Abstract
Introduction:
Critically ill neonates and those with complex medical conditions frequently require the use of central venous lines. Unfortunately, central line-associated bloodstream infections (CLABSIs) result in significant morbidity and mortality, and the cost and increased length of stay burden the healthcare system. Previous studies have demonstrated that standardized care bundles can decrease CLABSI rates, but achieving sustained improvement has proven difficult.
Methods:
All patients admitted to the Neonatal Intensive Care Unit between 2014 and 2020 who had a CVL were included in this study. First, we recorded all CLABSI events and total CVL days according to defined criteria. Then, in late 2016, we instituted simulation-based nursing training for CVL care.
Results:
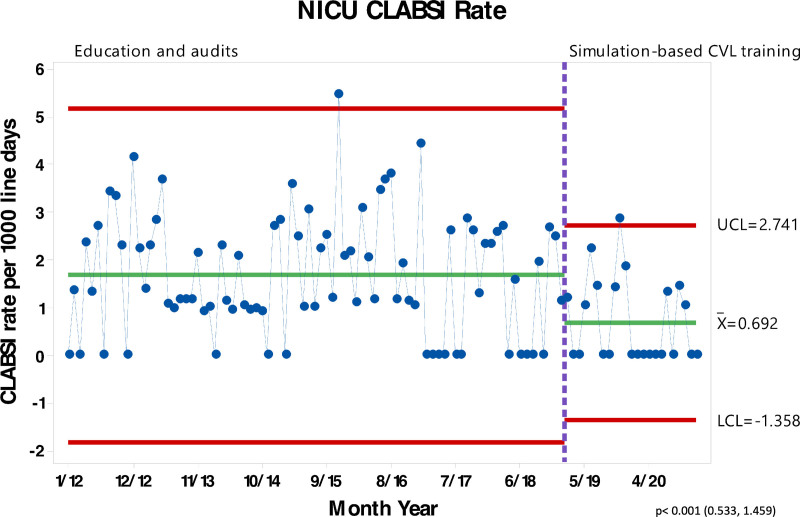
Job Instruction Sheets were initially introduced to Neonatal Intensive Care Unit nursing staff simultaneously with one-on-one teaching sessions between instructors and bedside nurses. Intermittent performance audits and re-education for identified deficiencies did not improve the CLABSI rate per 1000 line days. After instituting simulation-based CVL training in 2016, there was a decreased rate of CLABSI events per 1000 line days sustained over time (x = 0.692).
Conclusions:
Standardized care bundles and Hospital-acquired Condition interactor audits were insufficient to reduce the CLABSI rate. However, combining care bundles and education with simulation-based training significantly decreased CLABSI rates. One-on-one intensive training and continued ongoing monitoring were critical to producing a sustained reduction. This experience demonstrates that supervised, interactive education combined with simulation can significantly impact patient outcomes.
INTRODUCTION
Central line-associated bloodstream infections (CLABSIs) in the Neonatal Intensive Care Unit (NICU) occur more frequently and increase the morbidity and mortality for these children than in other ICUs.1,2 CLABSI rates in neonates have been reported from 3.2 to as high as 21.8 CLABSIs per 1000 central venous line days.3 In addition, CLABSIs are a major contributor to late-onset sepsis.4 This fact, coupled with a relatively immature immune system in neonates, makes preventing CLABSIs and nosocomial sepsis in this population a priority. In recent years, central line bundles were developed and, when implemented and used correctly, have proven successful in decreasing the CLABSI rate.5
Several factors can affect the CLABSI rate in the neonatal population. Some factors, such as immune system development, intestinal bacterial overgrowth, and duration of central venous access, can be challenging to modify.6,7 Other interventions, such as central line care by hospital staff, including standardized bundles, have reduced the CLABSI rate.8–10 A care bundle is a set of evidence-based practices combined to increase compliance to improve patient outcomes more than when these practices are used alone. Specific practices included in a bundle might include hand hygiene, skin cleaning agent, specific insertion sites, standardized insertion equipment, etc. In addition, bundles are used to improve line insertion and line maintenance.5 In 2013, as part of the Solutions of Patient Safety (SPS) initiative, our NICU adopted and implemented new patient care bundles to improve the CLABSI rate. In 2012, the CLABSI rate was 2.1 per 1000 CVL days. Bundled interventions aim to provide the bedside nurse with a structure to implement a systematic process successfully. Studies have shown that the reliable performance of these bundles improves patient outcomes, thus decreasing the overall CLABSI rate.5 However, after implementing the patient care bundles in the NICU, we did not have a sustained reduction in our NICU CLABSI rates.
