Abstract
Introduction
Percutaneous techniques for the surgical treatment of vertebral fractures are constantly progressing. There are different biomechanics involved.
Research question
Two percutaneous, monoaxial fixation systems with different reduction tools were analyzed in relation to their reduction capacity. Additionally, the impact of anterior fusion, fracture severity and bone quality on reduction and loss of reduction were examined.
Material and methods
117 cases were retrospectively included in the monocentric study. The subsample (N = 53) with complete data at follow-up times was used to analyze the influence of anterior fusion. The dependencies on fracture severity and bone quality were determined using Spearman and Pearson correlation.
Results
Both systems achieved equally good reduction (9° mean, 95%-CI: 8°–11°, p < 0.001). Anterior fused patients showed not significant (p = 0.057) less loss of reduction over time. Fracture severity had neither an influence on reduction or loss of reduction. Bone quality was positively correlated with greater amount of reduction and less loss of reduction. Early reduction within two days correlated with a greater amount of reduction (p = 0.006). Screw diameters and the patient's weight had no influence on loss of reduction. Complications occurred only in “V2” group.
Discussion and conclusion
Both systems are equivalent in reduction ability. The additional anterior fusion did not result in significantly lower reduction losses. The subsample being small, is a limitation. Good bone quality correlates with better initial reduction and less reduction loss. A preoperative bone density measurement can lead to optimization of surgical techniques.
Keywords: Thoracolumbar fracture, Spine, Percutaneous posterior fixation, Monoaxial, Anterior fusion, Loss of reduction
Highlights
-
•
Both percutaneous, monoaxial systems achieve equally good initial reduction path.
-
•
After seven month there is a relevant loss of reduction in patients with only posterior fixation as well as in patients who got an additional anterior fusion.
-
•
The better the bone quality, the better the reduction results and the less loss of reduction.
-
•
Surgery within two days after diagnosed fracture results in better initial reduction path.
1. Introduction
According to projections, there are around 10,000 serious cases of spinal injuries per year in Germany (Muller et al., 2008). The treatment of vertebral body fractures has made significant progress with the introduction of the more gentle, minimally invasive intervention options (Grass et al., 2006; Prokop et al., 2009).
The aim of this study is to compare two minimally invasive, percutaneous reduction systems with regard to the initial reduction result and to determine possible superiority. In addition, the loss of reduction dependent on a two-stage anterior fusion is examined using a subsample. Besides, the influence of fracture morphology, bone quality, time between date of the accident and treatment, screw diameter and the patient's weight on the reduction are also examined.
These two systems were compared: Ennovate FRI® from BBraun Aesculap (FA) and Viper® 2 from DePuy Synthes (V2). Both systems use monoaxial pedicle screws, but they differ in their technical properties.
2. Material and methods
Inclusion criteria have been a single traumatic fracture in the area of the thoracolumbar junction (Th 11-L 2) and treatment with one of the two percutaneous, monoaxial systems in a short level (bisegmental) manner. The indication for posterior fixation of the fractures was made in accordance with the recommendations of the Spine Section of the German Society for Orthopaedic and Trauma (DGOU) (Verheyden et al., 2018). Another requirement was that the cases had at least one CT taken preoperatively (T1) and one CT or X-ray immediately postoperatively (T3) in the supine position.
Patients who had one or more previous surgeries in the area of the fracture and patients who had an ankylosing spinal disease or an osteoporosis were excluded. C fractures (Vaccaro et al., 2013) were excluded as well because the standard treatment of C-type fractures in the German trauma center is open reduction and fixation.
All eligible cases according the inclusion and exclusion criteria admitted between January 2012 and December 2019 were included.
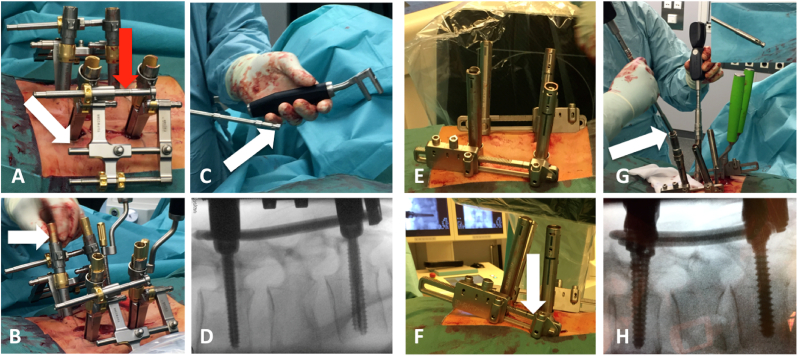
The reduction tools of both systems differ on the one hand in the position of the reduction lever point in relation to the vertebral joint and on the other hand in the rod pushing technique. In the FA system, the fulcrum is close to the vertebral joint, whereas in the V2 this point is above skin level. With the FA system, the rod is pressed in with an additional tool and the setscrew can be screwed in with absolutely no tension, whereas with the V2, the rod is pressed in with the Innie and tension can occur when the thread enters (see Fig. 1).
