ABSTRACT
Background: Complex post-traumatic stress disorder (CPTSD) describes chronic disturbances in self-organization (i.e. affect dysregulation; negative self-concept; severe difficulties in relationships) which are frequently observed in survivors of prolonged, repeated or multiple traumatic stressors. So far, evidence of psychodynamic treatment approaches for CPTSD is scarce.
Methods: In this single-centre observational pilot study, symptom change during a 6-week psychodynamic inpatient treatment in a multimodal psychosomatic rehabilitation centre was evaluated using repeated measures analyses of variance (ANOVAs). Patients completed questionnaires on PTSD and CPTSD symptoms (ITQ), anxiety, depression and somatization (BSI-18), functional impairment (WHODAS) and epistemic trust, mistrust and credulity (ETMCQ) before (T1) and at the end of treatment (T2). A hierarchical linear regression analysis was calculated to identify factors associated with improved CPTSD symptoms.
Results: A total of n = 50 patients with CPTSD were included in the study, of whom n = 40 (80%) completed treatment. Patients reported a significant reduction of CPTSD symptoms during treatment with a large effect size (−3.9 points; p < .001; η2 = .36), as well as a significant reduction of psychological distress (p < .001; η2 = .55) and functional impairment (p < .001; η2 = .59). At the end of treatment, 41.0% of patients no longer fulfilled the diagnostic criteria for CPTSD. Changes in epistemic stance included improved epistemic trust (β = –.34, p = .026) and decreased epistemic credulity (β = .37, p = .017), which together with lower age (β = .43, p = .012) and lower depression levels at baseline (β = .35, p = .054) were significantly associated with baseline adjusted mean change of CPTSD symptoms during therapy and explained 48% of its variance.
Discussion: In our study, patients reported a significant reduction of CPTSD symptoms and comorbid symptoms during a multimodal psychodynamic inpatient rehabilitation treatment. Improved epistemic trust may facilitate the establishment of a trusting therapeutic relationship, thus fostering an environment of openness for knowledge transfer (i.e. social learning) and the exploration of diverse viewpoints and perspectives in the therapeutic process.
KEYWORDS: Epistemic trust, psychosomatics, psychotherapy, psychodynamic, CPTSD, trauma, rehabilitation, inpatient
HIGHLIGHTS
Complex post-traumatic stress disorder (CPTSD) is a condition often found in individuals who have experienced severe trauma, such as childhood abuse or torture.
A study involving 50 patients with CPTSD showed significant improvements in symptoms and overall quality of life after undergoing a 6-week integrative multimodal psychodynamic inpatient rehabilitation treatment.
The study also highlighted that improvement in epistemic trust could be a potential mechanism of change contributing to the positive therapeutic outcomes.
Abstract
Antecedentes: El trastorno por estrés postraumático complejo (TEPTC) describe alteraciones crónicas en la autoorganización (es decir, desregulación afectiva; autoconcepto negativo; dificultades graves en las relaciones) que se observan con frecuencia en sobrevivientes de estresores traumáticos prolongados, repetidos o múltiples. Hasta ahora, hay escasa evidencia de enfoques de tratamiento psicodinámico para el TEPTC.
Método: En este estudio piloto observacional unicéntrico, se evaluó el cambio en los síntomas durante un tratamiento psicodinámico de seis semanas para pacientes hospitalizados en un centro de rehabilitación psicosomático multimodal, mediante el análisis de varianza de medidas repetidas (ANOVAs). Los pacientes completaron cuestionarios sobre síntomas de TEPT y TEPTC (ITQ), ansiedad, depresión y somatización (BSI-18), deterioro funcional (WHODAS) y confianza epistémica, desconfianza y credulidad (ETMCQ) antes (T1) y al final del tratamiento (T2). Se realizó un análisis de regresión lineal jerárquica para identificar los factores asociados con la mejoría de los síntomas del TEPTC.
Resultados: Un total de n = 50 pacientes con TEPTC fueron incluidos en el estudio, de los cuales n = 40 (80%) completaron el tratamiento. Los pacientes reportaron una reducción significativa de los síntomas del TEPTC durante el tratamiento con una gran magnitud del efecto (−3,9 puntos; p < .001; η2 = 0,36), así como una reducción significativa del malestar psicológico (p < .001; η2 = 0,55) y del deterioro funcional (p < .001; η2 = 0,59). Al final del tratamiento, el 41,0% de los pacientes ya no cumplían los criterios diagnósticos para TEPTC. Los cambios en la postura epistémica incluyeron una mejoría en la confianza epistémica (β = −0,34, p = .026) y disminución de la credulidad epistémica (β = 0,37, p = .017), que junto con una menor edad (β = 0,43, p = .012) y niveles más bajos de depresión al inicio (β = 0,35, p = .054) se asociaron significativamente con el cambio medio ajustado al inicio de los síntomas del TEPTC durante la terapia y explicaron el 48% de su varianza.
Discusión: En nuestro estudio, los pacientes informaron de una reducción significativa de los síntomas de TEPTC y de los síntomas comórbidos durante un tratamiento de rehabilitación psicodinámico multimodal para pacientes hospitalizados. Una mejoría en la confianza epistémica puede facilitar el establecimiento de una relación terapéutica de confianza, fomentando así un ambiente de apertura para la transferencia de conocimientos (es decir, el aprendizaje social) y la exploración de diversos puntos de vista y perspectivas en el proceso terapéutico.
PALABRAS CLAVES: Confianza epistémica, psicosomática, psicoterapia, psicodinámica, TEPTC, trauma, rehabilitación, hospitalización
1. Background
In 1992, Judith Herman introduced the concept of complex post-traumatic stress disorder (CPTSD) to describe the specific symptoms experienced by survivors of prolonged, repeated or multiple traumatic stressors (e.g. childhood sexual or physical abuse, domestic violence, genocide and torture) in addition to general PTSD symptoms (Herman, 1992). While this concept had not been included in the diagnostic classification systems for almost two decades, the new version of the International Classification of Diseases (ICD-11) by the World Health Organization (WHO) introduces the diagnostic entity of CPTSD (Maercker et al., 2013). The diagnostic criteria for CPTSD include the exposure to a traumatic event, three PTSD clusters (re-experiencing, avoidance, persistent perception of heightened current threat) as well as three additional symptom clusters representing pervasive and chronic disturbances in self-organization, namely (a) affect dysregulation, (b) a pervasive negative self-concept, and (c) difficulties in forming and maintaining relationships (World Health Organization, 2023). To meet the diagnostic criteria for CPTSD, these symptom clusters have to cause substantial impairment in the individual’s personal functioning. This relatively new diagnosis aims to capture the specific effect of chronic or repeated trauma on the mechanisms for self-organization and builds on concept of the ICD-10 diagnosis ‘Enduring personality change after catastrophic experiences’ (F62.0) (Maercker et al., 2022). A recent epidemiological study reported a one-month prevalence rate of 0.5% for CPTSD in the German general population (Maercker et al., 2018), while prevalence rates for CPTSD in mental health institutions are substantially higher, with numbers up to 50% (Maercker et al., 2022).
Historically, treatment outcomes for patients who would meet the new diagnostic criteria for CPTSD were consistently associated with poorer treatment outcomes than other forms of traumata (Karatzias, Murphy, et al., 2019). Previous research has suggested that depression and anxiety serve as significant predictors of treatment outcomes (Tunvirachaisakul et al., 2018). Although information regarding predictors for treatment outcomes in patients with CPTSD is still limited, recent studies have highlighted an association between the severity of CPTSD and comorbid affective disorders (Fung et al., 2022; Guzman Torres et al., 2023) as well as somatization (Astill Wright et al., 2021). While current treatment guidelines highlight the possible usefulness of different treatment approaches based on developments of cognitive behavioural therapy (McDonagh et al., 2005), such as Dialectical-Behaviour Therapy (DBT) (Bohus et al., 2013) or skills training in affective and interpersonal regulation (STAIRS) (Cloitre et al., 2002; Cloitre et al., 2010), due to the relatively new character of CPTSD, data on specified treatment approaches is scarce and more outcome-oriented research is warranted. While psychodynamic treatment approaches are frequently employed in mental health care for individuals with trauma-related disorders, their effectiveness remains under-researched. Advocates argue that psychodynamic methods can be especially beneficial in addressing the challenges posed by CPTSD.
