acceleration time (AT) and right ventricular ejection time (ET) was measured, and the PASP was calculated.
Results:
The tricuspid regurgitation velocity, tricuspid regurgitation pressure difference and PASP in Group A were higher than those in Group B (p < 0.05), and the AT and AT/ET values in Group A were lower than those in Group B (p < 0.05). Gestational age, tricuspid regurgitation velocity and tricuspid regurgitation pressure difference were positively correlated with PASP. However, AT/ET and AT value were negatively correlated with PASP.
Conclusion:
The abnormal increase of pulmonary artery can be assessed by color Doppler echocardiography of fetal tricuspid regurgitation, which is worth popularizing and applying in clinic.
Advances in knowledge:
It was suggested that the middle- and late-stage fetuses with moderate or greater tricuspid regurgitation and with >20 mmHg regurgitation pressure difference should be followed up in clinic. If PASP was ≥70 mmHg with symptoms of right heart failure, fetuses should be closely observed until 35–36 weeks old to ensure fetal safety and early delivery would be recommended.
Introduction
The diagnosis of heart disease in infants and young children should be based on color Doppler echocardiography. 1 Fetal tricuspid regurgitation can be detected by color Doppler echocardiography, which is considered a common condition. In fact, most of fetal tricuspid regurgitation are a small amount of fetal regurgitation, which is normal physiological reflux. 2,3 At present, scholars have evaluated the changes of pulmonary artery pressure in newborns (premature infants) by observing tricuspid blood flow velocity, 4 but limited clinical studies have been reported in terms of the changes and normal range of fetal pulmonary artery pressure in middle and late pregnancy. Based on several clinical studies, 5 pulmonary artery systolic pressure (PASP) is usually less than 20 mmHg (1mmHg = 0.133 kPa), which is a normal value. But other studies 6 suggest that fetal high pulmonary artery pressure decreases slowly after birth. Through the observation of fetuses in middle- and late-stage pregnancy with abnormally high pulmonary artery pressure, the researchers found that some fetuses could be accompanied by moderate or greater tricuspid regurgitation with high regurgitation pressure difference, and even with significantly enlarged right cardiac cavity. Moreover, the condition of right ventricular failure could occur, such as the effusion of thorax and abdominal cavity, and pericardial. Therefore, efforts have been made in the current study to explore the color Doppler echocardiography of the abnormal increase of PASP in the middle and late pregnancy, with an attempt to offer the differential evidence for the clinical diagnosis of the fetus with abnormal increase in PASP and ensure the health of the fetus.
Patients and methods
Study object
From August 2017 to January 2019, 52 fetuses of over 23 weeks’ old with moderate or greater tricuspid high speed regurgitation (including moderate) harboring varying degrees of right ventricle and right atrium enlargement were analyzed as Group A. Meanwhile, 88 fetuses of over 23 weeks’ old with tricuspid mild regurgitation or a small amount of regurgitation (velocity not exceeding 2.2 m/s) were selected as Group B. To be included in the current study, the following inclusion criteria should be met: (1) pregnant females with no history of chronic diseases such as hypertension, diabetes and hyperthyroidism; (2) patients with complete clinical data and good compliance; (3) patients with no family history of genetic disease; (4) patients with no history of smoking. Exclusion criteria were as follows: (1) patients harboring organic lesions such as ventricular septal defect; (2) patients with stenosis of pulmonary artery orifice; (3) patients with outflow tract obstruction affecting right ventricular contractility.
