1. CASE 1
A 12‐year‐old heathy boy presented to the emergency department (ED) for evaluation of chest pain after a flexion injury. Earlier that day, the patient participated in a wrestling match and reported sudden onset of chest pain after lifting and throwing an opponent to the mat. Point‐of‐care ultrasound (POCUS) was performed while awaiting x‐ray imaging. The transverse view did not reveal any abnormalities of the sternum. A longitudinal panoramic view of the sternum showed a discontinuity in the hyperechoic anterior cortex demonstrating a fracture (Figure 1).
FIGURE 1.
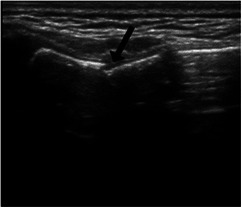
Point‐of‐care ultrasound (POCUS) image demonstrating anterior sternal cortical disruption (black arrow).
2. CASE 2
An 11‐year‐old healthy girl was presented to the ED for evaluation of sternal pain after a fall during gymnastics competition. She landed on her shoulders while attempting a back‐tuck maneuver (back‐flip), resulting in a hyperflexion injury to the anterior chest. POCUS was performed while awaiting x‐ray imaging. A longitudinal panoramic ultrasound view of the sternum revealed a widening of the sternomanubrial joint (Figure 2).
FIGURE 2.

Point‐of‐care ultrasound (POCUS) image demonstrating the diastasis of the sternomanubrial joint (black arrow).
3. DIAGNOSIS: PEDIATRIC STERNAL FRACTURES
Pediatric sternal fractures are relatively uncommon and poorly characterized. Review of the literature suggests that these injuries occur predominantly in the context of blunt traumatic forces, as might be experienced during a motor vehicle accident (MVA). 1 , 2 A growing body of evidence shows pediatric sternal fractures arising from low‐energy mechanisms of injury occur more often than generally recognized. 3 , 4 The standard anterior posterior chest radiograph obtained during trauma series imaging is often not sufficient to detect sternal fractures. A sternal fracture is diagnosed if a discontinuity or step in the linear sternal cortex is demonstrated. Evidence suggests POCUS has superior sensitivity and specificity compared to conventional radiography for diagnoses of minimally displaced sternal fractures. 5 , 6 Ultrasound avoids ionizing radiation and should be considered in cases where concern for a concomitant large vessel or internal organ injury is low.
Homme L, Homme K, Leng T. Two adolescents with chest pain after low‐energy mechanisms. JACEP Open. 2024;5:e13160. 10.1002/emp2.13160
REFERENCES
- 1. Rosenfeld EH, Lau P, Shah SR, et al. Sternal fractures in children: an analysis of the National Trauma Data Bank. J Pediatr Surg. 2019;54(5):980‐983. doi: 10.1016/j.jpedsurg.2019.01.031 [DOI] [PubMed] [Google Scholar]
- 2. Chalphin AV, Mooney DP. Pediatric sternal fractures: a single center retrospective review. J Pediatr Surg. 2020;55(7):1224‐1227. doi: 10.1016/j.jpedsurg.2019.10.002 [DOI] [PubMed] [Google Scholar]
- 3. Ferguson LP, Wilkinson AG, Beattie TF. Fracture of the sternum in children. Emerg Med J. 2003;20(6):518‐520. doi: 10.1136/emj.20.6.518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fukuhara S, Sameshima T, Matsuo H, et al. Sternal fracture complicated by a subcutaneous abscess in a 5‐year‐old boy and diagnosed using point‐of‐care ultrasound. J Emerg Med. 2019;56(5):536‐539. doi: 10.1016/j.jemermed.2018.12.040 [DOI] [PubMed] [Google Scholar]
- 5. Nickson C, Rippey J. Ultrasonography of sternal fractures. Australas J Ultrasound Med. 2011;14(4):6‐11. doi: 10.1002/j.2205-0140.2011.tb00131.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. You JS, Chung YE, Kim D, et al. Role of sonography in the emergency room to diagnose sternal fractures. J Clin Ultrasound. 2010;38(3):135‐137. doi: 10.1002/jcu.20669 [DOI] [PubMed] [Google Scholar]


