Abstract
Background
Sagittal imbalance can be caused by various etiologies and is among the most important indicators of spinal deformity. Sagittal balance can be restored through surgical intervention based on several radiographic measures. The purpose of this study is to review the normal parameters in the sitting position, which are not well understood and could have significant implications for non-ambulatory patients.
Methods
A systematic review was performed adhering to PRISMA Guidelines. Using R-software, the weighted means and 95% confidence intervals of the radiographic findings were calculated using a random effect model and significance testing using unpaired t-tests.
Results
10 articles with a total of 1066 subjects reported radiographic measures of subjects with no spinal deformity in the sitting and standing position. In the healthy individual, standing sagittal vertical axis −16.8°was significantly less than sitting 28.4° (p < 0.0001), while standing lumbar lordosis 43.3°is significantly greater than sitting 21.3° (p < 0.0001). Thoracic kyphosis was not significantly different between the two groups (p = 0.368). Standing sacral slope 34.3° was significantly greater than sitting 19.5° (p < 0.0001) and standing pelvic tilt 14.0° was significantly less than sitting 33.9° (p < 0.0001).
Conclusions
There are key differences between standing and sitting postures, which could lead to undue stress on surgical implants and poor outcomes, especially for non-ambulatory populations. There is a need for more studies reporting sitting and standing radiographic measures in different postures and spinal conditions.
Keywords: Spine, Sagittal alignment, Imaging
Highlights
-
•
Sagittal imbalance is a major cause of spinal deformity.
-
•
Normal characteristics in the sitting posture are rarely studied.
-
•
A set standard for normal sitting radiographic measurements is essential.
-
•
Standing and sitting positions differ significantly in radiographic assessments.
-
•
Radiographic differences in postures can lead to undue stress on surgical implants.
1. Introduction
The sagittal balance of a patient plays an important role in the health of the spine and is an indicator of the severity of spinal deformity [[1], [2], [3]]. Sagittal imbalance can be caused by various etiologies such as ankylosing spondylitis, degenerative conditions, and traumatic injury. It can lead to pain and difficulty with ambulation [4]. A goal of spinal deformity correction surgery is to restore sagittal balance guided by radiographic measurements in order to achieve optimal clinical improvements. Using standing radiographs, the standard modality, sagittal vertical axis (SVA), pelvic tilt (PT), sacral slope (SS), pelvic incidence (PI), thoracic kyphosis (TK), and lumbar lordosis (LL) are commonly measured for reference [5].
SVA is a measure of global spinal balance and represents the distance between a C7 vertical plumb line and the superior posterior corner of S1 [5]. A positive sagittal balance passes >2 cm in front of the superior posterior corner of S1 with >5 cm being abnormal [4,5], and while this method is not without criticism [5,6], it has been correlated with clinical symptoms [4]. PT is the magnitude in which the pelvis rotates around the femoral heads while SS characterizes the S1 endplate position and these values comprise PI (PI = PT + SS) which is anatomically fixed, specific for each individual, and solidified after adolescence [5,7]. Realignment of the lumbar spine to PI has been shown to improve outcomes [8,9], and PT and SS are clinical predictors as well [5,[10], [11], [12]]. LL has typically been measured from L1-S1 while TK varies but is generally measured from T1-12 or T5-12. The inflection point, which is the transition from TK to LL, has traditionally been T12-L1, but is now known to vary based on PI [7,13]. The SRS-Schwab classification [14], uses coronal curve type and a combination of the above radiological measurements including a PI-LL modifier, PT modifier, and global balance SVA modifier to plan for spinal surgery and has been correlated to health-related quality of life [5,15].
Changes in lifestyle, technology, environment, and population age have led to a considerable increase in time spent in the sitting position. There is a paucity in the literature regarding normal parameters in the sitting position, especially among non-ambulatory patients. The impact on lumbar alignment and pelvic compensation in sagittal balance has not been fully defined [[16], [17], [18], [19]]. For example, there is spinal straightening and pelvic retroversion upon sitting [20,21] owing to a general decrease in LL and an increase in PT [22,23]. This would indicate that spinal fusion based on standing sagittal radiographs alone would place the spine under undue stress in the sitting position [3,20]. Despite this, standing radiograph remains the standard for determining severity and approach to spinal deformity [13,18,24].
