Abstract
Background
A better understanding of how the prevalence of hearing loss and its associated factors change over time could help in developing an appropriate program to prevent the development of hearing loss.
Methods
Population-representative cross-sectional data from the United States National Health and Nutrition Examination Survey (NHANES) were used to estimate the trends in the prevalence of hearing loss among adults in the USA over the period 1999–2018. A total of 15,498 adult participants aged 20 years or older had complete audiometric examination data. Logistic regression was employed to evaluate the trend in hearing loss; weighted Rao-Scott χ2 tests and univariate logistic regression analyses were used to examine the association between hearing loss and relevant factors.
Results
The overall hearing loss prevalence in 1999–2018 was 19.1% 19.1 (95% CI, 18.0–20.2%). The prevalence of hearing loss decreased in cycles (P for trend < 0.001). For participants aged 20–69 years, the prevalence decreased from 15.6% (95% CI, 12.9–18.4%) in 1999–2000 to 14.9% (95% CI, 13.2– 16.6%) in 2015–2016; for participants aged > 70 years the prevalence decreased from 79.9% (95% CI, 76.1–83.8%) in 2005–2006 to 64.5% (95% CI, 58.8–70.2%) in 2017–2018. Participants with hearing loss were likely to be older, male, non-Hispanic white, and to have not completed high school. Mild hearing loss was more prevalent among those aged 20–79 years; in those aged over 80 years the prevalence of moderate hearing loss exceeded that of mild loss. Among all otologically normal participants, hearing thresholds increased with age across the entire frequency range.
Conclusions
The prevalence of hearing loss in USA adults changed over the period 1999–2018. The trends observed provide valuable insight for making public health plans and allocating resources to hearing care. Further investigation is necessary to monitor hearing loss and its potential risk factors.
Keywords: Hearing loss, Prevalence, NHANES, Adults
Introduction
Hearing loss is becoming an increasingly serious public health concern in the USA. According to the estimates of Global Burden of Disease Study (GBD), more than 1.5 billion people were affected by hearing loss in 2019, amounting to 20% of the global population. Of those affected, 1.17 billion people had mild hearing loss [1]. There are potential socioeconomic impacts of hearing loss, including underemployment, reduction of income, and low educational attainment [2]. Moreover, hearing loss is the third most common cause of years lived with disability (YLDs), and is responsible for 43.5 million YLDs globally [3]. Individually, hearing loss has effects on quality of life, psychosocial health [4], and economic independence [1, 5], and affects language discrimination, resulting in communication difficulties [6], low learning and work efficiency, and a reduction in social interaction [4, 7].
The prevalence of hearing loss and the distribution of hearing threshold levels over time are due to many factors: the change in the national population structure, the diversity of the labor force, lifestyle changes, an increase in occupational noise exposure and environmental noise, the emergence of new diseases, an improvement in the awareness of hearing loss, advances in clinical medicine, and the development of new pharmaceuticals [7–9]. Studies reported in the literature have shown differences in the prevalence of hearing loss, but there has been a lack of long-term and continuous trend analysis of the prevalence of hearing loss [3, 10–12]. As most studies of hearing loss use self-report forms as a survey tool, the prevalence of mild and unilateral hearing loss may have been underestimated [13, 14].
The World Health Organization (WHO) has adopted a more standardized grading system for hearing-loss severity that is based on hearing measurements. Hearing loss is classified as mild, moderate, moderately severe, profound, and complete or total hearing loss/deafness. The new grading system has resulted in the measure of the onset of mild hearing loss being reduced from a hearing threshold of 26 dB to 20 dB, and has added the definition of unilateral hearing loss (< 20 dB in the better ear, 35 dB or greater in the worse ear) [7]. In addition to the classification, the revised system provides a description of the consequences on communication capabilities that may accompany each severity level. The new WHO hearing loss standardized grading system enables identification of asymmetric hearing loss and unilateral deafness, a more accurate description of hearing loss, and a better understanding of the difficulties in listening to the surrounding environment and speech communication in people with different levels of hearing loss. According to the WHO’s World Report on Hearing, released in 2021 [7], the prevalence across all WHO regions of moderate or high-grade hearing loss is in the range 10.9–17.6% in people aged 60–69 years, rising to 41.9–51.2% in people aged 80–89 years, and 52.9–64.9% in people aged > 90 years.
Accurate and representative data on the prevalence of hearing loss are important to understand the consequences of hearing needs, and to make plans regarding the allocation of the limited resources available for hearing healthcare [15]. It is also important that the data on the distribution of hearing threshold levels in the otologically normal population are updated from time to time. Therefore, we analyzed the periodic prevalence of hearing loss among adults in the USA aged 20 years and older using data from NHANES for the period 1999–2018, which was obtained using pure tone audiometry testing. In addition, we compared the distribution of hearing threshold levels from NHANES with those given in ISO 7029:2017 (Acoustics – Statistical distribution of hearing thresholds related to age and gender). We aimed to characterize the changes in the prevalence of hearing loss in this population from 1999 to 2018, in order to evaluate whether adult hearing loss changed over that period. A better understanding of the trends in hearing loss and its prevalence and associated factors will provide policy makers and public health researchers with more evidence that they can use when developing targeted strategies for the prevention of hearing loss.
Methods
Study population
NHANES is a nationally representative survey conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC) to assess the health and nutritional status of the civilian, non-institutionalized US population. The survey utilizes a complex, multistage, probability sampling design.
The present study used the NHANES data for the period 1999–2018. We included the participants aged 20–69 years in the cycles 1999–2004, 2011–2012, and 2015–2016, and all participants aged 70 years or older in the cycles 2005–2006, 2009–2010, and 2017–2018, because these cycles included the variables of interest.
NHANES oversampled certain populations (e.g. Mexican Americans, non-Hispanic black Americans), which allowed for increased reliability and precision of health status indicator estimates for these groups. Audiometric examinations were conducted on half of the sample of interviewed adults aged 20–69 years in 1999–2004, and all of the adults interviewed at the mobile examination center in 2005–2018 (except 2013–2014). To account for the complex sampling design and non-responses in NHANES, we applied appropriate sample weights in our analyses.
We calculated the percentile distributions of hearing threshold levels based on 3,454 otologically normal participants (exclusions: ear infection, tinnitus, non-occupational noise exposure, occupational noise exposure, and unilateral hearing loss) (NHANES data for 1999–2018) stratified by age and sex.
Audiometric measurements
In 1999-2016, the audiometry exam sections were performed by technicians professionally trained by a certified audiologist from the National Institute for Occupational Safety and Health (NIOSH) in a dedicated sound-isolating room in the Mobile Examination Center (MEC). Instrumentation for the Audiometry Component included an Interacoustics Model AD226 audiometer with standard TDH-39 headphones and Etymotic EarTone 3A insert earphones. Audiometric calibration and background noise levels were checked using a Quest Model 1800 Precision Integrating Sound Level Meter and Model OB-300 1/3–1/1 octave filter set. Daily monitoring of calibration and ambient noise levels was accomplished with a Quest Model BA-201–25 Bioacoustic Simulator and Octave Band Monitor. The audiometers used in this survey met the specifications of ANSI S3.6–1996 for Type 3 audiometers. Hearing threshold testing was conducted on both ears of subjects at seven frequencies (500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz), and the testing threshold range was from –10 to 120 dB. Subjects using hearing aids who were not able to remove them for testing and subjects who had so much ear pain at the time of the examination that they could not tolerate headphones were excluded from the audiometry component of the survey. There were no other precluding conditions for any part of the audiology examination.
Beginning in the 2017–2018, the ART system was used to conduct the pure-tone air conduction hearing test on survey participants. The ART system is a comprehensive, high configurable audiometer designed for the research application. Instrumentation for the audiometry component included an Audiometric Research Tool (ART) system with standard TDH-49P headphones and Etymotic EarTone 3A insert earphones. Daily monitoring ambient noise levels was accomplished with a Quest Model BA-202-27 Bioacoustic Simulator.AUX data were entered directly into the computerized NHANES database system. Data from the ART system and Interacoustics Titan were captured electronically and uploaded into the survey information system automatically.
Definition of hearing loss
Hearing thresholds are usually measured by pure-tone audiometry, which estimates the minimum sound intensity of pure tones at a range of frequencies. The pure-tone average (PTA) is the average of the hearing-threshold level at frequencies of 500, 1000, 2000, and 4000 Hz in the better ear. The better ear was defined as the ear showing the lower PTA. Hearing loss was categorized according to the WHO classification: normal hearing(less than 20 dB), mild (20 to < 35 dB), moderate (35 to < 50 dB), moderately severe (50 to < 65 dB), severe (65 to < 80 dB), profound (80 to < 95 dB), and complete or total hearing loss/deafness (95 dB or greater); and unilateral hearing loss (< 20 dB in the better ear, 35 dB or greater in the worse ear) [7]. Since the numbers of subjects in the more refined categories were very small, severe hearing loss, profound hearing loss, and complete or total hearing loss/deafness were merged into the moderately severe hearing loss group.
Demographic variables
Information about age, sex, race/ethnicity, educational level, and family income/poverty level ratio was collected during the NHANES in-person interviews. Participants were grouped into 10-year categories by age. Race and ethnicity were categorized as Hispanic (including Mexican American and other Hispanic), non-Hispanic white, non-Hispanic black, and other (including non-black, non-Hispanic groups such as Asian-American, Native American, and mixed race). Educational level was grouped into the following categories: less than high school (including less than 9th grade, 9–11th grade (includes 12th grade with no diploma)), high school (high school graduate/GED or equivalent), and college or higher (including some college or AA degree, college graduate or above). Family income/poverty level ratio was used the poverty/income ratio (PIR), which was defined as the total family income divided by the poverty threshold, as determined by the US Census Bureau, for the year of the interview. It was grouped into the following categories: low (PIR ≤ 1.3), middle (1.3 < PIR ≤ 3.5), and high (PIR > 3.5).
Relevant variables
The occupational noise exposure in the NHANES cycles for 1999–2004 was defined as exposure to loud noise in the “current job.” In the 2005–2010 cycles, participants were asked whether they were exposed to job-related loud noise for at least 5 h per week. In the 2011–2012 and 2015–2018 cycles, participants were asked if they had ever had a job or a combination of two jobs that exposed them to loud noise for at least 4 h a day or on several days a week. We grouped the answers as “yes” and “no” (which included “no” and “never worked”) for the 2011–2012 and 2015–2018 cycles.
