Abstract
Introduction:
Untreated dental caries (UC), although preventable, is the most prevalent disease in the United States. UC diminishes quality of life and lowers productivity for millions of Americans and is notably higher among lower-income compared to higher-income persons.
Objective:
This study examines changes in disparities by income in past-year dental use (DU) and UC in 4 life stages (2–5, 6–19, 20–64, and ≥65 y) between 1999–2004 and 2011–2016. We also examined changes in dental safety net policies during this time.
Methods:
We obtained data on dependent variables, UC and DU, from cross-sectional, nationally representative surveys for 1999–2004 and 2011–2016. We used multivariable regression models with 3 main-effect explanatory variables: income (<200% or ≥200% federal poverty level), life stage, and survey period (1999–2004 or 2011–2016) and sociodemographic variables. We included 2-way interaction terms among main-effect variables to test whether disparities had changed over time in each life stage and a 3-way term to test changes in disparities differed across life stages.
Results:
Model-adjusted disparities in DU decreased for both preschool-age and school-age children, and disparities in UC decreased for school-age children. Changes in DU and UC disparities were not detectable for working-age adults and increased for retirement-age adults. Changes in DU and UC among preschool and school-age children were not significantly different from one another and were significantly different from changes among retirement-age adults. Compared to working-age adults, changes in disparities for DU and UC were significantly different for school-age children, and changes in DU were significantly different for preschool-age children. Between surveys, the dental safety net was expanded for youth but remained largely unchanged for adults.
Conclusions:
Expanding the dental safety net for youth could have contributed to increased access to dental care among children relative to adults and contributed to the decrease in disparities in DU and UC among youth.
Knowledge Transfer Statement:
Between 1999–2004 and 2011–2016, the dental safety net was expanded for youth but remained largely unchanged for adults. Using national survey data to compare changes in disparities in past-year dental use and untreated dental caries by income between adults and youth sheds light on the potential impact of expanding the dental safety net.
Keywords: health care disparities, dentists’ practice patterns, public policies, dental caries, Medicaid, Medicare
Introduction
Although largely preventable, untreated dental caries remains the most prevalent disease in the world (GBD 2016 Disease and Injury Incidence and Prevalence Collaborators 2017). Pain and infection resulting from untreated caries can diminish academic performance (Jackson et al. 2011), productivity (Righolt et al. 2018), and ability to eat healthy foods (GBD 2016 Disease and Injury Incidence and Prevalence Collaborators 2017). Treatment of severe caries among young children may require use of general anesthesia in a hospital. In 2011, almost 26,000 Medicaid-enrolled children in 6 US states (0.5% of enrollees), aged 1 to 20 y, received caries-related services in a hospital or ambulatory care setting at a cost of $2,581 (2011 US dollars) to Medicaid per hospitalization (Bruen et al. 2016). Productivity losses in the United States attributable to untreated caries were estimated at $4.9 billion in 2015 (Righolt et al. 2018). National data further indicate that over 34 million school hours were lost due to acute, unplanned dental care needs in 2008 (Naavaal and Kelekar 2018).
In 1999–2004, youth and working-age adults with low household income (<200% federal poverty level [FPL]) were at least twice as likely to have untreated caries as were their higher-income counterparts (Centers for Disease Control and Prevention [CDC] 2019). The disparity by income for working-age adults (23 percentage points [PP]) appeared to be larger than that among adolescents aged 12 to 19 y (14 PP). This difference may have been due to differences in Medicaid policy. Medicaid, the major health insurer for low-income persons in the United States, offers comprehensive dental services, including diagnostic, preventive, and restorative services to youth (Kaiser Family Foundation 2016). In contrast, Medicaid dental benefits for adults are not required by federal law but are offered as a state option, with most states providing only limited coverage. In 2000, only 24 states covered at least some nonemergency dental services (Decker and Lipton 2015).