Recently, studies in populations of total hip arthroplasty [[25], [26], [27], [28], [29], [30], [31], [32], [33]], adult spinal deformity [34], lumbar degenerative diseases [18,19,22], and lumbosacral fusion [23,35] have begun to employ standing versus sitting radiographic analysis with several groups showing significant differences in these classic radiographic measurements. However, these studies primarily look at the difference in measurements from sitting to standing and correlate to disease severity or pre- and post-operation. Studies in healthy populations are now emerging that show significant changes in measures between sitting and standing radiograph markers that may even be influenced by age, gender, and other modifications in body position [3,12,17,20,[36], [37], [38], [39], [40]]. Additionally, work is being performed in the artificial neural network space to predict sitting measures based on standing radiographs to inform surgical correction [[41], [42], [43]]. Therefore, the goal of this review is to understand the literature discussing sitting radiographs to be able to create a more informed approach to evaluating surgical goals.
2. Methods
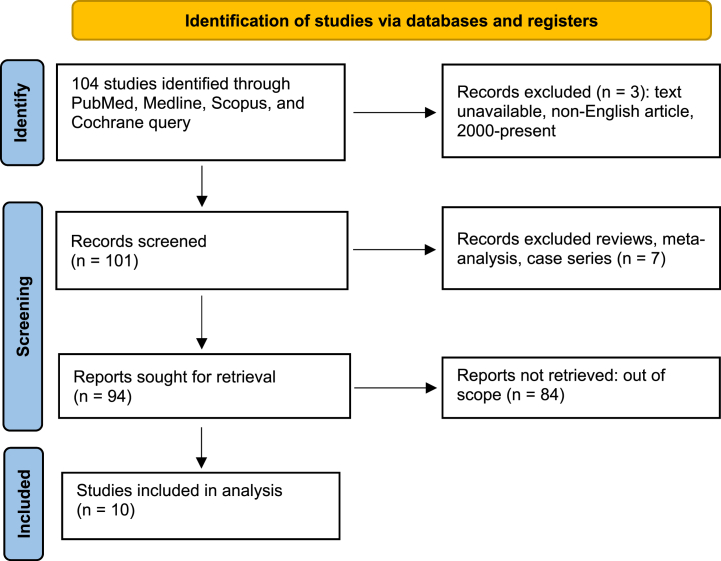
A systematic review was performed adhering to PRISMA Guidelines (Fig. 1). The PUBMED, MEDLINE, Scopus, Cochrane, Web of Science, and Google Scholar databases were searched for studies describing radiographic measures following sitting radiographic imaging. The keywords “sitting”, “standing”, “sagittal alignment”, and “sagittal balance” were used. All studies, since 2000, with radiographic outcomes for normal or healthy controls were included. The outcomes that were of interest included: sagittal vertical axis (SVA), thoracic kyphosis (TK), lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), and pelvic incidence (PI). Meta-analyses, systematic reviews, and other literature reviews were excluded but utilized for citation matching for studies that met our inclusion criteria. Exclusion criteria were based on the scope of the article and limitations in data. Using R-software, the weighted means and 95% confidence intervals (CI) of the radiographic findings in the normal or healthy group were calculated using a random effect model with the metamean package. The data are presented as mean [95% CI]. Unpaired t-tests were used to determine significant differences between standing and sitting groups. For age, the t-score of the Pearson correlation coefficient for each radiographic measure. For all these non-randomized studies, the Newcastle Ottawa Scale (NOS) was used for quality assessment [41].
Fig. 1.
Primsa flowchart.
3. Results
3.1. Characteristics of included trials
We gathered radiographic data from the literature that presented normal spinal measurements [3,[36], [37], [38],40,42,[44], [45], [46], [47]]. Ten articles were found to publish sitting and standing radiographic measures with a total sample size of 1066 subjects. The quality assessment for each study is presented in Supplementary Table 1. The median age of all studies was 34.4 years old.
3.2. Sagittal radiographic measures
From the random effects model, in the normal or healthy individual, we found that standing SVA (−16.8 [−32.7; −0.8]) was significantly less than sitting SVA (28.4 [17.4; 39.5]), p < 0.0001. Standing LL (43.3 [38.0; 48.5]) is greater than sitting LL (21.3 [16.8; 25.8]), p < 0.0001. Standing TK was not significantly greater than sitting TK, p = 0.368.
3.3. Pelvic radiographic measures
Standing PI (47.2 [46.3; 48.0]) and sitting PI (47.3[43.7; 50.9]) are not significantly different, p = 0.9114. For the pelvic radiographic findings, standing SS (34.3 [32.9; 35.7]) was significantly greater than sitting SS (19.5 [16.9; 21.9]), p < 0.0001. Standing PT (14.0 [11.0; 17.0]) was significantly less than sitting PT (33.9 [27.4; 40.5]), p < 0.0001. (Table 1, Table 2, Table 3).
