Abstract
This commentary’s objective was to identify whether female representation at critical care conferences has improved since our previous publication in 2018.
We audited the scientific programs from three international (International Symposium on Intensive Care and Emergency Medicine [ISICEM], European Society of Intensive Care Medicine [ESICM], and Society of Critical Care Medicine [SCCM]) and two national (State of the Art [SOA] and Critical Care Canada Forum) critical care conferences from the years 2017 to 2022.
We collected data on the number of female faculty members and categorized them into physicians, nurses, allied health professions (AHPs), and other.
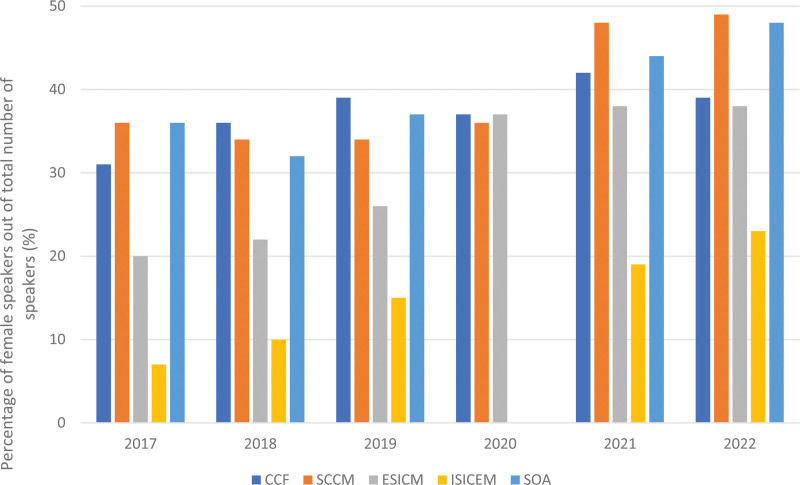
Across all conferences, there was an increased representation of females as speakers and moderators over the 6 years. However, at each conference, male speakers outnumbered female speakers. Only two conferences achieved gender parity in speakers, SCCM in 2021 (48% female) and 2022 and SOA in 2022 (48% female). These conferences also had the highest representation of female nursing and AHP speakers (25% in SCCM, 2021; 19% in SOA, 2022). While there was a statistically significant increase in female speakers (p < 0.01) in 2022 compared with 2016, there was a persistent gender gap in the representation of men and female physicians. While the proportion of female moderators increased in each conference every year, the increase was statistically only significant for ISICEM, ESICM, and SCCM (p < 0.05). The proportion of female nurses and AHP speakers increased in 2022 compared with 2016 (p < 0.0001) but their overall representation was low with the highest proportion (25%) in the 2022 SCCM conference and the lowest (0.5%) in the 2017 ISICEM conference.
This follow-up study demonstrates a narrowing but persisting gender gap in the studied critical care conferences. Thus, a commitment toward minimizing gender inequalities is warranted.
Keywords: critical care medicine, gender, inequality, intensive care conferences, workforce
The past decade has seen increased awareness of gender inequalities within healthcare and a rising number of initiatives address this. There is an observed paradox, where despite increased female enrolment into medical training, there is a persistent gender gap in the physician workforce (1). Reports from the U.K. General Medical Council demonstrate 20% more female doctors in 2019 compared with 2012 (2). The same increase is also observed in Australia (3) and the United States (4). Nonetheless, there is still a sparsity of female physicians in senior roles particularly in certain specialities, such as surgery, radiology, and critical care medicine. The proportion of female critical care physicians is low globally, ranging from 20% to 40% in different geographical regions (1).
Fewer female intensive care medicine (ICM) physicians may partly explain the observed gender disparity in leadership positions, academic roles, successful grant applications, first authorship in peer-reviewed journals, and salary (1). However, female representation in these areas is much lower than expected based on the female ICM specialist workforce (1), suggesting that proportionality does not account for this observation alone. Male physicians consistently outnumber their female counterparts both as faculty members at conferences (5) and as first or last authors of scientific articles (6). The COVID-19 pandemic has disproportionately affected the productivity and scientific output of female academics, leading to the loss of female scientific expertise from the public realm (7) and a widening of the gender gap in critical care medicine.
