Abstract
Introduction
COVID‐19 drastically impacted the landscape of the United States’ medical system. Limited data is available on the nationwide implantation trends in Cardiac Resynchronization Therapy Defibrillator (CRT‐D) devices before and during the pandemic. We aimed to explore the impact of the COVID‐19 pandemic on CRT‐D insertion rates and adverse outcomes related to delays in care.
Methods and Results
We conducted a retrospective cross‐sectional analysis using the National Inpatient Sample database between 2017 and 2020. Variables were identified using their ICD‐10 codes. Inclusion criteria: age ≥ 18 years, presenting for a nonelective admission, primary diagnosis of hypertensive heart disease, hypertensive heart, chronic kidney disease, or heart failure, and underwent insertion of a CRT‐D. Between 2017 and 2020, CRT‐D devices were inserted during 23,635 admissions. On average, 6198 devices were implanted yearly from 2017 to 2019, with only 5040 devices being implanted in 2020. Additionally, reduced implantation rates were noted for every cohort of hospital size, location, and teaching status during this year. The year 2020 also had the highest average death rate at 1.39%, but this difference was statistically insignificant (adjusted Wald test p = .767), and COVID‐19 was not associated with an increased risk of inpatient mortality (OR 0.22, 95% CI 0.03–1.82, p = .162).
Conclusion
The COVID‐19 pandemic has affected all facets of the healthcare system, especially surgical volume rates. CRT‐D procedures significantly decreased in 2020. This is the first retrospective study highlighting the trend of reduced rates of CRT‐D implantation as a response to the COVID‐19 pandemic.
Keywords: cardiac resynchronization therapy, COVID‐19, CRT‐D, defibrillator, heart failure
Central Illustration: Cardiac Resynchronization Therapy Defibrillator (CRT‐D) trends comparing pre‐COVID‐19 years (2017–2019) to COVID‐19 (2020). CRT‐D implants decreased on average in 2020, and there was an increase in average inpatient mortality in 2020.
1. INTRODUCTION
The COVID‐19 pandemic drastically changed how healthcare was utilized. 1 Office visits were canceled for months, and hospitalizations were dominated by the SARS‐CoV‐2 virus, while encounters for typical diseases significantly declined. 1 , 2 Procedure volume dropped considerably during the initial wave of COVID‐19, including those typically associated with life‐saving measures. 3 As the world adapted, many practitioners switched to telehealth visits and remote monitoring for their patients. 4 Simovic et al. conducted an online survey study in 28 European countries and reported a significant increase in remote cardiac implantable electronic device monitoring during the pandemic. 5 Surgical operations began to normalize over the following months. 3 , 6 Nevertheless, the delays in care experienced during this time have contributed to long‐term consequences for patient outcomes. 7 , 8
Pacing and cardiac resynchronization therapy (CRT) are vital therapeutic options for those patients in New York Heart Association (NYHA) II‐III, ambulatory IV heart failure with a reduced ejection fraction of ≤35%, QRS duration ≥150 ms, and left bundle branch block, as well as those with conditions such as syncope and bi‐fascicular block. 9 CRT has been shown to be beneficial in reducing morbidity and mortality, as well as reducing hospitalizations and improving quality of life. 10 , 11 From 2006 to 2013, studies have shown that CRT use has increased each year. 12 , 13 Given the increasing prevalence of heart failure and implantation rates of CRT, many heart failure patients benefited from this therapy in the pre‐COVID‐19 years. 14 , 15
The Heart Rhythm Society, the American College of Cardiology, and the American Heart Association issued guidance for managing invasive electrophysiology procedures during the COVID‐19 pandemic. The task force recommended and increasingly mandated postponing or canceling nonurgent and elective procedures, including cardiac resynchronization therapy device (CRT‐D) implantation in stable patients. 16 In patients with severe refractory heart failure where the implantation of CRT‐D is considered urgent, the task force issued several recommendations, including screening for COVID‐19, elective intubation of COVID‐19 patients, and performing the procedures in negative‐pressure operating rooms, as well as other recommendations. 16 COVID‐19 pneumonia's involvement in the cardiovascular system has also been well established, including pericarditis, myocarditis, heart failure, acute coronary syndrome, and arrhythmias. 17 , 18 It was found that 49% of patients who were deceased from COVID‐19 also had a comorbidity of heart failure. 19 Heart failure has been found to be the most common complication during exacerbations of COVID‐19, even in patients without a history of cardiovascular diseases. 20 To date, the literature is scarce on the impact of the pandemic on electrophysiological procedures for patients with heart failure, namely CRT with or without defibrillator capacity, its immediate effects on outcomes in the real world, and its impact on patient outcomes. We identified the impact of the COVID‐19 pandemic and aftermath on the utilization of CRT‐D and the outcomes associated with hospitalizations.