Since 1999–2004, several policies have been implemented to increase access to dental care, most of which have targeted youth. For example, the 2009 Children’s Health Insurance Program Reauthorization Act (CHIPRA) increased youth enrollment by about 4 million (Henry J. Kaiser Family Foundation 2009) and guaranteed comprehensive dental services to all children enrolled in the Children’s Health Insurance Program (Centers for Medicare & Medicaid Services [CMS] 2019; Mann 2014). Launched in 2010, the ensuing CMS Oral Health Initiative provided support to state programs (e.g., technical assistance, action plan templates, peer learning collaboratives) to increase by 10 PP both the percentage of enrollees, aged 1 to 20 y, who received a preventive dental service and the percentage of enrollees, aged 6 to 9 y, who received dental sealants (Chazin 2014; Mann 2014).
In contrast, state Medicaid dental benefits for adults have remained largely unchanged since 1999–2004. Only 11 states had Medicaid dental benefit policies for adults in 2012 that were different from those in 2000; 5 states added dental benefits and 6 states dropped benefits (Decker and Lipton 2015). Medicaid expansion, which some states began to implement in 2014, extended coverage to childless, nonpregnant, nondisabled adults under age 65 y with an income equal to or less than 133% of the FPL (Medicaid and CHIP Payment and Access Commission 2019). It is likely, however, that expansion had limited national impact—of the 27 states that had expanded Medicaid as of February 1, 2015, only 11 offered extensive dental services (i.e., a comprehensive mix of diagnostic, preventive, and restorative procedures with a per-person annual cap of at least $1,000) to Medicaid expansion enrollees (Center for Health Care Strategies 2015; Kaiser Family Foundation 2019). Moreover, access to dental care remains limited upon reaching retirement. Dental benefits are expressly excluded from traditional Medicare (Section 1862 (a)(12) of the Social Security Act). Enrollment in Medicare Advantage plans, of which about 42% offer dental benefits (Freed et al. 2019), however, increased from 5.2% in 2004 to 11.9% in 2011 to 17.6% in 2016 (Henry J. Kaiser Family Foundation 2017). It is likely that most low-income adults were not covered by Advantage plans—only 14% of Medicare beneficiaries with incomes <100% FPL had Advantage plans (Schoen et al. 2018) and less than 15% of Advantage enrollees had family incomes <$10,000, the FPL for a family of 1, in 2008 (Cooper and Trivedi 2012).
Policies also were implemented to increase access among preschoolers that did not differentiate by income. Recommendations include the following: 1) the American Academy of Pediatrics in 2003 that lowered the age for a child’s first dental visit from 3 y to soon after the first tooth erupts (about age 1 y; Hale 2003) and 2) the US Preventive Services Task Force in 2004 for the provision of fluoride varnish in a primary care setting to all children up to age 5 y (Calonge 2004; American Academy of Pediatrics 2008). In addition, implementation of the Affordable Care Act (ACA) in 2014 increased access to dental care among all children regardless of age and income by classifying pediatric dental care as an essential health benefit, thus mandating it be provided in the insurance exchanges (Patient Protection and Affordable Care Act of 2010). The ACA, however, did not include provisions to increase dental coverage among adults not enrolled in Medicaid (Vujicic 2014).
A recent analysis indicated that age- and sex-standardized estimates of untreated caries prevalence had decreased between 1999–2004 and 2011–2016 among low-income youth but not among low-income adults (CDC 2019). In this analysis, we use multivariable regression models to estimate changes in the effect of income on past-year dental use and untreated dental caries between 1999–2004 and 2011–2016 for different life stages. We then compare changes in untreated caries and dental use by income among life stages and discuss these changes within the context of policies implemented to increase dental use.
Methods
Study Population and Design
We used sequential cross-sectional, deidentified data collected in 1999–2004 and 2011–2016 for the Medical Expenditure Panel Survey (MEPS) administered by both the Agency for Healthcare Research and Quality and the CDC, as well as the National Health and Nutrition Examination Survey (NHANES) administered by the CDC. Both surveys are complex, multistage probability samples of the noninstitutionalized US population.
From the Household Component of MEPS, we used self-reported information on sociodemographic characteristics and use of clinical dental services. MEPS interviews subjects at 5 different occasions over 15 mo to limit recall bias (Health and Human Services 2014). MEPS has been reviewed and approved by the Westat institutional review board, established under a multiproject assurance (MPA M-1531) granted by the Office for Protection from Research Risks (OPRR). The project is reviewed and renewed annually. Additional information on MEPS is available at https://meps.ahrq.gov/survey_comp/hc_data_collection.jsp. From NHANES, we used information on untreated dental caries obtained during the dental examination in a mobile examination center and sociodemographic variables collected during the home interview. Visual/tactile oral health assessments were conducted by NHANES dentists who were trained prior to and monitored during data collection to ensure consistent assessment standards. NHANES protocols were approved by the National Center for Health Statistics Ethics Review Board. Additional information on NHANES is available at http://www.cdc.gov/nchs/nhanes.htm.