In our previous publication, we analyzed programs from five national and international critical care conferences between 2010 and 2016, and identified a gender gap among conference speakers, demonstrating that male physicians consistently outnumbered female physicians. With this follow-up study, we aimed to identify whether female representation at these conferences has improved since 2016 and to assess if there is gender difference in participation between physicians, nurses, and allied health professions (AHPs).
We audited the scientific programs from five ICM conferences: State of the Art (SOA), International Symposium on Intensive Care and Emergency Medicine (ISICEM), European Society of Intensive Care Medicine (ESICM), Society of Critical Care Medicine (SCCM), and Critical Care Canada Forum from the years 2017 to 2022. We recorded the gender of all of the moderators and speakers, as well as their professional role, using congress programs and internet searches. We obtained the scientific program from respective conference committees or websites. We then tabulated the proportion of female speakers and moderators, grouping speakers’ profession into physicians, nurses, AHPs, and other (pharmacists, basic scientists, lay speakers). If the speaker’s sex or profession was unclear, we searched for photos and biographies. Trends in number of female speakers, per year and per conference, were analyzed using linear regression, and proportions were compared using the chi-square test. Some data was missing due to conference cancellations during the height of the COVID-19 pandemic or unavailability of annual programs, despite contacting conference conveners.
WHAT HAS CHANGED?
Across all conferences, there was an increase in female representation as speakers and moderators over the 6 years (Table 1); at each conference, male speakers outnumbered female speakers (Fig. 1). By 2022, female physicians represented 38% or more of conference speakers in all studied conferences other than at ISICEM, where female representation was 23%. Two conferences achieved almost equal numbers in female and male speakers, SCCM in 2021 and 2022 and SOA in 2022. These two conferences also had the highest representation of nursing and AHP speakers. While there was a statistically significant increase in female speakers (p < 0.01) in 2022 compared with 2016, this did not extend to female physicians. Conversely, the proportion of female nurse and AHP speakers increased in 2022 compared with 2016 (p < 0.0001) but their overall representation was varied and low, with the highest proportion (25%) in the 2022 SCCM conference and the lowest (0.5%) in the 2017 ISICEM conference. In some conferences (SCCM and SOA), the increase in female speakers was explained by an increase in nurses and AHP, rather than by physicians. While the proportion of female moderators increased in each conference every year, the increase was statistically significant only for ISICEM, ESICM, and SCCM (p < 0.05). Female representation trends across these conferences are shown in Figure 1.
TABLE 1.
Female Representation Among Conference Speakers and Moderators
| Name of Conference | 2017, n (%) | 2018, n (%) | 2019, n (%) | 2020, n (%) | 2021, n (%) | 2022, n (%) |
|---|---|---|---|---|---|---|
