Abstract
Obesity significantly increases the risk of developing atrial fibrillation (AF) and atrial flutter (AFL) and evidence from randomized trials indicates that weight loss may reduce the burden of AF/AFL in obese patients; however, the relationship between obesity and healthcare resource utilization in AF/AFL patients is lacking. We sought to assess this relationship in patients with newly diagnosed AF/AFL in a nationally representative cohort of the United States by using the MarketScan® claims database. International Classification of Diseases, Tenth Revision [ICD 10] diagnosis codes were used to select individuals with a new diagnosis of AF/AFL in 2017 and 2018, adjudicate baseline variables and to classify them according to obesity status. Patients were followed for two years at which point all data was censored. The primary outcome of the study was hospitalizations due to AF/AFL. Cox proportional hazards regression models were used to assess the adjusted hazard ratio for obese versus non-obese patients. There were 55,271 patients with new onset AF/AFL, which included 43,314 (78.4 %) who were non-obese and 11,957 (21.6 %) who were obese. There were significantly more males than females among non-obese (65.3 % vs. 34.7 %) and obese individuals (62.3 % vs. 37.7 %). The average age (SD) was similar in the non-obese (54.5 (9.7)) and obese cohorts (54.7 (8.4)), respectively. The incidence of Emergency Department visits (4.0 % vs. 6.5 %), hospitalizations (5.5 % vs. 10.7 %), cardioversions (6.6 % vs. 12.7 %), and ablation procedures (5.3 % vs. 8.6 %) were significantly increased among obese patients.
Keywords: Atrial fibrillation, Obesity, Hospitalization, Cardioversion, Ablation, Resource utilization
1. Introduction
The prevalence of Atrial fibrillation/atrial flutter (AF/AFL) is increasing as our population ages. Approximately 33 million people have been diagnosed with atrial fibrillation worldwide with >3 million cases diagnosed in the United States alone. The number of cases in the US is estimated to rise to 12.1 million by 2030. In addition to a high prevalence, AF/AFL is associated with high healthcare resource utilization (HRU) [[1], [2], [3], [4]]. Data suggests that hospitalization cost of AF/AFL in the US was $6.65 billion annually in addition to $1.53 billion in outpatient cost and $235 million for medication cost. These are likely underestimates given the impact of AF/AFL on comorbid conditions such as stroke and heart failure [1].
Like AF/AFL, obesity is also increasing and it seems to have direct relationship with AF/AFL. The Center for Disease Control and Prevention (CDC) report that 42.4 % of the US population are obese; it was 30.5 % two decades prior and it cost the US $147 billion annually [4]. Obese patients have twice the prevalence of AF/AFL compared to non-obese patients and there is a graded relationship between body mass index (BMI) and the evolution of paroxysmal to permanent AF/AFL [[5], [6], [7]]. The relationship between obesity and AF/AFL is thought to be secondary to the structural and electrical remodeling of the atria that occurs in obese patients [8].
Despite the frequency of AF/AFL and obesity, there is limited research on the relationship between obesity and AF/AFL-related healthcare resource utilization (HRU). We sought to assess this relationship in a nationally representative sample of individuals with new onset AF/AFL.
2. Methods
This retrospective descriptive analysis utilized MarketScan® Commercial Claims and Encounters database. Those included were patients with new onset AF/AFL (according to the International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10] codes I48.0x, I48.1x, I48.2x, I48.9x) in 2017 and 2018. This cohort was then split into an obese cohort according to diagnosis codes (ICD-10 E66.8, E66.9, Z68.30, Z68.31, Z68.32, Z68.33, Z68.34, Z68.35, Z68.36, Z68.37, Z68.38, Z68.39, Z68.40, Z68.41, Z68.42, Z68.43, Z68.44, Z68.45) or non-obese. We were unable to stratify by degree of obesity due to inconsistent coding of obesity sub-classifications. Obesity was defined as having a body mass index of 30 or more or obese using ICD-10 codes. Participants were required to have a continuous enrollment from at least 1 year before the index. A 1-year clean period (2016) was used to ensure our index date reflected true new-onset AF/AFL. Patients lacking the above diagnosis codes and not in our predefined time periods were excluded.
The primary outcome of interest was AF/AFL related hospitalizations in the obese cohort compared to the non-obese cohort as hospitalization is typically associated with the highest cost among healthcare encounters. To be included as an AF/AFL related hospitalization, AF/AFL had to be either the primary or secondary diagnosis for the admission.
