Abstract
Because of the COVID-19 pandemic, several health care services, including cardiac rehabilitation (CR), had to transition to virtual delivery, for which formal evaluations are lacking. In this pilot study, we investigated the implementation of a virtual CR program by surveying 30 patients attending virtual CR. Virtual CR was well received, although patients provided recommendations to improve delivery such as offering individual sessions and changing how education materials were delivered. Virtual delivery of CR likely has a role in health care, either independently or as part of a hybrid model; however, further evaluation is required.
Résumé
En raison de la pandémie de COVID-19, plusieurs services de santé, comme la réadaptation cardiaque (RC), ont dû faire la transition vers le mode virtuel, pour lequel il manque d’évaluations formelles. Dans cette étude pilote, nous avons examiné la mise en œuvre d’un programme de RC virtuel en interrogeant 30 patients participant à un tel programme. La RC en mode virtuel a été accueillie favorablement, même si les patients ont formulé des recommandations pour en améliorer la prestation, comme offrir des séances individuelles et changer la façon dont le matériel éducatif est présenté. La prestation de la RC en mode virtuel a probablement un rôle à jouer dans les soins de santé, soit de manière indépendante, soit dans le cadre d’un modèle hybride; cependant, une évaluation plus poussée est requise.
Following an acute cardiac event, patients are advised to undergo cardiac rehabilitation (CR).1 As per the Canadian Heart and Stroke Foundation, CR programs are services provided with the goal to improve quality of life, lifestyle habits, and morbidity following an acute cardiac event.1 CR typically consists of exercise and educational components centred around improving physical fitness and disease self-management. CR has shown multiple benefits such as improvements in weight loss, reduction in nonfatal myocardial infarction (MI) mortality, improvements in anxiety, and positive changes in blood lipid levels.2 However, access and uptake of CR remains a challenge across Canada, resulting in a need to investigate alternative models of delivery that are accessible, equitable, and cost effective.3,4
The COVID-19 pandemic significantly affected the delivery of care in CR services, which resulted in many programs transitioning from in-person care to a virtual-care model.3,4 Previous work has investigated the experiences of those involved in providing and receiving virtual cardiology care. A cross-sectional study conducted at a large tertiary care centre in southwest Ontario found that 75% of cardiac patients were either satisfied or very satisfied with virtual care and that 58% of health care providers used virtual visits for the majority of patient follow-ups.5 Building on such findings, we sought to investigate the experiences of those attending a new virtual CR program at the same tertiary care centre in southwest Ontario.
The effectiveness of virtual CR delivery vs in-person delivery has been demonstrated. In a sample of 162 patients with coronary artery disease, virtual delivery showed a lower per-capita cost in terms of hospital service and medication use compared with in-person care.6 Virtual care also provided greater accessibility of CR services compared with in-person care because it is accessible remotely.7 Further research has demonstrated that virtual CR is more effective at lowering diastolic blood pressure and low-density lipoprotein (LDL) levels and increasing adherence to exercise programs compared with in-person CR.8 Although the efficacy of virtual CR has been thoroughly presented in the literature, patient satisfaction and experiences have not been studied rigourously. At a large tertiary hospital in the southwest health region of Ontario, Canada, a similar transition from in-person CR to virtual CR had to be made because of COVID-19. Therefore, we present patient experiences and satisfaction from those attending virtual CR at this centre.
Methods
Study design
A cross-sectional pilot study was conducted with patients attending a virtual CR program in Hamilton, Ontario, Canada. This collaborative work was undertaken by the Centre for Evidence-Based Implementation (CEBI) and the Cardiac Health and Rehabilitation Clinic (CHRC) at Hamilton Health Sciences. Study data were collected and managed using research electronic data capture (REDCap) tools hosted at the Population Health Research Institute, Hamilton, Ontario, Canada.9,10
Study setting
The newly transitioned virtual CR program in Hamilton (established in November 2021) provided sessions in a group format by video, telephone, or both. Patients were required to use their personal devices and have access to Wi-Fi to attend the sessions, which were hosted on Zoom Video Communications. The virtual CR program was led by a multidisciplinary team of physicians, nurses, kinesiologists, nutritionists, and social workers and consisted of educational sessions that covered topics such as nutrition, supervised exercise, stress management, smoking cessation support, and cardiac health education. During the 5-week course, patients were able to select programs most relevant to their health care needs and received supplementary program information via e-mail that contained exercise activities and access to their medical charts. The primary difference between our virtual and in-person CR program was that virtual CR converted all visits into group sessions and had the sessions done remotely. Further details on the CR program can be found in Supplemental Table S1.
