Abstract
Falls are the leading cause of fatal and non-fatal injuries in older adults. Walkers are often used by and prescribed to this population to reduce fall risk, however, walker users and walker non-users alike experience similar fall incidence rates. The role of walkers in preventing falls is unclear as some studies suggest walkers may be a fall-inciting factor. The purpose of this study was to analyze walker deficits by evaluating the circumstances and causes of falls in older adult walker users residing in long-term care facilities. Videos capturing 34 real-life falls involving wheeled walkers (rollators and two-wheeled walkers) in two retirement facilities were analyzed for 3 themes: walker type, fall direction, and activity at the time of fall. A frequency analysis of these themes was performed to determine common fall mechanisms. The results of this study suggest two-wheeled walker and rollator users most often fall sideways while turning and backward during weight transfer, respectively. Poor maneuverability, lateral stability, and wheel velocity control of the walkers contributed to the falls. Device improvements addressing these areas of deficiency may be necessary to mitigate falls occurring in older adult walker users.
Keywords: Assistive mobility device, elderly, fall circumstances, falls, walker design
Introduction
In older adults, falls are the leading cause of fatal and nonfatal injuries (Bergen et al., 2016). Approximately 30% of individuals over the age of 65 fall each year, with fall risk increasing with age (Hartholt et al., 2011; Tinetti et al., 1988). As a result of these falls, over 27,000 deaths and 800,000 hospitalizations occur each year in the U.S., amounting to US $19.2 billion in medical care costs (Bergen et al., 2016; Stevens et al., 2006). Falls resulting in minor injuries also have detrimental effects on an individual’s quality of life (Hartholt et al., 2011). Reduced functional status such as difficulties with mobility, usual activities, self-care, and anxiety and depression are common consequences of fall-related injuries and are associated with increased dependence and a higher risk of premature mortality (Hartholt et al., 2011; Hirvensalo et al., 2000; Olaya et al., 2018; Stel et al., 2004). To address this major public health concern, it is important to evaluate methods aiming to prevent and minimize fall occurrences in the aging population.
To reduce fall risk in older adults, clinicians often prescribe mobility aids such as walkers (Stel et al., 2004). It is estimated that at least 11.6% of community-dwelling individuals over the age of 65 utilize walkers and that this percentage will continue to grow as in recent decades the prevalence of walker use in this population has more than doubled (Gell et al., 2015; LaPlante et al., 1992). Walkers improve users’ mobility, promote independent locomotion, and increase levels of activity in users (Salminen et al., 2009). Additionally, individuals who fall while using a walker incur less severe injuries than nonusers as they are 8.5 times less likely to be hospitalized and 12 times less likely to suffer injuries requiring surgery (Luz et al., 2017). However, older individuals using walkers remain at risk of falls as an estimated 41,000 US emergency room visits per year are associated with walker use (Stevens et al., 2009). Moreover, studies have found no significant differences between fall incidence rates in walker users and non-users who have matched demographic backgrounds, medical conditions, physical capacity, and fall history (Gell et al., 2015). Other studies even suggest that walkers are indicators of fall risk (Kallin et al., 2004). Although this may be because individuals who are prescribed walkers are generally at an increased risk of falling, walkers cause destabilizing biomechanical effects that interfere with balance recovery techniques (Bateni & Maki, 2005; Bateni et al., 2004). The prevalence of falls amongst walker users and nonusers alike may indicate that although prescribed to do so, walkers may be deficient at preventing falls in the user population, pointing to a need for device improvement. Modifications to the design of walkers may be a mechanism through which the device’s ability to reduce fall risk can be maximized. Walker deficits remain largely unknown, therefore understanding how individuals fall while using walkers could inform redesign and aid in the mitigation of falls with walkers. Previous research analyzing walker use among older adults in long-term care facilities suggests improvement to clinical user device training to reduce falls (Sloot & Komisar, 2022). While this may be effective, a large percentage of walker users do not obtain walkers from medical professionals that provide training, but rather self-obtain the devices commercially or receive them from family, friends, or long-term care facility staff (Hill et al., 2022; Hunter et al., 2021; Liu, 2009). Furthermore, training may not be effective for a significant portion of walker users in long-term care affected by declines in cognitive functioning as dementia has been shown to impair walker use (Clarke et al., 2009; Hill et al., 2022).
