Abstract
Background
Diagnosing ischemia in emergency department (ED) patients with suspected acute coronary syndrome (sACS) is challenging with equivocal disposition of intermediate risk patients.
Objective
Compare sensitivity and specificity of magnetocardiography (MCG) versus standard of care (SOC) stress testing in diagnosing myocardial ischemia.
Methods
Multicenter, prospective, observational cohort study. ED patients with sACS and HEART score ≥ 3 underwent 90 s noninvasive MCG to detect myocardial ischemia. Results were blinded to the patient's clinicians. MCGs were read independently by 3 physicians blinded to clinical data. Myocardial ischemia was ≥70 % epicardial coronary artery stenosis, revascularization within 30 days, or 30-day major adverse cardiac events (MACE). Time to first test (TTT) and patient satisfaction for MCG and SOC were compared.
Results
Of enrolled patients (N = 390) (mean age 59 ± 12 years, 45 % female), 99 (25 %) underwent a non-invasive stress test: 42 (14 %) diagnosed with ischemia. MCG sensitivity was 66.7 % (50.5–80.4 %, 95 % CI) and specificity 57.1 % (50.0–63.3 %, 95 % CI) for detecting coronary ischemia. Noninvasive stress testing (stress echo, nuclear stress, and exercise stress) had the same sensitivity 66.7 % (95 % CI 29.9 % to 92.5 %) and a specificity of 89.9 % (95 % CI 81.7–95.3 %). Mean TTT was shorter for MCG, 3.18 h (SD 1.91) vs. SOC stress testing 22.71 (SD 15.23), p < 0.0001. Mean patient experience was MCG 4.7 versus 3.0 SOC stress testing (p < 0.0001).
Conclusion
MCG provides similar sensitivity and lower specificity as non-invasive stress testing in ED sACS patients. Time to test is shorter for MCG with higher patient satisfaction scores.
Keywords: Magnetocardiography, Cardiac ischemia, Chest pain, Emergency department, Acute coronary syndrome
1. Introduction
Patients with a chief complaint of chest pain result in approximately 10.5 million annual US emergency department (ED) visits and ranks as one of the most common chief complaints [1]. Despite notable advancements in diagnostic and treatment approaches, cardiovascular disease remains a foremost cause of mortality for men and women, accounting for 23.1 % of annual US deaths, with an estimated direct and indirect cost of $407.3 billion in 2018 [2].
When a patient presents to the ED with chest pain of potential cardiac origin, the current standard of care (SOC) involves the performance of an electrocardiogram (ECG), chest X-ray, and cardiac biomarkers. In those determined to be at intermediate risk for acute coronary syndrome (ACS), non-invasive cardiac testing is recommended by current chest pain guidelines [3]. Thus, non-invasive tests have become part of SOC for suspected intermediate risk ACS patients despite their limited sensitivity and specificity, protracted duration, high costs, exposure to radiation, and associated inconvenience to patients.
MCG is a potential solution to overcome the limitations associated with current non-invasive cardiac testing. MCG is a non-invasive test that measures and maps the magnetic fields emitted during the cardiac cycle and has the potential to detect electrophysiological changes occurring from ischemia. Unlike the two-dimensional linear measurements of an ECG, MCG captures signal changes as disruptions in tangential directions, providing a more comprehensive evaluation [4]. Furthermore, MCG's magnetic field measurements remain unaffected by variations in conductivity or body tissue composition, which can impede ECG measurements [[5], [6], [7]].
The exploration of cardiac magnetic field measurements dates to 1963 when Baule and McFee conducted studies at Syracuse University in New York [8]. Although initial attempts to employ MCG in a clinical setting showed promise, logistical challenges posed by older sensor technology impeded widespread adoption [9]. Recent advancements in sensor technology, as well as the capabilities of machine learning and computing, have reignited interest in MCG as a potential tool for prompt non-invasive risk stratification of chest pain patients. However, there is limited data comparing the diagnostic performance of MCG to SOC non-invasive stress testing. Therefore, the objective of this study was to compare the sensitivity and specificity of MCG for the detection of myocardial ischemia vs SOC non-invasive stress testing in ED sACS patients. In addition, the potential effect of MCG on patient throughput (time to first non-invasive cardiac testing) and patient experience were measured.