Psychodynamic psychotherapy in general comprises a variety of psychotherapeutic approaches that majorly operate on a supportive-interpretive continuum with the use of more supportive or interpretative interventions depending on a patient’s need and mental capacities (Leichsenring et al., 2023). Supportive interventions usually aim to strengthen psychosocial abilities (‘ego-functions’) that are currently not accessible to the person while interpretive interventions aim to enhance patient's insights about repetitive conflicts sustaining their problems. Psychodynamic interventions usually share a common focus on the identification of recurring patterns relating to the self and others (including the therapeutic relationship) as well as the expression and awareness of emotion, the exploration and understanding of defensive patterns, and the discussion of past experiences that have an impact on the person's present experiences (Leichsenring et al., 2023). Empirical and clinical findings suggest that engaging in psychodynamic approaches can lead to enhanced self-esteem, heightened capacity for processing trauma-related reactions through improved reflective functioning, increased reliance on mature defense mechanisms accompanied by a corresponding decrease in reliance on immature defenses, the internalization of more secure relational models, and improved social functioning (Paintain & Cassidy, 2018; Schottenbauer et al., 2008). Furthermore, it is noteworthy that the positive effects of psychodynamic psychotherapy often persist beyond the conclusion of the treatment (Schottenbauer et al., 2008).
From a psychodynamic perspective, especially in cases of early or prolonged abuse, disturbances in self-organization can arise, accompanied by feelings of helplessness, apathy, shame, guilt, and self-reproach. There is often a strong aversion to one's own body, a sense of desecration, and self-hatred. Neglect of self-care is common, with a failure to recognize and address personal needs. Distorted perceptions of the abuser can range from thoughts of revenge to idealization or paradoxical gratitude, believing in a special or supernatural connection (Schäfer et al., 2019). Consequently, the impaired relationship formation, repeated relationship breakdowns, social withdrawal, and persistent distrust of others observed in individuals with CPTSD (Schäfer et al., 2019) suggest a lack of secure attachment, trust in social relationships, and thus, a strongly impaired capacity for social learning in benign social situations, i.e. impaired epistemic trust. Epistemic trust describes the ability to assess the trustworthiness, relevance, and generalizability of information from others (Fonagy & Allison, 2014). Fonagy, Luyten (Fonagy et al., 2015) propose that epistemic trust supports the acquisition of new information, thereby fostering social functioning and resilience when confronting challenging information. However, individuals who have experienced childhood adversity and lack a secure attachment system may exhibit higher levels of epistemic disruption in the form of epistemic mistrust and epistemic credulity. A recent study underlined the specific role of epistemic mistrust and epistemic credulity as indirect moderators for the relationship between childhood abuse and CPTSD symptoms (Kampling et al., 2022). Epistemic mistrust refers to a tendency to view all information sources as unreliable or ill-intended, resulting in a resistance to being influenced by others. Conversely, epistemic credulity involves a lack of vigilance and discrimination between trustworthy and untrustworthy information, making individuals more vulnerable to misinformation and exploitation (Campbell et al., 2021).
It has been suggested that the interpersonal and regulatory problems in patients with CPTSD experience are in part attributable to mentalizing difficulties (Bateman, 2023) which in turn are also assumed to underpin epistemic disruptions and a lack of robust understanding of interpersonal motives. Ineffective mentalizing alongside social trauma and the resulting epistemic isolation might therefore cause a state of epistemic hypervigilance that undermines effective social communication and creates inflexibility in adapting to changed situations. Given that individuals with CPTSD often experience interpersonal disruptions, the concepts of epistemic trust, mistrust, and credulity hold significant relevance in psychotherapeutic treatment (Bateman, 2023). These concepts serve as the foundation for establishing a trusting relationship between the patient and their therapist, fostering an environment of openness for knowledge transfer and the exploration of diverse viewpoints and perspectives. It has been suggested that mentalizing difficulties may underpin the interpersonal and regulatory problems patients with CPTSD experience – subsequently undermining effective social communication and creating inflexibility in adapting to changed situations because of the epistemic hypervigilance which is associated with social trauma and the resulting epistemic isolation. By addressing mentalizing difficulties alongside epistemic disruptions in patients with CPTSD may be key to change and recovery (Bateman, 2023; Bateman et al., 2018).
In German-speaking countries, an integrative concept which combines psychodynamic with trauma-focused treatment approaches within a theoretical framework informed by affective neuroscience, resilience research, and attachment theory has been previously introduced (Wöller et al., 2012; Wöller et al., 2020). The integrative treatment approach is based on four cornerstones: (a) the psychodynamic relationship orientation focuses on the understanding of the patient’s symptoms against the background of current and earlier interpersonal relationships, and thus, focuses not only at the modification of the symptoms, but also the interpersonal relationships that maintain the current symptom pattern; (b) the resource orientation, i.e. activation of internal resources and enhancing the patients’ mastering and coping competencies as well as restoring the ability to activate positive internalized object relationships (e.g. by using imaginative techniques such as the imagination of a ‘safe place’); (c) the neurobiological orientation acknowledges the impaired capacity of emotion regulation and altered information processing, and thus, aims to improve emotion regulation and to process dysfunctional memories using trauma-specific techniques; and (d) the therapists’ well-being and mental health is reflected and emphasized to avoid the risk of vicarious traumatization and professional burnout (Wöller et al., 2012; Wöller et al., 2020).
The aim of this pilot study thus was to (a) investigate change in CPTSD symptoms and associated symptoms during a multimodal psychodynamic inpatient rehabilitation treatment for CPTSD based on the integrative treatment model, and (b) to evaluate the role of changes in epistemic trust, mistrust and credulity during therapy as a potential driver for therapeutic change.
2. Methods
2.1. Patients and procedures
All patients who were referred to the Psychosomatic Rehabilitation Center Montafon (Schruns, Austria) due to trauma-related symptoms were screened for PTSD and CPTSD using the ITQ (described in more detail below) as part of the clinical routine procedures. This included data from a total of n = 125 patients between June 2021 and August 2022. Patients who scored positive in the ITQ based on the defined cut-off (see below) underwent a specialized multimodal psychodynamic inpatient rehabilitation treatment, based on the integrative treatment model described in more detail below. To be included in the study, patients had to (a) be categorized as CPTSD cases based on the ITQ scoring method (see details below), (b) fluently speak German, (c) complete the routine questionnaire batteries in the rehabilitation facility, and (d) had to be willing to participate in the observational study. Treatment costs were being covered by the Austrian social security institution. In accordance with Austrian social security law, patients were required to receive a referral to the treatment centre from a medical doctor, including psychiatrists, general practitioners, and specialists from other fields such as neurology. Admission to the centre was contingent upon a primary ICD-10 diagnosis provided by the referring doctor or institution.
Data were collected in a systematic standardized survey procedure at the beginning (T1; within the first week) and end (T2; within the last week) of the inpatient treatment. At the time of the admission, patients were asked whether they were willing to participate in an observational study. Upon written informed consent, they were included. Data were collected electronically using a multifunctional web-based application called the Life App, which is based on the Computer-Based Health Evaluation Software (CHES) (Holzner et al., 2012). Data were included in the analysis if patients provided complete assessments at both time points. Sample size calculations indicated that a sample of n = 34 patients is sufficiently powered to detect a symptom change of a mean effect size (f = 0.25) in a single group pre–post design with two measurement points (α = 0.05; 1–β = 0.8; r = 0.5). The study has been approved by the Ethics Commission of the University of Innsbruck (no. 108/2022) and was conducted according to the principles of the Declaration of Helsinki.
2.2. Multimodal psychodynamic inpatient rehabilitation treatment
The inpatient treatment was offered by a multiprofessional team (including psychotherapists, psychiatrists, physiotherapists, psychologists, occupational therapists, art therapists and nursing staff) in a multimodal psychosomatic rehabilitation centre with a focus on psychotraumatology. The treatment lasted six weeks with nine hours of therapeutic units per week (i.e. one hour of trauma-specific individual therapy, three hours of trauma-specific group therapy, two hours of relaxation group therapy, one hour of goal-setting and two hours of resource activation). Patients received general multidisciplinary and multimodal therapies together with patients with other mental health issues, which typically included two hours of group sessions for relaxation training, one group session to develop medium-term goals and a therapy focus for the next week, two hourly group sessions for resource activation, as well as additional occupational therapy and physiotherapy. Relaxation training was typically provided by a clinical psychologist or psychotherapist, while group sessions focusing on goals and therapy focus as well as resource activation were led by a psychotherapist. In addition, patients had the possibility for creative therapies including music therapy offered by a music therapist as well as psychopharmacological treatment offered by on call psychiatrists if necessary. All therapists were educated in trauma-informed care. In addition, patients with trauma-related symptoms received trauma-specific treatment, including two 90-minute sessions of symptom-specific trauma-informed group therapy and one hour of individual psychotherapy per week. Trauma-specific individual and group therapy was offered by psychotherapist who were familiar with the psychodynamic treatment concept. Treatment planning was done on the bases of the guidelines of the Austrian social security institutions, which require certain frequencies for the respective therapies.