Fig. 1.
A) Ennovate FRI® BBraun Aesculap with shortened reduction spindle (red arrow) and fixed distance of the pedicle screw heads (white arrow) thus lordotic reduction is performed, fixation arms and the lever point are below skin level
B) screwed-in rod pusher (white arrow) thus reduces the rod into the tulip of the pedicle screw
C) tension-free screwingin of the setscrew, because the rod is already fixed in by the rodpusher
D) reduction result after screwing in the rod pusher and the setscrew
E) Viper® 2 DePuy Synthes before lordotic reduction and
F) after lordotic reduction, white arrow shows lever point above skin level
G) pressing in the rods via preloaded innie on the screw driver using the persuader (the rod is pushed by the Innie)
H) reduction result after screwing in the innies
The data were collected via the hospital information system (ORBIS; Daedalus Healthcare Group) of one German trauma center. All eligible cases according the inclusion criteria were analyzed.
Data collection in the Excel table included the bisegmental Cobb's angle of the base and upper plate (bCA) in the sagittal plane. All kyphotic angles were given a negative sign and all lordotic angles were given a positive sign. The bone quality, gender, date of birth, height and weight of the patients, the day of the accident and surgery, the day of discharge, the screw diameter, the fractured vertebra, the AOSpine classification and the used system were also recorded.
The bone quality was measured using the Hounsfield Units method according to Schreiber et al. (2011). For this purpose, a healthy vertebra adjacent to the fractured vertebra was imaged in the transverse plane in a pre- or, if not available, postoperative CT image of the patient. Three ellipse-shaped measurements (cranial, central, caudal) were then carried out, from which an average value was formed. It was important that this area covered as much of the cancellous bone as possible, while the cortex should remain outside the area.
Bone quality was defined as good with an average HU value above 180, low with values between 180 and 110, and poor with values below 110.
The fractures were initially classified by the examiner using the AOSpine classification (Vaccaro et al., 2013). A comparison was then made with the classification in the doctor's letter. Mismatched classifications were discussed with experienced clinicians.
Based on the data from Reinhold et al. (2010) and Scholz et al. (2018) we generally recommend anterior fusion in addition to posterior fixation. As there is no evidence for a clinical advantage of an additional anterior fusion to our knowledge, we leave the final decision to the patients themselves. Thus, the two groups (posterior only and posterior/anterior) are the result of the patient's decision for or against an anterior fusion.
If the patients decide to undergo an anterior fusion in addition to posterior fixation with a time delay, this was also recorded in a separate sheet of the same Excel table. The “second” day of the surgery was recorded to define the follow-up periods of the subsample.
There have been three surgeons at each technique. The most cases were done by B.W.U. He had educated the other both (F.W. and T.M.).
2.1. Times and periods
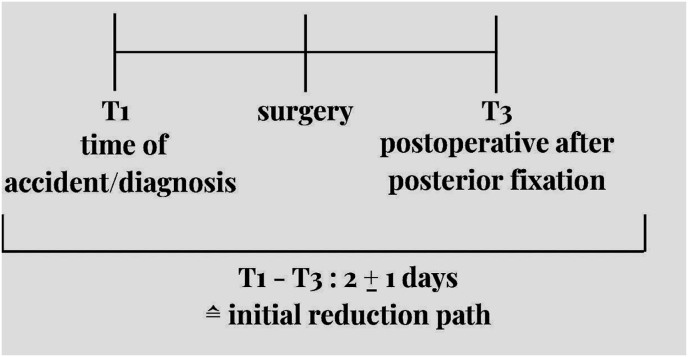
T1 was defined as the time, when the diagnosis was made. T2 was the bCA intraoperatively. Originally it was planned to use the intraoperative bCA for the outcome of the initial reduction. Unfortunately, the images intraoperatively were partwise that bad, that the use of T2 would have resulted in massive data loss. Thus, the intraoperatively data was not used in this study. Instead, T3 was used to define the initial reduction path.
