Abstract
Macrophages play a crucial role in coordinating the skeletal muscle repair response, but their phenotypic diversity and the transition of specialized subsets to resolution-phase macrophages remain poorly understood. To address this issue, we induced injury and performed single-cell RNA sequencing on individual cells in skeletal muscle at different time points. Our analysis revealed a distinct macrophage subset that expressed high levels of Gpnmb and that coexpressed critical factors involved in macrophage-mediated muscle regeneration, including Igf1, Mertk, and Nr1h3. Gpnmb gene knockout inhibited macrophage-mediated efferocytosis and impaired skeletal muscle regeneration. Functional studies demonstrated that GPNMB acts directly on muscle cells in vitro and improves muscle regeneration in vivo. These findings provide a comprehensive transcriptomic atlas of macrophages during muscle injury, highlighting the key role of the GPNMB macrophage subset in regenerative processes. Targeting GPNMB signaling in macrophages could have therapeutic potential for restoring skeletal muscle integrity and homeostasis.
INTRODUCTION
Skeletal muscle is the most abundant human body tissue, comprising 30–45% of body weight, and the maintenance of its integrity and homeostasis is of critical importance. The complete regeneration of skeletal muscle after injury requires coordinated communication among several distinct cell types, including immune cells, muscle stem cells (MuSCs), fibro-/adipogenic progenitors (FAPs), glial cells, and vascular cells1,2. Tight control of signal integration in the injury-induced immune response has been shown to promote regeneration in several tissues, such as the liver3, heart4, and skeletal muscle5. In the past, research on the role of macrophages in tissue regeneration has focused on their ability to phagocytose cellular debris. However, infiltrating macrophages can undergo a polarization shift toward an anti-inflammatory phenotype and exhibit various pro-regenerative functions. These functions include the remodeling of the extracellular matrix (ECM)6 and the stimulation of MuSC proliferation7. Disturbances in macrophage function lead to impaired muscle regeneration8, highlighting the importance of these cells in the regeneration process. It has been suggested that Ly6Clo macrophages contribute to skeletal muscle9,10 and myocardial tissue regeneration11. The core genes expressed in Ly6Clo macrophages include secretory cytokines and growth factors such as insulin-like growth factor 1 (IGF1)12, the growth differentiation factors GDF314, GDF1515, and transforming growth factor beta (TGF-β)13,15, which act in an anti-inflammatory manner and contribute to skeletal muscle regeneration.
Glycoprotein nonmetastatic melanoma protein B (GPNMB), which was initially identified as a regulator of tumor growth in melanoma with low metastatic potential16, is involved in the transendothelial migration of dendritic cells17. GPNMB also inhibits osteoclast differentiation by interacting with CD44 and inhibiting ERK activation18. In the brain, GPNMB is predominantly expressed in microglia, which serve as resident cells responsible for mediating inflammatory stimuli and neurodegeneration19. Furthermore, GPNMB expression is elevated in human liver samples from patients with hepatitis, cirrhosis, and paracetamol intoxication, all of which are associated with inflammatory diseases, compared to samples from healthy controls. Notably, the deletion of GPNMB in mice led to a significant increase in the levels of inflammatory cytokines in macrophages, suggesting that GPNMB may suppress the transition of macrophages toward a proinflammatory state20. However, the precise biological roles of GPNMB in macrophages during skeletal muscle regeneration remain to be elucidated.
In this study, we used a cardiotoxin (CTX)-induced skeletal muscle injury model, which induces myofiber necrosis and provides a highly reproducible framework. This model allowed us to visualize temporal changes in macrophage subsets and analyze their roles in muscle regeneration. We discovered that the expression of GPNMB was upregulated in a sustained manner, reaching its highest level on day 3, in a specific macrophage subset that coexpresses critical factors involved in macrophage-mediated muscle regeneration. Furthermore, myeloid-specific Gpnmb knockdown impaired the regeneration of skeletal muscle. The extrinsic administration of recombinant GPNMB to injured mice promoted myogenesis by activating myocyte differentiation. Overall, our study describes unrecognized macrophage subsets involved in muscle regeneration and demonstrated that GPNMB acts on myocytes in vitro and promotes muscle regeneration in vivo.
MATERIALS AND METHODS
Animals
All animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC) of China Medical University Hospital (license no. CMUIACUC-2023-061). Eight- to twelve-week-old female C57BL/6J mice were provided by the National Laboratory Animal Center (NLAC, Taiwan) and housed at the China Medical University Hospital Animal Center. Gpnmb−/− mice were generated in cooperation with the Transgenic Core Facility at the Academia Sinica, Taiwan. For this strain, exons 2–6 of the Gpnmb gene were deleted via CRISPR-Cas9 technology. The C57BL/6J wild-type strain was used as the control for animal experiments.
Cardiotoxin injections and cell isolation
A total of 40 μl of Naja pallida CTX (Merck KGaA), at a concentration of 10 μM in PBS, was injected into the TA muscle of anesthetized mice (i.m.). Furthermore, to investigate the potential impact of recombinant GPNMB (rGPNMB) on skeletal muscle regeneration, we simultaneously administered CTX at two concentrations (10 or 20 μg) of rGPNMB. Injured TA muscles were collected at the indicated time points after injury. To examine the regenerating myofibers, 10-mm cross sections were collected from the frozen TA muscles and stained with an embryonic myosin heavy chain (eMyHC, DSHB F1.652) antibody. The sections were imaged with a Nikon ECLIPSE Ti2 fluorescence microscope. Quantification of eMyHC staining was performed with ImageJ. Individual fibers were manually outlined to determine the cross-sectional area. At least 50 fibers per image and 3–5 images were analyzed at each indicated time point. We used a commercial murine skeletal muscle dissociation kit with a GentleMACS Octo Dissociator (Miltenyi Biotec). The TA muscles were excised and cut into small pieces following the manufacturer’s protocol. The digested product was filtered through a 70-μm cell strainer using a plunger to disrupt the undigested tissue and washed with RPMI-1640 containing 1% P/S, 20 mM HEPES, and supplemented with 0.5% serum. After resuspension in 47% Percoll (Cytiva) and centrifugation at 1500 rpm for 10 min, the cells were collected and washed for flow cytometric analysis or single-cell RNA-seq.
Magnetic separation of mononuclear cells and flow cytometric analysis
We used MACS separators to enrich the mononuclear cells obtained from the TA muscle to increase the number of macrophages. The mononuclear cells were isolated using anti-mouse CD90.2 and B220 MicroBeads (Miltenyi Biotec) through negative sorting per the manufacturer’s protocol to eliminate most T and B cells. Similarly, anti-mouse CD45 MicroBeads (Miltenyi Biotec) were used to sort the flowthrough. For flow cytometric analysis, we utilized TA muscle-derived mononuclear cells with a CytoFLEX flow cytometer (Beckman Coulter). In addition, fluorochrome-conjugated antibodies against CD45 (catalog 53-5773-82, eBioscience), CD11b (catalog 15-0112-82, eBioscience), CD68 (catalog 53-0681-82, eBioscience), Ly6C (catalog 17-5932-82, eBioscience), and GPNMB (catalog 50-5708-82, eBioscience) were used.
Cell culture
BMDCs from mice were cultured according to a previous protocol21. Briefly, bone marrow-derived cells from the femur and tibia were flushed out using Dulbecco’s modified essential medium (DMEM) and filtered through a 70-μm cell strainer. Red blood cells were removed using ACK lysis buffer (Thermo Fisher). BMDCs were cultured in DMEM supplemented with 10% fetal bovine serum, antibiotics (100 U/mL penicillin and 100 μg/mL streptomycin), and 20 ng/ml macrophage colony-stimulating factor (M-CSF; PeproTech) for 7 days to allow differentiation into BMDMs. The BMDMs were polarized into M1 or M2 macrophages by using LPS (100 ng/ml, Sigma Aldrich) plus IFN-γ (45 ng/ml, PeproTech) or IL-4 (10 ng/ml, PeproTech), respectively. C2C12 myoblasts were purchased from ATCC and cultured in DMEM supplemented with 10% FBS until confluency. After reaching confluency, the myoblasts were differentiated in DMEM supplemented with 1% horse serum for 72 h, as previously described22.