2.3. Measures
2.3.1. International Trauma Questionnaire (ITQ)
The ITQ is a self-report questionnaire to assess symptoms for post-traumatic stress disorder (PTSD) and CPTSD. The PTSD scale consists of six items to assess the three core elements of PTSD: re-experiencing (two items), avoidance (two items), and persistent perception of heightened current threat (two items) as well as a three item scale to assess the functional impairment by these symptoms. To assess CPTSD, the scale consists of an additional six items which evaluate the three core elements of disturbances in self-organization (DSO), namely affective dysregulation (two items), negative self-concept (two items), and problematic relationships (two items). The combination of PTSD and DSO symptoms allows the classification of CPTSD. Additionally, for both CPTSD and DSO three additional items assess the functional impairment caused by each syndrome.
All items are rated on a five-point Likert scale (from ‘not at all’ to ‘very much’). Since different scoring methods have been used for the ITQ, we separately calculated subscales for PTSD and DSO as recommended (Christen et al., 2021). To allow comparability with previous research, we additionally calculated two overall ITQ symptom scores (i.e. summing all PTSD and CPTSD items), with and without the two functional impairment (FI) scales. Thus, PTSD and DSO symptom scores range from 0 to 24 (i.e. the sum of the six items from each subscale), and the total ITQ scores range from 0 to 48 (i.e. the sum of the 12 ITQ items) and 0 to 72 (i.e. the sum of the 12 ITQ items and the 6 items on functional impairment). In our study, we primarily utilized the ITQ symptom scores excluding FI items for outcome assessment. However, we also presented results for the ITQ total score with FI items in Table 3 to enhance comparability with findings from other studies.
Table 3.
Mean change of CPTSD symptoms during treatment.
| T1 | T2 | |||||
|---|---|---|---|---|---|---|
| M | (SD) | M | (SD) | pa | eta | |
| Total ITQ score (without FI) | 36.1 | (6.6) | 28.9 | (9.2) | <.001 | .38 |
| Total ITQ score (with FI) | 54.1 | (9.1) | 44.2 | (13.6) | <.001 | .36 |
| ITQ: PTSD scale | 17.6 | (3.7) | 15.1 | (4.64) | .007 | .19 |
| Re-experiencing | 6.0 | (1.7) | 5.2 | (1.9) | .044 | .12 |
| Avoidance | 6.0 | (1.6) | 5.0 | (1.9) | .011 | .17 |
| Persistent perception of heightened current threat | 5.5 | (1.8) | 4.9 | (1.8) | .044 | .08 |
| Functional impairment | 8.9 | (2.4) | 7.8 | (2.9) | .044 | .11 |
| ITQ: DSO scale | 18.5 | (4.0) | 13.8 | (5.7) | <.001 | .42 |
| Affective dysregulation | 5.8 | (1.7) | 4.6 | (2.0) | .001 | .25 |
| Negative self-concept | 6.4 | (1.9) | 4.5 | (2.8) | <.001 | .34 |
| Problematic relationships | 6.2 | (1.6) | 4.7 | (1.8) | <.001 | .46 |
| Functional impairment | 9.1 | (2.1) | 7.6 | (2.7) | <.001 | .26 |
Notes: ITQ = International Trauma Questionnaire; DSO = disturbances in self-organization; ETMCQ = Epistemic Trust, Mistrust and Credulity Questionnaire; BSI-18 = Brief Symptom Inventory (18-item version); WHODAS = World Health Organization Disability Assessment Scale. Effect size values η2 ≥ 0.01 were considered small, η2 ≥ 0.06 as medium, and η2 ≥ 0.14 as large. aBonferroni-Holms corrected p-scores.
Symptom were coded as present if a score of 2 or higher was given by the patient. A diagnosis of PTSD was given if at least one of two symptoms of each of the three PTSD clusters were coded as present plus at least one functional impairment cluster associated with PTSD was given. A diagnosis of CPTSD was given if the diagnostic criteria for PTSD were fulfilled and at least one of two symptoms of each of the three DSO clusters were coded as present plus at least one functional impairment cluster associated with CPTSD was given (Cloitre et al., 2018). In line with the ICD-11 diagnostic rules, patients may receive a diagnosis of PTSD or CPTSD, but not both. Thus, when both PTSD and DSO were present, CPTSD was coded as present for this patient. The ITQ has been validated in several different languages and is the most frequently used measure to assess CPTSD (Christen et al., 2021; Karatzias et al., 2017; Maercker et al., 2022; Seiler et al., 2023).
2.3.2. Brief Symptom Inventory (BSI-18)
Psychological distress was assessed with the Brief Symptom Inventory (BSI-18), consisting of 18 items rated on a four-point Likert scale (from ‘not at all’ to ‘very often’). A total score and three subscale scores (depression, anxiety, somatization) can be calculated. Good reliability and validity for the subscales and total score have been reported (Franke, 2017; Franke et al., 2017)
2.3.3. Epistemic Trust, Mistrust and Credulity Questionnaire (ETMCQ)
The Epistemic Trust, Mistrust and Credulity Questionnaire (ETMCQ) is used to assess a person’s capability of epistemic trust. It consists of 15 items rated on a seven-point Likert scale (from ‘strongly disagree’ to ‘strongly agree’). Three subscales (‘epistemic trust’, ‘mistrust’, and ‘credulity) can be calculated. High trust reflects a person’s ability to be open to opportunities for social learning, while high mistrust indicates a tendency to treat information sources as unreliable and to rather avoid being influenced by communication from others. High credulity reflects a persons’ lack of clarity about their own position, which can lead to high vulnerability to misinformation and exploitation by others (Campbell et al., 2021) The German version is in the process of validation in a representative sample (Nolte et al., under review) that confirmed the three-factor structure and found good internal consistencies for Trust and Credulity while the score for Mistrust was acceptable.
2.3.4. World Health Organization Disability Assessment Scale (WHODAS)
The World Health Organization Disability Assessment Scale (WHODAS 2.0) is used to assess activity and participation limitations in conjunction with the International Classification of Functioning, Disability and Health (ICF). It consists of 36 items rated on a five-point Likert scale (from ‘none’ to ‘extreme or cannot do’). A total score and six domains of health-related quality of life (HRQOL) (mobility, cognition, self-care, social functioning, life activities, and participation in the society) can be calculated. The WHODAS 2.0 is scored on a continuum from 0 to 100, where 0 indicates the absence of disability in all domains and 100 indicates maximal disability. The WHODAS 2.0 has been identified as a valid and reliable self-report instrument for the assessment of disability (Federici, Bracalenti, Meloni, & Luciano, 2017).
2.4. Statistical procedures
Presentation of results was in accordance with the STROBE guidelines (Elm et al., 2007). Considering the potential variation in symptom severity across diverse treatment settings, we conducted a comparative analysis of baseline data obtained from the ITQ in relation to findings from other studies. This comparison of baseline symptom severity with samples from different studies allows readers to evaluate and draw comparisons between our study participants and those in other research investigations. This expectation is grounded in the anticipation that patients in our study exhibit baseline data comparable to those in similar research settings. Given the limited availability of data on ITQ baseline scores in psychosomatic inpatient rehabilitation treatments, we compared mean ITQ baseline scores to a sample of Afghan asylum seekers and refugees in Austria who took part in a recent psychotherapy treatment study in Austria (Knefel et al., 2022) and a sample of US veterans treated in a web-based mental health programme (Cloitre et al., 2021) using independent sample t-tests and Hedges’ g effect sizes, to account for difference in group size. Values of g < 0.1 were considered negligible, while values of g = 0.1–0.5 were considered small, g = 0.5–0.8 moderate and g > 0.8 as large effects (Ellis, 2010). Associations of baseline PTSD and CPTSD symptoms with comorbid psychopathological symptoms (depression, anxiety, somatization) and HRQOL were assessed with Pearson correlations. Primary outcome of the study was mean improvement of PTSD and CPTSD symptoms (ITQ subscales) during the inpatient treatment, which were evaluated with repeated measures ANOVAs. Missing data at T2 was imputed using the Expectation-Maximization-Algorithm if data was completely missing at random (MCAR). Secondary outcomes included mean changes of psychological distress (BSI-18), improvements in epistemic trust (ETMCQ) and impairments in activity and participation limitations (WHODAS). To account for inflation of alpha error, the Bonferroni-Holms correction was applied (Hemmerich, 2016; Holm, 1979). Effect size values η2 ≥ 0.01 were considered as small, η2 ≥ 0.06 as medium, and η2 ≥ 0.14 as large (Ellis, 2010).