Methods
The Philips iU22 and iE33, probes with convex array and frequency of 2-6MHz were used to equip the color echocardiography. Another cardiac probe, S5-1, was provided with a frequency of 2-8 MHz. The two groups of parturient females were detected by the same two color ultrasound doctors who had 8 year experiences in the color ultrasound department of Taian City Central Hospital. First of all, obstetrical examination was conducted. Pregnant females were in lateral position or supine position, if the fetal position was not good, they should be re-examined after 30–60min. The fetal amniotic fluid index, biparietal diameter and amniotic fluid index were examined by ultrasound to eliminate the abnormal fetus. Secondly, focuses had been laid on detecting the various sections of the fetal heart, adjusting the angle of the ultrasonic diagnostic instrument for pregnant females of different body types to observing for more than three times. The cross-section of the upper abdomen of pregnant females was performed to detect section of cardiovascular structure of fetuses, including fetal thoracic four-lumen heart, superior and inferior vena cava, three-vessel trachea, left and right ventricular outflow tract, five-chamber heart, long axis of ductus arteriosus, long axis of aortic arch and so on. Then the blood flow spectra of fetal aortic valve, mitral valve, tricuspid valve and pulmonary valve were observed. The cardiac position, the continuity of atrium and vein, atrioventricular and ventricular arteries were determined, and the intracardiac structures such as valve, foramen ovale and atrioventricular size were observed. After determining whether there was perforating blood flow in the atrial septum and ventricular septum, the atrioventricular septal defect and valvular disease fetus were removed and observe whether there was pulmonary vein in the left atrium, and remove the anomalous pulmonary vein drainage. When pulsed Doppler detection was used, the sampling volume should be placed at about 3 mm on the pulmonary valve, and the turning point of low velocity blood flow (from the starting point of pulmonary artery to the peak value of pulmonary artery blood flow) should be measured to get the AT result, which should be measured three times and the average value was taken. The ejection time (ET), pressure Gradient (PG) and tricuspid regurgitation peak velocity (TRV) of fetuses in Group A were measured by color Doppler ultrasonography. The results were measured three times, and the average value was taken.
The PASP was obtained based on TRV and the pressure gradient. The internal diameter, aorta and blood flow velocity above the pulmonary valve were measured by the direction of blood flow within 20° angle between the sound beam and the sound bundle, and the fetuses with pulmonary artery or aortic stenosis were removed. Follow-ups: the fetuses in Group A should be examined once a month until the pulmonary artery pressure returned to normal. If the fetus still had high pulmonary artery pressure before birth, it should be followed up until after birth.
Observation indicators
The color Doppler echocardiographic findings of the two groups were observed, and the pulmonary artery blood flow acceleration time (AT) and right ventricular ET were measured, and the PASP was calculated. The differences of PASP between the two groups were compared and the fetuses in Group A were followed-up.
PASP
The systolic pressure of right ventricle was the same as that of pulmonary artery in the case of right ventricular outflow tract obstruction or no pulmonary artery stenosis. The pressure gradient and TRV were measured three times based on simplified Bernoulli equation PASP = RAP+4 V2. RAP represented right atrial pressure and V was used to represent the maximum velocity of tricuspid regurgitation. 7
Fetal right atrial pressure
According to the evaluation method of adult right atrial pressure for assessment of fetuses. Considering the adult right atrial pressure is larger than that of infants and fetuses, and there was a lack of a unified standard of fetal right atrial pressure in clinic, 1/2 adult right atrial pressure was set as infant right atrial pressure and 1/3 adult right atrial pressure was set as fetal right atrial pressure due to the smaller pressure of fetus.
Adult right atrial pressure
When there was tricuspid regurgitation, 5, 10 and 15 mmHg were considered mild, moderate and severe respectively. Hence, right atrial pressure of fetal tricuspid regurgitation and grading were as follows: (1) a small amount of regurgitation, its site was limited to the tricuspid valve orifice; (2) 1.7 mmHg was mild regurgitation, the regurgitation site passed through the tricuspid valve orifice, but not more than 1/3 of the right atrium near the valve orifice, (3) 3.3 mmHg was moderate regurgitation, which could reach half of the area of the right atrium; (4) 5.0 mmHg was severe regurgitation, which could reach the right atrium near the top.
Statistical analysis
In this study, SPSS20.0 analysis was used to analyze the data. And t-test was used to compare the continuous variables, and the sample size of the two groups was processed (>50) according to the approximate normal distribution. The correlation between the variables was analyzed by Spearman correlation method. A p < 0.05 was considered significant difference.