Table 1.
Sagittal radiographic outcomes for normal group.
| Author | # Patients | Age mean (SD) | Standing mean (SD) |
Sitting mean (SD) |
||||
|---|---|---|---|---|---|---|---|---|
| SVA | TK | LL | SVA | TK | LL | |||
| Zhao et al., 202242 | 145 | 23.1 (2.3) | −20.1 (22.4) | 26.1 (10.2) | 50.4 (10.0) | 26.9 (10.2) | 20.0 (8.9) | 25.3 (11.8) |
| Zhou et al., 20203 | 140 | 23.2 (2.6) | −20.5 (20.8) | 26 (10.3) | 50.5 (9.4) | 25 (26.3) | 20.1 (8.7) | 25.5 (11.6) |
| Zhou et al., 20203 | 95 | 53.3 (6.2) | −9 (25.4) | 34 (9.6) | 51.7 (10.5) | 33.7 (21) | 29.3 (10.2) | 38.3 (11.6) |
| Nishida et al., 202044 | 113 | 45.2 | – | 24.1 (8.4) | 35.6 (9.6) | – | 22.8 (8.2) | – |
| Maekawa 201945 | 105 | 33.3 (8.4) | – | – | 49.3 (14.2) | – | – | 23.3 (13.4) |
| Maekawa 201945 | 80 | 61.6 (5.4) | – | – | 40.8 (11.5) | – | – | 24.9 (16.2) |
| Maekawa 201945 | 68 | 75.6 (4.6) | – | – | 42.1 (14.1) | – | – | 27.1 (14.8) |
| Chevillotte 201846 | 15 | 42.9 | – | – | 54.8 (9.8) | – | – | 15.9 (14.6) |
| Suzuki et al., 201838 | 25 | 26.9 (6.3) | – | – | 31.9 (10.4) | – | – | 7.9 (10.8) |
| Suzuki et al., 201640 | 73 | 34.4 (8.1) | – | – | 31.3 (10.4) | – | – | 15.5 (10.1) |
| Suzuki et al., 201640 | 107 | 67.6 (8.3) | – | – | 26.6 (12.8) | – | – | 16.0 (13.9) |
| Cho et al., 201547 | 30 | 31.1 (1.9) | – | – | 47.1 (0.5) | – | – | 17.7 (4.4) |
| Lee et al., 201437 | 10 | 25.4 (2.3) | – | – | 52.8 (7.9) | – | – | 13.5 (11.6) |
| Lee et al., 201437 | 10 | 66.7 (1.7) | – | – | 53.9 (15.9) | – | – | 27.9 (9.3) |
| Endo et al., 201236 | 50 | 31.5 (7.4) | – | – | 33.3 (11.2) | – | – | 16.7 (11.2) |
| Weighted Average (mean [95% CI]) | −16.8 [-32.7; −0.8] | 27.5 [20.6; 34.5] | 43.3 [38.0; 48.5] | 28.4 [17.4; 39.4] | 23.0 [16.1; 29.9] | 21.3[16.8; 25.7] | ||
Table 2.
Pelvic radiographic outcomes for normal group.
| Author | # Patients | Age mean (SD) | Standing mean (SD) |
Sitting mean (SD) |
||||
|---|---|---|---|---|---|---|---|---|
| SS | PT | PI | SS | PT | PI | |||
| Zhao et al., 202242 | 145 | 23.1 (2.3) | 34.9 (7.1) | 11.8 (6.5) | 46.6 (9.1) | 19.7 (8.7) | 28.4 (10.0) | 48.0 (9.1) |
| Zhou et al., 20203 | 140 | 23.2 (2.6) | 35.4 (7) | 11.9 (6.2) | 47.2 (9) | 19.7 (8.5) | 28.1 (9.9) | – |
| Zhou et al., 20203 | 95 | 53.3 (6.2) | 34.3 (8.8) | 14.2 (7) | 48.6 (9.7) | 28.2 (9.3) | 20.4 (10.4) | – |
| Nishida et al., 202044 | 113 | 45.2 | 32.6 (8.3) | 14.4 (7.3) | 47.0 (9.25) | 16.6 (9.4) | 65.17 (8.24) | – |
| Maekawa 201945 | 105 | 33.3 (8.4) | 34.6 (7.7) | 19.7 (16.4) | – | 18.1 (10.1) | 32.5 (12.7) | – |
| Maekawa 201945 | 80 | 61.6 (5.4) | 31.3 (8.5) | 22.2 (15.1) | – | 18.8 (10.1) | 33.3 (14.0) | – |
| Maekawa 201945 | 68 | 75.6 (4.6) | 31.6 (8.9) | 24.3 (15.8) | – | 20.1 (9.6) | 33.2 (14.7) | – |
| Chevillotte 201846 | 15 | 42.9 | 37.1 (6.3) | 12.1 (6.3) | 49.3 (8.1) | 11.3 (10.8) | 37.7 (10.4) | 48.7 (7.9) |
| Suzuki et al., 201640 | 73 | 34.4 (8.1) | 36.4 (7.2) | 10.3 (7.3) | – | 19.0 (9.7) | 27.6 (10.5) | – |
| Suzuki et al., 201640 | 107 | 67.6 (8.3) | 32.6 (8.6) | 15.3 (7.3) | – | 21.2 (10.9) | 27.5 (10.9) | – |