Objectives
The purpose of this study is to gain an understanding of walker deficits, rather than training deficits, by evaluating the circumstances and causes of falls in older adult walker users in long-term care facilities. This study may provide the knowledge to design an improved walker that specifically addresses walker limitations and maximizes the walker’s ability to mitigate falls.
Methods
Two researchers reviewed 41 videos from a public data set capturing falls involving wheeled walkers (two-wheeled walkers and rollators) in two retirement facilities (Robinovitch, 2018). For each video, the researchers used thematic coding to evaluate the prevalent fall mechanisms of falls with walkers. Codes were established to describe qualitative observations pertaining to three themes: walker type (two-wheeled walker or rollator), fall direction (forward, backward, or sideways), and activity at the time of the fall (forward walking, turning, standing, transferring from standing to sitting on the walker’s seat or stationary chair, transferring from sitting on the walker’s seat to standing, transferring to an upright position after bending over, collapsing the walker’s seat or misuse of walker). The researchers coded each fall video independently and then compared codes. Upon disagreement, the fall video in question was reviewed and discussed by both researchers until a consensus on codes was reached. Videos where the activity at the time of falling was coded as “misuse of walker” were excluded from further analysis.
For a total of 34 falls, we performed a frequency analysis of the codes used to describe the observed walker types, fall directions, and activities at the time of falling. The frequency of each possible fall circumstance was also determined (i.e., we calculated the percentage of total falls associated with each combination of walker type, fall direction, and activity at the time of falling). Code combinations with high-frequency rates were identified as common fall scenarios. The videos corresponding to these scenarios were further reviewed for walker design deficiencies and possible design solutions. Excluded from the frequency analysis were falls largely attributed to user error or misuse of the walker, including individuals using one hand to laterally drag the device, leaning backward on the device, and misjudging body trajectory when transferring to a seated position (n = 5). Also excluded were falls where the individual had no physical contact with the walker during and leading up to the fall (n = 2).
Results
Thirty-four falls (from sixteen individuals) were analyzed. Falls while using two-wheeled walkers made up 20.6% (7 of 34) of the observed falls, and the remaining 79.4% (27 of 34) involved rollators. Three individuals who used a rollator fell more than once, one individual who used a two-wheeled walker fell more than once, and one individual who used both a two-wheeled walker and a rollator fell more than once with each device. Participant demographics are reported in Table 1. For individuals who fell more than once, we report their demographics for their first fall with a given device only.
Table 1.
Participant demographics. Data are mean (SD) or n (%).
| Two-wheeled walker users (n = 4) | Rollator users (n = 13) | |
|---|---|---|
| Participant Age | 88.8 (5.9) | 86.8 (5.6) |
| Sex | ||
| Male | 0 (0%) | 6 (46.2%) |
| Female | 4(100%) | 7 (53.8%) |
Of the falls involving two-wheeled walkers, the backward and sideways fall directions each accounted for 42.9% (3 of 7) of total falls (Figure 1a). The majority of falls (3 of 7) occurred while turning the device, followed by weight transfers, walking, and standing (Figure 2a). For individuals who fell backward, transferring to an upright position after bending over, transferring to a chair, and standing activities had equal fall incidence rates of 14.3% (1 of 7). For individuals who fell sideways, all falls occurred while turning, making falling sideways while turning the most common combination of fall direction and activity for two-wheeled walker users, accounting for 42.9% (3 of 7) of falls (see Appendix).
Figure 1.