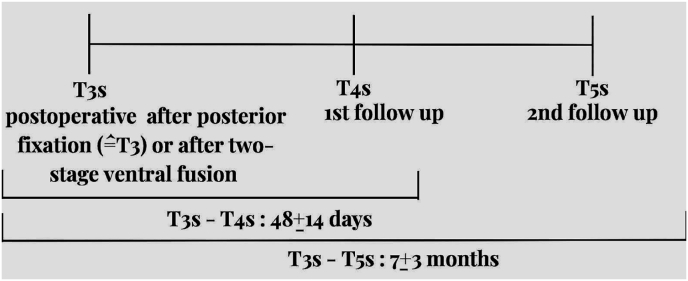
In order to be able to analyze the effect of anterior fusion on loss of reduction, we only used the group with complete follow-up data in our hospital information system in order to be able to work in a statistically clear and fair manner. To define and separate the times and periods of the subsample the suffix -s was used for “subsample” (e.g. T3s).
The times and periods are visually shown in Fig. 2, Fig. 3.
Fig. 2.
1time points and periods of the total sample.
Fig. 3.
time points and periods of the subsample.
3. Statistics
For the statistical analyses SPSS V26 (IBM Corp. IBM SPSS Statistics for Windows; IBM Corp, Armonk, NY) was used.
To answer the questions about the initial reduction outcome, a general linear model (GLM) for bias between the FA and V2 groups was performed. A GLM was also used for repeated measurements. The dependent variables were the bCA at T1 (preoperative) and T3 (immediately postoperative). The FA and V2 systems were between-subject factors.
To answer the questions about loss of reduction, a GLM for bias between the groups with and without additional anterior fusion was carried out. A GLM for repeated measures was also performed. Patients who did not receive additional anterior fusion and patients who did receive additional anterior fusion were between-subject factors.
A GLM for repeated measures was performed to examine the difference between the early reduction and late reduction groups. The within-subject factors were the bCA in T1 (preoperative) and T3 (immediately postoperative). Patients who got treatment within two days after accident and patients who got treatment after 2 day at time of accident were between-subject factors. In addition, a GLM was performed for bias between both groups.
The influence of fracture severity according to AOSpine was calculated using Spearman rank correlation coefficient (rs).
The influence of bone quality, patient weight and screw diameter were calculated using the Pearson correlation coefficient (r).
4. Results
4.1. Descriptive data of the total sample
After applying the inclusing and exclusing criteria, a total of 117 patients were included in the study. These were divided into the groups “FA” (N = 31) and “V2” (N = 86).
Age (p = 0.182), distribution of the fracture level (p = 0.21) and fracture classification (p = 0.077) did not differ significantly in both groups.
The overall sample had an average age of 49 ± 15 years at the time of the accident.
Men were more frequently represented (N = 74; 63%) than women (N = 43; 37%).
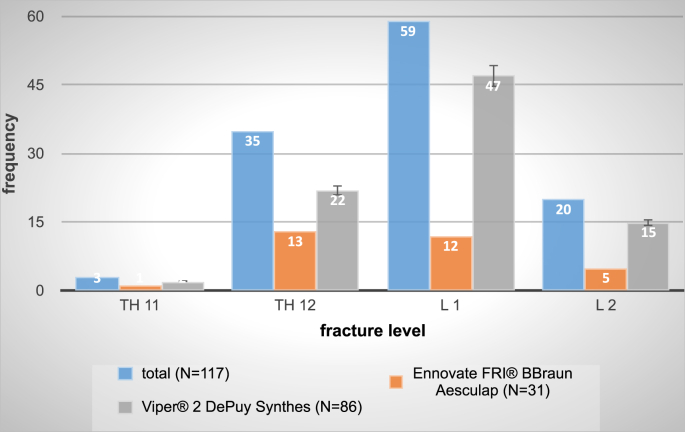
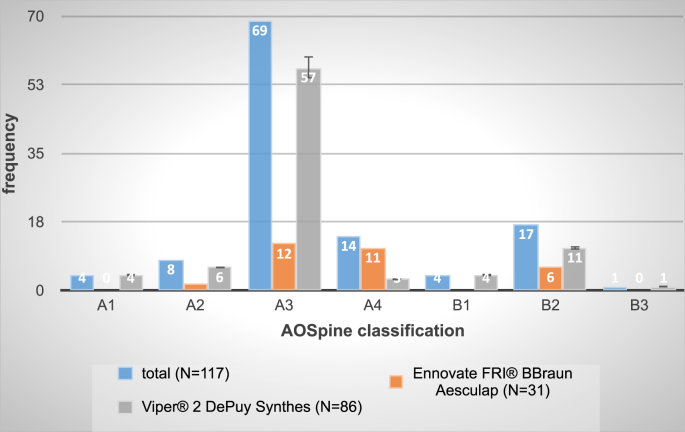
The distribution of the fracture level in the overall sample and separately in the “FA” and “V2” groups can be seen in Fig. 4. L 1 was the most frequently fractured vertebra with a number of 59 (50%). The distribution of fracture classification in the overall sample and separately in the “FA” and “V2” groups is shown in Fig. 5. The A3 fracture was the most frequently recorded fracture type with a number of 69 (59%).