Secondary outcomes assessed included cardioversions, ablations, transesophageal echocardiograms, and emergency department visits. The Current Procedural Terminology (CPT®) codes were used to define electrical cardioversion (92,960 and 92,961), catheter ablation (93,656, 93,662, 93,613, and 93,623), and transesophageal echocardiogram (TEE) (93318) procedures. To be included as an AF/AFL related emergency department visit, AF/AFL had to be either the primary or secondary diagnosis for the visit.
The CHA2DS2VASc scores were documented using ICD-10 codes: Congestive heart failure (I50.9, I11.0, I50.30, I50.20), hypertension (I10, I11.9, I12.9, I15.7, I15.8, I97.3, O16.9), diabetes (E10.9, E11.319, E11.622, E11.9, E13.9, O24.919, R73.03), prior TIA/CVA (G45.0, G45.1, G45.9, Z86.69, Z86.73, I63.9, I69.319, I69.32, I69.322, I69.328, I69.359, I69.391, I69.392, I69.398, I69.993), vascular disease (I25.10, I25.118, I25.119, I25.810, I25.811, I70.0, I73.9, I87.2, E10.51, E11.51, E13.51) were recorded. Sex for each patient was also documented. All patients in our cohorts were <66 years of age by convention when using MarketScan® Commercial Claims and Encounters database. Based on this information, the CHA2DS2VASc score was calculated for each patient.
Demographic and clinical characteristics at baseline were summarized using descriptive statistics (mean and standard error for continuous variables and percent for categorical variables). Cox proportional hazard regression models showing hazard ratios (HR) and 95 % confidence intervals (CIs) of hospitalization, cardioversion, ablation, TEE, and ED visit, for the association between obese status and the aforementioned outcomes of interest adjusting for sex, age, US regions, and comorbidity conditions listed above in the CHA2DS2VASc score.
Data was analyzed in SAS software version 9.4 (SAS Institute Inc.; Cary NC) and R software version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria) at a two-tailed alpha level of 0.05.
3. Results
There were 55,271 patients with new onset AF/AFL, which included 43,314 (78.4 %) who were non-obese and 11,957 (21.6 %) who were obese. There were significantly more males than females among non-obese (65.3 % vs. 34.7 %) and (62.3 % vs. 37.7 %) among obese individuals. The average age (SD) was similar at 54.5 (+/− 9.7) in the non-obese and 54.7 (+/− 8.4) in the obese cohort (Table 1).
Table 1.
Basic characteristics of participants according to obese status at baseline.
| Characteristics | Participants, no. (%) |
p-value | |
|---|---|---|---|
| Non-obese (N = 43,314) | Obese (N = 11,957) | ||
| Age, mean (SD), y | 54.5 ± 9.7 | 54.7 ± 8.4 | 0.008 |
| Age groups | <0.001 | ||
| 1–17 | 263 (0.6) | 7 (0.1) | |
| 18–34 | 1950 (4.5) | 405 (3.4) | |
| 35–44 | 3644 (8.4) | 1009 (8.4) | |
| 45–54 | 10,115 (23.4) | 3110 (26.0) | |
| 55–65 | 27,342 (63.1) | 7426 (62.1) | |
| Sex, % | <0.001 | ||
| Male | 28,286 (65.3) | 7453 (62.3) | |
| Female | 15,028 (34.7) | 4504 (37.7) | |
| Region of US, % | <0.001 | ||
| South | 19,669 (45.4) | 5745 (48.0) | |
| West | 5939 (13.7) | 1191 (10.0) | |
| North Central | 8908 (20.6) | 2674 (22.4) | |
| Northeast | 8716 (20.1) | 2328 (19.5) | |
| Unknown | 82 (0.2) | 19 (0.1) | |
| CHF, % | 971 (2.2) | 379 (3.2) | <0.001 |
| Hypertension, % | 16,748 (38.7) | 6426 (53.7) | <0.001 |
| Diabetes, % | 6291 (14.5) | 2614 (21.6) | <0.001 |
| Vascular Disease, % | 4587 (10.6) | 1542 (12.9) | <0.001 |
| Prior TIA/CVA, % | 1068 (2.5) | 358 (3.0) | 0.001 |
| CHA2DS2VASc, % | <0.001 | ||
| Score = 0 | 13,946 (32.2) | 2608 (21.8) | |
| Score = 1 | 17,302 (40.0) | 4589 (38.4) | |
| Score ≥ 2 | 12,066 (27.8) | 4760 (39.8) | |
Abbreviation: CHF: Congestive Heart Failure.