The non-occupational noise exposure in the 1999–2004 cycles was defined as exposure to noise at least once a month for a year outside work. In the 2005–2010 cycles, participants were asked whether they were exposed to noise for 5 h or more per week outside work. “At least 10 h per week in non-occupational noise exposure” was defined as exposure in the 2011–2012 and 2015–2018 cycles.
We used the results from the survey self-assessment questionnaire to identify the presence of tinnitus and/or ear infection. We grouped the answers as “yes” and “no”.
Statistical analyses
All statistical analyses were performed by considering the weights necessary due to the complex sampling design and according to the guidelines for the analysis of NHANES data. The weighted prevalences and 95% CIs of hearing loss were estimated. The demographic sample proportions were compared using the Rao-Scott χ2 tests from the survey. The survey univariate logistic regression was used to evaluate the trend in hearing loss. We provided percentile distributions of hearing threshold levels, stratified by age and sex. The relevant variables are used to show the stratified trends. All data analyses were performed using SAS 9.4 (SAS Institute, Cary, North Carolina, USA).
Ethics
NHANES has been approved by the NCHS Ethics Review Board. Data are released in 2-year cycles and are made publicly available online. Written informed consent is obtained from all survey participants. The Guangdong Pharmaceutical University Academic Review Board determined that the present study was exempt from approval because of the use of de-identified data.
Results
Baseline characteristics
Tables 1 and 2 shows the characteristics of survey participants according to the auditory threshold test in the 1999–2018 cycles of NHANES. A total of 15,498 individuals were included over 8 cycles (those without complete hearing threshold test data or aged under 20 years were excluded). Table is divided into Tables 1 and 2.
Table 1.
Characteristics of participants in NHANES according to the auditory threshold by cycle (1999–2006)
| Participants, N (%)a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | |||||||||
| Characteristic | Normal hearing | Hearing loss | P valueb | Normal hearing | Hearing loss | P valueb | Normal hearing | Hearing loss | P valueb | Normal hearing | Hearing loss | P valueb |
| Overall | 1346 | 309 | 1551 | 310 | 1462 | 288 | 120 | 543 | ||||
| Age, N (%), | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||
| 20–29 years | 378 | 5 | 424 | 12 | 405 | 11 | -c | -c | ||||
| 25.6 (20.2–31.1) | 1.9 (0.0–4.1) | 23.9 (20.8–27.1) | 3.6 (0.8–6.4) | 24.5 (22.3–26.7) | 5.1 (0.3–9.9) | |||||||
| 30–39 years | 330 | 18 | 366 | 26 | 353 | 15 | -c | -c | ||||
| 28.9 (24.0–33.8) | 8.2 (4.8–11.6) | 25.1 (20.9–29.3) | 9.6 (3.8–15.5) | 25.8 (23.0–28.6) | 5.8 (2.2–9.5) | |||||||
| 40–49 years | 267 | 38 | 363 | 45 | 309 | 39 | -c | -c | ||||
| 23.4 (19.8–27.0) | 16.3 (9.3–23.2) | 28.2 (24.5–31.8) | 19.8 (15.7–23.8) | 25.7 (22.9–28.6) | 17.7 (12.2–23.2) | |||||||
| 50–59 years | 187 | 74 | 231 | 87 | 204 | 75 | -c | -c | ||||
| 14.5 (11.7–17.2) | 28.7 (18.4–39.0) | 16.3 (13.4–19.2) | 35.7 (29.6–41.8) | 16.3 (13.5–19.1) | 36.7 (29.5–43.8) | |||||||
| 60–69 years | 184 | 174 | 167 | 140 | 191 | 148 | -c | -c | ||||
| 7.6 (6.0–9.3) | 45.0 (34.5–55.5) | 6.5 (5.1–7.8) | 31.3 (25.5–37.1) | 7.7 (6.3–9.1) | 34.7 (28.8–40.7) | |||||||
| 70–79 years | -c | -c | -c | -c | -c | -c | 101 | 301 | ||||
| 87.0 (80.3–93.6) | 62.9 (58.3–67.6) | |||||||||||
| 80 + years | -c | -c | -c | -c | -c | -c | 19 | 242 | ||||
| 13.0 (6.4–19.7) | 37.1 (32.4–41.7) | |||||||||||
| Sex, N (%) | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||
| Men | 580 | 204 | 655 | 209 | 651 | 173 | 47 | 294 | ||||
| 47.2 (43.4–51.0) | 67.1 (61.0–73.1) | 43.4 (40.0–46.8) | 68.8 (61.9–75.6) | 46.6 (43.5–49.8) | 60.0 (55.7–64.3) | 28.7 (22.6–34.7) | 43.6 (38.9–48.3) | |||||
| Women | 766 | 105 | 896 | 101 | 811 | 115 | 73 | 249 | ||||
| 52.8 (49.0–56.6) | 32.9 (26.9–39.0) | 56.6 (53.2–60.0) | 31.2 (24.4–38.1) | 53.4 (50.2–56.2) | 40.0 (35.7–44.3) | 71.3 (65.3–77.4) | 56.4 (51.7–61.1) | |||||
| Race, N (%) | 0.21 | 0.003 | < 0.001 | 0.36 | ||||||||
| Hispanic | 475 | 113 | 428 | 72 | 341 | 76 | 8 | 60 | ||||
| 17.9 (11.1–24.6) | 15.7 (5.6,25.9) | 13.8 (8.2–19.5) | 9.5 (4.6–14.4) | 12.7 (7.1–18.3) | 10.0 (4.9–15.1) | 2.6 (0.3–4.8) | 4.2 (2.6–5.7) | |||||
| Non-Hispanic white | 573 | 139 | 727 | 170 | 718 | 161 | 79 | 409 | ||||
| 66.9 (60.8–73.0) | 73.8 (62.7–84.8) | 68.7 (63.2–74.3) | 77.5 (70.2–84.8) | 69.5 (62.2–76.8) | 77.3 (69.6–85.1) | 85.2 (76.2–94.2) | 87.9 (83.8–92.1) | |||||
| Non-Hispanic black | 253 | 49 | 329 | 57 | 336 | 35 | 30 | 68 | ||||
| 11.3 (7.8–14.7) | 7.3 (2.6–12.0) | 11.9 (7.9–15.9) | 8.3 (3.6–13.0) | 12.7 (8.6–16.8) | 6.0 (2.8–9.2) | 10.3 (2.8–17.8) | 6.6 (3.7–9.6) | |||||
| Other | 45 | 8 | 67 | 11 | 67 | 16 | 3 | 6 | ||||
| 4.0 (1.9–6.1) | 3.2 (0.0–7.4) | 5.6 (3.9–7.2) | 4.7 (1.5–7.8) | 5.1 (3.5–6.7) | 6.7 (2.9–10.5) | 1.9 (0.0–4.5) | 1.3 (0.0–2.8) | |||||
| Educational level, N (%) | < 0.001 | < 0.001 | < 0.001 | 0.02 | ||||||||
| Less than high school | 429 | 153 | 396 | 113 | 330 | 106 | 30 | 216 | ||||
| 20.0 (17.0–22.9) | 36.9 (30.2–43.6) | 15.8 (13.4–18.3) | 25.2 (18.3–32.1) | 14.2 (12.4–16.0) | 22.4 (13.7–31.1) | 18.8 (9.0–28.6) | 32.1 (26.4–37.9) | |||||
| High school | 302 | 69 | 342 | 65 | 336 | 86 | 34 | 156 | ||||
| 23.8 (20.7–27.0) | 28.5 (23.2–33.8) | 23.9 (21.1–26.8) | 25.9 (22.0–29.8) | 24.3 (21.0–27.6) | 35.4 (25.8–45.0) | 28.7 (17.3–40.0) | 32.8 (27.7–37.8) | |||||
| College or higher | 615 | 87 | 813 | 132 | 796 | 96 | 56 | 171 | ||||
| 56.2 (51.8–60.5) | 34.6 (28.4–40.8) | 60.2 (55.9–64.5) | 48.9 (43.5–54.4) | 61.5 (59.0–63.9) | 42.2 (33.7–50.7) | 52.5 (37.0–68.0) | 35.1 (26.8–43.4) | |||||
| Poverty/income ratio, N (%) | 0.206 | 0.255 | 0.060 | 0.002 | ||||||||
| Low | 327 | 82 | 387 | 68 | 383 | 94 | 20 | 143 | ||||
| 20.3 (14.3–26.2) | 18.8 (8.9–28.8) | 19.4 (17.7–21.1) | 16.0 (10.0–22.0) | 18.8 (14.7–23.0) | 23.5 (15.6–31.4) | 12.4 (6.9–17.9) | 20.8 (16.8–24.8) | |||||
| Middle | 419 | 100 | 516 | 117 | 497 | 105 | 53 | 255 | ||||
| 29.2 (24.0–34.5) | 32.9 (23.8–41.9) | 30.1 (27.4–32.8) | 33.5 (25.4–41.7) | 33.9 (28.4–39.5) | 37.7 (30.9–44.5) | 43.4 (33.5–53.3) | 50.0 (43.8–56.2) | |||||
| High | 411 | 72 | 553 | 99 | 503 | 71 | 41 | 104 | ||||
| 40.2 (33.5–46.9) | 32.5 (18.0–47.0) | 44.5 (40.6–48.4) | 42.0 (32.8–51.2) | 42.0 (36.4–47.6) | 32.6 (22.9–42.2) | 37.2 (24.5–49.8) | 21.4 (16.4–26.4) | |||||
| Missing | 189 | 54 | 95 | 26 | 79 | 18 | 6 | 41 | ||||
| 10.3 (6.5–14.1) | 15.8 (6.7–25.0) | 6.0 (3.5–8.6) | 8.5 (4.9–12.1) | 5.3 (3.0–7.5) | 6.3 (3.8–8.7) | 7.1 (0.6–13.5) | 7.8 (4.7–10.8) | |||||
| Non-occupational noise exposure, N (%) | 0.18 | 0.10 | 0.49 | < 0.001 | ||||||||
| Yes | 267 | 49 | 364 | 84 | 393 | 72 | 8 | 97 | ||||
| 23.1 (19.7–26.4) | 19.5 (14.9–24.2) | 26.6 (23.5–29.6) | 34.0 (24.2–43.9) | 29.5 (26.5–32.5) | 27.2 (20.6–33.8) | 5.0 (1.4–8.5) | 15.6 (11.6–19.6) | |||||
| No | 1079 | 260 | 1187 | 226 | 1069 | 216 | 112 | 446 | ||||
| 76.9 (73.6–80.3) | 80.5 (75.8–85.1) | 73.4 (70.4–76.5) | 66.0 (56.1–75.8) | 70.5 (67.5–73.5) | 72.8 (66.2–79.5) | 95.0 (91.5–98.6) | 84.4 (80.4–88.4) | |||||
| Occupational noise exposure, N (%) | 0.002 | 0.11 | 0.35 | 0.02 | ||||||||
| Yes | 140 | 39 | 173 | 46 | 151 | 32 | 32 | 229 | ||||
| 11.5 (8.2–14.8) | 16.7 (9.9–23.5) | 12.0 (9.2–14.8) | 18.8 (11.8–25.7) | 11.7 (9.0–14.5) | 14.4 (8.7–20.1) | 20.2 (10.7–29.7) | 37.2 (31.7–42.8) | |||||
| No | 135 | 20 | 172 | 38 | 174 | 25 | 88 | 314 | ||||
| 12.3 (9.9–14.6) | 5.6 (1.8–9.5) | 13.0 (11.1–15.0) | 14.2 (9.0–19.4) | 14.1 (11.7–16.6) | 11.5 (7.0–16.1) | 79.8 (70.3–89.3) | 62.8 (57.2–68.3) | |||||
| Missing | 1071 | 250 | 1206 | 226 | 1137 | 231 | -c | -c | ||||
| 76.2 (72.8–79.6) | 77.7 (70.9–84.4) | 75.0 (72.4–77.5) | 67.0 (58.1–76.0) | 74.2 (70.2–78.1) | 74.0 (68.3–79.8) | |||||||
aThe estimates of the percentage of participants were weighted
bP values for overall differences in prevalence by stratum
cNo participants were observed in the sample
Table 2.