| Canadian Critical Care Forum | n = 124 | n = 118 | n = 108 | n = 175 | n = 144 | n = 116 |
| Women speakers | 38 (31) | 43 (36) | 42 (39) | 65 (37) | 60 (42) | 45 (39) |
| Women physician speakers | 31 (25) | 36 (31) | 30 (28) | 56 (32) | 45 (31) | 41 (35) |
| Women moderators | 30/87 (34) | 26/80 (33) | 29/73 (40) | 31/80 (41) | 26/58 (45) | 31/65 (48) |
| All nursing and AHPa | 10 (8) | 11 (9) | 13 (12) | 13 (7) | 17 (12) | 8 (7) |
| Women nursing and AHP | 7 (6) | 6 (5) | 11 (10) | 9 (5) | 12 (8) | 3 (3) |
| Other speakersb | 0 | 3 (3) | 2 (2) | 1 (1) | 3 (2) | 1 (1) |
| Program committee (female) | 2/12 (17) | 3/12 (25) | 3/13 (23) | 5/14 (36) | 6/15 (40) | 6/15 (40) |
| Society of Critical Care Medicine | n = 311 | n = 314 | n = 291 | n = 456 | n = 284 | n = 321 |
| Women speakers | 112 (36) | 107 (34) | 98 (34) | 163 (36) | 137 (48) | 156 (49) |
| Women physician speakerse | 62 (20) | 62 (20) | 50 (17) | 84 (18) | 62 (22) | 36 (11) |
| Women moderators | 25/91 (27) | 36/106 (34) | 36/97 (37) | — | — | 67/139 (48) |
| All nursing and AHPa | 71 (23) | 74 (24) | 77 (26) | 119 (26) | 105 (37) | 110 (34) |
| Women nursing and AHP | 49 (16) | 41 (13) | 45 (15) | 77 (17) | 71 (25) | 72 (22) |
| Other speakersb | 5 (2) | 6 (2) | 4 (1) | 2 (0.4) | 4 (1) | 1 (0.3) |
| European Society of Intensive Care Medicine | n = 345 | n = 391 | n = 320 | n = 317 | n = 448 | n = 391 |
| Women speakers | 69 (20) | 86 (22) | 83 (26) | 116 (37) | 172 (38) | 147 (38) |
| Women physician speakersf | 52 (15) | 64 (16) | 58 (18) | 90 (28) | 123 (27) | 117 (29) |
| Women moderatorse | 22/94 (23) | 21/62 (34) | 25/62 (42) | 25/36 (69) | 17/65 (26) | 62/150 (41) |
| All nursing and AHPa | 33 (10) | 37 (9) | 36 (11) | 36 (11) | 65 (15) | 32 (8) |
| Women nursing and AHP | 17 (5) | 22 (6) | 24 (8) | 26 (8) | 49 (11) | 22 (6) |
| Other speakersb | — | — | 1 (0.3) | 2 (0.6) | 1 (0.2) | 9 (2) |
| Program committee (female) | 2/17 (12) | 2/17 (12) | 2/17 (12) | 5/19 (26) | 4/19 (21) | 6/20 (30) |
| International Symposium on Intensive Care and Emergency Medicinec | n = 215 | n = 233 | n = 222 | — | n = 156 | n = 160 |
| Women speakers | 16 (7.4) | 24 (10.3) | 33 (14.9) | — | 29 (18.6) | 37 (23) |
| Women physician speakersf | 15 (7.0) | 20 (8.6) | 31 (14) | 28 (17.9) | 34 (21) | |
| Women moderatorsd,e | 10/151 (6) | 12/169 (7) | 30/196 (15) | — | 31/132 (23) | 30/143 (21) |
| All nursing and AHPa | 4 (2) | 6 (3) | 4 (2) | — | 3 (2) | 2 (1) |
| Women nursing and AHP | 1 (0.5) | 3(1) | 2 (1) | — | 1 (0.6) | 2 (1) |
| Other speakersb | 2 (1) | |||||
| State of the Artc | n = 122 | n = 101 | n = 103 | — | n = 165 | n = 159 |
| Women speakers | 44 (36) | 33 (32) | 38 (37) | — | 73 (44) | 76 (48) |
| Women physician speakers | 35 (29) | 19 (19) | 17 (17) | — | 34 (21) | 37 (23) |
| Women moderators | — | 8/25 (32) | — | — | 3/10 (30) | 20/35 (57) |
| All nursing and AHPa | 6 (5) | 11 (11) | 16 (16) | — | 24(15) | 38 (24) |
| Women nursing and AHPe | 6 (5) | 8(8) | 13(13) | — | 20 (12) | 30 (19) |
| Other speakersb | 7 (6) | 6 (6) | 0 | — | 7 (4) | 13 (8) |
AHP = allied health profession, n = the total number of speakers at each conference.
Men and women in nursing and AHPs.
Nonhealthcare speakers (e.g., patients, family members, laboratory scientists, etc.).