Study participants
All patients attending virtual CR between May and September 2022 received e-mails from a member of the virtual CR staff with an invitation to complete an online survey. Patients were informed that the survey responses would be kept confidential and that participation was voluntary.
Study variables
The online survey was developed by a collaborative team of virtual care specialists, knowledge translation researchers, physicians, patient partners, and the CR staff. Study investigators connected with patient partners known to the Cardiac Health Rehabilitation Clinic to review the survey before dissemination. The survey was informed by previous work by the study team and included 17 questions separated into 3 sections: Demographics, Technology and Privacy, and Patient Experience and Satisfaction.5 The Demographics section included age and racial background. The Technology and Privacy section aimed to identify patient concerns concerning health information privacy and comfort with using technology. Patient answers were provided in the form of multiple-choice questions, 7-point Likert scales (1 = strongly disagree, 7 = strongly agree), and open-text responses. Completion of each question was optional. Overall experience with the virtual CR program was measured on a 10-point scale (1 = very poor experience, 10 = very good experience). Higher numbers on all scales reflected a more positive/favourable response to the program. Additional details on the survey questions and their responses can be found in Supplemental Table S2.
Data analysis
Quantitative data were analyzed using Microsoft Excel. The Likert scales were calculated as a mean ± standard deviation (SD). Qualitative data from open-text responses was analyzed line by line and organized into themes based on the conventional content analysis approach.11 Data analysis was initially conducted by a member of the research team (M.F.) with regular, iterative discussions regarding theme generation with other team members (J.C., K.M.). Consensus on themes was achieved through discussions rather than through inter-rated reliability. Subthemes were determined based on the repetition of key words such as “diet,” “smoking,” and “resources.” Themes were then developed from subthemes and re-evaluated by team members J.C. and K.M. As data collection and analysis were not conducted simultaneously, and interviews or focus group methodology was not used, data saturation was not required.
Ethics
Full ethics review was waived by the Hamilton Integrated Research Ethics Board (HIREB), as this was considered quality-improvement work.
Results
Patient demographic information and response rate
Of the 96 survey emails circulated, responses were received from 30 patients (31% response rate) with 23 patients completing the open-text responses. One-half of the sample population (n = 15) were 60 to 69 years of age, 23% (n = 7) were 70 to 79 years of age, and 10% (n = 3) were 40 to 49 years of age. Sixty-three percent (n = 19) of respondents identified as male; 90% (n = 27) of respondents were from a White European racial-ethnic background. Additional patient demographics can be found in Supplemental Table S3.
Quantitative findings
Patient comfort with technology and sense of privacy
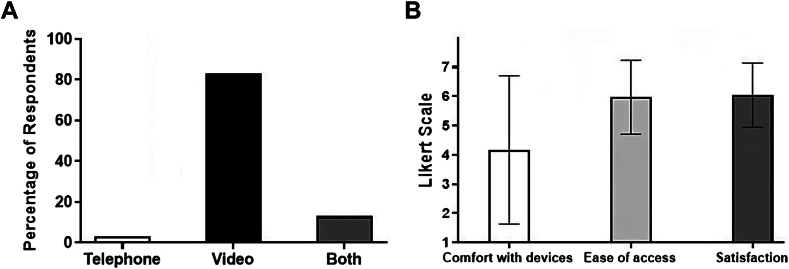
Patients completed their virtual CR by telephone (3%, n = 1), video call (83%, n = 25), or a combination of both (13%, n = 4) (Fig. 1A). On a 7-point Likert scale, patients reported a comfort with using technologic devices of 4.2 ± 2.5 and rated the ease of accessing virtual CR at 6.0 ± 1.3 (Fig. 1B). Seventy percent
Figure 1.
