Summary:
There are various types of chin deformities, and the least established surgical method for deformity correction may be reduction for anteroposterior macrogenia. Anteroposterior macrogenia is commonly corrected by either setback genioplasty or burring reduction, but these approaches are less likely to produce aesthetically pleasing results. Both procedures have poor reduction effects because of the low response rate of soft tissues to skeletal alterations. There is a high likelihood of chin ptosis and flattening. Setback genioplasty can also yield step deformities at the inferior mandibular border. To overcome these drawbacks of conventional methods, I developed a novel technique of coronal-splitting reduction genioplasty. I have performed more than 83 procedures with a high success rate over the past 10 years. Alloplastic chin implant-shaped bone fragments were resected from the prominent bony chin, in which the average thickness of resected bone was 8.2 mm. Sufficient sagittal reduction effects were then achieved in most cases, although the soft tissue response rate remains 25%–50%, as reported in the literature. The no-degloving technique with cephalic suspension of the mentalis muscle prevents chin ptosis. Combined bilateral oblique osteotomies of the inferior mandibular border contribute to minimizing obvious postoperative chin flattening. Moreover, macrogenia can be large in multiple planes, including anteroposterior, vertical, transverse, or their combinations. This new technique can handle all three planes by combining both bilateral oblique osteotomies of the inferior mandibular border and burr ostectomy. Overall, these findings suggest that the coronal-splitting genioplasty method may replace conventional methods for correcting macrogenia.
Takeaways
Question: Compared with conventional methods for correcting macrogenia, does the novel technique of coronal-splitting reduction genioplasty improve postoperative outcomes?
Findings: With coronal-splitting reduction genioplasty, the average thickness of resected bone fragments is 8.2 mm, which can result in greater skeletal alteration than is achievable with conventional methods, potentially providing a greater improvement in anteroposterior macrogenia reduction. Furthermore, in combination with bilateral oblique osteotomies of the mandibular inferior borders, the coronal-splitting method effectively achieves three-dimensional chin reduction. Aesthetic complications such as chin ptosis and flattening are largely avoided.
Meaning: Coronal-splitting reduction genioplasty is safe and effective for correcting macrogenia.
INTRODUCTION
The chin has a strong influence on facial aesthetics and harmony on both frontal and profile views. Some quantitative analyses are used to assess the position of the chin relative to the overall face, nose, and lips.1 Briefly, if the soft tissue pogonion lies anterior to the most projecting portion of the lower lip, anteroposterior macrogenia may exist.2 Anteroposterior macrogenia is commonly corrected by either setback genioplasty with a plate or burring of the pogonion.3,4 However, these approaches are less likely to produce aesthetically pleasing results. First, both procedures may provide insufficient surgical effects because of the low response rate of soft tissues to skeletal alterations.4 Second, there is a high likelihood of chin ptosis, which can be quite unaesthetic.5,6 Third, an unnatural, flattened appearance of the chin may result.7 Fourth, setback genioplasty can yield step deformities at the inferior border of the mandible.3
In 2011, I developed a new technique of coronal-splitting reduction genioplasty to overcome these drawbacks of conventional methods. This innovative technique was inspired by alloplastic chin augmentation for microgenia. I thought that, in contrast, an alloplastic implant-shaped bone fragment could be removed with better results for anteroposterior macrogenia. The osteotomy was performed in a similar manner as in sagittal splitting ramus osteotomy.
METHODS
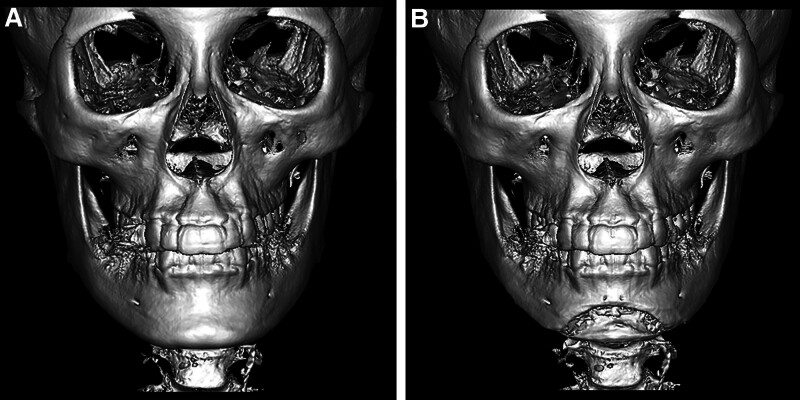
The procedure is demonstrated in the Video. Additionally, to facilitate an understanding of this procedure, pre- and postoperative computed tomographic images are shown in Figure 1.
Fig. 1.
