Abstract
Objectives
We aimed to investigate the efficacy of lifestyle interventions for the management of SSc.
Methods
We searched the MEDLINE, Embase, Web of Science and CINAHL databases in June 2021. We included studies conducted on five or more patients with SSc published between 1 January 2000 and the search date evaluating lifestyle interventions, excluding systematic reviews without meta-analyses. Critical appraisal was conducted using critical appraisal tools from the Joanna Briggs Institute. Thirty-six studies were included for full-text evaluation.
Results
A total of 17 studies evaluated the effect of physical exercise alone, whereas 14 studies evaluated educational interventions for mental health management, often with physical exercise as a central component. At an aggregated level, these studies support patient education and physical exercise for the improvement of physical function, in particular hand and mouth function. Studies on diet and nutrition were few (n = 5) and pertained to gastrointestinal as well as anthropometric outcomes; these studies were insufficient to support any conclusions.
Conclusion
Physical exercise and patient education should be considered for improving physical function in patients with SSc. These interventions can be provided alongside pharmacotherapy, but there is no evidence supporting that they can be a substitute. Further research should aim at assessing the effects of reductions of harmful exposures, including tobacco smoking and alcohol, improving sleep and enhancing social relations, three hitherto underexplored facets of lifestyle in the context of SSc.
Keywords: systemic sclerosis, lifestyle intervention, physical activity, physical exercise, patient education, self-management
Key messages .
The efficacy of lifestyle interventions in systemic sclerosis is underexplored.
Patient education enhances outcomes and physical exercise improves physical function in systemic sclerosis.
Lifestyle interventions constitute a supplement, not a substitute, to pharmacotherapy.
Introduction
SSc is a chronic connective tissue disease that primarily affects women, commonly in their fifth decade of life, and can manifest with limited cutaneous involvement, diffuse cutaneous involvement or with no cutaneous involvement [1]. The estimated prevalence ranges from <150–443 cases per million population, being higher in regions such as southern Europe, North America and Australia [1]. Areas commonly affected by skin fibrosis are the hands and face, which often results in impaired hand function [2] and microstomia [3]. Although advances in pharmacotherapy for rheumatic diseases have been achieved during the 21st century, the guidelines for non-pharmacological management in general, and lifestyle interventions in particular, are ill-defined.
Upon examination of the literature, the definition of a lifestyle intervention itself is not clearly characterized. The American College of Lifestyle Medicine (ACLM) defines lifestyle medicine as ‘a medical specialty that uses therapeutic lifestyle interventions as a primary modality’ and lists six fundamental domains as targets of lifestyle medicine: nutrition, exercise, stress, substance abuse, sleep and relationships [4]. Analogously, the British Society of Lifestyle Medicine specifies six ‘pillars of lifestyle medicine’: healthy eating, physical activity, mental well-being, minimizing harmful substances, sleep and healthy relationships [5]. As such, a lifestyle intervention can be any intervention that covers any or all six domains, i.e. physical activity and exercise, diet and nutrition, mental health, harmful exposures, sleep and social relations.
The importance of lifestyle in the management of rheumatic diseases is gaining recognition. The EULAR recently published recommendations regarding lifestyle behaviours and work participation aimed at preventing disease progression in patients with rheumatic and musculoskeletal diseases [6]. These 18 recommendations, accompanied by five overarching principles, were derived from systematic literature reviews geared toward six ‘lifestyle exposures’, i.e. exercise, diet, weight, alcohol, smoking and work participation [6]. Recently the EULAR also issued guidelines for the non-pharmacological management of SLE and SSc [7], following a thorough systematic literature review [8]. However, this review, while comprehensive, did not distinctly isolate lifestyle interventions from other approaches. Consequently, valuable insights into lifestyle interventions targeting modifiable health factors were obscured among the multitude of non-pharmacological management strategies examined. To bridge this gap in the literature, we herein conducted a systematic literature review to address the efficacy of lifestyle interventions in different aspects of the disease course in people living with SSc.
Methods
Inclusion and exclusion criteria
Inclusion criteria for studies included a date of publication between 1 January 2000 and the search date, having a cohort of patients with SSc (as defined by classification criteria and/or International Classification of Diseases codes) as a population under investigation and evaluation of a lifestyle intervention. Studies were excluded if they had fewer than five participants, if they were systematic reviews without a meta-analysis, had no data on a distinct SSc patient population, were duplicates, were written in a language other than English, Spanish, or Swedish or if they did not assess an intervention that comprised one or more of the following: physical activity and exercise, diet and nutrition, mental health, harmful exposures, sleep and social relations.