Fig. 4.
Frequencies of fractured vertebrae level divided into the total sample (blue), in the Ennovate FRI® BBraun Aesculap group (orange) and in the Viper® 2 DePuy Synthes group (gray).
Fig. 5.
Frequencies of the AOSpine classifications divided into the total sample (blue), in the Ennovate FRI® BBraun Aesculap group (orange) and in the Viper® 2 DePuy Synthes group (gray).
4.2. Initial reduction result and influence of fracture type and bone quality
Over time (T1-T3: 2 ± 1 days), means after surgical treatment, there was a significant change in the bCA of 9° (mean, 95%-CI: 8°–11°) in the overall sample (p < 0.001). The non-significant interaction effect shows that the reduction result does not differ between the two systems (p = 0.374). A superiority of one of the two systems could therefore not be determined.
The fracture severity according to the AOSpine classification also had no influence on the reduction result (p = 0.088).
The bone quality, on the other hand, showed a significant, positive correlation according to Pearson (p = 0.001, r = 0.354): the better the bone quality, the better the reduction.
Patients who were treated within two days of the accident initially achieved a better reduction result (on average 11° of reduction path, p = 0.006) than patients who were treated after two days after the accident (on average 8° reduction path).
4.3. Descriptive data of the subsample
To answer the questions about the impact of anterior fusion on loss of reduction, a subsample of 53 patients was formed, including 22 without and 31 with additional anterior fusion. The subsample was formed with patients who had imaging (X-ray or CT) at two comparable follow-up dates. A comparison was made between the extent of loss of reduction in patients with and without anterior fusion. Patients without enough follow up documentation were excluded in the subsample.
The system “FA” or “V2” no longer mattered here.
The average age of the subsample was 48 ± 14 years. However, the age differed significantly in the two groups (p = 0.027): the patients in the posterior only group were younger on average (43 ± 16 years) than the patients who were additionally anteriorly fused (51 ± 11 years).
The subsample had an average weight of 87 ± 19 kg. The average BMI was 28 ± 5 kg/m2.
Among the 53 patients, 16 were women (30%) and 37 men (70%).
The distribution of the fracture level (p = 0.559) and fracture classification (p = 0.103) did not differ significantly in both groups.
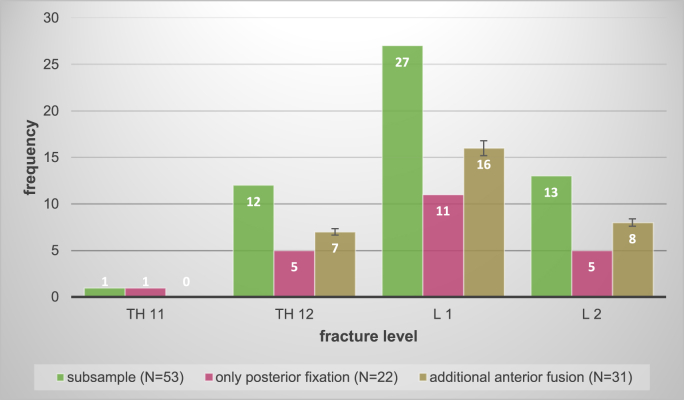
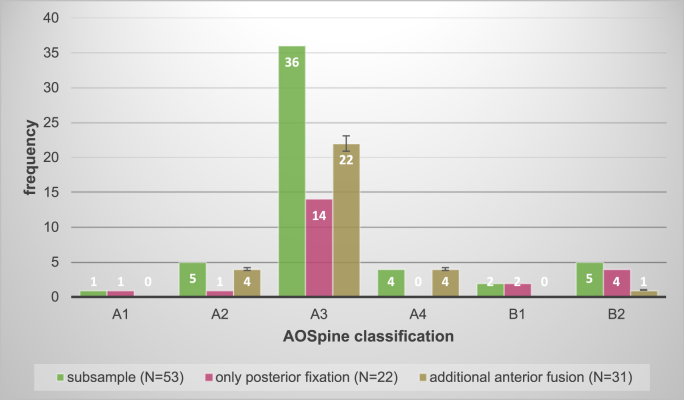
The distribution of the fracture level in the subsample and separately in the two groups can be seen in Fig. 6. L 1 was again the most frequently fractured vertebra with a number of 27 (51%). The distribution of fracture classification in the subsample and separately in the two groups is shown in Fig. 7. The A3 fracture was again the most frequently recorded fracture type with a number of 36 (68%).
