Abstract
Pemphigus is a chronic recurrent disease in dermatology. Although it is not very common, its treatment has been an increasing concern in recent years because it is difficult and long-lasting. At present, there are many papers on pemphigus treatment, and to better understand the research trends and research frontiers of pemphigus treatment, it is necessary to conduct a comprehensive systematic review and analysis. We combined bibliometric and visualization methods to analyze 1365 papers published in the Web of Science database from 1992 to 2022, including basic information about countries, institutions and authors, to gain a general understanding of the treatment of pemphigus. Among them, the United States is the country with the most output, Iran's Tehran University of Medical Sciences is the institution with the most published works, and Ahmed, A. Razzaque of Tufts University is the most influential scholar. In addition, we also learned about the research hotspots and frontiers of pemphigus treatment through a series of analyses on the frequency, clustering, keywords bursts and cited literature, and we briefly reviewed the highly cited literature. We found that the current research focuses in the study of pemphigus treatment are the types, pathogenesis, and treatment of pemphigus, including glucocorticoids, immunosuppressants and many other major treatment methods. Hailey-Hailey disease, genetic susceptibility, and traditional Chinese medicine are potential research hotspots. Rituximab is a research frontier. In conclusion, we hope to provide new research ideas for promoting the development of pemphigus treatment.
Keywords: Bibliometrics, Pathogenesis, Pemphigus, Rituximab, Treatment
1. Introduction
Pemphigus consists of a group of rare and severe autoimmune blistering diseases mediated by pathogenic autoantibodies mainly directed against desmosomal adhesion proteins [1]. According to the clinical manifestations and histopathological changes, the common types of pemphigus are pemphigus vulgaris (PV), pemphigus vegetans, pemphigus foliaceus (PF), and pemphigus erythematosus. PV is considered to be the most common type of pemphigus, accounting for 70% of all cases of pemphigus [2]. In addition, there are some special pemphigus types, including herpetiform pemphigus, drug-induced pemphigus, IgA pemphigus, and paraneoplastic pemphigus (PNP) that is associated with tumors [3,4]. Pemphigus may cause erythema, blisters, erosion, and ulcers, which may affect the skin as well as the mucosal surface of the mouth, eyes, and nose, leading to severe symptoms including pain, dysphagia, and malodor [5]. Epidemiological studies show that the incidence of pemphigus varies by region and race, but the overall incidence is 0.5–32/million per year [[6], [7], [8], [9], [10]]. The morbidity of women is slightly higher than that of men, and the average age of onset is between 40 and 60 years old [[9], [10], [11]]. Because of the large area of skin erosion, massive body fluid extravasation, and excessive loss of proteins, electrolytes and body fluids, pemphigus causes physical weakness, and pemphigus patients easily develop cormorbid sepsis, pneumonia, and other infections [11,12], which are also the main causes of death [13]. According to clinical investigations, therapy of pemphigus may also cause complications such as kidney disease, femoral head necrosis, hypertension, diabetes, and digestive tract diseases [[14], [15], [16]].
The pathogenesis of pemphigus is not yet fully understood. At present, most scholars believe that pemphigus is an autoimmune disease, and it is generally believed that the disease is mediated by autoantibodies to desmosome components. Autoantibodies, mainly IgG4, cause blistering in the epidermis by directly interfering with the interaction of desmosomes and subsequently destroying desmosomes and signaling pathways [17]. In addition, cytokines [18], T cells [19], and microRNAs (miRNAs) [20], among other factors, are also involved in its pathogenic process. There are many predisposing factors for pemphigus, including drugs, hormones, diseases, vaccines, genetic factors, diet, pregnancy, stress and environmental factors [21]. Fig. 1 shows a possible pathogenesis of pemphigus vulgaris.
Fig. 1.
A possible pathogenesis of pemphigus vulgaris.
The strategy of pemphigus treatment is to control the occurrence of new lesions and prevent recurrence. This is accomplished mainly through supportive treatment and drug treatment alongside the prevention and treatment of complications [14]. The general treatment is to provide strong supportive therapy and encourage the consumption of a nutritious and digestible diet. Attention should be given to maintaining the balance of water and electrolytes. Doctors will administer albumin, plasma or whole-blood supportive treatment to patients with systemic failure [22,23]. The main therapeutic drugs are glucocorticoids [24] and immunosuppressants [25], both of which can be used alone or in combination [[26], [27], [28]]. After the application of corticosteroids, cytotoxic drugs and immunobiologic agents with powerful anti-inflammatory and immunomodulatory effects, the mortality of pemphigus patients decreases to 3.3% [[8], [9], [10]]. Anti-infection treatment is required for patients with bacterial infection [29,30]. Pemphigus can also be treated by injecting new biological agents and administering human blood gamma immunoglobulin, immunoadsorption therapy, in vitro photochemical therapy, plasma exchange (PE), etc. [[31], [32], [33]]. How to properly choose these treatments and methods and whether they can be further improved are problems worth exploring.
This article will focus on the relevant bibliometric and visual analyses of pemphigus treatment. Bibliometric analysis has been widely used in literature analyses in recent years. It is a comprehensive knowledge system that integrates mathematics, statistics and philology and focuses on quantification. Analyzing these visual networks makes it possible to understand the direction of the publishing trends and author citation relationships [34]. Therefore, despite the diversity of research topics and publications on pemphigus treatment, bibliometric and visual analysis can help us quickly obtain an understanding of this disease that is based on the massive amount of information in the literature and determine the research hotspots in various periods as well as the future development direction of the discipline. In addition, through these analyses, we can more comprehensively understand which effective therapies can be selected and how to properly select them, and find out the advantages and development of some potential therapies. At the same time, we can also analyze and summarize the existing research results. This article presents the results of a practical, comprehensive and detailed review to provide a reference for future research on pemphigus.
Overall, our article mainly proposes to explore the following questions.
Question1
What effective methods are available for treating or alleviating pemphigus?
Question2
What are the hotspots in research on treatment of pemphigus-related fields in the past 30 years?
Question3
What is the current pioneering research in the field of pemphigus treatment?
Question4
What are the possible future research directions in the field of pemphigus treatment?
2. Data and methods
2.1. Literature retrieval strategy and data collection
In this cross-sectional study, literature information was retrieved from the Web of Science (WOS) (https://www.webofscience.com). The website is rated as the world’s most trusted publisher-independent global citation database. The database we selected is the Web of Science Core Collection (WOSCC), and we selected the Science Citation Index Expanded (SCI-EXPANDED). All searches were completed within one day to prevent any omission due to database updates. The retrieval strategy we selected was (TS=(Pemphigus)) AND TS= (Therapy OR Medicine OR Medication OR Treatment OR Drug); other standards are shown below.
-
(1)
Time span: index date: January 1, 1992 to December 31, 2022
-
(2)
Language: English
-
(3)
Document type: article or review article
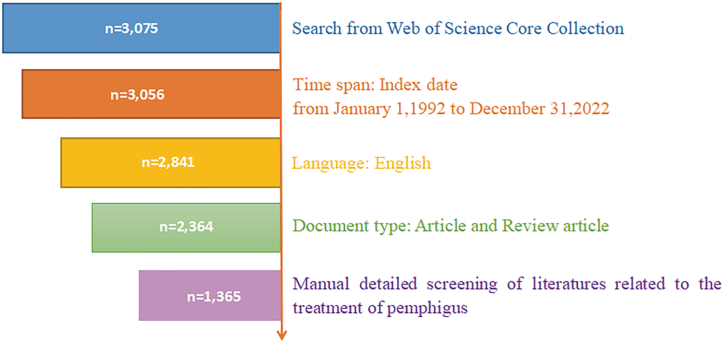
In the preliminary screening, 2364 articles were retrieved. By evaluating the title, abstract, keywords and even content of each article, repeated, withdrawn or unrelated articles were excluded, and 1365 articles were ultimately retained for the next step of literature evaluation and visual analysis. Fig. 2 Illustrates the preliminary screening process. Then, we exported the screening results in the format of a "plain text file" and "tab separated file", and we selected "full records and references" for future use.
Fig. 2.
Literature screening process.
2.2. Data analysis method and network mapping
The bibliometric and visual analysis work of this paper is mainly based on CiteSpace (version 6.1. R3, USA), VOSviewer (version 1.6.18, USA), Scimago Graphics (USA), R (version 4.3.1, USA) and online websites (https://bibliometric.com/app). We uploaded the "tab separated file" type data to the platform to analyze the annual general publishing trend and the annual publishing trend of different countries (Fig. 3), and we imported the data into VOSviewer to generate a national cooperation network modified by Scimago Graphics (Fig. 4). We used the R package “bibliometrix” developed by Massimo Aria and Corrado Cuccurullo to count the number of publications, citations and calculate the h-index for authors [35] (Table 4). The rest of the analysis was completed by CiteSpace using the exported "plain text file" data. Unless otherwise specified, the CiteSpace parameters referred to Li et al. [36].
Fig. 3.
The number of annual publications on the treatment of pemphigus from 1992 to 2022.