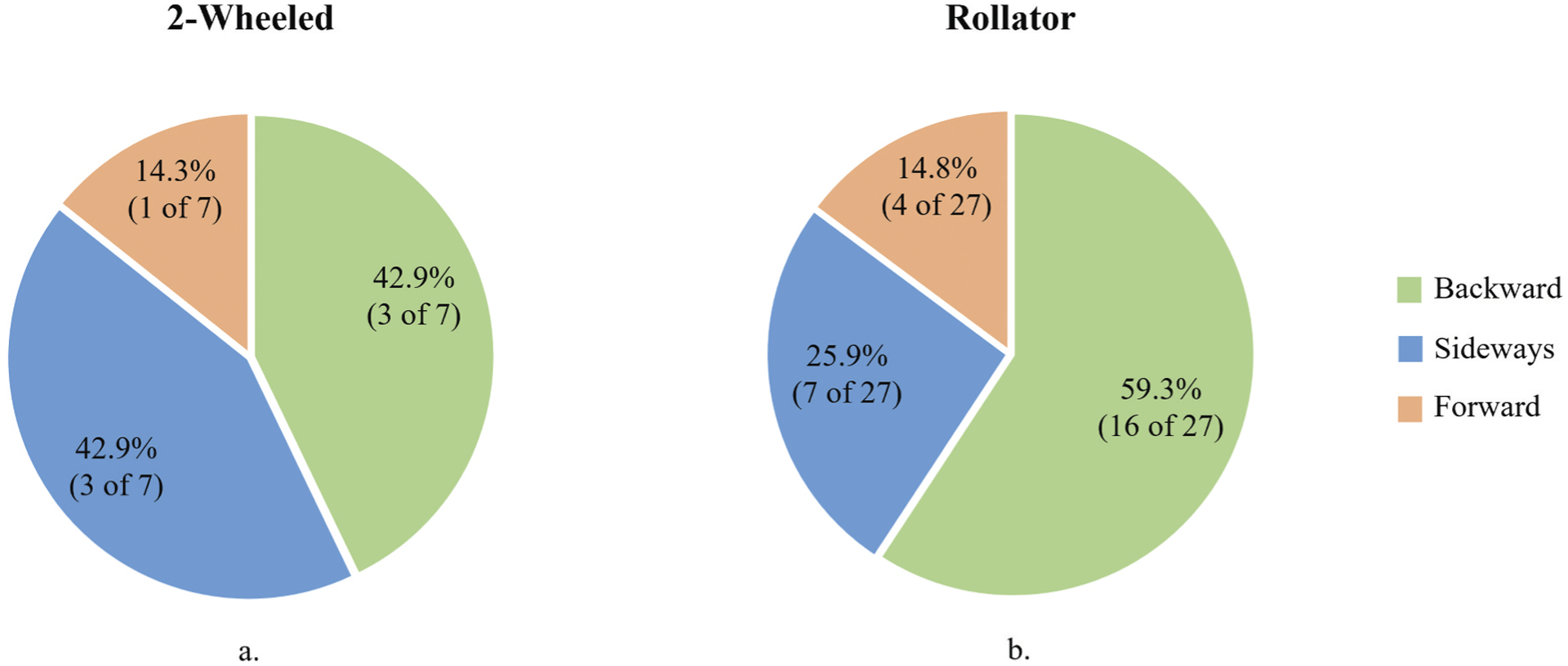
Recorded fall directions for falls with (a) a two-wheeled walker (n = 7) and (b) a rollator (n = 27).
Figure 2.