We defined a disparity as prevalencelow income – prevalencehigher income, where low-income was household income <200% FPL and higher-income ≥200% FPL. With MEPS data, we estimated disparities in past-year dental use (i.e., reported past-year dental expense) for 4 stages of life (preschool age, 1–5 y; school age, 6–19 y; working age, 20–64 y; and retirement age, ≥65 y) in 1999–2004 and 2011–2016. With NHANES data, we estimated disparities in prevalence of untreated dental caries in at least 1 permanent or primary tooth stratified for the same periods and life stages. Edentate persons were included in the analysis and classified as not having untreated dental caries. For dental use, a disparity would be present if the value were negative and, for untreated caries, a positive value. Decreases in disparities over time, however, would be indicated by a positive value for dental use and a negative value for untreated caries.
Outcome Measures
We estimated changes in disparities between 1999–2004 and 2011–2016 for untreated dental caries and past-year dental use for each life stage.
Statistical Analyses
We estimated outcomes with predicted marginals obtained from 2 multivariable logistic regression models (Bieler et al. 2010). The dependent variables were untreated dental caries and past-year dental use. Main effect independent variables in both models were household income (low or higher), survey period (1999–2004 or 2011–2016), and life stage. We included 2-way interaction terms for 1) survey period and income, 2) life stage and income, and 3) survey period and life stage, as well as a 3-way interaction term for survey period, income, and life stage. The 2-way interaction terms allowed us to examine whether outcomes were significant for each life stage, and the 3-way interaction term was used to examine whether outcomes varied across life stages. Covariates in the regression were age (a continuous variable to account for different age composition within a life stage); education level of respondents for adults, aged ≥20 y, and of head of household for persons aged <20 y (<high school, high school or equivalent, >high school); race/ethnicity (non-Hispanic Black, non-Hispanic White, Mexican American, other); and sex.
We used t tests to detect significant differences (P < 0.05). Analyses were conducted using SAS-callable SUDAAN 9.4 (Research Triangle Institute), a statistical software that accounted for the complex sample design of NHANES and MEPS and our use of the sample weights to obtain nationally representative estimates.
Policy Review
To identify policies implemented between 1999 and 2016 that would affect access to dental services, we reviewed 1) provisions of the ACA; 2) changes in recommendations from the US Preventive Services Task Force (USPSTF), the American Dental Association/American Academy of Pediatric Dentistry, and the American Medical Association/American Academy of Pediatrics related to dental preventive services; and 3) changes in national policies implemented by the CMS. To ensure we did not omit relevant policies, we reviewed the list of policies obtained from our review with subject area experts in children’s dental health policy (Children’s Dental Health Project) and adult dental health policy (Chavez et al. 2019). We then stratified identified policies by life stage and income group targeted.
Results
Sample
In MEPS and NHANES, there were, respectively, 24,502 and 4,538 preschool-age, 87,553 and 15,728 school-age, 219,409 and 19,690 working-age, and 46,714 and 6,272 retirement-age persons with data for all analysis variables.
Differences in Disparities in 1999–2004 and 2011–2016
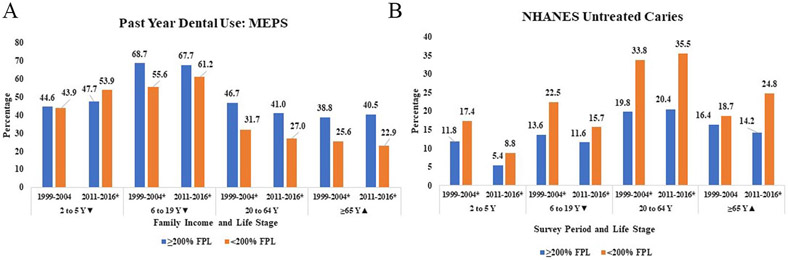
Prevalences of past-year dental use and untreated caries for each age group in both survey periods are provided in the Figure. In 1999–2004, disparities in dental use were significantly lower among preschoolers (−0.6 PP) than among other age groups and among school-age (−13.1 PP) compared to working-age persons (−15.0 PP; Table 1). In 2011–2016, disparities remained lowest among preschoolers (low-income groups were now more likely to have a past-year dental visit than their higher-income counterparts) compared to other life stages. Disparities in dental use among school-age children (−6.4 PP) were significantly lower than among either adult life stage, and the disparity among working-age adults (14.0 PP) was now less than that in retirement-age adults (17.6 PP).
