Abstract
Gestational diabetes mellitus (GDM) is the most prevalent pregnancy-related endocrinopathy, affecting up to 25% of pregnancies worldwide. Pregnant individuals who develop GDM have an increased risk of complications during pregnancy and birth, as well as future development of type 2 diabetes mellitus and CVD. This increased risk is subsequently passed along to the offspring, perpetuating a cycle of metabolic dysfunction across generations. GDM prevention strategies have had mixed results for many years, but more recent systematic reviews and meta-analyses have suggested potential new avenues of prevention. The objective of this review is to summarise the literature examining the efficacy of lifestyle interventions for the prevention of GDM and to uncover if specific individual-level characteristics influence this outcome. Based on the present literature, we determined that future trials should be designed to understand if initiation of lifestyle intervention in the preconception period is more effective to reduce GDM. Furthermore, trials initiated during pregnancy should be developed through the lens of precision prevention. That is, trials should tailor intervention approaches based on individual-level risk defined by the presence of modifiable and non-modifiable risk factors. Finally, future interventions might also benefit from just-in-time adaptive intervention designs, which allow for interventions to be modified in real-time based on objective assessments of an individual’s response.
Keywords: Behaviour, Diet, Exercise, Gestational diabetes mellitus (GDM), Individual, Lifestyle, Personalised medicine, Precision medicine, Prediction, Prescription, Response, Review
Graphical Abstract
Introduction
Gestational diabetes mellitus (GDM), which is defined as the first recognition of hyperglycaemia during pregnancy [1], is estimated to affect 10% to 25% of all pregnancies worldwide [1,2]. The variation among prevalence estimates is due, in part, to the diagnostic testing criteria being a matter of debate, and to phenotypic differences in the presentation of GDM between individuals, such as beta cell dysfunction, insulin resistance or a combination of these disorders [3,4,5]. Although GDM resolves with birth, it has been associated with increased risk of adverse maternal and offspring health outcomes following pregnancy. These include maternal development of type 2 diabetes [6,7,8], the metabolic syndrome [9,10] and CVD [11,12,13,14]. Children born to individuals who have GDM have an increased risk of developing obesity, type 2 diabetes and neurodevelopmental impairments [15].
The aetiology of GDM is complex and multifactorial. Mechanistic and epidemiological research has implicated genetic and environmental factors in the development of GDM [16]. Inherent risk factors for GDM are considered to be those with genetic or demographic origins and are commonly defined as non-modifiable risk factors. Alternatively, risks attributed to lifestyle habits, or the environment, are defined as modifiable risk factors. Identifying risk factors for phenotypic differences that exist within GDM is likely to be pertinent for prevention approaches.
For non-modifiable risk factors, GDM is more prevalent in individuals of advanced maternal age [17], Asian race, or Hispanic ethnicity [18]. Further, those with first-degree relatives affected by type 2 diabetes and a history of other hormonal disorders, including polycystic ovary syndrome, are also more likely to develop GDM [19,20,21,22]. Research into the genetic polymorphisms associated with GDM have identified several candidate genes, including some which modulate beta cell dysfunction (e.g. TCF7L2, MTNR1B and KCNQ1) and some that influence insulin action (e.g. CDKAL1 and IRS1). Interestingly, many of these candidate genes share a genetic architecture with type 2 diabetes [23,24]. However, further studies of non-modifiable risk factors are needed. For example, it is not clear at what age GDM risk increases, why racial and ethnic differences exist, or the specific genetic or epigenetic risks imparted by family history [19,22].
The development of GDM is also influenced by many risk factors associated with lifestyle behaviours and an individual’s broad environment. These include pre-pregnancy obesity, gestational weight gain (GWG) in early- and mid-pregnancy, dietary and physical activity habits during preconception and pregnancy, smoking (including recreational marijuana [25]), a shorter inter-pregnancy interval [20] and depression [26,27]. The maternal diet, including increased energy consumption and poor diet quality, such as low dietary fibre intake, increased glycaemic index foods and greater intake of sugar-sweetened beverages, has been implicated in GDM risk [28]. Additionally, higher GDM risk has been associated with lower levels of physical activity and sedentary behaviour prior to or in early pregnancy [29].
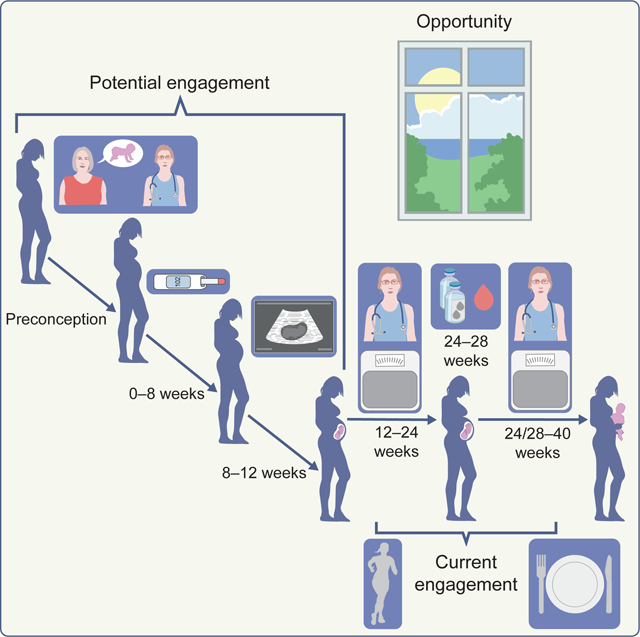
Further research is needed to better understand a broader set of risk factors, including those with physiological (e.g. gut microbiome and genetics), psychological (e.g. mental health and wellness) and social (e.g. access to healthcare, time and financial status) origins. Despite decades of research uncovering GDM risk factors, an enormous opportunity remains for research to develop and validate an individual-level risk factor assessment tool (Fig. 1). Such tools are currently being conceived and developed to direct those at greatest risk of GDM towards more precise, and possibly earlier, interventions, including during the inter-pregnancy interval [30,31,32]. Future studies are required to identify and understand which risk factors to target, and what intervention will elicit the most potent response (Fig. 1). Although outside of the scope of the present review, it is important for precision medicine efforts to identify those who might not benefit from preventive strategies. This includes women who develop GDM and may instead benefit from targeted approaches to treat GDM and to manage postpartum complications linked to GDM.
Fig. 1.