Based on our initial results, we identified several barriers, including high patient acuity, prolonged hospital length of stay, and prolonged requirement for central venous lines. Changing the safety culture in the NICU was a priority so that the nursing staff felt empowered to identify and confront non-compliant providers. Some unanticipated barriers included nursing staff turnover, buy-in from staff, funding, and the use of private rooms. Studies show that simulation is effective for training novice and experienced nurses. Repeating simulation assists in retaining those skills and maintaining the skills of more experienced staff.11 Education that includes scenario-based low-fidelity simulation is more effective than self-directed learning and didactic lectures.12 We aimed to improve our NICU CLABSI rates by instituting simulation-based CVL training and the previously established quality improvement measures. This experience describes how adding simulation-based CVL training to established quality improvement measures, including standardized care bundles, reduced CLABSI rates in our NICU.
METHODS
The NICU is a 48-bed unit with single patient rooms providing care for critically ill infants ranging in age from newborns (including premature) to 2 years of age. It is a Level IV facility serving a large five-state catchment area in the Southeast, providing surgical services and ECMO support for patients and caring for various disease processes and congenital anomalies. The NICU is staffed with a multidisciplinary approach with a team of board-certified neonatologists, certified neonatal nurse practitioners, registered nurses, dedicated respiratory therapists, discharge planners, pharmacists, social workers, chaplain support, and physical and occupational therapists. It has an average daily census of 45.4 patients and an average of 35 admissions per month. This study aimed to reduce the CLABSI rate in our level IV NICU.
Definitions
As defined by the National Health Safety Network (NHSN), a central line-associated bloodstream infection (CLABSI) is a laboratory-confirmed bloodstream infection (LCBI) where an eligible bloodstream infection (BSI) organism is identified, and an eligible central line is present on the LCBI day of the event (DOE) or the day before. An eligible BSI organism is any organism eligible for use to meet LCBI or mucosal barrier injury (MBI)-LCBI criteria, meaning an organism that is not an excluded pathogen for use in meeting LCBI or MBI-LCBI criteria. A primary BSI is an LCBI that is not secondary to an infection at another body site.13,14
The NHSN defines a CVL as any venous catheter “that terminates at or close to the heart or in one of the great vessels… used for infusion, withdrawal of blood, or hemodynamic monitoring. For data purposes, a central line … has been in place for more than two consecutive calendar days (on or after central line day 3), following the first access of the central line, in an inpatient location, during the current admission. Such lines are eligible for CLABSI events and remain eligible for CLABSI events until the day after removal from the body or patient discharge, whichever comes first.” Arterial and ECMO catheters are excluded from central lines for NHSN reporting purposes.13
Patients
The study included all patients admitted to the NICU from 2013 to 2020. We considered patients to have a CVL if it met the previously defined NHSN criteria. Central line days were calculated by documenting central lines present at 0800 each day. Patients with more than one CVL who developed a CLABSI were only counted as a single CLABSI event.
Timeline of Initial CLABSI Reduction Interventions
In 2013, the hospital joined Solutions for Patient Safety (SPS), a network of Children’s hospitals to reduce hospital-acquired conditions (HAC), including CLABSI events. This collaboration began the NICU’s journey to reduce CLABSIs, and multiple interventions were instituted with this goal. Then we added mandatory staff meetings and computer-based training from SPS for all staff.
Using a Plan Do Study Act (PDSA) methodology the following year, the NICU implemented patient care bundles for various HAC, including CLABSI. The first intervention was using a chlorhexidine gluconate product for all CVL dressing changes. Previously, the NICU utilized alcohol and/or betadine for dressing changes in patients less than two months old. As a result, there was a small initial reduction in the CLABSI rate, but this improvement was not sustained.
In 2015, we evaluated the staff’s knowledge about CLABSI events and prevention to review compliance with the bundle elements. We used oral Question and Answer sessions and chart audits for CLABSI bundle compliance. The chart audits indicated a need for re-education. Therefore, all new nursing hires were taught the process of changing fluids step-by-step with laminated bundle instructions placed on bedside carts. Regular reminders were also sent to staff through various methods of communication, including emails, posters in the unit, staff room boards, and discussions in staff meetings. During this same time, the NICU participated in the CLABSI 1:90 Collaborative, the Institute of Healthcare Improvement’s (IHI) 90-day learning cycles to advance quality in health care.15 This intervention included using Mayo stands in each patient room, documenting dressing integrity at shift report, and re-educating staff on the tubing change process. Also, in November 2015, we adjusted the schedule of changing needleless adaptors “cap” to Monday and Thursday (and upon admission for central venous lines placed on transferred infants from an outside hospital) rather than daily. In addition, we modified adaptor kits to include all elements needed for a single change.