Efferocytosis assay
An efferocytosis assay was designed to evaluate the capacity of macrophages to phagocytose apoptotic cells in the context of GPNMB deficiency. BMDMs were harvested from GPNMB-KO and WT mice. Mononuclear cells were isolated from the TA muscle on day 3 post-CTX-induced injury. C2C12 myoblasts were labeled with carboxyfluorescein succinimidyl ester (CFSE) to track their uptake by macrophages. C2C12 cell apoptosis was induced using staurosporine (STS) treatment. BMDMs were cocultured with CFSE-labeled apoptotic C2C12 cells for 24 hours to allow for efferocytosis. After cocultivation, macrophages were stained with anti-F4/80 and anti-CD11b antibodies to identify the population of interest. Flow cytometry was subsequently utilized to quantify the percentage of macrophages that phagocytosed apoptotic C2C12 cells, as indicated by double positivity for F4/80, CD11b, and CFSE fluorescence. The percentage of F4/80+CD11b+ macrophages containing CFSE+ material was compared between the GPNMB-KO and WT groups to assess the impact of GPNMB on the efferocytosis of macrophages.
Single-cell RNA-seq (10x Genomics)
We isolated fresh cells and enriched them using MicroBeads to obtain high-quality single-cell RNA sequencing data, as previously described23. We then encapsulated these cells in droplet emulsions using a 10x Chromium Controller (10x Genomics) to achieve 10,000 cells per sample. The scRNA-seq libraries were prepared according to the manufacturer’s protocol using the GenCode Single-Cell 3’ Gel Bead and Library V3 kit. Subsequently, we pooled the libraries and sequenced them on a NovaSeq 6000 System (Illumina) following the manufacturer’s instructions.
Single-cell RNA sequencing data processing
We obtained 31,395 single cells with a median of 80,046 reads per cell. Paired-end single-cell RNA sequencing (scRNA-seq) reads were demultiplexed, aligned to the mm10 reference genome, and processed for single-cell gene counting using Cell Ranger Software from 10X Genomics, Inc. (https://support.10xgenomics.com/single-cell-gene-expression/software). Downstream analysis of the combined sample gene counts was performed using Seurat, a scalable R-based package (version 4.3.0) designed for single-cell gene expression datasets. Gene counts were imported using the CreateSeuratObject function (min.cells = 25, min.features = 0), and low-quality cells were discarded using the following thresholds: a minimum of 500 and maximum of 5000 genes, a maximum of 10% of mitochondrial gene mapped reads, and a minimum of 1,000 and maximum of 40,000 UMIs. The total number of cells that passed quality control according to the abovementioned thresholds was 21,642. SCTransform normalization, which uses regularized negative binomial regression for normalizing sparse single-cell data and variance stabilization, was performed for the filtered dataset using the SCTransform function in Seurat, regressing the percentage of mitochondrial genes per cell (vars.to.regress = “percent.mt”).
Cell–cell communication analysis
Cellular communication networks were quantitatively inferred and analyzed using scRNA-seq data. The open-source R package CellChat was used to visualize the interactions among different cell groups24. Two hundred twenty-nine signaling pathway families were grouped as a library to analyze cell–cell communication. Circle, hierarchy, and river plots were generated according to the ligand–receptor interaction network.
Real-time qPCR
Total RNA was isolated from the TA muscle and C2C12 myoblasts with Direct-zol RNA Kits (Zymo Research), and mRNA levels for this study were determined by quantitative PCR on a CFX Opus 96 Real-Time PCR System (Bio-Rad, CA, USA). Primer 3 software was used across the intronic sequences to design all primers.
Statistical analysis
All the statistical analyses were performed with Student’s t test or ANOVA for comparisons of three or more groups using GraphPad Prism (GraphPad Software, V9.2.0). Differences were considered statistically significant when P < 0.05 (*p < 0.05, **p < 0.01, ***p < 0.001, ns: not significant).
RESULTS
Dynamics of macrophage subset changes during skeletal muscle regeneration
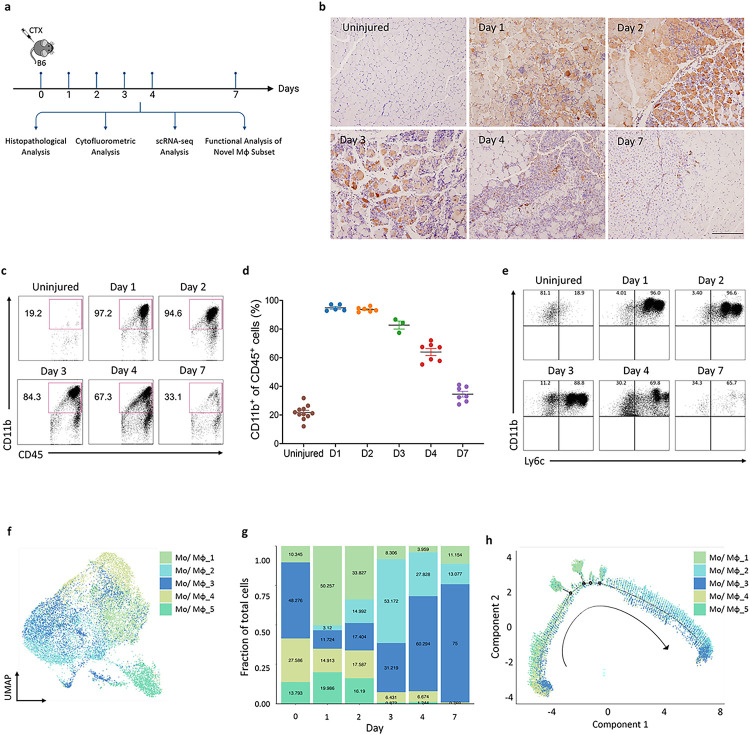
To reveal the changes in macrophage heterogeneity and identify the specific subsets influencing skeletal muscle regeneration following injury, we intramuscularly injected CTX into the tibialis anterior (TA) of mice. The TA tissues were collected at the designated time points for multiple analyses (Fig. 1a). Consistent with previous reports25, these infiltrated immune cells were mainly CD68+ monocytes/macrophages (Fig. 1b). Cytofluorometric analysis confirmed the robust infiltration of circulating monocytes and the generation of macrophage subsets in the regenerating muscle. These cells were initially proinflammatory Ly6Chi cells but transformed into anti-inflammatory Ly6Clo cells by day 4 (Fig. 1c–e). For unbiased analysis that integrates temporal gene profiling of macrophages with analysis of their potentially varying roles in muscle regeneration, we enriched CD90.2−B220−CD45+ cell populations by using magnetic beads at the indicated time points during skeletal muscle regeneration. Subsequently, single-cell RNA-seq (scRNA-seq) analysis was performed using the 10X Genomics Chromium platform (Fig. S1a). After standard quality control and the removal of doublets, high-quality transcriptomes from 21,642 cells were revealed. We performed graph-based Leiden clustering and utilized uniform manifold approximation and projection (UMAP) embeddings for visualization. All clusters were annotated by utilizing the scMCA_MNN-muscle dataset and differentially expressed genes (DEGs). Fifteen cell clusters were revealed, including five subsets of monocytes/macrophages (Mo/Mφ), five subsets of neutrophils, and one subset each of dendritic cells, T cells, B cells, muscle progenitor cells, and stromal cells (Fig. S1b and c). As expected, macrophages and neutrophils were the most abundant cell populations after, with proportions of 67.9% and 15.3%, respectively (Fig. S1c).
Figure 1. Identification of five distinct macrophage subsets during skeletal muscle regeneration via single-cell RNA-seq.