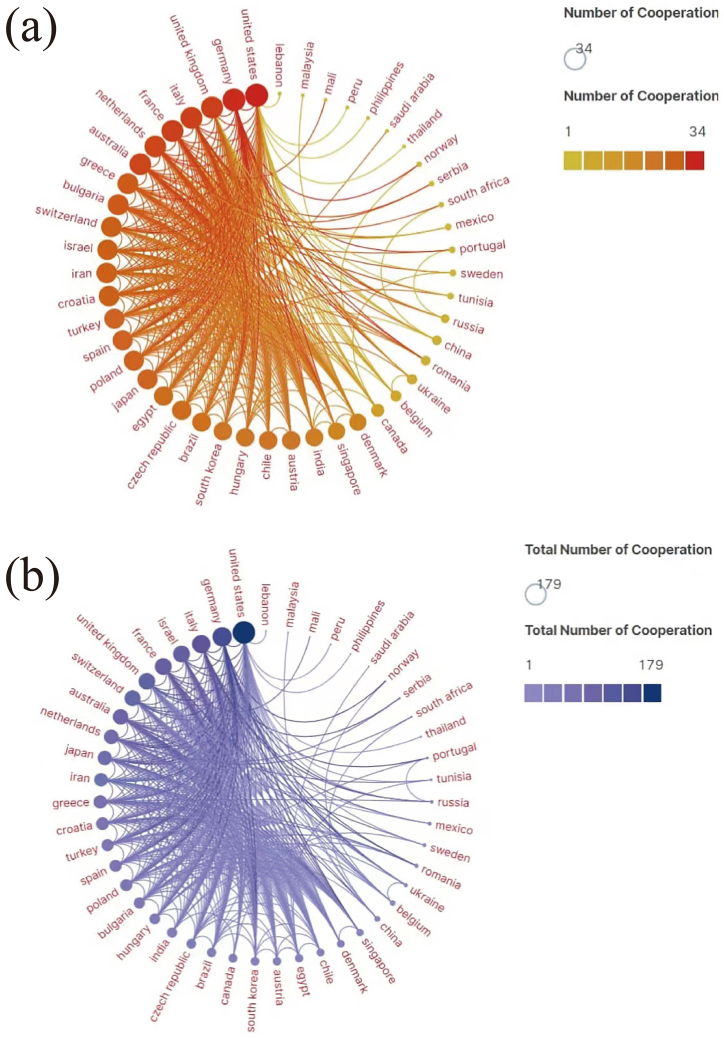
Fig. 4.
(a) Network of cooperation in pemphigus treatment. Each circle represents a country, the size of the circle and the shade of the inner color indicate the number of countries cooperating, and the line represents the cooperative relationship. (b) Network of countries’ cooperation in pemphigus treatment. Each circle represents a country, the size of the circle area and the shade of the inner color represent the total number of countries cooperating, and the lines represent cooperative relationships. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Table 4.
The top 10 authors of publications volume on the treatment of pemphigus from 1992 to 2022.
| Rank | Authors | Publications | H-index | Cited | Affiliations | Countries |
|---|---|---|---|---|---|---|
| 1 | Ahmed, A. Razzaque | 48 | 25 | 1952 | Tufts University | United States |
| 2 | Daneshpazhooh, Maryam | 42 | 15 | 775 | Tehran University of Medical Sciences | Iran |
| 3 | Schmidt, Enno | 40 | 24 | 1966 | University of Luebeck | Germany |
| 4 | Hashimoto, Takashi. | 38 | 19 | 1447 | Osaka City University | Japan |
| 5 | Zillikens, Detlef | 37 | 24 | 2185 | University of Luebeck | Germany |
| 6 | Hertl, Michael | 34 | 25 | 2306 | Philipps University Marburg | Germany |
| 7 | Balighi, Kamran | 31 | 11 | 454 | Tehran University of Medical Sciences | Iran |
| 8 | Joly, Pascal | 30 | 18 | 2083 | Universite de Rouen Normandie | France |
| 9 | Murrell, Dedee F | 26 | 12 | 658 | University of New South Wales Sydney | Sydney, NSW, Australia |
| 10 | Tavakolpour, Soheil | 25 | 11 | 331 | Dana-Farber Cancer Institute | United States |
3. Results
3.1. Analysis of annual publication trends
The annual publication volume of literature related to the treatment of pemphigus shows a steady upward trend as shown in Fig. 3. In 2001, the annual publication volume of literature related to the treatment of pemphigus reached 30 articles for the first time and continued to rise steadily until 2008, with the first significant increase. We evaluated the major events on pemphigus in that year and found that an international pemphigus meeting organized by Drs Bystryn, Luis Diaz, Sergei Grando, and John Stanley that was held at the National Institutes of Health (NIH),which developed a widely accepted pemphigus staging definition, and the reference was published in 2008 [37]. We speculate that this may have stimulated the development of research related to pemphigus. We also noticed another leap in the quantity of publications in 2011. We found that in 2010, “Clinical Dermatology of Traditional Chinese Medicine” and “Dermatology of Traditional Chinese Medicine” were successively published. Therefore, we speculate that this may have inspired scholars from various regions to conduct relevant research to some extent.
In addition, we also determined the top ten countries in terms of number of publications and the year of their first publication (Table 1). It should be noted that due to the cooperation between countries in some articles, the total number of articles in each country exceeds 1365. The United States ranks first, with an overwhelming number of 396 articles from 1992 to 2022, and the year of its first publication also ranks first, demonstrating the absolute dominance of the United States in this field. It is worth mentioning that since 2015, China has also been at the forefront of publishing, especially since 2020; China has become the second largest publishing country after the United States, and the gap is narrowing, indicating an increasing focus on pemphigus in China.
Table 1.
The top 10 countries on publications on treatment of Pemphigus from 1992 to 2022.
| Rank | Counts | Year of first publication | Countries |
|---|---|---|---|
| 1 | 396 | 1992 | United States |
| 2 | 138 | 1994 | Germany |
| 3 | 129 | 1992 | Italy |
| 4 | 108 | 1994 | Japan |
| 5 | 94 | 2006 | Iran |
| 6 | 74 | 1999 | China |
| 7 | 66 | 1995 | India |
| 8 | 59 | 1994 | Israel |
| 9 | 59 | 1995 | United Kingdom |
| 10 | 55 | 1996 | France |
3.2. Analysis of published journals
By analyzing the papers related to pemphigus treatment published in 322 journals, we determined the top ten journals in terms of the number of citations, as shown in Table 2, including publications, the average number of citations, impact factors (IF) in 2022, Journal Citation Reports (JCR) (https//: www.webofscience.com) and publishers. The papers published in these 10 journals accounted for 27.67% of the publications overall. Among them, the Archives of Dermatology changed its name to JAMA Dermatology in 2013, so its IF was counted only until 2014. The IF we present here is the IF after the name change of the journal. According to the number of publications and the total number of citations, the Journal of the American Academy of Dermatology ranked first, with 76 publications and 1773 citations, so this may be an entry point for the study of pemphigus treatment. Second, we also found articles published in two top journals: three articles in the New England Journal of Medicine and four articles in the Lancet, with IF of 158.5 and 168.9, respectively. The IF has become an international universal journal evaluation index. The IF is an index to evaluate not only the usefulness and display of journals but also the academic level of journals and even the quality of papers. The very high IF of these two journals also reflect their authority. Therefore, although these journals have published only three or four articles on pemphigus, the quality of these articles should be very high. It is also worth mentioning that JCR for most journals is now located in Q1, which also reflects their high quality and cutting-edge nature. In addition, Elsevier and Wiley account for 70% of the publishing organizations of these journals, indicating their advantages in this field.
Table 2.
The top ten journals with the most citations on the treatment of pemphigus from 1992 to 2022.
| Rank | Journals | Cited | Publications | Average cited | IF | JCR | Publishers |
|---|---|---|---|---|---|---|---|
| 1 | Journal of the American Academy of Dermatology | 1773 | 76 | 23.33 | 13.8 | Q1 | Elsevier |
| 2 | JAMA Dermatology | 1112 | 43 | 25.86 | 10.9 | Q1 | Amer Medical Assoc |
| 3 | British Journal of Dermatology | 1034 | 54 | 19.15 | 10.3 | Q1 | Wiley |
| 4 | Journal of the European Academy of Dermatology and Venerology | 498 | 49 | 10.38 | 9.2 | Q1 | Wiley |
| 5 | International Journal of Dermatology | 339 | 50 | 6.92 | 3.6 | Q1 | Wiley |
| 6 | Journal of Investigative Dermatology | 333 | 20 | 16.65 | 6.5 | Q1 | Elsevier |
| 7 | New England Journal of Medicine | 314 | 3 | 104.67 | 158.5 | Q1 | Massachusetts Medical Soc |
| 8 | Dermatology | 301 | 36 | 8.36 | 3.4 | Q2 | Karger |
| 9 | Lancet | 301 | 4 | 75.25 | 168.9 | Q1 | Elsevier |
| 10 | Clinical and Experimental Dermatology |
252 | 38 | 6.81 | 4.1 | Q1 | Wiley |
3.3. Analysis of cooperation networks
3.3.1. Countries
The cooperation and exchanges between different countries are of far-reaching significance, and the analysis of cooperative relations can show the influence of countries. Therefore, we combined two tools, VOSviewer and Scimago Graphica, to visually analyze the cooperation between countries. Countries that did not participate in the cooperation were excluded. The results are shown in Fig. 4. Forty-seven out of the fifty-five countries have cooperated internationally in the treatment of pemphigus. The country with the most cooperations is the United States, having partnered with a total of 34 countries, and the second-ranked country is the Germany, cooperating with 33 countries. The United Kingdom and France are tied for third with Italy, cooperating with 31 countries (Fig. 4(a)). Moreover, the United States also shows more enthusiasm in cooperation projects, with 179 collaborations with other countries. Germany ranked second with 134 cooperation projects, and Italy ranked third with 120 cooperation projects (Fig. 4(b)). These results all suggest that we can strengthen country cooperation and exchange with these countries in pemphigus treatment research.