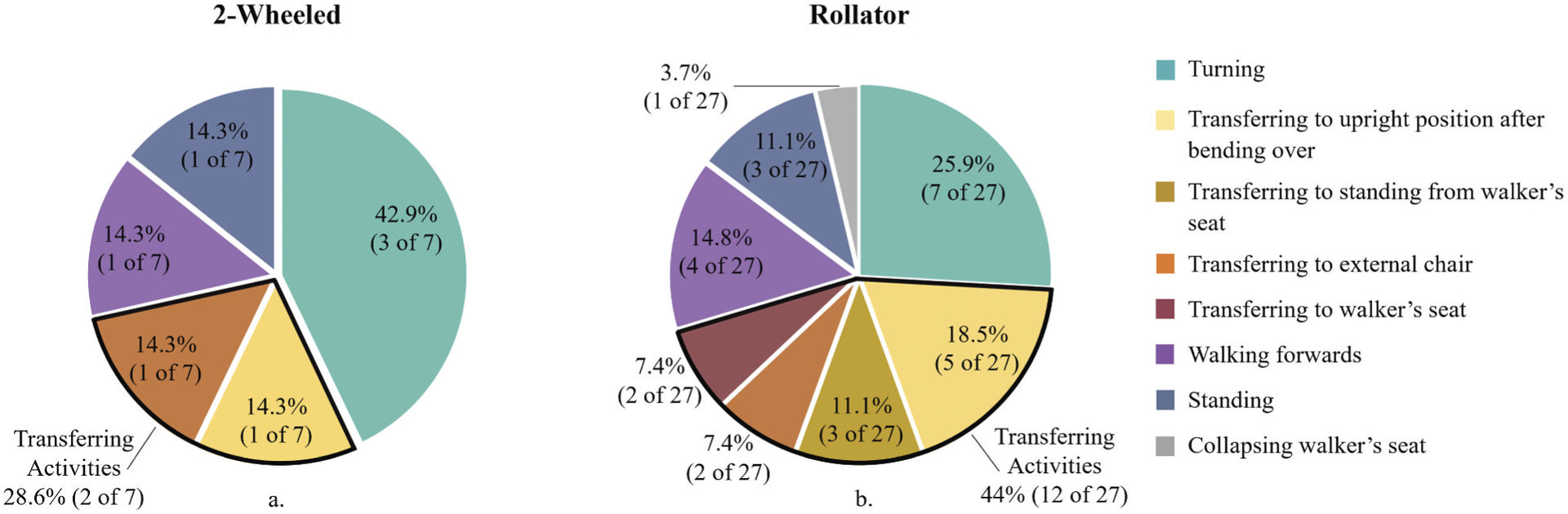
Recorded activities at the time of fall for falls with (a) a two-wheeled walker (n = 7) and (b) a rollator (n = 27).
Of individuals who fell while using a rollator, most fell backward (Figure 1b). The most common activity at the time of falling was turning, accounting for 25.9% (7 of 27) of falls, however, together, transferring activities accounted for 44.4% (12 of 27) of falls with a rollator. The activities with the fewest falls were collapsing the walker’s integrated seat and standing (Figure 2b). For the 16 individuals who fell backward, 75% (12 of 16) of falls were associated with a transferring activity. Falls in the backward direction while transferring were the most common combination of fall direction and activity for rollator users accounting for 44.4% (12 of 27) of falls (see Appendix).
Discussion
This study provides key evaluation of fall mechanisms associated with walker use and areas of deficiency in the designs of wheeled walkers. The results of this study indicate that backward and sideways falls are the most prevalent fall directions for wheeled walker users. This is consistent with studies that also investigated video-recorded falls in older adults with and without mobility aids occurring in long-term care facilities (Holliday et al., 1990; Komisar et al., 2022; Robinovitch et al., 2013; Sloot & Komisar, 2022). These results are an important addition to the existing literature on walker use as this study evaluates real-life falls in older adults involving different walker types.
For two-wheeled walker users, our results indicate that sideways falls are the most common. Lateral falls causing hip fractures are the costliest type of fall injury in older adults, so it is important walkers provide stability in this direction (Hartholt et al., 2011). However, the prevalence of falls in this direction demonstrates the current design of two-wheeled walkers is incapable of providing enough lateral stability to mitigate sideways tipping of the walker and lack of maneuverability may be an inciting fall-factor in this direction. In this study, all sideways falls occurred while turning, which was also identified as a problematic maneuver for two-wheeled walkers in interview and laboratory-based walking studies (Lindemann et al., 2016; Thies et al., 2020). Turning a two-wheeled walker is a difficult and risky activity because the front wheels are fixed. To compensate for this inability of the wheels to rotate, it is common for users to pick up their device to change directions, a behavior seen in this study (Bateni & Maki, 2005; Thies et al., 2020). Lifting the device causes drastic changes in lateral stability and thus is not a form of recommended use. Nonetheless, guidance on how to safely turn with two-wheeled walkers is not discussed in clinical or manufacturer user guidelines (Thies et al., 2020). This lack of guidance suggests a deficit exists in the turning functionality of two-wheeled walkers. However, turning is necessary for older adult users to navigate different environments safely and independently, an essential factor in maintaining good health (Hirvensalo et al., 2000). The turning capabilities of two-wheeled walkers need further investigation and improvement to mitigate lateral falls associated with this walker type.