No conferences were held for State of the Art and International Symposium on Intensive Care and Emergency Medicine (ISICEM) during the 2020 COVID-19 pandemic, so data are unavailable.
No moderators for ISICEM conference in 2021, as the conference was virtual.
p < 0.05.
p < 0.001.Dashes indicate missing values.
Figure 1.
Female speaker representation at the studied critical care conferences from 2017 to 2022. CCCF = Canadian Critical Care Forum, ESICM = European Society of Intensive Care Medicine, ISICEM = International Symposium on Intensive Care and Emergency Medicine, SCCM = Society of Critical Care Medicine, SOA = State of the Art.
PROMOTING THE ARGUMENT FOR GENDER EQUITY
We report an increase in representation of female speakers at the studied intensive care conferences over the last 6 years. While this needs to be applauded, it also prompts some important questions. The first question is how to benchmark or ascertain the “right” proportion of female speakers. We have previously advocated for “explicit targets which reflect, at a minimum, the proportion of women in the specialty” (8). At a local level, female representation may reflect the national average; for example, the U.K. Faculty of ICM reported 20% female ICM consultants in 2017 (9), with an average female speaker representation of 22% in 2017–2022. Conversely, 27.3% of active ICM physicians were female in the United States in 2019 (10), when the proportion of female at SCCM was never higher than 22%. Venkatesh et al (1) reported a mean proportion of female physicians across six intensive care societies of 40%. Consequently, to mirror the practicing workforce of ICM, international conference faculties could aim for a female representation of 40%. However, the gender data quoted from Venkatesh et al (1) represented six of 27 participating societies, highlighting a significant limitation in this area. For the benchmark of 40% to be accurate, national societies, training, and certifying bodies need up-to-date, gender disaggregated data on their members, which should be publicly available.
A second question frequently posed is around the importance of gender parity. We argue scientific bodies (training committees, expert panels, journal editors, grant awarding bodies, and conference faculties) are representative of the colleagues they are trying to educate and inform. Positive outcomes of gender parity in the workplace primarily come from the management sector, where improving gender-diversity has improved productivity, innovation, decision making, and employee retention and satisfaction (11). In the critical care field, the merits of gender parity—increased collaboration, expanding the breadth and balance of scientific topics that are presented, promoting engagement—have been elaborated elsewhere (5, 8). There is evidence that a female’s willingness to compete increases after observing a female role model, which subsequently increases their confidence in their own ability—a phenomenon not observed in men (12). Gender inequity results in females not feeling respected, valued or secure in their work, whereas the paucity of female leadership and role modeling positions creates an impression of limited success (13). Participation in conference faculties is only one piece of this puzzle, since available data suggest that females are under-represented in training programs, editorial boards, academic faculty, and authorship in high-impact journals (1, 7).
Previous studies have highlighted a number of institutional (lack of flexibility, opportunities, and limited job prospects) and interpersonal (bias against females) factors as key drivers of the gender gap in critical care (13). The observed increase in the number of female physician speakers may have been a result of such organizational changes: for example, the post-pandemic expansion of tele-conferences and virtual methods of participation may have facilitated the increased female representation. Furthermore, the ongoing calls for gender equity (6, 13, 14) may have increased awareness in the conferences’ scientific committees, resulting in more female speaker invitations. It is difficult to ascertain which of the above factors, if any, have contributed to the documented improvement, or if there are other marginal gains (e.g., more female sponsorship, increased scrutiny of the scientific programs). Recurrent concerns when gender quotas are being considered are those over meritocracy, tokenism and whether ensuring a fixed number of female speakers will somehow erode the quality of the science. This argument inherently assumes that the existing overrepresentation of men is based on a “natural superiority of talent,” hence, the paucity of females must be due to lack of merit (15). However, implementation of quotas in areas other than healthcare (e.g., politics) was associated with positive outcomes (more inclusive political party operation and recruitment, increased legislative diversity), without compromising candidate quality (16). Research on proposed strategies for gender equity and comparative assessments of their results is paramount.
