Introduction
In the management of patients with chronic venous disease (CVD), compression therapies, in the form of stockings, wraps, and/or bandages, are an indispensable treatment option. Used as both primary therapy and adjunct before and after venous interventions, the aim of compression therapies is to provide support to the calf muscle pump and to reduce venous hypertension in the lower limbs. 1 On a macroscopic level, additional pressure provided by compression improves venous and lymphatic return, augmenting that which is already provided by the calf muscle pump system. 2
Graduated compression also has effects on microscopic changes related to CVD. Compression has been shown to reduce the levels of inflammatory markers found in the systemic circulation and plays a role in improving microcirculation within the skin, improving tissue oxygenation, and reducing the level of several cytokines which may help with preventing skin breakdown as well as with healing of venous leg ulceration.3–6 As shown in several studies, the use of compression treatment is also effective in the management of CVD symptoms including swelling. 7
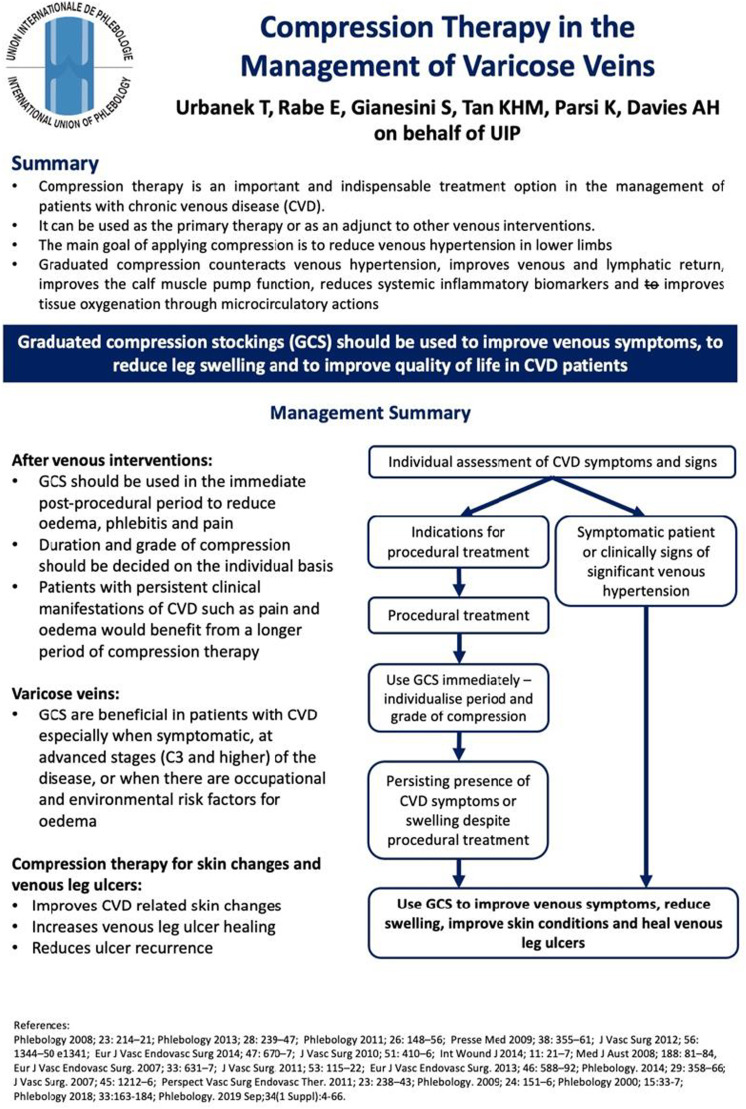
This one-page guideline from the International Union of Phlebology aims to highlight the use of compression therapy in the management of varicose veins. It summarises the indications for compression therapy and key clinical considerations that all medical professionals should remember when managing patients presenting with symptomatic CVD.
Management recommendations
It is recommended that graduated compression stockings (GCS) and other compression systems such as wraps and bandaging be used to improve symptoms, to reduce leg swelling, and to help improve quality of life in CVD patients. These may be applied as a primary treatment for symptomatic varicose veins (CEAP C2 disease), oedema related to varicose veins (C3), skin changes (C4), and active and healed venous ulceration (C5 and C6) and in the patients remaining symptomatic after venous interventions. Compression treatment also plays an important role in the avoidance of the local complications and swelling in the patients undergoing invasive varicose vein treatment.