2. METHODS AND MATERIALS
The Equator Network Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were observed to prepare the manuscript. 21
2.1. Study design/settings
The Agency for Healthcare and Research and Quality Healthcare Cost and Utilization Project's National Inpatient Sample (NIS) was utilized to perform a cross‐sectional, retrospective study from 2017 to 2020. The NIS is a publicly available, all‐payer inpatient healthcare database. It represents a 20% stratified sample of hospital discharges, excluding rehabilitation and long‐term acute care hospitals. The NIS database and software tools were developed for the Healthcare Cost and Utilization Project (HCUP). 22
2.2. Participants
Cases represent hospital encounters. If there are multiple admissions for the same patient, every admission is recorded as a separate encounter. We included all the admissions for patients with the following criteria: 18 years of age or older at the time of admission; nonelective admission; admission diagnosis of hypertensive heart disease, hypertensive heart with chronic kidney disease, or heart failure (ICD‐10 codes I11, I13, I50); insertion of a CRT device (ICD‐10 code 0JH**9*).
2.3. Variables
The primary objective was to analyze the temporal and national trends in characteristics, management, procedural utilization, and outcomes for admissions with a CRT device implantation. The primary outcome of this study was to assess the trend of CRT‐D implantations from 2017 to 2020 in patients that met the inclusion criteria. Secondary outcomes included mortality and hospital length of stay.
2.4. Data measurements
Age was reported in years. Race was divided into six categories: White, Black, Hispanic, Asian or Pacific Islander, Native American, and Other. Additional factors of interest included hospital bed size (i.e. small, medium, and large), hospital location/teaching status (i.e., rural, urban nonteaching, and urban teaching), median household income, and geographical location. Diagnoses and procedures were identified using the International Classification of Diseases, 10th Revision (ICD‐10) codes.
2.5. Ethical considerations
The Institutional Review Board is not required for studies utilizing the NIS databases, as they fall under the “limited data sets” category exempted by the HIPAA privacy regulations. Any subgroup identifying between one and ten patients was obfuscated per HCUP's data use agreement. Additionally, the study was conducted in agreement with and followed the principles of the Declaration of Helsinki.
2.6. Statistical methods
Baseline characteristics included patient demographics, hospital and location attributes, insurance, and disposition. Comorbidities were identified by the Elixhauser comorbidity software package. Continuous and categorical variables were presented as means with standard errors. The Rao‐Scott Chi‐square test compared categorical variables between groups. Hospital procedural volume was calculated yearly using the weighted quantity of CRT insertions and then divided into quintiles. Procedural volume was calculated using the total number of procedures, regardless of admission diagnosis. Stata 17 (College Station, TX, USA) was used for all statistical analyses, utilizing the “svy” function to account for complex survey methodology with weighting, consistent with HCUP's best practices. An alpha (p) value of .05 was used to ascertain statistical significance.
3. RESULTS
3.1. Patient demographics
Between 2017 and 2020, there were 23,635 index admissions during which CRT‐D devices were inserted and met the study inclusion criteria. Of all the included admission diagnoses, patients had a mean age of 69.27 years, and 70.55% identified as male. Of these patients, 64.92% identified as White, while 19.70% identified as Black. Of all the index admissions, 1310 patients (5.54%) were COVID‐19 positive, or 25.99% of CRT‐D implantations in the year 2020. Complete baseline characteristics are included in Table 1.
TABLE 1.
Baseline characteristics. Patient demographics and characteristics.