Search strategy
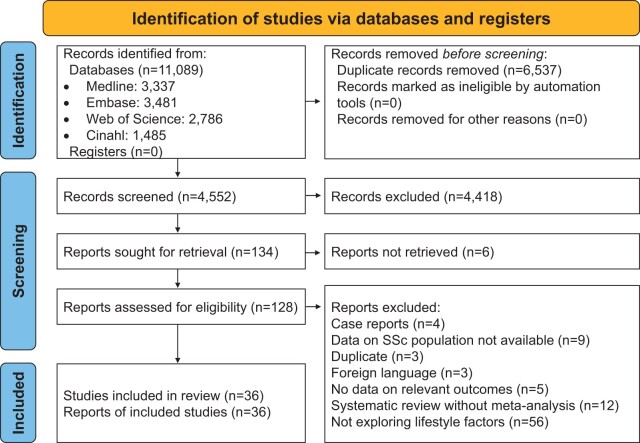
On 22 June 2021, the MEDLINE, Embase, Web of Science and CINAHL databases were searched for studies concerning non-pharmacological management for SSc. Two investigators (A.G. and J.C.) screened the 11 089 initial hits under supervision of one senior investigator (I.P.). Conflicts were solved upon discussion with two investigators (I.P. and C.B.). The search and study selection was documented according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement (Fig. 1) [9].
Figure 1.
Flowchart of study selection
Data extraction
Data extraction was conducted by one researcher (J.C.) under the supervision of one senior investigator (I.P.). Data extracted included the number of participants for each study, interventions or management strategies given to both experimental and control groups, the characteristics of the comparator group, outcomes and the efficacy of the intervention. These data are provided in Supplementary Table S1, available at Rheumatology Advances in Practice online.
Categorization
After data extraction and risk of bias (RoB) assessment, the studies were grouped by the category of lifestyle intervention they assessed. Studies combining exercise protocols with other educational interventions were separated from studies evaluating only physical exercise protocols, which in turn constituted their own group. Studies within the two above categories specifically evaluating the hand and mouth were further subgrouped into their own categories.
Quality assessment and evidence grading
RoB assessment for all included articles was conducted by one researcher (A.T.) using the Joanna Briggs Institute critical appraisal (CA) tools (checklists) [10]. Since all articles were already included before quality assessment for this review, the alternatives for overall appraisal ‘include’, ‘exclude’ and ‘seek further info’ were modified to ‘robust’, ‘weak’ and ‘intermediate’, respectively. The appropriate checklist for each study was selected based on the study design. A study was deemed weak if there were six or more checklist items it did not clearly fulfil, intermediate if there were three to five checklist items it did not clearly fulfil or robust if it clearly fulfilled all checklist items but two or fewer. After CA, studies were graded by level of evidence (LoE) according to the Oxford Centre for Evidence-Based Medicine [11].
Results
Study characteristics
Thirty-six studies were included. Of these, 17 evaluated physical activity and exercise alone rather than in combination with other interventions [12–28]. Fourteen studies evaluated the efficacy of mental health management [29–42] and five studies assessed diet and nutrition [43–47]. Fig. 1 presents a flowchart of the study selection. Studies and their characteristics, including the number of participants, interventions, characteristics of the comparator groups and outcomes are provided in Supplementary Table S1, available at Rheumatology Advances in Practice online.
Physical activity and exercise
General
A randomized controlled trial (RCT) examining the effect of a tailored home-based exercise program (CA: intermediate; LoE: 2) found improvements in 6-min walking distance (6MWD) [48], the physical component score (PCS) of the 36-item Short Form Health Survey (SF-36) [49] and the HAQ Disability Index (HAQ-DI) [15, 50]. Two RCTs evaluating the effect of exercise on microcirculation (CA: weak; LoE: 3) found no significant impact on cutaneous vascular conductance (CVC) after 12 weeks of high-intensity interval training alone [21]; however, this produced a significant effect when combined with endurance training [22]. An RCT evaluating tai chi (CA: weak; LoE: 3) found improvements in scores relating to balance (Berg Balance Scale [51]), sleep (Pittsburgh Sleep Quality Index [52]) and fatigue (Fatigue Severity Scale [53]), but not trunk lateral endurance (trunk lateral endurance test [23, 54]. Observational studies found that lower quadriceps strength associated with worse HAQ-DI scores (CA: robust; LoE: 3) [19] and that exercise habits associated with improved scores on the HAQ-DI and the Patient-Reported Outcomes Measurement Information System [55] (PROMIS; CA: intermediate; LoE: 3) [20]. Aerobic exercise improved maximum oxygen consumption (VO2max) without exacerbation of skin induration, RP or digital ulcers at an 8-week follow-up (CA: intermediate; LoE: 3) [17].