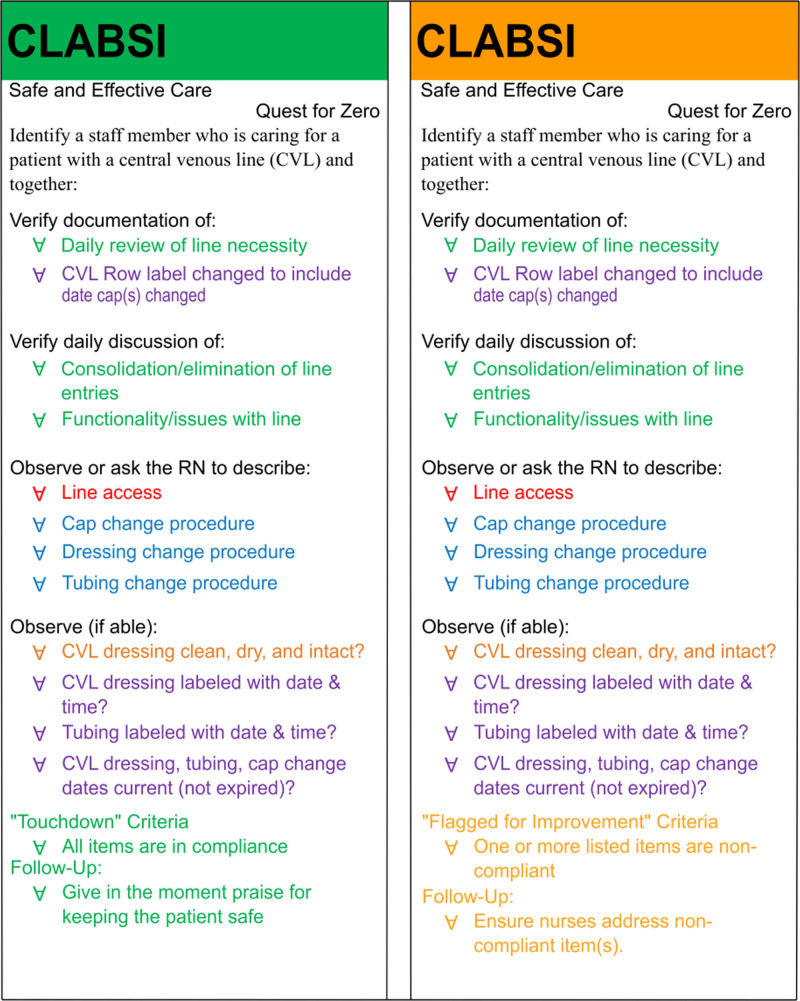
Initial efforts in January 2016 included the development of Kamishibai cards, or “K cards.”16–18 These laminated cards function like cue cards or work instructions for auditing a process. The NICU displayed them in the nursing conference rooms and reviewed them during daily huddles (Fig. 1).
Fig. 1.
Kamishibai “K” cards. Shown are the initial K cards introduced in 2016 and remain in use.
All of the previously described interventions are discussed in the literature as a part of care bundles, a set of interventions that, when used together, reduce CLABSI events.19 Even after standardizing CVL care, instituting patient care bundles, “K cards,” and a single intensive training of new staff, our CLABSI rate did not improve. It became clear from the previously described chart audits and one-on-one questioning of staff in 2015 that a single education initiative would not be adequate to provide a sustained reduction of CLABSIs. This finding formed the baseline phase for our study.
Simulation Intervention
In September 2016, nursing leadership attended the Solutions for Patient Safety (SPS) Annual Learning Session and learned about the teaching process of Job Instruction Sheets (JIS).20,21 NICU instituted a High-Reliability Unit (HRU), which included additional mandatory in-service training sessions for staff and one-on-one interactive training sessions utilizing the model of low-fidelity simulation.
