Abstract
Renal hydatid is an uncommon finding, reported in less than 5% patients with hydatid infection. Hydatid involvement of ureter and urinary bladder is an even rarer entity. Renal hydatid is typically unilateral, solitary and arises from cortex. It is essential to be aware of the imaging features of the hydatid cyst for proper diagnosis. Knowledge of the imaging features of various stages is essential since treatment decision is based on cyst stage. Hydatid cyst can mimic several entities both benign and malignant. We present a pictorial review to illustrate the radiological imaging features of hydatid disease involving kidney, ureter and bladder region and its complications.
Introduction
Hydatid disease is a parasitic disease caused by the Echinococcus, most commonly E. granulosus with worldwide distribution. 1 It is endemic in Middle East, South America, Australia and parts of North-west China. 2 Liver is the most commonly involved organ (75%), followed by lungs (15%). Kidney is the third most commonly involved organ, and ureter and urinary bladder involvement is uncommon. 3 Renal hydatid is usually secondary to disseminated hydatid disease or in association with hepatic hydatid. 4 Isolated renal involvement by hydatid is an uncommon. 1,5 It has varied imaging appearances and can easily be mistaken for other cystic lesions. 4 It is essential to be familiar with the imaging appearance and complications of hydatid involving the urinary system as the patients mostly present with non-specific clinical features and characteristic imaging findings help in establishing the diagnosis in such cases. 1
Pathophysiology
The causative agent of hydatid disease is Echinococcus larva; infections by E. granulosus are more common in incidence than E. multilocularis, and less invasive as infections by the latter mimic malignancy. 6
Dog is the definitive host of Echinococcus granulosus. Sheep is the usual intermediate host, but humans are accidental intermediate hosts. 2 Humans usually acquire the infection by close contact with the definitive host or ingestion of the Echinococcus ovum contaminated food and water which is excreted in the faeces of dog or any other definitive host. 1 The ovum is then digested in the duodenum and gains entry into the portovenous or lymphatic system with its subsequent deposition in liver and various organs including kidneys as illustrated in Figure 1. However, the mechanism of selective involvement of kidneys in isolated renal hydatid without hepatic or pulmonary involvement is not fully understood yet. 7
Figure 1.

Life cycle of Echinococcus.
Renal hydatid cysts are usually unilateral, solitary and arise from cortex, commonly in the upper pole. 3 The cyst wall is a trilaminar structure (Figure 2) comprising of the innermost endocyst or germinal layer which produces the scolex and brood capsules. The brood capsules are connected to the germinal layer by a stem and later get separated from it and float within the parent cyst fluid. The middle layer or the laminated layer protects the parasite from host immune response and reduces effect of therapeutic drugs. The outermost layer of pericyst is reactive inflammatory host tissue and encases the hydatid cyst. The intracystic fluid is clear, antigenic fluid which may potentially lead to eosinophilia or anaphylaxis if released into host circulation. 6
Figure 2.