Hand
An RCT by Rannou et al. [13] (CA: robust; LoE: 2) provided 4 weeks of personalized physical therapy to the experimental group and found an improvement in the HAQ-DI and hand function measured by the Cochin Hand Function Scale (CHFS) [56] after 4 weeks compared with patients receiving usual care. However, these improvements disappeared after 12 months. Stretching programs for hands improved scores in the Canadian Occupational Performance [57] after 3 months (CA: intermediate; LoE: 2) [12] but did not improve Hand Mobility in Scleroderma (HAMIS) test [2] scores at 9 or 18 weeks, regardless of adjunct treatment with paraffin baths (CA: intermediate; LoE: 2) [14]. Two RCTs evaluating functional impairment (CA: weak; LoE: 3) showed that app-delivered occupational therapy and stretching exercises administered through a telemedicine system were efficacious in improving hand function [25] as measured by a shortened version of the Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH) [58] and HAMIS [18]. A controlled quasi-experimental study (CA: intermediate; LoE: 3) found daily stretching exercises improved the range of motion in each finger in patients with SSc 1 month after baseline, and this improvement was maintained or further increased after 1 year from baseline [16].
Mouth
The RCT by Rannou et al. [13] (CA: robust; LoE: 2) showed that 1 month of personalized physical therapy produced a sustained improvement in oral aperture up to 1 year from baseline. Another RCT (CA: weak; LoE: 3) found 12 weeks of an orofacial exercise protocol improved scores in the Mouth Handicap in Systemic Sclerosis index [3] up to 20 weeks from baseline [24]. An uncontrolled quasi-experimental study (CA: robust; LoE: 4) found daily mouth stretching exercises improved oral aperture 18 weeks after baseline.
Mental health
General
An RCT evaluating the efficacy of a self-management website (CA: weak; LoE: 3) found no differences compared with issuing an educational patient-focused book when assessing PROMIS (primary outcome) scores at 16 weeks [35]. A controlled quasi-experimental study evaluating 3 weeks of patient education through occupational therapy (CA: robust; LoE: 3) found improvements in the HAQ-DI up to 24 weeks after baseline [34].
Hand
An RCT evaluating an educational program for self-management (CA: intermediate; LoE: 2) noted improvements in hand-related measures such as the HAMIS, Duruoz Hand Index [56], HAQ-DI and handgrip strength after 8 weeks [32]. A controlled quasi-experimental study (CA: intermediate; LoE: 3) found an educational self-management program for hands reduced the pain experienced by patients assessed using a visual analogue scale as well as improved CHFS scores after 24 weeks [36]. The protocol in this study was based on an uncontrolled study published the year before (CA: robust; LoE: 4), which also found amelioration of pain experienced by patients as well as improvements in CHFS scores after 8 weeks [42].
Mouth
An RCT evaluating the effect of patient education with emphasis on orofacial exercises (CA: intermediate; LoE: 2) found that face-to-face training increased oral aperture more than educational material alone at 12 months after baseline in per-protocol analysis [30]. Another RCT (CA: intermediate; LoE: 2) found an increase in oral aperture after 1 month of orofacial exercise, regardless of whether they received oral hygiene advice before or after [31]. Two RCTs by Yuen et al. [29, 33] examined the effects of oral health interventions, including instruction on dental product use and orofacial exercises. One of these studies [33] found an increase in oral aperture at 3 months, but not 6 months after baseline (CA: intermediate; LoE: 2), noting low adherence to the exercise program in particular, while the other study (CA: weak; LoE: 3) assessed gingival health and found significant improvements in the Löe–Silness gingival index [59] in both groups at 6 months after baseline, but a larger improvement in the intervention group compared with controls. Yet another multifaceted oral hygiene intervention was evaluated in an uncontrolled study by Poole et al. [39] (CA: intermediate; LoE: 4) and incorporated instruction of hand exercises on top of dental hygiene and orofacial exercise instruction. After a 6-month intervention, this study noted improvements in the Patient Hygiene Performance Index (PHP) [60] after 12 months from baseline, but no improvements in upper extremity measures such as the Keitel Function Test [61] or oral aperture [39].