3.3.2. Institutions
In terms of institutional cooperation, 1268 institutions participated in the study of pemphigus treatment. Table 3 lists the top 10 institutions in terms of the total number of publications, including citations, countries and main authors, based on the Web of Science. Tehran University of Medical Sciences has the largest number of publications (68, 1172 citations), and the second- and third-ranked institutions are the University of Pennsylvania (59, 2236 citations) and Harvard University (51, 1603 citations). In addition, 2/5ths of the top 10 institutions and two of the top three institutions are from the United States. This indicates that the United States is more active in research on pemphigus treatment. Besides, combined with the information in Table 3 and the following Table 4, we can see that most of the top ten authors are also the main authors of the top ten institutions. The University of California system is a university system with ten campuses in the United States. It has 38 publications in the field of pemphigus treatment research, with the University of California Davis and University of California Irvine accounting for 18 and 14 publications, respectively. This indicates that these two universities have conducted more research in this area. From the distribution characteristics of institutions, Iran, Germany and Japan have a small and relatively concentrated group of research institutions. In contrast, Italian and Chinese research institutions are not on the list, suggesting that their institutions are likely to be numerous and scattered.
Table 3.
The top 10 institutions of publications volume on the treatment of pemphigus from 1982 to 2022.
| Rank | Institutions | Publications | Cited | Countries | Main authors |
|---|---|---|---|---|---|
| 1 | Tehran University of Medical Sciences | 68 | 1172 | Iran | Balighi, Kamran Daneshpazhooh, Maryam Chams-Davatchi, Cheyda |
| 2 | University of Pennsylvania | 59 | 2236 | United States | Werth, Victoria P Ellebrecht, Christoph T. Stanley, John R. |
| 3 | Harvard University | 51 | 1603 | United States | Tavakolpour, Soheil Christen, William G. Farid, Ali Salehi |
| 4 | University of Lubeck | 48 | 2704 | Germany | Schmidt, Enno Zillikens, Detlef Ludwig, Ralf J. |
| 5 | Kurume University | 39 | 1356 | Japan | Ishii, Norito Koga, Hiroshi Nakama, Takekuni |
| 6 | University of California System | 38 | 1368 | United States | Grando, Sergei A Chernyavsky, Alexander I. Outerbridge, Catherine A. |
| 7 | New England Baptist Hospital | 35 | 1739 | United States | Guercan, Hakan, M Mabrouk, Dalia Malik, M. |
| 8 | Tel Aviv University | 34 | 1121 | Israel | Mimouni, Daniel Hodak, Emmilia Leshem, Yael Anne |
| 9 | Universite de Rouen Normandie | 33 | 2320 | France | Joly, Pascal Calbo, Sebastien Golinski, Marie-Laure |
| 10 | Philipps University Marburg | 31 | 2069 | Germany | Hertl, Michael Pollmann, Robert Moebs, Christian |
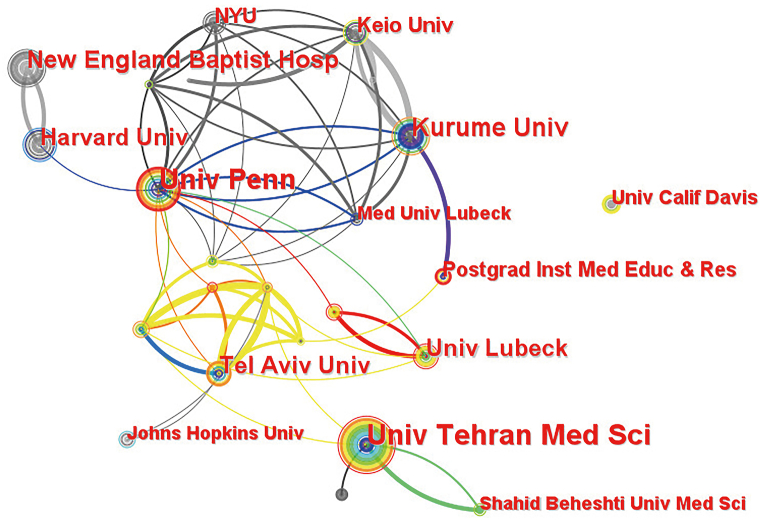
The CiteSpace analysis results of cooperation among institutions are shown in Fig. 5. The cooperation frequency between most institutions with a large number of published articles is not very high, and most of them cooperate with institutions with a small number of published articles. It is interesting to see from Fig. 5 that among four universities in the United States, namely, the University of Pennsylvania, Harvard University, University of California Davis, and New England Baptist Hospital, except for the close cooperation between New England Baptist Hospital and Harvard University, cooperation between these institutions is relatively rare. Moreover, the University of California Davis and the other three institutions never seem to work together.
Fig. 5.
Collaborative network of pemphigus treatment research institutions. Each circle represents an institution. The size of the circle is positively correlated with the number of articles published by the institution, and the thickness of the lines is positively correlated with the frequency of collaboration.
3.3.3. Authors
Based on the calculations of the R package, we ranked the screened articles from the WOS according to the number of relevant studies published by the authors (Table 4). It can be seen from the table that the United States and Germany are in a leading position for this metric. The table lists the top 10 authors with the largest number of articles related to pemphigus treatment. Ahmed, A. Razzaque of Tufts University ranked first with 48 articles. His citation frequency is 1,952, with an h-index of 25. The h-index is a mixed quantitative index that can be used to evaluate the number and level of academic output of researchers. We queried the h-index of these authors by R package. The h-index of all authors is above 10, indicating that their research is of great reference value. In addition, although Hertl, Michael of Germany did not have the highest number of documents on pemphigus treatment, his h-index and total citation frequency are both the highest, reaching 25 and 2306. This also indirectly indicates that the quality of his articles is very high.
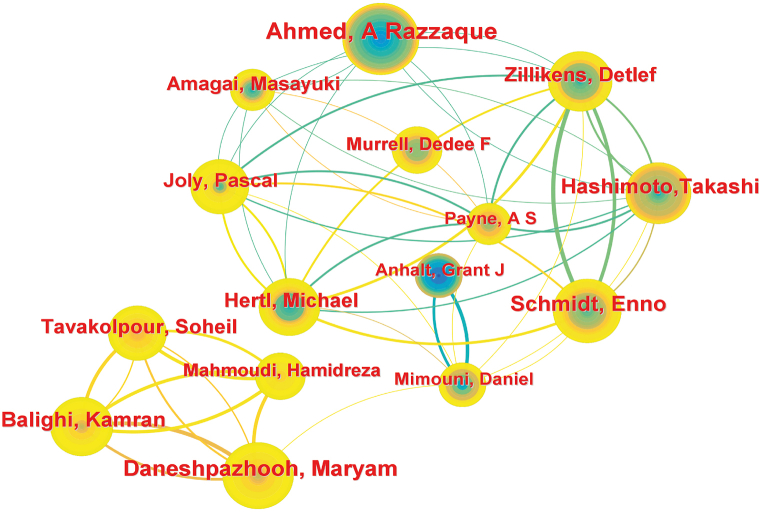
Then, we analyzed the cooperation between different authors. To make the result clearer, we simplified the result diagram as shown in Fig. 6. Among these, we found that most scholars have established cooperative relationships, and their cooperative relationships are intertwined, forming a cluster of interconnections. Because CiteSpace and the WOS process data in different ways, the top ten authors are somewhat different, but this does not affect the overall trend. When analyzing the cooperation between authors, so we retained the top 15 authors in Fig. 6, we used the data presented in CiteSpace (Fig. 6). Among them, Balighi, K., Tavakolpour, S., Mahmoudi, H., and Daneshpazhooh, M. are relatively independent than other authors, but they have had close cooperation with each other in recent years. The other 12 authors have relevant cooperation relationships, and each author has cooperated with at least two other authors, forming a "circle". Hertl, Michael has relevant cooperation relationships with 9 other authors in addition to Hashimoto, Takashi.
Fig. 6.
Top15 authors cooperative relationships in research on pemphigus treatment. Each circle represents an author, the circle size is positively related to the number of articles published by the author, and the thickness of the line is positively related to the degree of cooperation between the authors.
3.4. Analysis of keywords
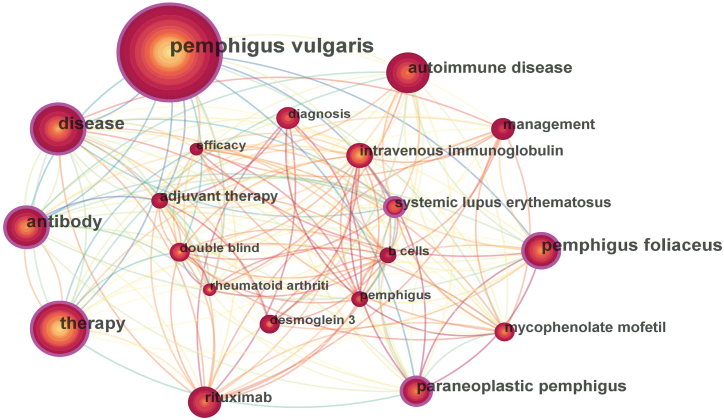
Keywords represent the main content of an article and are the fastest way to obtain the central focus of an article. We used CiteSpace to show the relationship between the keywords of the selected articles. Fig. 7 shows the keywords in CiteSpace. We also used CiteSpace to incorporate keywords, such as merging foliaceus into pemphigus foliaceus and vulgaris into pemphigus vulgaris. The top 20 keywords with the most occurrences are listed in Table 5, and the top 20 keywords are also displayed in Fig. 7 after adjustment. In Fig. 7, it can be seen that there is a very close correlation between the top 20 keywords, with the least demoglein (Dsg) 3 also associated with 8 keywords, and intravenous immunoglobulin (IVIg) having a close correlation with the other 19 keywords. Because the article focuses on the treatment of pemphigus, except for therapy, disease, management, pemphigus, efficacy and diagnosis, among which pemphigus vulgaris, pemphigus foliaceus, paraneoplastic pemphigus are also common types of pemphigus. Antibody, autoimmune disease, B cells and desmoglein (Dsg)3 suggest the nature and pathogenesis of pemphigus. In addition, mycophenolate mofetil (MMF), rituximab, intravenous immunoglobulin and adjuvant therapy are commonly mentioned and used methods and drugs for treating pemphigus, and double blinding is a commonly used experimental method to study their therapeutic effects. Systemic lupus erythematosus and rheumatoid arthritis are similar to pemphigus in certain areas, so it is sometimes necessary to pay attention to distinguishing them. We also clustered the keywords of pemphigus treatment and visualized the clusters using CiteSpace. Keyword clustering can preliminarily reflect the main classification of the content of the articles. We selected the clustering presentation method for the timeline, as shown in Fig. 8. There are 50 types of keyword clusters in the literature we imported, of which the first 10 are shown in Fig. 8, which include #0 foliaceus, #1 rituximab, #2 autoimmune disease, #3 monoclonal antibody rituximab, #4 mycophenolate mofetil, #5 single cycle, #6 term follow up, #7 immune globulin, #8 pemphigus foliaceus, and #9 therapy.