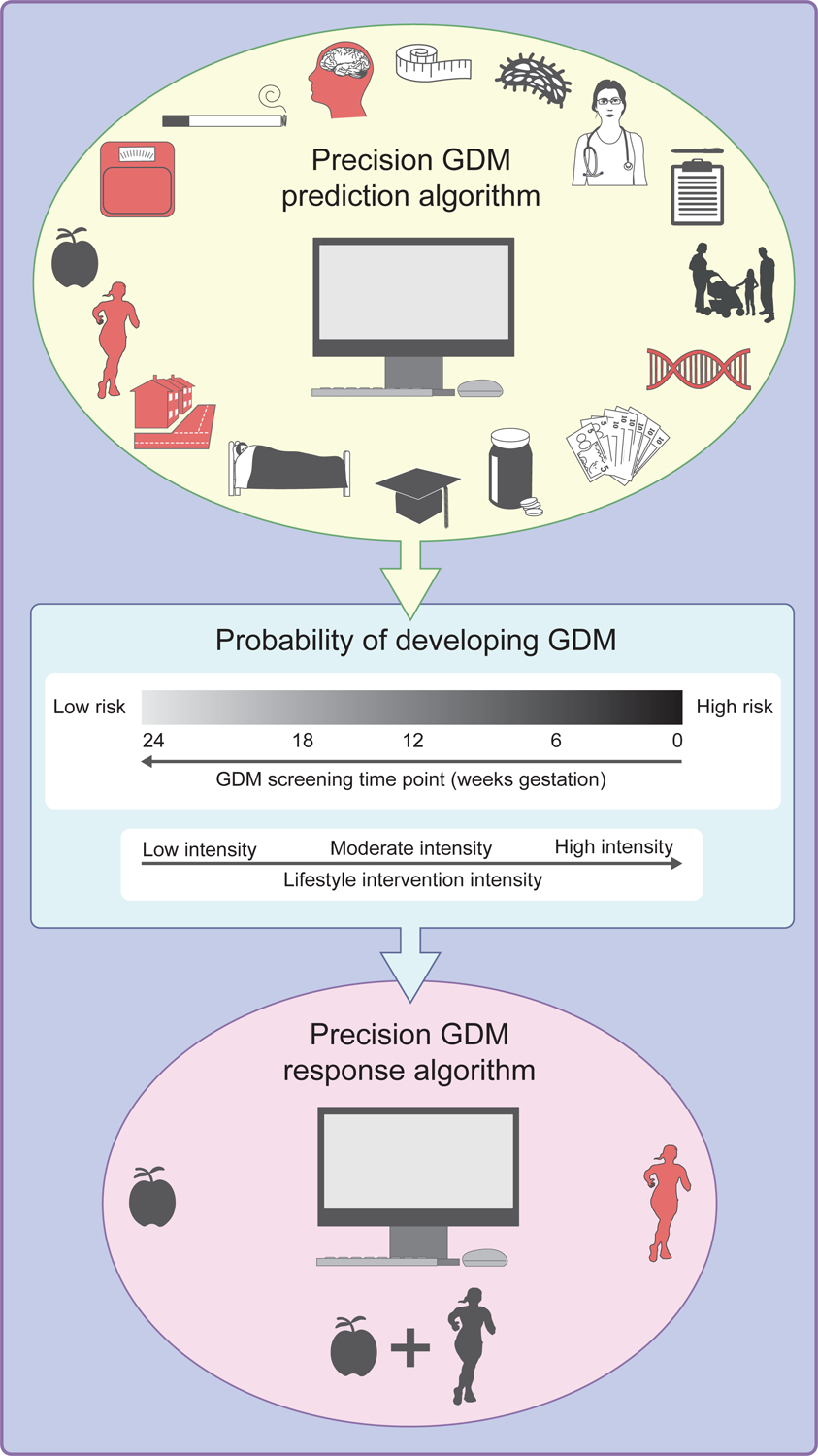
Opportunities for precision prescription of GDM. Careful and extensive phenotyping of people early in pregnancy can be used in future studies to develop prediction algorithms of GDM risk and to more precisely prescribe a GDM prevention plan. Jane Doe’s physician gathers her clinical and epidemiological traits (shown in red). The Precision GDM Prediction Algorithm uses these modifiable and non-modifiable risk factors to predict her probability of developing GDM. It turns out, Jane is at moderate-to-high risk of developing GDM. She would benefit from earlier screening and a moderate-to-high-intensity lifestyle intervention. Jane has a high-stress job and lives in a big city. She does not have access to green space nearby. While she does her best to eat healthy, her work hours have led to a sedentary lifestyle. Based on these and other factors, the Precision GDM Response Algorithm predicts Jane would respond best to a structured physical activity (exercise) intervention at a local gym with an exercise specialist. This figure is available as part of a downloadable slideset
State of the science: lifestyle intervention trials designed to prevent GDM
Lifestyle interventions are traditionally prescribed as the first approach to prevent GDM. Adherence to appropriate GWG [33,34,35], a nutritionally adequate and energy controlled diet [36], and regular physical activity [37,38] are recommended to optimise maternal and offspring health benefits.
Pre-pregnancy obesity and GWG are some of the strongest risk factors for GDM development [39,40]. Thus, researchers hypothesised that lifestyle interventions focused on limiting excessive GWG, especially in individuals with obesity, decrease incident GDM risk. As summarised below, when considered independently, prior RCTs examining the effects of dietary-, physical activity- and multi-modal strategies on GDM incidence have yielded conflicting results [41]. Nevertheless, meta-analyses have more recently determined that lifestyle interventions may elicit an overall protective effect against GDM (Table 1).
Table 1.
GDM prevention intervention studies: summary of meta-analyses
| Author, year | Exposure | Population | Trials | n | Comparison group | RR (95% CI) |
|---|---|---|---|---|---|---|
| Dietary | ||||||
| Rogozińska et al, 2015 | Diet-only based interventions | Both high- and low-risk women | 6 | 1309 | Interventions vs control groups | .67 (0.39, 1.15) |
| Bennett et al, 2018 | Diet-only based interventions | International, pregnant women | 11 | 3388 | Interventions vs control groups | .56 (0.36, 0.87) |
| Physical activity | ||||||
| Davenport, et al 2018 | Exercise-only interventions that measured subjective or objective amount of frequency, intensity, duration, volume or type of exercise only | Pregnant women with no contraindication to exercise | 26 | 6934 | Interventions vs control groups | .62 (0.52, 0.75)a |
| Sanabria-Martínez et al, 2015 | Exercise programme | Healthy pregnant women who had low physical activity levels or were sedentary | 13 | 2873 | Interventions vs control groups | .69 (0.52, 0.91) |
| Nasiri-Amiri et al, 2019 | Exercise activities | Obese or overweight pregnant women | 8 | 1441 | Interventions vs control groups | .76 (0.56, 1.03) |
| Bennett et al, 2018 | Physical activity | International, pregnant women | 10 | 2981 | Interventions vs control groups | .62 (0.50, 0.78) |
| Multi-modal/behavioural | ||||||
| Rogozińska et al, 2015 | Diet and lifestyle approaches | Both high- and low-risk women | 13 | 4745 | Interventions vs control groups | 0.95 (0.89, 1.2) |
| Bennett et al, 2018 | Dietary and physical activity components | International, pregnant women | 19 | 7724 | Interventions vs control groups | .90 (0.77, 1.05) |
| Cantor et al, 2021 | Interventions that could contain a counselling component (supervised or prescribed exercise or dietary programmes, or weight management), or interventions consisting of counselling only | Women who were pregnant or planning a pregnancy, with normal weight (BMI ≥ 18.5) | 43 | 19,752 | Interventions vs control groups | .87 (0.79, 0.95) |
Effect reported OR
Diet interventions
Both energy intake and diet quality play key roles in glucose homeostasis, insulin resistance and metabolic processes that influence energy stores within the body [42]. A 2015 study using National Health and Nutrition Examination Survey (NHANES) data showed that poor diet quality (Healthy Eating Index [HEI]-2010) was associated with the incidence of GDM during prior pregnancies [43]. Poor diet quality, even in the absence of excess energy intake, has been shown to have severe long-term detriments to beta cell function [44]. Poor diet quality may also lead to chronic insulin resistance and metabolic dysregulation, with downstream effects on the risk of the development of impaired glucose tolerance and type 2 diabetes [45]. As such, GDM prevention efforts have aimed to both enhance diet quality and manage energy intake.