Computed tomography images of coronal-splitting reduction genioplasty. A preoperative computed tomography image of a patient with macrogenia is shown (A). The patient underwent coronal-splitting osteotomy, in which the thickness of the resected bone was 8 mm. Bilateral inferior mandibular border osteotomies were performed toward the mandibular angles. A 3-mm vertical shortening was performed using a burr. A computed tomography image immediately after the surgery is shown (B). Subsequently, reduction of the prominent bony chin was accomplished on the anteroposterior, vertical, and transverse planes.
All operations were performed under general anesthesia. A lower labial incision was made through the mucosa, and the periosteum was dissected. The mental nerve was identified and preserved, and the lower border of the mandible was exposed after anterior subperiosteal dissection. Care must be taken to limit caudal dissection to preserve the lingual muscular attachment. The line for the coronal-splitting osteotomy was marked after the contour of the prominent bony chin. A caudal osteotomy line was drawn along the posterior margin of the base of the mandible. [See Video (online), which demonstrates coronal-splitting reduction genioplasty combined with bilateral osteotomies of the inferior border of the mandible.]
Video 1. This video demonstrates coronal splitting reduction genioplasty combined with bilateral osteotomies of the inferior border of the mandible.
A monocortical cut was made all around the marked line using a round 2-mm burr or an ultrasonic curettage device (SONOPET UST-2001, Stryker, USA). An oscillating saw was then used at the base of the mandible, which is imperative to avoid accidental fracture during splitting osteotomy. Coronal-splitting osteotomy was then performed using a chisel, resulting in only the lingual cortex remaining. Next, bilateral oblique osteotomies of the inferior mandibular border were routinely performed to minimizing postoperative chin flattening. The osteotomies were executed from the point 10 mm lateral to the midline of the base of the chin to approximately a few centimeters posteriorly to the mental foramina using a reciprocating saw.8 If needed, vertical shortening was performed by burr ostectomy. All sharp bony edges were smoothed with a burr.
Next, a cortical bone tunnel was made a few millimeters above the superior osteotomy line using a hole burr. The lower mentalis muscle was replaced superior to its original position to effectively move up the chin pad using a 3–0 absorbable suture with the bone tunnel. The wound was finally closed in two layers.
DISCUSSION
Conventional anteroposterior reduction genioplasty can yield poor aesthetic outcomes. The low response rates of soft tissues to skeletal alterations in reduction genioplasty can cause insufficient surgical effects.4 The response rates of soft tissues range from 0.85 to 1:1 in advancement and are at best 0.5:1 in posterior repositioning.8,9 In burr reduction ostectomy, the response rates range from 0.25:1 to 0.5:1.4
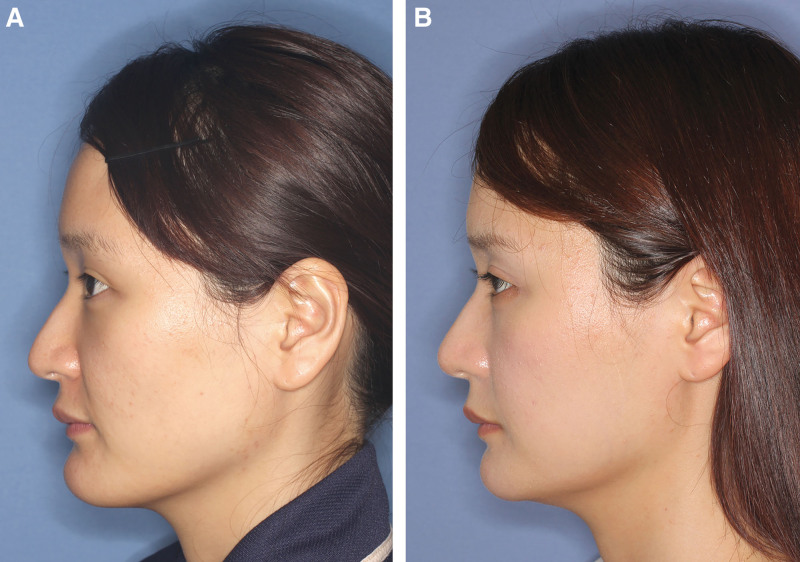
In this study, alloplastic chin implant–shaped bone fragments composed of both cortical and cancellous bone were resected from the prominent bony chin. The average thickness of resected bone was 8.2 mm (range, 5–12 mm), which may result in greater skeletal alteration compared with that in conventional methods.3 Therefore, coronal-splitting reduction genioplasty provided sufficient surgical effects for anteroposterior microgenia, although the soft tissue response rate remains 25%–50%, as reported in the literature (Fig. 2).4
Fig. 2.
Photographs of the patient with anteroposterior microgenia. A, A 28-year-old woman had macrogenia. She underwent both coronal-splitting reduction genioplasty and bilateral osteotomies of the inferior mandibular border. The thickness of the resected bone was 9 mm. B, The postoperative results at 16 months are shown. Anterior–posterior reduction of the chin was sufficiently achieved, whereas postoperative chin ptosis was avoided.