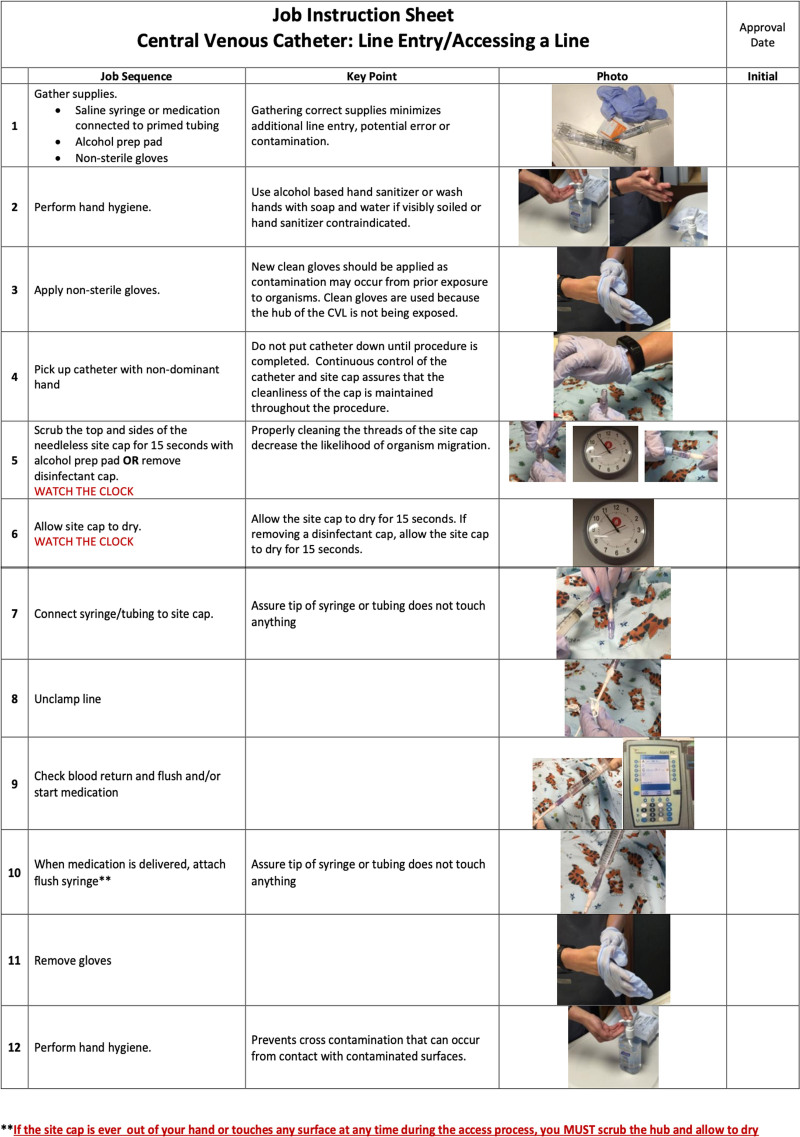
The initial simulation process utilized JIS and introduced and discussed them in multi-disciplinary meetings, including physicians and nursing staff, to adapt the concept of JIS to fit the needs of the NICU. A JIS is a visual aid that gives step-by-step written and pictorial instructions and the sequence for how to perform a certain procedure properly. This sheet also provides details and justification for the specific process. The included elements in the JIS were the cap change process, dressing changes, accessing central venous lines, and line draws utilizing a closed system. These JIS were utilized for one-on-one coaching of approximately 190 RNs in the NICU (Fig. 2).
Fig. 2.
Job Instruction Sheets. Shown is an example of a Job Instruction Sheet (JIS) developed for the process of central venous line (CVL) entry. These JIS are used for training and re-education when necessary.
