Abstract
Background and Aims:
Multiple sources of medical oxygen, namely liquid medical oxygen (LMO) tanks, pressure swing adsorption (PSA) plants, concentrators, and gaseous cylinders, are available at different healthcare facilities. These sources of oxygen have varying installation and operational costs. In low-resource settings, it is imperative to utilise these assets optimally. This study investigated the operational costs of multiple oxygen sources available at a healthcare facility.
Methods:
A Microsoft (MS) Excel-based model was developed to analyse and compare the oxygen manufacturing costs (in ₹/m3) using PSA plants and procurement costs (in ₹/m3) of LMO and third-party vendor-refilled cylinders.
Results:
The oxygen manufacturing costs for PSA plants of different capacities and running times on electricity and diesel generators (DGs) as a power source were calculated. This study highlights the cost-benefit of using PSA plants over LMO and third-party vendor-refilled cylinders as a source of oxygen. PSA plants are most economical when they are of higher capacity and used to their maximum capacity on electricity as the power source. On the contrary, they are most expensive when used on a DG set as a power source. Furthermore, this study provides evidence of PSA plants being more cost-effective for refilling cylinders using a booster compressor unit when compared to third-party vendor-cylinder refilling.
Conclusion:
Given their cost-effectiveness and low third-party dependence, they should be utilised to their maximum capacity as medical oxygen sources at healthcare facilities.
Keywords: Booster compressor units, cost analysis, gaseous cylinders, hospitals, liquid medical oxygen, medical oxygen, pressure swing adsorption plants
INTRODUCTION
Oxygen therapy is an essential component of clinical treatment and healthcare systems. Medical oxygen is either manufactured in liquid form with a purity of approximately 99.5%, or it can be manufactured in gaseous form with a purity of 90% or more.[1] It is free from dust particles, carbon particles, oil particles, moisture, bacteria, viruses, and fungi. It is transported and stored in medical-grade equipment such as liquid medical oxygen (LMO) tankers, LMO tanks, and medical oxygen gaseous cylinders. The most common storage sources of medical oxygen in healthcare facilities are compressed gas cylinders and LMO tanks. In contrast, oxygen concentrators and pressure swing adsorption (PSA) plants are the most common manufacturing sources.[2,3]
Since the commissioning of these PSA plants, many state governments and other stakeholders have been expressing concerns over the ‘high costs’ incurred in their operations, including electricity bills and costs of fuel for diesel generator (DG) sets, among other expenses. This has thus led to a perception that PSA plants are an expensive source of oxygen for a facility without evidence. The current study aimed to address this gap in the literature to investigate and compare the operational costs of PSA plants with the procurement (refilling) costs of LMO and jumbo cylinders (also known as D-type cylinders). A single indicator, oxygen production or procurement cost in Indian rupee/cubic metre (₹/m3), was considered.
METHODS
This study did not involve human subjects; therefore, ethical approval was not sought from an institutional review board, and the study was not registered on the Clinical Trials Registry-India. First, a Microsoft (MS) Excel-based model was developed to calculate medical oxygen production cost per cubic metre (in ₹/m3) by using PSA plants of different capacities running for various hours in the day on either electricity or DG set or both. The model included multiple inputs such as the unit price of electricity, price of diesel, human resource (HR) costs, annual comprehensive maintenance costs (which is approximately 5%–7% of the PSA plant procurement cost), and oxygen testing from National Accreditation Board for Testing and Calibration Laboratories-approved laboratory costs. The model was based on specifications data of PSA plants as provided by Absstem Technologies, Delhi, India [Tables S1 and S2]. In addition, for comparison with LMO and jumbo cylinders, the model included the rate contract costs (including transportation costs) and HR costs for these two sources.