Characteristic structure of hydatid cyst.
Clinical presentation
The clinical presentation is often non-specific ranging from asymptomatic patients to patients presenting with palpable mass, dull lumbar pain, dysuria or hematuria. Patients may also present with hydatiduria, i.e. presence of daughter vesicles in the urine. It is encountered in approximately 18% of patients and presents with colicky pain. 1,8 Urinary bladder hydatid cysts present with acute urinary retention, frequency and urgency. 9 Laboratory tests may show eosinophilia in 25–50% patients. 10
Radiological investigations
Imaging plays the key role in diagnosing and staging of hydatid cyst. 2 The imaging modalities helpful in diagnosis of hydatid cyst are ultrasound, CT and MRI. Ultrasound plays a vital role in diagnosing hydatid disease as it optimally detects hydatid sand, daughter cysts and floating membranes within the cyst and forms the basis for the international classification by WHO (World Health Organisation) expert group and gharbi classification (Tables 1 and 2). 11 Besides, it is also a useful modality helpful in follow up and treatment response assessment. 10
Table 1.
Gharbi classification of hydatid cyst 11
| Gharbi classification stage | Ultrasound appearance | Pathogenesis |
|---|---|---|
| Type I | Purely anechoic cyst with double echogenic walls + echogenic debris (hydatid sand) / “falling snowflake appearance” | Hydatid sand =
detached scolex/ brood capsule from the inner membrane, seen as
dependent tiny echogenic foci / debris Falling snowflake appearance = The echogenic foci of hydatid sand quickly fall to the most dependent portion of the cavity without forming visible strata. 12 |
| Type II | Fluid collection with a split wall | Split wall = Detached inner germinal layer resulting in a floating membrane inside the cyst |
| Type III | Fluid collection
with septa (multiloculated) |
Fluid with multiseptated cysts corresponding to daughter cysts |
| Type IV | Complex heterogeneous mass with hypoechoic appearance, a hyperechoic solid mass, or a lesion with an intermediate pattern, including both hypoechoic and hyperechoic structures | Intracystic infolded membranes, debris, hydatid sand |
| Type V | Cyst with reflecting thick walls | Calcified, usually dead hydatid cysts |
Table 2.
WHO/IWG-E classification of cystic Echinococcosis 11
| WHO/IWG-E classification | Image characteristics |
|---|---|
| CL | Univesicular, cystic lesion with uniform echoes, clear boundary, thin visible wall (Active form) |
| CE1 | Unilocular, simple cysts with uniform anechoic content. A visible cyst wall, hydatid sand and “snow flake sign” corresponding to hydatid sand are pathognomonic signs |
| CE2 | Multivesicular, multiseptated cysts; cysts septations produce “wheel-like”structures, and presence of daughter cysts is indicated by “rosette-like” or “honeycomb-like” structures. |
| CE3a | Detachment of laminated membrane from the cyst wall visible as “big snake sign” or as “Water-lily sign”. The hydatid status is transitional. |
| CE3b | Intracystic shadow of the daughter vesicles and solid septation, manifested as complex cyst shadow. The hydatid is dying. |
| CE4 | Heterogeneous degenerative contents with a ball of wool, contain no daughter cysts |
| CE5 | Intracystic solid degeneration and calcification of the cystic wall (inactive stage) |
WHO/ IWGE = World Health Organisation/ Informal Working Groups on Echinococcosis
CT is useful modality in anatomical mapping, demonstrating cyst wall or septal calcification, and depicting complications. 11
MRI is another modality which is helpful to depict the internal architecture of cystic component. 13 It is especially helpful in cases in which lesion is inaccessible to ultrasound. 14
CEUS (contrast-enhanced ultrasound) is an emerging promising modality with the advantage of demonstrating septal, nodular or solid component enhancement that too in continuous real time. This is helpful to differentiate from neoplasms. 15
Imaging findings
Renal hydatid
The ultrasound appearance of the hydatid cyst varies depending on the stage of hydatid. Ultrasound findings are anechoic cystic lesions with usually well-defined margins (Tables 1 and 2). The double echogenic lines of the cyst wall, representing pericyst and laminated cyst membrane, is a feature on ultrasound. 13 Internal septations, daughter cysts, echogenic debris and parasitic membranes are seen optimally within the cavity (Figure 3). The internal membranes of the cyst are visible as linear or curvilinear echogenic structures and are pathognomonic for hydatid cyst (Figure 4). The daughter cysts and hydatid sand (Figure 5) are seen to shift on ultrasound with postural change. 7 Multiple daughter vesicles arise from the germinal layer peripherally within the parent cyst which impart a multiloculated, “cysts within a cyst” appearance. 1 The contents of the hydatid matrix impart it an echogenic appearance which might be confused for solid component (Figure 6A). Colour Doppler and CEUS are effective supplementary tools especially in more advanced stages of solid appearing lesions, wherein lack of vascularity (Figure 6B) and lack of contrast enhancement (Figure 6C) are helpful to avoid misinterpreting them as neoplasms.
Figure 3.

Serologically and surgically proven renal hydatid in a young female: Ultrasonography depicting multivesicular cyst showing peripheral daughter cysts (*) and heteroechoic maternal matrix (M).
Figure 4.