| Lee et al., 201437 | 10 | 25.4 (2.3) | – | 8 (2.2) | 45 (7.1) | – | 40.3 (10.9) | – |
| Lee et al., 201437 | 10 | 66.7 (1.7) | – | 11.4 (7.2) | 50.1 (9.3) | – | 37.3 (9.1) | – |
| Endo et al., 201236 | 50 | 31.5 (7.4) | 37.2 (7.1) | 8.6 (5.5) | 46.3 (8.5) | 18.5 (10.9) | 30.9 (10) | 45.7 (8.2) |
| Weighted Average (mean [95% CI]) | 34.3 [32.9; 35.7] | 14.0 [11.0; 17.0] | 47.2 [46.3; 48.0] | 19.5 [16.9; 21.9] | 33.9 [27.4; 40.5] | 47.3[43.7; 50.9] | ||
Table 3.
Significance testing between sitting and standing radiographic measures.
| Radiographic Outcomes | p-value |
|---|---|
| SVA | <0.0001 |
| TK | 0.368 |
| LL | <0.0001 |
| SS | <0.0001 |
| PT | <0.0001 |
| PI | 0.9114 |
3.4. Age
Using a Pearson correlation coefficient, we found that standing SS (r(9) = −0.81, p = 0.002), standing PT (r(11) = 0.69, p = 0.008), and sitting LL (r(13) = 0.60, p = 0.03) were the radiographic measures to have a significant correlation of radiographic measure with age. There were insufficient number of studies to properly evaluate the correlation of age with SVA and sitting PI.
4. Discussion
Sagittal spinal deformities are typically measured via a standing profile. Radiographic findings are measured via a 36 cm standing image using either stitched images or full-standing radiographs. In normal standing posture, TK and LL can be assessed. The improper distribution of this balance can be caused by pathological or age-related spinal deformities, leading to functional disability. The normal values of kyphosis or lordosis are variable across the literature [[48], [49], [50]]. Cervical lordosis (CL) can be 30–50°, TK is 20–50°, and LL is between 31 and 79° [51]. The pelvis and lower limbs are also important components for the proper alignment of the vertebrae. The literature indicates standing SS is about 40°, PI is about 52°, and PT is < 20° [52]. Table 1, Table 2 display findings similar to these reported measures. The spine can compensate for sagittal imbalance with a lumbar lordotic state and increased pelvic tilt to maintain a proper center of gravity [53].
The purpose of this study was to find the differences between standing and sitting radiographic measures while creating a standard reference for all healthy subjects in the literature. The sitting spine has differences in various postural measures compared to standing radiographs. The normal sitting position induces thoracic and lumbar flexion, allowing for pelvic retroversion [38]. As expected, LL is decreased in the sitting position which may affect load sharing and stress distribution on posterior implants, such as pedicle screws [20]. Our findings suggest standing LL is reduced by nearly half. There is the forward displacement of the SVA in the sitting position, which could potentially lead to higher stress concentrations on anterior implants, such as interbody cages or anterior plates. The SS decreases from the standing to the sitting position, which indicates a more horizontal pelvis. PT was found to be increased in all patients in the sitting position compared to the standing position.