Table S1:
Compressor capacity, annual CMC, and DG set capacity of various PSA plants
| PSA Plant Capacity (LPM) | Compressor Capacity (kWh)* | Annual CMC Cost (₹)† | DG Set Capacity (kVa)‡ |
|---|---|---|---|
| 100 | 11 | 350,000 | 30 |
| 200 | 15 | 400,000 | 41 |
| 400 | 30 | 500,000 | 81 |
| 500 | 37 | 550,000 | 100 |
| 800 | 55 | 650,000 | 149 |
| 1000 | 75 | 720,000 | 203 |
| 1200 | 90 | 800,000 | 243 |
| 1500 | 110 | 850,000 | 297 |
| 2000 | 150 | 930,000 | 405 |
| 2500 | 200 | 950,000 | 540 |
| 3200 | 220 | 1,100,000 | 594 |
*The compressor capacity may vary marginally among various PSA plant models. †The annual CMC costs may vary marginally among various PSA plant suppliers. ‡The DG set capacity may vary marginally among various PSA plant models. In this study, the DG set capacity has been assumed to be 2.7 times the compressor capacity. CMC – Comprehensive Maintenance Contract; DG – Diesel Generator; PSA – Pressure Swing Adsorption; LPM – Litres Per Minute
Table S2:
Jumbo cylinder (JC) refilling capacity and refilling booster capacity of various PSA plants
| PSA Plant Capacity (LPM) | Refilling Capacity (JC/day)* | Refilling Booster Capacity (kWh)† |
|---|---|---|
| 100 | 15 | 2.5 |
| 200 | 31 | 5 |
| 400 | 62 | 10 |
| 500 | 77 | 12.5 |
| 800 | 123 | 20 |
| 1000 | 154 | 25 |
| 1200 | 185 | 30 |
| 1500 | 231 | 35 |
| 2000 | 309 | 50 |
| 2500 | 386 | 60 |
| 3200 | 494 | 80 |
*The cylinder refilling capacity (jumbo cylinders (JC)/day) may vary marginally among various PSA plant models. In this study, the refilling capacity has been assumed to be 75% of the total PSA plant capacity. †The refilling booster capacity (kWh) may vary marginally among various PSA plant models. JC – Jumbo Cylinders; PSA – Pressure Swing Adsorption; LPM – Litres Per Minute
While building the model, based on the data provided by Absstem Technologies (Delhi, India), the following key considerations were kept in mind:
Minimum compressor load of 40% if the PSA plant is utilised for less than 10 h/day.
2.7 as the factor to calculate the DG set capacity based on the PSA plant compressor capacity
4.16 as the factor to calculate the volume of diesel required (in litres) per hour to run the DG set
Once the model was developed, relevant input data on electricity unit price, cylinder refilling, and LMO refilling costs were collected telephonically from oxygen nodal persons/technicians/operators in hospitals (n = 6) in Madhya Pradesh. The lead author verified the data over one week in January 2023 through consultations with the Directorate of Health Services, Government of Madhya Pradesh, on the established LMO, gaseous oxygen cylinder refilling rate contracts, and electricity unit prices. The inclusion and exclusion criteria for the hospitals have also been provided [Table S3], along with details on the model input parameters [Table S4]. The collected model input data have been expressed as mean (standard deviation (SD)) for electricity unit price and rate contracts (including transportation costs) for LMO and cylinder refilling [Table S4]. A uniform HR cost for all three oxygen sources was assumed in the model. Relative change and relative difference methods were used to compare the operational costs of PSA plants and the procurement (refilling) costs of LMO and jumbo cylinders.