Diet and nutrition
Five selected studies examined the effect of diet and nutrition (CA: four intermediate, one weak). Two RCTs on this topic examining the effects of probiotics found no significant changes in the University of California, Los Angeles Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument (GIT-score) [62] compared with placebo after 60 days (CA: intermediate; LoE: 2) [43] and 8 weeks (CA: weak; LoE: 3) [44], respectively. However, the former study found an improvement in the GIT-score reflux component after 120 days [43] and the in latter study a decrease in Th17 cells after 8 weeks compared with placebo [44]. Conversely, one uncontrolled quasi-experimental study (CA: intermediate; LoE: 4) found that the use of probiotics associated with a significant reduction in total GIT-score as well as the reflux and bloating/distention component scores after 2 months [45].
Two quasi-experimental studies evaluated nutritional therapy. One found that nutritional support had no significant improvement in weight, body mass index (BMI) [63], energy intake or SF-36, with follow-up time points up to 12 months (CA: intermediate; LoE: 4) [46]. The other study found improvement in the abridged Patient-Generated Subjective Global Assessment [64] and a reduction in the number of patients classified as sarcopenic by DXA after 18 months (CA: intermediate; LoE: 4) [47]. The study did not find significant changes in caloric intake or macronutrient distribution in the enrolled patients [47].
Discussion
This systematic review of the literature assessed the current evidence for lifestyle interventions as viable management strategies for people living with SSc. The main categories of intervention were physical activity and exercise, mental health and diet and nutrition. Physical exercise in general improved functional impairment and aerobic capacity, while stretching exercises of the hands and mouth efficaciously ameliorated hand impairment and microstomia. Stretching exercises of the hands and mouth were in turn often central components of educational interventions, which in principle focused on different facets of self-management. Studies on diet and nutrition showed sparse efficacy of probiotics in alleviating gastrointestinal symptoms and limited use of nutritional therapy for improving body composition. Overall, there was no rigorous investigation as to how lifestyle affects global disease activity in SSc. Furthermore, none of the included studies aimed to replace pharmacotherapy with lifestyle interventions.
These findings are largely in line with the comprehensive body of evidence compiled in the EULAR recommendations for lifestyle behaviours and work participation [6], which conclude that physical exercise can be a safe and beneficial way to improve functional impairment. However, factors such as comorbidities and disease severity warrant caution when recommending physical exercise as a part of disease management, which, as always, should be tailored to the patient. Furthermore, the findings in this review also agree that the evidence for recommending specific diets for the management of rheumatic and musculoskeletal diseases is sparse [6]. Relating to the principal components of lifestyle medicine [4, 5], there are gaps in knowledge regarding the effect of sleep, social relations and the use of harmful substances (such as nicotine, tobacco and alcohol) on SSc specifically. For these lifestyle domains, there exist EULAR recommendation sets [6, 7, 65] and other systematic reviews [8, 66].
The categorization of interventions was not absolute, as many studies employed a combination of many different intervention categories. For example, studies on nutritional therapy [46, 47] consisted of counselling and informative meetings, as in the studies on patient education. Similarly, educational interventions often had exercise programs as a central constituent [29–33, 36, 39, 42]. The complexity of stratifying studies by category implies a tendency in current research toward examining multimodal approaches when evaluating lifestyle interventions. This may be based on mechanistic reasoning that certain lifestyle interventions should produce a larger effect size when made concurrently but complicates the assessment when trying to discern the efficacy of individual interventions in isolation.
A limitation that we encountered while compiling the evidence was the lack of a structured synthesis or meta-analysis. Moreover, the overall CA was derived from assessment by only one investigator, which potentially reduces the reliability of the RoB assessment. Despite this, there are strengths to this review in the form of a generous inclusion of studies spanning a period of >2 decades with varied study designs and a conservative approach in the CA of studies, treating unclearly fulfilled criteria as unfulfilled.
Considering that most of the studies included in this review were conducted in Europe (particularly Italy) and the USA, caution should be exercised when generalizing the findings to other regions, particularly those with different healthcare systems, demographics and environmental factors. While a focus on Western countries may provide valuable insights into lifestyle interventions in SSc, extrapolating these findings to populations worldwide should be approached with caution.