Results
Comparison of baseline data between the two groups
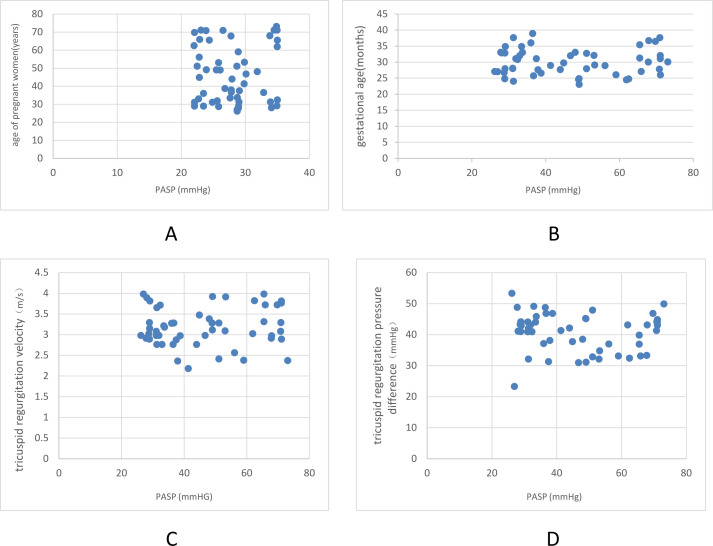
There was no significant difference in age between the two groups (p > 0.05), but the tricuspid regurgitation velocity, tricuspid regurgitation pressure difference and PASP in Group A were higher than those in Group B (p < 0.05), as laid out in Table 1. No correlation was observed between the age of pregnant females and PASP (r = 0.001, p = 0.674) (Figure 1A). However, gestational age, tricuspid regurgitation velocity and tricuspid regurgitation pressure difference were positively correlated with PASP (r = 0.421, 0.983, 0.918, p < 0.01), as shown in Figure 1B–D, respectively.
Table 1.
Comparison of baseline data between the two groups ( ±s)
| Group | Age (year) | Fetal age | Tricuspid regurgitation velocity (m/s) | Tricuspid regurgitation pressure difference (mmHg) | PASP (mmHg) |
|---|---|---|---|---|---|
| Group A (n = 52) | 27.90 ± 3.81 | 30.09 ± 3.81 | 3.18 ± 0.49 | 40.72 ± 11.87 | 46.48 ± 10.83 |
| Group B (n = 88) | 27.01 ± 3.76 | 29.91 ± 3.98 | 1.61 ± 0.28 | 10.83 ± 4.62 | 13.01 ± 3.82 |
| t value | 1.876 | 2.098 | 8.971 | 9.871 | 7.654 |
| p-value | 13.82 | 12.08 | <0.01 | <0.01 | <0.01 |
PASP, pulmonary artery systolic pressure.
Figure 1.
A. Correlation between age of pregnant females and PASP; B. Correlation between gestational age and PASP; C. Correlation between tricuspid regurgitation velocity and PASP; D. Correlation between tricuspid regurgitation pressure difference and PASP. PASP, pulmonary artery systolic pressure.
Comparison of AT and ET values of tricuspid between the two groups
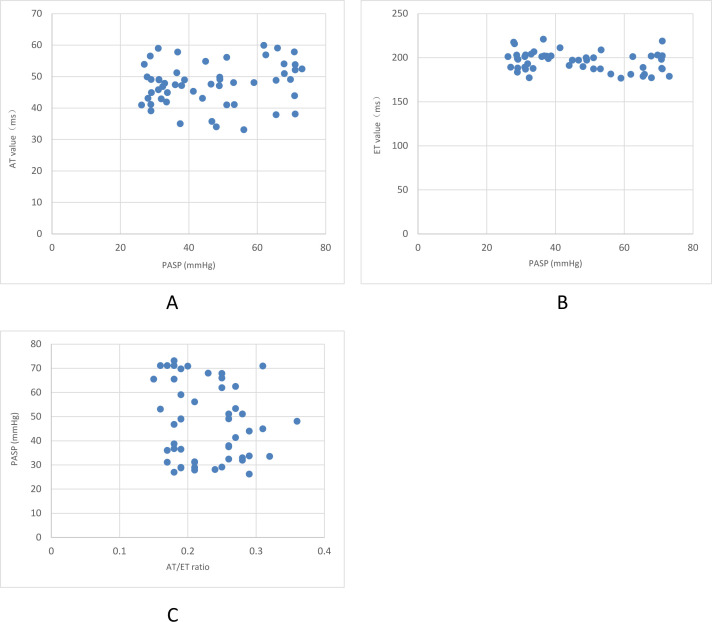
The AT and AT/ET in Group A were lower than those in Group B (p < 0.05), but there was no significant difference in ET between the two groups (p > 0.05), as shown in Table 2. PASP was negatively correlated with AT (r = 0.51, p < 0.01), as laid out in Figure 2A. PASP was negatively correlated with the ET in group A (r = −0.49, p < 0.01) and AT/ET in group A (r =-0. 49, p < 0.01), based on Figure 2B and C respectively.
Table 2.