Table S3:
Hospital inclusion and exclusion criteria
| Criteria | Description | |
|---|---|---|
| Inclusion | • | Public hospitals |
| • | Hospitals with all three sources of oxygen – LMO tank, PSA plants, and cylinder manifold | |
| Exclusion | • | Private hospitals |
| • | Hospitals that did not have all three sources of oxygen | |
LMO-Liquid Medical Oxygen; PSA-Pressure Swing Adsorption
Table S4:
Model input parameters
| PSA Plant | |
|---|---|
| Electricity cost (Mean (SD)) | ₹ 9.59 (1.79)/kWh* |
| Diesel cost | ₹ 90/L† |
| HR costs | ₹ 36,000/month for three operators/day at ₹ 12,000 per month‡ |
| Oxygen NABL testing cost | ₹ 60,000/year (four tests costing ₹ 15,000 each) |
|
| |
| Jumbo Cylinder | |
|
| |
| Refilling rate contract (including transportation costs) (Mean (SD)) | ₹ 336.67 (52.12)/cylinder§ |
| HR costs | ₹ 36,000/month for three operators/day at ₹ 12,000 per month‡ |
|
| |
| LMO | |
|
| |
| Refilling rate contract (including transportation costs) (Mean (SD)) | ₹ 39.5 (11.26)/m3|| |
| HR costs | ₹ 36,000/month for three operators/day at ₹ 12,000 per month‡ |
*The cost of electricity may vary among states, and it also may vary between rural and urban areas. †The cost of retail diesel is subject to the crude price, which is a volatile index. It is subject to change on a daily basis. ‡The HR costs may vary marginally within a state. §The cost of cylinder refilling may vary among states, and it also may vary between districts based on the distance between the cylinder refiller and the hospital. The cylinder refilling costs also fluctuate based on the demand. ||The cost of LMO refilling may vary among states and it also may vary between districts based on the distance between the LMO manufacturer and the hospital. The costs may also fluctuate based on the demand. LMO tank rental and maintenance costs have not been included. PSA – Pressure Swing Adsorption; HR – Human Resource; NABL – National Accreditation Board for Testing and Calibration Laboratories; LMO – Liquid Medical Oxygen; SD – Standard deviation
RESULTS
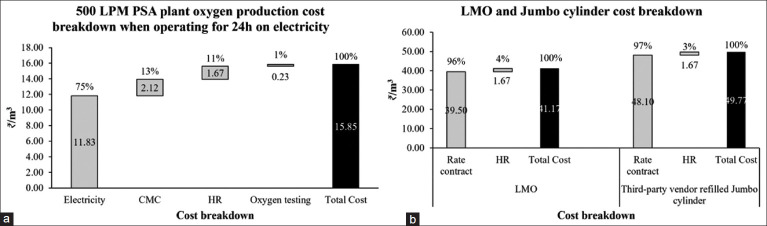
The MS Excel-based cost analysis model illustrates the per cubic metre cost (₹/m3) of oxygen from different sources for a hospital [Figure 1]. A PSA plant capacity of 500 litres per minute (LPM) has been considered, with a running time of 24 h/day. With usage/production of about 21,600 m3 in a month, the ₹/m3 costs of oxygen for LMO refilling and third-party vendor-refilled jumbo cylinders were calculated to be 2.59 and 3.13 times higher than PSA plant (when operating only on electricity), respectively.
Figure 1:
Cost comparison of oxygen sources. Error bars indicate SD (n = 6). LPM – Litres Per Minute; PSA – Pressure Swing Adsorption; LMO – Liquid Medical Oxygen; SD – Standard Deviation
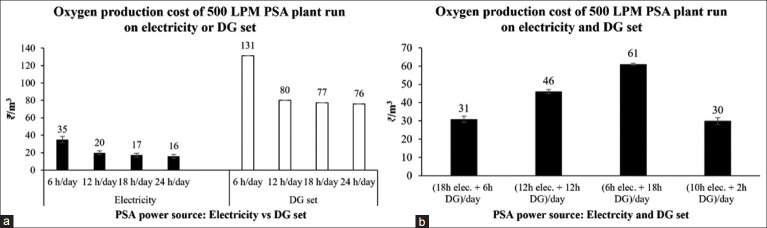
The overall monthly costs and the breakdown of oxygen production/procurement and delivery costs (electricity, HR, maintenance, etc.) for each source of oxygen were calculated [Table 1 and Figure 2].