Renal hydatid cyst in a young female: Ultrasonography showing floating parasitic membranes (arrow) seen as echogenic linear or curvilinear structures.
Figure 5.
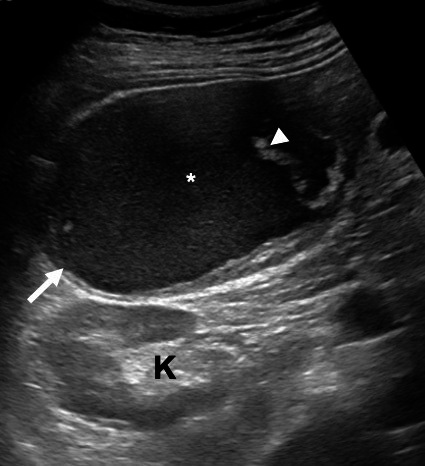
A 27-year-old male with multiple hydatid cysts in the abdomen. Ultrasound image showing a perinephric space hydatid (arrow) located anterior to the kidney (K) showing echogenic hydatid sand (*) dispersed throughout the cyst (“snowstorm”) alongwith echogenic parasitic membranes (arrowhead).
Figure 6.

Renal hydatid cyst in a 30-year-old female. Ultrasonography (A) showing peripheral daughter cysts and central echogenic solid-appearing maternal matrix (circle) simulating malignancy. (B) Central echogenic solid-appearing area showing no vascularity on colour Doppler making malignancy unlikely. (C) Central echogenic solid-appearing area showing no contrast enhancement on CEUS (right side of the image), making malignancy highly unlikely. CEUS, contrast-enhanced ultrasound.
Complete calcification of all components of the hydatid cyst is indicative of quiescence or death of the parasite. 12 It is important to note that partial calcification of the cyst does not necessarily indicate parasite death.
Various classification schemes have been suggested over the years for liver hydatid cysts on the basis of their ultrasound appearances; however, the classification system by Gharbi et al (Table 1) and the World Health Organisation (WHO) classification (Table 2) are the most commonly followed.
Recently, WHO proposed an international consensus classification of ultrasound features of cystic echinococcosis (CE) which allows grouping of cysts into three relevant categories as per treatment plan: active or fertile cysts (CE1 and 2), transitional cysts with compromised cyst integrity (CE3a and CE3b) and inactive or non-viable (CE4 and 5) (WHO and Echinococcosis, 2003) as illustrated in Figure 7. Usually, active cysts need to be treated by chemical therapy or surgery because of the potential of spreading to other organs. 2
Figure 7.
Illustration depicting the classification of hydatid cyst as per WHO/IWGE classification which can be grouped into active, transitional and inactive stages. WHO, World Health Organisation.
CT needs to be done in patients with complex cysts to rule out features of malignancy, and evaluate the extent of disease. The cyst wall and septations show high attenuation on NCCT (non-contrast CT) and may or may not show enhancement as depicted in Figure 8. Multivesicular cysts show mixed internal attenuation (Figures 9 and 10). 8 This appearance is attributed to the broken membranes within the maternal matrix. Findings of calcification and non-enhancing solid appearing content make neoplasm less likely which is a close mimicker (Figure 11A and B & C).
Figure 8.

Renal hydatid cyst in a young female. Dual energy CT (A) virtual unenhanced images show thick-walled cyst with hyperattenuating internal septations (arrow). (B) Iodine overlay map shows no iodine uptake suggesting non-enhancement of wall and septae.
Figure 9.

Renal hydatid cyst in a young female. CECT showing characteristic mixed internal attenuation renal hydatid cyst in right kidney (higher density of the central maternal matrix (*) compared to the multiple, irregularly arranged, peripheral, fluid attenuation daughter cysts, which are seen nearly completely occupying the mother cyst giving rise to a “rosette” appearance. CECT, contrast-enhanced CT.
Figure 10.

CECT abdomen depicts left renal hydatid cyst with characteristic “spoke-wheel” appearance, seen as multiple-rounded daughter cysts arranged at periphery with central high-density matrix. CECT, contrast-enhanced CT.
Figure 11.