| Calendar year | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | Total | Obs | p‐value | ||||||
| Patients per year | 6220 | 6270 | 6105 | 5040 | 23,635 | |||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | |||
| Covid‐19 | ||||||||||||
| No Covid | 100.00 | (0.00) | 100.00 | (0.00) | 100.00 | (0.00) | 74.01 | (1.48) | 94.46 | (0.41) | 22,325 | 0.000 |
| COVID‐19 Infection | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 25.99 | (1.48) | 5.54 | (0.41) | 1310 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,635 | ||||||
| Indicator of sex | ||||||||||||
| Male | 70.34 | (1.27) | 71.45 | (1.30) | 69.70 | (1.30) | 70.73 | (1.36) | 70.55 | (0.65) | 16,675 | 0.803 |
| Female | 29.66 | (1.27) | 28.55 | (1.30) | 30.30 | (1.30) | 29.27 | (1.36) | 29.45 | (0.65) | 6960 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,635 | ||||||
| Race (uniform) | ||||||||||||
| White | 64.98 | (1.65) | 64.08 | (1.69) | 64.38 | (1.65) | 66.57 | (1.74) | 64.92 | (0.83) | 14,965 | 0.072 |
| Black | 17.51 | (1.30) | 18.37 | (1.32) | 22.38 | (1.41) | 20.77 | (1.47) | 19.70 | (0.68) | 4540 | |
| Hispanic | 10.95 | (1.00) | 11.27 | (1.14) | 8.63 | (0.88) | 8.61 | (0.95) | 9.93 | (0.50) | 2290 | |
| Asian or Pacific Islander | 2.16 | (0.43) | 2.12 | (0.46) | 1.59 | (0.36) | 1.32 | (0.39) | 1.82 | (0.21) | 420 | |
| Native American | 0.83 | (0.29) | 0.41 | (0.18) | 0.59 | (0.25) | 0.41 | (0.20) | 0.56 | (0.12) | 130 | |
| Other | 3.57 | (0.58) | 3.76 | (0.57) | 2.43 | (0.43) | 2.33 | (0.51) | 3.06 | (0.27) | 705 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,050 | ||||||
| Insurance carrier, cleaned | ||||||||||||
| Medicare | 73.32 | (1.33) | 73.62 | (1.29) | 72.21 | (1.36) | 70.39 | (1.51) | 72.49 | (0.68) | 16,735 | 0.524 |
| Medicaid | 9.28 | (0.91) | 9.98 | (0.85) | 8.48 | (0.79) | 11.07 | (1.05) | 9.64 | (0.44) | 2225 | |
| Private insurance | 15.27 | (1.07) | 14.61 | (1.09) | 17.21 | (1.19) | 16.70 | (1.22) | 15.90 | (0.57) | 3670 | |
| Self‐pay | 2.13 | (0.42) | 1.79 | (0.40) | 2.10 | (0.43) | 1.84 | (0.45) | 1.97 | (0.21) | 455 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,085 | ||||||
| Median household income national quartile for patient ZIP Code | ||||||||||||
| 0–25th percentile | 31.09 | (1.53) | 30.65 | (1.54) | 31.29 | (1.50) | 33.80 | (1.71) | 31.61 | (0.77) | 7345 | 0.664 |
| 26th to 50th percentile (median) | 26.64 | (1.41) | 26.59 | (1.31) | 24.40 | (1.40) | 27.18 | (1.53) | 26.16 | (0.70) | 6080 | |
| 51st to 75th percentile | 23.52 | (1.28) | 24.07 | (1.29) | 23.82 | (1.32) | 21.97 | (1.39) | 23.41 | (0.65) | 5440 | |
| 76th to 100th percentile | 18.75 | (1.39) | 18.70 | (1.44) | 20.50 | (1.46) | 17.05 | (1.38) | 18.83 | (0.70) | 4375 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,240 | ||||||
| Bed size of hospital (STRATA) | ||||||||||||
| Small | 13.02 | (1.48) | 13.00 | (1.47) | 14.09 | (1.56) | 13.49 | (1.64) | 13.39 | (0.73) | 3165 | 0.990 |
| Medium | 24.60 | (1.84) | 23.21 | (1.79) | 22.69 | (1.82) | 22.82 | (1.87) | 23.36 | (0.82) | 5520 | |
