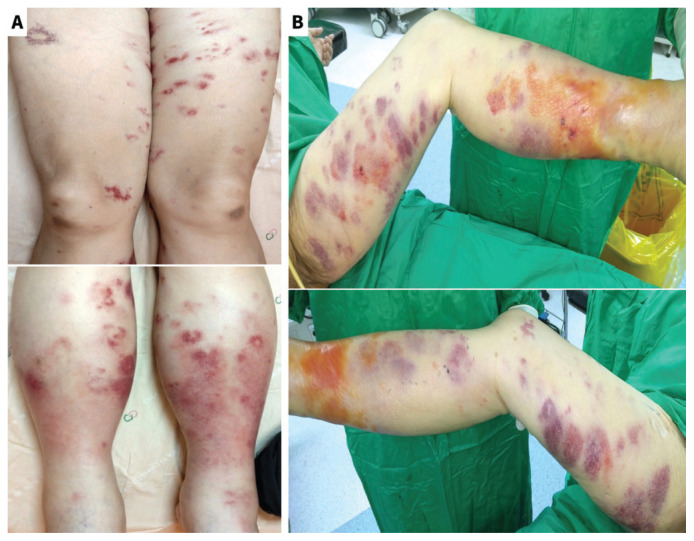
A 44-year-old woman presented to our emergency department in Chiayi City, Taiwan, with fever and a skin rash on both lower limbs (Figure 1A) for 1 day. She had eaten raw tuna and oysters 2 days earlier and had no other symptoms. She was taking iron supplements, having had a gastrectomy previously. There was no history of liver disease, and she had not been exposed to seawater. On arrival, she was hypotensive (72/38 mm Hg) and tachycardic; laboratory investigations showed elevated C-reactive protein (47.23 mg/L; reference range ≤ 3 mg/L) and lactate levels (4.23 mmol/L; reference range 0.5–2.2 mmol/L). The patient was started on inotropic agents and intravenous piperacillin–tazobactam, and admitted to the intensive care unit. Disseminated intravascular coagulation developed on the third day of hospitalization. On the same day, the patient’s blood cultures yielded Vibrio vulnificus, and her antibiotics were changed to ceftazidime and doxycycline. She developed painful bullae (Figure 1B). We incised and drained the bullae, releasing turbid fluid; this revealed fascial necrosis requiring urgent fasciotomy. Plastic surgeons performed débridement and bilateral fasciotomies, and the wounds were left open for 9 days after the procedure. We diagnosed primary septicemia due to V. vulnificus causing necrotizing fasciitis. Wounds were closed on day 12 of hospitalization, and the patient was discharged with no disability 21 days after hospital admission.
Figure 1:
(A) Multiple polymorphic erythematous macules and patches widely distributed on both thighs and legs without bullae formation in a 44-year-old female with necrotizing fasciitis caused by Vibrio vulnificus on the first day of hospitalization. (B) On the third day of hospitalization, multiple purpuric patches on both thighs and legs were seen as well as fluid-filled bullae formation on both legs.
Vibrio vulnificus primarily infects humans through raw seafood ingestion or exposure of wounds to contaminated water sources, such as warm brackish water, river estuaries, or marshes.1,2 Individuals with liver disease, diabetes, immunodeficiency, hemochromatosis (iron overload), or history of gastrointestinal surgery are at higher risk of severe infection.1 Primary septicemia, comprising 60% of cases, typically results in shock, severe cellulitis, blistering, or necrotizing fasciitis affecting both lower extremities.1 The recommended treatment is a third-generation cephalosporin in combination with doxycycline1,3 and emergency surgical débridement for severe soft tissue infection. 1,3 Despite aggressive treatment, the case fatality rate exceeds 50% for primary septicemia, particularly in cases with hypotension.1,2 The incidence is increasing in North America.2
Footnotes
Competing interests: None declared.
The authors have obtained patient consent.
This article has been peer reviewed.
References
- 1.Yun NR, Kim DM. Vibrio vulnificus infection: a persistent threat to public health. Korean J Intern Med (Korean Assoc Intern Med) 2018;33:1070–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Archer EJ, Baker-Austin C, Osborn TJ, et al. Climate warming and increasing Vibrio vulnificus infections in North America. Sci Rep 2023;13:3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu W, Shen X, Pan H, et al. Clinical features and treatment of patients with Vibrio vulnificus infection. Int J Infect Dis 2017;59:1–6. [DOI] [PubMed] [Google Scholar]