In conclusion, this systematic review found physical exercise and mental health management to be efficacious lifestyle interventions for improving functional impairment in patients with SSc, which we therefore advocate should be considered for patients suffering from hand or face involvement, reduced muscle function and reduced physical fitness. Importantly, it is worth mentioning that current evidence overall supports lifestyle interventions as a complement and not a substitute to pharmacotherapy. Future studies, preferably of RCT design, are needed for exploring other aspects of lifestyle interventions, namely concerning diet and nutrition, sleep, harmful exposures and social relations, and how these potentially impact the disease course and patient experience, particularly the degree of disease activity.
Supplementary Material
Acknowledgements
The authors express gratitude to Emma-Lotta Säätelä, librarian at the KI Library, for her help with the search strategy.
Contributor Information
Ioannis Parodis, Division of Rheumatology, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden; Department of Gastroenterology, Dermatology and Rheumatology, Karolinska University Hospital, Stockholm, Sweden; Department of Rheumatology, Faculty of Medicine and Health, Örebro University, Örebro, Sweden.
Alexander Tsoi, Division of Rheumatology, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden; Department of Gastroenterology, Dermatology and Rheumatology, Karolinska University Hospital, Stockholm, Sweden.
Alvaro Gomez, Division of Rheumatology, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden; Department of Gastroenterology, Dermatology and Rheumatology, Karolinska University Hospital, Stockholm, Sweden.
Jun Weng Chow, Division of Rheumatology, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden; Department of Gastroenterology, Dermatology and Rheumatology, Karolinska University Hospital, Stockholm, Sweden.
Charlotte Girard-Guyonvarc’h, Division of Rheumatology, Department of Medicine, University Hospital of Geneva and Faculty of Medicine, University of Geneva, Geneva, Switzerland.
Tanja Stamm, Section for Outcomes Research, Center for Medical Statistics, Informatics and Intelligent Systems, Medical University of Vienna, Vienna, Austria; Ludwig Boltzmann Institute for Arthritis and Rehabilitation, Vienna, Austria.
Carina Boström, Division of Physiotherapy, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden; Department of Occupational Therapy and Physiotherapy, Karolinska University Hospital, Stockholm, Sweden.
Supplementary material
Supplementary material is available at Rheumatology Advances in Practice online.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
Authors’ contributions
I.P. and C.B. were responsible for study conception and design, supervision of study selection and data extraction. I.P., C.G., T.S. and C.B. were responsible for the methodology. I.P., A.T., A.G. and J.C. were responsible for study selection and data extraction. A.T. was responsible for risk of bias assessment. I.P. and A.T. were responsible for drafting the manuscript. All authors reviewed and approved the final version of the manuscript and are responsible for its content.
Funding
I.P. has received grants from the Swedish Rheumatism Association (R-969696), King Gustaf V’s 80-year Foundation (FAI-2020–0741), Swedish Society of Medicine (SLS-974449), Nyckelfonden (OLL-974804), Professor Nanna Svartz Foundation (2021-00436), Ulla and Roland Gustafsson Foundation (2021-26), Region Stockholm (FoUI-955483) and Karolinska Institutet. C.B. has received grants from the Swedish Rheumatism Association and Norrbacka-Eugeniastiftelsen.
Disclosure statement: I.P. has received research funding and/or honoraria from Amgen, AstraZeneca, Aurinia, Bristol Myers Squibb, Eli Lilly, Gilead, GSK, Janssen, Novartis, Otsuka and Roche. The remaining authors have declared no conflicts of interest. The funders had no role in the design of the study; the collection, analyses or interpretation of data; writing of the manuscript or in the decision to publish the results.