2. Methods
2.1. Study design
MAGNETO (Accelerated Magnetocardiography in the Evaluation of Patients with Suspected Cardiac Ischemia) was a multicenter, prospective, observational cohort study that enrolled a convenience sample of ED patients presenting with sACS between January 2021 and October 2022 at four US sites. The study was approved by the Institutional Review Board at all sites. After their initial SOC evaluation, which included an ECG, assessment of hemodynamic stability, phlebotomy, chest X-ray, and cardiac monitoring, eligible patients (or their legally authorized representative) provided written informed consent and underwent an MCG scan.
2.2. Patient population
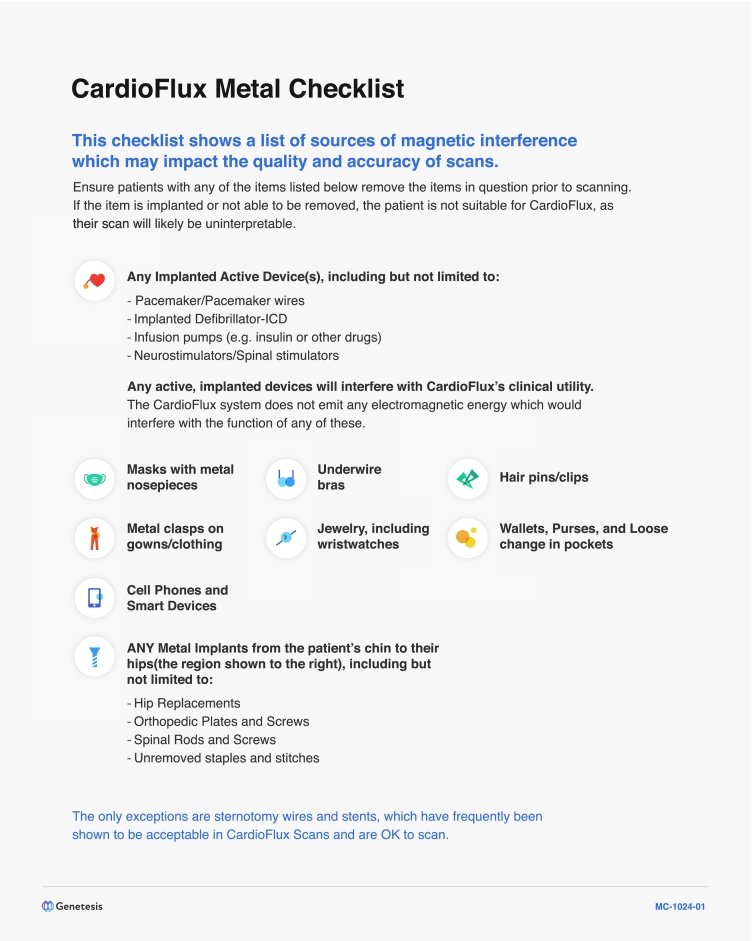
Adult (≥18 years of age) ED patients with sACS and a HEART score ≥3 were eligible for enrollment. Patients were required to be enrolled within the first 4 h of their ED clinical assessment for ACS. Those with ST elevation myocardial infarction on ECG, inability to fit within the MCG scanner, inability to ambulate, hemodynamic instability, or inability to lay flat for 5 min, were excluded. In addition, a metal checklist, (Fig. 1), was used to assess eligibility and exclude patients with significant metal, such as pacemakers or defibrillators.
Fig. 1.
Metal Checklist.