Fig. 7.
The frequency and correlation of top 20 keywords in the treatment of pemphigus research. Each circle represents a subject. The circle size and line thickness are positively related to the frequency of keyword occurrence.
Table 5.
The top 20 keywords related to the treatment of pemphigus from 1992 to 2022.
| Rank | Keywords | Counts | Rank | Keywords | Counts |
|---|---|---|---|---|---|
| 1 | pemphigus vulgaris | 555 | 11 | adjuvant therapy | 70 |
| 2 | therapy | 233 | 12 | systemic lupus erythematosus | 69 |
| 3 | disease | 210 | 13 | intravenous immunoglobulin | 62 |
| 4 | antibody | 206 | 14 | rheumatoid arthriti | 52 |
| 5 | pemphigus foliaceus | 160 | 15 | pemphigus | 51 |
| 6 | autoimmune disease | 147 | 16 | double blind | 46 |
| 7 | paraneoplastic pemphigus | 118 | 17 | efficacy | 44 |
| 8 | mycophenolate mofetil | 90 | 18 | diagnosis | 44 |
| 9 | rituximab | 85 | 19 | B cells | 42 |
| 10 | management | 72 | 20 | desmoglein 3 | 41 |
Fig. 8.
Timeline view of the top 10 largest clusters of citing articles and keywords in the field of pemphigus treatment. The highlighted and thickened timeline indicates that the cluster theme is a hot spot during this period (Q = 0.6444, S = 0.8425).
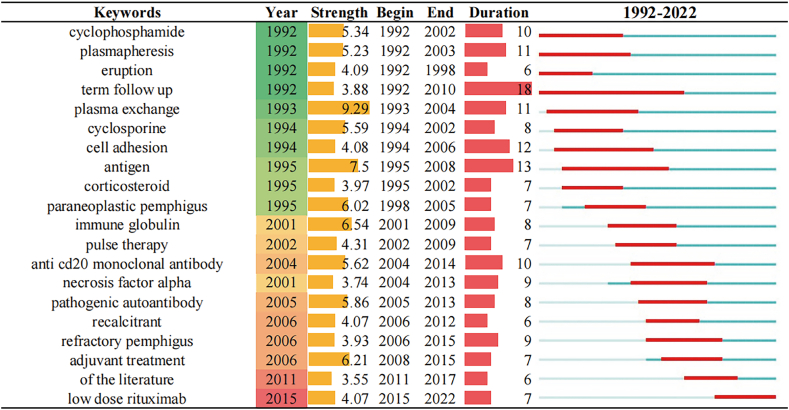
In addition, we also carried out keyword burst analysis in Fig. 9. In a certain period, keywords that are used more often are generally considered hot topics. We also list the top 20 keywords with the strongest bursts, among which PE began to burst in 1993, with a duration of 11 years and ranks first with a burst strength of 9.29. We also noticed that the keywords that appeared after 1995 were rarely able to burst for more than 10 years, while before 1995, they were more common, and even term follow up burst for 18 years from 1992 to 2010, which not only reflects the importance of long term follow up for the study of disease treatment but also indicates that with the development of the times, the changes in hotspots may also accelerate. In addition, antigen has the highest burst strength except for PE, and its burst duration is second only to term follow-up, reaching 13 years, which also reflects people’s attention to the pathogenesis of pemphigus. It is also worth noting that rituximab has burst since 2015 and is still a hot topic of discussion. According to this point, we searched the literature related to rituximab in the screened literature, with a total of 376 articles, of which the literature from 2015 to now accounted for 59.6%, and rituximab was also in the top ten keywords, which shows that rituximab plays an important role in the field of pemphigus treatment.
Fig. 9.
Top 20 keywords with the strongest citation bursts. The time period marked in red indicates a sudden increase in the frequency of keyword use during this period. Blue indicates a period of relative unpopularity. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
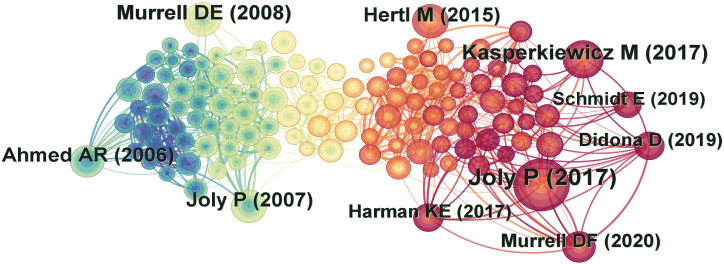
3.5. Analysis of the reference co-citation network
The co-citation analysis of literature was first proposed by the American intelligence scientist Small, Henry in 1973 [38]. CiteSpace was used for the citation analysis of co-cited literature to obtain the interactive network of these documents (Fig. 10) and the 10 studies with the highest number of citations (Table 6). After adjustment, we showed authors and years of the top 10 most-cited articles are shown in Fig. 10. Our analysis of them found that these articles could be roughly divided into two categories: clinical trials and treatment guidelines. These articles provide a solid and clear basis for the clinical treatment of pemphigus and contribute to other studies of pemphigus. Therefore, we hoped to find landmark studies with great significance in the treatment of pemphigus through literature co-citation analysis.
Fig. 10.
Network of co-cited references in the treatment of pemphigus. Each circle represents a citation, the size of the circle is positively correlated with the number of citations, and the link between the two circles represents two references cited in the same article.
Table 6.
The top 10 most highly cited documents in the field of pemphigus treatment.
| Rank | First authors | Title and Publication year | Citations | DOI | Journals |
|---|---|---|---|---|---|
| 1 | Joly, P | First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial (2017) | 154 | 10.1016/S0140-6736(17)30070-3 | Lancet |
| 2 | Kasperkiewicz, M | Pemphigus (2017) | 82 | 10.1038/nrdp.2017.26 | Nature Reviews Disease Primers |
| 3 | Murrell, DF | Diagnosis and management of pemphigus: Recommendations of an international panel of experts (2020) | 66 | 10.1016/j.jaad.2018.02.021 | Journal of the American Academy of Dermatology |
| 4 | Hertl, M | Pemphigus. S2 Guideline for diagnosis and treatment - guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV) (2015) | 59 | 10.1111/jdv.12772 | Journal of the European Society of Dermatology and Venereology |
| 5 | Murrell, DE | Consensus statement on definitions of disease, end points, and therapeutic response for pemphigus (2008) | 56 | 10.1016/j.jaad.2008.01.012 | Journal of the American Academy of Dermatology |
| 6 | Joly, P | A single cycle of rituximab for the treatment of severe pemphigus (2007) | 54 | 10.1056/NEJMoa067752 | New England Journal of Medicine |
| 7 | Ahmed, AR | Treatment of pemphigus vulgaris with rituximab and intravenous immune globulin (2006) | 53 | 10.1056/NEJMoa062930 | New England Journal of Medicine |
| 8 | Harman, KE | British Association of Dermatologists' guidelines for the management of pemphigus vulgaris 2017(2017) | 50 | 10.1111/bjd.15930 | British Journal of Dermatology |
| 9 | Schmidt, E | Pemphigus (2019) | 48 | 10.1016/S0140-6736(19)31778-7 | Lancet |
| 10 | Didona, D | Pemphigus: Current and Future Therapeutic Strategies (2019) | 44 | 10.3389/fimmu.2019.01418 | Frontiers in immunology |
We analyzed the top 10 most cited articles about pemphigus treatment (Table 6). The document type of 2 of these 10 articles are review article and 8 are article. Table 6 lists the titles, years and first authors of these cited references. The most cited document was an article about a pemphigus treatment trial published in the Lancet by Joly, P in 2017. It described a prospective, multicenter, parallel group, open label, randomized trial conducted in 25 French dermatological hospitals. Through the comparison between rituximab combined with prednisone and prednisone alone, the authors concluded that rituximab combined with short-term prednisone is more effective than prednisone alone in the treatment of pemphigus patients and can better reduce the side effects of drug treatment [39]. The article with the second-highest citation is an article on pemphigus published in Nature Reviews Disease Primers by Kasperkiewicz, M in 2017. This article introduces the three subtypes, pathogenesis, diagnosis and first-line treatment of pemphigus [40]. The third-ranked citation was the recommendation of an international expert group on the diagnosis and treatment of pemphigus published in the Journal of the American Academy of Dermatology by Murrell, DF in 2020. To try to standardize the diagnosis and management of pemphigus, a preliminary survey based on the European Dermatology Forum and the European Academy of Dermatology and Venereology guidelines was sent to a panel of international experts to determine the level of consensus. This international consensus includes intravenous CD20 (an antigen expressed on the surface of B cells) inhibitors as a first-line therapy option for moderate-to-severe pemphigus [41].
4. Discussion
4.1. General information
Although there have been previous literature reviews on pemphigus treatment, as far as we know, this is the first time that bibliometric and visualization methods have been combined to analyze pemphigus treatment, and the results reflect the systematic understanding and views over the past 30 years. We obtained 1365 articles related to pemphigus treatment from the WOSCC and grasped the overall direction and research focus of pemphigus treatment through bibliometric and visual analyses.