Patients should undergo individualised assessment of CVD symptoms and signs. GCS may firstly be provided for symptomatic patients or on identification of clinical signs that are indicative of venous hypertension as primary treatment or as a temporalising measure whilst awaiting venous procedures. Compression therapy is recommended for symptomatic varicose veins,7,8 or more severe stages of disease (C3 and above). It has been shown to improve CVD-related skin changes, reduce the venous leg ulcer–related pain complains, improve venous leg ulcer healing rates, and reduce the risk of ulcer recurrence.9–12 For patients with C6 disease, it should be noted that compression therapy is not the only indicated therapy and should be offered alongside good wound care and superficial venous intervention as appropriate. Additionally, compression should be offered to patients with occupational (e.g. occupations that require long durations of standing) or environmental risk factors for oedema. 13
Should patients undergo procedural treatment, GCS should be provided immediately post-procedure.14–19 This is recommended to help reduce post-procedural pain, oedema, and phlebitis. To increase the local pressure in these clinical settings, an additional eccentric compression to enhance the compression effectiveness can be applied. 20 Grade of compression and duration of therapy should be individualised, and patients with persistent clinical manifestations of CVD (e.g. oedema, pain) despite treatment would benefit from higher grades and longer durations of compression therapy. 21 There is no strong evidence that any specific form of compression therapy is better post-intervention, although studies have suggested that stockings may be more acceptable to patients. 22
Discussion
This article provides a one-page clinical practice guideline summarising compression therapy for the management of VVs. It is part of a series of publications for the UIP One-Page Guidelines which are aimed at ensuring that patients with venous disease receive timely and appropriate care based on current best evidence and expert consensus and in line with other guidelines and consensus documents from other institutions (Figure 1). 21
Figure 1.
The one-page guideline.
While it is undeniable that compression plays a large role in the management of all manifestations of CVD, the evidence in the current literature largely focuses on the efficacy of the compression in the venous leg ulcer treatment and recurrence prevention, the comparisons between compression and interventional treatment as well as the use of the periprocedural compression treatment in the patients undergoing invasive treatment of the chronic venous disease.18,23,24 Post-procedural compression is widely practiced and is recommended in this document, with compression type and duration to be individualised based on patient characteristics and symptom profile. While patients with symptoms such as pain and oedema that persist after venous intervention should be provided with compression for longer durations, the length of compression treatment is very much dependent on clinician zeitgeist before further treatment is considered or offered to this patient population.
Additionally, fewer studies, which are in the majority largely observational in design, have focused on the isolated effect of compression on symptomatic varicose veins when compared to no treatment.25,26 These studies, while undoubtedly showing a potential benefit of compression stockings, also fail to determine if these improvements are cost-effective due to the lack of health-related quality of life measures used. Due to often symptomatic CVD disease course, in many patients prolonged use of the medical compression stocking is advised. The question if asymptomatic CVD patients (e.g. C1 or C2) should be treated by compression to avoid disease progression is still open for the discussion. Despite an influence on the venous hypertension decrease, there are no well-designed studies available focusing on an influence of the compression on the CVD progression and no EBM recommendation can be made and proposed in this particular indication. A well-designed large randomised clinical trial with head-to-head comparison would be useful in clarifying these deficits in the literature.
It is also important to note that while compression has been shown to be useful in the management of CVD, it is only useful if patients are able to tolerate and comply to the compression regimen. Poor compliance to compression has been reported widely in the literature, with reasons for non-compliance including discomfort, difficulty putting compression on, and itchiness. 27 Improving adherence improves outcomes related to CVD, but no intervention has been shown to consistently improve compliance to compression. 28 Further work to understand the pitfalls of compression and develop multi-dimensional strategies to improve adherence is clearly required to maximise the benefit of compression therapies. The growing research and experience concerning the use of compression also increased the current knowledge on the potential contraindications to the compression treatment. In candidate for compression therapy, the subject of potential lack of the compliance, together with presence of the potential contraindications should be assessed. This in turn can potentially decrease the risk of the compression complications as well as allow to choose the optimal way to provide compression therapy for the individual patient. 29
Footnotes
Author contributions: K.P. and A.H.D. conceptualised the design of the short report and one-page guideline. T.U., E.R., and S.G. contributed to the literature review and formulation of the recommendations. M.T. contributed to the formatting and layout of the one-page guideline (Figure 1) and wrote the initial draft of the short report. All authors reviewed the short report prior to submission.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: Professor Alun Davies on behalf of the UIP.