Table 1:
Monthly cost for each source (in ₹)
| 500 LPM PSA plant (24 h on electricity) | LMO | Jumbo cylinders refilled by third-party vendor | |
|---|---|---|---|
| Volume of Oxygen (m3) | 21,600 | 21,600 | 21,600 (~3085 cylinders) |
| Electricity cost (₹/month) | 255,477 | NA | NA |
| CMC cost (₹/month) | 45,833 | 0 | 0 |
| HR cost (₹/month) | 36,000 | 36,000 | 36,000 |
| Oxygen testing cost (₹/month) | 5,000 | 0 | 0 |
| Procurement cost (₹/month) | 0 | 853,200 | 1,038,867 |
| Total cost (₹/month) | 342,311 | 889,200 | 1,074,867 |
LPM – Litres Per Minute; PSA – Pressure Swing Adsorption; LMO – Liquid Medical Oxygen; NA – Not Applicable; CMC – Comprehensive Maintenance Contract (CMC); HR – Human Resource
Figure 2:
Oxygen production/procurement and delivery cost breakdown (a) 500 LPM PSA plant (b) LMO and Jumbo cylinder. LPM – Litres Per Minute. PSA – Pressure Swing Adsorption; CMC – Comprehensive Maintenance Contract; HR – Human Resource; LMO – Liquid Medical Oxygen
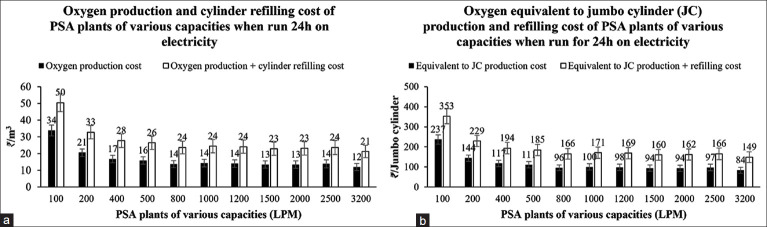
Post coronavirus disease (COVID)-19 second wave, the demand for medical oxygen has drastically decreased, and PSA plants are not running continuously over the day. Thus, the model was also used to calculate and compare the cost (₹/m3) of oxygen production when PSA plants are used at various capacities such as 25% (6 h/day), 50% (12 h/day), and 75% (18 h/day). Moreover, it was assumed that the cost of producing oxygen from PSA plants would vary depending on the source of power (electricity only, DG set only, or combined).
The per m3 cost of oxygen production is the lowest when PSA plants operate entirely on electricity and at 100% capacity (24 h/day) [Figure 3a]. However, if the PSA plant utilisation is only 25%, then the per m3 cost of production increases by 118.7%. On the contrary, when comparing the cost of oxygen production between only electricity and only DG set as the power source at 100% utilisation, the DG set is found to be 4.75 times more expensive than the PSA plant on electricity, 1.84 times more expensive than LMO refilling, and 1.52 times more expensive than jumbo cylinder refilling, which makes oxygen generation with only DG set as the most expensive source of medical oxygen in a health facility. Furthermore, assuming a 12-h daily utilisation of PSA plants, of which 10-h operation is using electricity and two hours is using DG set as the power source, the cost of oxygen production is ₹ 30 per m3, which is approximately 42% lower than jumbo cylinder refilling (₹ 51.43 per m3, data not shown) [Figure 3b].
Figure 3:
500 LPM PSA plant oxygen production costs (a) when run on only electricity or only DG set (b) when run in combination with both electricity and diesel generator for different running times. Error bars indicate SD (n = 6). LPM – Litres Per Minute; PSA – Pressure Swing Adsorption; DG – Diesel Generator; SD – Standard Deviation
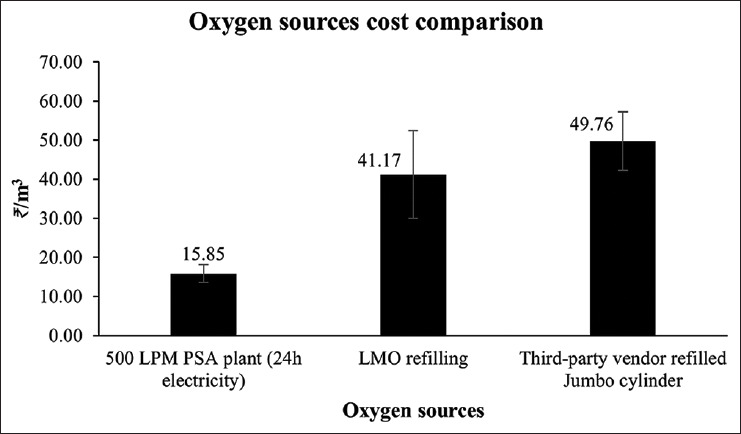
PSA plants can also be used to refill cylinders. It can be stated that the higher the capacity of the PSA plant, the cheaper the cost of oxygen manufacturing and cylinder refilling [Figure 4a]. When PSA plants operate at full daily capacity, the cost (₹/m3) of oxygen manufacturing and refilling from 100 LPM PSA plants is 2.83 and 2.37 times higher than 3200 LPM PSA plants, respectively. Moreover, for 1000 LPM and 2000 LPM PSA plants, the per m3 oxygen manufacturing cost is ₹14 and ₹13, respectively. In addition, it can be stated that the average increase in cost from oxygen production to oxygen refilling (equivalent to a Jumbo cylinder) is about 67% for PSA plants of various capacities [Figure 4b]. Furthermore, the third-party vendor cylinder refilling is approximately 1.88 times more expensive than on-site cylinder refilling using a 500 LPM plant [Table 2].