During the 30 years covered by this study, the number of documents related to pemphigus treatment basically showed a steady upward trend, which indicates that growth may continue in the future. Different countries, institutions and authors have demonstrated the core strength in this field. There is no doubt that the dominant regions for the study of pemphigus treatment are still in mostly western countries, especially the United States, which is in a leading position in many aspects of this analysis. The different research levels in different countries may also be related to the national development level to a certain extent. The United States, Germany, Great Britain and Italy, which are currently leading countries in the treatment of pemphigus, are all developed countries. However, judging from the publishing trend in recent years, China is also making continuous progress, with increasing focus on pemphigus treatment, and their number of studies has begun to increase significantly.
In addition, these high journal IF of articles on pemphigus treatment also indicate that people are increasingly aware of its importance, and cooperation between different countries, institutions and scholars in research has also become an international trend. It is worth mentioning that the United States, Germany, the United Kingdom and Italy are among the best in cooperation among countries, but in terms of institutions and authors, Iran has a place among them. China has not been among the best in terms of cooperation among countries, institutions or scholars. However, from the perspective of trends, China still has great potential. In any case, these cooperations will further promote academic progress and exchanges, as well as the exploration of the pathogenesis and treatment of pemphigus.
4.2. Research hotspots
In general, keyword co-occurrence analysis and keyword clustering can reflect the research focus in this field. According to the keyword analysis, we found that the three most mentioned research hotspots in the study of pemphigus treatment are the following: the investigation of pemphigus subtypes, the development of treatment methods, and the exploration of pathogenesis. Distinguishing different subtypes is the basis for implementing treatment. Different treatment methods are needed to better adapt to individual needs, while studying the pathogenesis is the basis for effective treatment.
4.2.1. Investigation of pemphigus subtypes
It is well known that determining the classification of diseases according to clinical manifestations is the basis of treatment. Therefore, the study of pemphigus subtypes can better explore their pathogenesis and help to develop targeted drugs for treatment. In addition, PV, PF and PNP are shown in the list of the top 20 keywords. These are also reflected in the keyword burst analysis, which showed that they are also research hotspots.
In PV, mucosal erosions often precede epidermal blistering. Most patients with PV have mucosal involvement first, which then develops into skin involvement [42,43]. Research discovered that in the mucosal-dominant phase of pemphigus vulgaris, autoantibodies (PV-IgG) primarily against Dsg3 are pathogenic, which is the most abundant desmoglein isoform in the mucosal epithelium [44]. During the mucocutaneous phase, the presence of both anti-Dsg3 and anti-Dsg1 antibodies can be found, and Dsg1 is strongly expressed in the superficial epidermis, usually correlating with skin blistering [44]. The combination of systemic corticosteroids and corticosteroid-sparing adjuvant drugs is considered the main therapy for PV [45,46]. Systemic corticosteroids (prednisone) are the basis of the treatment for PV [47]. Adjuvant drugs commonly used are azathioprine [48], MMF [25] and cyclosporine [49].
PF is common in middle-aged and elderly people, mainly in the head and upper part of the chest and back. Patients with PF usually show skin erosions, ulcers and scabs [50]. In PF, autoantibodies (PF-IgG) primarily against Dsg1 cause superficial epidermal blistering [44]. These fragile, superficial blisters and bullae of the cutaneous surface easily rupture to yield erosive lesions [51]. The main treatment for PF is systemic corticosteroids combined with azathioprine, MMF or methotrexate [47].
PNP is a special type of pemphigus first described by Anhalt in 1990 and is associated with tumors [52]. Moreover, PNP is a severe disease with extremely high mortality [53]. The most typical manifestation of PNP is stomatitis, most due to erosions and ulcerations of the oropharynx [54]. The skin lesions of PNP are polymorphic, and the common lesions are blisters, erosions and lichenoid eruptions [55]. These are characteristic clinical features caused by humoral and cell-mediated autoimmune reactions [55]. Autoreactive T cells and IgG autoantibodies against heterogeneous antigens, including plakin family proteins and desmosomal cadherins, contribute to the pathogenesis of PNP [55]. The treatment of PNP remains challenging. The treatment of the underlying malignancy is always recommended because it can result in PNP improvement [56]. Early detection and radical resection of tumors such as localized Castleman disease and benign thymoma can improve the condition of PNP or achieve complete remission within 1–2 years [56,57]. In terms of drug therapy, systemic corticosteroids (prednisolone) in combination with steroid-sparing agents (azathioprine, MMF, cyclosporine, etc.) have been widely used [55,56].
4.2.2. Development of treatment methods
Systemic corticosteroids are one of the main treatments for pemphigus, but long-term use of high doses of steroids may be associated with many serious side effects [47,58]. Therefore, most patients receive adjuvant therapy to reduce the need for steroids [47]. MMF and rituximab are commonly used as adjuvant therapies, and both appear in the top 20 keyword list. MMF is an immunosuppressive drug that is safe and effective for use in pemphigus patients [[59], [60], [61]]. MMF is well tolerated, and its use can effectively lead to a reduction in the required dose of immunosuppressants such as glucocorticoids without obvious adverse reactions [[62], [63], [64]]. Rituximab is superior to MMF in relieving pemphigus vulgaris and leading to a reduction in the glucocorticoid use, but the adverse reactions of rituximab are more serious than those of MMF [65]. PE has been studied since the 1990s, and lasted for a considerable period. PE can effectively remove pemphigus autoantibodies and retain coagulation factor XIII, fibrinogen, etc. PE can be used to treat patients with refractory or severe disease [66,67] and is well tolerated in patients with treatment-resistant pemphigus [68]. Therefore, these treatment methods may continue to be the focus of research.
In addition, IVIg is also in the top 20 keyword list, so it also merits extra attention. Studies have found that in recent years, IVIg has been used to treat autoimmune bullous diseases for which conventional treatment is ineffective [[69], [70], [71], [72]]. For example, IVIg is used to treat patients with relatively mild PF resistant to corticosteroids and dapsone [73]. Therefore, when patients do not respond to conventional immunosuppressive therapy, IVIg can be used as a single treatment [74,75]. It is also a safe biological agent for the treatment of juvenile pemphigus vulgaris. Headache and fatigue are the most common side effects, but the overall treatment effect is good [76,77].
4.2.3. Exploration of pathogenesis
The pathogenesis of pemphigus is also a research hotspot. Antibody, autoimmunity disease and B cells are all in the top 20 keywords, and they are all related to the cause of pemphigus. The pathogenesis of pemphigus is currently believed to be the production of IgG autoimmune antibodies related to epidermal adhesion molecules (mainly Dsg1 and Dsg3) in vivo [78]. After the combination of IgG autoimmune antibodies and desmoglein, epidermal keratinocytes are separated, and clinical manifestations are loose blisters or erosions in the epidermis at the lesion site [17,78]. In addition to desmoglein antibodies, nondesmoglein antibodies [78] and anti-muscarine acetylcholine receptor antibodies [79] also play an important role in the occurrence and development of pemphigus. B lymphocytes are important mediators of the systemic immune response, play an important role in the pathogenesis of autoimmune diseases with skin manifestations, and are considered to be related to the pathogenesis of pemphigus because of their changes in the treatment of pemphigus [80]. In addition to B cells, cytokines, T cells and miRNAs also participate in the pathogenic process [[18], [19], [20]]. Research on pathogenesis is continuing, and it is also reflected in clustering and highlighted keywords, which indicates that pathogenesis is also an important research hotspot.
4.2.4. Potential research hotspots
With the development of precision medicine, we found that some individuals have a genetic susceptibility to pemphigus [81], which is called familial benign pemphigus or Hailey-Hailey disease (HHD). This is a rare vesicular dermatosis characterized by recurrent erythema, which tends to be in the interchondral region [82]. It is an autosomal dominant genodermatosis caused by a mutation that leads to disrupted intracellular calcium signaling that impairs keratinocyte adhesion [83,84]. The incidence of HHD is estimated to be approximately 1/50,000 [85]. Although many treatments have been proposed, there is no “gold standard” treatment. These measures include topical glucocorticoids (such as aloxone and pervisone), antibacterial drugs and calcineurin inhibitors, oral antibiotics, and intratumoral injection of botulinum toxin [85]. Systemic therapies commonly used are oral tetracyclines and erythromycin, which can not only inhibit bacteria but also reduce epidermal lysis, as well as destructive treatment, including carbon dioxide laser and surgical resection [85,86]. Although there is no genetic susceptibility to pemphigus in general, HHD also needs attention. As one of the clusters, although there are few articles completely focusing on HHD and its genetic susceptibility, they can be reflected by clustering only when they are mentioned in the article. Therefore, they may be potential research hotspots.
In addition, we learned that traditional Chinese medicine can also treat pemphigus. After studying the relevant literature, we found that the treatment of pemphigus is mainly based on syndrome differentiation, and there have been specialized studies on the use of traditional Chinese medicines, such as wild chrysanthemum [87]. There are also treatment methods for the combination of traditional Chinese medicine and chemical medications, such as glucocorticoid combination therapy commonly used in pemphigus [88], and supplementation with traditional Chinese medicine may improve the survival rate of patients with pemphigus [89]. These results also show that the curative effect can be improved to a certain extent through auxiliary treatment with traditional Chinese medicine.