In rollator users, the prevalence of sideways falls was 17% lower than in two-wheeled walker users. The design of rollators addresses the turning and mediolateral maneuverability deficiencies of two-wheeled walkers by implementing two fixed back wheels and rotatable front wheels. However, the greater mediolateral mobility of rollators may contribute to decreased anteroposterior stability, as this study found that the prevalence of backward falls with rollators was 16% greater than that of two-wheeled walker users. Backward falls are health hazards for older adults and are associated with head/brain injuries, high hospital admission rates, and substantial treatment costs (Hartholt et al., 2011). This study found that backward falls occurred most often during weight transfer activities due to uncontrolled rolling of the device away from or into the user. As older adult walker users tend to grasp or hold their walker during sit-to-stand transfers, it is important for rollators to withstand the forces generated without rolling (Komisar et al., 2022). Most rollators have brake features to counteract uncontrolled rolling, but we observed that individuals failed to utilize these features. Similarly, Lindemann et al. found that for 83% of older adult rollator users, fixing the brakes during sit-to-stand weight transfers is problematic (Lindemann et al., 2016). Our findings emphasize the need for a more accessible, easily controlled braking mechanism for rollators to encourage user operation and reduce backward falls. Additionally, improvements to the braking design may increase walker stability during activities other than weight transfer. Although less frequent, lack of velocity control during turning and forward walking also causes falls in older adults.
To address some of the challenges rollator and two-wheeled walkers users face, smart walkers have been developed. However, these smart walkers are not typically practical for community ambulation as they are heavy, expensive, and complex (Martins et al., 2015). The motorized components added to smart walkers may aggravate the common complaints of typical walkers, such as being too “heavy,” “awkward,” “bulky,” and “difficult to use” (Mann et al., 1995). Furthermore, the required coordination between user and device during typical walker use demands a higher cognitive load than walking alone (Wright & Kemp, 1992). The additional complexity of smart walkers may require additional learning, attention, and coordination from its users which is not realistic for the subset of older adults with general cognitive decline. There is little research on the effectiveness of smart walkers in improving mobility, but one study suggests that the extra challenges of using smart walkers outweigh their benefits as there are no significant performance differences from a low-tech assistive mobility device (Rentschler et al., 2008). Considering these drawbacks of smart walkers, new walker designs must be simple and affordable with limited motor-driven aspects.
Implementing low-tech modifications to the existing design of two-wheeled walkers and rollators may be an effective solution to prevent falls with these devices. The authors suggest that modifications to two-wheeled walkers should target lateral stability, especially during turning, to reduce sideways falls in older adult users. Introducing additional degrees of freedom to the device’s wheel system or adjusting the size of the walker/ground interface (base of support) may be modifications that could improve lateral stability (Table 2). For rollators, modifications that provide additional control and assistance during transfers may reduce the number of backward falls due to uncontrolled rolling and misjudged body trajectories. Enhanced control of wheel velocity through modifications to the braking mechanism may be one approach to address rollator deficiencies (Table 2).
Table 2.
Author suggestions for two-wheeled walker and rollator modifications that may address device deficits.
| Two-wheeled walker | Rollator |
|---|---|
| Target deficit: Lateral stability | Target deficit: Wheel velocity control |
| 1. Front wheels with additional modes of rotation | 1. Reverse braking mechanism (engage brake to release wheels, disengage to stop wheels) |
| 2. Addition of a front rotating third wheel | 2. Visual indication of brake state |
| 3. Expandable/retractable base of support | 3. Adjustable wheel resistance |
| 4. Kickstand on existing legs | 4. Maximum rotation per minute threshold |
| 5. Alignment guides (positions mediolateral body-trajectory during transfers) |
In this study, we observed challenges with walkers identified in user interviews and laboratory walking studies directly translate to real-life falls. The analysis of falls in this study provides a greater understanding of walker deficits, their contributions to falls, and potential ways in which these falls may be reduced. One limitation of this study is the small sample size of falls involving two-wheeled walkers. Despite this limitation, our fall direction and activity results for two-wheeled walker users largely align with previously reported problems with two-wheeled walker use (Bateni et al., 2004; Lindemann et al., 2016; Mann et al., 1995; Thies et al., 2020, 2020). Additionally, some of the analyzed videos had poor resolution, low frame rates, or distant camera angles, which may have limited the coding researchers’ abilities to identify situational and environmental factors during video analysis. Although unlikely, these factors could have influenced the activity at the time of falling. The generalizability of the results of this study to all walker users may be limited as this study evaluates falls only in older adult walker users residing in long-term care facilities.