ORCID iDs
Matthew Tan https://orcid.org/0000-0002-5789-0353
Sergio Gianesini https://orcid.org/0000-0002-0440-5975
Kurosh Parsi https://orcid.org/0000-0003-0630-8877
Alun H Davies https://orcid.org/0000-0001-5261-6913
References
- 1.Blättler W, Kreis N, Lun B, et al. Leg symptoms of healthy people and their treatment with compression hosiery. Phlebology 2008; 23(5): 214–221. [DOI] [PubMed] [Google Scholar]
- 2.Blazek C, Amsler F, Blaettler W, et al. Compression hosiery for occupational leg symptoms and leg volume: a randomized crossover trial in a cohort of hairdressers. Phlebology 2013; 28(5): 239–247. [DOI] [PubMed] [Google Scholar]
- 3.Abu-Own A, Shami SK, Chittenden SJ, et al. Microangiopathy of the skin and the effect of leg compression in patients with chronic venous insufficiency. J Vasc Surg 1994; 19(6): 1074–1083. [DOI] [PubMed] [Google Scholar]
- 4.Castro-Ferreira R, Cardoso R, Leite-Moreira A, et al. The role of endothelial dysfunction and inflammation in chronic venous disease. Ann Vasc Surg 2018; 46: 380–393. [DOI] [PubMed] [Google Scholar]
- 5.Murphy MA, Joyce WP, Condron C, et al. A reduction in serum cytokine levels parallels healing of venous ulcers in patients undergoing compression therapy. Eur J Vasc Endovasc Surg 2002; 23: 349–352. [DOI] [PubMed] [Google Scholar]
- 6.Beidler S, Douillet C, Berndt D, et al. Multiplexed analysis of matrix metalloproteinases in leg ulcer tissue of patients with chronic venous insufficiency before and after compression therapy Wound Repair Regen. 2008;16: 642–648 [DOI] [PubMed] [Google Scholar]
- 7.Biswas S, Clark A, Shields DA. Randomised clinical trial of the duration of compression therapy after varicose vein surgery. Eur J Vasc Endovasc Surg 2007; 33(5): 631–637. [DOI] [PubMed] [Google Scholar]
- 8.Couzan S, Assante C, Laporte S, et al. Booster study: comparative evaluation of a new concept of elastic stockings in mild venous insufficiency. Presse Medicale (Paris, France: 1983). 2008;38(3):355-361. [DOI] [PubMed] [Google Scholar]
- 9.Brizzio E, Amsler F, Lun B, et al. Comparison of low-strength compression stockings with bandages for the treatment of recalcitrant venous ulcers. J Vasc Surg 2010; 51(2): 410–416. [DOI] [PubMed] [Google Scholar]
- 10.Finlayson KJ, Courtney MD, Gibb MA, et al. The effectiveness of a four-layer compression bandage system in comparison with class 3 compression hosiery on healing and quality of life in patients with venous leg ulcers: a randomised controlled trial. Int Wound J 2014; 11(1): 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Couzan S, Leizorovicz A, Laporte S, et al. A randomized double-blind trial of upward progressive versus degressive compressive stockings in patients with moderate to severe chronic venous insufficiency. J Vasc Surg 2012; 56(5): 1344–1350. [DOI] [PubMed] [Google Scholar]
- 12.Vandongen YK, Stacey MC. Graduated compression elastic stockings reduce lipodermatosclerosis and ulcer recurrence. Phlebology 2000; 15(1): 33–37. [Google Scholar]
- 13.Hagan MJ, Lambert SM. A randomised crossover study of low ankle pressure graduated compression tights in reducing flight induced ankle oedema. Medical journal of Australia 2008; 188(2): 81–84. [DOI] [PubMed] [Google Scholar]
- 14.Mariani F, Marone EM, Gasbarro V, et al. Multicenter randomized trial comparing compression with elastic stocking versus bandage after surgery for varicose veins. J Vasc Surg 2011; 53(1): 115–122. [DOI] [PubMed] [Google Scholar]