LIMITATIONS
The current study has several limitations: we have reported gender disparities and did not address other inequalities, such as ethnicity or disability. Emerging data demonstrates that gender inequalities are more profound when racial characteristics are taken into account (6). Unfortunately, inconsistent recording of speakers’ ethnicity made this challenging. Second, we categorized speakers as female or male but did not use further differentiation in gender. Last, our methodological design relied on scientific programs and internet searches, which may have introduced erroneous interpretations of demographic information.
CONCLUSIONS
In conclusion, the present follow-up study evaluating gender equality in the studied medical conferences shows improvement but ongoing disparity. The efforts of the organizing committees should be applauded, as the progress demonstrates a commitment toward minimizing the gender inequalities in academic critical care medicine. Nonetheless, further efforts to understand the reasons behind any persisting gender disparity, address the very low representation of nurses and AHP and identify which strategies are more effective in reducing it are warranted.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Venkatesh B, Mehta S, Angus DC, et al. : Women in intensive care study: A preliminary assessment of international data on female representation in the ICU physician workforce, leadership and academic positions. Crit Care 2018; 22:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.General Medical Council: The Changing Medical Workforce. 2020. Available at: https://www.gmc-uk.org/-/media/documents/somep-2020-chapter-3_pdf-84686032.pdf. Accessed March 5, 2024
- 3.Modra L, Yong S: Towards gender balance in the Australian intensive care medicine workforce. Med J Aust 2018; 211:300–302 [DOI] [PubMed] [Google Scholar]
- 4.Association of American Medical Colleges: Granting Medical School Applications and Matriculants by School, State of Legal Residence, and Gender, 2023-2024. 2023. Available at: https://www.aamc.org/media/5976/download. Accessed March 5, 2024
- 5.Mehta S, Rose L, Cook D, et al. : The speaker gender gap at critical care conferences. Crit Care Med 2018; 46:991–996 [DOI] [PubMed] [Google Scholar]
- 6.Chander S, Luhana S, Sadarat F, et al. : Gender and racial differences in first and senior authorship of high-impact critical care randomized controlled trial studies from 2000 to 2022. Ann Intensive Care 2023; 13:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gabster BP, van Daalen K, Dhatt R, et al. : Challenges for the female academic during the COVID-19 pandemic. Lancet 2020; 395:1968–1970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehta S, Burns KEA, Machado FR, et al. : Gender parity in critical care medicine. Am J Respir Crit Care Med 2017; 196:425–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faculty of Intensive Care Medicine: Women in Intensive Care. 2017. Available at: https://www.ficm.ac.uk/careersworkforceworkforce/women-in-intensive-care-medicine. Accessed March 5, 2024
- 10.American Medical Association: AMA Physician Masterfile. 2021. Available at: https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2021. Accessed March 5, 2024
- 11.Shannon G, Jansen M, Williams K, et al. : Gender equality in science, medicine, and global health: Where are we at and why does it matter? Lancet 2019; 393:560–569 [DOI] [PubMed] [Google Scholar]
- 12.Schier UK: Female and male role models and competitiveness. J Econ Behav Organ 2020; 173:55–67 [Google Scholar]
- 13.Leigh JP, Grood C, Ahmed SB, et al. : Toward gender equity in critical care medicine: A qualitative study of perceived drivers, implications, and strategies. Crit Care Med 2019; 47:e286–e291 [DOI] [PubMed] [Google Scholar]
- 14.Vincent JL, Juffermans NP, Burns KEA, et al. : Addressing gender imbalance in intensive care. Crit Care 2021; 25:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray R: Quotas for men: Reframing gender quotas as a means of improving representation for all. Amer Polit Sci Rev 2014; 108:520–532 [Google Scholar]
- 16.Barnes TD, Holman MR: Gender quotas, women’s representation, and legislative diversity. J Politics 2020; 82:1271–1286 [Google Scholar]