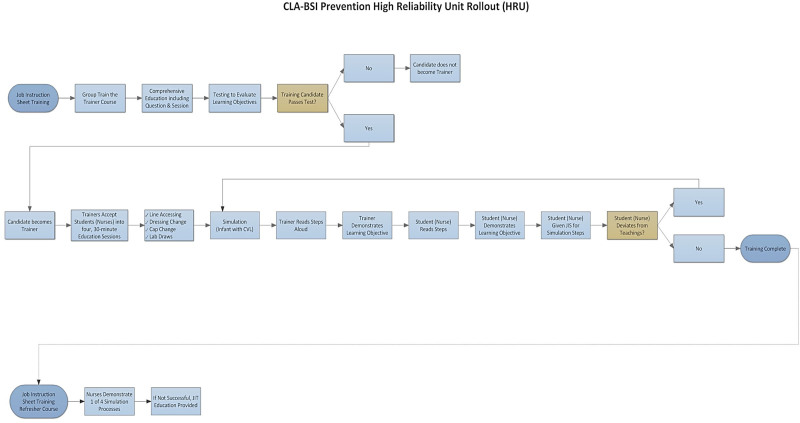
The simulation process started with a “train the trainer” day. During this training session, select nurses designated to teach the process attended a two-hour training session and were given step-by-step instructions and were taught in the same format they would be teaching others. Nursing leadership taught each component (cap change, dressing change, accessing CVLs, and line draws) with a unique JIS and at an individual station simulated at the patient’s bedside. The low-fidelity simulation stations included a simulation doll with a CVL, a patient bed, a mayo stand, gloves, alcohol-based hand gel, and additional supplies. Nurses rotated through each station and were taught to complete the process on each topic identified with a JIS. The individual process steps included:
The trainer reads the entire JIS, which includes “what process to do” and the explanation of “why you do it.”
Then, the trainer reads the process and coaches the RN on the proper technique of the procedure.
The trainee RN then reads the JIS aloud.
The trainee RN then demonstrates the process for the trainer.
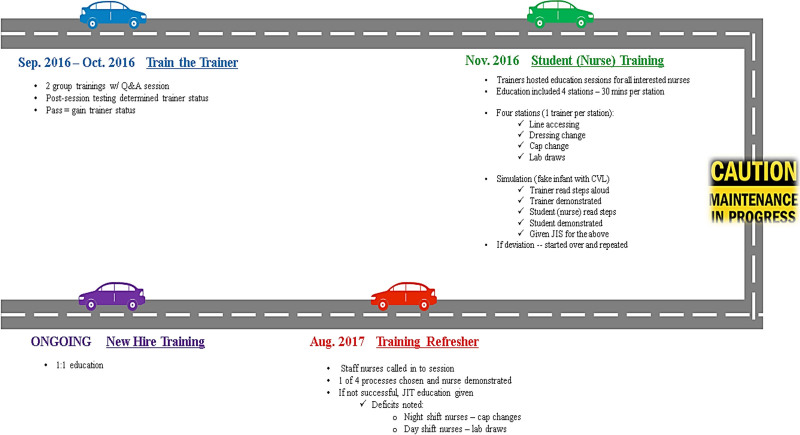
Figure 3 shows the process map of the training process. If the trainee deviates from the proper technique or process, they are given further education and job instruction training using the standards of simulation-based mastery learning.22
Fig. 3.
Process Map for Implemented Program of Training and Simulation.
The outcome of this study was the CLABSI rate. Process measures included audits to maintain compliance with the bundles. Data were analyzed using Minitab 18 (Minitab Statistical Software 2010, Minitab Inc., State College, PA). A Chi-Square analysis for NICU CLABSI rate was performed for baseline (education and audits) data compared with improvement (Simulation-based CVL training) data.
RESULTS
In response to the increase in CLABSI rate, the NICU staff began the ongoing simulation education and instruction in September 2016. Using job instruction sheets and one-on-one training sessions, we created central line simulations to mimic real-life patient scenarios described in the methods section. According to regular audits, all nurses go through the simulation during orientation and then again as needed. Intense and continued staff simulation training produced an impressive reduction in the NICU CLABSI rate with a centerline shift in February 2019. The reduced rate was sustained and showed continued improvement through 2020, with a reduced rate of 0.692 (Fig. 4).
Fig. 4.
NICU CLABSI Rate per 1000 line days.
The NICU also experienced more months with zero CLABSI events in the 2017 to 2020 period (24 months) compared to the 2014 to 2016 time period (5 months). Based on the control chart of CLABSI rates by month, we demonstrate a significant trend for improvement (p = 0.001, Chi-square analysis). With a reduction in CLABSI events, process variability tapered in the post-implementation phase with an upper control limit of 2.741 (Fig. 4). We used the Healthcare IHI rules for special cause variation to determine this process change.
While there was an ongoing overall goal to reduce the number of central line days, there were no major interventions after implementing these processes. In addition, the average daily census for the unit remained stable, ranging from 44.8 to 45.8 over the study period. Figure 5 shows a summary timeline of interventions.
Fig. 5.
Timeline of Interventions.