The awareness of these drastic changes in most radiographic measures is important in the pre-operative planning of surgical intervention, especially for a non-ambulatory population. To surgically manipulate the spine without these considerations could prevent the natural sitting position and induce undue stress on implants, leading to junctional failure and repeat procedures. Radiographic measures should be compared to the normal criteria established in research such as this systematic review. The major limitation of this analysis is due to the limited number of studies looking at pre-operative vs postoperative changes in sitting vs standing radiographic measures [34,54]. This does not allow us to draw direct conclusions on the impact of these specific changes in sitting and standing radiographic measures on outcomes in various spinal disorders. Another limitation of the manuscript is that we include a wide range of mean ages, 23.1–75.6 years old, in the weighted mean. We did demonstrate that several radiographic measures are significantly correlated with age, which represents a moderating factor in the data. Additionally, the literature has shown differences among upright versus erect sitting postures. When sitting in a natural position, a vague C shape is formed, which can significantly affect the values of various measures [18]. Two studies indicated the use of a natural sitting position [44,46], while the remaining indicated an erect sitting position [3,[36], [37], [38],40,42,45,47]. This was not controlled for in our systematic review and should be a noted limitation.
Conducting a well-controlled and targeted study to increase our understanding of the consequences of radiographic measurements for spinal surgery is critical. To reduce heterogeneity, specific patient categories should be created based on age, spinal condition, and surgical aims. Radiographic measurement techniques with precise parameters and approved measurement instruments should be developed. To achieve consistency and accuracy, standardized patient positioning techniques should be implemented. Incorporating proven outcome measures, such as patient-reported outcomes and functional assessments, will provide a complete picture of the clinical impact. By applying these recommendations, future research will be able to give a thorough understanding of the association between radiographic measurements and surgical outcomes, thereby improving clinical decision-making and patient outcomes across a wide range of spinal disorders and demographics.
5. Conclusion
The spinopelvic relationship is complex. As demonstrated in this systematic review, there are major differences in the standards of reference for sitting and standing radiographs. Assessing radiographic measures in different postures could lead to a better understanding of sagittal balance and influence decision-making during surgery.
Disclosures
The authors have no conflicts of interest.
Conflict of interest
Nothing to disclose.
Data availability statement
All data supporting the findings of this study are available within the manuscript.
CRediT authorship contribution statement
Rajiv Dharnipragada: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Nick Bostrom: Writing – original draft, Methodology, Data curation. Mario Bertogliat: Writing – review & editing, Methodology, Investigation. Lalitha S. Denduluri: Writing – review & editing, Methodology, Investigation, Data curation. Sanjay Dhawan: Writing – review & editing, Writing – original draft, Validation, Supervision. Bryan Ladd: Writing – review & editing, Writing – original draft, Validation, Supervision. Sarah Woodrow: Writing – review & editing, Writing – original draft, Supervision, Conceptualization. Ann M. Parr: Writing – review & editing, Writing – original draft, Validation, Supervision, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e28545.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Schwab F.J., Blondel B., Bess S., et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine. 2013;38(13):E803–E812. doi: 10.1097/BRS.0b013e318292b7b9. [DOI] [PubMed] [Google Scholar]
- 2.Shin E.K., Kim C.H., Chung C.K., et al. Sagittal imbalance in patients with lumbar spinal stenosis and outcomes after simple decompression surgery. Spine J. 2017;17(2):175–182. doi: 10.1016/j.spinee.2016.08.023. [DOI] [PubMed] [Google Scholar]
- 3.Zhou S., Sun Z., Li W., et al. The standing and sitting sagittal spinopelvic alignment of Chinese young and elderly population: does age influence the differences between the two positions? Eur. Spine J. 2020;29(3):405–412. doi: 10.1007/s00586-019-06185-w. [DOI] [PubMed] [Google Scholar]