Figure.
Model-adjusted prevalence of past-year dental use (A) and untreated dental caries (B) for higher- and lower-income persons by life stage and survey period (1999–2004 and 2011–2016). FPL, federal poverty level; MEPS, Medical Panel Expenditure Survey; NHANES, National Health and Nutrition Examination Survey. *Significant (P < 0.05) disparity in survey. ▼Significant (P < 0.05) decrease in disparity by income over time. ▲Significant increase in disparity by income over time.
Table 1.
Disparities in Past-Year Dental Use and Untreated Caries by Income in 1999–2004 and 2011–2016.
| Age (y) | Past-Year Dental Use Disparity | Untreated Caries Disparity | ||||
|---|---|---|---|---|---|---|
| 1999–2004, % (SE) |
2011–2016, % (SE) |
Change | 1999–2004, % (SE) |
2011–2016, % (SE) |
Change | |
| 2–5 | −0.6 (1.5)a,b,c | 6.2 (1.5)a,b,c | 6.8 (2.1)d | 5.6 (1.8)b | 3.5 (0.1)b,c | −2.1 (2.1)e |
| 6–19 | −13.1 (0.9)b | −6.4 (1.0)b,c | 6.7 (1.3)d | 8.9 (1.2)b,c | 4.1 (1.1)b,c | −4.9 (1.5)d |
| 20–64 | −15.0 (1.0) | −14.0 (0.5)c | 1.0 (1.0) | 14.0 (1.20)c | 15.1 (1.2)c | −1.1 (1.6)e |
| ≥65 | −13.2 (1.0) | −17.6 (0.1) | −4.4 (1.3)d | 2.3 (1.5) | (2.2) | 8.2 (2.7)d |
Significantly different from age 6–19 y.
Significantly different from age 20–64 y.
Significantly different from age ≥65 y.
Change significantly different.
Unstable estimate, relative standard error >30%.
In 1999–2004, disparities in untreated caries among preschool (5.6 PP) and school-age children (8.9 PP) were not statistically different from one another (Table 1); the disparity in each of these age groups was significantly lower than the disparity among working-age adults (14.0 PP). The statistically insignificant disparity among retirement-age (2.3 PP) was lower than that among working-age and school-age persons. In 2011–2016, disparities among preschool (3.5 PP) and school-age (4.1 PP) children, which were not statistically different from one another, were lower than disparities among working-age (15.1 PP) and retirement-age (14.5 PP) adults. The disparity among retirement-age adults, however, was lower than that among working-age adults.
Changes in Disparities from 1999–2004 to 2011–2016
For dental use, we detected decreases in disparities among preschoolers (Table 1) and school-age children, and for untreated caries, we found decreases among school-age children. We did not detect changes in disparities among working-age adults and found increases among retirement-age adults (Table 1). The only group for whom untreated caries significantly increased between surveys was low-income, retirement age adults (Appendix Fig. 1).
Changes in disparities for dental use among youth (both preschool and school-age) differed from changes among working-age and retirement-age adults (Table 2). Changes in disparities for untreated dental caries differed between school-age children and both working-age and retirement-age adults and between preschool-age children and retirement-age adults. Changes in disparities among working-age adults differed from changes among retirement-age adults.
Table 2.