Comparison of tricuspid AT, ET and AT/ ET between the two groups ( ±s, ms)
| Group | AT | ET | AT/ET |
|---|---|---|---|
| Group A (n = 52) | 47.56 ± 4.97 | 195.70 ± 16.42 | 0.23 ± 0.02 |
| Group B (n = 88) | 55.18 ± 8.97 | 197.84 ± 17.08 | 0.27 ± 0.04 |
| t value | 1.876 | 2.098 | 1.071 |
| p-value | 13.82 | 12.08 | 14.09 |
AT, acceleration time; ET, ejection time.
Figure 2.
A. Correlation between PASP and AT; B. Correlation between PASP and ET in Group A; C. Correlation between PASP and AT/ET in Group A. AT,acceleration time; ET, ejection time; PASP, pulmonaryartery systolic pressure.
Follow-ups
A total of 52 cases in Group A were followed up. Figure 3 showed fetal color Doppler echocardiography with increased PASP. Fig. A and B respectively showed that the regurgitation bundle reached the middle of the right atrium, which was moderate tricuspid regurgitation; and the regurgitation bundle reaches the top of the right atrium, which was severe tricuspid regurgitation. Among them, 40 cases (76.92%) of fetal with PASP <50 mmHg, disappeared tricuspid regurgitation or mild regurgitation, and the internal diameters of right atrium and right ventricle returned to normal. Severe PASP ≥70 mmHg occurred in 12 cases (23.08%), accompanied by right heart failure, such as pericardial effusion and right ventricular cavity enlargement, and early delivery with 36–37 gestational weeks would be recommended. After birth, PASP of seven cases returned to normal, heart failure improved, and two cases returned to normal within 30 days, one case returned to normal within 90 days, and one case returned to normal within 106 days. Of the 12 cases, only 1 case of neonatal dyspnea caused by persistent increase of PASP and hypoxia who was admitted to hospital and given ventilator to help breathe. The patient was discharged on the 21st day of admission and died on the 22nd day of admission.
Figure 3.
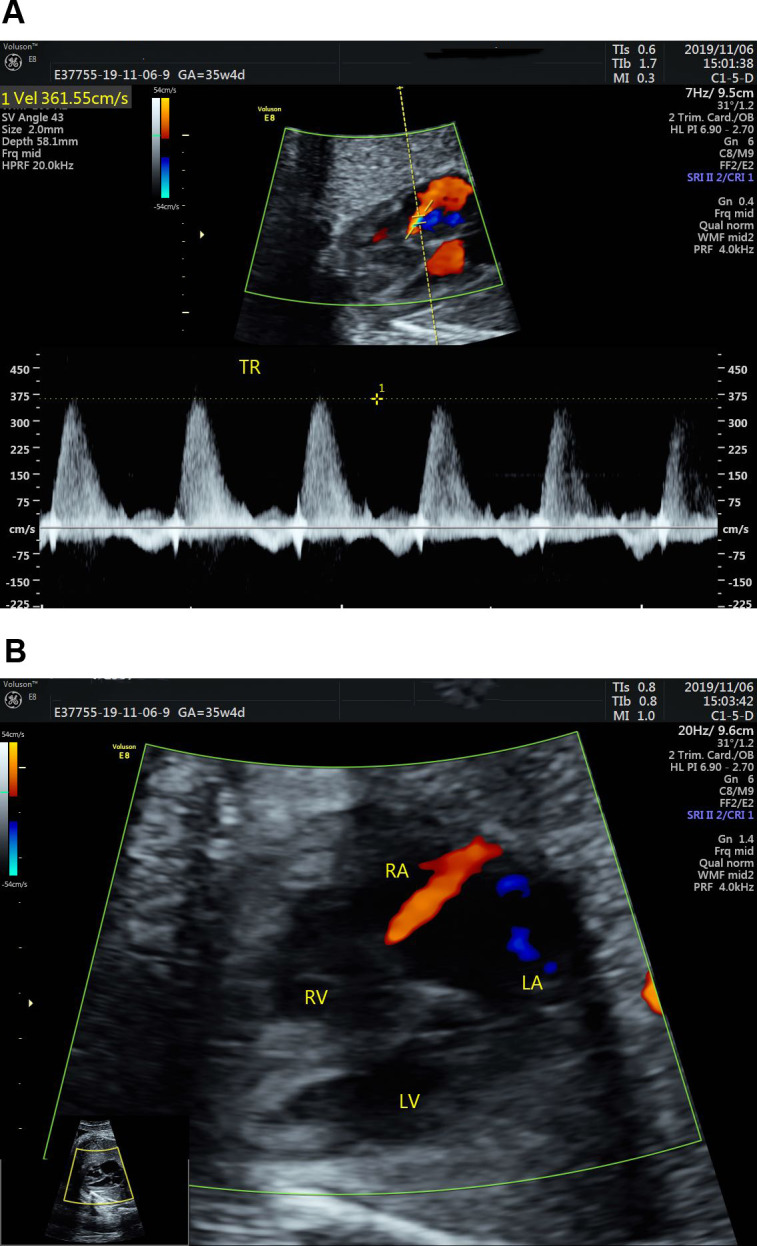
(A) The regurgitation bundle reached the middle of the right atrium; (B) The regurgitation bundle reaches the top of the right atrium.