The obese population had a statistically significant higher proportion of heart failure (3.2 % vs. 2.2 %, p < 0.001), hypertension (53.7 % vs. 38.7 %, p < 0.001), diabetes (21.6 % vs. 14.5 %, p < 0.001), and vascular disease (12.9 % vs. 10.6 %, p < 0.001). There were more TIA/CVA events (3.0 % vs. 2.5 %, p = 0.001) in the obese cohort compared to the non-obese cohort (Table 1).
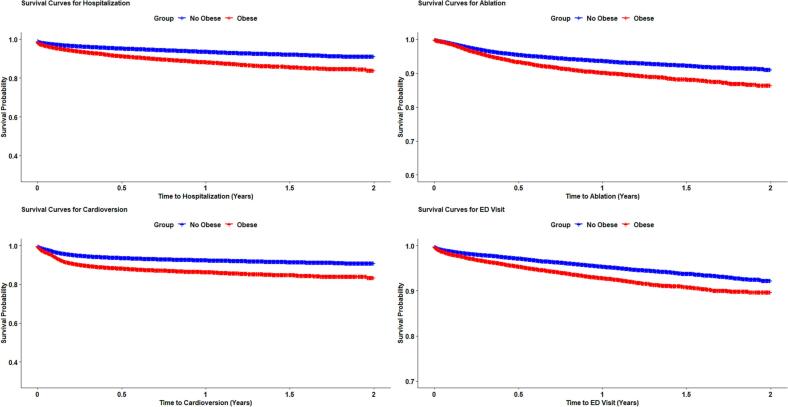
Compared with individuals without obesity, the rate of Emergency Department visits (4.0 % vs. 6.5 %), hospitalizations (5.5 % vs. 10.7 %), cardioversions (6.6 % vs. 12.7 %, p < 0.001), and ablation procedures (5.3 % vs. 8.6 %, p < 0.0001) were significantly higher (Fig. 1). Obese individuals had significantly higher risk of hospitalizations (adjusted Hazard Ratio (HR): 1.86; 95 % CI: 1.74, 1.99), cardioversions (HR: 2.00; 95 % CI: 1.86.1, 2.13), ablation procedures (HR: 1.62; 95 % CI: 1.50, 1.74), and emergency department visits (HR: 1.60; 95 % CI: 1.47, 1.74) compared to the non-obese cohort (Table 2). No significant association was found for TEE, which could be due to a smaller sample size, (HR: 1.39; 95 % CI: 0.73, 2.67) (Table 2). Regression analysis was performed for the calculated hazard ratios. Both cohorts were followed for two years after the diagnosis of AF/AFL was made.
Fig. 1.
Non -Obese Vs. Obese Survival Curves.
Table 2.
Cox proportional hazards regression models showing hazard ratios (HR) and 95 % confidence intervals of hospitalization, cardioversion, ablation, TEE, and ED visit, according to obese status (N = 55,271).
| Outcomes | Participants, no. (%) |
|
|---|---|---|
| Non-obese (N = 43,314) | Obese (N = 11,957) | |
| Hospitalization | ||
| No. of events (%) | 2393 (5.5) | 1278 (10.7) |
| Incidence rates (95 % CI), per 1000 PY | 67.1 (64.5, 69.8) | 124.5 (117.9, 131.5) |
| Model 1 | 1 (Ref) | 1.89 (1.77, 2.03) |
| Model 2 | 1 (Ref) | 1.86 (1.74, 1.99) |
| Cardioversion | ||
| No. of events (%) | 2866 (6.6) | 1517 (12.7) |
| Incidence rates (95 % CI), per 1000 PY | 81.5 (78.5, 84.5) | 151.5 (144.1, 159.4) |
| Model 1 | 1 (Ref) | 1.91 (1.80, 2.04) |
| Model 2 | 1 (Ref) | 2.00 (1.86, 2.13) |
| Ablation | ||
| No. of events (%) | 2295 (5.3) | 1022 (8.6) |
| Incidence rates (95 % CI), per 1000 PY | 64.2 (61.6, 66.9) | 97.6 (91.8, 103.8) |
| Model 1 | 1 (Ref) | 1.55 (1.44, 1.67) |
| Model 2 | 1 (Ref) | 1.62 (1.50, 1.74) |
| TEE | ||
| No. of events (%) | 33 (0.08) | 13 (0.11) |
| Incidence rates (95 % CI), per 1000 PY | 0.89 (0.63, 1.25) | 1.16 (0.68, 2.01) |
| Model 1 | 1 (Ref) | 1.38 (0.72, 2.61) |
| Model 2 | 1 (Ref) | 1.39 (0.73, 2.67) |
| Emergency department visit | ||
| No. of events (%) | 1725 (4.0) | 774 (6.5) |
| Incidence rates (95 % CI), per 1000 PY | 47.7 (45.5, 50.0) | 72.7 (67.7, 78.0) |
| Model 1 | 1 (Ref) | 1.55 (1.42, 1.69) |
| Model 2 | 1 (Ref) | 1.60 (1.47, 1.74) |
Model 1: Unadjusted.