Figure 4:
Oxygen production and cylinder refilling cost from PSA plants of different capacities running for 24 hours daily on electricity (a) ₹/m3 (b) ₹/Jumbo cylinder. Error bars indicate SD (n = 6). PSA – Pressure Swing Adsorption; LPM – Litres Per Minute; JC – Jumbo Cylinder; SD – Standard Deviation
Table 2:
Equivalent jumbo cylinder costs from various sources of oxygen
| Jumbo Cylinder Refilling Type | Equivalent Jumbo Cylinder Cost (₹) |
|---|---|
| PSA plant (500 LPM, 24 h on electricity) | 110.93 |
| LMO refilling | 288.17 |
| Third-party vendor cylinder refilling | 348.34 |
| Onsite refilling with 500 LPM PSA plant (24 h on electricity) | 185.21 |
PSA – Pressure Swing Adsorption; LPM – Litres Per Minute; LMO – Liquid Medical Oxygen
DISCUSSION
Optimising the utilisation of oxygen sources is paramount to having a resilient medical oxygen ecosystem in a healthcare facility. The utilisation would depend on the system’s safety, continuity, ease of use, strength, and financial viability.[2,4,5] The model developed in this study can evaluate the economic impact of using electricity versus the DG set for running the PSA plant. The model can also investigate the cost implications of refilling cylinders with PSA plants. This study highlights the cost-benefit of using PSA plants over LMO and third-party vendor-refilled cylinders as a source of oxygen. It illustrates that the PSA plants are most economical when they are of higher capacity and used to their maximum capacity, with electricity as the power source. On the contrary, PSA plants are the most expensive source of oxygen when operating using a DG set. The model also suggests that if only electricity is the power source for a PSA plant, then for it to be cost-effective for manufacturing oxygen, it should be run for a minimum of 10 h/day if its capacity is lower than 200 LPM and for a minimum 5 h/day otherwise. If the PSA plant is also being used for refilling cylinders using electricity, it should be run for a minimum of 18 h/day if its capacity is lower than 200 LPM and for a minimum of 8 h/day otherwise. However, as PSA plants in India are most likely to be run on both electricity and DG sets due to intermittent power supply, the cost of oxygen production would be between PSA plant costs running entirely on electricity and PSA plant costs running entirely with DG set. Therefore, the model also illustrates that if a PSA plant of less than 200 LPM capacity must be run for 24 h/day with both electricity and DG set as the power sources, then for it to be cost-effective for manufacturing, it should be run for less than 2 h/day on DG set and for refilling, it should not be run at all on DG set. On the contrary, if the capacity is more significant than 200 LPM, running with DG set should not exceed 9 h (37%) for manufacturing and 3 h (10%) for refilling. In this study, the optimal running time on the DG set was also investigated, that is, if the maximum running time for a PSA plant is 12 h/day. It was found that if the capacity is less than 200 LPM, it should not be used on the DG set at all for either manufacturing or refilling cylinders; however, if the capacity is more significant than 200 LPM, the utilisation with the DG set should be less than 4 h (out of the total 12 h) for manufacturing and less than 1 h for refilling [Table S5]. It is worth noting that the model output is highly sensitive to the input parameters such as electricity and diesel price and LMO and cylinder refilling rate contracts (including transportation costs). Because many PSA plants have already been installed and commissioned, their utilisation can be enhanced by installing a booster compressor (bottling unit) for onsite refilling of jumbo cylinders.