Discussion
The persistent abnormal increase of pulmonary artery PASP in middle- and late-stage fetus accounts for only 0.2% in clinic, but the mortality rate of the disease reaches as high as 20%, which poses a great threat to the safety, growth and development of fetus. 8,9 Therefore, in clinical practice, the abnormal increase of pulmonary artery PASP in the middle and late stage of fetus should be diagnosed and treated in early period in order for the safety of the fetus. Currently, the commonly used clinical examination methods include electrocardiogram, cardiac catheterization and echocardiography, with different diagnostic effect. The gold-standard for the diagnosis of pulmonary artery pressure in clinic is the direct measurement of cardiac catheterization. But since it is an invasive operation with serious complications, fetuses in middle and late stage are not recommended. According to study supported by Schmitz et al., 10 Bernoulli equation in ultrasonic Doppler method is effective in detecting pulmonary artery pressure in adults and infants, which has been widely used in clinic. The measurement value of color Doppler echocardiography is similar to that of cardiac catheterization, and color Doppler echocardiography has the advantages of simple operation, reliable data, repeated examination, non-trauma, low cost and so on. The most important part in the detection of pulmonary artery PASP by color Doppler echocardiography is to accurate evaluate the flow velocity of tricuspid regurgitation and right atrial pressure. In order to accurately evaluate the flow velocity of tricuspid regurgitation, the different sections of cardiac vascular structure should be measured. In this study, the most obvious section of tricuspid regurgitation was found on the thoracic four-lumen heart, superior and inferior vena cava, three-vessel trachea, left and right ventricular outflow tract, five-lumen heart, long axis of ductus arteriosus and long axis of aortic arch. The peak velocity of tricuspid regurgitation in late fetus was measured by color Doppler echocardiography to determine the position of pulmonary artery PASP. There involve position changes fetuses in the middle and late stage, making it difficult to operate, and error value may occur in Doppler, but more than three consecutive tests were used in the detection, and in order to avoid the inaccuracy of the measured values, ultrasonic beam should be parallel to the tricuspid regurgitation or 20° between them. The excessive angle between ultrasonic beam and tricuspid regurgitation should be avoided to cause in smaller results, and the detection error was less than 5%. The results of this study confirm the feasibility of this method for detecting the peak velocity of tricuspid regurgitation in mid-to-late stage fetuses.
The study by Tuo et al 11 suggested that the application of color Doppler echocardiography in the premature closure of fetal arterial catheters can effectively detect the fetal accompanying severe tricuspid regurgitation; and Zhan et al 12 confirmed that the use of color Doppler echocardiography can effectively detect abnormal increase in pulmonary arterial systolic blood pressure in the second and third trimester fetuses. A study by de Boode et al 13 also confirmed that the use of echocardiography can effectively diagnose and classify neonatal pulmonary hypertension. It is conducive to clinical diagnosis and timely treatment, and has important guiding value for clinical evaluation. The results of our study showed that tricuspid regurgitation velocity, tricuspid regurgitation pressure difference and PASP in Group A were higher than those in Group B, and AT and AT/ ET in Group A were lower than those in Group B (p < 0.05), indicating that the persistent abnormal increase of pulmonary artery PASP fetus in the middle and late stage had higher tricuspid regurgitation velocity, tricuspid regurgitation pressure difference and PASP. However, the AT of pulmonary artery blood flow and the time of right ventricular ejection were lower than those of normal fetus in middle and late stage. These findings all confirmed that color Doppler echocardiography can effectively detect the persistent abnormal increase in pulmonary artery PAPS, which has high application value in clinics.