(A) Types of virtual cardiac rehabilitation visits and (B) Patient experience and satisfaction with virtual visits. (A) Values presented as percentage or (B) 7-point Likert Scale with mean ± SD.
(n = 21) of patients thought that their privacy was securely maintained in virtual CR at the same level that it was for in-person care, whereas 17% (n = 5) of patients reported being unsure if their privacy was securely maintained when using virtual CR.
Patient lifestyle changes following virtual CR
A majority of patients (86%, n = 25) reported lifestyle modifications following virtual CR attendance. Such changes included smoking cessation (8%, n = 2), increased aerobic exercise (48%, n = 12), and improved dietary choices (32%, n = 8). More specifically, patients reduced consumption of red meat, sugar, and incorporated the Mediterranean diet.
Patient satisfaction, experience, and preferences
The majority of patients (86%, n = 25) thought that virtual CR met their goals and expectations, whereas 93% (n = 27) thought that the virtual education sessions were beneficial. Patients rated their overall satisfaction on a 7-point Likert scale as 6.0 ± 1.1 (Fig. 1B). Their overall experience with virtual CR on a 10-point scale was reported to be 8.6 ± 1.4. Furthermore, 66% (n = 19) of patients preferred either a hybrid of in-person and virtual CR, or exclusively virtual CR.
Qualitative findings
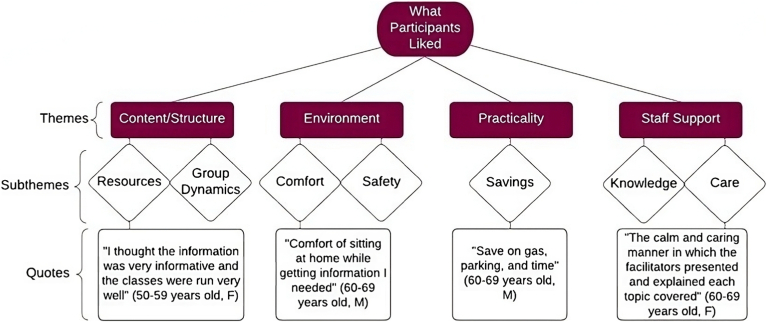
Open-text responses were completed by 77% (n = 23) of the sample population. Figure 2 illustrates how themes and subthemes around patient enjoyment of virtual CR were organized. The first favourable theme emerged around the content and structure of virtual CR. Subthemes within this group included beliefs that virtual CR resources were accessible as well as informative and that group dynamics were helpful. Patients found that they could learn from others in a group setting, with other patients raising questions to the health care team that were relevant and useful to their personal recovery. The second favourable theme emerged around the environment of virtual CR. Within this theme, patients reported that they felt safe with the ability to complete CR in their home environment as they were limiting their risk of exposure to COVID-19. The third favourable theme emerged around the practicality that virtual CR offered, as both time and money for transportation and parking were saved in a virtual model. The fourth theme emerged around the positive experiences with staff support. Patients found the staff to be knowledgeable about cardiac health and accommodating to their needs through their attentive listening. The patients were also appreciative of the excellent communication from the staff about their health.
Figure 2.
What patients liked about virtual cardiac rehabilitation. F, female; M, male.