Limiting excessive GWG through reduction in energy intake and improvements to diet quality (e.g. low glycaemic index foods) have been investigated as strategies in prior RCTs. A 2015 meta-analysis of six trials (n=1309) determined that diet interventions, including partial meal replacement to aid in appropriate energy balance, promotion of nutritious eating, and/or energy intake counselling, did not result in a statistically significant reduction in the risk of GDM (RR 0.67 [95% CI 0.39, 1.15]) [46]. However, when intervention effects were stratified by BMI across three trials, a significant reduction in the risk of GDM was evident in women having overweight or obesity (RR 0.40 [95% CI 0.18, 0.86]). With the inclusion of five additional trials and another 2079 individuals, a 2018 meta-analysis (n=3388) observed that diet-only interventions were effective in reducing GDM risk (RR 0.56 [95% CI 0.36, 0.87]) [47] (Table 1). However, in studies that specifically included or stratified women having overweight or obesity, diet interventions no longer produced a significant reduction of GDM risk. In this case, the authors surmised that diet interventions targeting weight reduction through decreased energy intake have been implemented too late for those who enter pregnancy having overweight or obesity. Thus, findings from these meta-analyses suggest that previous trials did not result in a physiologically relevant attenuation of GWG to lessen GDM risk. Although findings from the Rogozińska et al (2015) [46] and Bennett et al (2018) [47] meta-analyses differed when examining GDM risk stratified by BMI, it is important to note that compared with Rogozińska et al [46], who focused on dietary manipulation as a treatment to prevent GDM, Bennett et al [47] included intervention trials focused on appropriate GWG as the primary outcome with prevention of GDM as a downstream benefit. These study results identify an opportunity to test the efficacy of preconception and/or early pregnancy interventions in women with high pre-pregnancy BMI. Similarly, future studies are needed to understand whether other individual-level characteristics can explain the heterogeneity of GDM risk reduction in response to diet interventions.
Physical activity interventions
Unstructured (i.e. free-living) and structured (i.e. exercise) physical activity has been shown to improve glucose homeostasis through robust effects on insulin sensitivity. This is a direct result of attenuated insulin resistance and increased skeletal muscle glucose disposal via increasing fat-free mass over time [29]. These mechanisms are why physical activity is often prescribed to prevent and treat non-pregnant individuals at risk of developing type 2 diabetes [48]. Thus, exercise and other physical activity interventions have been hypothesised to have the potential to reduce GDM risk.
A 2018 meta-analysis of 26 trials (n=6934) confirmed previous evidence suggesting that prenatal exercise-only interventions significantly reduced the odds of GDM incidence (OR 0.62 [95% CI 0.52, 0.75]) [49]. In the same year, a separate meta-analysis of only ten trials (n=2981) supported these results (RR 0.62 [95% CI 0.50, 0.78]) [47] (Table 1). However, they also reported that, in those studies specifically including or stratifying women having overweight or obesity, physical activity interventions did not produce a significant reduction in GDM risk [47,50]. The difference in the number of included trials was due to Davenport et al [49] specifically focussing on GDM RCTs, while Bennett et al [47] included RCTs focused on reducing GWG with GDM incidence as a secondary outcome. In the following year, a meta-analysis of eight trials limited to pregnant women having overweight or obesity (n=1441) found that, while exercise interventions alone did not have a significant effect on reducing GDM incidence, incidence was 24% lower among those in the exercise intervention group compared with standard care group (RR 0.76 [95% CI 0.56, 1.03]) [51] (Table 1). Therefore, physical activity interventions may have differential impacts depending on pre-pregnancy body weight status, or current effect size estimates might be limited by the number of trials and population sample sizes. Others have also speculated that the lack of efficacy in women having overweight or obesity was due to an inability to limit excess GWG throughout physical activity interventions [47]. Notably, a preconception weight loss trial in women with prior GDM diagnosis is currently underway to establish if a behavioural intervention, which incorporates physical activity, may be effective in reducing the risk of GDM during a subsequent pregnancy [31]. Further research is needed to understand if individuals with other specific characteristics or risk factors can differentially benefit from prenatal exercise interventions.
Regarding the physical activity prescription, several identified components of such programmes have the potential to reduce GDM risk [52]. These include exercise bouts of 40 to 60 min performed at least three times per week at a moderate intensity, including aerobic exercise, resistance training or a combination of modalities; completion of at least 80% of the prescribed bouts; and initiating the programme as early as possible during pregnancy. Finally, maintaining a pre-pregnancy physical activity routine throughout pregnancy was also shown protective against GDM [29], especially in those having overweight or obesity.
Behavioural and multi-modal interventions
Social cognitive theory models have been found to benefit weight control in pregnant populations [31]. Interventions that have been developed according to behaviour change theories are able to capitalise on the ever-changing intersection between the individual and environment. These interventions commonly reinforce behaviour change techniques such as goal setting, self-monitoring and self-regulation skills to create sustained behavioural changes. A recent systematic review of 43 studies (n=19752) by the United States Preventive Services Task Force investigated prenatal behavioural interventions aimed to foster appropriate GWG [35]. Most of these interventions were multi-modal interventions which consisted of at least one structured element (e.g. supervised exercise, prescribed exercise, dietary recommendations or programmes, or intensive weight management) in conjunction with behavioural counselling, or behavioural counselling only. Almost all of the included trials tested interventions initiated during pregnancy. However, two trials were initiated prior to pregnancy. These trials focused on either reducing GDM risk or pre-pregnancy weight loss. Provider-patient interactions within the interventions ranged from fewer than two contacts (low-intensity) to greater than 12 (high-intensity), with 3–11 contacts considered moderate-intensity. The task force reported that multi-modal interventions were significantly associated with lower GDM risk (RR 0.87 [95% CI 0.79, 0.95]) (Table 1). In stratified analyses, there were no statistically significant effects of the interventions on GDM risk by BMI category (RR 0.80–0.90 [95% CI 0.65, 1.50] for all weight category stratifications). However, notably, the trials with the highest efficacy were those that were moderate-to-high intensity or required ≥3 patient contacts. Of note, the glycaemic thresholds for GDM diagnosis varied among the reviewed trials. Although a stratified analysis to test the timing of the intervention was not conducted, the authors discussed that the time of intervention implementation and outcomes ascertainment may have impacted the findings.