Conclusions
Older adults remain at risk for falling when using two-wheeled walkers and rollators. The results of this study suggest sideways falls while turning and backward falls during weight transfer are the most common fall circumstances that affect older adults in long-term care facilities who use two-wheeled walkers and rollators, respectively. The primary contributors to the observed falls were poor maneuverability, lateral stability, and velocity control of these devices. Designing, building, and testing prototype walkers that address the areas of deficiency identified by this study is an important next step in reducing the number of falls that occur while using wheeled walkers.
Appendix
Table A1.
Percentages of total falls (n = 34) by fall direction and activity at the time of fall.
| Activity at the time of fall | Fall direction | Total | ||
|---|---|---|---|---|
| Forward | Backward | Sideways | ||
| Turning | 0.00 | 8.82 | 20.59 | 29.41 |
| Walking forward | 8.82 | 0.00 | 5.88 | 14.71 |
| Standing | 5.88 | 2.94 | 2.94 | 11.76 |
| Transferring to upright position after bending over | 0.00 | 17.65 | 0.00 | 17.65 |
| Transferring to standing from walker’s seat | 0.00 | 8.82 | 0.00 | 8.82 |
| Transferring to walker’s seat | 0.00 | 5.88 | 0.00 | 5.88 |
| Transferring to external chair | 0.00 | 8.82 | 0.00 | 8.82 |
| Collapsing walker’s seat | 0.00 | 2.94 | 0.00 | 2.94 |
| Total | 14.71 | 55.88 | 29.41 | 100.00 |
Table A2.
Percentages of falls involving two-wheeled walkers (n = 7) by fall direction and activity at the time of fall.
| Activity at the time of fall | Fall direction | Total | ||
|---|---|---|---|---|
| Forward | Backward | Sideways | ||
| Turning | 0.00 | 0.00 | 42.86 | 42.86 |
| Walking forward | 14.29 | 0.00 | 0.00 | 14.29 |
| Standing | 0.00 | 14.29 | 0.00 | 14.29 |
| Transferring to upright position after bending over | 0.00 | 14.29 | 0.00 | 14.29 |
| Transferring to standing from walker’s seat | 0.00 | 0.00 | 0.00 | 0.00 |
| Transferring to walker’s seat | 0.00 | 0.00 | 0.00 | 0.00 |
| Transferring to external chair | 0.00 | 14.29 | 0.00 | 14.29 |
| Collapsing walker’s seat | 0.00 | 0.00 | 0.00 | 0.00 |
| Total | 14.29 | 42.86 | 42.86 | 100.00 |
Table A3.
Percentages of falls involving rollators (n = 27) by fall direction and activity at the time of fall.