Percentage Point Difference between Changes in Disparities for Untreated Caries Prevalence and Past-Year Dental Use by Income (Household Income <200% Federal Poverty Level [FPL] or Household Income ≥200% FPL) between 1999–2004 and 2011–2016, National Health and Nutrition Examination Survey and Medical Expenditure Survey.
| Life Stagea | School-Age Children 6–19 y (P Value) |
Working-Age Adults 20–64 y (P Value) |
Retirement-Age Adults ≥65 y (P Value) |
|---|---|---|---|
| Preschool-age children 2–5 y | UC 2.7 (0.24) DU −0.2 (0.94) |
UC −3.2 (0.16) DU −5.9 (0.01) |
UC −10.4 (<0.01) DU −11.2 (<0.01) |
| School-age children | UC −5.9 (<0.01) DU −5.7 (<0.01) |
UC −13.1 (<0.01) DU −11.0 (<0.01) |
|
| Working-age adults | UC −7.2 (<0.01) DU −5.3 (<0.01) |
DU, past-year dental use; UC, untreated caries prevalence.
Life stage in column is reference group. Difference in disparities = value for row – value for column.
Policies
A description of identified policies is provided in Table 3. The ACA and Medicaid expansion would have increased access among all children and low-income adults. The impact of these policies, however, would have been attenuated because they were not in place in 3 of the 6 y in the later survey. The effect of Medicaid expansion would have been further attenuated because only 11 of the states that expanded Medicaid covered dental services (Center for Health Care Strategies 2015; Kaiser Family Foundation 2019). The effect on changes in disparities from 2 of the policies that would have increased access among both low- and higher-income preschoolers also may have been reduced because they were implemented during the later years in the first survey period. The remaining policies implemented between the surveys would have increased access among low-income preschool and school-age children. Increased uptake of Medicare Advantage plans, of which some cover dental services, may have increased access among higher-income relative to lower-income retirement-age adults.
Table 3.
Summary of National Policies Affecting Access to Dental Care Implemented between 1999 and 2016.
| Year Implemented | Targeted Life Stage | Targeted Income Group |
Policy |
|---|---|---|---|
| 2003 | Preschool | All | American Academy of Pediatrics–recommended age for child’s first dental visit changed from 3 y of age to when first tooth erupts (about age 1 y). |
| 2003 | Retirement, some special Medicare populations | Medicare Modernization Act (Medicare Prescription Drug, Improvement, and Modernization Act of 2003) allows private Medicare Advantage plans. These plans can provide dental insurance. From 2004 to 2016, percentage of Medicare enrollees with Medicare Advantage plans increased from 5.2% to 17.6%. In 2016, 42% of Medicare Advantage enrollees had plans that covered restorative dental care. | |
| 2004 | Preschool | All | US Preventive Services Task Force (USPSTF) recommends primary care providers deliver fluoride varnish. |
| 2009 | Preschool, school | Lowa | Children’s Health Insurance Program Reauthorization Act of 2009 expands coverage by increasing percentage of eligible children who are enrolled and providing states latitude to expand eligibility criteria; introduces quality initiative that led to Oral Health Initiative. |
| 2010 | Preschool, school | Low | Centers for Medicare & Medicaid Services implements Oral Health Initiative that includes reaching goals below by 2015: • Increasing percentage of enrolled children, aged 1 to 20 y, receiving dental preventive service by 10 percentage points • Increasing percentage of enrolled children, aged 6 to 9 y, receiving dental sealant on a permanent molar tooth by 10 percentage points |
| 2014 | Preschool | All | Affordable Care Act (ACA): USPSTF grade B recommendations (fluoride varnish) must be provided with no copay. |
| 2014 | Preschool, school | Higher | ACA: pediatric dental care is classified as essential health benefit and must be covered by most insurance plans with no copay, when provided in network. |
| 2014 | Working, retirement | Low | ACA/Medicaid expansion: allowed states to increase eligibility income thresholds for pregnant women and parents and to cover childless adults. Must be included in most individual and small group health plans, including those sold through the Health Insurance Marketplace. Note: Number of state Medicaid agencies offering full (covering extractions and at least preventative, diagnostic, and restorative care), limited (covering more than just emergency dental services but not enough to be considered full coverage), and emergency dental services to adults changed, respectively, from 9, 15, and 19 in 2005; to 9, 18, and 14 in 2010; to 15, 19, and 13 in 2016.b |
In most states, Children’s Health Insurance Program income eligibility limit exceeded “low income” as defined in this article (i.e., <200% federal poverty level).