4.3. Research frontiers
Based on the number of keywords, keyword clustering and keyword emergence, rituximab may have a leading edge in the treatment of pemphigus. Rituximab is a monoclonal antibody that binds to the CD-20 antigen of B lymphocytes, which causes B cell depletion and a subsequent reduction in pathogenic autoantibodies [90]. At present, the earliest research on rituximab in the treatment of pemphigus can be traced back to the successful treatment case published by Heizmann, M in 2001 [91], who proposed that rituximab may be an effective alternative drug for the treatment of PNP. Rituximab can be used alone to treat pemphigus [92,93] or in combination with glucocorticoids, corticosteroids, etc. [[94], [95], [96]]. However, rituximab increases the risk of Pneumocystis jiroveci pneumonia (PJP) and may have side effects such as urticaria and shingles [[97], [98], [99]]. In 2018, the United States Food and Drug Administration (FDA) approved rituximab as the first-line drug for the treatment of moderate and severe pemphigus. Rituximab is associated with the risk of long-term cardiovascular and metabolic outcomes in pemphigus patients, but the risk is low compared to that with other immunosuppressants [100]. Over the years, the efficacy of rituximab in the treatment of pemphigus has gradually improved, and research on its efficacy is also increasing [39,101,102]. In keyword burst analysis, low-dose rituximab has been cited since 2015. In the timeline view, references on the topic of "rituximab" have been published many times in recent years with a continued trend. All these findings indicate that the application of rituximab is the frontier in the treatment of pemphigus.
5. Conclusion
This study systematically summarized, analyzed and showed the contributions of various countries, institutions and scholars to the treatment of pemphigus through bibliometrics and visualization software such as CiteSpace and VOSviewer. Fortunately, the treatment of pemphigus has received increasing attention and research. Although the pathogenesis of pemphigus has not been completely identified at present, research on its treatment is relatively vast. This study was also a systematic summary based on published related literature, through which we hope to provide effective reference for the treatment of pemphigus.
6. Limitations
-
(1)
We searched and evaluated the relevant literature only in the WOSCC, which may have led to the omission of excellent articles from other sources.
-
(2)
We analyzed and referred to only the English language literature, which may also have led to missing some other excellent articles.
-
(3)
As the literature irrelevant to the research topic was manually excluded, there may have been selection bias in the screening process.
-
(4)
The analysis process was written by combining subjective with some objective situations, and the actual situation may be biased.
Data availability statement
Data associated with our study hasn't been deposited into a publicly available repository, but the datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Declarations
Review and approval by an ethics committee was not required for this study because this study does not involve relevant content.
Informed consent was not required for this study because this study does not involve relevant content.
Funding
This work was supported by Three-year Action Plan for Shanghai [project number: ZY (2021–2023)-0211], National Natural Science Foundation of China (81973730), Local Colleges Faculty Constitution of Shanghai MSTC 2022 (22010504300), and Shanghai Collaborative Innovation Center for Chronic Disease Prevention and Health Services (2021 Science and Technology 02–37).
CRediT authorship contribution statement
Xiujing Wang: Writing – original draft, Visualization, Validation, Resources, Methodology, Investigation, Formal analysis. Chaohong Huang: Writing – original draft, Visualization, Validation, Resources, Methodology, Investigation, Formal analysis. Wenjie Li: Writing – review & editing, Validation, Supervision. Yanlong Hong: Writing – review & editing, Validation, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Wenjie Li, Email: liwenjie@shutcm.edu.cn.
Yanlong Hong, Email: hfuir@163.com.
References
- 1.Schmidt E., Kasperkiewicz M., Joly P. Pemphigus. Lancet. 2019;394(10201):882–894. doi: 10.1016/S0140-6736(19)31778-7. [DOI] [PubMed] [Google Scholar]
- 2.Montagnon C.M., et al. Intraepithelial autoimmune blistering dermatoses: clinical features and diagnosis. J. Am. Acad. Dermatol. 2021;84(6):1507–1519. doi: 10.1016/j.jaad.2020.11.075. [DOI] [PubMed] [Google Scholar]
- 3.Malik A.M., et al. An Updated review of pemphigus diseases. Medicina-Lithuania. 2021;57(10):1080. doi: 10.3390/medicina57101080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kridin K., Schmidt E. Epidemiology of pemphigus. JID innovations. 2021;1(1) doi: 10.1016/j.xjidi.2021.100004. 100004-100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costan V.V., et al. Comprehensive review on the pathophysiology, clinical variants and management of pemphigus(Review) Exp. Ther. Med. 2021;22(5):1335. doi: 10.3892/etm.2021.10770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alpsoy E., Akman-Karakas A., Uzun S. Geographic variations in epidemiology of two autoimmune bullous diseases: pemphigus and bullous pemphigoid. Arch. Dermatol. Res. 2015;307(4):291–298. doi: 10.1007/s00403-014-1531-1. [DOI] [PubMed] [Google Scholar]
- 7.Lee Y.B., et al. Incidence and death rate of pemphigus vulgaris and pemphigus foliaceus in Korea: a nationwide, population-based study (2006-2015) J. Dermatol. (Tokyo) 2018;45(12):1396–1402. doi: 10.1111/1346-8138.14667. [DOI] [PubMed] [Google Scholar]
- 8.Joly P., Litrowski N. Pemphigus group (vulgaris, vegetans, foliaceus, herpetiformis, brasiliensis) Clin. Dermatol. 2011;29(4):432–436. doi: 10.1016/j.clindermatol.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Kridin K. Pemphigus group: overview, epidemiology, mortality, and comorbidities. Immunol. Res. 2018;66(2):255–270. doi: 10.1007/s12026-018-8986-7. [DOI] [PubMed] [Google Scholar]
- 10.Zhu X., et al. Epidemiology of pemphigus vulgaris in the Northeast China: a 10-year retrospective study. J. Dermatol. (Tokyo) 2014;41(1):70–75. doi: 10.1111/1346-8138.12286. [DOI] [PubMed] [Google Scholar]
- 11.Spaeth S., et al. IgG, IgA and IgE autoantibodies against the ectodomain of desmoglein 3 in active pemphigus vulgaris. Br. J. Dermatol. 2001;144(6):1183–1188. doi: 10.1046/j.1365-2133.2001.04228.x. [DOI] [PubMed] [Google Scholar]
- 12.Oursler J.R., et al. Human autoantibodies AGAINST DESMOPLAKINS IN paraneoplastic pemphigus. J. Clin. Invest. 1992;89(6):1775–1782. doi: 10.1172/JCI115781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Porro A.M., et al. Pemphigus vulgaris. An. Bras. Dermatol. 2019;94(3):264–278. doi: 10.1590/abd1806-4841.20199011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balighi K., et al. Temporal course of avascular femoral head necrosis in patients with pemphigus vulgaris. Journal Der Deutschen Dermatologischen Gesellschaft. 2016;14(10):1016–1021. doi: 10.1111/ddg.13079. [DOI] [PubMed] [Google Scholar]
- 15.Mahajan V.K., et al. Twelve-year clinico-therapeutic experience in pemphigus: a retrospective study of 54 cases. Int. J. Dermatol. 2005;44(10):821–827. doi: 10.1111/j.1365-4632.2005.02218.x. [DOI] [PubMed] [Google Scholar]
- 16.Amber K.T., et al. Targeted therapies for autoimmune bullous diseases: current Status. Drugs. 2018;78(15):1527–1548. doi: 10.1007/s40265-018-0976-5. [DOI] [PubMed] [Google Scholar]
- 17.Ellebrecht C.T., Maseda D., Payne A.S. Pemphigus and pemphigoid: from disease Mechanisms to Druggable pathways. J. Invest. Dermatol. 2022;142(3 PT B):907–914. doi: 10.1016/j.jid.2021.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Satyam A., et al. Involvement of T(H)1/T(H)2 cytokines in the pathogenesis of autoimmune skin disease-Pemphigus vulgaris. Immunol. Invest. 2009;38(6):498–509. doi: 10.1080/08820130902943097. [DOI] [PubMed] [Google Scholar]
- 19.Araghi F., et al. The emerging role of T cells in pemphigus vulgaris: a systematic review. Clin. Exp. Med. 2023;23(4):1045–1054. doi: 10.1007/s10238-022-00855-8. [DOI] [PubMed] [Google Scholar]
- 20.Wang M., et al. Increased miR-424-5p expression in peripheral blood mononuclear cells from patients with pemphigus. Mol. Med. Rep. 2017;15(6):3479–3484. doi: 10.3892/mmr.2017.6422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tavakolpour S. Pemphigus trigger factors: special focus on pemphigus vulgaris and pemphigus foliaceus. Arch. Dermatol. Res. 2018;310(2):95–106. doi: 10.1007/s00403-017-1790-8. [DOI] [PubMed] [Google Scholar]
- 22.Sikora M., et al. The Use of naltrexone in Dermatology. Current Evidence and future directions. Curr. Drug Targets. 2019;20(10):1058–1067. doi: 10.2174/1389450120666190318121122. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed A.R. Treatment of autoimmune mucocutaneous blistering diseases with intravenous immunoglobulin therapy. Expet Opin. Invest. Drugs. 2004;13(8):1019–1032. doi: 10.1517/13543784.13.8.1019. [DOI] [PubMed] [Google Scholar]