- 4.Glassman S.D., Berven S., Bridwell K., Horton W., Dimar J.R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30(6):682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 5.Cheung J.P.Y. The importance of sagittal balance in adult scoliosis surgery. Ann. Transl. Med. 2020;8(2):35. doi: 10.21037/atm.2019.10.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roussouly P., Gollogly S., Noseda O., Berthonnaud E., Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine. 2006;31(11):E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]
- 7.Le Huec J.C., Faundez A., Dominguez D., Hoffmeyer P., Aunoble S. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int. Orthop. 2015;39(1):87–95. doi: 10.1007/s00264-014-2516-6. [DOI] [PubMed] [Google Scholar]
- 8.Le Huec J.C., Aunoble S., Philippe L., Nicolas P. Pelvic parameters: origin and significance. Eur. Spine J. 2011;20(Suppl 5):564–571. doi: 10.1007/s00586-011-1940-1. Suppl 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berven S., Wadhwa R. Sagittal alignment of the lumbar spine. Neurosurg. Clin. 2018;29(3):331–339. doi: 10.1016/j.nec.2018.03.009. 29933801. [DOI] [PubMed] [Google Scholar]
- 10.Borkar S.A., Sharma R., Mansoori N., Sinha S., Kale S.S. Spinopelvic parameters in patients with lumbar degenerative disc disease, spondylolisthesis, and failed back syndrome: comparison vis-à-vis normal asymptomatic population and treatment implications. J. Craniovertebral Junction Spine. 2019;10(3):167–171. doi: 10.4103/jcvjs.JCVJS_70_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shin J.K., Lee J.S., Goh T.S., Son S.M. Correlation between clinical outcome and spinopelvic parameters in ankylosing spondylitis. Eur. Spine J. 2014;23(1):242–247. doi: 10.1007/s00586-013-2929-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hey H.W.D., Tan J.H., Ong B., Kumar A., Liu G., Wong H.K. Pelvic and sacral morphology and their correlation with pelvic incidence, lumbar lordosis, and lumbar alignment changes between standing and sitting postures. Clin. Neurol. Neurosurg. 2021;211 doi: 10.1016/j.clineuro.2021.107019. [DOI] [PubMed] [Google Scholar]
- 13.Roussouly P., Gollogly S., Berthonnaud E., Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 14.Schwab F., Ungar B., Blondel B., et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077–1082. doi: 10.1097/BRS.0b013e31823e15e2. [DOI] [PubMed] [Google Scholar]
- 15.Smith J.S., Klineberg E., Schwab F., et al. Change in classification grade by the SRS-Schwab Adult Spinal Deformity Classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine. 2013;38(19):1663–1671. doi: 10.1097/BRS.0b013e31829ec563. [DOI] [PubMed] [Google Scholar]
- 16.Dunstan D.W., Howard B., Healy G.N., Owen N. Too much sitting--a health hazard. Diabetes Res. Clin. Pract. 2012;97(3):368–376. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 17.Sun Z., Zhou S., Jiang S., Zou D., Yu M., Li W. Variations of sagittal alignment in standing versus sitting positions under the roussouly classification in asymptomatic subjects. Global Spine J. 2022;12(5):772–779. doi: 10.1177/2192568220962436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun Z., Zhou S., Wang W., Zou D., Li W. Differences in standing and sitting spinopelvic sagittal alignment for patients with posterior lumbar fusion: important considerations for the changes of unfused adjacent segments lordosis. BMC Muscoskel. Disord. 2020;21(1):760. doi: 10.1186/s12891-020-03777-2. Published 2020 Nov 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kusakabe T., Endo K., Aihara T., et al. Differences in cervical sagittal alignment between the standing and sitting positions. J. Orthop. Sci. 2019;24(6):1005–1009. doi: 10.1016/j.jos.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Hey H.W.D., Teo A.Q.A., Tan K.A., et al. How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J. 2017;17(6):799–806. doi: 10.1016/j.spinee.2016.03.056. [DOI] [PubMed] [Google Scholar]
- 21.Vaughn J.J., Schwend R.M. Sitting sagittal balance is different from standing balance in children with scoliosis. J. Pediatr. Orthop. 2014;34(2):202–207. doi: 10.1097/BPO.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 22.Lazennec J.Y., Clark I.C., Folinais D., Tahar I.N., Pour A.E. What is the impact of a spinal fusion on acetabular implant orientation in functional standing and sitting positions? J. Arthroplasty. 2017;32(10):3184–3190. doi: 10.1016/j.arth.2017.04.051. [DOI] [PubMed] [Google Scholar]