Characteristics of participants in NHANES according to the auditory threshold by cycle (2009–2018)
| Participants, N (%)a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009–2010 | 2011–2012 | 2015–2016 | 2017–2018 | |||||||||
| Characteristic | Normal hearing | Hearing loss | P valueb | Normal hearing | Hearing loss | P valueb | Normal hearing | Hearing loss | P valueb | Normal hearing | Hearing loss | P valueb |
| Overall | 187 | 685 | 3285 | 533 | 3589 | 674 | 202 | 414 | ||||
| Age, N (%) | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||
| 20–29 years | -c | -c | 828 | 12 | 840 | 14 | -c | -c | ||||
| 24.8 (19.6–30.0) | 2.4 (0.7–4.0) | 24.4 (22.1–26.7) | 1.8 (0.6–3.1) | |||||||||
| 30–39 years | -c | -c | 731 | 26 | 838 | 28 | -c | -c | ||||
| 21.5 (18.6–24.4) | 3.8 (2.0–5.6) | 22.8 (20.3–25.2) | 4.6 (2.0–7.1) | |||||||||
| 40–49 years | -c | -c | 671 | 67 | 787 | 73 | -c | -c | ||||
| 22.8 (19.9–25.6) | 14.4 (9.1–19.7) | 21.9 (19.7–24.1) | 12.6 (9.7–15.4) | |||||||||
| 50–59 years | -c | -c | 616 | 156 | 644 | 195 | -c | -c | ||||
| 19.8 (17.3–22.3) | 36.3 (30.0–42.7) | 19.1 (17.2–21.1) | 33.7 (28.3–39.2) | |||||||||
| 60–69 years | -c | -c | 439 | 272 | 480 | 364 | -c | -c | ||||
| 11.1 (8.9–13.3) | 43.1 (37.3–48.9) | 11.8 (9.8–13.8) | 47.3 (41.9–52.7) | |||||||||
| 70–79 years | 163 | 397 | -c | -c | -c | -c | 175 | 260 | ||||
| 87.4 (80.8–94.0) | 58.4 (55.0–61.7) | 89.0 (82.4–95.5) | 67.9 (62.7–73.0) | |||||||||
| 80 + years | 24 | 288 | -c | -c | -c | -c | 27 | 154 | ||||
| 12.6 (6.0–19.2) | 41.6 (38.3–45.0) | 11.0 (4.5–17.6) | 32.1 (27.0–37.3) | |||||||||
| Sex, N (%) | 0.002 | < 0.001 | < 0.001 | 0.65 | ||||||||
| Male | 59 | 349 | 1601 | 343 | 1606 | 430 | 78 | 192 | ||||
| 26.5 (17.9–35.2) | 43.2 (39.4–47.1) | 47.4 (45.2–49.7) | 65.6 (58.7–72.4) | 46.2 (45.0–47.5) | 64.2 (58.7–69.7) | 35.9 (28.4–43.3) | 38.1 (31.7–44.5) | |||||
| Female | 128 | 336 | 1684 | 190 | 1983 | 244 | 124 | 222 | ||||
| 73.5 (64.8–82.1) | 56.8 (52.9–60.6) | 52.6 (50.3–54.8) | 34.4 (27.6–41.3) | 53.8 (52.5–55.0) | 35.8 (30.3–41.3) | 64.1 (56.7–71.6) | 61.9 (55.5–68.3) | |||||
| Race, N (%) | < 0.001 | < 0.001 | < 0.001 | 0.66 | ||||||||
| Hispanic | 33 | 83 | 653 | 120 | 1098 | 262 | 31 | 53 | ||||
| 8.2 (1.2–15.2) | 5.7 (1.9–9.4) | 14.8 (9.5–20.2) | 10.4 (5.1–15.7) | 16.6 (10.7–22.4) | 13.7 (7.4–20.1) | 8.7 (5.1–12.4) | 7.6 (3.9–11.2) | |||||
| Non-Hispanic white | 101 | 497 | 1114 | 213 | 1051 | 222 | 93 | 232 | ||||
| 71.8 (63.8–79.8) | 85.2 (80.3–90.1) | 64.9 (56.4–73.3) | 75.8 (67.7–83.8) | 61.4 (52.8–69.9) | 70.8 (61.9–79.7) | 74.0 (68.0–79.9) | 78.1 (70.0–86.3) | |||||
| Non-Hispanic black | 41 | 82 | 936 | 123 | 834 | 107 | 51 | 77 | ||||
| 13.4 (7.7–19.2) | 6.5 (3.9–9.2) | 12.4 (7.4–17.4) | 7.0 (2.9–11.1) | 12.4 (7.5–17.3) | 7.3 (3.6–10.9) | 9.4 (5.3–13.4) | 7.9 (3.7–12.1) | |||||
| Other | 12 | 23 | 582 | 77 | 606 | 83 | 27 | 52 | ||||
| 6.6 (3.6–9.6) | 2.6 (1.2–4.0) | 7.9 (5.5–10.3) | 6.9 (4.2–9.5) | 9.6 (7.0–12.3) | 8.2 (4.7–11.8) | 7.9 (3.1–12.7) | 6.4 (2.5–10.3) | |||||
| Educational level, N (%) | 0.07 | < 0.001 | 0.04 | 0.002 | ||||||||
| Less than high school | 57 | 228 | 576 | 159 | 700 | 226 | 27 | 101 | ||||
| 21.3 (13.2–29.4) | 28.3 (21.9–34.7) | 13.0 (9.6–16.5) | 18.5 (12.9–24.1) | 12.5 (9.2–15.8) | 18.4 (11.7–25.0) | 7.0 (3.3–10.6) | 15.4 (12.2–18.5) | |||||
| High school | 37 | 171 | 666 | 137 | 774 | 150 | 47 | 106 | ||||
| 23.6 (17.7–29.6) | 26.7 (22.0–31.4) | 18.5 (15.4–21.6) | 27.1 (21.4–32.7) | 19.9 (17.7–22.2) | 18.8 (12.5–25.1) | 26.5 (19.0–34.0) | 29.6 (22.4–36.7) | |||||
| College or higher | 93 | 286 | 2043 | 237 | 2115 | 298 | 128 | 207 | ||||
| 55.0 (44.2–65.8) | 45.0 (38.4–51.7) | 68.5 (62.6–74.4) | 54.4 (46.2–62.6) | 67.6 (62.7–72.6) | 62.8 (55.3–70.3) | 66.5 (60.4–72.7) | 55.0 (47.8–62.3) | |||||
| Poverty/income ratio, N (%) | 0.200 | 0.263 | 0.444 | 0.436 | ||||||||
| Low | 37 | 159 | 1072 | 182 | 995 | 229 | 33 | 73 | ||||
| 14.6 (8.5–20.7) | 16.8 (13.5–20.1) | 23.2 (18.7–27.8) | 20.5 (15.8–25.1) | 19.1 (15.8–22.3) | 18.5 (13.6–23.4) | 9.1 (6.0–12.3) | 10.9 (7.8–14.0) | |||||
| Middle | 78 | 308 | 1004 | 160 | 1291 | 231 | 83 | 190 | ||||
| 41.6 (31.5–51.8) | 48.2 (42.0–54.4) | 30.9 (26.3–35.5) | 35.1 (26.4–43.8) | 33.7 (30.2–37.1) | 29.9 (23.0–36.8) | 38.3 (25.8–50.8) | 42.2 (31.9–52.6) | |||||
| High | 48 | 165 | 988 | 142 | 985 | 153 | 61 | 95 | ||||
| 31.9 (24.0–39.9) | 28.0 (21.6–34.5) | 40.9 (33.8–47.9) | 36.9( 28.2–45.6) | 40.5 (35.3–45.7) | 45.0 (34.6–55.4) | 42.8 (29.6–56.1) | 33.8 (22.6–45.0) | |||||
| Missing | 24 | 53 | 221 | 49 | 318 | 61 | 25 | 56 | ||||
| 11.8 (6.3–17.3) | 7.0 (4.6–9.3) | 5.0 (3.3–6.7) | 7.5 (3.0–12.0) | 6.8 (5.3–8.2) | 6.6 (3.4–9.7) | 9.7 (2.8–16.7) | 13.0 (8.2–17.8) | |||||
| Non-occupational noise exposure, N (%) | 0.31 | 0.38 | < 0.001 | 0.08 | ||||||||
| Yes | 15 | 79 | 396 | 72 | 474 | 137 | 9 | 39 | ||||
| 7.6 (2.3–12.9) | 10.3 (5.6–14.9) | 12.3 (10.2–14.4) | 15.0 (9.8–20.2) | 14.7 (12.8–16.6) | 24.6 (20.2–29.1) | 4.6 (0.4–8.8) | 8.4 (5.5–11.3) | |||||
| No | 172 | 606 | 2889 | 461 | 3115 | 537 | 193 | 375 | ||||
| 92.4 (87.1–97.7) | 89.7 (85.1–94.4) | 87.7 (85.6–89.8) | 85.0 (79.8–90.2) | 85.3 (83.4–87.2) | 75.4 (70.9–79.8) | 95.4 (9.2–99.6) | 91.6 (88.7–94.5) | |||||
| Occupational noise exposure, N (%) | < 0.001 | < 0.001 | < 0.001 | 0.12 | ||||||||
| Yes | 31 | 228 | 1064 | 242 | 1104 | 293 | 53 | 157 | ||||
| 13.1 (8.1–18.1) | 31.0 (26.8–35.1) | 33.0 (29.0–37.0) | 51.7 (42.0–61.4) | 31.1 (28.1–34.1) | 43.7 (38.9–48.6) | 23.7 (14.3–33.0) | 32.1 (25.1–39.0) | |||||
| No | 156 | 457 | 2221 | 291 | 2485 | 381 | 149 | 257 | ||||
| 86.9 (81.9–91.9) | 69.0 (64.9–73.2) | 67.0 (63.0–71.0) | 48.3 (38.6–58.0) | 68.9 (65.9–71.9) | 56.3 (51.4–61.1) | 76.3 (67.0–85.7) | 67.9 (61.0–74.9) | |||||
| Missing | -c | -c | -c | -c | -c | -c | -c | -c | ||||
aThe estimates of the percentage of participants were weighted
bP values for overall differences in prevalence by stratum
cNo participants were observed in the sample
Prevalence of and trend in hearing loss in the population
The prevalence of hearing loss in the sample overall was 19.1% (95% CI, 18.0–20.2%). It was significantly higher in the elderly, those with lower educational levels, and those who experienced noise exposure. Among people aged 20–69 years, the prevalence decreased from 15.6% (95% CI, 12.9–18.4%) in 1999–2000 to 14.9% (95% CI, 13.2–16.6%) in 2015–2016; among those aged 70 years or more it decreased from 79.9% (95% CI, 76.1–83.8%) in 2005–2006 to 64.5% (95% CI, 58.8–70.2%) in 2017–2018. However, the prevalence of hearing loss increased with age within the same survey cycle. The prevalence of hearing loss decreased significantly in the age groups 30–39, 60–69, 70–79, and 80 years and over (all P for trend < 0.05). A significant increase in the prevalence of hearing loss was observed in women, non-Hispanic whites, high school and college or higher educational level subgroups, middle PIR and high PIR subgroups, and those experiencing non-occupational noise exposure (all P for trend < 0.05). Detailed subgroup results are shown in Table 3.