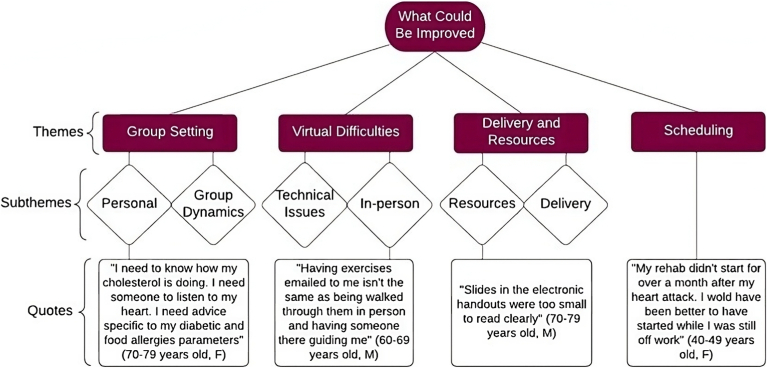
Four themes emerged that pertain to aspects of virtual CR that patients felt could be improved (Fig. 3). The first theme was the group setting. Although there were some positive features about the group setting, as mentioned previously, patients found that there was limited personalization. In particular, when patients had questions related to specific aspects of their health (eg, management of diabetes), they thought that these questions were not addressed adequately in a group setting. The second theme focused on virtual difficulties. Patients expressed technical challenges with the virtual CR program, such as delays connecting to the Zoom meetings. Patients reported a preference for exercise sessions to be delivered in person, as they thought it was not as effective as having the sessions provided virtually. Thirdly, patients found that the delivery of the material was repetitive with previously provided resources and that the viewing of the resources was difficult as the font size was reportedly a challenge. The final theme was that patients felt that scheduling was condensed, and a preference would be for more classes spread out over a longer period.
Figure 3.
What could be improved with virtual cardiac rehabilitation. F, female; M, male.
Discussion
We conducted a single centre cross-sectional study exploring the experiences of cardiac patients attending a recently transitioned virtual CR program. Quantitative analysis responses and qualitative analysis derived from open-text survey responses indicate that the virtual CR program met patients’ goals and expectations, with a shared belief that attendance was beneficial to their health. Consistent with the literature, patients stated that virtual CR resulted in lifestyle changes, including sustained improvements to exercise habits, such as increased walking, and improved dietary choices.12,13 Furthermore, despite some patients reporting limited comfort with using technology, the virtual CR program was generally accessible from a technical and logistical perspective. These findings around accessibility offer an alternative to individuals who have had acute cardiac events and would benefit from CR, although, under previous circumstances, could not attend in-person programs.2 As such, the availability of virtual CR may improve mortality and morbidity outcomes for those at risk. Virtual CR was found to be informative and contained many resources to improve health literacy among those who attended, improving upon another suggested cause of the underuse of CR.2 Virtual CR was also more cost effective and safer, further increasing accessibility across a diverse patient population.
Although virtual CR was generally well received by patients, changes could be implemented for improvement. Group sessions, instead of individual ones, likely made patients feel that their needs were not noticed and consequently that their care was affected. Some patients reported technical difficulties, which may have affected their attendance and engagement with the virtual program. Given that dropout during CR programs can be high, there is a need to ensure that technology issues are promptly resolved among both program providers and recipients, whether related to issues connecting to the Zoom meetings or technical delays when patients were accessing their medical charts. Furthermore, the compressed nature of the schedule across 5 weeks made attendance difficult for patients. Steps to improve upon these findings include offering personal sessions in addition to the group sessions. Developing a virtual CR program that is spread out over a longer period can increase patient attendance and allow them to receive complete care.
The favourable themes and suggestions for improvement presented in this paper are consistent with other findings of virtual CR.5,14,15 The literature describes the need for technologic literacy as a limitation to virtual CR; however, the research presented in this paper has illustrated that virtual CR was accessible from a patient perspective.14 Another concern with providing care virtually is maintaining privacy. However, results from this research indicate that most respondents believed that their personal health information was kept private and secure when collected virtually at the same level as it would be kept when collected in person. These findings may assist in improving the acceptability of virtual care across CR.
Limitations
There were limitations to this research. First, the survey assessed virtual CR at a single centre; as such, generalizability of the findings is to be determined. Second, the respondent demographic was not diverse, as most respondents were male, between 60 and 79 years of age, and from a White European racial-ethnic backgrounds. Furthermore, it is probable that patients with greater comfort in using technologic devices completed both the virtual CR and the survey, resulting in a selection bias. Third, the lower response rate of 31% resulted in a smaller sample size, which affects the generalizability of these findings. Fourth, analysis of open-text qualitative responses was limited, as we did not undertake data saturation, member checking, or inter-rater reliability checks, which are often used for interview or focus group-based qualitative studies. Furthermore, although our question selection in the patient survey was guided by previous work from the study team, a limited number of domains relating to patient experience were explored. Further research is warranted to investigate additional domains in follow-up surveys of cardiac patients attending virtual CR using established frameworks, such as the theoretical domains framework, to provide a more comprehensive investigation into the barriers and facilitators of virtual CR.5,16 These aspects of the study may limit its generalizability and validity.