Several analyses have evaluated whether dietary or physical activity interventions alone or combined in a multi-modal approach differentially affect risk for GDM. In a 2015 meta-analysis of 13 RCTs (n=4745) testing the efficacy of diet and lifestyle component interventions, GDM incidence rates were found to be lower in the intervention group compared with a control group, but the effect was not significant (RR 0.95 (95% CI 0.89, 1.2]) [46] (Table 1). These findings were corroborated in a 2018 meta-analysis with six additional RCTs (n=7724) testing the efficacy of combined diet and physical activity interventions (RR 0.90 [95% CI 0.77, 1.05]) [47] (Table 1). Although the multi-modal approach of enhancing diet quality and increasing physical activity should logically reduce GDM, it remains unclear as to why this is not the case. One group postulated that interventions with multiple components implemented in tandem may be overwhelming for patients and, therefore, not sustainable [47]. Moreover, focusing on one type of behaviour (diet or physical activity), with supervision and frequent visits with a counsellor or medical professional, was also previously suggested [35]. As individuals are undergoing pregnancy-related stress and physical duress, Bennett et al suggest that the addition of too many major lifestyle changes could induce an effect opposite to that intended [47].
Further research is required to investigate if multi-modal interventions produce a significant reduction in GDM risk when implemented pre-conception. As mentioned previously, diet and/or physical activity interventions, alone or in combination, seem to be less effective in reducing GDM risk in those having overweight or obesity compared with normal weight [53]. However, these findings remain speculative as others suggest a protective effect of diet interventions in women having overweight or obesity [46]. As such, multi-modal approaches in this population need to test if this is due to intervention timing, or if the specific goals within each component need to be more precisely prescribed. However, these types of programmes may need to be bolstered by increased individual-level counselling opportunities in order to be successful, as the need for professional advice and support during this period is critical.
Limitations of past GDM prevention trials
The Finnish Gestational Diabetes Prevention Study (RADIEL) trial established that inclusion of individualised counselling for diet, physical activity and weight control from trained study nurses, in addition to one group meeting with a dietitian, reduced GDM incidence compared with usual care (13.9% vs 21.6%) [54]. Current literature is limited in testing the impact of increased provider contacts. Secondary data analyses in future trials to stratify GDM risk by number of contacts, or the inclusion of individual-level prescriptions for the intervention components, may prove beneficial.
Most RCTs have not tested the efficacy of preconception interventions or implemented interventions earlier in the pregnancy, such as prior to 8–12 weeks gestation. A 2019 systematic review identified two studies that initiated a structured physical activity intervention between 10 to 14 weeks of gestation [55, 56, 57] as compared with the more common 16 to 20 weeks of gestation in other trials (Table 1). These ‘early pregnancy intervention’ trials were effective in reducing GDM risk (OR 0.10 [95% CI 0.01, 0.80]) [56] and GDM incidence (22.0% physical activity intervention vs 40.6% standard care; p<0.001) [57]. Earlier intervention initiation allows for longer programme involvement and provides more opportunities for counselling and activity sessions to be completed.
To date, GDM prevention interventions have been predominantly rigid in their prescription throughout the entirety of their prescribed programme. Past trials have not yet fully capitalised on real-time monitoring of behaviour change that is now possible through e-health technology and wearables. In the weight management and type 2 diabetes arena, interventions are increasingly designed to adjust intervention delivery based on the individual-level engagement and response. These just-in-time adaptive interventions (JITAIs) rely on near real-time collected objective or subjective information. Using this information, an a priori decision tree can tailor and retailor the intervention to each individual. These novel approaches can leverage technologies and wearables, such as continuous glucose monitoring (CGM), and other mobile technologies or applications (apps) collecting and capturing real-time diet and physical activity to evaluate intervention effects on glycaemic control. Based upon these individual-level data, rapid and direct feedback can be channelled to support behaviour changes more strongly in those individuals with the highest need. As such, JITAIs are effective for weight management in non-pregnant women [58] and show promise in pregnant women with type 1 diabetes [30].
The future for GDM prevention
Upon reviewing this body of literature, several key questions remain. That is, (1) how can we determine those who would benefit most from GDM prevention interventions; (2) when should interventions be initiated; (3) how can we optimise interventions to the needs and physiology of each individual; and (4) how can interventions be continuously adapted based on individual-level response?
Future opportunities for individualised intervention prescriptions
The individual RCTs and meta-analyses demonstrate that there is a critical need to transition from the one-size-fits-most approach for diet and physical activity recommendations during pregnancy to a personalised approach that considers individual-level risk factors, behaviours and socioeconomic situation. Although RCTs included in the previously described meta-analyses varied in their specific approach, most were based on pre-defined diet and physical activity recommendations. Diet and GWG guidelines have recently improved upon their past recommendations with more specific guidance on energy needs and weight gain by BMI class and by trimester [33, 59]. However, energy intake is not necessarily reflective of diet quality, and other research suggests that energy balance might not be a contributor at all [60]. Some individuals may need fewer adjustments to their lifestyle to achieve optimal pregnancy outcomes. When considering the individuality of each pregnancy and results of recent RCTs, it is apparent that there is ambiguity in what constitutes the most effective diet and physical activity practices.
Effective interventions require knowledge of individual-level risk. Early pregnancy screening is thereby needed to understand if a person has a low, moderate or high risk for developing GDM. Risk prediction tools should consider a wide range of clinical characteristics and physiological measures such as glucose metabolism and insulin sensitivity, and include novel biomarkers from metabolomic, genetic and microbiome studies (Fig. 1). Although there is currently insufficient evidence to support that screening and treatment for GDM starting in early pregnancy is beneficial, effective algorithms using early pregnancy risk factors to predict who may develop GDM will help target approaches to reduce risk of GDM development and, in turn, pregnancy, birth and postpartum complications. Such risk prediction tools can be paired with lifestyle intervention RCTs. Together, clinicians can begin to understand how different intervention approaches can benefit individuals based on their risk profiles (Fig. 1). For example, if an individual has a high-stress job, sedentary lifestyle, and already consumes a healthy diet, the tool may consider these factors, along with physiological characteristics, to predict that the most potent mode to reduce GDM risk would be through a structured physical activity intervention (Fig. 1). After identifying the appropriate intervention strategies, monitoring individual-level responses to the intervention is the next critical opportunity for future research (Fig. 2). For example, if CGM demonstrates a positive glycaemic response to an exercise intervention, the intervention could be further adapted to refine the exercise dose, modality and intensity (Fig. 2). This JITAI approach should be approached iteratively. In addition to CGM, JITAIs based on multi-modal interventions would benefit from real-time information input from other Bluetooth-connected devices such as scales for weight monitoring, wearables for physical activity and sleep tracking, and other self-monitoring mobile applications (e.g. diet trackers). Through real-time provision of information to the individual and simultaneous viewing by the clinician, these technological advancements offer the exciting ability to tailor the intervention to each individual and throughout the duration of the programme (Fig. 2). Each of the feedback mechanisms, including body weight, CGM, physical activity and dietary behaviours, may present challenges in interpretation due to an overload of data received. If interventions include content specialists, are properly prescribed, and educational opportunities are effectively provided, this presents a greater opportunity for intervention success. Additionally, with the advent of artificial intelligence technologies to interpret abundant amounts of data, in addition to proper counselling targeted to individual goals, we may further overcome these challenges and enhance intervention efficacy.