Table S5:
PSA plants' number of hours of operation on electricity and DG set for their cost-effective utilisation
| PSA plant capacity (LPM) | Minimum no. of h/day when used only with electricity | Maximum no. of h/day on DG set when used for 24 h/day | Maximum no. of hours on DG set if used for 12 h/day | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Manufacturing (h/day) | Manufacturing + Cylinder Refilling (h/day) | Manufacturing (h/day) | Manufacturing + Cylinder Refilling (h/day) | Manufacturing (h/day) | Manufacturing + Cylinder Refilling (h/day) | |
| 100 | 10 | 18 | 2 | 0 | 0 | 0 |
| 200 | 6 | 10 | 8 | 1 | 2 | 0 |
| 400 | 5 | 8 | 8 | 2 | 3 | 0 |
| 500 | 5 | 8 | 8 | 2 | 3 | 1 |
| 800 | 5 | 8 | 9 | 3 | 4 | 1 |
| 1000 | 5 | 8 | 9 | 3 | 4 | 1 |
| 1200 | 5 | 8 | 9 | 3 | 4 | 1 |
| 1500 | 5 | 8 | 9 | 3 | 4 | 1 |
| 2000 | 5 | 8 | 9 | 3 | 4 | 1 |
| 2500 | 5 | 8 | 9 | 3 | 4 | 1 |
| 3200 | 5 | 8 | 9 | 3 | 4 | 1 |
LPM – Litres per minute; PSA – Pressure Swing Adsorption; DG – Diesel generator
Smith et al.[6] have illustrated that PSA plant-based social enterprise models are a viable and sustainable strategy for changing the landscape of oxygen access for needy patients. In addition, a 2021 report by the Institute for Transformative Technologies (ITT) and Oxygen Hub illustrated the cost of oxygen manufacturing using different technologies, including PSA plants in sub-Saharan Africa.[7] Furthermore, Aljaghoub et al.[8] conducted a comparative analysis of various oxygen production techniques, such as cryogenic separation, PSA, and membrane technology. They ranked membrane technology as the top production method based on its positive social and environmental impact. Moreover, Balys et al.[9] illustrated a significant reduction in oxygen procurement costs due to on-site production with PSA plants in Poland. In addition, Bhat et al.[10] and Madaan et al.[11] discussed different sources of medical oxygen available at hospitals in India; however, the authors did not explicitly present the cost-benefit analysis of various medical oxygen sources. Moreover, Bradley et al.[12] developed a cost-effectiveness model for comparing concentrators and cylinders with intermittent power in low-resource healthcare facilities. They concluded that storing energy in batteries provided better cost optimisation. Bradley et al.[13] also conducted an in-depth comparative cost analysis between five oxygen supply technologies. They found concentrators to be the most effective option, followed by the low-pressure commercial generation system. McAllister et al.[14] analysed the cost of using oxygen concentrators versus cylinders. They revealed that having a minimum number of concentrators with cylinder backup costs only 55% of the average existing cost.
This study does have limitations. The model did not account for approximately 5% of oxygen wastage in oxygen cylinders due to residual pressure (<10 bar) or the wastage in LMO tanks due to evaporation.[15,16] In addition, for cost analysis, the model only considers the operational costs of oxygen sources. However, to estimate the actual economic impact on the sustainability of using various sources of oxygen, installation and operating costs should be considered, along with the break-even analysis. In addition, the transportation costs for oxygen cylinders refilled by PSA plants could be included.
CONCLUSION
The study highlights that the PSA plants are the most economical when they are of higher capacity and used to their maximum capacity on electricity as the power source. They are the most expensive when used on a DG set as a power source. Furthermore, the study provides evidence of PSA plants being more cost-effective for refilling cylinders using a booster compressor unit when compared to third-party vendor-cylinder refilling.