Table 3.
Trends of the prevalence of hearing loss among the US adult population by cycle
| Variables | Overall | 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2009–2010 | 2011–2012 | 2015–2016 | 2017–2018 | P for trenda |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 6 | 7 | 8 | 9 | |||
| No. of participants overall | 15498 | 1655 | 1861 | 1750 | 663 | 872 | 3818 | 4263 | 616 | |
| No. of participants with hearing loss | 3756 | 309 | 310 | 288 | 543 | 685 | 533 | 674 | 414 | |
| Overall prevalenceb | 19.1 (18.0–20.2) | 15.6 (12.9–18.4) | 15.3 (12.7–17.8) | 14.8 (12.3–17.2) | 79.9 (76.1–83.8) | 79.1 (72.7–85.5) | 14.2 (12.3–16.2) | 14.9 (13.2–16.6) | 64.5 (58.8–70.2) | < 0.001 |
| Age, N (%) | ||||||||||
| 20–29 years | 2929 | 5 | 12 | 11 | -c | -c | 12 | 14 | -c | 0.29 |
| 1.4 (0.0–2.8) | 2.6 (0.7–4.6) | 3.5 (0.2–6.7) | 1.6 (0.6–2.6) | 1.3 (0.5–2.1) | ||||||
| 30–39 years | 2731 | 18 | 26 | 15 | -c | -c | 26 | 28 | -c | 0.03 |
| 5.0 (3.1–6.9) | 6.5 (2.8–10.1) | 3.8 (1.4–6.1) | 2.8 (1.6–4.0) | 3.4 (1.7–5.1) | ||||||
| 40–49 years | 2659 | 38 | 45 | 39 | -c | -c | 67 | 73 | -c | 0.17 |
| 11.4 (7.6–15.2) | 11.2 (8.1–14.4) | 10.7 (7.5–13.8) | 9.5 (6.3–12.7) | 9.1 (7.0–11.2) | ||||||
| 50–59 years | 2469 | 74 | 87 | 75 | -c | -c | 156 | 195 | -c | 0.18 |
| 26.9 (16.4–37.4) | 28.2 (21.8–34.6) | 28.1 (20.9–35.2) | 23.3 (19.1–27.5) | 23.6 (19.1–27.0) | ||||||
| 60–69 years | 2559 | 174 | 140 | 148 | -c | -c | 272 | 364 | -c | 0.02 |
| 52.3 (41.9–62.6) | 46.6 (38.2–55.0) | 44.0 (39.4–48.5) | 39.2 (32.6–45.8) | 41.2 (36.0–46.5) | ||||||
| 70–79 years | 1397 | -c | -c | -c | 301 | 397 | -c | -c | 260 | < 0.001 |
| 74.2 (68.4–80.0) | 74.2 (63.3–80.1) | 58.1 (51.4–64.8) | ||||||||
| 80 + years | 754 | -c | -c | -c | 242 | 288 | -c | -c | 154 | 0.03 |
| 91.9 (89.3–94.5) | 92.6 (88.1–97.1) | 84.1 (77.1–91.2) | ||||||||
| Sex, N (%) | ||||||||||
| Male | 7471 | 204 | 209 | 173 | 294 | 349 | 343 | 430 | 192 | 0.10 |
| 20.9 (17.2–24.5) | 22.2 (17.7–26.7) | 18.2 (14.4–22.1) | 85.8 (82.2–89.4) | 86.1 (80.6–91.6) | 18.6 (15.2–22.1) | 19.5 (17.5–21.6) | 65.9 (59.1–72.7) | |||
| Female | 8027 | 105 | 101 | 115 | 249 | 336 | 190 | 244 | 222 | < 0.001 |
| 10.4 (7.3–13.4) | 9.0 (6.8–11.3) | 11.5 (9.9–13.1) | 75.9 (70.7–81.1) | 74.5 (66.2–82.9) | 9.8 (8.0–11.6) | 10.4 (8.3–12.6) | 63.7 (55.9–71.5) | |||
| Race, N (%) | ||||||||||
| Hispanic | 3906 | 113 | 72 | 76 | 60 | 83 | 120 | 262 | 53 | 0.29 |
| 14.0 (10.3–17.8) | 11.0 (9.0–13.0) | 12.0 (8.0–16.0) | 86.5 (78.7–94.3) | 72.5 (60.3–84.7) | 10.4 (8.4–12.4) | 12.7 (10.4–14.9) | 61.1 (51.4–70.8) | |||
| Non-Hispanic white | 6499 | 139 | 170 | 161 | 409 | 497 | 213 | 222 | 232 | < 0.001 |
| 17.0 (13.4–20.5) | 16.9 (13.7–20.1) | 16.2 (13.8–18.5) | 80.4 (75.8–85.1) | 81.8 (74.9–88.7) | 16.2 (14.1–18.4) | 16.8 (14.7–18.9) | 65.7 (59.3–72.2) | |||
| Non-Hispanic black | 3408 | 49 | 57 | 35 | 68 | 82 | 123 | 107 | 77 | 0.09 |
| 10.8 (6.5–15.0) | 11.2 (7.4–15.1) | 7.6 (5.7–9.5) | 71.9 (63.3–80.5) | 64.8 (56.3–73.3) | 8.5 (6.1–10.9) | 9.3 (8.1–10.5) | 60.5 (51.2–69.8) | |||
| Other | 1685 | 8 | 11 | 16 | 6 | 23 | 77 | 83 | 52 | 0.53 |
| 12.8 (1.5–24.1) | 13.1 (9.3–17.0) | 18.6 (8.7–28.4) | 73.0 (73.0–73.0) | 59.9 (52.0–67.8) | 12.7 (8.6–16.7) | 13.0 (9.4–16.6) | 59.5 (50.1–68.9) | |||
| Educational level, N (%) | ||||||||||
| Less than high school | 3847 | 153 | 113 | 106 | 216 | 228 | 159 | 226 | 101 | 0.08 |
| 25.5 (20.5–30.6) | 22.3 (17.1–27.4) | 21.4 (14.3–28.5) | 87.2 (83.1–91.2) | 83.4 (77.0–89.8) | 19.0 (15.6–22.5) | 20.5 (16.6–24.3) | 80.0 (72.0–88.1) | |||
| High school/GED or equivalent | 3478 | 69 | 65 | 86 | 156 | 171 | 137 | 150 | 106 | < 0.001 |
| 18.1 (14.9–21.4) | 16.3 (12.7–19.9) | 20.2 (16.8–23.6) | 82.0 (75.4–88.6) | 81.1 (72.7–89.4) | 19.5 (16.1–23.0) | 14.2 (10.4–18.0) | 67.0 (58.6–75.4) | |||
| College or higher | 8173 | 87 | 132 | 96 | 171 | 286 | 237 | 298 | 207 | < 0.001 |
| 10.3 (7.8–12.7) | 12.8 (10.2–15.3) | 10.6 (7.5–13.8) | 72.7 (64.2–81.2) | 75.6 (68.2–83.0) | 11.6 (9.5–13.8) | 14.0 (11.8–16.2) | 60.1 (53.0–67.1) | |||
| Poverty/income ratio, N (%) | ||||||||||
| Low | 4284 | 82 | 68 | 94 | 143 | 159 | 182 | 229 | 73 | 0.15 |
| 14.7(9.4–20.0) | 12.9 (9.9–15.9) | 17.8 (13.5–22.1) | 87.0 (84.1–89.9) | 81.4 (72.0–90.8) | 12.7 (10.4–15.0) | 14.5 (12.1–16.9) | 68.4 (61.2–75.6) | |||
| Middle | 5407 | 100 | 117 | 105 | 255 | 308 | 160 | 231 | 190 | 0.03 |
| 17.2 (12.2–22.3) | 16.7 (11.8–21.6) | 16.1 (12.0–20.3) | 82.1 (77.3–86.9) | 81.4 (75.3–87.5) | 15.8 (11.6–20.0) | 13.5 (10.4–16.5) | 66.7 (55.9–77.6) | |||
| High | 4492 | 73 | 99 | 71 | 104 | 165 | 142 | 153 | 95 | < 0.001 |
| 13.0 (8.4–17.6) | 14.5 (11.3–17.8) | 11.9 (8.6–15.1) | 69.6 (61.7–77.6) | 76.9 (68.3–85.4) | 13.0 (10.1–16.0) | 16.3 (13.7–18.8) | 58.9 (49.2–68.6) | |||
| Missing | 1315 | 54 | 26 | 18 | 41 | 53 | 49 | 61 | 56 | 0.19 |
| 22.1 (14.2–30.1) | 20.3 (13.8–26.8) | 17.1 (11.0–23.1) | 81.4 (74.4–88.4) | 69.1 (54.2–84.1) | 19.9 (11.7–28.1) | 14.6 (8.5–20.6) | 70.8 (55.8–85.9) | |||
| Non-occupational noise exposure, N (%) | ||||||||||