Model 2: adjusted for age (years), sex (male/female), region of US (Northeast, North Central, West, South, Unknown), diabetes, hypertension, heart failure, vascular disease, and prior TIA/CVA (each yes/no).
4. Discussion
The association of obesity and AF/AFL has been well established. Obesity is not only associated with new-onset AF/AFL but a higher prevalence of recurrent and permanent AF/AFL [5,8]. The primary findings of our retrospective analysis suggest higher risk of hospitalizations, cardioversions, and ablation procedures in obese patients with AF/AFL compared to non-obese. It was also not surprising to see higher rates of comorbid conditions such as heart failure, hypertension, diabetes, and vascular disease in the obese cohort. The relationship of obese patients undergoing a higher rate of Emergency Department visits, hospitalizations, and AF/AFL related procedures infers a significantly higher healthcare resource utilization (HRU) and further validates the importance of emphasizing weight loss to our patients.
Obesity has been correlated to a significant number of additional acute and chronic medical conditions aside from AF/AFL. A nationally representative cross-sectional survey with 16,884 participants confirmed this observation [11]. Based on their survey, they found prevalence ratios highest for type 2 diabetes and gallbladder disease however there was also a higher prevalence of hypertension and osteoarthritis [11]. Obesity can also produce and contribute to the severity of obstructive sleep apnea [12] for which a multitude of comorbid conditions can be traced.
Perhaps the strongest correlation for obesity is its direct and indirect link to a plethora of cardiovascular disease. Obesity directly impacts the cardiovascular system through structural and functional adaptations to acclimatize excess body weight [14]. Additionally, adipokine release seen in the obese leads to a chronic state of inflammation and interferes with vascular homeostasis [14]. Through the body's adaptation to excess weight various pathologies are born of which AF/AFL is no exception.
Numerous trials have confirmed a high prevalence of new onset, recurrent, and permanent atrial fibrillation in the obese population [8,9], however, there is limited data demonstrating increased resource utilization in these patients [10]. Augmenting our knowledge of the associations of AF/AFL and obesity with HRU will support healthcare systems incentive for weight loss.
Progressive weight loss has demonstrated significant reduction in AF/AFL burden among obese patients and has been correlated to long-term freedom from AF/AFL when the weight loss is maintained [8,9]. This further validates the importance of emphasizing weight loss to our patients.
This retrospective analysis utilizing claims data is hypothesis generating but is limited in forming conclusions. The sizable number of patients included and simplicity of our analysis contribute to its validity and strength. We acknowledge that our observations are limited to a younger population and the same relationships may not apply to individuals older than 65. Additionally, despite the effort to account for the comorbidities seen in the obese population, the impact of confounders cannot be completely excluded and thus our findings do not conclude an independent relationship between obesity and the observed outcomes.
Our analysis supports the hypothesis that obese patients with new onset AF/AFL have significantly higher HRU than non-obese patients. The higher resource burden in the obese population seems to be driven primarily by higher rates of hospitalization as well as cardioversion and ablation procedures. This data may help catalyze additional focus on treating the obesity epidemic and concentrate our understanding on the cause for increased healthcare resources used in obese patients with new onset AF/AFL.
Ethical statement
Our retrospective descriptive analysis utilized decoded claims data and thus informed consent was not applicable.