| Activity at the time of fall | Fall direction | Total | ||
|---|---|---|---|---|
| Forward | Backward | Sideways | ||
| Turning | 0.00 | 11.11 | 14.81 | 25.93 |
| Walking forward | 7.41 | 0.00 | 7.41 | 14.81 |
| Standing | 7.41 | 0.00 | 3.70 | 11.11 |
| Transferring to upright position after bending over | 0.00 | 18.52 | 0.00 | 18.52 |
| Transferring to standing from walker’s seat | 0.00 | 11.11 | 0.00 | 11.11 |
| Transferring to walker’s seat | 0.00 | 7.41 | 0.00 | 7.41 |
| Transferring to external chair | 0.00 | 7.41 | 0.00 | 7.41 |
| Collapsing walker’s seat | 0.00 | 3.70 | 0.00 | 3.70 |
| Total | 14.81 | 59.26 | 25.93 | 100.00 |
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Bateni H, Heung E, Zettel J, Mcllroy WE, & Maki BE (2004). Can use of walkers or canes impede lateral compensatory stepping movements? Gait & Posture, 20(1). 10.1016/S0966-6362 [DOI] [PubMed] [Google Scholar]
- Bateni H, & Maki BE (2005). Assistive devices for balance and mobility: Benefits, demands, and adverse consequences. Archives of Physical Medicine and Rehabilitation, 86(1). 10.1016/j.apmr.2004.04.023 [DOI] [PubMed] [Google Scholar]
- Bergen G, Stevens MR, & Burns ER (2016). Falls and fall injuries among adults aged ≥65 years — United States, 2014. MMWR Morbidity and Mortality Weekly Report, 65(37), 993–998. 10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- Clarke P, Chan P, Santaguida PL, & Colantonio A (2009). The use of mobility devices among institutionalized older adults. Journal of Aging and Health, 21(4), 611–626. 10.1177/0898264309333313 [DOI] [PubMed] [Google Scholar]
- Gell NM, Wallace RB, Lacroix AZ, Mroz TM, & Patel KV (2015). Mobility device use in older adults and incidence of falls and worry about falling: Findings from the 2011–2012 national health and aging trends study. Journal of the American Geriatrics Society, 63(5), 853–859. 10.1111/jgs.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EMM, Panneman MJM, van der Cammen TJM, & Patka P (2011). Societal consequences of falls in the older population: Injuries, healthcare costs, and long-term reduced quality of life. Journal of Trauma - Injury, Infection and Critical Care, 71(3), 748–753. 10.1097/TA.0b013e3181f6f5e5 [DOI] [PubMed] [Google Scholar]
- Hill KD, Meyer C, Burton E, Hunter SW, Suttanon P, Dawes H, & Lee D-CA (2022). Examining gait aid use and user safety by older people with dementia: Perspectives of informal carers to inform practice. Disability and Rehabilitation, 1–9. 10.1080/09638288.2022.2148302 [DOI] [PubMed] [Google Scholar]
- Hirvensalo M, Rantanen T, & Heikkinen E (2000). Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. Journal of the American Geriatrics Society, 48(5), 493–498. 10.1111/j.1532-5415.2000.tb04994.x [DOI] [PubMed] [Google Scholar]
- Holliday PJ, Fernie GR, Gryfe CI, & Griggs GT (1990). Video recording of spontaneous falls of the elderly. ASTM Special Technical Publication, 1103. 10.1520/stp15497s [DOI] [Google Scholar]
- Hunter SW, Meyer C, Divine A, Hill KD, Johnson A, Wittich W, & Holmes J (2021). The experiences of people with Alzheimer’s dementia and their caregivers in acquiring and using a mobility aid: A qualitative study. Disability and Rehabilitation, 43(23), 3331–3338. 10.1080/09638288.2020.1741700 [DOI] [PubMed] [Google Scholar]
- Kallin K, Jensen J, Olsson LL, Nyberg L, & Gustafson Y (2004). Why the elderly fall in residential care facilities, and suggested remedies. The Journal of Family Practice, 53(1), 41–52. [PubMed] [Google Scholar]
- Komisar V, van Schooten KS, Aguiar OMG, Shishov N, & Robinovitch SN (2022). Circumstances of falls during sit-to-stand transfers in older people: A cohort study of video-captured falls in long-term care. Archives of Physical Medicine and Rehabilitation, 104 (4), 533–540. 10.1016/j.apmr.2022.10.012 [DOI] [PubMed] [Google Scholar]
- LaPlante MP, Hendershot GE, & Moss AJ (1992). Assistive technology devices and home accessibility features: Prevalence, payment, need, and trends. Advance Data, (217), 1–11. [PubMed] [Google Scholar]
