Background
A common sequela of post-stroke hemiplegia is shoulder pain accompanied by decreased range of motion (ROM) and muscle spasticity.1,2 Many therapies have been used for post-stroke shoulder pain but all are limited in their effectiveness.1 Although acupuncture has been reported to be effective for post-stroke shoulder pain, its mechanisms are unclear.3 We explored the use of acupuncture in a patient with post-stroke shoulder pain and muscle spasticity that was documented by surface electromyography (sEMG).
Case report
A 52-year-old Japanese female, who provided informed consent, was the subject of this care report. She was 6 months post-stroke secondary to a bleed in the right putamen and had right-sided incomplete paralysis. After a course of rehabilitation therapy, she had recovered right shoulder abduction to 90°. As her ROM increased, she developed pain inferior to the right acromion with shoulder abduction to 90°. She also complained of tightness at the location of her right pectoralis major muscle with abduction.
Acupuncture treatment
The patient was treated once a week using a retaining needle technique until the seventh treatment. Needles (0.14 mm diameter) were inserted to a depth of up to 10 mm at the following traditional acupuncture points: LI4, LI10, LI11, TE5 and TE10 in the right arm; and GB21, SI14 and BL18 bilaterally at the shoulder and the trunk. Her complaints were slightly reduced with improvement in shoulder abduction to 120° after each treatment, but abduction had regressed to 90° by the next treatment.
Therefore, we used sEMG to assess the involved muscles before the eighth treatment. We found excessive electrical activity in the right levator scapulae at rest and the right pectoralis major during shoulder abduction, compared to the same muscles on the unaffected left side (Figure 1(a) and (b)). To suppress the excessive moto neuronal activity to these muscles, which we inferred was the cause of glenohumeral malalignment and pain,2 we then inserted needles directly into the (five to seven) tender and indurated areas of these muscles. We used strong manual needle manipulation (a sparrow pecking technique and a bidirectional rotating technique). For the treatment, the patient was asked to maintain a position that elicited maximal shoulder pain.
Figure 1.
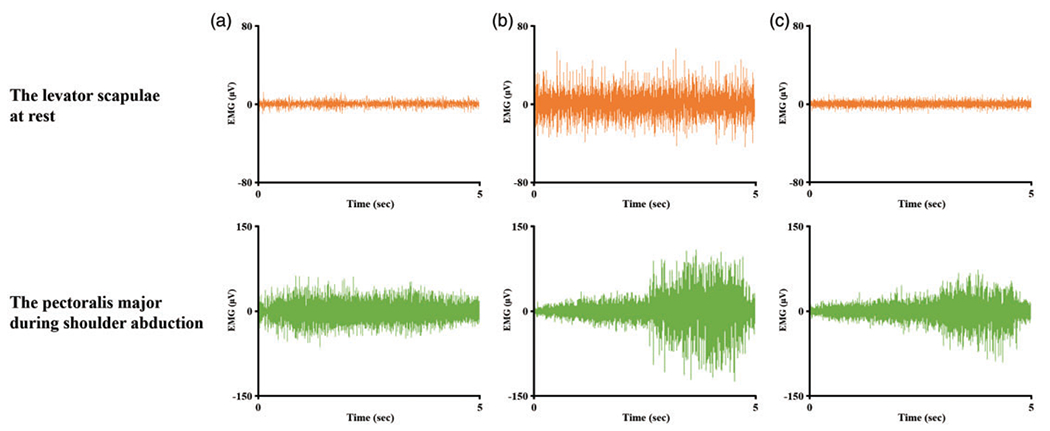
Surface electromyography (sEMG) of the levator scapulae and pectoralis major was recorded (Neuropack X1, MEB-2306; Nihon Kohden Corporation, Japan) using disposable silver/silver chloride bipolar surface electrodes (NSC electrode, NM-317Y3; Nihon Kohden Corporation, Japan) applied to the muscle belly of each muscle. During the electromyographic examination, the patient was sitting upright with her eyes closed. Software for sEMG (LabChart Pro8 AD Instruments, Japan) was used. The grounding electrodes were placed on the subject’s skin at the acromion and mid-clavicular area. Electrical signals were amplified, recorded and digitized with the main unit of the DC-230B of Neuropack X1. The root mean square values (in μV) were used as indices of the signal amplitude. Three consecutive sEMG rest position and shoulder abduction tracks, with a duration of 5 s each, were obtained: (a) unaffected (left) side before acupuncture; (b) affected (right) side before acupuncture; and (c) affected (right) side after acupuncture.
Findings
After acupuncture, electrical activity of the right levator scapulae at rest and the right pectoralis major during shoulder abduction was reduced (Figure 1(c)) to a similar level as the same muscles on the unaffected side. The sEMG integrated value for the levator scapulae at rest decreased from 26.9 to 6.25 μV s and for the pectoralis major during shoulder abduction decreased from 200.9 to 131.3 μVs. Before the eighth treatment, shoulder pain was 58 mm on a visual analogue scale (VAS, where 0 = no pain and 100 = worst pain) with 90° abduction; post-treatment it was 44 mm on the VAS with 150° abduction. The patient also admitted to reduce tightness of the right pectoralis major with abduction.
For the ninth treatment, pre-acupuncture shoulder abduction was maintained at 120° and improved to 150° after the treatment; abduction was maintained at 150° thereafter.
Commentary
This patient’s shoulder pain likely arose from impingement of the head of the humerus and the acromion due to glenohumeral malalignment with excessive activity in the levator scapulae and pectoralis major. Direct and more intense stimulation with needle insertion into these muscles likely inhibited excessive moto neuronal activity, which normalized muscle activity that might promote external rotation of the humerus and scapula. This would be expected to alleviate post-stroke shoulder pain. sEMG is a useful tool to objectively examine the origin of musculoskeletal pain with excessive motoneuronal activity and to examine the acupuncture mechanisms involved in pain reduction.
It is important, in light of the opioid crisis,4 to consider not only the adverse effects associated with the use of opioids and antispasmodics but also the side effects of non-steroidal anti-inflammatory drugs.1,5 An increase in shoulder abduction and reduction of pain concomitant with the normalization of excessive sEMG activity may justify the use of acupuncture as an intervention that has few side effects3 as the first-line option to treat post-stroke shoulder pain, although controlled clinical studies are required to further evaluate its potential use.
Funding
This publication was made possible with a grant from the National Institutes of Health, National Institute of Child Health and Human Development (NICHD) (grant no. R01HD091210). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NICHD. The final peer-reviewed manuscript is subject to the National Institutes of Health Public Access Policy.
Footnotes
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Treister AK, Hatch MN, Cramer SC, et al. Demystifying post-stroke pain: from etiology to treatment. PM&R 2017; 9(1): 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohannon RW, Larkin PA, Smith MB, et al. Shoulder pain in hemiplegia: statistical relationship with five variables. Arch Phys Med Rehabil 1986; 67(8): 514–516. [PubMed] [Google Scholar]
- 3.Lee GE, Son C, Lee J, et al. Acupuncture for shoulder pain after stroke: a randomized controlled clinical trial. Eur J Integr Med 2016; 8(4): 373–383. [Google Scholar]
- 4.DeWeerdt S. Tracing the US opioid crisis to its roots. Nature 2019; 573(7773): S10–S12. [DOI] [PubMed] [Google Scholar]
- 5.Zorowitz RD, Smout RJ, Gassaway JA, et al. Usage of pain medications during stroke rehabilitation: the Post-Stroke Rehabilitation Outcomes Project (PSROP). Top Stroke Rehabil 2005; 12(4): 37–49. [DOI] [PubMed] [Google Scholar]