Discussion
Except for retirement-age adults, differences in disparities across life stages during 1999–2004 were largely consistent with policies that were in place. Disparities in past-year dental use and untreated caries were notably higher among working-age adults, for whom a limited dental safety net existed, compared to youth. Moreover, changes in disparities from 1999–2004 to 2001–2014 were largely consistent with changes in dental safety net policies implemented between the 2 surveys. There were no detectable changes in disparities in dental use or untreated caries among working-age adults. There were, however, notable increases in disparities from 1999–2004 to 2001–2014 in both dental use and untreated caries among retirement-age persons that could have been attributable to increased enrollment in Medicare Advantage plans among higher-income persons. Furthermore, these increases in disparities from 1999–2004 to 2001–2014 among retirement-age adults exceeded those among other life stages. Finally, changes in disparities in dental use among youth significantly differed from changes among adults, suggesting that there were true improvements among the age groups for whom the dental safety net was expanded relative to age groups for whom the safety did not expand. Similarly, the improvement in the disparity in untreated dental caries among school-age children relative to the change for working-age adults was statistically significant.
We believe this is the first analysis to detect an increase in untreated caries (6 PP) among low-income, retirement-age adults from 1999–2004 to 2011–2016. Two other studies that examined this issue did not find an increase (CDC 2019; Griffin et al. 2019). Differences in findings could be due to different models that did not control for the same variables, but it could also be due to inclusion criteria—ours was the only study to include edentate adults. Including edentate adults could result in higher estimated changes between surveys due to increased tooth retention. A recent surveillance summary (CDC 2019) did not detect a difference (statistically insignificant change of 2.4 PP) in age- and sex-standardized prevalence of untreated caries among dentate lower-income, retirement-age adults between 1999–2004 (26.2%) and 2011–2016 (28.6%). Between surveys, however, edentulism significantly decreased from 38.4% to 28.6%. Increases in prevalence, if edentate adults were included, would be 4.3 PP, from 16.1% (61.6% * 26.2%) to 20.4% (71.4% * 28.6%). The change among all low-income, retirement-age adults would be about 70% higher than that among dentate adults. Similarly, the reported significant decrease among higher-income dentate adults (4.3 PP) in the surveillance summary was greater than the decrease among all adults (2.9 PP) in our study. Thus, between surveys, caries risk among both low- and higher-income, retirement-age adults may have increased due to tooth retention, whereas access to clinical dental care likely only increased for higher-income adults. Prevalence of edentulism will likely continue to decrease as baby boomers age, suggesting that the need for primary and secondary caries preventive services among older adults relative to other age groups may increase as well.
One surprising finding was that after controlling for covariates, dental utilization among preschool-age children in 2011–2016 was higher for low-income children relative to their higher-income counterparts, whereas among school-age children, the disparity by income persisted. Expansions in the dental safety net likely were not a factor since changes would have affected both preschool and school-age children. The change in the recommended age for the first dental visit, however, only affected preschool-age children. This policy change could have played a role if messaging and promotion regarding the age 1 dental visit primarily targeted lower-income families.
This study had some limitations. Including both age and life stage as independent variables in our model increased the probability of multicollinearity. With multicollinearity, estimates remain unbiased, but the probability of rejecting a true association is increases (Wooldridge 2015). Second, NHANES and MEPS do not include institutionalized persons in their sampling frame. Thus, we did not have data on adults living in nursing homes or assisted living facilities, about 6.5% of retirement-age adults in 2010 (Institute of Medicine Food Forum 2010). Data suggest these adults have poorer oral health than their community-dwelling counterparts (Griffin et al. 2019), so it is likely that untreated caries prevalence among all retirement-age adults was underestimated relative to the other life stages. Third, in our review of policies, we only explored the effect of national policies to expand access to dental care. We did not include changes in state-specific policies such as Medicaid reimbursements, the comprehensiveness of Medicaid dental benefits for adults, or dental coverage/benefits in employer and private health insurance plans. Nor did we consider policies aimed at stimulating supply as opposed to demand for dental care. For example, during our study period, the Health Resources and Services Administration (2017) expanded clinical dental capacity in federally qualified health centers such that the number of patients receiving dental services increased from 3.4 million in 2009 to 4.8 million in 2014 (Surdu and Langelier 2018). We did not include supply-side policy changes because we could not determine if available capacity varied by life stage, and the number of patients receiving dental services was relatively small when compared to the low-income population represented in our study (about 102 million low-income persons in 2011–2016). Finally, effects of the Great Recession of 2008 to 2010 may have reverberated into 2011–2016. This could have reduced demand for dental care among persons who formerly had financial access (e.g., private dental insurance), which, in turn, could have increased dental capacity for low-income persons with public dental insurance.