The abnormal tricuspid regurgitation in the middle and late stage of fetal is mainly due to the excessive burden of right ventricular resistance and the evident increase of right ventricular systolic pressure leads to tricuspid regurgitation. 14 In addition, fetuses without atresia or pulmonary artery stenosis also have the possibility of tricuspid regurgitation, and the regurgitation pressure difference can exceed 70 mmHg. What’s worse, they could be accompanied by right ventricular failure symptoms such as significantly enlarged right atrium and right ventricle, and pericardial effusion. Abnormal tricuspid regurgitation often occurs in pulmonary atresia without ventricular septal defect or severe pulmonary valve stenosis. Based on several earlier clinical studies, the cause of fetal pulmonary hypertension is premature closure of ductus arteriosus. The study by Yaman et al 15 confirmed this conclusion through animal experiments. Zhang et al 16 demonstrated through studies that premature closure of the fetal ductus arteriosus can cause 70% of the blood in the pulmonary artery unable to be excreted, resulting in an increase in pulmonary artery pressure and volume, followed by the overweight right ventricular systolic phase and severe tricuspid regurgitation with pericardial effusion. Based on the present study, when the systolic pressure of pulmonary artery increased in most fetuses in the middle and late stage, the ductus arteriosus was not completely closed, but it was also accompanied by a large number of rapid tricuspid regurgitation and severe pulmonary hypertension, which was highly associated with the increase of pulmonary vascular resistance and ductus arteriosus contraction. Our study suggested that the main evidence of increased pulmonary vascular resistance was the shorter peak value of branch blood flow becomes after the increase of fetal pulmonary artery pressure.
Related studies 17 have confirmed that pulmonary artery PASP of fetus in the middle- and late stage is closely linked to tricuspid regurgitation and regurgitation velocity. In clinical practice, the increase of fetal pulmonary artery pressure in the middle and late stage will inevitably increase the systolic pressure of the right ventricle, while the tricuspid in fetus of the middle and late stage is too weak to withstand regurgitation. If the fetal pulmonary artery pressure in the middle- and late stage increases to moderate or mild, tricuspid often occurs moderate or mild regurgitation, resulting in slight enlargement of the right atrium and right ventricle without affecting the right ventricular function, so the fetus is safe. In the current study, if the moderate or greater tricuspid regurgitation with >20 mmHg pressure difference, the fetuses should be followed up. If fetus in the middle- and late stage was not accompanied by the signs of right heart failure, such as pericardial effusion, heart rate acceleration, they should be maintained until the date of birth, with safe profile. If the pulmonary artery pressure continues to increase in the middle- and late stage of fetus, it must be closely observed. If tricuspid regurgitation in fetus was aggravated, accompanied by signs of right heart failure, such as pericardial effusion, increased heart rate with >70 mmHg transvalvular pressure difference, they should be closely observed until 35 weeks of pregnancy until birth. And early delivery would be recommended. Pulmonary circulation should be opened after neonatal crying to cause slow decline of pulmonary artery pressure, which help prevent heart failure of newborns. The aggregated results of this study showed that 52 cases in Group A were followed up, of which 40 cases (76.92%) had <50 mmHg fetal pulmonary artery PASP and disappeared tricuspid regurgitation or only mild regurgitation. 12 cases (23.08%) had severe PASP of ≥70 mmHg with signs of right heart failure, early delivery with 36–37 gestational weeks would be recommended. After birth, seven newborns returned to normal PASP, heart failure improved, two newborns returned to normal within 30 days, one newborn returned to normal within 90 days, and one newborn returned to normal within 106 days. Of the 12 cases, only 1 newborn had dyspnea due to persistent increase of pulmonary artery PASP and hypoxia. The patient was admitted to hospital and was given ventilator to help breathe, and discharged on the 21st day of admission and died on the 22nd day. The results are similar to those of Hosono et al 18 and Evans et al.. 19 In this study, the cause of neonatal death was hypoxia caused by incomplete opening of pulmonary circulation after birth, and persistent pulmonary hypertension induced by continuous increase of pulmonary vascular resistance. Considering some fetuses returned to normal before birth, there is no answer to the specific reasons. Based on our study, pulmonary artery PASP in most of fetus of the middle- and late stage returned to normal before birth, and the middle- and late-fetal pulmonary artery PASP was maintained at <50 mmHg, which may be related to endocrine disorders and transient oligohydramnios caused by mental stress in pregnant females. And PASP in fetuses of middle- and late stage maintained in 50–70mmHg until after birth. Additionally, it was closely related to incomplete opening of lung tissue, imperfect development of small pulmonary vessels and high vascular resistance. Therefore, further researches are warranted on the changes of fetal pulmonary hypertension. Admittedly, there are several limitations in this study. First, the pulmonary artery PASP of fetuses in the middle and late stage was evaluated based on the calculation of tricuspid regurgitation pressure difference. Considering the possibility of changed position, the angle between ultrasound beam and tricuspid regurgitation is too large, resulting in small results. It has a certain impact on the accuracy of pulmonary artery pressure measurement. Second, studies with larger sample size and longer follow-ups are required to confirm the current results.