| Large | 62.38 | (2.13) | 63.80 | (2.13) | 63.23 | (2.19) | 63.69 | (2.25) | 63.25 | (0.96) | 14,950 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,635 | ||||||
| Location/teaching status of hospital (STRATA) | ||||||||||||
| Rural | 1.93 | (0.48) | 2.15 | (0.57) | 3.03 | (0.60) | 2.28 | (0.56) | 2.35 | (0.27) | 555 | 0.120 |
| Urban nonteaching | 17.85 | (1.49) | 17.15 | (1.64) | 12.61 | (1.36) | 14.29 | (1.52) | 15.55 | (0.68) | 3675 | |
| Urban teaching | 80.23 | (1.55) | 80.70 | (1.71) | 84.36 | (1.47) | 83.43 | (1.61) | 82.10 | (0.72) | 19,405 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,635 | ||||||
| Region of hospital | ||||||||||||
| Northeast | 20.82 | (2.07) | 19.14 | (1.96) | 19.25 | (2.01) | 18.75 | (2.00) | 19.53 | (0.86) | 4615 | 0.675 |
| Midwest | 17.36 | (1.58) | 19.78 | (1.88) | 17.28 | (1.70) | 19.25 | (1.81) | 18.38 | (0.77) | 4345 | |
| South | 43.81 | (2.22) | 42.58 | (2.28) | 48.08 | (2.37) | 47.42 | (2.40) | 45.36 | (0.99) | 10,720 | |
| West | 18.01 | (1.60) | 18.50 | (1.70) | 15.40 | (1.55) | 14.58 | (1.57) | 16.73 | (0.72) | 3955 | |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 23,635 | ||||||
3.2. CRT‐D utilization trends
Cardiac resynchronization therapy devices were implanted in 23,635 admissions from 2017 to 2020. Trends are summarized in the Central Illustration (Graphical Abstract). The overall yearly trend of CRT device insertions is presented in Figure 1. During this time period, CRT‐D procedures had a steady decline after reaching a peak in March of 2018, with the largest yearly decrease noted in 2020. On average, 6198 devices were implanted yearly between 2017 and 2019. Device implantation decreased to 5040 occurrences in 2020. Monthly CRT‐D implantation rates from 2017 to 2020 are represented in Figure 2. The largest monthly decreases in CRT‐D insertion volume during 2020 were noted between March to April and November to December. By the end of 2020, CRT‐D insertions reached the lowest that they had been between the years of 2017 and 2020, although there was a brief increase in insertions in October 2020. A reduction in implantations was noted in every region of the United States during 2020, compared to the respective yearly mean between 2017 and 2019; the percent reductions are plotted by region in Figure 3.
FIGURE 1.
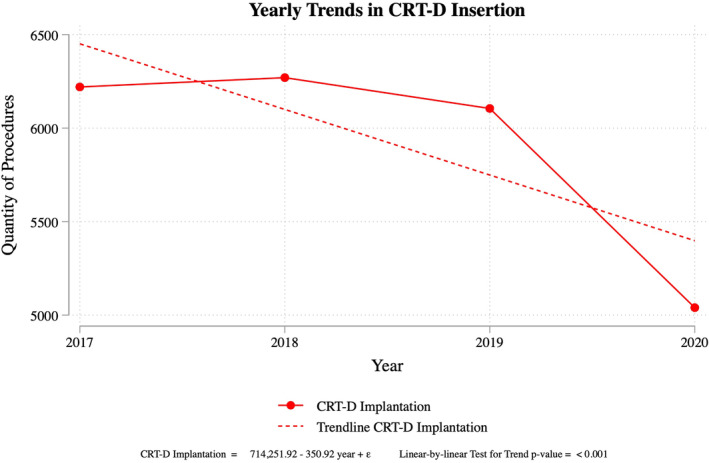
Yearly Trends of CRT‐D Implantation. Quantity of CRT implantations by year from 2017 to 2020. During this time period, CRT‐D implantation rates peaked in 2018 and were the lowest in 2020. There was a significant overall downward trend in implantations. The trends correlate with the start of COVID‐19 pandemic.
FIGURE 2.
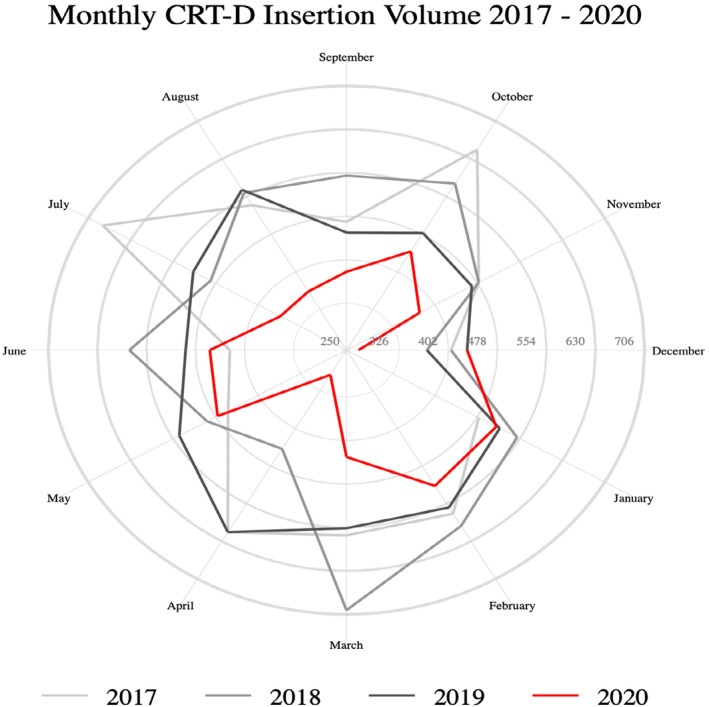
Monthly CRT‐D Implantation. Quantity of CRT‐D implantations by month from 2017 to 2020. CRT‐D implantations broken down by month reveal that there was a significant decline in implantations from February to April 2020, as well as an overall lower number of implantations in the year. The years 2017 to 2019 show a baseline of greater CRT‐D implantations when compared to 2020. source: National inpatient sample
FIGURE 3.