Fig. 6.
Frequencies of fractured vertebrae level divided into the total subsample (green), in the group “only posterior fixation” (pink) and in the group “additional anterior fusion” (brown).
Fig. 7.
Frequencies of the AOSpine classifications divided into the total subsample (green), in the group “only posterior fixation” (pink) and in the group “additional anterior fusion” (brown). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
4.4. Loss of reduction and influence of fracture type, bone quality and other factors
The results show that there is a loss of reduction in both groups, both without (N = 22) and with additional anterior fusion (N = 31): The patients stabilized posteriorly alone experienced a long-term loss of reduction (T3s-T5s: 7 ± 3 months) of an average of 6°. The patients who were additionally stabilized anteriorly showed a long-term reduction loss of an average of 4°. However, the difference between the two groups was not statistically significant (p = 0.057).
The fracture severity according to the AOSpine classification also had no significant influence with regard to loss of reduction (p = 0.546).
The bone quality, on the other hand, showed a positive correlation according to Pearson (r = 0.283): The better the bone quality, the less loss of reduction there is in the construct.
Neither patient weight (p = 0.807) nor screw diameter (p = 0.059) had an influence on loss of reduction over time.
4.5. Complications
All nine complications in the follow-up period of this study, implant-specific or -unspecific, occurred in patients of the “V2” group. In the “FA” group no complications occurred (see Table 1).
Table 1.
Complications (only in “Viper® 2” DePuy Synthes group).
| complication | time |
|
|---|---|---|
| Before additional anterior fusion | After additional anterior fusion | |
| implant breakage | 2 | – |
| innie loosening | 2 | 2 |
| non-implant-specific (e.g. pneumonia) | 1 | 2 |
5. Discussion
In the international context, the indication for surgical treatment of A3 fractures according to AOSpine classification is viewed controversially (Li et al., 2023; Chou et al., 2024). When determining the indication, we follow the recommendations of the DGOU Spine Section which, in addition to the fracture classification, also takes into account the fracture-related change in the mono- and bisegmental Cobb angle and advocates surgical intervention from a ∂-Cobb of 10–15°.
5.1. Reduction path and loss of reduction
It was assumed that the FA system would achieve a better initial outcome because the leverage point of this system is closer to the facet joint and is associated with better biomechanics. However, the assumption could not be confirmed: a reduction of 9° could be achieved regardless of the system. This reflects results from the literature (Prokop et al., 2012; Chung et al., 2020).
However, there is a loss of reduction over time in posterior fixation of vertebral fractures (Knop et al., 1997; Spiegl et al., 2016), as in the groups in this study (6° in patients treated posteriorly only, 4° in patients with additional anterior fusion). Loss of reduction is documented in many other studies (5.1° after 60 days in mainly open, monoaxially operated patients in (Spiegl et al., 2016); 5° in combined treated patients in (Ullrich et al., 2018)). Reinhold et al. conducted a comparative study similar to this one. Unlike us, however, they found significantly higher reduction loss (average 6.1°) in patients treated posteriorly only than after combined treatment (average 3.8°) (Reinhold et al., 2009). The follow-up period of 30 months was significantly longer than the period in this study.
Anterior fusion and its supposedly positive effect on loss of reduction remains a controversial topic. In this study no advantage was found regarding loss of reduction in patients with anterior fusion. However, overall it must be noted that the size of the subsample with regard to loss of reduction was relatively small (53 patients). This is a limitation. Furthermore, the question remains at what point there is a relevant loss of reduction. Is the limit set at 5° (Spiegl et al., 2016; Rajasekaran et al., 2015), the loss of reduction of the anterior fusion group with an average of 4° is below the limit and no longer of any significance.
At long last the patient's clinical condition (including pain, mobility) should also be criteria in the assessment of long-term reduction success. It would have been desirable if the patients in this study completed standardized questionnaires before and after follow-up, regardless of whether they had anterior fusion or not. However, the retrospective character of this study did not allow it.