Conclusions
Virtual CR was generally well received and was an overall satisfying and positive experience for patients at our large tertiary care centre in Hamilton, Canada. The data presented in this paper may serve as a foundation for virtual cardiovascular care and may provide direction for the implementation of virtual care models in other health centres. Continual evaluation of this pilot project is warranted.
Acknowledgements
We would like to acknowledge the virtual cardiac rehabilitation team at the Cardiac Health Rehabilitation Clinic at Hamilton General Hospital.
Ethics Statement
The research reported has adhered to the relevant ethical guidelines. Full ethics review was waived by the Hamilton Integrated Research Ethics Board (HIREB), as this was considered quality-improvement work.
Patient Consent
The authors confirm that patient consent forms have been obtained for this article.
Funding Sources
No funding was provided for this article.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 137 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2023.10.013.
Supplementary Material
References
- 1.Heart and Stroke. Cardiac Rehabilitation (cardiac rehab) https://www.heartandstroke.ca/heart-disease/recovery-and-support/cardiac-rehabilitation Available at:
- 2.Menezes A.R., Lavie C.J., Milani R.V., Forman D.E., King M., Williams M.A. Cardiac rehabilitation in the United States. Prog Cardiovasc Dis. 2014;56:522–529. doi: 10.1016/j.pcad.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 3.Moulson N., Bewick D., Selway T., et al. Cardiac rehabilitation during the COVID-19 era: guidance on implementing virtual care. Can J Cardiol. 2020;36:1317–1321. doi: 10.1016/j.cjca.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lam J., Ahmad K., Gin K., Chow C.M. Deliver cardiac virtual care: a primer for cardiovascular professionals in Canada. CJC Open. 2022;4:148–157. doi: 10.1016/j.cjco.2021.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanderson K.E., Spithoff K.D., Corovic M., Langdon K.M., Schwalm J.D. An evaluation of cardiology virtual care during the COVID-19 pandemic. CJC Open. 2021;3:1294–1299. doi: 10.1016/j.cjco.2021.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maddison R., Rawstorn J.C., Stewart R.A.H., et al. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart. 2019;105:122–129. doi: 10.1136/heartjnl-2018-313189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dalal H.M., Doherty P., McDonagh S.T., Paul K., Taylor R.S. Virtual and in-person cardiac rehabilitation. BMJ. 2021;373:n1270. doi: 10.1136/bmj.n1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rawstorn J.C., Gant N., Direito A., Beckmann C., Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102:1183–1192. doi: 10.1136/heartjnl-2015-308966. [DOI] [PubMed] [Google Scholar]
- 9.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 12.Lear S.A., Singer J., Banner-Lukaris D., et al. Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the Internet. Circ Cardiovasc Qual Outcomes. 2014;7:952–959. doi: 10.1161/CIRCOUTCOMES.114.001230. [DOI] [PubMed] [Google Scholar]
- 13.Mendell J., Bates J., Banner-Lukaris D., et al. What do patients talk about? A qualitative analysis of online chat sessions with health care specialists during a “virtual” cardiac rehabilitation program. Telemed E-Health. 2019;25:71–78. doi: 10.1089/tmj.2017.0206. [DOI] [PubMed] [Google Scholar]
- 14.Ajibade A., Younas H., Pullan M., Harky A. Telemedicine in cardiovascular surgery during COVID-19 pandemic: a systematic review and our experience. J Card Surg. 2020;35:2773–2784. doi: 10.1111/jocs.14933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brewer L.C., Kaihoi B., Schaepe K., et al. Patient-perceived acceptability of a virtual world-based cardiac rehabilitation program. Digit Health. 2017;3:1–8. doi: 10.1177/2055207617705548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cane J., O'Connor D., Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Sci. 2012;7:1–17. doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.