Renal hydatid in a 34-year-old male: NCCT (A, B) showing right renal hydatid with peripheral wall calcification (small arrow) and intracystic contents. CECT(C) showing no enhancement. Findings of non-enhancing solid appearing content precludes malignancy. CECT, contrast-enhanced CT.
The MRI features helpful in diagnosis of hydatid cyst are hypointense wall (represented by the dense, fibrous pericyst) along with intermediate signal intensity detached membranes on T 2 weighted imaging seen as intracystic twisted-linear structure (serpent-sign) (Figure 12). 11 The multivesicular hydatid shows mixed signal intensity due to mixed contents. The daughter cysts seen as round cysts attached to the wall appear hypointense on T 1 weighted images and hyperintense on T 2 weighted imaging in relation to central maternal matrix (Figure 13). 13
Figure 12.

Renal hydatid in a 16 year old female: T 2WI images show hypointense wall represented by the fibrous pericyst (arrow) and intracystic twisted-linear structures (arrowhead) indicative of detached membranes (serpent-sign or snake-sign). T 2WI, T 2 weighted imaging.
Figure 13.

Renal hydatid in a 16-year-old female: Coronal T 2WI MRI image shows multivesicular hydatid shows mixed signal intensity due to difference in contents. The daughter cysts (arrowhead) seen as small cystic structures attached to the cyst wall in relation to central maternal matrix (arrow). T 2WI, T 2 weighted imaging.
Ureter and urinary bladder hydatid
Primary hydatid disease of the urinary bladder is very uncommon (<1% of all cases). Hematogenous spread of infection results in development of cyst in the wall of urinary bladder. Parasitic membranes or daughter cysts can be visualised within ureter or urinary bladder lumen in event of cyst rupture into collecting system (Figures 14 and 15). 16–18 The imaging appearance of ureteral and urinary bladder hydatid are same as that of renal hydatid. There is added value of CT and MR Urography since the delayed post-contrast phase helps in visualising the cysts and membranes as filling defects, which may otherwise be missed due to the same attenuation of the cyst content and urine.
Figure 14.

Renal hydatid cyst rupture into pelvicalyceal system: Ultrasonography (A) shows echogenic debris (hydatid sand) and echogenic linear and curvilinear membranes (arrow) within pelvicalyceal system and proximal ureter. T 2W MRI (B) coronal images depicting linear intermediate signal intensity and hypointense detached membranes (arrow) within the pelvis and upper ureter. T 2W, T 2 weighted.
Figure 15.

Urinary bladder hydatid cyst: Ultrasonography image (A) showing linear echogenic membranes (arrow) and debris (hydatid sand) in dependent part of urinary bladder. Excretory phase CECT axial image (B) shows linear filling defect (arrow) within the urinary bladder lumen indicative of parasitic membranes. CECT, contrast-enhanced CT.
Complications
Complications of renal hydatid cyst are rupture into collecting system or perinephric space and secondary infection. 11 Ultrasound can help diagnose these complications by demonstrating parasitic membranes and debris within the pelvicalyceal system in case of rupture (Figure 14A). The same findings can be confirmed on CT and MRI (Figure 14B). Detection of subcapsular or perinephric collection can raise suspicion of subcapsular rupture (Figure 16). Demonstration of air foci within the cyst is highly suggestive of secondary infection.
Figure 16.