5.2. Fracture severity
Since B fractures are associated with injury to the tension strap and thus with significant stability limitations, it was speculated whether reduction of these fractures would result in a worse radiological outcome. However, the results of the study show that the AOSpine classification has neither an influence on the initial reduction result nor on the loss of reduction. Other studies also come to this conclusion (Knop et al., 1997; Spiegl et al., 2016).
The significance of this result is limited by the classification of the fractures by sometimes only the non-expert examiner. This may have led to misjudgments. But a misjudgment by experienced surgeons is also possible.
However, the AOSpine classification has moderate interrater and substantial intrarater reliability (Kepler et al., 2016; Kaul et al., 2017). Even if the interpretation of the kappa limit values can be viewed critically and has weaknesses (McHugh, 2012), the AOSpine classification as a whole shows a high level of agreement between different observers (Urrutia et al., 2015), when compared to other classification systems and non dependent from the examiner's expertise (Sadiqi et al., 2015). Thus, the limitation of possible misjudgment of the fracture severity is no longer that weight-bearing.
5.3. Bone quality
The Hounsfield Units used for determining bone quality are an alternative method to the gold standard clinical imaging methods, DXA and qCT (Schreiber et al., 2011; Pickhardt et al., 2011; Thomasius et al., 2018).
The bone quality had an influence on the initial reduction result: as the bone quality increased, the outcome also improved. The same applied to the loss of reduction, but only to the patients with anterior fusion.
The literature often shows positive connections between good bone quality and better long-term outcomes (Schreiber et al., 2014; Nguyen et al., 2015). Ullrich et al. were also able to determine a connection in a 2018 study: patients in the “low” and “medium” bone quality groups showed a significant higher loss of reduction than patients in the “good” bone quality group, after anterior fusion of thoracolumbar fractures (Ullrich et al., 2018).
Good bone quality means increased stiffness overall and robustness of the entire instrumentation as a construct (Röhl et al., 2009). It correlates with the mechanical properties of the bone (Knöller et al., 2005). Reduced bone quality is accompanied by a reduction in the fixation of the pedicle screw in the bone, which is why, for example, in patients with osteoporosis additional stabilization using cement augmentation of the screw or a long-range instrumentation should be considered (Weiser et al., 2017).
Bone quality is therefore becoming increasingly important in the treatment planning of thoracolumbar vertebral fractures. It cannot be influenced straight away, but depending on the quality, the technology and material used in treatment can and must be adapted (Ullrich et al., 2018).
5.4. Complications
As expected, screw loosening occurred more frequently in the “V2” group than in the “FA” group. This is because of the different techniques. In V2 the rod is pressed into the tulip via the Innie pre-loaded in the “Persuader”. This means that the Innie runs into the tulip under more or less tension and the thread entry is exposed to an increased risk of damage. This can result in the positive connection between the Innie and tulip threads and thus also the power transmission being reduced. In contrast to this, in FA, the rod is pressed into the tulip of the screw using a rod pusher and the setscrew can run completely tension-free into the thread of the tulip regardless of the press-in pressure of the rod and can then be tightened in a torque-controlled manner. This technique reduces the risk of damage to the thread and therefore improves it form fit and power transmission. Loosening of the locking screws has been described in the literature as a complication of percutaneous stabilization (Weiβ et al., 2015).
Implant breakage was observed in two cases of the “V2” group before anterior fusion. None occurred in the “FA” group. Jutte and Castelein in 2002 described the fact that implant breakages occur less frequently if the vertebral body fracture had additional anterior fusion (Jutte et al., 2002). They saw a susceptibility to implant or screw fractures in only posterior stabilized vertebral body fractures in the area of the lower lumbar spine. A clinical consequence of these data may be a broader indication for anterior fusion of vertebral body fractures.
5.5. Limitations
There are several limitations of this study. First of all, the number of patients included in the study is relatively small, and the “FA” group is clearly smaller than the “V2” group. Therefore, a distortion of results is possible.
Secondly, the difference between angles in CT and X-Ray imaging must be considered (Hong et al., 2015).
Another limitation is the possibly wrong fracture classification. Especially the B fractures tend to be misclassified as only A fractures, because the ligamentous structures are not well seen in CT imaging and a MR imaging is only added in special cases (Schnake et al., 2008).
6. Conclusion
The results show that the minimally invasive reduction of thoracolumbar fractures in the area of the thoracolumbar junction works equally well with both systems. An initial reduction result of 9° is achieved. All patients experience a relevant loss of reduction over the course of about six months. In absolute terms, patients with an additional ventral fusion experience less loss of reduction over time. These results were not significant.