2.3. Magnetocardiography scanning process
MCG scans were performed at times of clinical convenience and without interference or delay of any SOC testing or procedures during each participant's ED stay. The treating clinicians and research subjects were blinded to the MCG scan results. MCG scans were performed using a 36-magnetometer system (CardioFlux; Genetesis Inc., Ohio, USA). Before the scan, patients removed all jewelry, electronic devices, and other removable metal objects. Following standard operating procedure, the MCG operator positioned the sensor array approximately 1 cm above the patient's anterior chest wall. The patient's bed was automatically inserted into the magnetic shield, ensuring correct positioning. MCG scans were performed for 90 s at rest. Fig. 2 depicts an image of the MCG device.
Fig. 2.
Image of MCG device.
MCG = magnetocardiogram.
MCG scans were independently evaluated for the presence or absence of ischemia by three trained physicians: two ED physicians and one cardiologist. These physicians were blinded to all clinical and patient information including the patients' clinical status, demographics or past medical history, laboratory, EKG, stress test and other results. The interpretation of MCG involved a quantitative and qualitative assessment of five specific features of the cardiac magnetic field map: QRS multipolarity, T wave multipolarity, RT angle, T wave dynamics, and ST segment abnormalities. For purposes of this study, each of these features was weighted equally and was considered binary as either ischemia or no ischemia. An abnormality observed in any of these five features was considered indicative of ischemia, while the absence of abnormalities was considered a non-ischemic determination.
2.3.1. Standard of care non-invasive stress testing
SOC testing and treatment were performed at the discretion of the treating physician. Non-invasive stress testing modalities included nuclear imaging (i.e., MPI-SPECT), stress echocardiogram, and exercise treadmill ECG (GXT).
2.4. Outcomes
The primary outcome was myocardial ischemia, which was objectively defined as ≥70 % stenosis in an epicardial coronary artery identified during invasive angiography, coronary intervention (either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)), or 30-day major adverse cardiac event (MACE) defined as all-cause mortality, myocardial infarction, or coronary revascularization. The study staff collected clinical data and assessed MACE by performing ≥30-day follow-up phone call and medical record review.
The time-to-test (TTT) was measured as the interval between the time of the patient's ED encounter with their provider and the start of their MCG and their first SOC non-invasive stress test. Patient satisfaction was measured in patients who underwent both MCG and stress testing using a five-point Likert scale. Patients self-reported their satisfaction with each testing procedure by selecting one of the following response options: “Very Dissatisfied,” “Dissatisfied,” “Neutral,” “Satisfied,” and “Very Satisfied.”
2.5. Sample size calculation
A sample size of N = 22 was calculated using a one-sided paired t-test at an alpha level of 0.025 and a non-inferiority margin of 7.5 % for the sensitivity of detecting myocardial ischemia at 80 % power. Assuming a 15 % prevalence of myocardial ischemia, n = 147 subjects were required for non-invasive coronary testing to determine non-inferiority of the sensitivity outcome between MCG and SOC non-invasive cardiac testing. Additionally, n = 125 subjects were needed to undergo non-invasive testing and found to be without myocardial ischemia to demonstrate non-inferiority for specificity. Ultimately, 390 subjects were enrolled to ensure sufficient power to meet primary and secondary endpoints.
2.6. Statistical analysis
The primary analysis aimed to compare the sensitivity and specificity of MCG (SnMCG and SpMCG) with SOC non-invasive testing (SnSOC and SpSOC) for detecting myocardial ischemia. Clinically relevant non-inferiority would be established if the lower confidence bound at the 97.5 % confidence level for the estimated difference in sensitivities (SnMCG - SnSOC) or specificities (SpMCG - SpSOC) is <7.5 % and 10 %, respectively. Hypothesis testing was performed using a one-sided normal approximation test at an alpha level of 0.025. The datasets used for analysis included clinical, MCG, procedural, and outcome data expressed as binary, categorical, and continuous variables.