Renal hydatid rupture into sub capsular and perinephric space: CECT axial images (A) shows a as breach (arrow) of normal parenchyma. Coronal images (B) show fluid (*) in subcapsular and perinephric location. CECT, contrast-enhanced CT.
Differential diagnosis
Unilocular hydatid looks similar to a simple cyst but double echogenic walls of hydatid along with “hydatid sand” and “snowstorm appearance” on ultrasound can help in diagnosis.
Complex, multivesicular renal hydatid needs to be differentiated from hemorrhagic cyst, chronic abscesses and malignancies. The papillary renal cell carcinoma is a very close differential as it is a hypovascular tumour (Figure 17). Presence of multiple daughter cysts is helpful to exclude tumour. A heterogenous multilocular cystic lesion on CT favours diagnosis of hydatid over malignancy. However, malignancy can be predicted by septal and nodular enhancement on contrast-enhanced imaging studies. 19 Both malignancy and hydatid cyst are managed by surgical excision and final diagnosis is always established by subsequent histopathology. 19 Thus, a combination of clinical, radiological, serological and pathological findings is required for definitive diagnosis of hydatid cyst disease, imaging by ultrasound or CT is considered the main tools for diagnosis, and serology and other tests are considered complementary. 2,20 Counter immunological electrophoresis against arch-5 is the only test with the best specificity for hydatid disease. 19 The utility of fine needle aspiration cytology in hydatid cyst is limited because of the potential risk of anaphylaxis and cyst seeding, however, some reports in published literature have depicted it as a relatively safe procedure, which proved useful to reach the definitive diagnosis. 20
Figure 17.