(a) Schematic showing the experimental timeline for CTX-induced skeletal muscle injury in mice, delineating the key analyses performed at various days post-injury. (b) Immunohistochemical detection of Cd68+ macrophages within injured muscle at specified time intervals post-injury. The magnification scale bar represents 100 μm. (c) Flow cytometric analysis showed a surge in CD11b+ cells immediately after injury, which diminishes starting from day 3. (d) Graphical representation of CD11b+ cell percentages, corresponding to flow cytometry results depicted in (c). (e) The transition of macrophage phenotypes from proinflammatory Ly6chi early post-injury to anti-inflammatory Ly6clo by day 4, as assessed by flow cytometry. (f) UMAP plot illustrating the distribution of five identified monocyte/macrophage subsets across the time series. (g) Bar graph showing the relative frequencies of each monocyte/macrophage subset at the designated time points post-injury. (h) Pseudotime analysis projecting the potential developmental trajectories of the monocyte/macrophage subsets identified.
Identification of five distinct macrophage subsets during skeletal muscle regeneration
We reclustered our scRNA-seq data of the macrophage subsets and identified five groups of macrophage subsets (Fig. 1f) whose distributions changed dynamically at different time points (Fig. 1g). Pseudotime analysis was performed on all five cell clusters along the injury-to-regeneration trajectory via Monocle (v3) to delineate the expression patterns of genes following muscle injury (Figs. 1h and S2a). These dynamic changes suggest that the unique macrophage subset distributions may have critical biological functions at specific time points. The five distinct macrophage clusters (Mo/Mφ clusters: 1, 2, 3, 4, and 5) shared a common core of expressed macrophage markers, including Adgre1, Cd68, Csf1r, Fcgr1, Lgals3, and Lyz2 (Fig. S1d). However, they exhibited distinct transcriptional profiles: Cluster 1 exhibited increased expression of the M2 macrophage activation markers Arg1 and Mrc1; Cluster 2 exhibited increased expression of genes associated with tissue regeneration, such as Igf1 and Gdf15, which is in line with the recently described finding that GDF15 is a critical effector during skeletal regeneration20; and Cluster 3 exhibited increased expression of genes associated with immune response activation and antigen presentation, including H2-Aa, H2-Ab1, and H2-Eb1. Moreover, the proportion of cells in Cluster 3 was notably greater than that of cells in other clusters in both the uninjured and regenerative stages; Cluster 4 exhibited high expression of genes involved in proinflammatory responses, such as Ifitm6, Gsr, and Hp; Cluster 5 exhibited increased expression of Acod1 (aconitate decarboxylase 1, also known as immunoresponsive gene 1), a key regulator of immunometabolism during infection and inflammation (Fig. S1e). During the acute inflammatory stage (days 1 and 2), most cells were cells from Clusters 1, 4, and 5, while there were only minor increases in the numbers of cells in Clusters 2 and 3. With the transition from the acute inflammatory stage to the regenerative stage (day 3), the proportions of cells in Clusters 1, 4, and 5 decreased, and there was a marked increase in the proportion of cells in Cluster 2, which then declined by day 7. In contrast, the proportion of cells in Cluster 3 gradually and consistently increased over 7 days, peaking at the regenerative stage. Thus, our findings identified five macrophage subsets with dynamic changes throughout the regenerative process. Although the Clusters 2 and 3 subsets were present in high proportions during the inflammatory-to-regenerative transition stage on day 3, Cluster 2 cells expressed relatively higher levels of genes involved in macrophage-mediated tissue regeneration than did Cluster 3 cells (Fig. S1e). For example, IGF1 is one of the best-characterized growth factors and has been shown to regulate muscle regeneration26. IGF1 binds its receptor IGF1R to phosphorylate the intracellular adapter protein insulin receptor substrate-1 (IRS-1), which in turn activates the PI3K/AKT pathway to facilitate skeletal muscle regeneration. Moreover, ablation of triggering receptor expressed on myeloid cells-2 (TREM2), a major macrophage sensor known for supporting immune cell responses, has been noted to impede hepatic reparative processes in response to metabolic disruptions27,28. In view of these findings, it is conceivable that the macrophage Cluster 2 we identified could play a role in facilitating muscle regeneration.
A tissue-regenerative macrophage subset exhibiting a resident macrophage gene signature
Resident and recruited macrophages play distinct roles in immune defense, with resident macrophages providing a constant level of immune surveillance, while recruited macrophages respond to acute infections or injuries. To visualize differential gene expression patterns, we summarized the origin of each monocyte/macrophage subset and examined the known marker genes associated with resident and recruited macrophages29. Resident macrophage signature genes, such as Axl, Cd74, and Cxcl16, were highly expressed in Clusters 2 and 3. Clusters 4 and 5 were characterized by the expression of the recruited macrophage markers Cxcr2, Ifitm1, and Sell. (Fig. S2a and b). However, it is noteworthy that Cluster 2 was conspicuously absent on day 0 (Fig. 1g), suggesting that Cluster 2 cells may not originate from resident macrophages. Our subsequent cell trajectory analysis demonstrated that Clusters 4 and 5 were the major infiltrating macrophage populations and likely contributed to Cluster 2 subset formation (Fig. S3a). Our findings revealed that clusters 1, 4, and 5 consisted of inflammatory macrophages. In contrast, clusters 2 and 3 were tissue-resident macrophages in the inflammatory-to-regenerative transition stage during skeletal muscle regeneration.
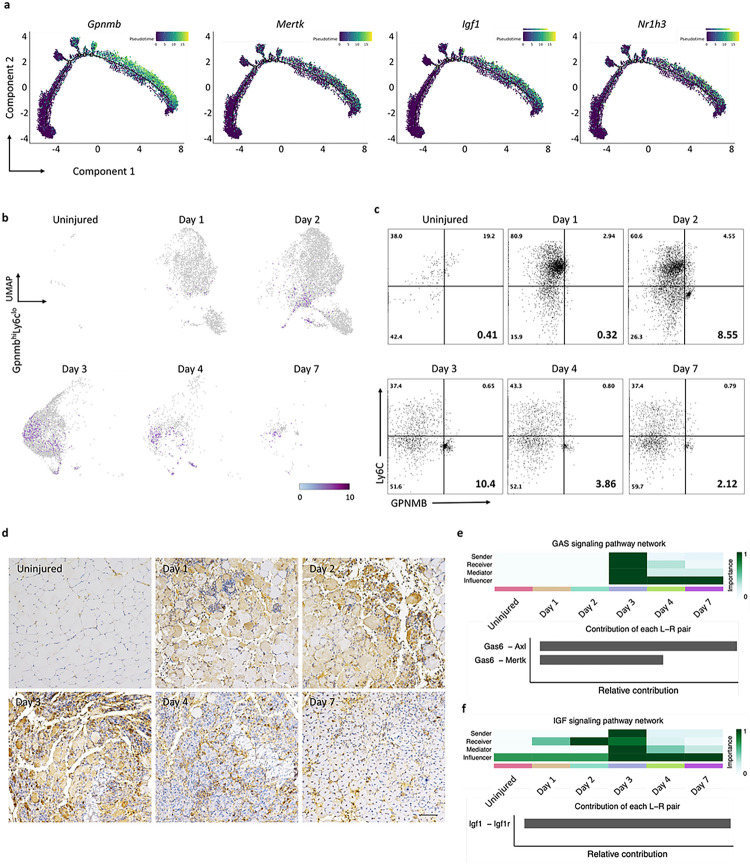
Identification of GPNMB-expressing macrophages as critical effectors in skeletal muscle regeneration
A key analysis in the investigation of the molecular mechanisms underlying changes in the state of macrophages is the identification of differentially expressed genes along the pseudotime trajectory, i.e., that determined by trajectory inference30 from single-cell RNA-sequencing data. This inferred trajectory highlights the key effectors within macrophage subsets that govern the biological processes of regeneration. By integrating the relative trajectory positions of the macrophage clusters with the distribution density of each identified group (Fig. 1h), Cluster 4 cells were identified as mainly present at the beginning of the trajectory; Cluster 3 cells were predominant at both ends of the trajectory, cells in Clusters 1 and 5 were identified at the early and middle positions, and Cluster 2 cells were identified at the end of the pseudotime axis. Notably, the positions of Cluster 3 cells at both ends of the pseudotime axis, together with their high proportions in uninjured muscle (Fig. 1g), suggest that Cluster 3 may represent a subset with steady-state characteristics. To further investigate the biological and functional roles of Cluster 2 macrophages during skeletal muscle regeneration, volcano plots were generated to visualize the DEGs in Cluster 2 cells vs. cells in Clusters 1, 3, 4, and 5. The top 10 up- and downregulated DEGs are labeled in the plots; among these DEGs, the Gpnmb gene was significantly upregulated, specifically in Cluster 2 (Fig. S3b). To further investigate the importance of macrophages with high GPNMB expression in tissue regeneration, we analyzed significantly activated macrophage marker genes31 using a pseudotime approach, focusing on critical factors involved in tissue regeneration and fibrosis. We found that Mertk, Igf1, and Nr1h3 exhibited the same expression pattern as Gpnmb (Fig. 2a); previous studies have highlighted the significance of these genes in tissue regeneration26,32–34. Nuclear receptor subfamily 1 group H member 3 (Nr1h3) is a gene that encodes a transcription factor involved in lipid metabolism and cholesterol homeostasis.