The inter-rater agreement among the three MCG scan readers was assessed using Krippendorff's alpha. A value >0.8 is considered excellent, and between 0.67 and 0.8 is considered very good. A 95 % confidence interval was calculated using the bootstrapping algorithm. Discrepancies in MCG interpretation were adjudicated by accepting the majority interpretation of 2 of 3 physicians.
The time-to-test (TTT) was calculated for both MCG and SOC non-invasive stress test. The overall TTT was determined as the difference between the time of the patient's ED encounter with their provider and the start of their diagnostic test. The TTT for MCG was compared to the TTT for their first non-invasive stress test using a two-sided paired t-test. Descriptive statistics were used to summarize the time required for each diagnostic procedure in terms of continuous variables for both MCG and stress test.
The median numeric Likert scale responses were calculated to assess patient satisfaction with MCG and stress testing across four categories, total time, comfort, recovery, and overall experience. The Likert scale response categories for patient satisfaction were summarized for MCG and stress testing using the median (IQR) score values for each scale.
3. Results
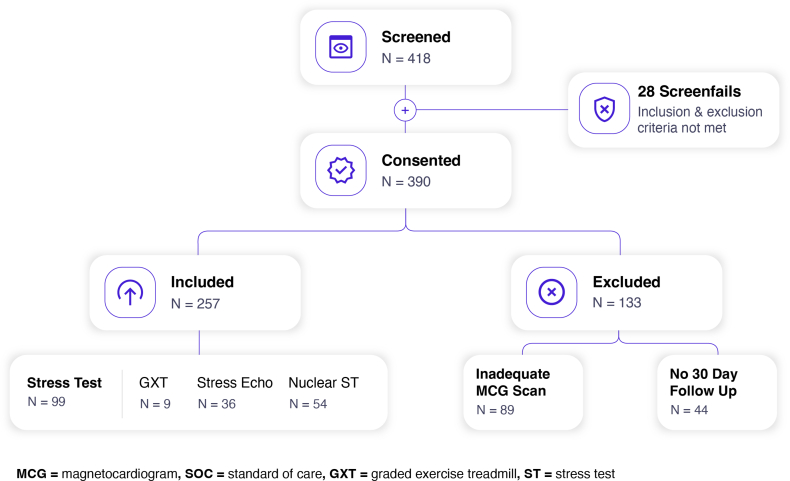
A total of 390 patients were included, 174 (45 %) were female, and the average age was 59.1 ± 12 years. Other demographic features are listed in Table 1. Overall, 89 had uninterpretable MCG scans due to interference from metal in the patient (e. g., dental fillings) or other interference, resulting in 301 MCG scans available for analysis. The Consort Diagram is shown in Fig. 3.
Table 1.
Baseline characteristics of subjects (N = 301).