- 24.Toosi R., et al. Efficacy and safety of biosimilar rituximab in patients with pemphigus vulgaris: a prospective observational study. J. Dermatol. Treat. 2021;32(1):33–40. doi: 10.1080/09546634.2019.1617831. [DOI] [PubMed] [Google Scholar]
- 25.Enk A.H., Knop J. Mycophenolate is effective in the treatment of pemphigus vulgaris. Arch. Dermatol. 1999;135(1):54–56. doi: 10.1001/archderm.135.1.54. [DOI] [PubMed] [Google Scholar]
- 26.Ljubojevic S., et al. Pemphigus vulgaris: a review of treatment over a 19-year period. J. Eur. Acad. Dermatol. Venereol. 2002;16(6):599–603. doi: 10.1046/j.1468-3083.2002.00504.x. [DOI] [PubMed] [Google Scholar]
- 27.Corven C.B., et al. Treatment of pemphigus vulgaris by azathioprine and low doses of prednisone (Lever scheme) Annales De Dermatologie Et De Venereologie. 2003;130(1):13–15. [PubMed] [Google Scholar]
- 28.Scheinfeld N. Red blood cell anemia in a patient with pemphigus vulgaris induced by the use of mycophenolate mofetil and prednisone. J. Dermatol. Treat. 2007;18(4):243–245. doi: 10.1080/09546630701287324. [DOI] [PubMed] [Google Scholar]
- 29.Shahrigharahkoshan S., et al. A review of reported infectious events following rituximab therapy in pemphigus patients. Dermatol. Ther. 2022;35(3) doi: 10.1111/dth.15264. [DOI] [PubMed] [Google Scholar]
- 30.Schinner C., et al. Stabilization of desmoglein-2 binding rescues arrhythmia in arrhythmogenic cardiomyopathy. Jci Insight. 2020;5(9) doi: 10.1172/jci.insight.130141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eming R., Hertl M. Immunoadsorption in pemphigus. Autoimmunity. 2006;39(7):609–616. doi: 10.1080/08916930600972040. [DOI] [PubMed] [Google Scholar]
- 32.Frydman A.S., Fairley J.A. New and innovative interventions in the management of pemphigus. G. Ital. Dermatol. Venereol. 2011;146(3):211–224. [PubMed] [Google Scholar]
- 33.Genovese G., et al. Treatment of autoimmune bullous diseases during pregnancy and Lactation: a review focusing on pemphigus and pemphigoid Gestationis. Front. Pharmacol. 2020;11 doi: 10.3389/fphar.2020.583354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klimo P., Jr., et al. Bibliometrics. J. Neurosurg. 2016;124(3):877–878. doi: 10.3171/2015.7.JNS151647. [DOI] [PubMed] [Google Scholar]
- 35.Aria M., Cuccurullo C. Bibliometrix: an R-tool for comprehensive science mapping analysis. Journal of Informetrics. 2017;11(4):959–975. [Google Scholar]
- 36.Li W., et al. Bibliometric and visual analysis of nocturnal enuresis from 1982 to 2022. Frontiers in Pediatrics. 2022;10 doi: 10.3389/fped.2022.972751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murrell D.E., et al. Consensus statement on definitions of disease, end points, and therapeutic response for pemphigus. J. Am. Acad. Dermatol. 2008;58(6):1043–1046. doi: 10.1016/j.jaad.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Henry s. Co-Citation in the Scientific literature: a new measure of the relationship between two documents. J. Am. Soc. Inf. Sci. 1973;24(4):265–269. [Google Scholar]
- 39.Joly P., et al. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet. 2017;389(10083):2031–2040. doi: 10.1016/S0140-6736(17)30070-3. [DOI] [PubMed] [Google Scholar]
- 40.Kasperkiewicz M., et al. Pemphigus. Nat. Rev. Dis. Prim. 2017;3 doi: 10.1038/nrdp.2017.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murrell D.F., et al. Diagnosis and management of pemphigus: Recommendations of an international panel of experts. J. Am. Acad. Dermatol. 2020;82(3) doi: 10.1016/j.jaad.2018.02.021. 575-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malik M., Ahmed A.R. Involvement of the female genital tract in pemphigus vulgaris. Obstet. Gynecol. 2005;106(5):1005–1012. doi: 10.1097/01.AOG.0000185258.74177.91. [DOI] [PubMed] [Google Scholar]
- 43.Venugopal S.S., Murrell D.F. Diagnosis and clinical features of pemphigus vulgaris. Immunol. Allergy Clin. 2012;32(2) doi: 10.1016/j.iac.2012.04.003. 233-233. [DOI] [PubMed] [Google Scholar]
- 44.Spindler V., Waschke J. Pemphigus-A disease of desmosome dysfunction caused by multiple mechanisms. Front. Immunol. 2018;9:136. doi: 10.3389/fimmu.2018.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carson P.J., Hameed A., Ahmed A.R. Influence of treatment on the clinical course of pemphigus vulgaris. J. Am. Acad. Dermatol. 1996;34(4):645–652. doi: 10.1016/s0190-9622(96)80066-1. [DOI] [PubMed] [Google Scholar]
- 46.Hertl M., et al. Pemphigus. S2 guideline for diagnosis and treatment - guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV) J. Eur. Acad. Dermatol. Venereol. 2015;29(3):405–414. doi: 10.1111/jdv.12772. [DOI] [PubMed] [Google Scholar]
- 47.Porro A.M., Hans Filho G., Santi C.G. Consensus on the treatment of autoimmune bullous dermatoses: pemphigus vulgaris and pemphigus foliaceus - Brazilian Society of Dermatology. An. Bras. Dermatol. 2019;94(2):S20–S32. doi: 10.1590/abd1806-4841.2019940206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chaidemenos G., et al. High dose oral prednisone vs. prednisone plus azathioprine for the treatment of oral pemphigus: a retrospective, bi-centre, comparative study. J. Eur. Acad. Dermatol. Venereol. 2011;25(2):206–210. doi: 10.1111/j.1468-3083.2010.03753.x. [DOI] [PubMed] [Google Scholar]
- 49.Lapidoth M., et al. The efficacy of combined treatment with prednisone and cyclosporine in patients with pemphigus - preliminary-study. J. Am. Acad. Dermatol. 1994;30(5):752–757. doi: 10.1016/s0190-9622(08)81506-x. [DOI] [PubMed] [Google Scholar]
- 50.Cheng H.F., et al. Pemphigus foliaceus complicated by disseminated cutaneous herpes simplex virus infection in an elderly man. Hong Kong Journal of Dermatology & Venereology. 2013;21(2):73–77. [Google Scholar]
- 51.James K.A., Culton D.A., Diaz L.A. Diagnosis and clinical features of pemphigus foliaceus. Dermatol. Clin. 2011;29(3) doi: 10.1016/j.det.2011.03.012. 405-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaplan I., et al. Neoplasms associated with paraneoplastic pemphigus: a review with emphasis on non-hematologic malignancy and oral mucosal manifestations. Oral Oncol. 2004;40(6):553–562. doi: 10.1016/j.oraloncology.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 53.Fukumoto T., et al. Paraneoplastic pemphigus presenting as erythrodermic lichenoid dermatitis with concomitant features of pemphigus foliaceus. J. Dermatol. (Tokyo) 2007;34(9):645–649. doi: 10.1111/j.1346-8138.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 54.Anhalt G.J. Paraneoplastic pemphigus. J. Invest. Dermatol. Symp. Proc. 2004;9(1):29–33. doi: 10.1111/j.1087-0024.2004.00832.x. [DOI] [PubMed] [Google Scholar]
- 55.Kim J.H., Kim S.-C. Paraneoplastic pemphigus: paraneoplastic autoimmune disease of the skin and mucosa. Front. Immunol. 2019;10:1259. doi: 10.3389/fimmu.2019.01259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Antiga E., et al. S2k guidelines on the management of paraneoplastic pemphigus/paraneoplastic autoimmune multiorgan syndrome initiated by the European Academy of Dermatology and Venereology (EADV) J. Eur. Acad. Dermatol. Venereol. 2023;37(6):1118–1134. doi: 10.1111/jdv.18931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang J., et al. Improved outcomes after complete resection of underlying tumors for patients with paraneoplastic pemphigus: a single-center experience of 22 cases. J. Cancer Res. Clin. Oncol. 2011;137(2):229–234. doi: 10.1007/s00432-010-0874-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yamagami J. B-cell targeted therapy of pemphigus. J. Dermatol. (Tokyo) 2023;50(2):124–131. doi: 10.1111/1346-8138.16653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kawashita M.Y., et al. Mycophenolate mofetil as an adjuvant therapy for classic and endemic pemphigus foliaceus. J. Dermatol. (Tokyo) 2005;32(7):574–580. doi: 10.1111/j.1346-8138.2005.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 60.Esmaili N., et al. Treatment of pemphigus vulgaris with mycophenolate mofetil as a steroid-sparing agent. Eur. J. Dermatol. 2008;18(2):159–164. doi: 10.1684/ejd.2008.0354. [DOI] [PubMed] [Google Scholar]
- 61.Megahed M., et al. Treatment of cicatricial pemphigoid with mycophenolate mofetil as a steroid-sparing agent. J. Am. Acad. Dermatol. 2001;45(2):256–259. doi: 10.1067/mjd.2001.114746. [DOI] [PubMed] [Google Scholar]
- 62.Doukaki S., et al. Mycophenolate mofetil and enteric-coated mycophenolate sodium in the treatment of pemphigus vulgaris and pemphigus foliaceus. J. Dermatol. Treat. 2015;26(1):67–72. doi: 10.3109/09546634.2014.880395. [DOI] [PubMed] [Google Scholar]
- 63.Powell A.M., et al. An evaluation of the usefulness of mycophenolate mofetil in pemphigus. Br. J. Dermatol. 2003;149(1):138–145. doi: 10.1046/j.1365-2133.2003.05269.x. [DOI] [PubMed] [Google Scholar]
- 64.Chams-Davatchi C., et al. Open trial of mycophenolate mofetil in the treatment of resistant pemphigus vulgaris. Annales De Dermatologie Et De Venereologie. 2002;129(1):23–25. [PubMed] [Google Scholar]