Macrogenia can be large in multiple planes: anteroposterior, vertical, transverse, or their various combinations.2 Combined bilateral oblique osteotomies of the inferior mandibular border are essential for enhancing the aesthetic appearance of the results. First, transverse reduction of the chin is achieved. Second, full-thickness resection of the mental tubercles contributes to less noticeable postoperative chin flattening. If needed, vertical reduction is performed using a burr. Thus, this new surgical procedure can handle all planes. (See figure, Supplement Digital Content 1, which shows pre- and postoperative frontal views of the patient in Fig. 2. Transverse, vertical, and anteroposterior reduction of the chin was balanced, and postoperative flattening of the chin was avoided. http://links.lww.com/PRSGO/D141.)
Setback genioplasty is associated with a fairly high rate of witch chin deformity, which is characterized by soft tissue ptosis.6 To avoid this displeasing chin deformity with the presented procedure, the following three points are important. First, subperiosteal dissection should stop at the posterior margin of the base of the mandible to preserve soft tissue contact with the lingual cortex as much as possible.3,10 Second, suspension of the soft tissue chin pad superior to its original position with the bone tunnel is critical to prevent the descent of soft tissue. Third, submental liposuction is needed for patients who have developed excess submental soft tissue.
In this retrospective case series, no major complications were observed. Most patients were satisfied with the surgical results; however, some complained about the aesthetic results. It is impossible to adjust the postoperative chin projection due to unpredictable changes in the soft tissue. Thus, overcorrection or undercorrection can occur, both subjectively and objectively. Two patients requested a further reduction. Clockwise rotation of the bimaxillary complex was performed for both patients. In contrast, filler injection was performed for one patient who complained of overcorrected chin retraction. Two patients complained of indistinct labiomental folds postoperatively. The V-Y plasty technique on the wet vermilion or filler injection at the vermilion border was somewhat useful in such cases. Patients with shallow labiomental folds may be contraindicated.
There are technical limitations to this procedure. Macrogenia can be caused by volumetric excess of the overlying soft tissue alone; if so, clockwise rotation of the bimaxillary complex is needed. Patients with skeletal class III malocclusion require consideration of orthognathic surgery in addition to (or instead of) genioplasty.
Despite these technical limitations, I have performed more than 83 procedures with a high success rate over the past 10 years. Overall, this study suggests that the novel technique of coronal-splitting reduction genioplasty may replace conventional methods for correcting macrogenia.
DISCLOSURE
The author has no financial interest to declare in relation to the content of this article.
PATIENT CONSENT
The patient provided written consent for the use of her image.
ACKNOWLEDGMENTS
The author thanks Dean M. Toriumi, MD, for professional proofreading of the article and Kiyonori Harii, MD, for collecting references. The author also thanks Mizuho Kamisawa and Sakiko Katsumata for formatting the figures and editing the video.
Supplementary Material
Footnotes
Published online 8 April 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Riedel RA. An analysis of dentofacial relationships. Am J Orthodonti. 1957;43:103–119. [Google Scholar]
- 2.Guyuron B, Michelow BJ, Willis L. Practical classification of chin deformities. Aesthetic Plast Surg. 1995;19:257–264. [DOI] [PubMed] [Google Scholar]
- 3.Bell WH, Brammer JA, McBride KL, et al. Reduction genioplasty: surgical techniques and soft-tissue changes. Oral Surg Oral Med Oral Pathol. 1981;51:471–477. [DOI] [PubMed] [Google Scholar]
- 4.Guyuron B, Weinfeld AB. Genioplasty. In: Guyuron B, ed. Plastic Surgery: Indications and Practice. New York, N.Y.: Elsevier; 2012:179–197. [Google Scholar]
- 5.Zide BM, Boutros S. Chin surgery III: revelations. Plast Reconstr Surg. 2003;111:1542–50; discussion 1551. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez-Ulloa M. Ptosis of the chin. The witches’ chin. Plast Reconstr Surg. 1972;50:54–57. [DOI] [PubMed] [Google Scholar]
- 7.Warren SM, Allori AC, McCarthy JG. Autologous contouring the lower face. In: Aston SJ, Steinbrech DS, Walden JL, eds. Aesthetic Plastic Surgery. New York, N.Y.: Elsevier; 2009:411–422. [Google Scholar]
- 8.Rosen HM. Osseous genioplasty. In: Aston SJ, Beasley RW, Throne HM, Barlett SP, Gunter GC, Spear SL, eds. Grabb and Smith’s Plastic Surgery. 6th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2007:557–561. [Google Scholar]
- 9.Hohl TH, Epker BN. Macrogenia: a study of treatment results, with surgical recommendations. Oral Surg Oral Med Oral Pathol. 1976;41:545–567. [DOI] [PubMed] [Google Scholar]
- 10.Zhang BH, Byrd R, Bradley C, et al. Osseous genioplasty: prevention of witch’s chin deformity with no-degloving technique. Plast Reconstr Surg. 2021;148:720e–726e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.