References
- 1. Allanore Y, Simms R, Distler O. et al. Systemic sclerosis. Nat Rev Dis Primers 2015;1:15002. [DOI] [PubMed] [Google Scholar]
- 2. Sandqvist G, Eklund M.. Hand Mobility in Scleroderma (HAMIS) test: the reliability of a novel hand function test. Arthritis Care Res 2000;13:369–74. [PubMed] [Google Scholar]
- 3. Mouthon L, Rannou F, Bérezné A. et al. Development and validation of a scale for mouth handicap in systemic sclerosis: the Mouth Handicap in Systemic Sclerosis scale. Ann Rheum Dis 2007;66:1651–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American College of Lifestyle Medicine. What is lifestyle medicine? 2022. https://lifestylemedicine.org/ACLM/ACLM/About/What_is_Lifestyle_Medicine_/Lifestyle_Medicine.aspx?hkey=26f3eb6b-8294-4a63-83de-35d429c3bb88
- 5. British Society of Lifestyle Medicine. The pillars of lifestyle medicine. 2022. https://bslm.org.uk/
- 6. Gwinnutt JM, Wieczorek M, Balanescu A. et al. 2021 EULAR recommendations regarding lifestyle behaviours and work participation to prevent progression of rheumatic and musculoskeletal diseases. Ann Rheum Dis 2022;82:48–56. [DOI] [PubMed] [Google Scholar]
- 7. Parodis I, Girard-Guyonvarc’h C, Arnaud L. et al. EULAR recommendations for the non-pharmacological management of systemic lupus erythematosus and systemic sclerosis. Ann Rheum Dis 2023;doi:10.1136/ard-2023-224416. [DOI] [PubMed] [Google Scholar]
- 8. Parodis I, Gomez A, Tsoi A. et al. Systematic literature review informing the EULAR recommendations for the non-pharmacological management of systemic lupus erythematosus and systemic sclerosis. RMD Open 2023;9:e003297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aromataris E, Munn Z, eds. JBI manual for evidence synthesis. 2020. https://synthesismanual.jbi.global (1 April 2024, date last accessed).
- 11. Howick J, Chalmers I, Glasziou P. et al. The Oxford levels of evidence 2. 2011. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (1 April 2024, date last accessed).
- 12. Stefanantoni K, Sciarra I, Iannace N. et al. Occupational therapy integrated with a self-administered stretching program on systemic sclerosis patients with hand involvement. Clin Exp Rheumatol 2016;34(Suppl 100):157–61. [PubMed] [Google Scholar]
- 13. Rannou F, Boutron I, Mouthon L. et al. Personalized physical therapy versus usual care for patients with systemic sclerosis: a randomized controlled trial. Arthritis Care Res 2017;69:1050–9. [DOI] [PubMed] [Google Scholar]
- 14. Gregory WJ, Wilkinson J, Herrick AL.. A randomised controlled trial of wax baths as an additive therapy to hand exercises in patients with systemic sclerosis. Physiotherapy 2019;105:370–7. [DOI] [PubMed] [Google Scholar]
- 15. Filippetti M, Cazzoletti L, Zamboni F. et al. Effect of a tailored home-based exercise program in patients with systemic sclerosis: a randomized controlled trial. Scand J Med Sci Sports 2020;30:1675–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mugii N, Hasegawa M, Matsushita T. et al. The efficacy of self-administered stretching for finger joint motion in Japanese patients with systemic sclerosis. J Rheumatol 2006;33:1586–92. [PubMed] [Google Scholar]
- 17. Oliveira NC, dos Santos Sabbag LM, de Sá Pinto AL, Borges CL, Lima FR.. Aerobic exercise is safe and effective in systemic sclerosis. Int J Sports Med 2009;30:728–32. [DOI] [PubMed] [Google Scholar]
- 18. Piga M, Tradori I, Pani D. et al. Telemedicine applied to kinesiotherapy for hand dysfunction in patients with systemic sclerosis and rheumatoid arthritis: recovery of movement and telemonitoring technology. J Rheumatol 2014;41:1324–33. [DOI] [PubMed] [Google Scholar]
- 19. Lima TR, Guimaraes FS, Carvalho MN. et al. Lower limb muscle strength is associated with functional performance and quality of life in patients with systemic sclerosis. Braz J Phys Ther 2015;19:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Azar M, Rice DB, Kwakkenbos L. et al. Exercise habits and factors associated with exercise in systemic sclerosis: a Scleroderma Patient-centered Intervention Network (SPIN) cohort study. Disabil Rehabil 2018;40:1997–2003. [DOI] [PubMed] [Google Scholar]
- 21. Mitropoulos A, Gumber A, Crank H, Akil M, Klonizakis M.. The effects of upper and lower limb exercise on the microvascular reactivity in limited cutaneous systemic sclerosis patients. Arthritis Res Ther 2018;20:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mitropoulos A, Gumber A, Akil M, Klonizakis M.. Exploring the microcirculatory effects of an exercise programme including aerobic and resistance training in people with limited cutaneous systemic sclerosis. Microvasc Res 2019;125:103887. [DOI] [PubMed] [Google Scholar]