- 65.Werth V.P., et al. Rituximab versus mycophenolate mofetil in patients with pemphigus vulgaris. N. Engl. J. Med. 2021;384(24):2295–2305. doi: 10.1056/NEJMoa2028564. [DOI] [PubMed] [Google Scholar]
- 66.Miyamoto S., et al. Selective plasma exchange for the removal of pemphigus autoantibodies, fibrinogen, and factor XIII in pemphigus vulgaris. Ther. Apher. Dial. 2017;21(3):226–231. doi: 10.1111/1744-9987.12555. [DOI] [PubMed] [Google Scholar]
- 67.Kumar R., et al. Therapeutic plasma exchange-A new dawn in the treatment of pemphigus vulgaris. Indian J. Dermatol. 2015;60(4):419. doi: 10.4103/0019-5154.160509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sagi L., et al. The role of therapeutic plasma exchange in pemphigus vulgaris. J. Eur. Acad. Dermatol. Venereol. 2011;25(1):82–86. doi: 10.1111/j.1468-3083.2010.03703.x. [DOI] [PubMed] [Google Scholar]
- 69.Engineer L., Bhol K.C., Ahmed A.R. Analysis of current data on the use of intravenous immunoglobulins in management of pemphigus vulgaris. J. Am. Acad. Dermatol. 2000;43(6):1049–1057. doi: 10.1067/mjd.2000.108366. [DOI] [PubMed] [Google Scholar]
- 70.Altman E.M. Novel therapies for pemphigus vulgaris. Am. J. Clin. Dermatol. 2020;21(6):765–782. doi: 10.1007/s40257-020-00544-w. [DOI] [PubMed] [Google Scholar]
- 71.Levy A., et al. Treatment of pemphigus with intravenous immunoglobulin. Annales De Dermatologie Et De Venereologie. 2004;131(11):957–961. doi: 10.1016/s0151-9638(04)93805-7. [DOI] [PubMed] [Google Scholar]
- 72.Tappeiner G., Steiner A. High-dosage intravenous gamma globulin: therapeutic failure in pemphigus and pemphigoid. J. Am. Acad. Dermatol. 1989;20(4):684–685. doi: 10.1016/s0190-9622(89)80148-3. [DOI] [PubMed] [Google Scholar]
- 73.Kawakami T., et al. Four mild but refractory cases of pemphigus foliaceus successfully treated with intravenous immunoglobulin. J. Dermatol. (Tokyo) 2013;40(11):869–873. doi: 10.1111/1346-8138.12280. [DOI] [PubMed] [Google Scholar]
- 74.Teixeira T.A., et al. Refractory endemic pemphigus foliaceous in adolescence successfully treated with intravenous immunoglobulin. An. Bras. Dermatol. 2011;86(4):133–136. doi: 10.1590/s0365-05962011000700035. [DOI] [PubMed] [Google Scholar]
- 75.Daoud Y.J., Foster C.S., Ahmed A.R. Eyelid skin involvement in pemphigus foliaceus. Ocul. Immunol. Inflamm. 2005;13(5):389–394. doi: 10.1080/09273940590951025. [DOI] [PubMed] [Google Scholar]
- 76.Asarch A., Ahmed R. Treatment of juvenile pemphigus vulgaris with intravenous immunoglobulin therapy. Pediatr. Dermatol. 2009;26(2):197–202. doi: 10.1111/j.1525-1470.2008.00808.x. [DOI] [PubMed] [Google Scholar]
- 77.Seidling V., et al. Analysis of high-dose intravenous immunoglobulin therapy in 16 patients with refractory autoimmune blistering skin disease: high efficacy and No serious adverse events. Acta Derm. Venereol. 2013;93(3):346–349. doi: 10.2340/00015555-1471. [DOI] [PubMed] [Google Scholar]
- 78.Sinha A.A., Sajda T. The evolving story of autoantibodies in pemphigus vulgaris: development of the "super compensation hypothesis". Front. Med. 2018;5:218. doi: 10.3389/fmed.2018.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lakshmi M.J.D., et al. Correlation of antimuscarinic acetylcholine receptor antibody titers and antidesmoglein antibody titers with the severity of disease in patients with pemphigus. J. Am. Acad. Dermatol. 2017;76(5):895–902. doi: 10.1016/j.jaad.2016.11.039. [DOI] [PubMed] [Google Scholar]
- 80.Daneshvar E., et al. Elevated serum level of B-cell activating factor (BAFF) after rituximab therapy in pemphigus vulgaris patients suggests a possible therapeutic efficacy of B-cell depletion therapies combined with anti-BAFF agents. Int. J. Dermatol. 2023;62(4):567–574. doi: 10.1111/ijd.16363. [DOI] [PubMed] [Google Scholar]
- 81.Petzl-Erler M.L. Beyond the HLA polymorphism: a complex pattern of genetic susceptibility to pemphigus. Genet. Mol. Biol. 2020;43(3):E369. doi: 10.1590/1678-4685-GMB-2019-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Farahnik B., et al. Interventional treatments for Hailey-Hailey disease. J. Am. Acad. Dermatol. 2017;76(3) doi: 10.1016/j.jaad.2016.08.039. 551-551. [DOI] [PubMed] [Google Scholar]
- 83.Mauro T.M. Yeast researchers consider Hailey-Hailey disease. J. Invest. Dermatol. 2004;123(6):XXII–XXIII. doi: 10.1111/j.0022-202X.2004.23482.x. [DOI] [PubMed] [Google Scholar]
- 84.Deng H., Xiao H. The role of the ATP2C1 gene in Hailey-Hailey disease. Cell. Mol. Life Sci. 2017;74(20):3687–3696. doi: 10.1007/s00018-017-2544-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ben Lagha I., Ashack K., Khachemoune A. Hailey-hailey disease: an update review with a focus on treatment data. Am. J. Clin. Dermatol. 2020;21(1):49–68. doi: 10.1007/s40257-019-00477-z. [DOI] [PubMed] [Google Scholar]
- 86.Jasans-Barcelo M., et al. Improvement of Hailey-Hailey disease with low-dose naltrexone. Br. J. Dermatol. 2020;182(6):1500–1502. doi: 10.1111/bjd.18861. [DOI] [PubMed] [Google Scholar]
- 87.Shao Y.H., et al. Chrysanthemum indicum L.: A comprehensive review of its botany, phytochemistry and pharmacology. Am. J. Chin. Med. 2020;48(4):871–897. doi: 10.1142/S0192415X20500421. [DOI] [PubMed] [Google Scholar]
- 88.Zhou T., et al. Beneficial effects and safety of corticosteroids combined with traditional Chinese medicine for pemphigus: a systematic review. Evid. base Compl. Alternative Med. 2015;2015 doi: 10.1155/2015/815358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu P.-Y., et al. Complementary Chinese herbal medicine therapy improves survival in patients with pemphigus: a retrospective study from a Taiwan-based registry. Front. Pharmacol. 2020;11 doi: 10.3389/fphar.2020.594486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hebert V., Joly P. Rituximab in pemphigus. Immunotherapy. 2018;10(1):27–37. doi: 10.2217/imt-2017-0104. [DOI] [PubMed] [Google Scholar]
- 91.Heizmann M., et al. Successful treatment of paraneoplastic pemphigus in follicular NHL with rituximab: report of a case and review of treatment for paraneoplastic pemphigus in NHL and CLL. Am. J. Hematol. 2001;66(2):142–144. doi: 10.1002/1096-8652(200102)66:2<142::AID-AJH1032>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 92.Santiago-Vazquez M., et al. Successful treatment of recalcitrant pediatric pemphigus vulgaris with rituximab. Clin. Pediatr. 2023;62(6):541–547. doi: 10.1177/00099228221140801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Verma G., et al. Experience of rituximab therapy in pemphigus: a three-year retrospective study from a Sub-Himalayan State. Indian J. Dermatol. 2022;67(4):477. doi: 10.4103/ijd.ijd_169_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mazaherpour E., et al. Applicability of glucocorticoid toxicity index in pemphigus: comparison between two groups of rituximab-treated and rituximab-naive patients. Dermatol. Ther. 2022;35(12) doi: 10.1111/dth.15902. [DOI] [PubMed] [Google Scholar]
- 95.Zhao W., et al. Comparison of guidelines for management of pemphigus: a review of systemic corticosteroids, rituximab, and other immunosuppressive therapies. Clin. Rev. Allergy Immunol. 2021;61(3):351–362. doi: 10.1007/s12016-021-08882-1. [DOI] [PubMed] [Google Scholar]
- 96.Maho-Vaillant M., et al. Rituximab and corticosteroid effect on desmoglein-specific B cells and desmoglein-specific T follicular helper cells in pemphigus. J. Invest. Dermatol. 2021;141(9) doi: 10.1016/j.jid.2021.01.031. 2132-2132. [DOI] [PubMed] [Google Scholar]
- 97.Wei K.C., et al. Fatal infection of Pneumocystis jiroveci pneumonia in a pemphigus patient treated with rituximab. J. Eur. Acad. Dermatol. Venereol. 2017;31(8):E350–E351. doi: 10.1111/jdv.14144. [DOI] [PubMed] [Google Scholar]
- 98.Wei K.C., et al. Pneumocystis jirovecii pneumonia infection in pemphigus patients treated with rituximab: an observational nationwide epidemiological study in Taiwan. Eur. J. Dermatol. 2018;28(5):713–715. doi: 10.1684/ejd.2018.3373. [DOI] [PubMed] [Google Scholar]
- 99.Gupta J., et al. Low-dose rituximab as an adjuvant therapy in pemphigus. Indian J. Dermatol., Venereol. Leprol. 2017;83(3):317–325. doi: 10.4103/ijdvl.IJDVL_1078_14. [DOI] [PubMed] [Google Scholar]
- 100.Kridin K., Mruwat N., Ludwig R.J. Association of rituximab with risk of long-term cardiovascular and metabolic outcomes in patients with pemphigus. Jama Dermatology. 2023;159(1):56–61. doi: 10.1001/jamadermatol.2022.5182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Schmidt E., Goebeler M., Zillikens D. In: Contemporary Challenges in Autoimmunity. Shoenfeld Y., Gershwin M.E., editors. 2009. Rituximab in severe pemphigus; pp. 683–691. [Google Scholar]
- 102.Mezni L., et al. Rituximab in the treatment of pemphigus: a single-center Moroccan analysis of 43 cases. J. Invest. Dermatol. 2022;142(12) S205-S205. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data associated with our study hasn't been deposited into a publicly available repository, but the datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.