| No | 12943 | 260 | 226 | 216 | 446 | 606 | 461 | 537 | 375 | 0.001 |
| 16.2 (13.4–19.1) | 13.9 (11.1–16.7) | 15.2 (12.3–18.1) | 78.0 (73.6–82.3) | 78.6 (72.8–84.5) | 13.8 (11.9–15.8) | 13.4 (11.5–15.3) | 63.6 (57.5–69.6) | |||
| Yes | 2555 | 49 | 84 | 72 | 97 | 79 | 72 | 137 | 39 | < 0.001 |
| 13.6 (9.4–17.8) | 18.8 (13.6–23.9) | 13.8(10.4–17.2) | 92.6 (87.4–97.7) | 83.6 (70.6–96.6) | 16.8 (10.3–23.3) | 22.7 (20.3–25.2) | 76.8 (67.4–86.1) | |||
| Occupational noise exposure, N (%) | ||||||||||
| No | 7363 | 20 | 38 | 25 | 314 | 457 | 291 | 381 | 257 | 0.49 |
| 7.8 (3.2–12.5) | 16.4 (10.8–22.0) | 12.4 (8.0–16.8) | 75.8 (69.0–82.6) | 75.0 (68.1–81.9) | 10.7 (8.9–12.4) | 12.5 (10.5–14.5) | 61.8 (54.0–69.6) | |||
| Yes | 4014 | 39 | 46 | 32 | 229 | 228 | 242 | 293 | 157 | 0.59 |
| 21.2 (16.7–25.7) | 22.0 (13.2–30.8) | 17.6 (11.1–24.0) | 88.0 (83.5–92.5) | 89.9 (85.2–94.7) | 20.6 (16.9–24.4) | 19.8 (17.4–22.2) | 71.1 (62.8–79.5) | |||
| Missing | 4121 | 250 | 226 | 231 | -c | -c | -c | -c | -c | 0.59 |
| 15.9 (12.5–19.3) | 13.9 (11.0–16.8) | 14.8 (12.3–17.2) | ||||||||
aP values for trends were calculated using weighted logistic regression models, which included the survey cycle as a continuous variable
bEstimates of the percentage of participants were weighted
cNo participants were observed in the sample
Prevalence of hearing loss by severity and unilateral hearing loss in the population
Table 4 shows the prevalence of hearing loss according to the severity of hearing loss by age and cycle. The prevalence of hearing-loss severity (mild hearing loss, moderate hearing loss, and moderately severe hearing loss) increased statistically significantly by cycle. The most prevalent type of hearing loss was mild (20 to < 35 dB). The prevalence of mild hearing loss was 12.0 to 45.1% and moderate hearing loss was 1.8 to 29.0% in each survey cycle.
Table 4.
Estimated prevalence of hearing loss grade in the US adult population
| Unilateral hearing loss | Mild hearing loss | Moderate hearing loss | Moderately severe hearing loss | |
|---|---|---|---|---|
| No. of participants overall | 208 | 2623 | 852 | 281 |
| Participants, N (%) | 1.3 (1.0–1.5) | 14.4 (13.6–15.2) | 3.6 (3.2–4.0) | 1.0 (0.8–1.3) |
| Cycle | ||||
| 1999–2000 | 22 | 247 | 49 | 13 |
| 1.1 (0.5–1.7) | 12.9 (11.0–14.8) | 2.3 (1.0–3.5) | 0.5 (0.1–0.9) | |
| 2001–2002 | 16 | 248 | 49 | 13 |
| 1.1 (0.7–1.5) | 12.4 (10.8–13.9) | 2.4 (1.4–3.4) | 0.5 (0.2–0.8) | |
| 2003–2004 | 30 | 240 | 37 | 11 |
| 1.5 (0.8–2.2) | 12.3 (10.2–14.5) | 2.0 (1.1–2.9) | 0.4 (0.0–0.9) | |
| 2005–2006 | 2 | 291 | 172 | 80 |
| 0.3 (0.0–0.8) | 45.1 (41.4–48.8) | 23.7 (20.8–26.6) | 11.0 (7.0–15.2) | |
| 2009–2010 | 6 | 351 | 245 | 89 |
| 0.8 (0.3–1.2) | 40.8 (37.0–44.7) | 29.0 (24.4–33.5) | 9.2 (7.5–11.1) | |
| 2011–2012 | 54 | 439 | 76 | 18 |
| 1.3 (0.9–1.7) | 12.0 (10.4–13.6) | 1.8 (1.2–2.4) | 0.5 (0.1–0.8) | |
| 2015–2016 | 70 | 549 | 102 | 23 |
| 1.5 (1.0–1.9) | 12.3 (10.7–13.9) | 2.1 (1.6–2.6) | 0.5 (0.2–0.8) | |
| 2017–2018 | 8 | 258 | 122 | 34 |
| 1.1 (0.1–2.1) | 40.8 (36.5–45.1) | 18.0 (13.8–22.1) | 5.8 (2.7–8.8) | |
| P for trend | 0.401 | < 0.001 | < 0.001 | 0.003 |
| Age, N (%) | ||||
| 20–29 years | 22 | 50 | 2 | 2 |
| 0.7 (0.2–1.2) | 2.0 (1.1–2.8) | 0.1 (0.0–0.2) | 0.0 (0.0–0.1) | |
| 30–39 years | 28 | 95 | 16 | 2 |
| 1.0 (0.5–1.5) | 3.7 (2.8–4.6) | 0.6 (0.1–1.0) | 0.1 (0.0–0.2) | |
| 40–49 years | 33 | 229 | 25 | 8 |
| 1.2 (0.6–1.9) | 8.9 (7.7–10.2) | 1.2 (0.5–1.9) | 0.3 (0.0–0.5) | |
| 50–59 years | 60 | 500 | 70 | 17 |
| 1.9 (1.3–2.6) | 22.3 (19.9–24.8) | 2.8 (1.8–3.7) | 0.7 (0.3–1.2) | |
| 60–69 years | 49 | 849 | 200 | 49 |
| 1.8 (1.1–2.6) | 33.9 (31.0–36.7) | 8.3 (6.8–9.9) | 1.8 (1.0–2.6) | |
| 70–79 years | 13 | 618 | 260 | 80 |
| 0.9 (0.3–1.4) | 44.6 (41.8–47.4) | 17.4 (14.6–20.2) | 5.4 (3.7–7.0) | |
| > 80 years | 3 | 282 | 279 | 123 |
| 0.4 (0.0–0.9) | 36.7 (33.2–40.3) | 37.2 (33.7–40.8) | 16.0 (12.6–19.5) | |
| P for trend | 0.01 | < 0.001 | < 0.001 | < 0.001 |
P values for trends were calculated using weighted logistic regression models, which included the survey cycle as a continuous variable
There was a statistically significant increasing trend in the prevalence of hearing-loss severity by age (all P for trend < 0·001). The prevalence of unilateral hearing loss was more prevalent in the 50–59 years old group, affecting 1.9% (95% CI, 1.3–2.6%) of subjects, as compared with 0.4% (95% CI, 0.0–0.9%) of subjects in the over 80 years old group; the prevalence across all age groups ranged from 0.4% to 1.9%. Mild hearing loss was the most common type of hearing loss in the 20–79 years old group, and the prevalence was the highest in the 70–79 years old group 44.6% (95% CI, 41.8–47.4%). In the over 80 years old group, the prevalence of moderate hearing loss (37.2% (95% CI, 33.7–40.8%)) exceeded that of mild hearing loss (36.7% (95% CI, 33.2–40.3%)).
Hearing thresholds of different frequencies in the otologically normal population
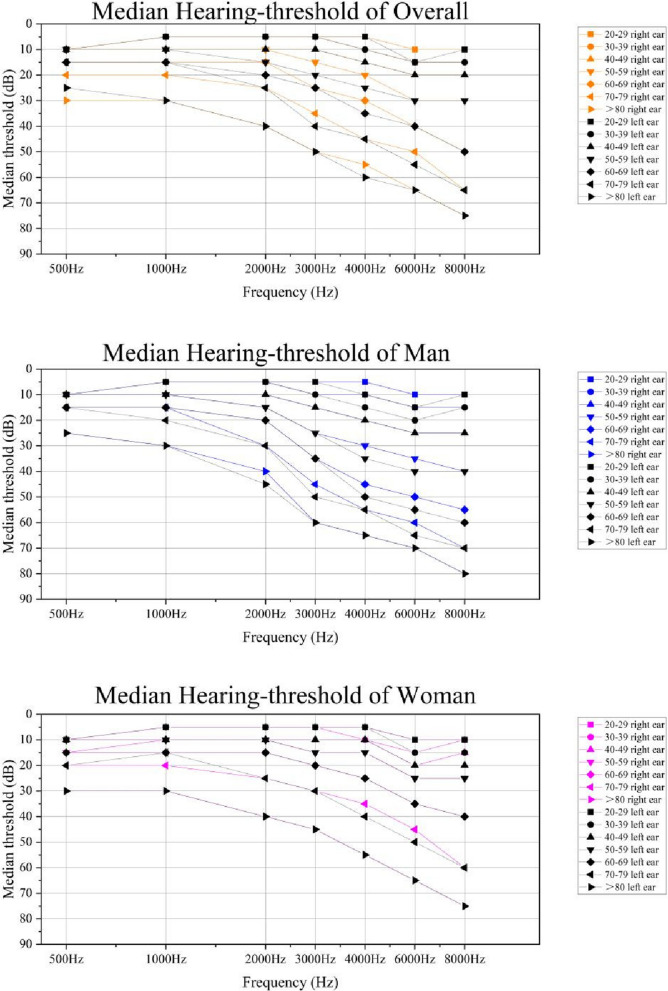
Figure 1 shows the median of pure tone thresholds (right ear and left ear) presented by age.