Complex renal mass in 50-year-old male: T 2WI (A) show internal hypointense contents and linear structures with no definite post-contrast enhancement on post-gadolinium (B) images. Ultrasonography (C) showed a complex mass with echogenic solid-appearing area showing no colourflow on Doppler. In absence of daughter vesicles, maternal matrix and detached membranes, diagnosis of hydatid seemed unlikely. The histopathological diagnosis was papillary renal cell carcinoma. T 2WI, T 2 weighted imaging.
Treatment
Preferred treatment of renal hydatid disease is surgical removal. 5 Removal of hydatid with pericystectomy is the usual treatment to spare the kidney. Extensive involvement may lead to nephrectomy. Surgical excision of intact cyst is preferred treatment for urinary bladder hydatid. 17 1-month pre- and post-operative course of Albendazole helps to decrease the risk of anaphylaxis. It also reduces the tension inside the cyst and help to reduce the recurrence rate. 18
Conclusion
Hydatid involvement of kidney, ureter and urinary bladder is rare, however, radiologists must be aware of the imaging appearance, especially in endemic areas to make proper diagnosis. Hydatid should be considered as a differential for complex cystic lesions of kidney. Sonography is important imaging modality for diagnosing hydatid disease, whereas CT scan and MRI may be used to evaluate complication and to delineate the extent before surgery.
Footnotes
Authors’ contributions: Shivani Gupta – Conception and design of work, Literature search, manuscript preparation, Chandan J Das - Conception and design of work, Manuscript editing All authors read and approved the final manuscript.
Contributor Information
Shivani Gupta, Email: shivani040891@gmail.com, Department of Radiodiagnosis, AIIMS, New Delhi, India .
Chandan Jyoti Das, Email: dascj@yahoo.com, Department of Radiodiagnosis, AIIMS, New Delhi, India .
REFERENCES
- 1. Ishimitsu DN, Saouaf R, Kallman C, Balzer BL . Renal hydatid disease . RadioGraphics 2010. ; 30: 334 – 37 . doi: 10.1148/rg.302095149 [DOI] [PubMed] [Google Scholar]
- 2. Rexiati M, Mutalifu A, Azhati B, Wang W, Yang H, Sheyhedin I, et al. . Diagnosis and surgical treatment of renal hydatid disease: a retrospective analysis of 30 cases . PLoS ONE 2014. ; 9: e96602 . doi: 10.1371/journal.pone.0096602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rami M, Khattala K, ElMadi A, Afifi MA, Bouabddallah Y . The renal hydatid cyst: report on 4 cases . Pan Afr Med J 2011. ; 8: 31 . doi: 10.4314/pamj.v8i1.71147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhaya A, Shinde AP . Isolated renal hydatid presenting as a complex renal lesion followed by spontaneous hydatiduria . World J Radiol 2015. ; 7: 180 – 83 . doi: 10.4329/wjr.v7.i7.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Turgut AT, Odev K, Kabaalioglu A, Bhatt S, Dogra VS . Multitechnique evaluation of renal hydatid disease . AJR Am J Roentgenol 2009; 192: 462–67. 10.2214/AJR.08.1129 [DOI] [PubMed] [Google Scholar]
- 6. Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A . Hydatid disease from head to toe . Radiographics 2003. ; 23: 475 – 94 . doi: 10.1148/rg.232025704 [DOI] [PubMed] [Google Scholar]
- 7. Misra A, Mandal S, Das M, Mishra P, Mitra S, Nayak P . Isolated renal hydatid disease: varied presentations, treatments, dilemmas, and the way ahead: case report series . Afr J Urol 2021. ; 27( 1 . doi: 10.1186/s12301-021-00183-5 [DOI] [Google Scholar]
- 8. Volders WK, Gelin G, Stessens RC . Best cases from the AFIP. hydatid cyst of the kidney: radiologic-pathologic correlation . Radiographics 2001. ; 21 Spec No: S255 - 60 . doi: 10.1148/radiographics.21.suppl_1.g01oc16s255 [DOI] [PubMed] [Google Scholar]
- 9. Kumar S, Singh S . . [ Internet ]. Current Topics in Echinococcosis IntechOpen 2015. . Available from : https://www.intechopen.com/chapters/48601 [Google Scholar]
- 10. Jahangiri F, Sayyahfar S, Zarei E, Hoseini R, Nasiri SJ . Renal hydatid cyst or a simple cyst? report of a rare case . Arch Pediatr Infect Dis 2018; 7(1). 10.5812/pedinfect.68459 [DOI] [Google Scholar]
- 11. Mehta P, Prakash M, Khandelwal N . Radiological manifestations of hydatid disease and its complications . Trop Parasitol 2016. ; 6: 103 – 12 . doi: 10.4103/2229-5070.190812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS . Hydatid disease: radiologic and pathologic features and complications . Radiographics 2000. ; 20: 795 – 817 . doi: 10.1148/radiographics.20.3.g00ma06795 [DOI] [PubMed] [Google Scholar]
- 13. Marrone G, Crino’ F, Caruso S, Mamone G, Carollo V, Milazzo M, et al. . Multidisciplinary imaging of liver hydatidosis . World J Gastroenterol 2012. ; 18: 1438 – 47 . doi: 10.3748/wjg.v18.i13.1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stojkovic M, Rosenberger K, Kauczor H-U, Junghanss T, Hosch W . Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl Trop Dis 2012. ; 6( 10 ): e1880 . doi: 10.1371/journal.pntd.0001880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lerchbaumer MH, Putz FJ, Rübenthaler J, Rogasch J, Jung E-M, Clevert D-A, et al. . Contrast-enhanced ultrasound (CEUS) of cystic renal lesions in comparison to CT and MRI in a multicenter setting . Clin Hemorheol Microcirc 2020. ; 75: 419 – 29 . doi: 10.3233/CH-190764 [DOI] [PubMed] [Google Scholar]
- 16. Srinivas MR, Deepashri B, Lakshmeesha MT . Imaging spectrum of hydatid disease: usual and unusual locations . Pol J Radiol 2016. ; 81: 190 – 205 . doi: 10.12659/PJR.895649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arif SH, Mohammed AA . Primary hydatid cyst of the urinary bladder . BMJ Case Rep 2018. ; 2018: bcr-2018-226341 . doi: 10.1136/bcr-2018-226341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mongha R, Narayan S, Kundu AK . Primary hydatid cyst of kidney and ureter with gross hydatiduria: A case report and evaluation of radiological features . Indian J Urol 2008. ; 24: 116 – 17 . doi: 10.4103/0970-1591.38617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bhat GS, Burude VA, Hegde SD, Tembadamani VS . Isolated renal hydatid cyst masquerading as cystic renal cell carcinoma: A case report . J Clin Diagn Res 2015. ; 9: P D07 - 8 . doi: 10.7860/JCDR/2015/11488.5730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sinan T, Sheikh M, Chisti FA, Al Saeed O, Sheikh Z, Hira PR, et al. . Diagnosis of abdominal hydatid cyst disease: the role of ultrasound and ultrasound-guided fine needle aspiration cytology . Med Princ Pract 2002. ; 11: 190 – 95 . doi: 10.1159/000065809 [DOI] [PubMed] [Google Scholar]