| Overall |
No ischemia |
Ischemia |
P-value | |
|---|---|---|---|---|
| n | 301 | 259 | 42 | |
| Demographics | ||||
| Age (yrs.), median [Q1,Q3] | 58.0 [50.0,66.0] | 58.0 [49.0,65.0] | 63.5 [56.0,69.8] | 0.005 |
| Female sex, n (%) | 127 (42.2 %) | 113 (43.6 %) | 14 (33.3 %) | 0.278 |
| Race, n (%) | 0.138 | |||
| White Origins in Europe, Middle East, North Africa | 146 (48.5) | 119 (45.9) | 27 (64.3) | |
| Black/African American | 143 (47.5) | 129 (49.8) | 14 (33.3) | |
| Indigenous and/or Alaskan Native | 5 (1.7) | 5 (1.9) | ||
| Mixed race | 4 (1.3) | 4 (1.5) | ||
| Asian | 3 (1.0) | 2 (0.8) | 1 (2.4) | |
| Ethnicity, n (%) | 0.373 | |||
| Not Hispanic or Latino | 290 (96.3) | 248 (95.8) | 42 (100.0) | |
| Hispanic or Latino or Spanish origin | 11 (3.7) | 11 (4.2) | ||
| Cardiovascular risk factors | ||||
| BMI, median [Q1,Q3] | 30.9 [26.8,35.4] | 30.9 [26.7,35.8] | 30.5 [26.8,34.0] | 0.867 |
| Diabetes, n (%) | 68 (22.6) | 56 (21.6) | 12 (28.6) | 0.424 |
| Hypertension, n (%) | 217 (72.1) | 184 (71.0) | 33 (78.6) | 0.410 |
| Hyperlipidemia, n (%) | 165 (54.8) | 135 (52.1) | 30 (71.4) | 0.030 |
| Current or former smoker, n (%) | 167 (55.5) | 141 (54.4) | 26 (61.9) | 0.462 |
| Family history of CVD, n (%) | 100 (33.2) | 80 (30.9) | 20 (47.6) | 0.050 |
| Medications, n (%) | ||||
| Statins | 127 (42.2) | 104 (40.2) | 23 (54.8) | 0.107 |
| Beta blockers | 113 (37.5) | 89 (34.4) | 24 (57.1) | 0.008 |
| Aspirin | 85 (28.2) | 68 (26.3) | 17 (40.5) | 0.086 |
| Calcium channel blockers | 64 (21.3) | 52 (20.1) | 12 (28.6) | 0.296 |
| ACE-I/ARB | 53 (17.6) | 50 (19.3) | 3 (7.1) | 0.089 |
| Nitrates | 48 (15.9) | 35 (13.5) | 13 (31.0) | 0.008 |
| Prior cardiac interventions, mean (SD) | ||||
| Number of previous stents | 2.4 (1.9) | 1.9 (1.4) | 3.4 (2.4) | 0.019 |
This table depicts the demographics and baseline characteristics of the two groups where ischemia was defined as ≥70 % epicardial coronary artery stenosis, revascularization within 30 days, or 30-day major adverse cardiac events (MACE).
Fig. 3.
Consort diagram.
MCG = magnetocardiogram, SOC = standard of care, GXT = graded exercise treadmill, ST = stress test.
3.1. Efficacy of magnetocardiography compared to SOC non-invasive stress testing
The sensitivity and specificity of MCG was 66.7 % (95 % CI 50.5 %–80.5 %) and 57.1 % (95 % CI 50.9 %–63.3 %), respectively. This is compared to a sensitivity of 66.7 % (95 % CI 29.9 %–92.5 %) and a specificity of 89.9 % (95 % CI 81.7 %–95.3 %) for the composite SOC group for detecting myocardial ischemia. Sample size and performance of each individual modality are listed in Table 2. Within the group that underwent both stress testing and had interpretable MCG (n = 70), there were 6 subjects (8.6 %) who had ischemia. Four of the six subjects were detected by stress testing and MCG. Two of the six (33.3 %) subjects were missed by nuclear stress testing, while MCG identified both patients with ischemia. Both individuals had negative serial troponins. One had 100 % (distal LAD) and 90 % (first diagonal) stenosis and underwent PCI. The other patient had multivessel disease including the left main, left anterior descending, left circumflex and right coronary artery, and 100 % stenosis on at least one of the culprit vessels and underwent CABG surgery (Table 3). Assessment for ischemia up to 30 days post-discharge resulted in a follow-up completion rate of 85.4 %. The Inter-rater agreement among the readers for MCG analysis was 0.7911 95 % CI (0.7236–0.852), with all three adjudicators having the same interpretation in 84 % of the cases.
Table 2.