For the secondary analysis a hierarchical multiple linear regression model was calculated to identify contributing factors associated with mean change in CPTSD and DSO score during treatment. To account for baseline differences, the ‘performance score’ (T2D) of the mean PTSD / DSO change was created as dependent variable. The T2D is based on the formula ‘T2 + (T2 – T1)’, which reflects the individual performance and considers the functional status at beginning of rehabilitation (changes from T1 to T2; Δ) without problems of mathematical coupling or regression effects, as seen in ANCOVA (Wagner et al., 2022; Zdravkovic et al., 2022). Adjusting for baseline differences is crucial for contextualizing study outcomes. Specifically, patients with more unfavourable initial outcome scores (i.e. very high ITQ scores at the commencement of treatment) typically exhibit a larger delta (i.e. the difference between pre- and post-treatment scores) compared to those starting treatment with lower symptom scores. Conversely, for patients with more favourable baseline scores, even minor changes in symptom scores still signify a meaningful improvement. Consequently, incorporating baseline data adjustment may enhance the sensitivity to detect treatment effects and mitigate the impact of regression to the mean, thereby offering a clearer and more accurate depiction of the intervention's effect. Based on previous research, patients baseline depression, anxiety and somatization scores were added as predictors for mean PTSD / DSO symptoms severity change. Additionally, we hypothesized that alterations in the patient's epistemic stance could impact their ability to derive benefits from the treatment, consequently influencing changes in PTSD / DSO symptom severity.
Therefore, we constructed two stepwise regression models co: initially with the ITQ PTSD symptom score and subsequently with the ITQ DSO symptom score as dependent variables (DVs). Both models consisted of three steps. To account for sociodemographic factors (age, sex, relationship status), these variables were added as independent variables (IVs) in the initial step. Subsequently, characteristics of comorbid baseline symptoms (i.e. anxiety, depression, somatization) were introduced as IVs to the model in the second step. In the third step, mean changes in potential critical success factors for therapy outcome (epistemic stance: epistemic trust, mistrust and credulity) were added as IVs to the model. R2 was calculated to evaluate the explained variance of the dependent variable for each step. Furthermore, we explored whether there was a significant increase in explained variance (R2) at each step, thereby shedding light on potential contributing factors to changes in PTSD and DSO symptom severity during the course of treatment. As suggested by Cohen (Cohen, 1988), R2 ≥ .26 was interpreted as substantial, R2 ≥ .13 as moderate and R2 ≥ .02 as weak. Standardized coefficients and p-values are presented for each independent variable. Durbin-Watson statistic was calculated to test for autocorrelation, with values between 1.5 to 2.5 considered acceptable. p < .05 was interpreted as statistically significant. All statistical analyses were conducted with SPSS (v21).
3. Results
Of the initially screened n = 125 patients, a total of n = 50 patients (40.0%) fulfilled the CPTSD criteria based on the ITQ and were therefore included in the study. The majority of patients were female (72.0%), single (42.0%) and between 40 and 60 years old (54.0%). Most frequent diagnoses were depressive disorders (52.0%) and trauma-related disorders (26.0%). No patients dropped out of treatment. For details, see Table 1.
Table 1.
Sociodemographic data (n = 50).
| N | % / (SD) | |
|---|---|---|
| Mean age (SD): 43.0 (13.4) | ||
| <40 | 21 | 42.0% |
| 40–60 | 27 | 54.0% |
| >60 | 2 | 4.0% |
| Missing | – | – |
| Sex | ||
| Male | 14 | 28.0% |
| Female | 36 | 72.0% |
| Missing | – | – |
| Relationship status | ||
| Divorced | 8 | 16.0% |
| Single | 21 | 42.0% |
| Married | 13 | 26.0% |
| Widowed | 2 | 4.0% |
| Missing | 6 | 12.0% |
| ICD-10 diagnosisa | ||
| Depressive disorder (F32-F34) | 26 | 52.0% |
| Anxiety disorder (F41) | 2 | 4.0% |
| PTSD / CPTSD (F43.1 / F62.0) | 13 | 26.0% |
| Adjustment disorder (F43.0, F43.2, F43.9) | 6 | 12.0% |
| Somatization disorder (F44, F45, F54) | 1 | 2.0% |
| Other disorder | 2 | 4.0% |
Notes: SD = standard deviation; PTSD = post-traumatic stress disorder; CPTSD = complex post-traumatic stress disorder.
ICD-10 main diagnosis at referral, given by the referring medical doctor or institution.
A total of n = 8 patients (16%) did not complete the ITQ at the end of treatment. Analysis of missing data for the ITQ (T1: 0%; T2: 12.0% – 18.0% on item level) revealed that data at T2 was missing completely at random (χ2 (55) = 62.6, p = .23), thus data was imputed using the EM algorithm. Additionally, missing data analysis showed no missing data for the ETMCQ, MZQ or BSI-18 at T1 and T2, and few missing items for the WHODAS (on item level: T1 = 2.0%–4.0%; T2 = 2.0%–6.0%). Patients who were included in the study did not differ from excluded patients in terms of age (43.0 vs. 47.3 years; p = .07), sex (42.4% vs. 39.6% m/f; p = .77) or relationship status (p = .39). However, included patients reported significantly higher levels of depression (15.0 vs. 8.4 points; p < .001), anxiety (13.2 vs. 8.2 points; p < .001) and somatization (8.4 vs. 5.9 points; p = .003) than excluded patients, as well as lower epistemic trust (5.0 vs. 4.3 points; p < .001) and higher epistemic mistrust (4.7 vs. 3.9 points; p < .001), epistemic credulity (4.3 vs. 3.3 points; p < .001) and impairment of HRQOL and functioning (37.0 vs. 24.0 points, p < .001).
3.1. Baseline characteristics
The most frequently reported type of trauma was childhood abuse or severe childhood neglect (n = 15, 30.0%), followed by experiences of domestic violence or severe domestic conflicts in adulthood (n = 9, 18.0%), and the death or severe disease of a loved one (n = 7, 14.0%). Another 12.0% (n = 6) reported sexual abuse, severe mobbing (n = 3, 6.0%), or suffering from a severe disease (n = 2, 4.0%). The remaining 16.0% (n = 8) did not specify the type of trauma. While 18.0% indicated that the traumatic experience had occurred within the last year (n = 9), another 20.0% had experienced the trauma 1–5 years ago, 34.0% (n = 17) 5–20 years ago, and 22.0% (n = 11) more than 20 years ago. The remaining three patients (6.0%) did not provide any information regarding the timepoint of the abuse.
Half of the patients (n = 25) reported previous mental health treatment, with 8.0% (n = 2) having their first mental health treatment within the last year, 20.0% (n = 5) 1–5 years ago, 16.0% (n = 4) 10–20 years ago, and the remaining 16.0% (n = 4) more than 20 years ago. A total of n = 28 (56%) reported their motivation for this treatment: almost half of the patients (n = 13, 46.4%) were referred to the centre by mental health experts (psychiatrists, psychotherapists), another 25.0% (n = 7) by general practitioners, 17.9% (n = 5) were self-motivated, and the remaining 10.7% (n = 3) were motivated by family and friends.
Patients in our sample reported a mean ITQ DSO symptom score of 18.1 points (± 4.0), with highest scores for the subscale ‘negative self-concept’ (6.3 ± 1.9 points), followed by ‘problematic relationships’ (6.1 ± 1.7 points) and ‘affective dysregulation’ (5.8 ± 1.7 points). Mean scores for the ITQ PTSD scales were 17.3 (± 3.5), with highest scores for re-experiencing (5.9 ± 1.7) and avoidance (5.9 ± 1.6), followed by persistent perception of heightened current threat (5.4 ± 1.8). Both PTSD (17.3 vs. 13.7 points; p < .001, g = 0.96) and DSO scores were significantly higher (18.1 vs. 12.4; p < .001, g = 1.31) with large effect sizes compared to Afghan asylum seekers and refugees in Austria, which took part in a recent psychotherapy treatment study in Austria (Knefel et al., 2022) and the total ITQ score (without functional impairment) was significantly higher compared to a sample of US veterans with a moderate effect size (35.7 vs. 31.0 points, p = .001, g = 0.50) (Cloitre et al., 2021). When comparing the patient’s epistemic stance with participants from a representative German sample, clear signs of epistemic disruption can be described: patients in our sample showed significantly lower levels of trust (21.5 vs. 24.8 points; p < .001) as well as higher levels of mistrust (18.6 vs. 14.1 points; p < .001) and credulity (16.6 vs. 12.0 points; p < .001).
All patients reported values above the clinical cut-off for depression (n = 50, 100%) as assessed by the BSI-18 subscales, 96.0% (n = 48) reported values above the cut-off for anxiety and 82.0% (n = 41) for somatization. A higher PTSD symptom score was associated with higher somatization and anxiety scores. Higher somatization scores showed highest correlations with trauma re-experiencing, while persistent perception of heightened current threat was associated with higher anxiety score. Additionally, higher PTSD scores were also associated with more functional impairment and reduced HRQOL.
As for the DSO symptoms, as significant association was found with higher depression scores. This correlation was mainly driven by the patients’ negative self-concept. The negative self-concept was also associated with higher anxiety scores, while no significant associations were found with somatization scores. Additionally, higher DSO scores correlated with more functional impairment and worse HRQOL. For details, see Table 2.