- 23.Wang S., Zhou Q., Xu L., et al. Impact of lumbar fusion on sitting spinopelvic balance: multisegmental versus monosegmental. Clin. Neurol. Neurosurg. 2021;209 doi: 10.1016/j.clineuro.2021.106905. [DOI] [PubMed] [Google Scholar]
- 24.Laouissat F., Sebaaly A., Gehrchen M., Roussouly P. Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur. Spine J. 2018;27(8):2002–2011. doi: 10.1007/s00586-017-5111-x. [DOI] [PubMed] [Google Scholar]
- 25.Lin Y.H., Lin Y.T., Chen K.H., Pan C.C., Shih C.M., Lee C.H. Paradoxical spinopelvic motion: does global balance influence spinopelvic motion in total hip arthroplasty? BMC Muscoskel. Disord. 2021;22(1):974. doi: 10.1186/s12891-021-04865-7. Published 2021 Nov 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buckland A.J., Abotsi E.J., Vasquez-Montes D., Ayres E.W., Varlotta C.G., Vigdorchik J.M. Lumbar spine degeneration and flatback deformity alter sitting-standing spinopelvic mechanics-implications for total hip arthroplasty. J. Arthroplasty. 2020;35(4):1036–1041. doi: 10.1016/j.arth.2019.11.020. [DOI] [PubMed] [Google Scholar]
- 27.Hagiwara S., Orita S., Nakamura J., et al. Impact of spinal alignment and stiffness on impingement after total hip arthroplasty: a radiographic study of pre- and post-operative spinopelvic alignment. Eur. Spine J. 2021;30(9):2443–2449. doi: 10.1007/s00586-020-06589-z. [DOI] [PubMed] [Google Scholar]
- 28.Homma Y., Ishii S., Yanagisawa N., et al. Pelvic mobility before and after total hip arthroplasty. Int. Orthop. 2020;44(11):2267–2274. doi: 10.1007/s00264-020-04688-6. [DOI] [PubMed] [Google Scholar]
- 29.Loppini M., Longo U.G., Ragucci P., Trenti N., Balzarini L., Grappiolo G. Analysis of the pelvic functional orientation in the sagittal plane: a radiographic study with eos 2D/3D technology. J. Arthroplasty. 2017;32(3):1027–1032. doi: 10.1016/j.arth.2016.09.015. 27789098. [DOI] [PubMed] [Google Scholar]
- 30.Ochi H., Baba T., Homma Y., Matsumoto M., Nojiri H., Kaneko K. Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. Eur. Spine J. 2016;25(11):3699–3706. doi: 10.1007/s00586-015-4217-2. [DOI] [PubMed] [Google Scholar]
- 31.Heckmann N., McKnight B., Stefl M., Trasolini N.A., Ike H., Dorr L.D. Late dislocation following total hip arthroplasty: spinopelvic imbalance as a causative factor. J Bone Joint Surg Am. 2018;100(21):1845–1853. doi: 10.2106/JBJS.18.00078. [DOI] [PubMed] [Google Scholar]
- 32.Innmann M.M., Merle C., Gotterbarm T., Ewerbeck V., Beaulé P.E., Grammatopoulos G. Can spinopelvic mobility be predicted in patients awaiting total hip arthroplasty? A prospective, diagnostic study of patients with end-stage hip osteoarthritis. Bone Joint Lett. J. 2019;101-B(8):902–909. doi: 10.1302/0301-620X.101B8.BJJ-2019-0106.R1. [DOI] [PubMed] [Google Scholar]
- 33.Haffer H., Wang Z., Hu Z., Muellner M., Hipfl C., Pumberger M. Effect of coronal and sagittal spinal malalignment on spinopelvic mobility in patients undergoing total hip replacement: a prospective observational study. Clin Spine Surg. 2022;35(6):E510–E519. doi: 10.1097/BSD.0000000000001300. [DOI] [PubMed] [Google Scholar]
- 34.Yoshida G., Ushirozako H., Hasegawa T., et al. Preoperative and postoperative sitting radiographs for adult spinal deformity surgery: upper instrumented vertebra selection using sitting C2 plumb line distance to prevent proximal junctional kyphosis. Spine. 2020;45(15):E950–E958. doi: 10.1097/BRS.0000000000003452. [DOI] [PubMed] [Google Scholar]
- 35.Borgeaud T., Le Huec J.C., Faundez A. Pelvic and spinal postural changes between standing-sitting positions following lumbosacral fusion: a pilot study. Int. Orthop. 2022;46(8):1839–1846. doi: 10.1007/s00264-022-05365-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Endo K., Suzuki H., Nishimura H., Tanaka H., Shishido T., Yamamoto K. Sagittal lumbar and pelvic alignment in the standing and sitting positions. J. Orthop. Sci. 2012;17(6):682–686. doi: 10.1007/s00776-012-0281-1. [DOI] [PubMed] [Google Scholar]
- 37.Lee E.S., Ko C.W., Suh S.W., Kumar S., Kang I.K., Yang J.H. The effect of age on sagittal plane profile of the lumbar spine according to standing, supine, and various sitting positions. J. Orthop. Surg. Res. 2014;9(1):11. doi: 10.1186/1749-799X-9-11. Published 2014 Feb 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suzuki H., Endo K., Sawaji Y., et al. Radiographic assessment of spinopelvic sagittal alignment from sitting to standing position. Spine Surg Relat Res. 2018;2(4):290–293. doi: 10.22603/ssrr.2017-0074. Published 2018 Mar 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan F., Zander T., Reitmaier S., Bashkuev M., Schmidt H. How reproducible do we stand and sit? Indications for a reliable sagittal spinal assessment. Clin. Biomech. 2019;70:123–130. doi: 10.1016/j.clinbiomech.2019.08.011. [DOI] [PubMed] [Google Scholar]