Fig. 1.
Median Hearing thresholds in dB as a function of frequencies at different ages
Based on hearing threshold testing of National Health and Nutrition Examination Survey (NHANES) data from 1999–2018. Data represent estimated median of pure-tone thresholds assessed in the right and left ear among U.S. adults of overall, male and female, by seven frequencies (500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz), NHANES1999-2018. Data were weighted to be nationally representative
Table 5 shows the pure tone thresholds (average of participant’s right ear and left ear) and the pure tone thresholds according to ISO 7029:2017 at the median, and the 10th, 25th, 75th, and 90th percentile values for men and women, according to age and frequency in the otologically normal population. Among the otologically normal population, hearing thresholds increased with age across the entire frequency range. Hearing thresholds for the otologically normal population tend to exceed the ISO age- and sex-adjusted thresholds. However, the hearing thresholds for the over 80 years old group were better than the theoretical ISO norm thresholds for 1000, 2000, 6000, and 8000 Hz.
Table 5.
Hearing thresholds (in decibels): comparison of the otologically normal population stratified by age and sex with standard values given in ISO 7029:2017 (Acoustics – Statistical distribution of hearing thresholds related to age and gender)
| Frequency (Hz) | Age (years) | Hearing threshold (dB) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | ||||||||||
| P10 | P25 | P50 | P75 | P90 | P10 | P25 | P50 | P75 | P90 | ||
| 500 | 20–29 | 0(-5) | 2.5(-3) | 5.0(0) | 10.0(4) | 15.0(8) | 0(-5) | 2.5(-2) | 7.5(0) | 10.0(4) | 15.0(7) |
| 30–39 | 0(-5) | 2.5(-3) | 7.5(0) | 12.5(4) | 17.5(8) | 0(-6) | 2.5(-3) | 7.5(0) | 10.0(4) | 15.0(8) | |
| 40–49 | 0(-5) | 2.5(-2) | 7.5(1) | 10.0(4) | 15.0(6) | 0(-5) | 2.5(-2) | 7.5(1) | 12.5(5) | 17.5(8) | |
| 50–59 | 0(-4) | 5.0(-1) | 7.5(3) | 12.5(6) | 20.0(10) | 2.5(-3) | 7.5(0) | 10.0(3) | 15.0(7) | 22.5(11) | |
| 60–69 | 2.5(-2) | 5.0(2) | 10.0(6) | 17.5(11) | 25.0(16) | 2.5(0) | 7.5(3) | 12.5(6) | 17.5(12) | 27.5(16) | |
| 70–79 | 5.0(3) | 7.5(6) | 15.0(10) | 22.5(17) | 22.5(23) | 5.0(3) | 10.0(7) | 12.5(12) | 25.0(18) | 32.5(24) | |
| > 80 | 15.0(8) | 15.0(12) | 15.0(16) | 27.5(24) | 35.0(32) | 12.5(6) | 22.5(12) | 22.5(19) | 30.0(27) | 35.0(35) | |
| 1000 | 20–29 | 0(-6) | 2.5(-3) | 5.0(0) | 7.5(4) | 12.5(7) | 0(-5) | 0(-3) | 2.5(0) | 5.0(3) | 10.0(7) |
| 30–39 | 0(-6) | 2.5(-3) | 7.5(0) | 10.0(4) | 15.0(8) | 0(-6) | 2.5(-3) | 5.0(0) | 10.0(4) | 15.0(8) | |
| 40–49 | 0(-4) | 5.0(-1) | 7.5(2) | 12.5(5) | 20.0(8) | 2.5(-5) | 5.0(-2) | 7.5(1) | 12.5(5) | 17.5(8) | |
| 50–59 | 2.5(-3) | 7.5(0) | 10.0(4) | 15.0(9) | 22.5(13) | 2.5(-3) | 7.5(0) | 10.0(4) | 12.5(8) | 20.0(12) | |
| 60–69 | 5.0(-1) | 7.5(3) | 12.5(8) | 20.0(15) | 25.0(21) | 5.0(1) | 7.5(4) | 12.5(8) | 17.5(13) | 30.0(19) | |
| 70–79 | 5.0(4) | 15.0(8) | 17.5(13) | 22.5(22) | 30.0(29) | 7.5(5) | 12.5(9) | 15.0(14) | 25.0(22) | 37.5(28) | |
| > 80 | 20.0(11) | 20.0(15) | 20.0(21) | 22.5(29) | 37.5(37) | 15.0(11) | 15.0(17) | 20.0(24) | 35.0(32) | 37.5(40) | |
| 2000 | 20–29 | -2.5(-6) | 0(-3) | 2.5(0) | 7.5(3) | 12.5(7) | -2.5(-5) | 0(-3) | 2.5(0) | 7.5(3) | 12.5(6) |
| 30–39 | -2.5(-6) | 0(-3) | 5.0(1) | 10.0(4) | 17.5(8) | 0(-6) | 2.5(-3) | 5.0(0) | 10.0(4) | 15.0(7) | |
| 40–49 | 0.0(-3) | 2.5(0) | 7.5(3) | 12.5(7) | 20.0(11) | 0(-5) | 2.5(-2) | 7.5(2) | 12.5(5) | 17.5(9) | |
| 50–59 | 2.5(-1) | 5.0(2) | 12.5(6) | 17.5(13) | 27.5(19) | 2.5(-2) | 5.0(1) | 10.0(5) | 15.0(10) | 20.0(14) | |
| 60–69 | 2.5(2) | 7.5(7) | 15.0(12) | 27.5(22) | 35.0(30) | 5.0(2) | 7.5(6) | 12.5(10) | 22.5(17) | 30.0(24) | |
| 70–79 | 12.5(8) | 17.5(14) | 25.0(21) | 60.0(31) | 60.0(39) | 5.0(7) | 12.5(13) | 20.0(19) | 35.0(28) | 40.0(35) | |
| > 80 | 32.5(18) | 32.5(24) | 40.0(32) | 40.0(40) | 40.0(47) | 12.5(17) | 22.5(24) | 27.5(32) | 40.0(41) | 52.5(49) | |
| 3000 | 20–29 | 0(-6) | 2.5(-3) | 5.0(0) | 10.0(3) | 15.0(7) | -2.5(-6) | 0(-3) | 2.5(0) | 7.5(3) | 10.0(7) |
| 30–39 | 0(-6) | 2.5(-3) | 7.5(1) | 12.5(5) | 20.0(8) | -2.5(-7) | 0(-3) | 5.0(0) | 10.0(4) | 15.0(8) | |
| 40–49 | 2.5(-3) | 7.5(0) | 12.5(4) | 20.0(9) | 32.5(13) | 0(-4) | 5.0(-1) | 7.5(2) | 12.5(6) | 20.0(10) | |
| 50–59 | 7.5(0) | 12.5(4) | 17.5(9) | 27.5(17) | 42.5(24) | 2.5(-1) | 7.5(2) | 12.5(6) | 17.5(12) | 25.0(17) | |
| 60–69 | 10.0(5) | 20.0(10) | 27.5(17) | 40.0(27) | 55.0(37) | 5.0(3) | 10.0(8) | 17.5(13) | 25.0(21) | 37.5(28) | |
| 70–79 | 15.0(12) | 22.5(19) | 27.5(27) | 62.5(38) | 62.5(48) | 12.5(10) | 17.5(16) | 27.5(23) | 42.5(33) | 47.5(41) | |
| > 80 | 37.5(25) | 37.5(33) | 52.5(41) | 52.5(47) | 55.0(53) | 17.5(22) | 27.5(30) | 40.0(38) | 45.0(48) | 57.5(57) | |
| 4000 | 20–29 | -2.5(-6) | 2.5(-3) | 5.0(0) | 10.0(4) | 15.0(7) | -5(-6) | 0(-3) | 5.0(0) | 7.5(4) | 12.5(7) |
| 30–39 | 0(-6) | 5.0(-2) | 10.0(1) | 17.5(5) | 25.0(9) | -2.5(-7) | 2.5(-3) | 5.0(1) | 12.5(5) | 15.0(8) | |
| 40–49 | 7.5(-2) | 10.0(1) | 15.0(4) | 25.0(10) | 37.5(15) | 2.5(-4) | 5.0(-1) | 10.0(3) | 15.0(7) | 22.5(11) | |
| 50–59 | 7.5(2) | 15.0(6) | 22.5(11) | 35.0(20) | 50.0(28) | 5.0(-1) | 10.0(3) | 12.5(7) | 20.0(14) | 27.5(19) | |
| 60–69 | 12.5(7) | 25.0(13) | 35.0(20) | 50.0(32) | 67.5(43) | 7.5(4) | 12.5(9) | 20.0(15) | 30.0(24) | 45.0(32) | |
| 70–79 | 22.5(16) | 32.5(24) | 40.0(33) | 65.0(45) | 65.0(55) | 17.5(12) | 25.0(19) | 47.5(27) | 52.5(37) | 62.5(46) | |
| > 80 | 50.0(32) | 50.0(40) | 55.0(50) | 55.0(55) | 60.0(59) | 25.0(27) | 35.0(35) | 40.0(43) | 52.5(53) | 67.5(62) | |
| 6000 | 20–29 | 2.5(-6) | 7.5(-3) | 12.5(0) | 17.5(4) | 22.5(8) | 2.5(-6) | 7.5(-3) | 10.0(0) | 17.5(4) | 22.5(8) |
| 30–39 | 5(-6) | 7.5(-2) | 15.0(1) | 20.0(6) | 30.0(11) | 5.0(-7) | 10.0(-3) | 12.5(1) | 17.5(6) | 25.0(10) | |
| 40–49 | 10(-2) | 15.0(2) | 22.5(6) | 27.5(13) | 37.5(19) | 7.5(-4) | 12.5(-1) | 17.5(4) | 25.0(9) | 32.5(14) | |
| 50–59 | 15(3) | 20.0(8) | 25.0(14) | 42.5(25) | 57.5(35) | 12.5(-1) | 15.0(4) | 22.5(10) | 30.0(17) | 40.0(24) | |
| 60–69 | 17.5(10) | 32.5(18) | 45.0(26) | 60.0(40) | 72.5(53) | 15.0(5) | 20.0(12) | 27.5(19) | 42.5(30) | 57.5(39) | |
| 70–79 | 35(22) | 35.0(32) | 55.0(43) | 62.5(55) | 70.0(66) | 17.5(15) | 25.0(24) | 45.0(33) | 52.5(45) | 65.0(56) | |
| > 80 | 57.5(43) | 57.5(53) | 60.0(64) | 60.0(66) | 87.5(69) | 27.5(35) | 42.5(43) | 47.5(52) | 70.0(62) | 72.5(72) | |
| 8000 | 20–29 | 2.5(-6) | 5.0(-3) | 10.0(0) | 15.0(5) | 22.5(9) | 2.5(-6) | 7.5(-3) | 10.0(0) | 17.5(5) | 20.0(9) |
| 30–39 | 5(-6) | 7.5(-2) | 12.5(2) | 20.0(7) | 27.5(12) | 5.0(-7) | 10.0(-3) | 12.5(1) | 20.0(7) | 25.0(11) | |
| 40–49 | 10(-2) | 15.0(2) | 22.5(7) | 32.5(15) | 40.0(22) | 7.5(-4) | 12.5(0) | 17.5(5) | 25.0(11) | 35.0(17) | |
| 50–59 | 17.5(4) | 25.0(10) | 32.5(16) | 45.0(29) | 65.0(40) | 12.5(0) | 17.5(6) | 25.0(12) | 35.0(21) | 45.0(29) | |
| 60–69 | 20(13) | 37.5(21) | 57.5(30) | 72.5(46) | 85.0(60) | 20.0(6) | 25.0(14) | 37.5(23) | 52.5(35) | 70.0(45) | |
| 70–79 | 42.5(26) | 57.5(37) | 57.5(50) | 65.0(63) | 75.0(74) | 22.5(18) | 27.5(28) | 52.5(39) | 60.0(52) | 70.0(63) | |
| > 80 | 62.5(44) | 62.5(59) | 65.0(75) | 65.0(76) | 77.5(77) | 32.5(40) | 37.5(49) | 57.5(60) | 67.5(70) | 77.5(80) | |
() = ISO 7029:2017 (Acoustics – Statistical distribution of hearing thresholds related to age and gender)
The median values of hearing thresholds in men in over 80 years old group tended to be better than the ISO 7029:2017 values for 500, 1000, 6000, and 8000 Hz, whereas they were worse for very high frequencies.