- 23. Cetin SY, Calik BB, Ayan A.. Investigation of the effectiveness of Tai Chi exercise program in patients with scleroderma: a randomized controlled study. Complement Ther Clin Pract 2020;40:101181. [DOI] [PubMed] [Google Scholar]
- 24. Maddali Bongi S, Passalacqua M, Landi G. et al. Rehabilitation of the face and temporomandibular joint in systemic sclerosis. Ther Adv Musculoskelet Dis 2021;13:1759720X211020171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Murphy SL, Barber M, Huang S. et al. Intensive and app-delivered occupational therapy to improve upper extremity function in early diffuse cutaneous systemic sclerosis: a pilot two-arm trial. Rheumatology (Oxford) 2021;60:5002–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pizzo G, Scardina GA, Messina P.. Effects of a nonsurgical exercise program on the decreased mouth opening in patients with systemic scleroderma. Clin Oral Invest 2003;7:175–8. [DOI] [PubMed] [Google Scholar]
- 27. Pinto AL, Oliveira NC, Gualano B. et al. Efficacy and safety of concurrent training in systemic sclerosis. J Strength Cond Res 2011;25:1423–8. [DOI] [PubMed] [Google Scholar]
- 28. Defi IR, Gultom C, Chorman MJ, Jennie J.. High-intensity interval training can improve hand grip strength, inspiratory muscle, and quality of life in systemic sclerosis subjects. Reumatologia 2021;59:98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yuen HK, Marlow NM, Reed SG. et al. Effect of orofacial exercises on oral aperture in adults with systemic sclerosis. Disabil Rehabil 2012;34:84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Uras C, Mastroeni S, Tabolli S. et al. A comparison between two educational methods in the rehabilitation of the microstomia in systemic sclerosis: a randomized controlled trial. Clin Rehabil 2019;33:1747–56. [DOI] [PubMed] [Google Scholar]
- 31. Cüzdan N, Türk İ, Çiftçi V. et al. The effect of a home-based orofacial exercise program on oral aperture of patients with systemic sclerosis: a single-blind prospective randomized controlled trial. Arch Rheumatol 2021;36:176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gokcen N, Badak SO, Sarpel T, Sertdemir Y, Erken E.. The efficacy of a home-based, self-administered hand exercise program for patients with systemic sclerosis: a randomized controlled, evaluator-blind, clinical trial. J Clin Rheumatol 2022;28:e422–9. [DOI] [PubMed] [Google Scholar]
- 33. Yuen HK, Weng Y, Bandyopadhyay D. et al. Effect of a multi-faceted intervention on gingival health among adults with systemic sclerosis. Clin Exp Rheumatol 2011;29(2 Suppl 65):S26–32. [PMC free article] [PubMed] [Google Scholar]
- 34. Zanatta E, Rodeghiero F, Pigatto E. et al. Long-term improvement in activities of daily living in women with systemic sclerosis attending occupational therapy. Br J Occup Ther 2017;80:417–22. [Google Scholar]
- 35. Khanna D, Serrano J, Berrocal VJ. et al. Randomized controlled trial to evaluate an internet-based self-management program in systemic sclerosis. Arthritis Care Res 2019;71:435–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Landim S, Bertolo M, Del Rio A. et al. Sustained efficacy of a concise self-management programme for hands in systemic sclerosis: a longitudinal case-control observational study. Rheumatology (Oxford) 2020;59:3330–9. [DOI] [PubMed] [Google Scholar]
- 37. Samuelson UK, Ahlmen EM.. Development and evaluation of a patient education program for persons with systemic sclerosis (scleroderma). Arthritis Care Res 2000;13:141–8. [DOI] [PubMed] [Google Scholar]
- 38. Brown SJ, Somerset ME, McCabe CS, McHugh NJ.. The impact of group education on participants’ management of their disease in lupus and scleroderma. Musculoskelet Care 2004;2:207–17. [DOI] [PubMed] [Google Scholar]
- 39. Poole J, Conte C, Brewer C. et al. Oral hygiene in scleroderma: the effectiveness of a multi-disciplinary intervention program. Disabil Rehabil 2010;32:379–84. [DOI] [PubMed] [Google Scholar]
- 40. Poole JL, Skipper B, Mendelson C.. Evaluation of a mail-delivered, print-format, self-management program for persons with systemic sclerosis. Clin Rheumatol 2013;32:1393–8. [DOI] [PubMed] [Google Scholar]
- 41. Poole JL, Mendelson C, Skipper B, Khanna D.. Taking charge of systemic sclerosis: a pilot study to assess the effectiveness of an internet self-management program. Arthritis Care Res 2014;66:778–82. [DOI] [PubMed] [Google Scholar]