Fig. 2.
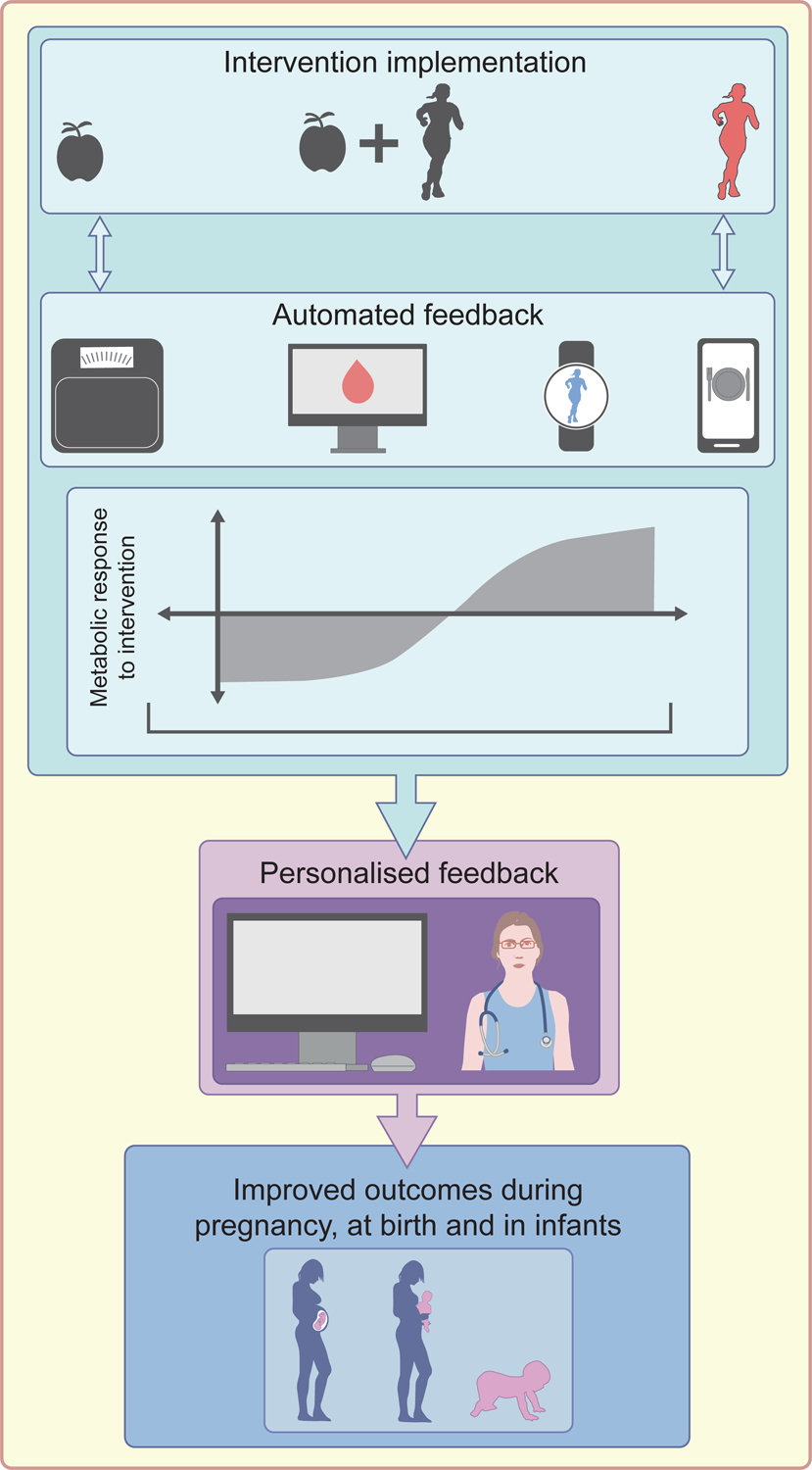
Opportunities for precision prevention of GDM. Future interventions serve to benefit from a multitude of emerging e-health devices and tools which provide an objective assessment of health and behaviours in near real-time. Using a just-in-time adaptive approach, interventions can adapt to the response of each person in real-time to maximise an individual-level response. As Jane Doe begins her prescribed exercise intervention, she is provided with wearables (activity tracker), CGM and other e-health technologies (Bluetooth scale and diet tracker app). She is coached on how to interpret these health outcomes and behaviours on the basis of her exercise prescription. This information is simultaneously transmitted to her clinician, who provides personalised feedback. These metabolic responses and health behaviour information help clinicians determine how to adjust the intervention intensity and mode to allow for improved GDM risk and future pregnancy, birth and infant outcomes. This figure is available as part of a downloadable slideset
Finally, as new diet and physical activity JITAIs are developed with the goal to target individual-level risk, other factors such as psychological readiness to change, access to food, and cultural food choices will need to be addressed to ensure future programmes can benefit everyone [61].
Future opportunities for earlier interventions
Most pregnant individuals learn of their pregnancy and enter prenatal care between 8 to 12 weeks gestation [62], and GDM testing occurs at around 24 weeks gestation [63]. In previous RCTs, most pregnant individuals did not commence interventions before 16 weeks, often to up to 20 weeks gestation (Table 1). This leaves a missed window of opportunity to engage individuals in appropriate behaviours earlier in pregnancy (i.e. prior to the shift from a period of high insulin sensitivity to increased insulin resistance) or preconception. Shorter interventions limit the time in which improvements to modifiable risk factors can occur [64]. However, starting interventions in the preconception period is complicated by many logistic challenges; most pregnancies are ‘unplanned’ [65] and, even if planned, in America and European countries few couples consult health providers prior to pregnancy [66]. Furthermore, uncertainty exists as to how preconception interventions, particularly those leading to rapid weight loss, may impact the placentation process [67]. Some behavioural change interventions prior to pregnancy have proven effective in improving offspring outcomes [68]. However, the list of interventions is relatively short, and they primarily focus on diet supplementation [68] with few focussing on behavioural counselling to achieve optimal pre-pregnancy weight [69]. Of note, several preconception trials testing reduction in GDM risk are ongoing [31,32]. Additionally, the National Institutes of Health (NIH) recently released a call for grant applications centred on pre-pregnancy care (NOT-HD-19–019). With increased recognition of the importance of trials during preconception, the field is working towards understanding the optimal time of implementation [70,71].