Sensitivity and specificity with 95 % confidence intervals (CI) for MCG and SOC non-invasive cardiac testing.
| Diagnostic test | Sensitivity (95 % CI) | Specificity (95 % CI) |
|---|---|---|
| MCG (301) | 66.7 % (50.5–80.45) | 57.1 % (50.9–63.3 %) |
| Stress testing (99) | 66.7 % (29.9–92.5 %) | 89.9 % (81.7–95.3 %). |
| GXT (9) | N/A* | 100 % (63.4–100 %) |
| Stress echo (36) | 100 % (2.5–100 %) | 88.6 % (73.3–96.8 %) |
| Nuclear ST (54) | 62.5 % (24.5–91.5 %) | 87.0 % (73.7–95.15) |
MCG = magnetocardiogram, SOC = standard of care, GXT = graded exercise treadmill, ST = stress test.
Table 3.
Concordance of stress testing and interpretable MCG.
| Concordance table: stress test and MCG N = 70 |
MCG + n = 41 |
MCG − n = 29 |
|---|---|---|
| Stress Test + n = 10 |
10 4 ischemic: • 6 Nuclear ST (3 ischemic) • 4 Stress Echo (1 ischemic) |
0 0 ischemic |
| Stress Test − n = 60 |
31 2 ischemic: • 16 Nuclear ST (2 ischemic) • 11 Stress Echo (0 ischemic) • 4 Exercise ST (0 ischemic) |
29 0 ischemic: • 11 Nuclear ST • 13 Stress Echo • 5 Exercise ST |
There were 70 cases where SOC (nuclear stress, stress echo, or exercise stress test) was performed and an interpretable MCG was available. There was agreement between stress testing and MCG in 39 cases and disagreement in 31 cases. There were six subjects (6/70) that had ischemia. MCG correctly identified all six of these individuals as having ischemia. There were 2 false negative stress tests (33 %, 2/6). These were both nuclear stress tests. In the two patients with false negative nuclear stress tests, subsequent invasive coronary angiography revealed 100 % stenosis in one patient who underwent PCI, and the other patient had multivessel obstructive disease with 100 % stenosis in one vessel and >70 % stenosis in multiple other vessels and required CABG.
3.2. Time to test
The mean time-to-test (TTT) for MCG were compared to those of stress test. The mean (± sd) TTT for MCG was 3.2 (±1.9) compared to the stress test of 22.8 (±15.2) hours. These results demonstrate that we were able to perform MCG much sooner than that of SOC non-invasive stress testing.
3.3. Patient satisfaction and preference for MCG
The median patient satisfaction rating for the MCG test across all four questions was 5 (very satisfied) compared to 3 (neutral) for stress testing. The results with the interquartile values are listed in Table 4. These results demonstrate a significantly better reported patient experience with the MCG procedure when compared to stress testing across all four criteria.
Table 4.
Median Likert rating for MCG and stress testing.
| Variable of patient experience rating | MCG (n = 30) | Stress test (n = 30) |
|
|---|---|---|---|
| Total time spent from test preparation to completion | Median | 5 | 3 |
| IQR (Q1,Q3) | 1 (4,5) | 2 (2,4) | |
| Your comfort during the test | Median | 5 | 3 |
| IQR (Q1,Q3) | 0 (5,5) | 2 (2,4) | |
| Your recovery after the test | Median | 5 | 3 |
| IQR (Q1,Q3) | 0 (5,5) | 1 (3,4) | |
| Your overall experience | Median | 5 | 3 |
| IQR (Q1,Q3) | 0 (5,5) | 2 (2,4) | |
4. Discussion
When comparing MCG to SOC non-invasive stress testing, MCG demonstrated comparable sensitivity but reduced specificity. Within the cohort of patients that underwent stress testing, MCG identified all those with ischemia by SOC testing. MCG identified two additional patients with ischemia that were not detected by nuclear stress testing, both having 100 % stenosis with one patient requiring PCI and stent, and the other either requiring CABG.
Some non-invasive stress testing modalities are recognized to have improved sensitivity and specificity over others, such as nuclear stress testing. However, this comes at the added cost of requiring more time to perform and involves the use of radiation or medications to induce vasodilation. MCG, by comparison, is a non-invasive modality that is performed at rest with no radiation and no medication.