Study data availability
De-identified data may be requested with reasonable justification from the authors (email to the corresponding author) and shall be shared upon request.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Geneva: World Health Organization; 2023. Foundations of Medical Oxygen Systems; pp. 1–80. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Clinical-Oxygen-2023.1 . [Google Scholar]
- 2.World Health Organization. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF); 2019. WHO-UNICEF Technical Specifications and Guidance for Oxygen Therapy Devices; pp. 1–149. Available from: https://www.who.int/publications/i/item/9789241516914 . [Google Scholar]
- 3.nhsrcindia.org [homepage on the Internet] National Health Systems Resource Centre (NHSRC) c2023. Available from: https://nhsrcindia.org/sites/default/files/2021-09/Guidance%20Note%20on%20LMO%20Storage%20Tanks%20as%20on%2003082021%20%281%29.pdf. [Last accessed on 2023 Apr 10]
- 4.Haque E, Tarek SA, Sarker F, Haque MA, Mamun KA. A systematic review on medical oxygen ecosystem: Current state and recent advancements. medRxiv. 2022:1–25. doi: 10.1101/2022.10.23.22281394. [Google Scholar]
- 5.peso.gov.in [homepage on the Internet] Petroleum and Explosives Safety Organization (PESO) c2023. Available from: https://peso.gov.in/web/gas-cylinder-rules-2016. [Last accessed on 2023 Apr 12]
- 6.Smith V, Changoor A, McDonald C, Barash D, Olayo B, Adudans S, et al. A comprehensive approach to medical oxygen ecosystem building: An implementation case study in Kenya, Rwanda, and Ethiopia. Global Health Sci Pract. 2022;10:1–14. doi: 10.9745/GHSP-D-21-00781. doi: 10.9745/GHSP-D-21-00781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Closing the Medical Oxygen Gap in Sub-Saharan Africa: A Case for a Decentralized Hub-Spoke Network of Pressure Swing Adsorption Plants. Institute for Transformative Technologies (ITT) and Oxygen Hub. 2021. pp. 1–29. Available from: https://oxygenhub.org/wp-content/uploads/2021/01/ClosingO2GapinSSA.pdf .
- 8.Aljaghoub H, Alasad S, Alashkar A, AlMallahi M, Hasan R, Obaideen K, et al. Comparative analysis of various oxygen production techniques using multi-criteria decision-making methods. Int J Thermofluids. 2023;17:1–9. [Google Scholar]
- 9.Bałys M, Brodawka E, Korzeniewska A, Szczurowski J, Zarębska K. LCA and economic study on the local oxygen supply in Central Europe during the COVID-19 pandemic. Sci Total Environ. 2021;786:1–14. doi: 10.1016/j.scitotenv.2021.147401. doi: 10.1016/j.scitotenv. 2021.147401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhat N, Moses V, Chetan N. Economical synthesis of oxygen to combat the COVID-19 pandemic. Hygiene Environ Health Adv. 2023;6:1–6. doi: 10.1016/j.heha.2023.100048. doi: 10.1016/j.heha. 2023.100048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madaan N, Paul BC, Guleria R. Meeting oxygen requirements of rural India: A self-contained solution. Indian J Public Health. 2021;65:82–4. doi: 10.4103/ijph.IJPH_1405_20. [DOI] [PubMed] [Google Scholar]
- 12.Bradley BD, Qu S, Peel D, Howie SR, Cheng YL. Storing oxygen or storing energy? A cost-effectiveness model for comparing appropriate medical oxygen supply systems in low-resource health facilities with intermittent power. Proceedings of the 7th International Conference on Appropriate Healthcare Technologies for Developing Countries, London, UK, IET, September 18-19, 2012. :1–6. [Google Scholar]
- 13.Bradley BD, Qu S, Cheng YL, Peel D, Howie SR. Options for medical oxygen technology systems in low-resource settings: A framework for comparison. Proceedings of the 2012 IEEE Global Humanitarian Technology Conference, Seatle, WA, USA, IEEE, 2012 October 21-24, 2012. :356–362. [Google Scholar]
- 14.McAllister S, Thorn L, Boladuadua S, Gil M, Audas R, Edmonds T, et al. Cost analysis and critical success factors of the use of oxygen concentrators versus cylinders in sub-divisional hospitals in Fiji. BMC Health Serv Res. 2021;21:1–7. doi: 10.1186/s12913-021-06687-8. doi: 10.1186/s12913-021-06687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shi F, Zeng F, Zhou Z. Analysis on variation of oxygen loss rate in AIP system. J Phys Confer Ser. 2021;2029:1–7. doi: 0.1088/1742-6596/2029/1/012154. [Google Scholar]
- 16.Duprez F, Michotte JB, Cuvelier G, Legrand A, Mashayekhi S, Reychler G. Accuracy of oxygen flow delivered by compressed-gas cylinders in hospital and prehospital emergency care. Respir Care. 2018;63:332–8. doi: 10.4187/respcare.05657. [DOI] [PubMed] [Google Scholar]