Conclusion
There are a multitude of modifiable and non-modifiable risk factors that influence GDM risk, and each should be given their respective mechanistic consideration when developing strategies for prevention. To advance the field, future interventions should test whether the timing of programme initiation matters and seek to understand if there are differential effects based on specific individual-level risk profiles or phenotypes. As such, the future is positioned to take advantage of emerging technology that promises to evolve the notion of precision prescription and precision prevention of GDM. Once a deeper understanding of the specific individual-level determinants to GDM risk are elucidated, interventions may be prescribed and adapted based on other considerations, such as socioeconomic disparities and access to care. Within the emerging field of precision prevention for GDM we propose that imminent opportunities for advancement include: (1) the development and validation of algorithms to accurately predict GDM risk; (2) using GDM risk to design new intervention approaches and to develop prediction models of intervention response; and finally (3), develop modern JITAI that incorporate innovative technologies to continuously assess the individual-level intervention response to adapt intervention approaches in real-time to ensure success against GDM development.
Research In Context.
- What is already known about this subject?
- GDM is a highly prevalent pregnancy-related endocrinopathy.
- Previous trials have been largely unsuccessful in reducing risk of GDM development.
- Recent systematic reviews and meta-analyses have highlighted that specific modifiable and non-modifiable risk factors may be key in understanding how to prescribe lifestyle intervention to reduce GDM risk.
- What is the key question?
- How do we improve interventions to reduce GDM risk?
- What are the new findings?
- Specific risk factors such as prior diagnosis of GDM and having overweight/obesity play a key role in GDM development.
- Initiation of interventions prior to pregnancy have been challenging but present an avenue for limiting future GDM risk.
- Intervention intensity, such as mode and clinician contact, and modification using just-in-time adaptive intervention (JITAI) designs may prove effective to limit GDM risk.
- How might this impact clinical practice in the foreseeable future?
- Using prediction algorithms to identify those with the greatest risk for GDM development earlier, such as before conception, may help to determine who benefits most from lifestyle approaches.
- Adapting lifestyle approaches based on real-time feedback allow for clinicians to better support behaviour changes in women at risk for GDM.
Questions that remain.
How can we determine those who would benefit most from GDM prevention interventions?
When should GDM prevention interventions be initiated?
How can we optimise GDM prevention interventions to meet the needs and physiology of each individual?
How can GDM prevention interventions be continuously adapted based on individual-level response leveraging real-time feedback?
Funding
MFH was supported by an American Diabetes Association Pathways Award #1-15-ACE-26. NG was supported by a grant from the National Institute of Health (R01HD094150). LMR and JRS are supported in part by R01 NR017644, R01 DK124806.
ABBREVIATIONS
- CGM
Continuous glucose monitoring
- GDM
Gestational diabetes mellitus
- GWG
Gestational weight gain
- JITAI
Just-in-Time Adaptive Interventions
Footnotes
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
REFERENCES
- 1.American Diabetes Association (2021) Management of diabetes in pregnancy: Standards of medical care in diabetes—2021. Diabetes Care 44(Supplement 1):S200–S210. 10.2337/dc21-S014 [DOI] [PubMed] [Google Scholar]
- 2.Lowe WL Jr, Scholtens DM, Lowe LP, et al. (2018) Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA 320(10):1005–1016. 10.1001/jama.2018.11628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powe CE, Allard C, Battista MC et al. (2016) Heterogeneous contribution of insulin sensitivity and secretion defects to gestational diabetes mellitus. Diabetes Care 39(6):1052–1055. 10.2337/dc15-2672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cundy T (2012) Proposed new diagnostic criteria for gestational diabetes--a pause for thought? Diabet Med 29(2):176–180. doi: 10.1111/j.1464-5491.2011.03407.x [DOI] [PubMed] [Google Scholar]
- 5.Metzer BE, Buchanan TA, Coustan DR, et al. (2007) Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 30(Supplement 2):S251–S260. 10.2337/dc07-s225 [DOI] [PubMed] [Google Scholar]
- 6.Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: A systematic review. Diabetes Care 25(10):1862–1868. 10.2337/diacare.25.10.1862 [DOI] [PubMed] [Google Scholar]
- 7.Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet 373(9677):1773–1779. 10.1016/S0140-6736(09)60731-5 [DOI] [PubMed] [Google Scholar]
- 8.Hakkarainen H, Huopio H, Cederberg H, Pääkkönen M, Voutilainen R, Heinonen S (2016) The risk of metabolic syndrome in women with previous GDM in a long-term follow-up. Gynecol Endocrinol 32(11):920–925. 10.1080/09513590.2016.1198764 [DOI] [PubMed] [Google Scholar]
- 9.Xu Y, Shen S, Sun L, Yang H, Jin B, Cao X (2014) Metabolic syndrome risk after gestational diabetes: a systematic review and meta-analysis. PLoS One 9(1):e87863. 10.1371/journal.pone.0087863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hakkarainen H, Huopio H, Cederberg H, Voutilainen R, Heinonen S (2018) Future risk of metabolic syndrome in women with a previous LGA delivery stratified by gestational glucose tolerance: a prospective cohort study. BMC pregnancy and childbirth 18(1):326. 10.1186/s12884-018-1958-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah BR, Retnakaran R, Booth GL (2008) Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care 31(8):1668–1669. 10.2337/dc08-0706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alberti KG, Eckel RH, Grundy SM, et al. (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. 10.1161/CIRCULATIONAHA.109.192644 [DOI] [PubMed] [Google Scholar]
- 13.Retnakaran R (2009) Glucose tolerance status in pregnancy: a window to the future risk of diabetes and cardiovascular disease in young women. Curr Diabetes Rev 5(4):239–244. 10.2174/157339909789804378 [DOI] [PubMed] [Google Scholar]
- 14.Fraser A, Nelson SM, Macdonald-Wallis C, et al. (2012) Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation 125(11):1367–1380. 10.1161/CIRCULATIONAHA.111.044784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farahvar S, Walfisch A, Sheiner E (2019) Gestational diabetes risk factors and long-term consequences for both mother and offspring: a literature review. Expert Rev Endocrinol Metab 14(1):63–74. 10.1080/17446651.2018.1476135 [DOI] [PubMed] [Google Scholar]