In terms of throughput and resource utilization, the implementation of an MCG pathway could significantly reduce patients' length of stay (LOS). The median TTT for patients undergoing MCG was 2.9 h, whereas it was 22.9 h for all stress tests. These values are independent of the time taken to perform the tests. While the test performance time from initiation to completion of stress test was not measured, the time to perform an MCG from initiation to completion is approximately 5 min. Excluding study performance time, this substantially reduced TTT and potential reduction in LOS is paramount in the current healthcare landscape, characterized by limited resources, overcrowded emergency departments, and increased boarding of admitted and observed patients who remain in the ED.
Patient satisfaction scores serve as a key administrative benchmark in healthcare. When comparing the overall satisfaction scores between MCG and Stress testing, MCG yielded significantly higher patient satisfaction across all four evaluated categories.
Given that MCG is performed at rest without medication, contrast, or radiation, and has comparable sensitivity in detecting ischemia in ED sACS patients with significantly faster TTT and better patient satisfaction, adoption of MCG in the ED workflow may have many advantages. Although more rigorous studies are needed, MCG has the potential to be a “rule-out” ischemia modality, with improved ED throughput and better overall patient experience.
5. Limitations
While current American College of Cardiology guidelines allow for patients with a HEART score of 3 to be safely discharged with serial negative hsTn, many of these patients are kept for further testing or observation, possibly due to variations in ED physician practices, concerns about follow-up, timeliness of stress tests, and barriers to outpatient testing. Since this practice is not uncommon, subjects with a HEART score of 3 were therefore included in this study and may have contributed to the low rate of positive SOC myocardial ischemia diagnoses in our cohort. Future studies will need to identify the performance of MCG in higher “at risk” populations.
While MCG scan analysis is dependent on adequate signal to noise magnetic waveform analysis, there were 89 subjects that had inadequate or uninterpretable scans. Analysis of these scans revealed multiple potential reasons including failure to identify metal causing interference (i.e., extensive metal dental fillings) and external electromagnetic interference. Further evaluation is needed to improve the MCG scan yield. Additionally, patients with intraventricular conduction delay may have a negative impact on MCG interpretation like cases of left bundle branch block interfering with interpretation of an ECG. This requires further investigation.
Patients with acute STEMI and/or hemodynamically unstable patients were excluded for safety reasons and the need for immediate intervention. The exclusion of these potentially very sick patients may impact the specificity of our results. They were, however, also excluded from non-invasive stress testing.
The higher patient satisfaction scores in the MCG cohort may be explained by the shorter length of testing needing to complete the MCG as compared to most types of SOC non-invasive testing. Prospective validation of this finding may need to wait until there is increased adoption and availability of this technology.
Lastly, as specific non-invasive stress testing was not specified by our study protocol, it is difficult to determine how test selection could result in outcome variation. For example, of the nine exercise stress tests, all were negative. The low sample size reflects the limited use of this test in the real world and does not allow for statistical analysis individually. Similarly, of the 36 stress echoes, 35 were negative. The sample was highly skewed with limited prevalence of disease preventing accurate assessment of sensitivity and specificity. Future studies using a standard evaluation protocol is warranted.
6. Conclusion
In intermediate risk ED patients with sACS, MCG had comparable sensitivity, though reduced specificity, for the diagnosis of acute myocardial ischemia compared to SOC non-invasive stress testing modalities. In this intermediate risk ED population, ACC/AHA guidelines recommend non-invasive stress testing and serial troponin assessment. The reduced specificity must be balanced against comparable sensitivity for a very efficient non-invasive test in the ED setting.