The severity of the injury according to the AOSpine classification has no influence on the reduction result or loss of reduction.
The bone quality, on the other hand, shows a positive correlation in both cases: the higher the patient's bone quality (measured in HU), the better is the initial reduction and there is less loss of reduction. These results confirm the already existing results in the literature. In practice, this means that determining bone quality should continue to play a major role in the treatment decision.
An earlier reduction within the first two days after the accident enables a better initial reduction result. The time until surgical treatment should therefore be kept as short as possible.
Contrary to expectations, the selection of screw diameters and the weight of the patients did not show any influence on loss of reduction. There is still too little data in the literature and further research is needed.
Any invasive procedure can be accompanied by complications. It was assumed that Innie loosening only occurred in the “V2” group; this suggests a technical disadvantage of the instrument. Implant breakage occurs less frequently/not at all in patients with ventral fusion. Minimally invasive spine surgery is and still will become increasingly important in the future. Innovations and technical progress should be encouraged in this area as patients benefit from it.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling Editor: Prof F Kandziora
References
- Chou T.-Y., et al. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit: a systematic review and meta-analysis. Global Spine J. 2024;14(2):740–749. doi: 10.1177/21925682231181875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung W.H., et al. Minimally invasive reduction of thoracolumbar burst fracture using monoaxial percutaneous pedicle screws: surgical technique and report of radiological outcome. J. Orthop. Surg. 2020;28(1) doi: 10.1177/2309499019888977. [DOI] [PubMed] [Google Scholar]
- Grass R., et al. [Percutaneous dorsal versus open instrumentation for fractures of the thoracolumbar border. A comparative, prospective study] Unfallchirurg. 2006;109(4):297–305. doi: 10.1007/s00113-005-1037-6. [DOI] [PubMed] [Google Scholar]
- Hong J.T., et al. Comparative analysis of global spine alignment using whole spine CT and X-ray: correlative analysis of reciprocal and physiologic changes of the cervical alignment. Global Spine J. 2015;5(1_Suppl. l) s-0035-1554535-s-0035-1554535. [Google Scholar]
- Jutte P.C., Castelein R.M. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur. Spine J. 2002;11(6):594–598. doi: 10.1007/s00586-002-0469-8. [DOI] [PubMed] [Google Scholar]
- Kaul R., et al. Reliability assessment of AOSpine thoracolumbar spine injury classification system and Thoracolumbar Injury Classification and Severity Score (TLICS) for thoracolumbar spine injuries: results of a multicentre study. Eur. Spine J. 2017;26(5):1470–1476. doi: 10.1007/s00586-016-4663-5. [DOI] [PubMed] [Google Scholar]
- Kepler C.K., et al. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons. Eur. Spine J. 2016;25(4):1082–1086. doi: 10.1007/s00586-015-3765-9. [DOI] [PubMed] [Google Scholar]
- Knöller S.M., et al. Range of motion in reconstruction situations following corpectomy in the lumbar spine: a question of bone mineral density? Spine. 2005;30(9):E229–E235. doi: 10.1097/01.brs.0000161000.36376.c5. [DOI] [PubMed] [Google Scholar]
- Knop C., et al. Fractures of the thoracolumbar spineLate results and consequences of dorsal instrumentation. Unfallchirurg. 1997;100(8):630–639. doi: 10.1007/s001130050168. [DOI] [PubMed] [Google Scholar]
- Li T., et al. Efficacy and safety of conservative treatment compared with surgical treatment for thoracolumbar fracture with score 4 Thoracolumbar Injury Classification and Severity (TLICS): a systematic review and meta-analysis. Clinical Spine Surgery. 2023 doi: 10.1097/BSD.0000000000001503. 10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M.L. Interrater reliability: the kappa statistic. Biochem. Med. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- Muller C.W., et al. [Traumatology of the spine] Chirurg. 2008;79(10):920–926. doi: 10.1007/s00104-008-1517-7. 918. [DOI] [PubMed] [Google Scholar]