Table 2.
Pre-treatment associations of ITQ total scores and subscales with BSI-18 depression, anxiety and somatization scales and WHODAS HRQOL total score.
| Somatization | Anxiety | Depression | HRQOL impairment | |
|---|---|---|---|---|
| PTSD total score | .32 * | .44** | .16 | .60*** |
| Re-experiencing | .44 ** | .35* | –.02 | .50** |
| Avoidance | –.04 | .15 | .14 | .30 |
| Persistent perception of heightened current threat | .27 | .43** | .22 | .46** |
| Functional impairment | .31* | .32* | .18 | .34* |
| DSO total score | .03 | .24 | .41** | .42** |
| Affective dysregulation | .13 | .16 | .17 | .35* |
| Negative self-concept | .03 | .32* | .51*** | .42** |
| Problematic relationship | –.11 | .05 | .26 | .24 |
| Functional impairment | .28* | .23 | .42** | .42** |
Note: PTSD = post-traumatic stress disorder; DSO = disturbances in self-organization; HRQOL = health-related quality of life.
*p < 0.05, **p < 0.01, ***p < 0.001.
3.2. Symptom improvement during therapy
Patients in our sample reported a statistically significant reduction of the total ITQ score during the inpatient treatment with a large effect size (p < .001; η2 = .34). Regarding PTSD core symptoms, a significant improvement with large effect size was observed (p = .010; η2 = .15). However, this was mainly caused by a reduction of avoidance (p = .014; η2 = .13), while changes in re-experiencing (p = .06) and persistent perception of heightened current threat (p = .11) were not statistically significant. In terms of improvements in DSO, a significant reduction in symptom severity with large effect sizes was observable (p < .001; η2 = .36), with the largest effect found for the subscale ‘problematic relationships’ (p < .001; η2 = .43). For details, see Table 3.
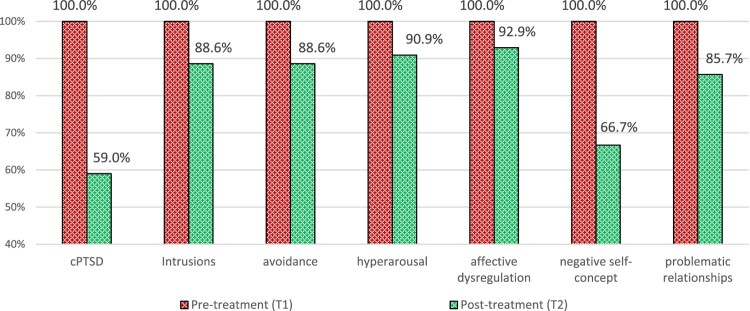
While before treatment all patients fulfilled criteria for CPTSD, the number was reduced to 59.0% at the end of treatment. The biggest reduction of symptoms above the cut-off was observed for the DSO scale ‘negative self-concept’ (66.7%), while highest clinically relevant scores were found for the DSO scale ‘affective dysregulation’. For details see Figure 1.
Figure 1.
Proportion of patients above the clinical cut-off for PTSD and DSO and the three respective ITQ subscales before and after treatment.
In addition, the sample reported significantly improved depression (p < .001; η2 = .59), anxiety (p < .001; η2 = .44) and somatization scores (p = .008; η2 = .19) as well as improved HRQOL (p < .001; η2 = .59), all with large effect sizes. As for changes in their epistemic stance, patients reported a significantly improved epistemic trust (p = .026; η2 = .14) with a large effect size, while overall the level of epistemic mistrust (p = .47) and epistemic credulity (p = .90) did not significantly change. For details, see Table 4.
Table 4.
Mean change of epistemic trust, mistrust and credulity, psychological distress and quality of life during treatment.
| T1 | T2 | |||||
|---|---|---|---|---|---|---|
| M | (SD) | M | (SD) | pa | eta | |
| ETMCQ: epistemic trust | 21.5 | (5.5) | 23.6 | (4.9) | .026 | .14 |
| ETMCQ: Epistemic mistrust | 18.6 | (3.9) | 18.2 | (3.9) | .47 | .01 |
| ETMCQ: Epistemic credulity | 16.6 | (5.1) | 16.9 | (4.4) | .90 | <.01 |
| BSI-18 total score | 36.6 | (10.9) | 23.3 | (13.2) | <.001 | .55 |
| BSI-18: depression | 15.0 | (4.3) | 8.5 | (5.7) | <.001 | .59 |
| BSI-18: anxiety | 13.2 | (5.3) | 8.5 | (5.1) | <.001 | .44 |
| BSI-18: Somatization | 8.4 | (4.6) | 6.3 | (4.4) | .008 | .19 |
| WHODAS: total score | 54.3 | (13.0) | 38.9 | (20.0) | <.001 | .59 |
| WHODAS: cognition | 53.4 | (16.3) | 38.3 | (21.8) | <.001 | .27 |
| WHODAS: mobility | 39.1 | (24.9) | 24.8 | (25.5) | <.001 | .30 |
| WHODAS: self-care | 29.7 | (24.1) | 18.1 | (17.8) | .003 | .23 |
| WHODAS: getting along | 56.5 | (19.1) | 42.8 | (23.2) | <.001 | .28 |
| WHODAS: household activities | 53.0 | (26.8) | 32.7 | (34.1) | <.001 | .34 |
| WHODAS: work activities | 66.9 | (31.1) | 48.3 | (31.2) | .026 | .17 |
| WHODAS: social participation | 64.2 | (14.9) | 49.9 | (22.5) | <.001 | .30 |
Notes: ETMCQ = Epistemic Trust, Mistrust and Credulity Questionnaire; BSI-18 = Brief Symptom Inventory (18-item version); WHODAS = World Health Organization Disability Assessment Scale. Effect size values η2 ≥ 0.01 were considered small, η2 ≥ 0.06 as medium, and η2 ≥ 0.14 as large. aBonferroni-Holms corrected p-scores.
3.3. Epistemic trust, mistrust and credulity as mediators of improvement in PTSD and DSO symptoms during therapy
To identify factors that were associated with baseline-adjusted mean changes in overall PTSD symptoms during the therapy, a hierarchical multiple linear regression analysis was performed. The Durbin-Watson values were 2.23 and thus indicated there was no autocorrelation detected in the sample.
Neither the sociodemographic factors added in step 1, nor the baseline psychopathology factors added in step 2 were significantly associated with baseline-adjusted changes in the PTSD symptom score (p = .13–90) and neither of the models were statistically significant (p = .43 – .46). However, when changes in baseline adjusted ETMCQ subscales were added to the model, improvements in epistemic trust (β = –.30, p = .047) and epistemic credulity (β = .39, p = .013) were associated with improvements in the PTSD symptoms during therapy. The final model explained 40% of its variance and was statistically significant (p = .014). For details, see Table 5.
Table 5.
Hierarchical multiple linear regression model for the influence of sociodemographic factors, baseline psychopathology and changes in epistemic trust, mistrust and credulity on the mean change of PTSD symptoms (T2D).
| Step 1: Sociodemographic factors |
Step 2: Baseline psychopathology factors |
Step 3: Improved epistemic trust |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | ||||
| LL | UL | LL | UL | |||||||||
| Age | –.20 | –.52 | .111 | −20 | –.16 | –.52 | .21 | .39 | –.08 | –.41 | .23 | .59 |
| Gender (male = 0) | .02 | –.286 | .326 | .90 | .02 | –.29 | .33 | .90 | .02 | –.25 | .29 | .89 |
| Depression (T1) | – | – | – | – | .28 | –.08 | .62 | .13 | .23 | –.11 | .56 | .19 |
| Anxiety (T1) | – | – | – | – | –.21 | –.61 | .20 | .32 | –.15 | –.50 | .21 | .41 |
| Somatization (T1) | – | – | – | – | .15 | –.24 | .52 | .45 | .10 | –.24 | .43 | .56 |
| Epistemic trust (T2D)a | – | – | – | – | – | – | – | – | –.30 | –.62 | .00 | .047 |
| Epistemic mistrust (T2D)b | – | – | – | – | – | – | – | – | .21 | –.10 | .50 | .19 |
| Epistemic credulity (T2D)b | – | – | – | – | – | – | – | – | .39 | .09 | .68 | .013 |
| R2 (Sig. model) | .04 | (.43) | .11 | (.46) | .40 | (.014) | ||||||
| Δ R2 (Sig. of Δ R2) | – | – | .07 | (.39) | .29 | (.003) | ||||||
Notes: Lower values of dependent variable (T2D PTSD mean change) indicate symptom improvement; β: standardized coefficient; CI = confidence interval; LL = lower limit; UL = upper limit; ahigher values indicate improvement; b lower values indicate improvement; significant factors displayed in bold.