A negative resting MCG takes <5 min to complete and has the same likelihood of ruling out coronary ischemia without the need or risk of exercise, pharmaceuticals, or radiation associated with current stress modalities. MCG has high interrater reliability and demonstrates faster TTT and improved patient satisfaction. Further research should evaluate more in-depth comparison with specific non-invasive diagnostic tests in cohorts at higher risk of ACS and measure the financial impact of implementing MCG in the ED workflow.
Ethical statement
Informed consent was obtained from all individuals in the study. The research was approved by the institutional review board of all the participating study sites. The study complied with all institutional policies, all state and federal regulations, and was conducted in accordance with the approved protocol, HIPPA privacy protections, and the Code of Ethics of the World Medical Association (Declaration of Helsinki) international research principles under the International Code of Harmonization (ICH) Good Clinical Practice (GCP).
This study was funded by a research grant from Genetesis, Inc. The study sponsor participated in developing the study design. A professional biostatistician performed the data analysis. The study investigators and all authors provided critical input for the study design and methodology, had free access to the study data, led data analysis and interpretation, had sole discretion in the writing of the report, and made the decision to submit the manuscript for publication.
Role of the sponsor
The study sponsor participated in developing the study design. A professional biostatistician performed the data analysis. The study investigators and all authors provided critical input for the study design and methodology, had free access to the study data, led data analysis and interpretation, had sole discretion in the writing of the report, and made the decision to submit the manuscript for publication.
CRediT authorship contribution statement
Sharon E. Mace: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. W. Frank Peacock: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. Jason Stopyra: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. Simon A. Mahler: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. Claire Pearson: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. Margarita Pena: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. Carol Clark: Writing – review & editing, Writing – original draft, Investigation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.National Hospital Ambulatory Medical Care Survey: 2021 Emergency Department Summary Tables. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2021-nhamcs-ed-web-tables-508.pdf Published online 2021.
- 2.American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93–e621. doi: 10.1161/CIR.0000000000001123. Feb 21. (Epub 2023 Jan 25. Erratum in: Circulation. 2023 Feb 21;147(8):e622. Erratum in: Circulation. 2023 Jul 25;148(4):e4) [DOI] [PubMed] [Google Scholar]
- 3.Committee Writing, Kontos M.C., de Lemos J.A., et al. ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2022 doi: 10.1016/j.jacc.2022.08.750. Published online October 6, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Camm A.J., Henderson R., Brisinda D., Body R., Charles R.G., Varcoe B., Fenici R. Clinical utility of magnetocardiography in cardiology for the detection of myocardial ischemia. In. J. Electrocardiol. 2019;57 doi: 10.1016/j.jelectrocard.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Roth B.J., Wikswo J.P. Electrically silent magnetic fields. Biophys. J. 1986;50:4. doi: 10.1016/S0006-3495(86)83513-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dutz S., Bellemann M.E., Leder U., Haueisen J. Passive vortex currents in magneto- and electrocardiography: comparison of magnetic and electric signal strengths. Phys. Med. Biol. 2006;51(1) doi: 10.1088/0031-9155/51/1/011. [DOI] [PubMed] [Google Scholar]
- 7.Brockmeier K., Schmitz L., De Jesus Bobadilla Chavez J., et al. Magnetocardiography and 32-lead potential mapping: repolarization in normal subjects during pharmacologically induced stress. J. Cardiovasc. Electrophysiol. 1997;8(6) doi: 10.1111/j.1540-8167.1997.tb01824.x. [DOI] [PubMed] [Google Scholar]
- 8.Baule G., McFee R. Detection of the magnetic field of the heart. Am. Heart J. 1963;66(1) doi: 10.1016/0002-8703(63)90075-9. [DOI] [PubMed] [Google Scholar]
- 9.L. Chaikovsky J.K.T.H., et al. Proceedings of the 12th International Conference on Biomagnetism. Biomag; 2001. Detection of coronary artery disease in patients with normal or unspecifically changed ECG on the basis of magnetocardiography; pp. 565–568. Published online. [Google Scholar]