- Nguyen H.S., et al. Posterolateral lumbar fusion: relationship between computed tomography Hounsfield units and symptomatic pseudoarthrosis. Surg. Neurol. Int. 2015;6(Suppl. 24):S611–S614. doi: 10.4103/2152-7806.170443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickhardt P.J., et al. Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J. Bone Miner. Res. 2011;26(9):2194–2203. doi: 10.1002/jbmr.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prokop A., et al. [Minimally invasive percutaneous instrumentation for spine fractures] Unfallchirurg. 2009;112(7):621–624. doi: 10.1007/s00113-008-1556-z. 626-624. [DOI] [PubMed] [Google Scholar]
- Prokop A., et al. Minimalinvasive Versorgung von thorakolumbalen Wirbelfrakturen. Trauma Berufskrankh. 2012;14(3):335–343. [Google Scholar]
- Rajasekaran S., Kanna R.M., Shetty A.P. Management of thoracolumbar spine trauma. Indian J. Orthop. 2015;49(1):72–82. doi: 10.4103/0019-5413.143914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhold M., et al. Operative Behandlung traumatischer Frakturen der Brust- und Lendenwirbelsäule. Unfallchirurg. 2009;112(3):294–316. doi: 10.1007/s00113-008-1539-0. [DOI] [PubMed] [Google Scholar]
- Reinhold M., et al. Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur. Spine J. 2010;19(10):1657–1676. doi: 10.1007/s00586-010-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Röhl K., et al. Biomechanical analysis of expansion screws and cortical screws used for ventral plate fixation on the cervical spine. Eur. Spine J. 2009;18(9):1335–1341. doi: 10.1007/s00586-009-1087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadiqi S., et al. The influence of spine surgeons' experience on the classification and intraobserver reliability of the novel AOSpine thoracolumbar spine injury classification system: an international studys. Spine. 2015;40(23):E1250–E1256. doi: 10.1097/BRS.0000000000001042. [DOI] [PubMed] [Google Scholar]
- Schnake K.J., et al. Typ-B-Distraktionsverletzungen der thorakolumbalen Wirbelsäule. Unfallchirurg. 2008;111(12):977–984. doi: 10.1007/s00113-008-1503-z. [DOI] [PubMed] [Google Scholar]
- Scholz M., et al. Prospective randomized controlled comparison of posterior vs. posterior–anterior stabilization of thoracolumbar incomplete cranial burst fractures in neurological intact patients: the RASPUTHINE pilot study. Eur. Spine J. 2018;27(12):3016–3024. doi: 10.1007/s00586-017-5356-4. [DOI] [PubMed] [Google Scholar]
- Schreiber J.J., et al. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. JBJS. 2011;93(11):1057–1063. doi: 10.2106/JBJS.J.00160. [DOI] [PubMed] [Google Scholar]
- Schreiber J.J., et al. An association can be found between Hounsfield units and success of lumbar spine fusion. HSS J. 2014;10(1):25–29. doi: 10.1007/s11420-013-9367-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegl U.J.A., et al. Zeitverzögerte Indikationsstellung zur additiv ventralen Versorgung thorakolumbaler Berstungsfrakturen. Unfallchirurg. 2016;119(8):664–672. doi: 10.1007/s00113-015-0056-1. [DOI] [PubMed] [Google Scholar]
- Thomasius F., et al. DVO Leitlinie 2017 zur Prophylaxe, Diagnostik und Therapie der Osteoporose bei postmenopausalen Frauen und Männern. Osteologie. 2018;27(3):154–160. [Google Scholar]
- Ullrich B.W., et al. Hounsfield units as predictor for cage subsidence and loss of reduction: following posterior-anterior stabilization in thoracolumbar spine fractures. Eur. Spine J. 2018;27(12):3034–3042. doi: 10.1007/s00586-018-5792-9. [DOI] [PubMed] [Google Scholar]
- Urrutia J., et al. An independent interobserver reliability and intraobserver reproducibility evaluation of the new AOSpine thoracolumbar spine injury classification system. Spine. 2015;40(1):E54–E58. doi: 10.1097/BRS.0000000000000656. [DOI] [PubMed] [Google Scholar]
- Vaccaro A.R., et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine. 2013;38(23):2028–2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- Verheyden A.P., et al. Treatment of fractures of the thoracolumbar spine: recommendations of the spine section of the German Society for Orthopaedics and Trauma (DGOU) Global Spine J. 2018;8(2_Suppl. l):34S–45S. doi: 10.1177/2192568218771668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser L., et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur. Spine J. 2017;26(11):2891–2897. doi: 10.1007/s00586-017-5091-x. [DOI] [PubMed] [Google Scholar]
- Weiß T., Gonschorek O., Bühren V. OUP; 2015. Der perkutane Fixateur interne an der Wirbelsäule Komplikationsrate eines neuen VerfahrensComplication results of a new technique. [Google Scholar]