Conclusions
Color Doppler echocardiography is able to clearly and accurately evaluate the tricuspid regurgitation velocity and tricuspid regurgitation in the middle- and late-stage fetus, which exerts advantages of simple operation, repeated detection, non-trauma and low price. It is considered to have important clinical value and significance in obstetrics. In addition, the aggregated results of this study demonstrated that, in most fetuses in the middle and late stage with mild-to-moderate tricuspid, the pulmonary artery PASP returned to normal regurgitation before birth. Most of the fetuses with more than 70 mmHg returned to normal, and only one case died after discharge. It was suggested that the middle- and late-stage fetuses with moderate or greater tricuspid regurgitation and with >20 mmHg regurgitation pressure difference should be followed up in clinic. If PASP was ≥70 mmHg with symptoms of right heart failure, fetuses should be closely observed until 35–36 weeks’ old to ensure fetal safety and early delivery would be recommended.
Footnotes
The authors Hong Cui and Juan Su contributed equally to the work.
Contributor Information
Hong Cui, Email: mifygf@163.com, Department of Ultrasound, Taian City Central Hospital, Taian, Shandong, China .
Juan Su, Email: htnzld@163.com, Department of Ultrasound, Taian City Central Hospital, Taian, Shandong, China .
Wen-Wen Liang, Email: hpywdm@163.com, Department of Ultrasound, Taian City Central Hospital, Taian, Shandong, China .
Hong-Ling Wang, Email: ntkpfe@163.com, Department of Ultrasound, Taian City Central Hospital, Taian, Shandong, China .
Hui-Feng Wang, Email: wanghuifeng0303@163.com, Department of Ultrasound, Taian City Central Hospital, Taian, Shandong, China .
REFERENCES
- 1. Yi Y, Tong T, Liu T, Lin Q, Xiong Y, Xu J . Prenatal diagnosis of idiopathic infantile arterial calcification without fetal hydrops . Echocardiography 2017. ; 34: 311 – 4 . doi: 10.1111/echo.13420 [DOI] [PubMed] [Google Scholar]
- 2. Yeo L, Romero R . Color and power Doppler combined with fetal intelligent navigation echocardiography (fine) to evaluate the fetal heart . Ultrasound Obstet Gynecol 2017. ; 50: 476 – 91 . doi: 10.1002/uog.17522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kumar Vikraman S, Chandra V, Balakrishnan B, Jaiman S, Batra M, Kannoly G . Unguarded tricuspid orifice---a rare cause of fetal right atrial dilatation with characteristic color doppler sign: Case report with review of literature . J Clin Ultrasound 2017. ; 45: 370 – 4 . doi: 10.1002/jcu.22416 [DOI] [PubMed] [Google Scholar]
- 4. Mauermann E, Vandenheuvel M, François K, Bouchez S, Wouters P . A novel Speckle-Tracking based method for quantifying tricuspid annular velocities in TEE . J Cardiothorac Vasc Anesth 2019. ; 33: 2636 – 44 . doi: 10.1053/j.jvca.2019.05.036 [DOI] [PubMed] [Google Scholar]
- 5. Zhan H, Liu C, Yin H . Follow-Up value of ultrasound in fetal tricuspid regurgitation Chinese . Journal of Ultrasonography 2014. ; 23: 979 – 82 . [Google Scholar]
- 6. Hu Q, Ren WD, Mao J, Li J, Qiao W, Bi WJ, et al. . Changes in pulmonary artery pressure during early transitional circulation in healthy full-term newborns . Ultrasonics 2015. ; 56: 524 – 9 . doi: 10.1016/j.ultras.2014.10.005 [DOI] [PubMed] [Google Scholar]
- 7. Blankenship W, Lind J, Arcilla RA . Atrial pressures and pulmonary circulation time in the newborn infant . Acta Paediatr Scand 1965. ; 54: 446 – 56 . doi: 10.1111/j.1651-2227.1965.tb06400.x [DOI] [PubMed] [Google Scholar]