- 16.Johns EC, Denison FC, Norman JE, Reynolds RM (2018) Gestational diabetes mellitus: Mechanisms, treatment, and complications. Trends Endocrinol Metab 29(11):743–754. 10.1016/j.tem.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 17.Mills TA and Lavender T (2011) Advanced maternal age. Obstetrics, Gynaecology & Reproductive Medicine 21(4):107–111. 10.1016/j.ogrm.2010.12.003 [DOI] [Google Scholar]
- 18.Lin J, Liu H, Wu DD, Hu H-T, Wang H-H, Zhou C-L, et al. (2020) Long interpregnancy interval and adverse perinatal outcomes: A retrospective cohort study. Sci. China Life Sci 63, 898–904 (2020). 10.1007/s11427-018-9593-8 [DOI] [PubMed] [Google Scholar]
- 19.Yong HY, Shariff ZM, Yusof BNM, et al. (2020) Independent and combined effects of age, body mass index and gestational weight gain on the risk of gestational diabetes mellitus. Sci Rep 10:8486. 10.1038/s41598-020-65251-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Solomon CG, Willett WC, Carey VJ, et al. (1997) A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA 278(13): 1078–1083. [PubMed] [Google Scholar]
- 21.Cypryk K, Szymczak W, Czupryniak L, Sobczak M, Lewiński A (2008) Gestational diabetes mellitus - an analysis of risk factors. Endokrynologia Polska 59(5):393–397. [PubMed] [Google Scholar]
- 22.Lo JC, Feigenbaum SL, Escobar GJ, Yang J, Crites YM, Ferrara A (2006) Increased prevalence of gestational diabetes mellitus among women with diagnosed polycystic ovary syndrome: a population-based study. Diabetes Care 29(8):1915–1917. 10.2337/dc06-0877 [DOI] [PubMed] [Google Scholar]
- 23.Yahaya T, Salisu T, Abdulrahman YB, Umar AK (2020) Update on the genetic and epigenetic etiology of gestational diabetes mellitus: A review. Egyptian Journal of Medical Human Genetics 21:Article Number 13. 10.1186/s43042-020-00054-8 [DOI] [Google Scholar]
- 24.Powe CE and Kwak SH (2020) Genetic studies of gestational diabetes and glucose metabolism in pregnancy. Curr Diab Rep 20(12):69. 10.1007/s11892-020-01355-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corsi DJ, Walsh L, Weiss D, et al. (2019) Association between self-reported cannabis use and maternal, perinatal, and neonatal outcomes. JAMA 322(20):145–152. 10.1001/jama.2019.8734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hinkle SN, Buck Louis GM, Rawal S, Zhu Y, Albert PS, Zhang C. (2016). A longitudinal study of depression and gestational diabetes in pregnancy and the postpartum period. Diabetologia 59(12):2594–2602. 10.1007/s00125-016-4086-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minschart C, De Weerdt K, Elegeert A, et al. (2021) Antenatal Depression and Risk of Gestational Diabetes, Adverse Pregnancy Outcomes, and Postpartum Quality of Life. J Clin Endocrinol Metab 106(8):e3110–e3124. 10.1210/clinem/dgab156 [DOI] [PubMed] [Google Scholar]
- 28.Moses RG and Brand-Miller JC (2009) Dietary risk factors for gestational diabetes mellitus: are sugar-sweetened soft drinks culpable or guilty by association? Diabetes Care 32(12):2314–2315. 10.2337/dc09-1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tobias DK, Zhang C, van Dam RM, Bowers K, Hu FB (2011) Physical activity before and during pregnancy and risk of gestational diabetes mellitus: a meta-analysis. Diabetes Care 34(1):223–229. 10.2337/dc10-1368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scott EM, Feig DS, Murphy HR, Law GR, CONCEPTT Collaborative Group (2020) Continuous glucose monitoring in pregnancy: Importance of analyzing temporal profiles to understand clinical outcomes. Diabetes Care 44(8):dc192527. 10.2337/dc19-2527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Phelan S, Jelalian E, Coustan D, et al. (2021) Protocol for a randomized controlled trial of pre-pregnancy lifestyle intervention to reduce recurrence of gestational diabetes: Gestational Diabetes Prevention/Prevención de la Diabetes Gestacional. Trials, 22(1):256. 10.1186/s13063-021-05204-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bogaerts A, Ameye L, Bijlholt M, Amuli K, Heynickx D, Devlieger R. (2017) INTER-ACT: prevention of pregnancy complications through an e-health driven interpregnancy lifestyle intervention – study protocol of a multicentre randomised controlled trial. BMC Pregnancy Childbirth 17, 154. 10.1186/s12884-017-1336-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. Rasmussen KM, Yaktine AL, editors. Washington (DC): National Academies Press (US); 2009. [PubMed] [Google Scholar]
- 34.Guo XY, Shu J, Fu XH, et al. (2019) Improving the effectiveness of lifestyle interventions for gestational diabetes prevention: A meta-analysis and meta-regression. BJOG: An International Journal of Obstetrics and Gynaecology 126(3):311–320. 10.1111/1471-0528.15467 [DOI] [PubMed] [Google Scholar]
- 35.Cantor A, Jungbauer RM, McDonagh MS, et al. (2021) Counseling and Behavioral Interventions for Healthy Weight and Weight Gain in Pregnancy: A Systematic Review for the U.S. Preventive Services Task Force. JAMA 325(20):2094–2109. 10.1001/jama.2021.4230 [DOI] [PubMed] [Google Scholar]
- 36.The American College of Obstetricians and Gynecologists. Nutrition during Pregnancy. Retrieved August 31, 2021, Available from: https://www.acog.org/womens-health/faqs/nutrition-during-pregnancy
- 37.The American College of Obstetricians and Gynecologists. Physical Activity and Exercise During Pregnancy and the Postpartum Period. Retrieved June 20, 2021, Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2020/04/physical-activity-and-exercise-during-pregnancy-and-the-postpartum-period
- 38.Sanabria-Martínez G, García-Hermoso A, Poyatos-León R, Álvarez-Bueno C, Sánchez-López M, Martínez-Vizcaíno V (2015) Effectiveness of physical activity interventions on preventing gestational diabetes mellitus and excessive maternal weight gain: a meta-analysis. BJOG: An International Journal of Obstetrics and Gynaecology 122(9):1167–1174. 10.1111/1471-0528.13429 [DOI] [PubMed] [Google Scholar]
- 39.Baci Y, Ustuner I, Keskin HL, Ersoy R, Avsar AF (2013) Effect of maternal obesity and weight gain on gestational diabetes mellitus. Gynecol Endocrinol 29(2):133–136. 10.3109/09513590.2012.730571 [DOI] [PubMed] [Google Scholar]
- 40.Catalano PM (2010) The impact of gestational diabetes and maternal obesity on the mother and her offspring. J Dev Orig Health Disp 1(4):208–215. 10.1017/S2040174410000115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Griffith RJ, Alsweiler J, Moore AE, et al. (2020) Interventions to prevent women from developing diabetes during pregnancy: an overview of Cochrane systematic reviews. Cochrane Database of Systematic Reviews 2020, Issue 6. Art. No.: CD012394. 10.1002/14651858.CD012394.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pang G, Xie J, Chen Q, Hu Z (2014) Energy intake, metabolic homeostasis, and human health. Food Science and Human Wellness 3(3–4):89–103. 10.1016/j.fshw.2015.01.001 [DOI] [Google Scholar]
- 43.Xiao RS, Simas TA, Person SD, Goldberg RJ, Waring ME (2015) Diet quality and history of gestational diabetes mellitus among childbearing women, United States, 2007–2010. Preventing Chronic Disease 12:E25. 10.5888/pcd12.140360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Ridder D, Kroese F, Evers C, Adriannse M, Gillebaart M (2017) Healthy diet: Health impact, prevalence, correlates, and interventions. Psychol Health 32(8):907–941. 10.1080/08870446.2017.1316849 [DOI] [PubMed] [Google Scholar]