- Lindemann U, Schwenk M, Klenk J, Kessler M, Weyrich M, Kurz F, & Becker C (2016). Problems of older persons using a wheeled walker. Aging Clinical and Experimental Research, 28(2), 215–220. 10.1007/s40520-015-0410-8 [DOI] [PubMed] [Google Scholar]
- Liu H (2009). Assessment of rolling walkers used by older adults in senior-living communities. Geriatrics and Gerontology International, 9(2), 124–130. 10.1111/j.1447-0594.2008.00497.x [DOI] [PubMed] [Google Scholar]
- Luz C, Bush T, Shen X, & Pruchno R (2017). Do canes or walkers make any difference? Nonuse and fall injuries. Gerontologist, 57(2), 211–218. 10.1093/geront/gnv096 [DOI] [PubMed] [Google Scholar]
- Mann WC, Hurren D, Tomita M, & Charvat B (1995). An analysis of problems with walkers encountered by elderly persons. Physical and Occupational Therapy in Geriatrics, 13(1–2). 10.1080/J148v13n01_01 [DOI] [Google Scholar]
- Martins M, Santos C, Frizera A, & Ceres R (2015). A review of the functionalities of smart walkers. Medical Engineering & Physics, 37(10). 10.1016/j.medengphy.2015.07.006 [DOI] [PubMed] [Google Scholar]
- Olaya B, Moneta MV, Doménech-Abella J, Miret M, Bayes I, Ayuso-Mateos JL, & Haro JM (2018). Mobility difficulties, physical activity, and all-cause mortality risk in a nationally representative sample of older adults. Journals of Gerontology - Series A Biological Sciences & Medical Sciences, 73(9), 1272–1279. 10.1093/gerona/glx121 [DOI] [PubMed] [Google Scholar]
- Rentschler AJ, Simpson R, Cooper RA, & Boninger ML (2008). Clinical evaluation of Guido robotic walker. The Journal of Rehabilitation Research and Development, 45(9), 1281. 10.1682/JRRD.2007.10.0160 [DOI] [PubMed] [Google Scholar]
- Robinovitch SN (2018). Databrary - sharing videos of falls in long term care.
- Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Sims-Gould J, & Loughi M (2013). Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. Lancet, 381(9860). 10.1016/S0140-6736(12)61263-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salminen AL, Brandt Å, Samuelsson K, Töytäri O, & Malmivaara A (2009). Mobility devices to promote activity and participation: A systematic review. Journal of Rehabilitation Medicine, 41(9). 10.2340/16501977-0427 [DOI] [PubMed] [Google Scholar]
- Sloot L, & Komisar V (2022). Real-life movement analysis: Circumstances of falls involving walkers in frail older persons living in long term care. Gait & Posture, 97, S256–S257. 10.1016/j.gaitpost.2022.07.155 [DOI] [Google Scholar]
- Stel VS, Smit JH, Pluijm SMF, & Lips P (2004). Consequences of falling in older men and women and risk factors for health service use and functional decline. Age and Ageing, 33(1), 58–65. 10.1093/ageing/afh028 [DOI] [PubMed] [Google Scholar]
- Stevens JA, Corso PS, Finkelstein EA, & Miller TR (2006). The costs of fatal and non-fatal falls among older adults. Injury Prevention, 12(5), 290–295. 10.1136/ip.2005.011015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Thomas K, Teh L, & Greenspan AI (2009). Unintentional fall injuries associated with walkers and canes in older adults treated in U.S. emergency departments. Journal of the American Geriatrics Society, 57(8), 1464–1469. 10.1111/j.1532-5415.2009.02365.x [DOI] [PubMed] [Google Scholar]
- Thies SB, Bates A, Costamagna E, Kenney L, Granat M, Webb J, Howard D, Baker R, & Dawes H (2020). Are older people putting themselves at risk when using their walking frames? BMC Geriatrics, 20 (1). 10.1186/s12877-020-1450-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thies SB, Russell R, Al-Ani A, Belet T, Bates A, Costamagna E, Kenney L, & Howard D (2020). An investigation of the effects of walking frame height and width on walking stability. Gait and Posture, 82, 248–253. 10.1016/j.gaitpost.2020.09.017 [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, & Ginter SF (1988). Risk factors for falls among elderly persons living in the community. New England Journal of Medicine, 319(26), 1701–1707. 10.1056/nejm198812293192604 [DOI] [PubMed] [Google Scholar]
- Wright DL, & Kemp TL (1992). The dual-task methodology and assessing the attentional demands of ambulation with walking devices. Physical Therapy, 72(4), 306–312. 10.1093/ptj/72.4.306 [DOI] [PubMed] [Google Scholar]