- 8. Sukegawa S, Yamamoto Y, Sato K, Tanaka S, Tanaka T, Mitsuhashi N . Ultrasound evaluation of fetal critical aortic stenosis using the left atrium area/cardiac area ratio and the Doppler patterns in the pulmonary veins . J Med Ultrason 2019. ; 46: 267 – 72 . doi: 10.1007/s10396-018-0905-y [DOI] [PubMed] [Google Scholar]
- 9. Okazaki T, Nakazawa N, Ogasawara Y, Shoji H, Shimizu T, Makino S, et al. . Increase in fetal pulmonary artery diameters during late gestation is a predictor of outcome in congenital diaphragmatic hernia with liver herniation . J Pediatr Surg 2011. ; 46: 2254 – 9 . doi: 10.1016/j.jpedsurg.2011.09.010 [DOI] [PubMed] [Google Scholar]
- 10. Schmitz AJ, Weinzheimer HR, Fahnenstich H, Lê TP, Redel DA, Kowalewski S . Color Doppler echocardiographic evaluation of tricuspid regurgitation and systolic pulmonary artery pressure in the full-term and preterm newborn . Angiology 1997. ; 48: 725 – 34 . doi: 10.1177/000331979704800809 [DOI] [PubMed] [Google Scholar]
- 11. Tuo G, Volpe P, Buffi D, De Robertis V, Marasini M . Assessment of the ductus arteriosus in fetuses with tetralogy of Fallot and the implication for postnatal management . Congenit Heart Dis 2014. ; 9: 382 – 90 . doi: 10.1111/chd.12158 [DOI] [PubMed] [Google Scholar]
- 12. Zhan H, Yin H, Tao G, Xu F, Liu C . The follow-up observation on the abnormal elevation of fetal pulmonary artery systolic pressure at middle and late stages by Doppler echocardiography . Chinese Journal of Ultrasonography 2018. ; 27: 771 – 6 . [Google Scholar]
- 13. de Boode WP, Singh Y, Molnar Z, Schubert U, Savoia M, Sehgal A, et al. . Application of Neonatologist performed echocardiography in the assessment and management of persistent pulmonary hypertension of the newborn . Pediatr Res 2018. ; 84( Suppl 1 ): 68 – 77 . doi: 10.1038/s41390-018-0082-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Geipel A, Gembruch U . Screening performance of first trimester nuchal translucency, ductus venosus blood flow and tricuspid regurgitation for cardiac defects . Z Geburtshilfe Neonatol 2012. ; 216: 157 – 61 . doi: 10.1055/s-0032-1316345 [DOI] [PubMed] [Google Scholar]
- 15. Yaman C, Arzt W, Tulzer G, Tews G . Spontaneous constriction of the fetal ductus arteriosus . Z Geburtshilfe Neonatol 1999. ; 203: 44 – 6 . [PubMed] [Google Scholar]
- 16. Zhang Y, Zhao B, Liu Z, Cai J, Fan S . Clinical significance of constriction of the fetal ductus arteriosus diagnosed by echocardiography . Chinese Journal of Ultrasonography 2013. ; 22: 305 – 7 . [Google Scholar]
- 17. Müller S, Velik-Salchner C, Edlinger M, Bonaros N, Heinz A, Feuchtner G, et al. . Intracardiac Doppler echocardiography for monitoring of pulmonary artery pressures in high-risk patients undergoing transcatheter aortic valve replacement . J Am Soc Echocardiogr 2016. ; 29: 83 – 91 . doi: 10.1016/j.echo.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 18. Hosono T . Right ventricular flow dynamics in the early neonatal period assessed by pulsed Doppler echocardiography . J Cardiol 1987. ; 17: 895 – 905 . [PubMed] [Google Scholar]
- 19. Evans NJ, Archer LN . Postnatal circulatory adaptation in healthy term and preterm neonates . Arch Dis Child 1990. ; 65( 1 Spec No ): 24 – 6 . doi: 10.1136/adc.65.1_Spec_No.24 [DOI] [PMC free article] [PubMed] [Google Scholar]