In conclusion, we found that dental outcomes typically improved for low-income relative to higher-income youth. This could have been attributable to expansions in the dental safety net for this life stage. These improvements were not observed among adults for whom the safety net remained limited. Trends in increased tooth retention and differential access to dental care by income likely contributed to increased disparities between surveys among retirement-age adults. Disparities could further increase if current trends in edentulism and a limited dental safety net persist.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors received no financial support and declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Footnotes
A supplemental appendix to this article is available online.
References
- American Academy of Pediatrics. 2008. Policy statement: preventive oral health intervention for pediatricians. Pediatrics. 122(6):1387–1194. [DOI] [PubMed] [Google Scholar]
- Bieler GS, Brown GG, Williams RL, Brogan DJ. 2010. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 171(5):618–623. [DOI] [PubMed] [Google Scholar]
- Bruen BK, Steinmitz E, Byshee T, Glassman P, Ku L. 2016. Potentially preventable dental care in operating rooms for children enrolled in Medicaid. J Am Dent Assoc. 147(9):702–708. [DOI] [PubMed] [Google Scholar]
- Calonge N. 2004. Prevention of dental caries in preschool children: recommendations and rationale. Am J Prev Med. 26(4):326–329. [DOI] [PubMed] [Google Scholar]
- Center for Health Care Strategies. 2015. Medicaid adult dental benefits: an overview. 2015 [accessed 2019 Nov 1]. https://www.padental.org/Images/OnlineDocs/Advocacy/DayOnTheHill/CHCS_Medicaid_Adult_Dental_Benefits.pdf [Google Scholar]
- Centers for Disease Control and Prevention. 2019. Oral health surveillance report: trends in dental caries and sealants, tooth retention, and edentulism, United States, 1999–2004 to 2011–2016. Atlanta (GA): CDC, US Department of Health and Human Services. [Google Scholar]
- Centers for Medicare & Medicaid Services. 2019. CHIP reports & evaluations [accessed 2019 Nov 1]. https://www.medicaid.gov/chip/reports-and-evaluations/index.html [Google Scholar]
- Chavez EM, Calvo JM, Jones JA. 2019. Oral health and older Americans: a Santa Fe Group white paper [accessed 2019 Nov 23]. http://santafegroup.org/manage/wp-content/uploads/2018/01/Oral-Health-and-Older-Americans-A-Santa-Fe-Group-White-Paper.pdf [Google Scholar]
- Chazin S. 2014. Medicaid contracting strategies to improve children’s oral health care access. Technical Assistance Brief, Center for Health Care Strategies, October 2014 [accessed 2019 Mar 23]. https://www.chcs.org/media/Medicaid-Contracting-Strategies-to-Improve-Childrens-Oral-Health-Access.pdf [Google Scholar]
- Children’s Health Insurance Program Reauthorization Act of 2009, Pub. L. 111–3, § 501(d), 123 STAT. 87 (February 4, 2009).