DISCUSSION
This article describes how our Level IV NICU achieved a significant and sustained reduction in the CLABSI rate by utilizing a structured bedside simulation program incorporating JIS in addition to patient care bundles. In addition, the NICU demonstrated ongoing improvement in the CLABSI rate even following the study conclusion.
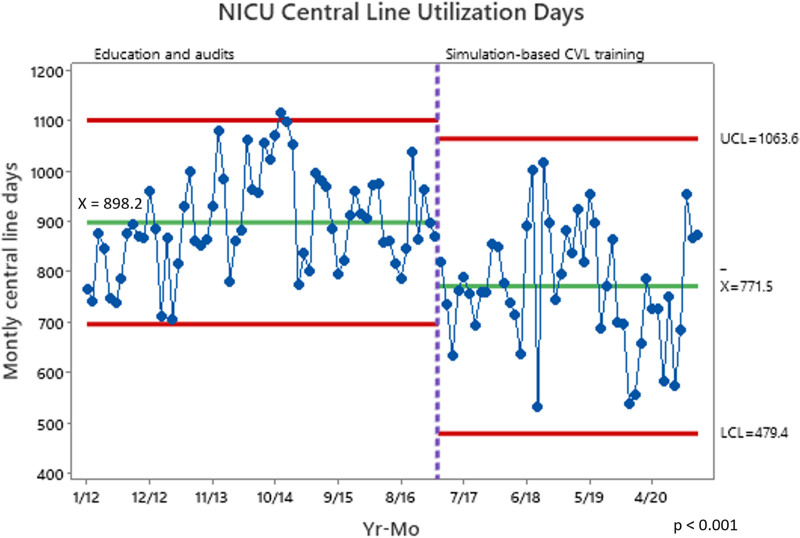
Overall CVL placement numbers and length of use of CVLs within the NICU have also decreased, mirroring a trend within all hospital areas. This result is demonstrated in Central Line Days (Fig. 6), showing a control chart with baseline days of 898.2 and post-intervention line days of 771.5. This result is found to be a significant difference using the Student’s t-test (p < 0.001 CI 98.1, 187.5). The process change began in March 2017, when the IHI special case rules began. However, in a population of infants with chronic and complex medical issues, multiple or prolonged use of central lines is often unavoidable. These medically complex neonates typically have an increased length of stay and cost, but CLASBIs frequently worsen these metrics. In addition, previous studies have demonstrated that the cost of a single CLABSI remains significant, with a mean attributable cost and length of stay of over $50,000 and 19 days, respectively.23 Therefore, the cost of both the staff time and supplies required to provide intensive training and audits is a valuable investment for intensive care units and hospital systems.
Fig. 6.
NICU Central Line Utilization Days.
Increased morbidity and mortality and healthcare expenses highlight the critical need to find methods for further reduction of CLABSIs. Single-center and multicenter studies have demonstrated that adding standardized care bundles and checklists reduced CLABSI rates in NICUs.24 A large study of adult ICUs demonstrated that central line bundles such as those promoted by Institute for Healthcare Improvement (IHI) and other groups effectively reduce CLABSI rates, but only if compliance is very high > 95%.25 This article also describes a temporary reduction in CLABSI rates following the inclusion of care bundles, however, this NICU could not obtain a sustained reduction. Other studies have shown how simulation reduces CLABSI infections; however, most focus on CVL placement.19,26,27 Additional studies have focused on using simulation for CVL access and maintenance and have demonstrated positive results.28,29 These results extend these studies and demonstrate that intense education in central line care and, more importantly, re-education performed in a simulation atmosphere can result in sustained reductions in CLABSI rates.
Simulation training has been used in industries with risks to human life, such as aviation, military, and nuclear power plants. This methodology has also been used in healthcare and is becoming more common in educating staff and improving team performance. Studies have shown that simulation-based training can produce short-term and sustained improvement in skills.30 Both low- and high-fidelity scenarios are more effective than traditional didactic learning and can be used in nursing education for central line insertion and care.11,12 High-fidelity simulation using lifelike devices that provide real-time feedback is a growing trend in education and training, but they are expensive and staff intensive. But a low-fidelity simulation using simple and low-cost interventions performs well in practicing and improving skills.31,32
Anticipated barriers to successfully implementing care bundles and simulation included the requirement to train many nurses (about 190). The NICU obtained administrative support to provide the overtime payments necessary to train the entire nursing staff and the increased supplies required for the teaching sessions. We also anticipated some staff members would be reluctant to confront non-compliant providers, which is essential to establishing a safety culture. Transitioning to a new NICU facility with private rooms was another barrier during this period. This change posed an initial challenge for the bedside nurses accustomed to a more open format and resulted in a temporary increase in nursing turnover. Another unavoidable and ongoing barrier is the nursing staff turnover, requiring continued replacement and education of new staff members. This barrier requires nursing leadership to offer training for new hires continually. HAC (Hospital-acquired condition) interactor audits were used as a part of the SPS collaborative to maintain compliance with the bundles. Staff are retrained as necessary to maintain compliance.