- 15.Bakker NA, Schieven LW, Bruins RM, et al. Compression stockings after endovenous laser ablation of the great saphenous vein: a prospective randomized controlled trial. Eur J Vasc Endovasc Surg 2013; 46(5): 588–592. [DOI] [PubMed] [Google Scholar]
- 16.Reich-Schupke S, Feldhaus F, Altmeyer P, et al. Efficacy and comfort of medical compression stockings with low and moderate pressure six weeks after vein surgery. Phlebology 2014; 29(6): 358–366. [DOI] [PubMed] [Google Scholar]
- 17.Kern P, Ramelet AA, Wütschert R, et al. Compression after sclerotherapy for telangiectasias and reticular leg veins: a randomized controlled study. J Vasc Surg 2007; 45(6): 1212–1216. [DOI] [PubMed] [Google Scholar]
- 18.Benigni JP, Allaert FA, Desoutter P, et al. The efficiency of pain control using a thigh pad under the elastic stocking in patients following venous stripping: results of a case–control study. Perspect Vasc Surg Endovasc Ther 2011; 23(4): 238–243. [DOI] [PubMed] [Google Scholar]
- 19.Lugli M, Cogo A, Guerzoni S, et al. Effects of eccentric compression by a crossed-tape technique after endovenous laser ablation of the great saphenous vein: a randomized study. Phlebology 2009; 24(4): 151–156. [DOI] [PubMed] [Google Scholar]
- 20.Mosti G, Mattaliano V, Arleo S, et al. Thigh compression after great saphenous surgery is more effective with high pressure. Int Angiol 2009; 28: 274–280. [PubMed] [Google Scholar]
- 21.Rabe E, Partsch H, Hafner J, et al. Indications for medical compression stockings in venous and lymphatic disorders: an evidence-based consensus statement. Phlebology 2018; 33(3): 163–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim CS, Davies AH. Graduated compression stockings. CMAJ (Can Med Assoc J) 2014; 186(10): E391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schul MW, Eaton T, Erdman B. Compression versus sclerotherapy for patients with isolated refluxing reticular veins and telangiectasia: a randomized trial comparing quality-of-life outcomes. Phlebology 2011; 26(4): 148–156. [DOI] [PubMed] [Google Scholar]
- 24.Sell H, Vikatmaa P, Albäck A, et al. Compression therapy versus surgery in the treatment of patients with varicose veins: a RCT. Eur J Vasc Endovasc Surg 2014; 47(6): 670–677. [DOI] [PubMed] [Google Scholar]
- 25.National Clinical Guideline Centre (UK) . Varicose veins in the legs: the diagnosis and management of varicose veins. London: National Institute for Health and Care Excellence (NICE), 2013. (NICE Clinical Guidelines, No. 168.) 8, Conservative Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK328015/ [PubMed] [Google Scholar]
- 26.Kakkos SK, Timpilis M, Patrinos P, et al. Acute effects of graduated elastic compression stockings in patients with symptomatic varicose veins: a randomised double blind placebo controlled trial. Eur J Vasc Endovasc Surg 2018; 55(1): 118–125. [DOI] [PubMed] [Google Scholar]
- 27.Ayala A, Guerra JD, Ulloa JH, et al. Compliance with compression therapy in primary chronic venous disease: results from a tropical country. Phlebology 2019; 34(4): 272–277. [DOI] [PubMed] [Google Scholar]
- 28.Bar L, Brandis S, Marks D. Improving adherence to wearing compression stockings for chronic venous insufficiency and venous leg ulcers: a scoping review. Patient Prefer Adherence 2021: 2085–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rabe E, Partsch H, Morrison N, et al. Risks and contraindications of medical compression treatment - a critical reappraisal. An international consensus statement. Phlebology 2020; 35(7): 447–460. [DOI] [PMC free article] [PubMed] [Google Scholar]