Figure 2. Temporal single-cell sequencing unveils GPNMB+ macrophage signaling as a dominant subset of tissue regeneration.
(a) Trajectory plots tracing the gene expression profiles mirroring the Gpnmb pattern within the monocyte/macrophage subsets suggest synchronous gene expression events that may underpin shared functional pathways in regeneration. (b) UMAP series depicting the dynamic expression of the GpnmbhiLy6clo macrophage subset throughout the regenerative timeline. The UMAPs consecutively illustrate the prevalence and distribution of the GpnmbhiLy6clo population at each time point following skeletal muscle injury, highlighting the shifts in the macrophage landscape. (c) Flow cytometric quantification capturing the temporal prevalence of the GpnmbhiLy6clo population. The analysis delineates the frequency of this subset at progressive intervals post-injury, reflecting its involvement in the regenerative process. (d) Immunohistochemical staining of TA muscle sections across a temporal spectrum, identifying the presence of GPNMB-expressing cells. The staining intensity indicates the cellular localization and temporal expression pattern of GPNMB during the regeneration phases. (e and f) Heatmap analysis summarizing the relative engagement of cell populations in GAS and IGF signaling pathways. Upper panel offers insights into the predominant cellular functions at each time point, while the lower panel details the contribution of specific ligand-receptor pairs to the composite signaling communication network.
In the late stage of tissue regeneration, macrophages adopt an anti-inflammatory phenotype that helps to suppress inflammatory responses and restore normal tissue structure and function. However, a dysregulated response can result in persistent inflammation and maladaptive regeneration, ultimately leading to tissue-destructive fibrosis. Previous studies have indicated that, in a chronic inflammatory environment, the GPNMB secreted by macrophages can stimulate excessive deposition of ECM, ultimately leading to pulmonary fibrosis35. After skeletal muscle injury, macrophages play a key role in clearing apoptotic cells and aiding tissue regeneration, a process that involves the conversion of infiltrating monocytes to macrophages with inflammatory and regenerative phenotypes. Our results revealed time-dependent gene expression changes in Gpnmb and Ly6c, revealing that the GpnmbhiLy6clo macrophage population was predominantly enriched in Cluster 2 on day 3 (Fig. 2b). These findings highlight the importance of identifying specific GPNMB-expressing macrophage subsets during skeletal muscle regeneration. Based on the temporal dynamics of GPNMB expression and previous descriptions of tissue-resident macrophages36,37, we named this cell subset GPNMBhiLy6Clo “regenerative macrophages”. To validate the findings from single-cell RNA-seq analysis, we employed flow cytometry to assess the abundance of the GPNMBhiLy6Clo subset in the CD45+CD11b+ cell population in murine muscle postinjury and observed a peak on day 3, followed by a decrease to approximately 10.4%. Furthermore, our histological staining of tissue sections from various time points revealed cells with prominent GPNMB staining on day 3 (Fig. 2c). These findings suggest that macrophages with high GPNMB expression exhibit characteristics reminiscent of M2 macrophages. To validate the findings from single-cell RNA-seq analysis, we employed flow cytometry to identify the GPNMBhiLy6Clo subset in the CD45+CD11b+ cell population in murine muscle postinjury and observed a peak in the proportion on day 3, followed by a decrease to approximately 10.4%. Furthermore, our histological staining of tissue sections at various time points revealed prominent GPNMB-positive cells on day 3 (Fig. 2d). These findings suggest that macrophages with high GPNMB expression exhibit characteristics reminiscent of M2 macrophages.
CellChat identifies communication patterns and predicts the functions of macrophage subsets involved in skeletal muscle regeneration
Since a direct comparison of DEGs might not comprehensively capture the intricate signaling network, we conducted a thorough investigation of macrophage cellular communication dynamics. We performed CellChat24 analysis at distinct time points and revealed regulatory cell–cell interactions. On day 3, we observed increased levels of tissue regeneration-related signaling factors, including IGF12,38, GAS39,40, GDF14, and nicotinamide phosphoribosyltransferase (NAMPT)7. On day 3, macrophages tended to send signals of IGF and GDF and receive signals of IGF, GAS, and GDF (Fig. S4a). Inflammatory signals, such as IL-1, IL-2, and TNF in macrophages, were abundant on days 1 and 2 (Fig. S4b). In addition to the signaling pathway network as a time-resolved signature, we also predicted the putative interactions among ligand and receptor pairs (Fig. 2e and f). On day 3, three critical skeletal muscle regeneration signaling pathways, GAS6/AXL, GAS6/MERTK, and IGF1/IGF1R, were highly enriched. IGF1/IGF1R has been demonstrated to promote skeletal muscle regeneration12,38. The TYRO3, AXL, and MERTK (TAM) receptor tyrosine kinases and their cognate glycoprotein ligands growth arrest-specific 6 (GAS6) and protein S (PROS1) are critical regulators of tissue homeostasis and inflammation41. Our results are consistent with the concept that TAM receptors are activated in macrophages in response to tissue injury42. The heightened activity of these three critical pathways confirms their roles in muscle regeneration and highlights their coordinated contribution to regenerative mechanisms.
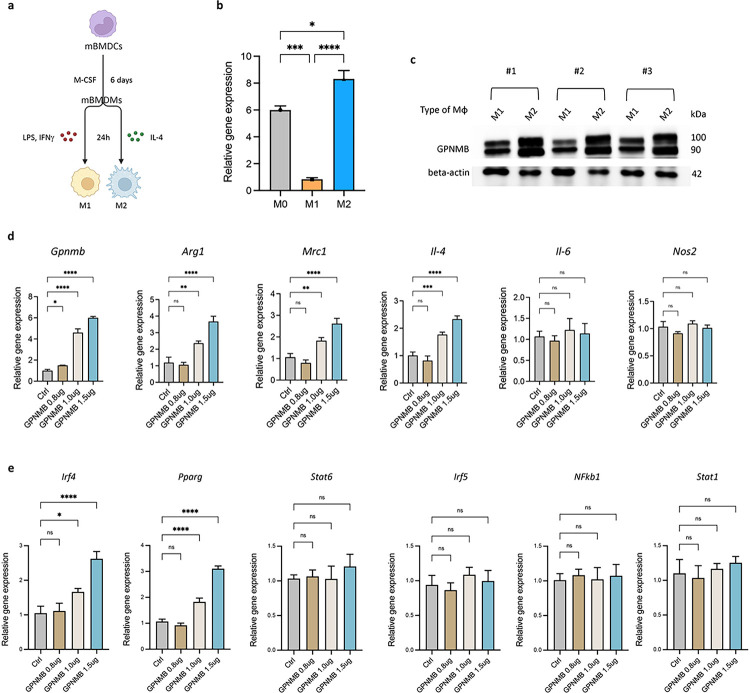
GPNMB promotes M2 macrophage polarization via the upregulation of specific transcription factors
To validate this hypothesis, we isolated murine bone marrow-derived cells (BMDCs) and induced their differentiation into M1 and M2 macrophages in vitro (Fig. 3a). mRNA and protein expression analyses revealed a significant increase in GPNMB expression in M2 macrophages (Fig. 3b and c). These results indicate that GPNMB is a marker of M2 macrophages involved in muscle tissue regeneration and led us to hypothesize that the overexpression of GPNMB promotes M2 macrophage polarization. We conducted GPNMB overexpression experiments to verify this hypothesis in murine bone marrow-derived macrophages (mBMDMs). Our findings demonstrated that ectopic GPNMB expression increased the expression of M2 macrophage markers without affecting the expression of M1 macrophage markers (Fig. 3d). The overexpression of GPNMB was found to activate key transcription factors linked to M2 macrophage polarization, such as Irf4 and Pparg. In contrast, the expression of the critical regulators Irf5, Nfkb1, and Stat1 in M1 macrophages was unaffected by ectopic GPNMB expression (Fig. 3e), indicating that GPNMB may serve as part of the M2 gene expression program in macrophages.