- Cooper A, Trivedi AN. 2012. Fitness memberships and favorable selection in Medicare Advantage plans. N Engl J Med. 366(2):150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker SL, Lipton BJ. 2015. Do Medicaid benefit expansions have teeth? The effect of Medicaid adult dental coverage on the use of dental services and oral health. J Health Econ. 44:212–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed M, Neuman T, Jacobson G. 2019. Drilling down on dental coverage and costs for Medicare beneficiaries. Kaiser Family Foundation Issues Brief; 2019 [accessed 2020 April 29]. https://www.kff.org/medicare/issue-brief/drilling-down-on-dental-coverage-and-costs-for-medicare-beneficiaries/ [Google Scholar]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. 2017. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 390(10100):1211–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SO, Griffin PM, Li C-H, Bailey WD, Brunson D, Jones JA. 2019. Changes in older adults’ oral health and disparities: 1999–2004 and 2011–2016. J Am Geriatr Soc. 67(6):1152–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale KJ. 2003. American Academy of Pediatrics Section on Pediatric Dentistry. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 111(5):1113–1116. [DOI] [PubMed] [Google Scholar]
- Health and Human Services. 2014. Oral health [accessed 2017 July 14]. www.healthypeople.gov/2020/topics-objectives/topic/oral-health/objectives
- Health Resources and Services Administration. 2017. 2014 Health Center Program Grantee data [accessed 2020 Feb 15]. https://bphc.hrsa.gov/uds/datacenter.aspx?year=2014
- Henry J. Kaiser Family Foundation. 2009. The Kaiser Commission on Medicaid and the Uninsured. State Children’s Health Insurance Program (CHIP): reauthorization history, revised February 2009 [accessed 2019 Jan 2]. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7743-02.pdf. [Google Scholar]
- Henry J Kaiser Family Foundation. 2017. Medicare Advantage 2017 spotlight: enrollment market update [accessed 2019 Nov 23]. https://www.kff.org/medicare/issue-brief/medicare-advantage-2017-spotlight-enrollment-market-update/ [Google Scholar]
- Institute of Medicine Food Forum. 2010. Providing healthy and safe foods as we age: workshop summary. Washington, DC: National Academies Press; [accessed 2019 Nov 25]. https://www.ncbi.nlm.nih.gov/books/NBK51841 [PubMed] [Google Scholar]
- Jackson SL, Vann WF Jr, Kotch JB, Pahel BT, Lee JY. 2011. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 101(10):1900–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. 2016. Access to dental care in Medicaid: spotlight on nonelderly adults [accessed 2019 Dec 20]. http://files.kff.org/attachment/issue-brief-access-to-dental-care-in-medicaid-spotlight-on-nonelderly-adults [Google Scholar]
- Kaiser Family Foundation. 2019. Status of state action on the Medicaid Expansion decision [accessed 2019 Nov 1]. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- Mann C. 2014. Update on CMS oral health initiative and other oral health related items (CMCS Informational Bulletin). Baltimore (MD): Center for Medicaid and CHIP Services. [Google Scholar]
- Medicaid and CHIP Payment and Access Commission. 2019. Medicaid 101: Eligibility [accessed 2019 Nov 1]. https://www.macpac.gov/medicaid-101/eligibility/ [Google Scholar]
- Medicare Prescription Drug, Improvement, and Modernization Act of 2003, Pub. L. 108-183 (December 8, 2003). [Google Scholar]
- Naavaal S, Kelekar U. 2018. School hours lost due to acute unplanned dental care. Health Behav Policy Rev. 5(2):66–73. [Google Scholar]
- Patient Protection and Affordable Care Act of 2010. Pub. L. No. 114–148 (March 23, 2010), as amended through May 1, 2010 [accessed 2019 Nov 23]. https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf [Google Scholar]
- Righolt AJ, Jevdjevic M, Marcenes W, Listl S. 2018. Global-, regional-, and country-level economic impacts of dental diseases in 2015. J Dent Res. 97(5):501–507. [DOI] [PubMed] [Google Scholar]
- Schoen C, Davis K, Willink A, Buttorff C. 2018. A policy option to enhance access and affordability for Medicare’s low-income beneficiaries [accessed 2020 May 27]. https://www.commonwealthfund.org/publications/issue-briefs/2018/sep/medicare-low-income-beneficiaries [PubMed] [Google Scholar]
- Surdu S, Langelier M. 2018. Trends in the provision of oral health services by federally qualified health centers. Rensselaer (NY): Oral Health Workforce Research Center, Center for Health Workforce Studies, School of Public Health, SUNY Albany; [accessed 2020 May 27]. http://www.oralhealthworkforce.org/wp-content/uploads/2018/02/OHWRC_Trends_in_Provision_of_Oral_Health_Services_by_FQHCs_2018.pdf [Google Scholar]
- Vujicic M. 2014. A tale of two safety nets. J Am Dent Assoc. 145(1):83–85. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM. 2015. Introductory econometrics: a modern approach. 6th ed. Boston (MA): Cengage Learning. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.