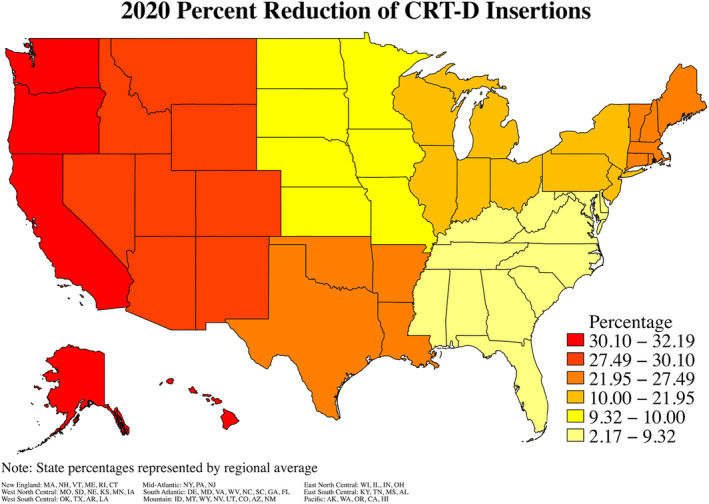
Reduction in CRT‐D Implantation by Region. The percent difference of CRT‐D implantations in 2020 from the average yearly rate between 2017 and 2019 based on the region of the United Statesa. The west region had the greatest reduction in CRT‐D implantation rates, followed by the Central South region. The lowest reduction in implantation rates occurred in the Southeast region. aMade by taking the average insertion total by region from 2017 to 2019, then finding the % difference between that average and the 2020 totals.
CRT‐D yearly implantation rates, grouped by hospital characteristics and patient demographics, are presented in Figure 4. Reduced implantation rates were noted in 2020 when compared to the average of the previous 3 years for every subcohort, including hospital size, location, and teaching status. The reduction in implantations for patients identified as Black was significant in 2020 (adjusted Wald test p = .036), while all other races showed no statistical significance (p > .05, all). There was no statistically significant change in rates associated with elderly patients, identified as those above 75 years of age (p = .756).
FIGURE 4.
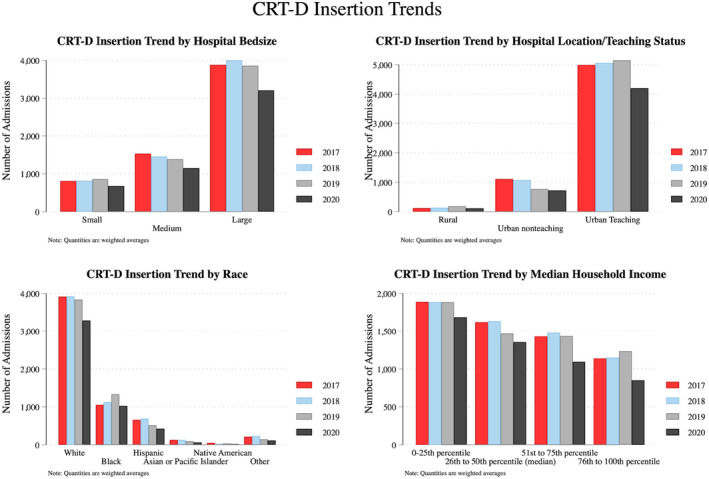
CRT‐D Trends by Hospital and Patient Characteristics. Yearly trends of CRT‐D implantation, stratified by hospital bedside, location and teaching status, race, and median household income. CRT‐D insertions were greater in large hospitals, as well as in urban teaching hospitals. CRT‐D insertions occurred greatest in people of White race and in those in 0‐25th percentile for median household income. Overall numbers were decreased for all categories in the year 2020 when compared to the years 2017–2019.