When COVID restrictions were put into place in March 2020, it affected the ability to perform simulations and other group activities. There was concern that this would negatively affect the CLABSI rate. However, rates continued to improve. Possible explanations for ongoing improvements include a limited number of caregivers and visitors with access to the patient and increased personal concern with hand hygiene and universal masking. But along with decreased viral infections, etc., CLABSI infections were also less after initiating COVID precautions.
In conclusion, we have demonstrated that a sustained reduction in CLABSI events, even in units with complex patients with multiple central venous lines, can be obtained through intensive one-on-one training and ongoing simulation. These studies also lend indirect support for simulation in other patient care outcomes.
ACKNOWLEDGMENTS
The authors would like to acknowledge the hard work and effort of the frontline staff of nurses, physicians, and other team members who cared for these patients and ultimately are responsible for the decreased CLABSI rates and excellent outcomes.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online October 18, 2022
Drs. Martin and Chewning contributed equally to this work.
To cite: Hightower, HB, Young JA, Thomas J, Smith JS, Hobby-Noland D, Palombo G, McCaskey M, Benton B, Hutto C, Coghill C, McCullough B, Leslie Hayes L, Martin C, Chewning JH. Reduction of Central Line Associated Bloodstream Infections in a Tertiary Neonatal Intensive Care Unit through Simulation Education. Pediatr Qual Saf 2022;7:e610.
REFERENCES
- 1.Ceballos K, Waterman K, Hulett T, et al. Nurse-driven quality improvement interventions to reduce hospital-acquired infection in the NICU. Adv Neonatal Care. 2013;13:154–163; quiz 164–165. [DOI] [PubMed] [Google Scholar]
- 2.Hooven TA, Polin RA. Healthcare-associated infections in the hospitalized neonate: a review. Early Hum Dev. 2014;90 Suppl 1:S4–S6. [DOI] [PubMed] [Google Scholar]
- 3.Folgori L, Bielicki J, Sharland M. A systematic review of strategies for reporting of neonatal hospital-acquired bloodstream infections. Arch Dis Child Fetal Neonatal Ed. 2013;98:F518–F523. [DOI] [PubMed] [Google Scholar]
- 4.Payne V, Hall M, Prieto J, et al. Care bundles to reduce central line-associated bloodstream infections in the neonatal unit: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2018;103:F422–F429. [DOI] [PubMed] [Google Scholar]
- 5.Pogorzelska-Maziarz M. The use and effectiveness of bundles for prevention of central line–associated bloodstream infections in neonates. J Perinat Neonat Nurs. 2016;30:148–159. [DOI] [PubMed] [Google Scholar]
- 6.Collins A, Weitkamp JH, Wynn JL. Why are preterm newborns at increased risk of infection? Arch Dis Child Fetal Neonatal Ed. 2018;103:F391–F394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanderson E, Yeo KT, Wang AY, et al. ; NICUS Network. Dwell time and risk of central-line-associated bloodstream infection in neonates. J Hosp Infect. 2017;97:267–274. [DOI] [PubMed] [Google Scholar]
- 8.Balla KC, Rao SP, Arul C, et al. Decreasing central line-associated bloodstream infections through quality improvement initiative. Indian Pediatr. 2018;55:753–756. [PubMed] [Google Scholar]
- 9.Mobley RE, Bizzarro MJ. Central line-associated bloodstream infections in the NICU: successes and controversies in the quest for zero. Semin Perinatol. 2017;41:166–174. [DOI] [PubMed] [Google Scholar]
- 10.Wilder KA, Wall B, Haggard D, et al. CLABSI reduction strategy: a systematic central line quality improvement initiative integrating line-rounding principles and a team approach. Adv Neonatal Care. 2016;16:170–177. [DOI] [PubMed] [Google Scholar]
- 11.Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. 2016;16:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shepherd IA, Kelly CM, Skene FM, et al. Enhancing graduate nurses’ health assessment knowledge and skills using low-fidelity adult human simulation. Simul Healthc. 2007;2:16–24. [DOI] [PubMed] [Google Scholar]