Figure 3. Ectopic GPNMB enhances M2 macrophage polarization by modulating key regulatory genes.
(a) Experimental scheme for differentiating murine bone marrow-derived cells (mBMDCs) into M1 and M2 macrophages, followed by LPS, IFNγ, and IL-4 treatment. (b) Quantitative PCR analysis shows significantly higher GPNMB expression in M2 polarized macrophages than in M0 and M1. (c) Western blot confirming the increased protein levels of GPNMB in M2 macrophages across three independent experiments. (d)Ectopic expression of GPNMB in mBMDMs leads to the upregulation of M2-associated markers Arg1, Mrc1, and IL-4, with no significant effect on the M1 markers IL-6 and Nos2. (e)Overexpression of GPNMB results in heightened expression of M2-related transcription factors Irf4 and Pparg, suggesting a potential pathway for GPNMB-mediated macrophage polarization.
GPNMB knockout impairs skeletal muscle regeneration
To investigate the role of GPNMB in muscle regeneration, we generated GPNMB-knockout mice and subjected them to CTX-induced muscle injury. The temporal evolution of muscle regeneration was monitored and compared with that of wild-type (WT) C57BL/6 controls (Fig. 4a). Western blot analysis of muscle tissue extracts confirmed the absence of the GPNMB protein in the KO group, confirming that the observed phenotypic differences were attributable to GPNMB deficiency (Fig. 4b). The gross morphological analysis of the TA muscles from the GPNMB-KO mice revealed marked impairment in muscle regeneration at days 4 and 7 postinjury (Fig. 4c). Compared with those from the WT mice, the injured muscles from the GPNMB-KO mice were visibly less striated. Histological evaluations conducted through hematoxylin and eosin (H&E) staining provided further insights into the compromised regenerative response in GPNMB-KO mice. Without GPNMB, the injured muscles exhibited exacerbated inflammatory responses and a notable delay in myofiber regeneration (Fig. 4d). The injured sites in the GPNMB-KO mice were characterized by increased cellular infiltration and a lack of newly formed myofibers. This phenotype starkly contrasted with the organized regenerative patterns observed in WT controls. Quantitative analyses were performed to measure the cross-sectional area (CSA) of muscle fibers, a key indicator of regenerative progress. On day 4 postinjury, the mean CSA of regenerating myofibers in GPNMB-KO mice was significantly reduced, indicating a failure to initiate the regenerative process properly. This defect persisted through day 7, with KO mice displaying markedly smaller myofibers than WT mice (Fig. 4e). The statistical significance of these differences was confirmed, underscoring the necessity of GPNMB for efficient muscle regeneration. Our findings unveil a previously unappreciated role for GPNMB in facilitating muscle tissue repair, suggesting that GPNMB may act as a modulator of the cellular and molecular events that orchestrate the complex process of muscle regeneration following acute injury.
Figure 4. Impaired muscle regeneration in GPNMB-knockout mice post-CTX injury.
(a)Schematic of the experimental design for assessing muscle regeneration in GPNMB-KO and C57BL/6 control mice following CTX injection. (b and c)Representative images of tibialis anterior muscles from GPNMB-KO and WT mice at uninjured, day 4, and day 7 post-injury, demonstrating differences in muscle morphology. (d) Hematoxylin and eosin staining of TA muscle sections revealed histological changes during regeneration, with GPNMB-KO mice showing reduced tissue repair compared to controls. (e) Quantitative analysis of cross-sectional area of muscle fibers in uninjured, day 4, and day 7 post-injury muscle sections confirmied statistically significant impairment of regeneration in GPNMB-KO mice.
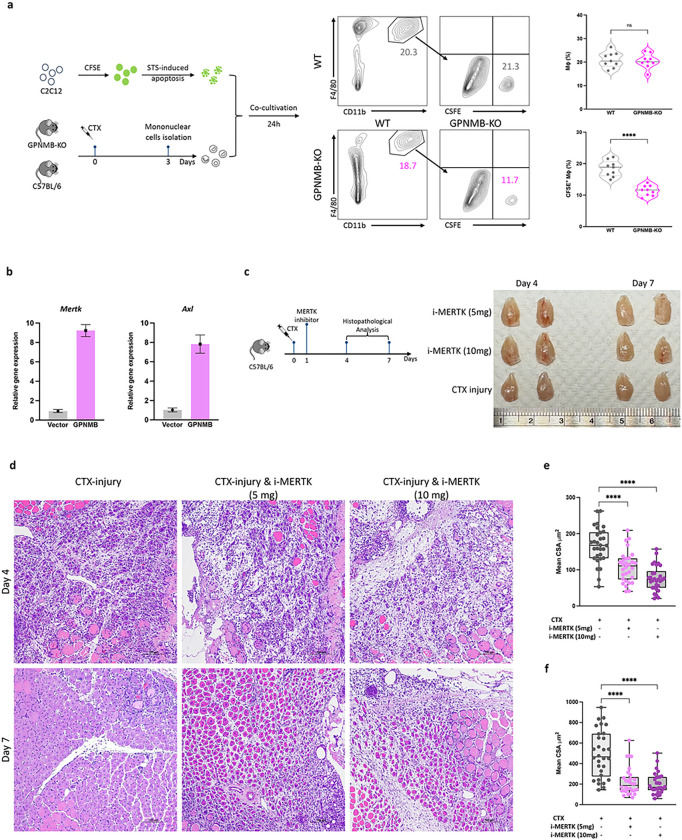
Impaired macrophage efferocytosis and muscle regeneration following GPNMB knockout and MERTK inhibition
GPNMB overexpression in primary murine macrophages led to the upregulation of the expression of efferocytosis-related genes, including Mertk and Axl, suggesting that GPNMB plays a regulatory role in the genetic orchestration of the efferocytosis process (Fig. 5a). We further investigated the functional role of GPNMB in macrophage-mediated efferocytosis. GPNMB-deficient macrophages exhibit a marked reduction in the phagocytosis of apoptotic cells. Fluorescence microscopy and flow cytometry analyses revealed that compared with their wild-type counterparts, mBMDMs from GPNMB-KO mice exhibited significantly decreased uptake of CFSE-labeled apoptotic C2C12 myoblasts, underscoring the importance of GPNMB in the clearance of apoptotic cells (Fig. 5b). To understand the broader implications of GPNMB deficiency for muscle regeneration, we further explored the impact of disruption of efferocytosis on muscle regeneration by employing a pharmacological approach to inhibit MERTK. The administration of a MERTK inhibitor resulted in significant deficits in muscle tissue architecture and repair, as evidenced by histopathological evaluations (Fig. 5c–f). Notably, administering the inhibitor led to a dose-dependent exacerbation of muscle repair impairment, particularly at higher dosages (Fig. 5c). Histological analysis of muscle regeneration revealed that MERTK inhibition, particularly at a higher dosage, severely compromised the muscle repair process on days 4 and 7 postinjury. These morphological defects were confirmed by measuring muscle fiber CSA and length (Fig. 5d–f). These results underscore the importance of the GPNMB-MERTK axis in muscle regeneration and highlight a potential therapeutic target for promoting tissue repair following injury.
Figure 5. Diminished macrophage efferocytosis and impaired muscle regeneration following GPNMB-knockout and MERTK inhibition.