Our results show lower median values across the entire frequency range (except for 500 and 3,000 Hz) for women in over 80 years old group, compared with those given in ISO 7029:2017, Compared with the ISO 7029:2017 norms for women over 80 years old, the thresholds obtained in this study were better for 1000, 2000, 3000, 4000, 6000, and 8000 Hz but worse for 500 Hz.
Discussion
In this study we used the temporal cross-sectional data from NHANES (1999 to 2018) to explore temporal trends in the prevalence of hearing loss among adults in the USA. It was found that, overall, there has been a statistically significant decrease in the prevalence of hearing loss among US adults over the years studied. However, the severity of hearing loss statistically significantly increased by cycle. Among US adults, mild hearing loss was more prevalent in those aged 20–79 years, while in those aged over 80 years the prevalence of moderate hearing loss exceeded that of mild loss. The prevalence of hearing loss also varied significantly by age group, sex, race, educational level, PIR, and noise exposure. Over the study period, the prevalence of hearing loss increased significantly among women, non-Hispanic whites, those with high school and college or higher educational levels, those with a middle or high PIR, and those experiencing non-occupational noise exposure.
While the prevalence of hearing loss in US adults showed a decreasing trend, the severity of hearing loss increased by cycles. A number of factors could account for the decrease in the prevalence of hearing loss, including demographic shifts, lifestyle changes, increased awareness of using hearing protection, increased noise control measures, and improvements in the accessibility and affordability of hearing care [7, 9, 12]. Hearing loss is a progressive process that, without appropriate intervention, gradually worsens over time. The lack of adequate coverage and the low uptake of hearing healthcare have contributed to the annual increase in the severity of hearing loss [15, 16].
We observed that age was significantly associated with the prevalence of hearing loss. In some age subgroups (30–39, 60–69, 70–79, and > 80 years), the prevalence of hearing loss decreased by cycle. In the present study, the prevalence of unilateral hearing loss did not simply increase with age, but increased up to a certain age group and then decreased. The prevalence of unilateral hearing loss increased from 20 to 59 years old, and decreased after age 60 years. This finding is consistent with reports in the current literature [17, 18]. The prevalence of age-related hearing loss (ARHL) would be expected to increase as the number of older Americans increases due to aging of the population. ARHL is not a single event but the result of multiple factors (such as genetic, biological, social, psychological, and environmental factors) experienced from prenatal to childhood and adulthood to old age. The opposite result observed in our study may be related to the delayed onset of ARHL due to the delay in the onset of chronic disease due to following a healthy lifestyle, which effectively reduces the burden of age-related disease [15]. In recent years, the risk of ARHL may have been greatly reduced by people making healthy lifestyle choices, such as following a good diet, engaging in physical activity, and avoiding smoking, in addition to engaging in preventive behaviors such as ensuring protection from loud noise [19].
In our study, the prevalence of hearing loss in men was higher than that in women, but it was increasing by cycle in women. Hearing loss in women may be related to decreased estrogen. Numerous studies have demonstrated that estrogen has a positive effect on hearing function [20], and the hearing threshold declines in post-menopausal women due to the decline in estrogen levels. Therefore, as the population ages, the gender difference between the prevalence of hearing loss will reduce, as the prevalence of hearing loss in women increases by cycle. Even though the prevalence of hearing loss in men shows no significant overall temporal trend, it is still a significant concern because the prevalence in men is higher than in women. Studies have shown that men are more likely to suffer from noise-induced hearing loss (NIHL) [21].
We also found in this study that non-Hispanic blacks have a lower prevalence of hearing loss than other racial groups, while non-Hispanic whites are more likely to have hearing loss. This finding is similar to the findings of some previous studies [11, 12, 22]. However, evidence from previous studies suggests that hearing loss is very common among black and Hispanic subgroups, including Mexicans and Cubans [23]. Their culture, perceptions concerning hearing protection, and factors associated with changing one’s behavior may contribute to differences in hearing loss between ethnicities.
The findings from our study suggested that the higher the level of education [10] the lower the likelihood that a person will experience hearing loss. This may be related to the fact that people with a higher educational level are more likely to have access to an environment with less noise exposure and more resources for hearing protection [24].
This study showed an increased prevalence of hearing loss in the group who experienced noise exposure. Noise exposure is an important factor in hearing loss, and is strongly related to sex and occupation [25], which may have contributed to the higher prevalence of hearing loss in men and those who experience occupational noise exposure. Although the preventive strategy and measurements made to prevent hearing loss due to exposure to noise have gradually improved in the USA, there is room for further improvement [26]. The increase in hearing loss due to occupational noise exposure may be related to existing regulations for noise in the workplace, which strike a balance between hearing protection and economic development, underestimate the adverse health and social costs of noise-induced hearing loss, and do not fully protect workers from hearing injury [27]. On the other hand, as an economy develops, people have more opportunities and time to be exposed to recreational noise. Although noise control policies and regulations in entertainment venues have been developed to help people avoid exposure to loud noise [28, 29], the increasing prevalence of hearing loss associated with non-occupational noise exposure indicates that more effective measures regarding noise control and hearing protection are needed.
Hearing thresholds for otologically normal population tend to exceed the ISO 7029:2017 age- and sex-adjusted hearing thresholds. However, with respect to the percentile values of hearing threshold distributions observed in the otologically normal population, hearing sensitivity was found to be less pronounced in the over 80 years old group at all frequencies, except for 500 kHz, than as described in ISO 7029:2017. Similar findings have been reported in some other studies [30, 31]. This finding may be related to genetic disposition and the change of lifestyle.
The findings of our study have important public health implications. To reduce the growing burden of hearing loss in the USA, better integrated interventions for hearing healthcare need to be developed through periodic evaluation of the trend in hearing loss and a better understanding of the risk factors for hearing loss. The epidemiological information provided by this study comprehensively illustrate the change in the prevalence of hearing loss, and provide an understanding of the developing trend of hearing loss. Our study may provide valuable insights for those who need to understand the hearing needs of a population, make public health plans related to hearing, and make policy decisions and allocate resources for hearing care. The results of this study show that the hearing threshold levels for each frequency have changed. Our data can provide a reference for updating the ISO 7029:2017 age- and sex-adjusted hearing thresholds, in order to bring the standard more in line with the real-world situation in the population.
In this study we analyzed the nationally representative auditory data for 1999–2018 from NHANES to calculate the prevalence of and estimate the trends in hearing loss among adults. Few prior studies have evaluated hearing-loss trends over such an extended period. Furthermore, in NHANES, hearing loss was assessed using the gold standard objective audiometric measurement, which has been proven to be reliable in many studies. However, the limitations of this study should be considered. First, this study was cross-sectional and therefore could not examine the causality of the association of potential risk factors with hearing loss. Moreover, because of the NHANES study design, the age of the study participants was not continuous in the cycle, which was not conducive to extrapolation, and therefore more studies are needed that involve carrying out this hearing test on the same age group. Finally, Selective bias has been addressed as far as possible by adjusting the weights to make the population representative. Measurement error caused by the change of the measurement instrument in audiometric methods is likely to exist.
Conclusions
In this survey study, the estimated prevalence of hearing loss decreased from 1999 to 2018; the prevalence among those aged 60 years or older remained high but decreased. Mild hearing loss was more prevalent among US adults aged 20–79 years, while in those aged over 80 years the prevalence of moderate hearing loss exceeded that of mild loss. We observed that hearing thresholds tend to exceed the ISO 7029:2017 age- and sex-adjusted hearing thresholds for the otologically normal population, while the percentile of the hearing threshold distribution for people over 80 years old is lower than given in ISO 7029:2017. It is of great importance to continue to monitor hearing threshold distributions in the elderly, the trends in hearing loss, and the factors that influence hearing loss in the same age groups looked at in this study.