3.3. Mortality, healthcare utilization
The year 2020 had the highest average death rate during admission at 1.39%, but this difference was statistically insignificant (adjusted Wald test p = .767), and COVID‐19 was not associated with an increased risk of inpatient mortality (OR 0.22, 95% CI 0.03–1.82, p = .162). There was an insignificant increase in the odds of mortality in 2020 when compared to previous years (OR 1.43, 95% CI 0.62–3.26, p = .401). However, patients who had comorbidities, as classified by the Elixhauser comorbidity index, had a statistically significant 57% increase in mortality (OR 1.57, 95% CI 1.38–1.78, p < .001) for each additional medical condition over this 4‐year time period. There was no significant difference in hospital length of stay in 2020 (OR −0.28, 95% CI −0.90–0.34, p = .380); however, a COVID‐19 diagnosis was associated with a 0.19‐day longer length of stay (OR 1.19, 95% CI 0.24–2.14, p = .014). Length of stay was also significantly increased for CRT‐D patients in hospitals with large bed sizes (OR 1.61, 95% CI 1.00–2.22, p < .001) and if it was an urban teaching hospital (OR 1.42, 95% CI 0.37–2.47, p < .008).
4. DISCUSSION
This retrospective review aimed to investigate the national and temporal effects of the COVID‐19 pandemic on the annual prevalence of surgical procedures involving CRT‐D insertion. We identified a substantial decrease in CRT‐D implants that occurred in the year 2020 from the previous 3‐year collective average. This decline in insertion rates was consistent across all geographic locations and hospital characteristics that were analyzed. Our findings align with those of other studies that demonstrated a drastic COVID‐19‐induced decrease in surgical procedures. To highlight this point, a large retrospective review by Levya et al. analyzed the rates of various cardiac procedures, including percutaneous coronary intervention, coronary artery bypass graft, and valve replacements, that were undertaken during the 3 months following the announcement of a national England lockdown in March of 2020. 6 During this 3‐month timeframe, there was a 63% decrease in cardiac operations compared to the same period in 2019. Previously, a cross‐sectional study was completed analyzing the NIS database for CRT and CRT‐D trends from 2006 to 2012 and revealed that there was an overall decrease in CRT procedures over these years. 13
Despite the number of CRT‐D implantations from 2017 to 2020, there was an overall decrease in implantations, with the lowest total occurring in December 2020. It was also found that in patients with comorbidities, there was a statistically significant increase in mortality for each additional comorbidity over the 4 years. An overall reduction in implantations occurred in 2020 for each subcohort of hospital size, location of the hospital in the United States by region, and teaching status. There was a decrease in implantations across races and household income status in 2020 when compared to the previous 3 years. Based on the demographics of the patients receiving CRT‐D implantation, there was a significant reduction in implantations in patients identifying as Black in 2020. These results were consistent with a multicenter retrospective cohort study using the National Cardiovascular Registry Data from 2010 to 2014, which found that 88.6% of eligible patients received CRT‐D, but there were disparities with lower usage in patients who were Black or had nonprivate insurance. 23 Given the nature of heart failure and the reduction in implantations during COVID‐19, many of the patients who needed CRT‐D may have expired during this time.
The COVID‐19 pandemic led to many care delays and healthcare issues for various diseases. Many other specialties were also greatly affected by the pandemic, and a decrease in therapeutic interventions and elective procedures led to delayed management, imaging, and follow‐up, along with increased decompensations and potential missed diagnoses. 8 , 24 Cardiac interventions and procedures also showed an overall decline from 2019 to July 2020 and included decreases in percutaneous coronary intervention, coronary artery bypass grafting, and ablations, amongst others. 6
There were also significant positive outcomes from CRT‐D and the increased usage of remote monitoring during the pandemic. Providers were able to better predict heart failure exacerbations, detect arrhythmias, identify malfunctions, decrease healthcare visits and costs, and reduce exposure to COVID‐19. 4 Alerts from the remote heart failure monitoring system allowed for prompt interventions to prevent further progression and reduce hospitalizations when compared with the traditional in‐office CRT‐D evaluation. 25 The European Heart Rhythm Association survey before and during the pandemic showed a significant increase in the use of remote monitoring for pacemakers, loop recorders, cardiovascular electronic implantable devices (CEIDs), and CRT‐p, as well as a decrease in in‐office visits during the pandemic. 5 ICD and CRT‐D remote monitoring also showed a significant reduction in the physical activity and heart rate of patients when comparing pre‐COVID and during COVID. 26
Delays in implantation and many patients not being able to receive CRT‐D could have potentially detrimental consequences for advanced heart failure patients. The COMPANION trial analyzed NYHA heart failure class III and IV patients and found that CRT‐D reduced mortality and hospitalizations from heart failure by 40% and also decreased overall mortality from any cause by 36% compared to medical management. 27 Khazanie et al. also found that CRT‐D patients benefited from a decreased risk of death at 3 years, lower all‐cause readmissions, and cardiovascular readmissions when compared to medical therapy. 28 The benefits of CRT‐D have been highlighted in prior studies and literature. The patients who were delayed in receiving this therapy due to COVID‐19 may have had overall poor outcomes, which could be due to decreased healthcare availability and use during this time, the patient's not meeting criteria for CRT‐D or not being optimized on guideline‐directed medical therapy, and low procedure volumes in certain hospitals. 29 Possible delays could also be attributed to patients being deterred from medical care during the pandemic, mortality from other reasons, illness due to COVID‐19, and other comorbidities.