(a) This panel illustrates the experimental setup and subsequent flow cytometry analysis for evaluating macrophage efferocytosis. On day 3 post-CTX-induced muscle injury, mononuclear cells were isolated from both WT and GPNMB-KO mice and co-cultured with CFSE-labeled, staurosporine (STS)-induced apoptotic C2C12 myoblasts for 24 hours. Flow cytometry was then employed to assess the phagocytosis of apoptotic cells by CD11b+F4/80+ macrophages. The rightmost graph in Panel A provides a quantitative comparison between the WT and GPNMB-KO groups, showing a significant decrease in efferocytosis efficiency in the GPNMB-KO macrophages, as reflected by their reduced uptake of CFSE-labeled apoptotic bodies. (b) Quantitative PCR analysis reveals that overexpression of GPNMB in primary macrophages significantly increases the mRNA levels of key efferocytosis genes, Mertk and Axl. (c) Left panel, schematic of the experimental design depicting the treatment of C57BL/6 mice with a MERTK inhibitor post-CTX injury to evaluate its effect on muscle regeneration. Right panel, gross morphology of TA muscles from mice treated with MERTK inhibitor doses shows dose-dependent effects on muscle appearance. (d) Histological examination of muscle regeneration by H&E staining at days 4 and 7 post-CTX injury with or without MERTK inhibitor treatment, highlighting the impact of MERTK signaling on tissue repair. (e and f) Statistical analysis of muscle fiber CSA and length at days 4 and 7 post-injury, with MERTK inhibition leading to a marked reduction in both parameters, signifying compromised regenerative capacity.
GPNMB stimulation promotes muscle regeneration and the myogenic differentiation of murine myoblasts
Previous research has indicated that the GPNMB expressed on macrophages undergoes enzymatic processing by disintegrin and metalloproteinase domain-containing protein 10 (ADAM10)43 to generate soluble GPNMB. Soluble GPNMB has critical functions; for example, it interacts with CD44 to promote cancer cell stemness and metastasis44. Via a similar pathway, soluble GPNMB promotes mesenchymal stromal cell survival, proliferation, and migration45. Moreover, the binding of soluble GPNMB to syndecan-4 impedes the extravasation of activated T cells into inflamed skin46. To investigate the potential of GPNMB to promote myogenic differentiation of myoblasts, we performed myotube differentiation assays using C2C12 cells with or without the addition of recombinant GPNMB (rGPNMB). C2C12 cells treated with or without rGPNMB treatment were collected at several time points during the differentiation process, including 0 (before differentiation), 12, 24, and 72 hours. The expression of Myod and Myog gradually increased during myoblast differentiation, and the addition of rGPNMB significantly increased their expression. However, rGPNMB only temporarily elevated the expression of the early differentiation marker Myf2a at 12 hours and did not affect the expression of the myoblast proliferation marker Myf5 at any time point (Fig. 6a). Immunofluorescence staining revealed that treatment with rGPNMB resulted in increased MyHC expression (Fig. 6b) and the formation of larger myotubes (Fig. 6c) containing a greater number of nuclei (Fig. 6d) in C2C12 cells than in the rGPNMB withdrawal group. Furthermore, our in vitro data indicate that rGPNMB facilitates myoblast differentiation. In vivo, we examined the role of exogenous GPNMB in facilitating skeletal muscle regeneration by administering 10 or 20 μg of rGPNMB to injured skeletal muscle. The results showed that the delivery of rGPNMB restored muscle architecture at the injury site (Fig. 6e). Specifically, on day 4, compared to injury alone, a single dose of rGPNMB led to a significant increase in the CSA of the TA muscle (225 ± 110.2 vs. 128 ± 43.2 μm2, p = 0.019, in the 10 μg group; 408 ± 139.5 vs. 128 ± 43.2 μm2, p < 0.0001, in the 20 μg group) Fig. 6f. Furthermore, on day 7, the effect of rGPNMB was sustained, as shown by the marked increase in the CSA of the TA muscle (728 ± 246.6 vs. 471 ± 195.3 μm2, p = 0.0013 in the 10 μg group; 1051 ± 340.9 vs. 471 ± 195.3 μm2, p < 0.0001 in the 20 μg group) Fig. 6g.
Figure 6. GPNMB stimulation promotes muscle regeneration and myogenic differentiation of murine myoblasts.
(a) Following GPNMB overexpression, quantitative real-time PCR was utilized to monitor the temporal expression of key myogenic regulatory factors in C2C12 cells, including Myf5, Myf2a, Myod, and Myog. (b)Immunofluorescent staining for MyHC of C2C12 myoblast cultured in differentiation medium with (100 ng/mL or 200 ng/mL) or without rGPNMB. C2C12 myoblasts were induced to differentiate for three days; (c) fusion indices were calculated by expressing the number of nuclei within MyHC-positive myotubes with ≥2 nuclei as a percentage of the total nuclei, and (d) the myotube width was measured at 3 different points on the cell. The average width per myotube was calculated. Data are presented as mean±s.d. of three independent experiments. (e)H&E staining of injured mouse TA muscle on days 4 and 7 with (10 μg or 20 μg) or without rGPNMB. Scale bar: 100 μm. (f) and (g)Cross-sectional area of myofibers from injured only and treated with rGPNMB (10 μg and 20 μg) groups on days 4 and 7. Data are presented as mean±s.d. (n=3) of each time point.
DISCUSSION
Skeletal muscle regeneration is a complex process orchestrated by various types of cells, including muscle stem cells, FAPs, and immune cells1. The contributions of macrophages to muscle regeneration promotion have been recognized for many years9. Recent studies have demonstrated that macrophage-derived cells such as IGF113, GDF1515, and NAMPT7 are effectors of skeletal muscle regeneration. In this study, we provide the first temporal single-cell transcriptional characterization of macrophage subsets during skeletal muscle regeneration and highlight the heterogeneity of the macrophage population and its importance in the dynamics of muscle regeneration. We identified five macrophage clusters that differed in gene expression signatures and temporal dynamics during muscle regeneration. In particular, we identified a subset of macrophages characterized by elevated expression of GPNMB, IGF1, GDF15, and NAMPT. Furthermore, nutrient and oxygen availability, danger signals, antigens, or instructional signals from other cells trigger changes in key metabolic regulatory events in immune cells. Previous studies have linked macrophage activation status to metabolic remodeling47, such as the enhancement of FAO and OXPHOS in M2 macrophages, which are crucial for M2 activation48. We found that Cluster 1 macrophages exhibited significantly increased expression of M2 macrophage genes, including those involved in FAO, oxidative phosphorylation, and the TCA cycle. These results suggest that high GPNMB expression in Cluster 1 macrophages plays a role in facilitating metabolic reprogramming to support M2 activation.
GPNMB has recently been reported to regulate macrophage inflammatory responses by inhibiting NF-κB signaling through its interaction with CD4420. However, the function of GPNMB varies among different tissue cells. For instance, liver-derived GPNMB binds to the CD44 receptor on white adipose tissue, leading to an increase in lipogenesis via the CD44-PI3K-mTORC pathway and resulting in obesity and insulin resistance49. Furthermore, the soluble form of GPNMB has been demonstrated to promote the recruitment of mesenchymal stromal cells, thereby promoting cutaneous wound healing18,50. Additionally, growth factors such as IGF1 can promote skeletal muscle regeneration, and NAMPT can activate muscle stem cells through C-C motif chemokine receptor type 5. Here, we report a previously unrecognized subset of macrophages that contributes to muscle regeneration. Importantly, our CellChat results provided insights into the autocrine/paracrine mechanisms involving IGF1, GAS, GDF, and NAMPT signaling interactions among macrophages at different stages of muscle regeneration.