Acknowledgements
We appreciate the efforts of all the researchers who collected National Health and Examination Survey (NHANES) data sets, the Centers for Disease Control and Prevention, and individuals who participated in the NHANES studies. We would like to thank Miss Julie Gorman (senior copyeditor, UK) and Jessie Chan (Academic Client Service Manager, China) from New Bridge Translation (www.newbridgetranslation.com.cn) for their excellent language services, including translating and copyediting with academic integrity.
Abbreviations
- U.S.
United States
- GBD
Global Burden of Disease Study
- YLDs
Years lived with disability
- WHO
World Health Organization
- NHANES
National Health and Nutrition Examination Survey
- CDC
Center for Health Statistics ant the Centers for Disease Control and Prevention
- NIOSH
National Institute for Occupational Safety and Health
- MEC
Mobile Examination Center
- PTA
Pure-tone average
- PIR
Poverty/income ratio
- ARHL
Age-related hearing loss
- NIHL
Noise-induced hearing loss
- P10
10Th percentile
- P25
25Th percentile
- P50
50Th percentile
- P75
75Th percentile
- P90
90Th percentile
Authors’ contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. QC, LW and WY had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: FM, WY, QC, and LW. Acquisition, analysis, or interpretation of data: FM, SZ, QZ, XY, HJ, QC, and WY Drafting of the manuscript: FM, WY, QC, and LW. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: FM, SZ, and QZ. Administrative, technical, or material support: WY, QC, and LW. Interpretation of data: All authors. Supervision: QC, LW. Conflict of Interest Disclosures: None reported.
Funding
Not applicable.
Availability of data and materials
The datasets analyzed during the current study are available in the NHANES repository, https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
Declarations
Ethics approval and consent to participate
NHANES has been approved by the NCHS Ethics Review Board. Data are released in 2-year cycles and are made publicly available online. Written informed consent is obtained from all survey participants. The Guangdong Pharmaceutical University Academic Review Board determined that the present study was exempt from approval because of the use of de-identified data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Wenhan Yang, Email: wenhan-yang@gdpu.edu.cn.
Liang Wang, Email: Liang_Wang1@baylor.edu.
Qingsong Chen, Email: cqs@gdpu.edu.cn.
References
- 1.McDaid D, Park A, Chadha S. Estimating the global costs of hearing loss. Int J Audiol. 2021;60(3):162–170. doi: 10.1080/14992027.2021.1883197. [DOI] [PubMed] [Google Scholar]
- 2.Emmett SD, Francis HW. The socioeconomic impact of hearing loss in U.S. adults. Otol Neurotol. 2015;36(3):545–550. doi: 10.1097/MAO.0000000000000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haile LM, Abdoli A, Abdollahi M, Akalu Y, Alanezi FM, Alanzi TM, Alipour V, Al-Raddadi RM, Amu H, Ashbaugh C, et al. Hearing loss prevalence and years lived with disability, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet. 2021;397(10278):996–1009. doi: 10.1016/S0140-6736(21)00516-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shukla A, Harper M, Pedersen E, Goman A, Suen JJ, Price C, Applebaum J, Hoyer M, Lin FR, Reed NS. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryng Head Neck. 2020;162(5):622–633. doi: 10.1177/0194599820910377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huddle MG, Goman AM, Kernizan FC, Foley DM, Price C, Frick KD, Lin FR. The economic impact of adult hearing loss: a systematic review. JAMA Otolaryngol. 2017;143(10):1040–1048. doi: 10.1001/jamaoto.2017.1243. [DOI] [PubMed] [Google Scholar]
- 6.Barker AB, Leighton P, Ferguson MA. Coping together with hearing loss: a qualitative meta-synthesis of the psychosocial experiences of people with hearing loss and their communication partners. Int J Audiol. 2017;56(5):297–305. doi: 10.1080/14992027.2017.1286695. [DOI] [PubMed] [Google Scholar]
- 7.Organization WH . World report on hearing. 2021. [Google Scholar]
- 8.Olusanya BO, Davis AC, Hoffman HJ. Hearing loss: rising prevalence and impact. B World Health Organ. 2019;97(10):646. doi: 10.2471/BLT.19.224683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cunningham LL, Tucci DL. Hearing loss in adults. N Engl J Med. 2017;377(25):2465–2473. doi: 10.1056/NEJMra1616601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yuri Agrawal EAPJ. Prevalence of hearing loss and differences by demographic characteristics among US adults data from the national health and nutrition examination survey, 1999–2004. Arch Intern Med. 2008;14(168):1522–1530. doi: 10.1001/archinte.168.14.1522. [DOI] [PubMed] [Google Scholar]
- 11.Goman AM, Lin FR. Prevalence of hearing loss by severity in the United States. Am J Public Health. 2016;106(10):1820–1822. doi: 10.2105/AJPH.2016.303299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffman HJ, Dobie RA, Losonczy KG, Themann CL, Flamme GA. Declining prevalence of hearing loss in US adults aged 20 to 69 years. JAMA Otolaryngol Head Neck Surg. 2017;143(3):274. doi: 10.1001/jamaoto.2016.3527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dillard LK, Nelson-Bakkum ER, Walsh MC, Schultz A. Self-reported hearing loss is associated with poorer perceived health care access, timeliness, satisfaction, and quality: findings from the survey of the health of Wisconsin. Disabil Health J. 2023;16(1):101394. doi: 10.1016/j.dhjo.2022.101394. [DOI] [PubMed] [Google Scholar]
- 14.Nayu Ikeda CJLM. Tracking population health based on self-reported impairments: trends in the prevalence of hearing loss in US adults, 1976–2006. Am J Epidemiol. 2009;170(1):80–87. doi: 10.1093/aje/kwp097. [DOI] [PubMed] [Google Scholar]
- 15.Adults COAA, Policy BOHS, Division HAM, National Academies of Sciences EAM . Hearing health care for adults: priorities for improving access and affordability. Washington, DC: National Academies Press (US); 2016. [PubMed] [Google Scholar]
- 16.Goman AM, Reed NS, Lin FR. Addressing estimated hearing loss in adults in 2060. JAMA Otolaryngol. 2017;143(7):733–734. doi: 10.1001/jamaoto.2016.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jun HJ, Hwang SY, Lee SH, Lee JE, Song J, Chae S. The prevalence of hearing loss in South Korea: data from a population-based study. Laryngoscope. 2015;125(3):690–694. doi: 10.1002/lary.24913. [DOI] [PubMed] [Google Scholar]
- 18.Golub JS, Lin FR, Lustig LR, Lalwani AK. Prevalence of adult unilateral hearing loss and hearing aid use in the United States. Laryngoscope. 2018;128(7):1681–1686. doi: 10.1002/lary.27017. [DOI] [PubMed] [Google Scholar]
- 19.Davis A, McMahon CM, Pichora-Fuller KM, Russ S, Lin F, Olusanya BO, Chadha S, Tremblay KL. Aging and hearing health: the life-course approach. Gerontologist. 2016;56 Suppl 2(Suppl 2):S256–S267. doi: 10.1093/geront/gnw033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shuster BZ, Depireux DA, Mong JA, Hertzano R. Sex differences in hearing: probing the role of estrogen signaling. J Acoust Soc Am. 2019;145(6):3656. doi: 10.1121/1.5111870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villavisanis DF, Berson ER, Lauer AM, Cosetti MK, Schrode KM. Sex-based differences in hearing loss: perspectives from non-clinical research to clinical outcomess. Otol Neurotol. 2020;41(3):290–298. doi: 10.1097/MAO.0000000000002507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Su BM, Chan DK. Prevalence of hearing loss in US children and adolescents. JAMA Otolaryngol Head Neck Surg. 2017;143(9):920. doi: 10.1001/jamaoto.2017.0953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lor M, Thao S, Misurelli SM. Review of hearing loss among racial/ethnic minorities in the United States. Western J Nurs Res. 2021;43(9):859–876. doi: 10.1177/0193945920976402. [DOI] [PubMed] [Google Scholar]
- 24.Agrawal Y, Niparko JK, Dobie RA. Estimating the effect of occupational noise exposure on hearing thresholds: the importance of adjusting for confounding variables. Ear Hearing. 2010;31(2):234–237. doi: 10.1097/AUD.0b013e3181c6b9fd. [DOI] [PubMed] [Google Scholar]
- 25.Flamme GA, Stephenson MR, Deiters K, Tatro A, van Gessel D, Geda K, Wyllys K, McGregor K. Typical noise exposure in daily life. Int J Audiol. 2012;51 Suppl 1(01):S3–S11. doi: 10.3109/14992027.2011.635316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerr MJ, Neitzel RL, Hong O, Sataloff RT. Historical review of efforts to reduce noise-induced hearing loss in the United States. Am J Ind Med. 2017;60(6):569–577. doi: 10.1002/ajim.22627. [DOI] [PubMed] [Google Scholar]
- 27.Sheppard A, Ralli M, Gilardi A, Salvi R. Occupational noise: auditory and non-auditory consequences. Int J Environ Res Public Health. 2020;17(23):8963. doi: 10.3390/ijerph17238963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beach EF, Cowan R, Mulder J, O Brien I. Applying the hierarchy of hazard control to regulation of sound levels in entertainment venues. Ann Work Expos Heal. 2020;64(4):342–349. doi: 10.1093/annweh/wxaa018. [DOI] [PubMed] [Google Scholar]
- 29.Beach EF, Mulder J, O Brien I, Cowan R. Overview of laws and regulations aimed at protecting the hearing of patrons within entertainment venues. Eur J Public Health. 2021;31(1):227–233. doi: 10.1093/eurpub/ckaa149. [DOI] [PubMed] [Google Scholar]
- 30.von Gablenz P, Holube I. Hearing threshold distribution and effect of screening in a population-based German sample. Int J Audiol. 2016;55(2):110–125. doi: 10.3109/14992027.2015.1084054. [DOI] [PubMed] [Google Scholar]
- 31.Williams W, Carter L, Seeto M. Hearing threshold levels for a population of 11 to 35 year old Australian females and males. Int J Audiol. 2014;53(5):289–293. doi: 10.3109/14992027.2013.873957. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available in the NHANES repository, https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.