To identify factors that are associated with baseline-adjusted mean changes in overall DSO symptoms during the therapy, a hierarchical multiple linear regression analysis was performed. The Durbin-Watson values were 2.16 and thus indicated there was no autocorrelation detected in the sample.
In Step 1 sociodemographic factors were included in the model. Neither of the included factors significantly predicted mean change of DSO symptoms and the overall model was not statistically significant (p = .67). The variables included in Step 1 explained 2% of variance mean change in DSO symptoms and the model was statistically significant (p = .031).
While the baseline psychopathology factors added in step 2 increased the overall explained variance to 13%, none of the variables were significantly associated with the mean change in DSO symptoms and neither the model (p = .44) nor the change in explained variance (p = .27) was statistically significant.
In the third step, baseline adjusted mean changes of epistemic trust, mistrust and credulity were added as independent variables. The overall explained variance significantly increased to 48% (p = .001) and the overall model was statistically significant (p = .005). Improved epistemic trust (β = –.34, p = .026) and decreased epistemic credulity (β = .37, p = .017) were identified as significant predictors for the mean change of DSO symptoms during therapy. Additionally, after adding the ETMCQ subscales to the mode, lower age (β = .43, p = .012) was also a statistically significant predictor and lower depression levels at baseline were borderline significant (β = .35, p = .054). For details, see Table 6.
Table 6.
Hierarchical multiple linear regression model for the influence of sociodemographic factors, baseline psychopathology and changes in epistemic trust, mistrust, and credulity on the mean change of DSO symptoms (T2D).
| Step 1: Sociodemographic factors |
Step 2: Baseline psychopathology factors |
Step 3: Improved epistemic trust |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | ||||
| LL | UL | LL | UL | |||||||||
| Age | –.15 | –.18 | .48 | .38 | –.32 | –.07 | .72 | .11 | –.43 | .10 | .77 | .012 |
| Gender (male = 0) | .01 | –.33 | .32 | .97 | .003 | –.32 | .32 | .98 | –.09 | –.23 | .31 | .78 |
| Depression (T1) | – | – | –.40 | –.01 | .78 | .06 | –.35 | –.01 | .68 | .054 | ||
| Anxiety (T1) | – | – | .07 | –.52 | .37 | .74 | –.08 | –.29 | .45 | .66 | ||
| Somatization (T1) | – | – | .02 | –.40 | .37 | .92 | .09 | –.41 | .24 | .59 | ||
| Epistemic trust (T2D)a | – | – | – | – | –.34 | –.70 | –.05 | .026 | ||||
| Epistemic mistrust (T2D)b | – | – | – | – | .26 | –.04 | .62 | .08 | ||||
| Epistemic credulity (T2D)b | – | – | – | – | .37 | .07 | .65 | .017 | ||||
| R2 (Sig. model) | .02 | (.67) | .13 | (.44) | .48 | (.005) | ||||||
| Δ R2 (Sig. of Δ R2) | – | – | .11 | (.27) | .35 | (.001) | ||||||
Notes: Lower values of dependent variable (T2D DSO mean change) indicate symptom improvement; β: standardized coefficient; CI = confidence interval; LL = lower limit; UL = upper limit; ahigher values indicate improvement; blower values indicate improvement; significant factors displayed in bold.
4. Discussion
The aim of this study was to evaluate mean change in CPTSD symptom severity during a 6-week multimodal psychodynamic inpatient rehabilitation treatment and to identify potential mechanisms of change underpinning therapy outcome. A total of n = 50 patients who fulfilled CPTSD diagnostic criteria were included in the study. Baseline PTSD and DSO scores were associated with higher rates of depression, anxiety and somatization as well as impaired functioning. The results of our study indicated a significant reduction of trauma-related symptoms. However, patients reported more improvement of DSO than of PTSD symptoms. Improvement of epistemic trust and reduction of epistemic mistrust during therapy were associated with improved trauma-related symptoms, especially DSO ones.
CPTSD is a newly introduced diagnostic category and both epidemiological and clinical data remain limited. While the prevalence of CPTSD in the general population is relatively low, previous studies have shown elevated levels of patients with CPTSD in mental health settings (Maercker et al., 2022). In our study, almost half of all initially screened 125 inpatients fulfilled the criteria for CPTSD. This is a higher rate than in comparable studies and might be explained by the trauma-specialized treatment approach of the rehabilitation clinic. Still, a study in an unselected sample of n = 662 patients from a German rehabilitation centre reported that 13.3% of patients screened positive for CPTSD and 9.5% for PTSD (Brenner et al., 2019), which was comparable to prevalence rates in trauma-exposed community samples (Cloitre et al., 2018). This indicates that trauma-related disorders including PTSD and CPTSD are prevalent conditions among psychosomatic patients. Nevertheless, only approximately 26% of patients meeting the criteria for CPTSD diagnosis had been officially diagnosed with PTSD (i.e. F43.1) or CPTSD (i.e. F62.0) according to ICD-10 by the referring medical doctor or institution. This suggests that trauma-related symptoms are likely to be underreported within the health-care system. In our sample, very high levels of comorbidities were found: all patients reported clinically relevant levels of depression, more than 95% for anxiety and more than 80% for symptoms associated with somatization disorders. In line with previous literature, PTSD symptoms were associated with anxiety, while DSO symptoms correlated with heightened levels of depression (Hyland et al., 2017). It has been reported that patients with CPTSD often also show elevated levels of dissociation and borderline personality disorder, as well as depression, anxiety, somatization, suicidal ideation and self-harm (Astill Wright et al., 2021; Fung et al., 2022; Guzman Torres et al., 2023; Hyland et al., 2018). Given the potentially high prevalence amongst psychosomatic patients and the substantial rate of comorbid disorders – including personality disorders and suicidality – reported for patients with CPTSD (Brenner et al., 2019; Karatzias, Hyland et al., 2019), evidence on specifically tailored interventions and potential mechanisms for change are much needed for psychosomatic treatment facilities, to ensure that patients with CPTSD receive the best possible care and treatment available.
In our study, patients reported a substantial reduction of trauma-related symptoms as well as substantially reduced depression, anxiety and somatization scores, each with large effect sizes. The effect sizes for DSO symptoms correspond to a Cohen’s d of over 1.0 and a Cohens’ d of 0.8–0.9 for PTSD symptoms (Lenhard & Lenhard, 2016). Patients reported a reduction of 43.3% in their depressive symptoms, of 35.6% in their anxiety and 25.0% of their somatization symptoms. In the psychodynamic treatment manual, it is advised to prioritize addressing depressive comorbidity through the implementation of guilt-relieving, and encouraging interventions, particularly when patients are grappling with elevated superego pressure or feelings of failure.
However, when mean changes of the DSO and PTSD subscale are analysed separately, it was evident that patients showed larger improvements for their DSO symptoms (reduction of 22.7%) than the core PTSD symptoms (reduction of 12.7%). These results are in line with previously reported effects of treatments for CPTSD (Schäfer et al., 2019). Largest improvements were observed for patients’ disturbances in relationships and negative self-concept, while lowest improvements were observed for intrusive symptoms and persistent perception of heightened current threat symptoms. We additionally observed that level of affective dysregulation remains relatively high at the end of treatment. In the psychodynamic treatment concept of the clinic a strong focus is put on building up a stable therapeutic alliance, improving emotion regulation, and strengthening coping capacities (Wöller et al., 2012; Wöller et al., 2020). Given the relatively short treatment duration of six weeks, severely traumatized patients had not proceeded if trust in the therapeutic relation has not been sufficiently given and emotion regulation (phobia of trauma) have not sufficiently been improved. Thus, the treatment strongly focused on the patients’ interpersonal relationships but did not regularly include elements of trauma confrontation or exposure which are typically employed in trauma-focused cognitive–behavioural treatment approaches (Paintain & Cassidy, 2018). Moreover, the initial focus on addressing perpetrator introjects was frequently crucial for patient stabilization. Perpetrator introjects involve the unconscious internalization of identification with the aggressor, often manifesting in negative perceptions of the perpetrator directed towards the individual (e.g. ‘you are to blame’, ‘you are worthless’, ‘you don't deserve any better’, ‘you are nothing’, ‘you wanted it this way’, or ‘you enjoyed it’). These internalized views typically operate covertly and secretly from the background, leading to seemingly inevitable patterns of behaviours that harm both oneself and others. As a result, traumatized individuals harbour both perpetrator and victim components within themselves, making it challenging to learn to differentiate and identify the dominant aspect in any given moment (Wöller et al., 2012; Wöller et al., 2020).
Due to the design of the study, it is not possible to evaluate how these changes in trauma-symptoms affect the patients’ mental health and social functioning at follow up. However, we currently collect data for a follow-up study of patients with CPTSD treated at the facility to evaluate the long-term development of symptoms after treatment. Since in Austria psychosomatic in-patient rehabilitation treatments are only covered for about six weeks by the insurance system, elements of trauma confrontation or exposure may not be suitable for most of the severely traumatized patients. It may be beneficial to offer outpatient trauma exposure treatments as a follow-up treatment for the inpatient rehabilitation if patients have been sufficiently stabilized.