Macrophages secrete factors that facilitate tissue regeneration by promoting the proliferation, differentiation, and activation of various cell types, including stem and precursor cells. These cells adopt an anti-inflammatory phenotype during the later stages of tissue regeneration to suppress inflammatory responses and restore typical tissue structure. Dysregulation of this process can lead to persistent inflammation and maladaptive regeneration processes, ultimately resulting in tissue-destructive fibrosis31. Our RNA velocity analysis revealed the temporal dynamics of macrophages and identified Gpnmb, Mertk, Igf1, and Nr1h3 as pivotal indicators during skeletal muscle regeneration. These findings highlight the importance of GPNMB in this regenerative process. In response to efferocytosis, MERTK is activated by the intracellular modification of membrane cholesterol, which yields steroid metabolites that activate Nr1h3, which binds directly to the MERTK promoter to promote transcription51. Previous studies have shown that GAS6 can bind to phosphatidylserine (PtdSer), which is externalized on apoptotic cell membranes52, and activate MERTK on macrophages6; this provides positive feedback to further increase MERTK expression and ultimately shift macrophage polarization toward the M2 phenotype. Our results showed that the day 3 cell populations and Cluster 1 subset have the characteristics of both receivers and senders of signals in the GAS6 signaling pathway. Discrepancies in the expression patterns of proinflammatory and anti-inflammatory markers, as opposed to those of established genes, suggest the complexity of macrophage activation and the influence of environmental factors, warranting further research. Importantly, we identified a specific subset of high-GPNMB-expressing macrophages, termed GPNMBhiLy6Clo regenerative macrophages, characterized by their time-dependent gene expression patterns and macrophage surface markers. Immunohistochemical staining revealed a high level of accumulation of these GPNMBhiLy6Clo macrophages in the injured skeletal muscle area,supporting their involvement in tissue regeneration. In vitro examination of the expression of GPNMB in murine M1 and M2 macrophages revealed that GPNMB was significantly upregulated in M2 macrophages compared with M1 macrophages, suggesting that GPNMB plays a role in M2 macrophage polarization. A gain-of-function assay was conducted to further validate that GPNMB overexpression promotes M2 polarization, indicating that GPNMB may serve as a macrophage M2 marker. In summary, our study revealed the importance of GPNMB-expressing macrophages, along with the genes Mertk, Igf1, and Nr1h3, in tissue regeneration. Our study also revealed the significance of GPNMB-expressing macrophages and associated genes in tissue regeneration by revealing the gene expression timeline of regenerative macrophage subsets in injured muscle.
Muscle regeneration was indicated by significant increases in the CSA and multinuclear myofiber count in the TA muscle following the injection of rGPNMB. These results demonstrate the potential therapeutic role of GPNMB in promoting skeletal muscle regeneration. However, GPNMB may regulate multiple cell types involved in skeletal muscle regeneration in addition to infiltrating macrophages; these other cell types include FAPs and MuSCs. Further research is needed to elucidate the specific interactions and contributions of GPNMBhiLy6Clo/regenerative macrophages and other cell types to the overall process of skeletal muscle regeneration. The findings presented in this single-cell study revealed the dynamics of macrophage subpopulation evolution during skeletal muscle regeneration and revealed the critical role of GPNMBhiLy6Clo regenerative macrophages in this process. Our analyses suggested that these macrophages secrete soluble GPNMB into the microenvironment to promote the proliferation, differentiation, and maturation of MuSCs or myogenic progenitors. This research highlights the potential of GPNMB as a therapeutic target for promoting skeletal muscle regeneration and suggests a possible mechanism through which GPNMB exerts its effects.
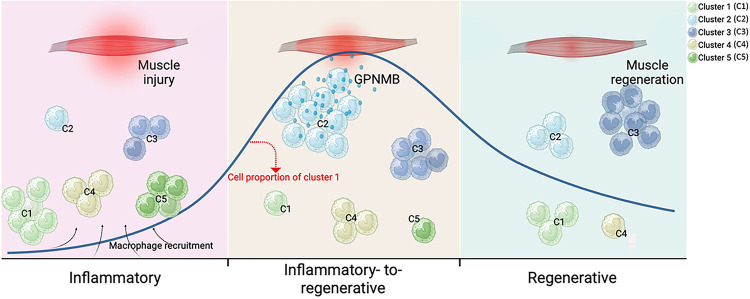
Figure 7. GPNMB-expressing macrophage contributes to skeletal muscle regeneration.
The dynamic response of skeletal muscle to injury can be broadly categorized into three primary stages: the inflammatory, the inflammatory-to-regenerative, and the regenerative stage. Following muscle injury, muscle tissues recruit monocyte-derived macrophages, categorized into five distinct clusters (C1, 2, 3, 4, and 5) based on their inflammatory profiles. Our study identifies that macrophages with high GPNMB expression during the transitional phase from inflammation to regeneration are crucial in activating and expanding muscle progenitor cells. This process aids in the transition of macrophages towards an anti-inflammatory phenotype, which is critical for the resolution of inflammation and the subsequent muscle repair and regeneration. The dynamic shifts in macrophage subsets, highlighted by changes in the proportions of Cluster 2, underscore the importance of GPNMB as an effector in muscle regeneration. This figure was generated using Biorender.com.
ACKNOWLEDGMENTS
We acknowledge the financial support from the China Medical University Hospital and the School of Medicine, National Yang Ming Chiao Tung University. This publication includes data generated at the UC San Diego IGM Genomics Center utilizing an Illumina NovaSeq 6000 purchased with funding from a National Institutes of Health SIG grant (#S10 OD026929). We gratefully acknowledge the technical expertise of Chih-Sin Hsu for data analysis and appreciate the contributions of Wan-Chun Chang and Bingxiu Guo in the construction of the 10x single-cell transcriptome 3’ gene expression library, which was provided by the Genomics Center for Clinical and Biotechnological Applications of the Cancer Progression Research Center at National Yang Ming Chiao Tung University, and the National Core Facility for Biopharmaceuticals of the National Science and Technology Council. The authors would like to thank Fu-Mei Hsieh at BIOTOOLS Co., Ltd in Taiwan for kindly supporting the analysis of single-cell RNA-seq data. This work was supported by the National Science and Technology Council, Taiwan (NSTC 112-2314-B-039-024, NSTC 111-2314-B-039-083) and China Medical University Hospital (C1110812016-7, DMR-112-142, DMR-112-147, DMR-111-191, EXO-113-004, EXO-113-005). This work was supported in part by National Institutes of Health grants R01HL108735, R01HL106579, and R01HL121365 (to S.C).
Footnotes
Declarations
CONFLICT OF INTEREST
The authors declare no competing interests.