- 45.Saisho Y (2015) β-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J Diabetes 6(1):109–124. 10.4239/wjd.v6.i1.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rogozińska E, Chamillard M, Hitman GA, Khan KS, Thangaratinam S (2015) Nutritional manipulation for the primary prevention of gestational diabetes mellitus: a meta-analysis of randomised studies. PloS ONE 10(2):e0115526. 10.1371/journal.pone.0115526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bennett CJ, Walker RE, Blumfield ML, et al. (2018) Interventions designed to reduce excessive gestational weight gain can reduce the incidence of gestational diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials. Diabetes Research and Clinical Practice 141:69–79. 10.1016/j.diabres.2018.04.010 [DOI] [PubMed] [Google Scholar]
- 48.Ruchat S-M and Mottola MF (2013) The important role of physical activity in the prevention and management of gestational diabetes mellitus. Diabetes Metabolism Research and Reviews 29(5):334–346. 10.1002/dmrr.2402 [DOI] [PubMed] [Google Scholar]
- 49.Davenport MH, Ruchat SM, Poitras VJ, et al. (2018). Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. British journal of sports medicine, 52(21), 1367–1375. 10.1136/bjsports-2018-099355 [DOI] [PubMed] [Google Scholar]
- 50.Ming W-K, Ding W, Zhang CJP, et al. (2019) The effect of exercise during pregnancy on gestational diabetes mellitus in normal-weight women: A systematic review and meta-analysis. BMC Pregnancy Childbirth 18:Article Number 440. 10.1186/s12884-018-2068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nasiri-Amiri F, Sepidarkish M, Shirvani MA, Habibipour P, Tabari N (2019) The effect of exercise on the prevention of gestational diabetes in obese and overweight pregnant women: a systematic review and meta-analysis. Diabetology & Metabolic Syndrome 11:72. 10.1186/s13098-019-0470-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lust O, Chongsuwat T, Lanham E, Chou AF, Wickersham E (2021) Does exercise prevent gestational diabetes mellitus in pregnant women? A clin-iq. J Patient Cent Res Rev 8(3):281–285. 10.17294/2330-0698.1811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shepherd E, Gomersall JC, Tieu J, Han S, Crowther CA, Middleton P (2017) Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev 2017(11):CD010443. 10.1002/14651858.CD010443.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Koivusalo SB, Rönö K, Klemetti MM, et al. (2016) Gestational Diabetes Mellitus Can Be Prevented by Lifestyle Intervention: The Finnish Gestational Diabetes Prevention Study (RADIEL): A Randomized Controlled Trial. Diabetes Care 39(1):24–30. 10.2337/dc15-0511 [DOI] [PubMed] [Google Scholar]
- 55.Makaruk B, Galczak-Kondraciuk A, Forczek W, Grantham W, Charmas M (2019) The effectiveness of regular exercise programs in the prevention of gestational diabetes mellitus-A systematic review. Obstet Gynecol Surv 74(5):303–312. 10.1097/OGX.0000000000000673 [DOI] [PubMed] [Google Scholar]
- 56.Cordero Y, Mottola MF, Vargas J, Blanco M, Barakat R (2015) Exercise is associated with a reduction in gestational diabetes mellitus. Med Sci Sports Exerc 47(7):1328–1333. 10.1249/MSS.0000000000000547 [DOI] [PubMed] [Google Scholar]
- 57.Wang C, Wei Y, Zhang X, et al. (2017) A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol 216(4):340–351. 10.1016/j.ajog.2017.01.037 [DOI] [PubMed] [Google Scholar]
- 58.Hardeman W, Houghton J, Lane K, Jones A, Naughton F (2019) A systematic review of just-in-time adaptive interventions (JITAIs) to promote physical activity. International Journal of Behavioral Nutrition and Physical Activity 16:Article Number 13. 10.1186/s12966-019-0792-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Department of Health and Human Services. Dietary Guidelines for American, 2020–2025. 9th Edition. 2020. Dec. Retrieved June 20, 2021, Available from: https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials
- 60.Most J, Broskey NT, Altazan AD, et al. (2019) Is energy balance in pregnancy involved in the etiology of gestational diabetes in women with obesity? Cell Metab 29(2):231–233. 10.1016/j.cmet.2018.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Downs DS, Chasan-Taber L, Evenson KR, Leiferman J, Yeo S (2013) Physical activity and pregnancy. Research Quarterly for Exercise and Sport 83(4):485–502. 10.1080/02701367.2012.10599138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fowler JR, Mahdy H, Jack BW. Pregnancy. [Updated 2021 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Jan. Retrieved August 31, 2021, Available from: https://www.ncbi.nlm.nih.gov/books/NBK448166/ [Google Scholar]
- 63.American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019. Jan;42(Supplement 1):S13–S28. 10.2337/dc19-S002 [DOI] [PubMed] [Google Scholar]
- 64.Pentecost M and Meloni M (2020) “It’s never too early”: Preconception care and postgenomic models of life. Front Sociol 5:21. 10.3389/fsoc.2020.00021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arteaga S, Caton L, Gomez AM (2019) Planned, unplanned and in-between: the meaning and context of pregnancy planning for young people. Contraception (99)1:16–21. 10.1016/j.contraception.2018.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Poels M, Koster MPH, Franx A, van Stel HF (2017) Parental perspectives on the awareness and delivery of preconception care. BMC Pregnancy and Childbirth 17:Article Number 324. 10.1186/s12884-017-1531-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hoek J, Steegers-Theunissen R, Sinclair K, Schoenmakers S (2020) The Science of Preconception. In: Shawe J, Steegers E, Verbiest S (eds) Preconception Health and Care: A Life Course Approach. Springer, Cham. 10.1007/978-3-030-31753-9_3 [DOI] [Google Scholar]
- 68.Temel S, van Voorst SF, Jack BW, Denktaş S, Steegers EAP (2014) Evidence-based preconception lifestyle interventions. Epidemiologic Reviews 36(1):19–30. 10.1093/epirev/mxt003 [DOI] [PubMed] [Google Scholar]
- 69.Schoenaker DAJM, de Jersey S, Willcox J, Francois ME, Wilkinson S (2020) Prevention of gestational diabetes: The role of dietary intake, physical activity, and weight before, during, and between pregnancies. Semin Reprod Med 38(6):352–365. 10.1055/s-0041-1723779 [DOI] [PubMed] [Google Scholar]
- 70.Flynn AC, Pryke E, Wadhera M, Poston L, White SL (2021) A preconception intervention targeted at women with modifiable risk factors before pregnancy to improve outcomes; protocol for the Get Ready! feasibility trial. Pilot Feasibility Stud 7(1):86. 10.1186/s40814-021-00824-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Edwards KJ, Maslin K, Andrade J, Jones RB, Shawe J (2021) mHealth as a primary mode of intervention for women at risk of, or diagnosed with, gestational diabetes: a scoping review protocol. JBI Evid Synth 19(3):660–668. 10.11124/JBIES-20-00151 [DOI] [PubMed] [Google Scholar]