- 40.Suzuki H., Endo K., Mizuochi J., et al. Sagittal lumbo-pelvic alignment in the sitting position of elderly persons. J. Orthop. Sci. 2016;21(6):713–717. doi: 10.1016/j.jos.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 41.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010 Sep;25(9):603–605. doi: 10.1007/s10654-010-9491-z. Epub 2010 Jul 22. PMID: 20652370. [DOI] [PubMed] [Google Scholar]
- 42.Zhao M., He Y., Li S., Chen H., Li W., Tian H. An artificial neural network model based on standing lateral radiographs for predicting sitting pelvic tilt in healthy adults. Front Surg. 2022;9 doi: 10.3389/fsurg.2022.977505. Published 2022 Sep. 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.He Y., Zhao M., Xu T., Li S., Tian H., Li W. Novel cross LSTM for predicting the changes of complementary pelvic angles between standing and sitting. J. Biomed. Inf. 2022;128 doi: 10.1016/j.jbi.2022.104036. [DOI] [PubMed] [Google Scholar]
- 44.Nishida N., Izumiyama T., Asahi R., Iwanaga H., Yamagata H., Mihara A., Nakashima D., Imajo Y., Suzuki H., Funaba M., Sugimoto S., Fukushima M., Sakai T. Changes in the global spine alignment in the sitting position in an automobile. Spine J. 2020 Apr;20(4):614–620. doi: 10.1016/j.spinee.2019.11.016. Epub 2019 Dec 9. PMID: 31821889. [DOI] [PubMed] [Google Scholar]
- 45.Maekawa A., Endo K., Suzuki H., Sawaji Y., Nishimura H., Matsuoka Y., Murata K., Takamatsu T., Seki T., Konishi T., Kusakabe T., Aihara T., Yamamoto K. Impact of pelvic incidence on change in lumbo-pelvic sagittal alignment between sitting and standing positions. Eur. Spine J. 2019 Sep;28(9):1914–1919. doi: 10.1007/s00586-019-05891-9. Epub 2019 Mar 11. PMID: 30859390. [DOI] [PubMed] [Google Scholar]
- 46.Chevillotte T., Coudert P., Cawley D., Bouloussa H., Mazas S., Boissière L., Gille O. Influence of posture on relationships between pelvic parameters and lumbar lordosis: comparison of the standing, seated, and supine positions. A preliminary study. Orthop Traumatol Surg Res. 2018 Sep;104(5):565–568. doi: 10.1016/j.otsr.2018.06.005. Epub 2018 Jul 31. Erratum in: Orthop Traumatol Surg Res. 2019 Feb;105(1):197. PMID: 30009961. [DOI] [PubMed] [Google Scholar]
- 47.Cho I.Y., Park S.Y., Park J.H., Kim T.K., Jung T.W., Lee H.M. The effect of standing and different sitting positions on lumbar lordosis: radiographic study of 30 healthy volunteers. Asian Spine J. 2015 Oct;9(5):762–769. doi: 10.4184/asj.2015.9.5.762. Epub 2015 Sep 22. PMID: 26435796; PMCID: PMC4591449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boseker E.H., Moe J.H., Winter R.B., Koop S.E. Determination of "normal" thoracic kyphosis: a roentgenographic study of 121 "normal" children. J. Pediatr. Orthop. 2000;20(6):796–798. doi: 10.1097/00004694-200011000-00019. [DOI] [PubMed] [Google Scholar]
- 49.Bernhardt M., Bridwell K.H. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14(7):717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 50.Hardacker J.W., Shuford R.F., Capicotto P.N., Pryor P.W. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine. 1997;22(13):1472–1480. doi: 10.1097/00007632-199707010-00009. [DOI] [PubMed] [Google Scholar]
- 51.Roussouly P., Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur. Spine J. 2010;19(11):1824–1836. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Royen B.J., Toussaint H.M., Kingma I., et al. Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur. Spine J. 1998;7(5):408–412. doi: 10.1007/s005860050098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schwab F., Patel A., Ungar B., Farcy J.P., Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine. 2010;35(25):2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 54.Nishiyama D., Iwasaki H., Kozaki T., Taniguchi T., Taniguchi W., Harada T., Yamada H. Prediction of pelvic inclination in the sitting position after corrective surgery for adult spinal deformity. Spine Surg Relat Res. 2020 Feb 26;4(3):242–246. doi: 10.22603/ssrr.2019-0119. PMID: 32864491; PMCID: PMC7447342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data supporting the findings of this study are available within the manuscript.