References
- 1.Giordani L. et al. High-dimensional single-cell cartography reveals novel skeletal muscle-resident cell populations. Mol. Cell 74, 609–621.e6 (2019). [DOI] [PubMed] [Google Scholar]
- 2.Wosczyna M. N. & Rando T. A. A muscle stem cell support group: coordinated cellular responses in muscle regeneration. Dev. Cell 46, 135–143 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X. et al. Prolonged hypernutrition impairs TREM2-dependent efferocytosis to license chronic liver inflammation and NASH development. Immunity 56, 58–77.e11 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fidler T. P. et al. The AIM2 inflammasome exacerbates atherosclerosis in clonal haematopoiesis. Nature 592, 296–301 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shang M. et al. Macrophage-derived glutamine boosts satellite cells and muscle regeneration. Nature 587, 626–631 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sapudom J. et al. 3D in vitro M2 macrophage model to mimic modulation of tissue repair. NPJ Regen. Med. 6, 83 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ratnayake D. et al. Macrophages provide a transient muscle stem cell niche via NAMPT secretion. Nature 591, 281–287 (2021). [DOI] [PubMed] [Google Scholar]
- 8.Tidball J. G. & Villalta S. A. Regulatory interactions between muscle and the immune system during muscle regeneration. Am. J. Physiol. Regul. Integr. Comp. Physiol. 298, R1173–R1187 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnold L. et al. Inflammatory monocytes recruited after skeletal muscle injury switch into antiinflammatory macrophages to support myogenesis. J. Exp. Med. 204, 1057–1069 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang X. et al. Heterogeneous origins and functions of mouse skeletal muscle-resident macrophages. Proc. Natl. Acad. Sci. U. S. A. 117, 20729–20740 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sicklinger F. et al. Basophils balance healing after myocardial infarction via IL-4/IL-13. J. Clin. Invest. 131, e136778 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tonkin J. et al. Monocyte/macrophage-derived IGF-1 orchestrates murine skeletal muscle regeneration and modulates autocrine polarization. Mol. Ther. 23, 1189–1200 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varga T. et al. Macrophage PPARgamma, a lipid activated transcription factor controls the growth factor GDF3 and skeletal muscle regeneration. Immunity 45, 1038–1051 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patsalos A. et al. A growth factor-expressing macrophage subpopulation orchestrates regenerative inflammation via GDF-15. J. Exp. Med. 219, e20210420 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stepien D. M. et al. Tuning macrophage phenotype to mitigate skeletal muscle fibrosis. J. Immunol. 204, 2203–2215 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weterman M. A. et al. nmb, a novel gene, is expressed in low-metastatic human melanoma cell lines and xenografts. Int. J. Cancer 60, 73–81 (1995). [DOI] [PubMed] [Google Scholar]
- 17.Shikano S., Bonkobara M., Zukas P. K. & Ariizumi K. Molecular cloning of a dendritic cell-associated transmembrane protein, DC-HIL, that promotes RGD-dependent adhesion of endothelial cells through recognition of heparan sulfate proteoglycans. J. Biol. Chem. 276, 8125–8134 (2001). [DOI] [PubMed] [Google Scholar]
- 18.Sondag G. R. et al. Osteoactivin inhibition of osteoclastogenesis is mediated through CD44-ERK signaling. Exp. Mol. Med. 48, e257 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Voet S., Prinz M. & van Loo G. Microglia in central nervous system inflammation and multiple sclerosis pathology. Trends Mol. Med. 25, 112–123 (2019). [DOI] [PubMed] [Google Scholar]
- 20.Prabata A., Ikeda K., Rahardini E. P., Hirata K. I. & Emoto N. GPNMB plays a protective role against obesity-related metabolic disorders by reducing macrophage inflammatory capacity. J. Biol. Chem. 297, 101232 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toda G., Yamauchi T., Kadowaki T. & Ueki K. Preparation and culture of bone marrow-derived macrophages from mice for functional analysis. STAR Protoc. 2, 100246 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoshiko Y., Hirao K. & Maeda N. Differentiation in C(2)C(12) myoblasts depends on the expression of endogenous IGFs and not serum depletion. Am. J. Physiol. Cell Physiol. 283, C1278–C1286 (2002). [DOI] [PubMed] [Google Scholar]
- 23.Yamazaki A. et al. Preparation of single cell suspensions enriched in mouse brain vascular cells for single-cell RNA sequencing. STAR Protoc. 2, 100715 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jin S. et al. Inference and analysis of cell-cell communication using CellChat. Nat. Commun. 12, 1088 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Markworth J. F. et al. Resolvin D1 supports skeletal myofiber regeneration via actions on myeloid and muscle stem cells. JCI Insight 5, e137713 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang J. et al. Bone marrow-derived IGF-1 orchestrates maintenance and regeneration of the adult skeleton. Proc. Natl. Acad. Sci. U. S. A. 120, e2203779120 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coelho I., Duarte N., Barros A., Macedo M. P. & Penha-Goncalves C. Trem-2 promotes emergence of restorative macrophages and endothelial cells during recovery from hepatic tissue damage. Front. Immunol. 11, 616044 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaitin D. A. et al. Lipid-associated macrophages control metabolic homeostasis in a Trem2-dependent manner. Cell 178, 686–698.e14 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen J. et al. Single-cell RNA sequencing identified novel Nr4a1(+) Ear2(+) anti-inflammatory macrophage phenotype under myeloid-TLR4 dependent regulation in anti-Glomerular Basement Membrane (GBM) Crescentic Glomerulonephritis (cGN). Adv. Sci. (Weinh.) 9, e2200668 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trapnell C. et al. The dynamics and regulators of cell fate decisions are revealed by pseudotemporal ordering of single cells. Nat. Biotechnol. 32, 381–386 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wynn T. A. & Vannella K. M. Macrophages in tissue repair, regeneration, and fibrosis. Immunity 44, 450–462 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Runyan C. E. et al. Impaired phagocytic function in CX3CR1(+) tissue-resident skeletal muscle macrophages prevents muscle recovery after influenza A virus-induced pneumonia in old mice. Aging Cell 19, e13180 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schiaffino S. & Mammucari C. Regulation of skeletal muscle growth by the IGF1-Akt/PKB pathway: insights from genetic models. Skelet. Muscle 1, 4 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Snodgrass R. G. et al. Efferocytosis potentiates the expression of arachidonate 15-lipoxygenase (ALOX15) in alternatively activated human macrophages through LXR activation. Cell Death Differ. 28, 1301–1316 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang J. et al. Macrophage-derived GPNMB trapped by fibrotic extracellular matrix promotes pulmonary fibrosis. Commun. Biol. 6, 136 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nickl B., Qadri F. & Bader M. Anti-inflammatory role of Gpnmb in adipose tissue of mice. Sci. Rep. 11, 19614 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silva W. N. et al. Macrophage-derived GPNMB accelerates skin healing. Exp. Dermatol. 27, 630–635 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sakai H. et al. Exogenous insulin-like growth factor 1 attenuates cisplatin-induced muscle atrophy in mice. J. Cachexia Sarcopenia Muscle 12, 1570–1581 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Zaeed N., Budai Z., Szondy Z. & Sarang Z. TAM kinase signaling is indispensable for proper skeletal muscle regeneration in mice. Cell Death Dis. 12, 611 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shirakawa K. et al. MerTK expression and ERK activation are essential for the functional maturation of osteopontin-producing reparative macrophages after myocardial infarction. J. Am. Heart Assoc. 9, e017071 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rothlin C. V., Carrera-Silva E. A., Bosurgi L. & Ghosh S. TAM receptor signaling in immune homeostasis. Annu. Rev. Immunol. 33, 355–391 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeBerge M. et al. Macrophage AXL receptor tyrosine kinase inflames the heart after reperfused myocardial infarction. J. Clin. Invest. 131, e139576 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rose A. A. et al. ADAM10 releases a soluble form of the GPNMB/Osteoactivin extracellular domain with angiogenic properties. PLoS One 5, e12093 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liguori M. et al. The soluble glycoprotein NMB (GPNMB) produced by macrophages induces cancer stemness and metastasis via CD44 and IL-33. Cell. Mol. Immunol. 18, 711–722 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu B., Sondag G. R., Malcuit C., Kim M. H. & Safadi F. F. Macrophage-associated osteoactivin/GPNMB mediates mesenchymal stem cell survival, proliferation, and migration via a CD44-dependent mechanism. J. Cell. Biochem. 117, 1511–1121 (2016). [DOI] [PubMed] [Google Scholar]
- 46.Ramani V., Chung J. S., Ariizumi K. & Cruz P. D. Jr. Soluble DC-HIL/Gpnmb modulates T-lymphocyte extravasation to inflamed skin. J. Invest. Dermatol. 142, 1372–1380.e5 (2022). [DOI] [PubMed] [Google Scholar]
- 47.O’Neill L. A. & Pearce E. J. Immunometabolism governs dendritic cell and macrophage function. J. Exp. Med. 213, 15–23 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Odegaard J. I. & Chawla A. Alternative macrophage activation and metabolism. Annu. Rev. Pathol. 6, 275–297 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gong X. M. et al. Gpnmb secreted from liver promotes lipogenesis in white adipose tissue and aggravates obesity and insulin resistance. Nat. Metab. 1, 570–583 (2019). [DOI] [PubMed] [Google Scholar]
- 50.Yu B., Alboslemy T., Safadi F. & Kim M. H. Glycoprotein nonmelanoma clone B regulates the crosstalk between macrophages and mesenchymal stem cells toward wound repair. J. Invest. Dermatol. 138, 219–227 (2018). [DOI] [PubMed] [Google Scholar]
- 51.A-Gonzalez N. et al. Apoptotic cells promote their own clearance and immune tolerance through activation of the nuclear receptor LXR. Immunity 31, 245–258 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bosurgi L. et al. Macrophage function in tissue repair and remodeling requires IL-4 or IL-13 with apoptotic cells. Science 356, 1072–1076 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]