A further aim of this study was to investigate the role of epistemic trust, mistrust and credulity as potential mediators for treatment outcomes. In our sample, improvements in epistemic trust and reduction of epistemic credulity were significantly associated with a reduction in both DSO and PTSD symptoms, whereas contrary to previous research (Tunvirachaisakul et al., 2018) neither depression nor anxiety or somatization levels at baseline were identified as predictors of treatment outcomes in our sample. The linear regression models explained 40% of the variance for improvement in PTSD symptoms and 48% in DSO symptoms, respectively. This is in line with results from the general German population, which identified epistemic mistrust and credulity as significant predictors for personality functioning (Kampling et al., 2022). Bateman (Bateman, 2023) has argued that the epistemic isolation which is associated with ineffective mentalizing alongside social trauma may cause a state of epistemic hypervigilance that undermines effective social communication and learning and which creates inflexibility in adapting to changed situations. Our results indicate that improvements in epistemic trust – which is defined as the ability to evaluate whether information from other persons or sources is trustworthy, relevant to the self, and generalizable to other contexts and is associated with secure attachment (Fonagy & Allison, 2014) – and epistemic credulity – i.e. a pronounced lack of vigilance and appropriate discrimination between trustworthy and untrustworthy information, which results in an increased vulnerability to be misinformed and exploited – may be understood as key mechanisms of change in psychotherapeutic approaches for individuals with CPTSD. This is in line with previous literature which highlighted that individuals with higher levels of epistemic trust are selectively and appropriately open to social learning in benign social circumstances (Campbell et al., 2021) and thus may be better prepared to build a trustful relationship with their therapist. This may result in more openness towards transfer of knowledge in the broader sense including the learning differing perspectives and, thus, to improve the ability for mentalizing (Fonagy et al., 2015). Contrarily, individuals who are exposed to adversities in childhood and have not developed a secure attachment system may display higher levels of epistemic mistrust or epistemic credulity (Campbell et al., 2021). Given that individuals with CPTSD often experience interpersonal disruptions and the concepts of epistemic trust, mistrust, and credulity hold significant relevance in psychotherapeutic treatment and may be a key element for positive change and recovery (Bateman, 2023; Bateman et al., 2018). In addition, it is noteworthy that individuals with CPTSD often seek assistance in psychiatric treatment facilities, yet a majority do not experience symptom relief, as indicated by unpublished data from the authors. Our findings lend support to the notion that a psychodynamic, relationship-oriented approach may serve as a robust foundation for subsequent psychotherapeutic interventions, marking the initiation of a healing process.
This study has several strengths and limitations: firstly, to our knowledge this is the first study to present outcome data for an integrative psychodynamic rehabilitation inpatient treatment programme for patients with CPTSD. The data in this study stem from an unselected sample of rehabilitation inpatients and thus can be considered to be relatively representative for psychosomatic inpatient samples in Austria. However, since no control group was available in this setting and patients were not randomized across different treatment modalities, the causal interpretation of our results remains limited. Since the data was collected in a single centre in Austria, generalizability of the results may be limited. Due to the pilot character of the study, the sample size was relatively small and did not allow for more detailed subgroup analyses. Based on the promising results of this study, we currently are preparing a controlled multi-centre study to test and compare the treatment approach in a larger sample of patients with CPTSD.
5. Conclusion
The diagnosis of CPTSD is relatively new and there is a need for outcome data for different therapeutic programmes to identify best practice approaches and key mechanisms of change. Previous studies indicated that CPTSD might be a relatively prevalent disorder amongst patients in psychosomatic rehabilitation and that specific treatment approaches are warranted. Our results indicate that the applied multimodal psychodynamic inpatient rehabilitation programme is an effective treatment approach for patients with CPTSD: patients reported substantial changes for trauma-related symptoms as well as comorbid symptoms such as depression, anxiety and somatization improvement in HRQOL and functioning levels. Improvements in epistemic trust were identified as a potential mechanism of change and may be understood as a common and transdiagnostic factor in psychosomatic and psychotherapeutic treatments.
Supplementary Material
Disclosure statement
No potential conflict of interest was reported by the author(s).
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University of Innsbruck (AN2015-0175 351/4.18).
Data availability statement
The data sets analysed in this manuscript are not publicly available due to ethical and legal restrictions (data contain potentially identifying and sensitive patient information). If not already reported within this work, the authors may provide descriptive data on individual medical indicators for admission and discharge or the expected change due to in-patient health care for various groups and diagnoses. Requests for access to anonymized data sets should be directed to the corresponding author.
References
- Astill Wright, L., Roberts, N. P., Lewis, C., Simon, N., Hyland, P., Ho, G. W. K., McElroy, E., & Bisson, J. I. (2021). High prevalence of somatisation in ICD-11 complex PTSD: A cross sectional cohort study. Journal of Psychosomatic Research, 148, Article 110574. 10.1016/j.jpsychores.2021.110574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman, A., Campbell, C., Luyten, P., & Fonagy, P. (2018). A mentalization-based approach to common factors in the treatment of borderline personality disorder. Current Opinion in Psychology, 21, 44–49. 10.1016/j.copsyc.2017.09.005 [DOI] [PubMed] [Google Scholar]
- Bateman, A. (2023). Mentalization based treatment – trauma focused (MBT-TF): Rationale of a mentalizing model for treatment of people who have experienced developmental trauma.
- Bohus, M., Dyer, A. S., Priebe, K., Krüger, A., Kleindienst, N., Schmahl, C., Niedtfeld, I., & Steil, R. (2013). Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: A randomised controlled trial. Psychotherapy and Psychosomatics, 82(4), 221–233. 10.1159/000348451 [DOI] [PubMed] [Google Scholar]
- Brenner, L., Köllner, V., & Bachem, R. (2019). Symptom burden and work-related impairment among patients with PTSD and complex PTSD. European Journal of Psychotraumatology, 10(1), Article 1694766. 10.1080/20008198.2019.1694766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, C., Tanzer, M., Saunders, R., Booker, T., Allison, E., Li, E., O’Dowda, C., Luyten, P., & Fonagy, P. (2021). Development and validation of a self-report measure of epistemic trust. PLoS One, 16(4), e0250264. 10.1371/journal.pone.0250264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christen, D., Killikelly, C., Maercker, A., & Augsburger, M. (2021). Item response model validation of the German ICD-11 international trauma questionnaire for PTSD and CPTSD. Clinical Psychology in Europe, 3(4), e5501. 10.32872/cpe.5501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., Koenen, K. C., Cohen, L. R., & Han, H. (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. 10.1037/0022-006X.70.5.1067 [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L., Gan, W., & Petkova, E. (2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry, 167(8), 915–924. 10.1176/appi.ajp.2010.09081247 [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., Karatzias, T., & Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. 10.1111/acps.12956 [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Hyland, P., Prins, A., & Shevlin, M. (2021). The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. European Journal of Psychotraumatology, 12(1), Article 1930961. 10.1080/20008198.2021.1930961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum. [Google Scholar]
- Ellis, P. D. (2010). The essential guide to effect sizes: Statistical power, meta-analysis, and the interpretation of research results. Cambridge University Press. [Google Scholar]
- Elm, E. V., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., & Vandenbroucke, J. P. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ, 335(7624), 806–808. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federici, S., Bracalenti, M., Meloni, F., & Luciano, J. V. (2017). World Health Organization disability assessment schedule 2.0: An international systematic review. Disabil Rehabil, 39(23), 2347–2380. 10.1080/09638288.2016.1223177 [DOI] [PubMed] [Google Scholar]
- Fonagy, P., & Allison, E. (2014). The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy, 51(3), 372–380. 10.1037/a0036505 [DOI] [PubMed] [Google Scholar]
- Fonagy, P., Luyten, P., & Allison, E. (2015). Epistemic petrification and the restoration of epistemic trust: A new conceptualization of borderline personality disorder and its psychosocial treatment. Journal of Personality Disorders, 29(5), 575–609. 10.1521/pedi.2015.29.5.575 [DOI] [PubMed] [Google Scholar]
- Franke, G. H. (2017). Mini-Symptom-Checklist (BSI-18). Manual. Hogrefe. [Google Scholar]
- Franke, G. H., Jaeger, S., Glaesmer, H., Barkmann, C., Petrowski, K., & Braehler, E. (2017). Psychometric analysis of the Brief Symptom Inventory 18 (BSI-18) in a representative German sample. BMC Medical Research Methodology, 17(1), 14. 10.1186/s12874-016-0283-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung, H. W., Chien, W. T., Lam, S. K. K., & Ross, C. A. (2022). Investigating post-traumatic stress disorder (PTSD) and complex PTSD among people with self-reported depressive symptoms. Frontiers in Psychiatry, 13, Article 953001. 10.3389/fpsyt.2022.953001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzman Torres, E., Krause-Utz, A., & Sack, M. (2023). Predictors of complex PTSD: The role of trauma characteristics, dissociation, and comorbid psychopathology. Borderline Personality Disorder and Emotion Dysregulation, 10(1), 1. 10.1186/s40479-022-00208-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmerich, W. (2016). StatistikGuru: Calculator to adjust the α-levels. https://statistikguru.de/rechner/adjustierung-des-alphaniveaus.html.
- Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391. 10.1002/jts.2490050305 [DOI] [Google Scholar]
- Holm, S. (1979). A simple sequential rejective method procedure. Scandinavian Journal of Statistics, 6, 65–70. [Google Scholar]
- Holzner, B., Giesinger, J. M., Pinggera, J., Zugal, S., Schöpf, F., Oberguggenberger, A. S., Gamper, E. M., Zabernigg, A., Weber, B., & Rumpold, G. (2012). The Computer-Based Health Evaluation Software (CHES): A software for electronic patient-reported outcome monitoring. BMC Medical Informatics and Decision Making, 12(1), 126. 10.1186/1472-6947-12-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland, P., Shevlin, M., Brewin, C. R., Cloitre, M., Downes, A. J., Jumbe, S., Karatzias, T., Bisson, J. I., & Roberts, N. P. (2017). Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International Trauma Questionnaire. Acta Psychiatrica Scandinavica, 136(3), 313–322. 10.1111/acps.12771 [DOI] [PubMed] [Google Scholar]
- Hyland, P., Shevlin, M., Fyvie, C., & Karatzias, T. (2018). Posttraumatic stress disorder and complex posttraumatic stress disorder in DSM-5 and ICD-11: Clinical and behavioral correlates. Journal of Traumatic Stress, 31(2), 174–180. 10.1002/jts.22272 [DOI] [PubMed] [Google Scholar]
- Kampling, H., Kruse, J., Lampe, A., Nolte, T., Hettich, N., Brähler, E., Sachser, C., Fegert, J. M., Gingelmaier, S., Fonagy, P., Krakau, L., Zara, S., & Riedl, D. (2022). Epistemic trust and personality functioning mediate the association between adverse childhood experiences and posttraumatic stress disorder and complex posttraumatic stress disorder in adulthood. Frontiers in Psychiatry, 13, Article 919191. 10.3389/fpsyt.2022.919191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., Bisson, J. I., Roberts, N. P., & Brewin, C. R. (2017). PTSD and complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(sup7), 1418103. 10.1080/20008198.2017.1418103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T., Hyland, P., Bradley, A., Cloitre, M., Roberts, N. P., Bisson, J. I., & Shevlin, M. (2019). Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: Findings from a trauma-exposed population based sample of adults in the United Kingdom. Depression and Anxiety, 36(9), 887–894. 10.1002/da.22934 [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., Hyland, P., Maercker, A., Ben-Ezra, M., Coventry, P., Mason-Roberts, S., Bradley, A., & Hutton, P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. 10.1017/S0033291719000436 [DOI] [PubMed] [Google Scholar]
- Knefel, M., Kantor, V., Weindl, D., Schiess-Jokanovic, J., Nicholson, A. A., Verginer, L., Schäfer, I., & Lueger-Schuster, B. (2022). A brief transdiagnostic psychological intervention for Afghan asylum seekers and refugees in Austria: A randomized controlled trial. European Journal of Psychotraumatology, 13(1), Article 2068911. 10.1080/20008198.2022.2068911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leichsenring, F., Abbass, A., Heim, N., Keefe, J. R., Kisely, S., Luyten, P., Rabung, S., & Steinert, C. (2023). The status of psychodynamic psychotherapy as an empirically supported treatment for common mental disorders – an umbrella review based on updated criteria. World Psychiatry, 22(2), 286–304. 10.1002/wps.21104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhard, W., & Lenhard, A. (2016). Computation of effect sizes. https://www.psychometrica.de/effect_size.html.
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., van Ommeren, M., Jones, L. M., Humayan, A., Kagee, A., Llosa, A. E., Rousseau, C., Somasundaram, D. J., Souza, R., Suzuki, Y., Weissbecker, I., Wessely, S. C., First, M. B., & Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry, 12(3), 198–206. 10.1002/wps.20057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker, A., Hecker, T., Augsburger, M., & Kliem, S. (2018). ICD-11 prevalence rates of posttraumatic stress disorder and complex posttraumatic stress disorder in a German nationwide sample. Journal of Nervous & Mental Disease, 206(4), 270–276. 10.1097/NMD.0000000000000790 [DOI] [PubMed] [Google Scholar]
- Maercker, A., Cloitre, M., Bachem, R., Schlumpf, Y. R., Khoury, B., Hitchcock, C., & Bohus, M. (2022). Complex post-traumatic stress disorder. The Lancet, 400(10345), 60–72. 10.1016/S0140-6736(22)00821-2 [DOI] [PubMed] [Google Scholar]
- McDonagh, A., Friedman, M., McHugo, G., Ford, J., Sengupta, A., Mueser, K., Demment, C. C., Fournier, D., Schnurr, P. P., & Descamps, M. (2005). Randomized trial of cognitive-behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology, 73(3), 515–524. 10.1037/0022-006X.73.3.515 [DOI] [PubMed] [Google Scholar]
- Paintain, E., & Cassidy, S. (2018). First-line therapy for post-traumatic stress disorder: A systematic review of cognitive behavioural therapy and psychodynamic approaches. Counselling and Psychotherapy Research, 18(3), 237–250. 10.1002/capr.12174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer, I., Gast, U., Hofmann, A., Knaevelsrud, C., Lampe, A., Liebermann, P., Lotzin, A., Maercker, A., Rosner, R., & Wöller, W. (2019). S3-Leitlinie Posttraumatische Belastungsstörung. Springer Verlag. [Google Scholar]
- Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., & Gray, S. H. (2008). Contributions of psychodynamic approaches to treatment of PTSD and trauma: A review of the empirical treatment and psychopathology literature. Psychiatry: Interpersonal and Biological Processes, 71(1), 13–34. 10.1521/psyc.2008.71.1.13 [DOI] [PubMed] [Google Scholar]
- Seiler, N., Davoodi, K., Keem, M., & Das, S. (2023). Assessment tools for complex post traumatic stress disorder: A systematic review. International Journal of Psychiatry in Clinical Practice, 27(3), 292–300. 10.1080/13651501.2023.2197965 [DOI] [PubMed] [Google Scholar]
- Tunvirachaisakul, C., Gould, R. L., Coulson, M. C., Ward, E. V., Reynolds, G., Gathercole, R. L., Grocott, H., Supasitthumrong, T., Tunvirachaisakul, A., Kimona, K., & Howard, R. J. (2018). Predictors of treatment outcome in depression in later life: A systematic review and meta-analysis. Journal of Affective Disorders, 227, 164–182. 10.1016/j.jad.2017.10.008 [DOI] [PubMed] [Google Scholar]
- Wagner, B., Zdravkovic, A., Pirchl, M., Puhan, M. A., Zwick, R. H., Grote, V., Crevenna, R., & Fischer, M. J. (2022). Performance score (T2D) – a new perspective in the assessment of six-minute walking tests in pulmonary rehabilitation. Diagnostics, 12(10), 2402. 10.3390/diagnostics12102402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2023). 6B41 complex post traumatic stress disorder. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/585833559
- Wöller, W., Leichsenring, F., Leweke, F., & Kruse, J. (2012). Psychodynamic psychotherapy for posttraumatic stress disorder related to childhood abuse–principles for a treatment manual. Bulletin of the Menninger Clinic, 76(1), 69–93. 10.1521/bumc.2012.76.1.69 [DOI] [PubMed] [Google Scholar]
- Wöller, W., Lampe, A., Schellong, J., Leichsenring, F., Kruse, J., & Mattheß, H. (2020). [Psychodynamic Treatment for Complex Posttraumatic Stress Disorder]. Stuttgart: Klett-Cotta.
- Zdravkovic, A., Grote, V., Pirchl, M., Stockinger, M., Crevenna, R., & Fischer, M. J. (2022). Comparison of patient- and clinician-reported outcome measures in lower back rehabilitation: Introducing a new integrated performance measure (t2D). Quality of Life Research, 31(1), 303–315. 10.1007/s11136-021-02905-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets analysed in this manuscript are not publicly available due to ethical and legal restrictions (data contain potentially identifying and sensitive patient information). If not already reported within this work, the authors may provide descriptive data on individual medical indicators for admission and discharge or the expected change due to in-patient health care for various groups and diagnoses. Requests for access to anonymized data sets should be directed to the corresponding author.