4.1. Limitations
Due to the retrospective nature of this study, this study is subject to missing confounders and cannot be used to determine causality. This study also relied on ICD codes, which leads to the potential for under‐identification or missing all potential cases. The data gathered in this study was from the NIS database, and admissions were determined using only the primary diagnosis by which patients presented to the hospital, which is consistent with HCUP's best‐use methodologies. Patients presenting with alternate diagnoses but who were otherwise qualified to be included in this study were excluded, potentially lowering the sample size.
5. CONCLUSION
The COVID‐19 pandemic affected implantation rates of CRT‐D in the United States. As COVID‐19 plateaus, CRT‐D insertions may potentially return to pre‐pandemic levels. Delays in implantation may have long‐term consequences for those requiring life‐saving therapy, particularly those with multiple comorbidities. The CRT‐D trends and associated demographics highlighted through the analysis of the NIS database showed significant effects of the pandemic on CRT‐D insertions in the year 2020. More studies are needed to identify the effects of this delay and the associated clinical and patient outcomes.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interests for this article.
ETHICS
Not applicable.
PATIENT CONSENT
Not applicable.
CLINICAL TRIAL REGISTRATION
Not applicable.
ACKNOWLEDGMENTS
None.
Johal A, Udongwo N, Imburgio S, Mararenko A, Akhlaq H, Dandu S, et al. Negative effects of COVID‐19 on the implantation rate of cardiac resynchronization therapy with defibrillator device. J Arrhythmia. 2024;40:237–246. 10.1002/joa3.12994
REFERENCES
- 1. Czeisler MÉ. Delay or avoidance of medical care because of COVID‐19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rubin R. COVID‐19's crushing effects on medical practices, some of which might not survive. JAMA. 2020;324(4):321–323. 10.1001/jama.2020.11254 [DOI] [PubMed] [Google Scholar]
- 3. Mattingly AS, Rose L, Eddington HS, Trickey AW, Cullen MR, Morris AM, et al. Trends in US surgical procedures and health care system response to policies curtailing elective surgical operations during the COVID‐19 pandemic. JAMA Netw Open. 2021;4(12):e2138038. 10.1001/jamanetworkopen.2021.38038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Popiolek‐Kalisz J, Kalisz G. Cardiac resynchronization therapy remote monitoring–COVID‐19 pandemic experiences and future perspectives. Curr Probl Cardiol. 2022;47(1):100874. 10.1016/j.cpcardiol.2021.100874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Simovic S, Providencia R, Barra S, Kircanski B, Guerra JM, Conte G, et al. The use of remote monitoring of cardiac implantable devices during the COVID‐19 pandemic: an EHRA physician survey. Europace. 2022;24(3):473–480. 10.1093/europace/euab215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leyva F, Zegard A, Okafor O, Stegemann B, Ludman P, Qiu T. Cardiac operations and interventions during the COVID‐19 pandemic: a nationwide perspective. Europace. 2021;23(6):928–936. 10.1093/europace/euab013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lau D, McAlister FA. Implications of the COVID‐19 pandemic for cardiovascular disease and risk‐factor management. Can J Cardiol. 2021;37(5):722–732. 10.1016/j.cjca.2020.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tapper EB, Asrani SK. The COVID‐19 pandemic will have a long‐lasting impact on the quality of cirrhosis care. J Hepatol. 2020;73(2):441–445. 10.1016/j.jhep.2020.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, et al. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy [published correction appears in Eur heart J. 2022 may 1;43(17):1651]. Eur Heart J. 2021;42(35):3427–3520. 10.1093/eurheartj/ehab364 [DOI] [PubMed] [Google Scholar]
- 10. Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac‐resynchronization therapy for the prevention of heart‐failure events. N Engl J Med. 2009;361(14):1329–1338. 10.1056/NEJMoa0906431 [DOI] [PubMed] [Google Scholar]
- 11. Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, et al. Cardiac‐resynchronization therapy for mild‐to‐moderate heart failure. N Engl J Med. 2010;363(25):2385–2395. 10.1056/NEJMoa1009540 [DOI] [PubMed] [Google Scholar]