- 13.Bloodstream infection event (central line-associated bloodstream infection and non-central line associated bloodstream infection). National Healthcare Safety Network Patient Safety Component Manual. 2019:3–45. [Google Scholar]
- 14.Edwards JR, Peterson KD, Andrus ML, et al. National Healthcare Safety Network (NHSN) Report; data summary for 2006; issued June 2007. Am J Infect Control. 2007;35:290–301. [DOI] [PubMed] [Google Scholar]
- 15.Martin LA, Mate K. IHI innovation system. IHI White Paper; 2018. [Google Scholar]
- 16.Jurecko L, M.D. Kamishibai Card Rounding Helps Prevent Hospital Acquired Infections. Children’s Hospitals Today. Vol Summer 2015: Children’s Hospital Association; 2015. [Google Scholar]
- 17.Bennett D. “K Cards” put focus on safety. The Q Report. Vol Fall 2016: University of Florida Health; 2016. [Google Scholar]
- 18.Shea G, Smith W, Koffarnus K, et al. Kamishibai cards to sustain evidence-based practices to reduce healthcare-associated infections. Am J Infect Control. 2019;47:358–365. [DOI] [PubMed] [Google Scholar]
- 19.Steiner M, Langgartner M, Cardona F, et al. Significant reduction of catheter-associated blood stream infections in preterm neonates after implementation of a care bundle focusing on simulation training of central line insertion. Pediatr Infect Dis J. 2015;34:1193–1196. [DOI] [PubMed] [Google Scholar]
- 20.Lyren A, Brilli RJ, Zieker K, et al. Children’s hospitals’ solutions for patient safety collaborative impact on hospital-acquired harm. Pediatrics. 2017;140:e20163494. [DOI] [PubMed] [Google Scholar]
- 21.Lyren A, Coffey M, Shepherd M, et al.; SPS Leadership Group. We will not compete on safety: how children’s hospitals have come together to hasten harm reduction. Jt Comm J Qual Patient Saf. 2018;44:377–388. [DOI] [PubMed] [Google Scholar]
- 22.Reed T, Pirotte M, McHugh M, et al. Simulation-based mastery learning improves medical student performance and retention of core clinical skills. Simul Healthc. 2016;11:173–180. [DOI] [PubMed] [Google Scholar]
- 23.Goudie A, Dynan L, Brady PW, et al. Attributable cost and length of stay for central line-associated bloodstream infections. Pediatrics. 2014;133:e1525–e1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zachariah P, Furuya EY, Edwards J, et al. Compliance with prevention practices and their association with central line-associated bloodstream infections in neonatal intensive care units. Am J Infect Control. 2014;42:847–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Furuya EY, Dick AW, Herzig CT, et al. Central line-associated bloodstream infection reduction and bundle compliance in intensive care units: a national study. Infect Control Hosp Epidemiol. 2016;37:805–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen R, Gesser-Edelsburg A, Singhal A, et al. Deconstruction of central line insertion guidelines based on the positive deviance approach-Reducing gaps between guidelines and implementation: A qualitative ethnographic research. PLoS One. 2019;14:e0222608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allen GB, Miller V, Nicholas C, et al. A multitiered strategy of simulation training; kit consolidation; and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control. 2014;42:643–648. [DOI] [PubMed] [Google Scholar]
- 28.Page J, Tremblay M, Nicholas C, et al. Reducing oncology unit central line-associated bloodstream infections: initial results of a simulation-based educational intervention. J Oncol Pract. 2016;12:e83–e87. [DOI] [PubMed] [Google Scholar]
- 29.Zingg W, Cartier V, Inan C, et al. Hospital-wide multidisciplinary; multimodal intervention programme to reduce central venous catheter-associated bloodstream infection. PLoS One. 2014;9:e93898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halamek LP, Cady RAH, Sterling MR. Using briefing; simulation and debriefing to improve human and system performance. Semin Perinatol. 2019;43:151178. [DOI] [PubMed] [Google Scholar]
- 31.Massoth C, Röder H, Ohlenburg H, et al. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ. 2019;19:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garvey AA, Dempsey EM. Simulation in neonatal resuscitation. Front Pediatr. 2020;8:59. [DOI] [PMC free article] [PubMed] [Google Scholar]