CRediT authorship contribution statement
Jonathan Norton: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Andrew Foy: Writing – review & editing, Writing – original draft, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Djibril M. Ba: Writing – review & editing, Writing – original draft, Supervision, Software, Methodology, Formal analysis, Data curation, Conceptualization. Guodong Liu: Writing – review & editing, Writing – original draft, Supervision, Software, Resources, Methodology, Investigation, Data curation, Conceptualization. Doug Leslie: Software, Methodology, Formal analysis, Data curation, Conceptualization. Yue Zhang: Writing – review & editing, Writing – original draft, Validation, Data curation. Gerald V. Naccarelli: Writing – review & editing, Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Chung M., Refaat M., Shen W., et al. Atrial fibrillation. J. Am. Coll. Cardiol. 2020 Apr;75(14):1689–1713. doi: 10.1016/j.jacc.2020.02.025. https://www.jacc.org/doi/full/10.1016/j.jacc.2020.02.025 [DOI] [PubMed] [Google Scholar]
- 2.Delaney J.A., Yin X., Fontes J.D., Wallace E.R., Skinner A., Wang N., Hammill B.G., Benjamin E.J., Curtis L.H., Heckbert S.R. Hospital and clinical care costs associated with atrial fibrillation for Medicare beneficiaries in the Cardiovascular Health Study and the Framingham Heart Study. SAGE Open Med. 2018 Feb 20;6 doi: 10.1177/2050312118759444. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5826000/ PMID: 29511541; PMCID: PMC5826000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naccarelli G.V., Varker H., Lin J., Schulman K.L. Increasing prevalence of atrial fibrillation and flutter in the United States. Am. J. Cardiol. 2009 Dec 1;104(11):1534–1539. doi: 10.1016/j.amjcard.2009.07.022. https://www.sciencedirect.com/science/article/pii/S0002914909013885?via%3Dihub PMID: 19932788. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention 2022. https://www.cdc.gov/obesity/data/adult.html
- 5.Wang T.J., Parise H., Levy D., D’Agostino R.B., Sr., Wolf P.A., Vasan R.S., Benjamin E.J. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004 Nov 24;292(20):2471–2477. doi: 10.1001/jama.292.20.2471. https://jamanetwork.com/journals/jama/fullarticle/199858 PMID: 15562125. [DOI] [PubMed] [Google Scholar]
- 6.Foy A.J., Mandrola J., Liu G., Naccarelli G.V. Relation of obesity to new-onset atrial fibrillation and atrial flutter in adults. Am. J. Cardiol. 2018 May 1;121(9):1072–1075. doi: 10.1016/j.amjcard.2018.01.019. https://www.sciencedirect.com/science/article/pii/S0002914918301619?via%3Dihub Epub 2018 Feb 6. PMID: 29501206. [DOI] [PubMed] [Google Scholar]
- 7.Pandey A., Gersh B.J., McGuire D.K., Shrader P., Thomas L., Kowey P.R., Mahaffey K.W., Hylek E., Sun S., Burton P., Piccini J., Peterson E., Fonarow G.C. Association of body mass index with care and outcomes in patients with atrial fibrillation: results from the ORBIT-AF Registry. JACC Clin. Electrophysiol. 2016 Jun;2(3):355–363. doi: 10.1016/j.jacep.2015.12.001. https://www.sciencedirect.com/science/article/pii/S2405500X15004478?via%3Dihub Epub 2015 Dec 9. PMID: 29766895. [DOI] [PubMed] [Google Scholar]
- 8.Pathak R.K., Middeldorp M.E., Meredith M., Mehta A.B., Mahajan R., Wong C.X., Twomey D., Elliott A.D., Kalman J.M., Abhayaratna W.P., Lau D.H., Sanders P. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: a long-term follow-up study (LEGACY) J. Am. Coll. Cardiol. 2015 May 26;65(20):2159–2169. doi: 10.1016/j.jacc.2015.03.002. https://www.sciencedirect.com/science/article/pii/S0735109715007615?via%3Dihub Epub 2015 Mar 16. PMID: 25792361. [DOI] [PubMed] [Google Scholar]
- 9.Wingerter Rebecca, Steiger Nathaniel, Austin Burrows N.A., Estes Mark. Impact of lifestyle modification on atrial fibrillation. Am. J. Cardiol. 2020;125(2):289–297. doi: 10.1016/j.amjcard.2019.10.018. ISSN 0002-9149. [DOI] [PubMed] [Google Scholar]
- 10.Deshmukh Abhishek, Pant Sadip, Kumar Gagan, Badheka Apurva O., Paydak Hakan. Impact of obesity on atrial fibrillation hospitalization. Int. J. Cardiol. 2012;159(3):241–242. doi: 10.1016/j.ijcard.2012.05.090. ISSN 0167-5273. [DOI] [PubMed] [Google Scholar]
- 11.Must A., Spadano J., Coakley E.H., Field A.E., Colditz G., Dietz W.H. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. https://jamanetwork.com/journals/jama/article-abstract/192030 [DOI] [PubMed] [Google Scholar]
- 12.Hargens T.A., Kaleth A.S., Edwards E.S., Butner K.L. Association between sleep disorders, obesity, and exercise: a review. Nat. Sci. Sleep. 2013 Mar 1;5:27–35. doi: 10.2147/NSS.S34838. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3630986/ PMID: 23620691; PMCID: PMC3630986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koliaki C., Liatis S., Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019 Mar;92:98–107. doi: 10.1016/j.metabol.2018.10.011. https://pubmed.ncbi.nlm.nih.gov/30399375/ Epub 2018 Nov 3. PMID: 30399375. [DOI] [PubMed] [Google Scholar]