- 12. Hatfield LA, Kramer DB, Volya R, Reynolds MR, Normand SL. Geographic and temporal variation in cardiac implanted electric devices to treat heart failure. J Am Heart Assoc. 2016;5(8):e003532. 10.1161/JAHA.116.003532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lindvall C, Chatterjee NA, Chang Y, Chernack B, Jackson VA, Singh JP, et al. National trends in the use of cardiac resynchronization therapy with or without implantable cardioverter‐defibrillator. Circulation. 2016;133(3):273–281. 10.1161/CIRCULATIONAHA.115.018830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–1146. 10.1136/hrt.2003.025270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Patel N, Viles‐Gonzalez J, Agnihotri K, Arora S, Patel NJ, Aneja E, et al. Frequency of in‐hospital adverse outcomes and cost utilization associated with cardiac resynchronization therapy defibrillator implantation in the United States. J Cardiovasc Electrophysiol. 2018;29(10):1425–1435. 10.1111/jce.13701 [DOI] [PubMed] [Google Scholar]
- 16. Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M, et al. Guidance for cardiac electrophysiology during the COVID‐19 pandemic from the Heart Rhythm Society COVID‐19 task force; electrophysiology section of the American College of Cardiology; and the electrocardiography and arrhythmias Committee of the Council on clinical cardiology. Heart Rhythm O2. 2020;17(9):e233–e241. 10.1016/j.hrthm.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID‐19. Nat Med. 2020;26(7):1017–1032. 10.1038/s41591-020-0968-3 [DOI] [PubMed] [Google Scholar]
- 18. Douedi S, Mararenko A, Alshami A, al‐Azzawi M, Ajam F, Patel S, et al. COVID‐19 induced bradyarrhythmia and relative bradycardia: an overview. J Arrhythm. 2021;37(4):888–892. 10.1002/joa3.12578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study [published correction appears in BMJ. 2020 mar 31;368:m1295]. BMJ. 2020;368:m1091. 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lin KC, Wang CC, Huang WC, Hwang JJ. Considerations when managing heart failure during the COVID‐19 pandemic‐consensus from the Taiwan Society of Cardiology. Acta Cardiol Sin. 2021;37(2):125–129. 10.6515/ACS.202103_37(2).20200916A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies [published correction appears in Ann intern med. 2008 Jan 15;148(2):168]. Ann Intern Med. 2007;147(8):573–577. 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 22. HCUP‐US NIS Overview . https://www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed February 4, 2023.
- 23. Marzec LN, Peterson PN, Bao H, Curtis JP, Masoudi FA, Varosy PD, et al. Use of cardiac resynchronization therapy among eligible patients receiving an implantable cardioverter defibrillator: insights from the National Cardiovascular Data Registry Implantable Cardioverter Defibrillator Registry. JAMA Cardiol. 2017;2(5):561–565. 10.1001/jamacardio.2016.5388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nunoo‐Mensah JW, Rizk M, Caushaj PF, Giordano P, Fortunato R, Dulskas A, et al. COVID‐19 and the global impact on colorectal practice and surgery. Clin Colorectal Cancer. 2020;19(3):178–190.e1. 10.1016/j.clcc.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ezer P, Gergics M, Szokodi I, Kónyi A. Impact of remote monitoring in heart failure patients with cardiac implantable electronic devices during COVID‐19 pandemic: a single center experience. J Cardiothorac Surg. 2022;17(1):213. 10.1186/s13019-022-01963-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mascioli G, Lucca E, Napoli P, Giacopelli D. Impact of COVID‐19 lockdown in patients with implantable cardioverter and cardiac resynchronization therapy defibrillators: insights from daily remote monitoring transmissions. Heart Vessel. 2021;36(11):1694–1700. 10.1007/s00380-021-01843-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, et al. Cardiac‐resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350(21):2140–2150. 10.1056/NEJMoa032423 [DOI] [PubMed] [Google Scholar]
- 28. Khazanie P, Hammill BG, Qualls LG, Fonarow GC, Hammill SC, Heidenreich PA, et al. Clinical effectiveness of cardiac resynchronization therapy versus medical therapy alone among patients with heart failure: analysis of the ICD registry and ADHERE. Circ Heart Fail. 2014;7(6):926–934. 10.1161/CIRCHEARTFAILURE.113.000838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sandhu A, Bao H, Minges KE, Varosy PD, Borne RT, Zipse MM, et al. Use of cardiac resynchronization therapy defibrillator in US hospitals. JAMA Cardiol. 2019;4(8):804–809. 10.1001/jamacardio.2019.1755 [DOI] [PMC free article] [PubMed] [Google Scholar]