- 42. Landim SF, Bertolo MB, Marcatto de Abreu MF. et al. The evaluation of a home-based program for hands in patients with systemic sclerosis. J Hand Ther 2019;32:313–21. [DOI] [PubMed] [Google Scholar]
- 43. Low AHL, Teng GG, Pettersson S. et al. A double-blind randomized placebo-controlled trial of probiotics in systemic sclerosis associated gastrointestinal disease. Semin Arthritis Rheum 2019;49:411–9. [DOI] [PubMed] [Google Scholar]
- 44. Marighela TF, Arismendi MI, Marvulle V. et al. Effect of probiotics on gastrointestinal symptoms and immune parameters in systemic sclerosis: a randomized placebo-controlled trial. Rheumatology (Oxford) 2019;58:1985–90. [DOI] [PubMed] [Google Scholar]
- 45. Frech TM, Khanna D, Maranian P. et al. Probiotics for the treatment of systemic sclerosis-associated gastrointestinal bloating/distention. Clin Exp Rheumatol 2011;29(2 Suppl 65):S22–5. [PubMed] [Google Scholar]
- 46. Ortiz-Santamaria V, Puig C, Soldevillla C. et al. Nutritional support in patients with systemic sclerosis. Reumatol Clin 2014;10:283–7. [DOI] [PubMed] [Google Scholar]
- 47. Doerfler B, Allen TS, Southwood C. et al. Medical Nutrition Therapy for Patients With Advanced Systemic Sclerosis (MNT PASS): a pilot intervention study. J Parenter Enteral Nutr 2017;41:678–84. [DOI] [PubMed] [Google Scholar]
- 48. Guyatt GH, Sullivan MJ, Thompson PJ. et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985;132:919–23. [PMC free article] [PubMed] [Google Scholar]
- 49. Ware JE Jr, Sherbourne CD.. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 50. Fries JF, Spitz P, Kraines RG, Holman HR.. Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137–45. [DOI] [PubMed] [Google Scholar]
- 51. Berg KO, Wood-Dauphinee SL, Williams JI, Maki B.. Measuring balance in the elderly: validation of an instrument. Can J Public Health 1992;83(Suppl 2):S7–11. [PubMed] [Google Scholar]
- 52. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ.. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 53. Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD.. The Fatigue Severity Scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989;46:1121–3. [DOI] [PubMed] [Google Scholar]
- 54. McGill SM, Childs A, Liebenson C.. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil 1999;80:941–4. [DOI] [PubMed] [Google Scholar]
- 55. Cella D, Yount S, Rothrock N. et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap Cooperative Group during its first two years. Med Care 2007;45(5 Suppl 1):S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Duruöz MT, Poiraudeau S, Fermanian J. et al. Development and validation of a rheumatoid hand functional disability scale that assesses functional handicap. J Rheumatol 1996;23:1167–72. [PubMed] [Google Scholar]
- 57. Law M, Baptiste S, McColl M. et al. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther 1990;57:82–7. [DOI] [PubMed] [Google Scholar]
- 58. Gummesson C, Ward MM, Atroshi I.. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 2006;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Löe H, Silness J.. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand 1963;21:533–51. [DOI] [PubMed] [Google Scholar]
- 60. Podshadley AG, Haley JV.. A method for evaluating oral hygiene performance. Public Health Rep 1968;83:259–64. [PMC free article] [PubMed] [Google Scholar]
- 61. Keitel W, Hoffmann H, Weber G, Krieger U.. [Evaluation of the percentage of functional decrease of the joints using a motor function test in rheumatology]. Dtsch Gesundheitsw 1971;26:1901–3. [PubMed] [Google Scholar]
- 62. Khanna D, Hays RD, Maranian P. et al. Reliability and validity of the University of California, Los Angeles Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument. Arthritis Rheum 2009;61:1257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL.. Indices of relative weight and obesity. J Chronic Dis 1972;25:329–43. [DOI] [PubMed] [Google Scholar]
- 64. Vigano AL, di Tomasso J, Kilgour RD. et al. The abridged patient-generated subjective global assessment is a useful tool for early detection and characterization of cancer cachexia. J Acad Nutr Diet 2014;114:1088–98. [DOI] [PubMed] [Google Scholar]
- 65. Rausch Osthoff AK, Niedermann K, Braun J. et al. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis 2018;77:1251–60. [DOI] [PubMed] [Google Scholar]
- 66. Wieczorek M, Gwinnutt JM, Ransay-Colle M. et al. Smoking, alcohol consumption and disease-specific outcomes in rheumatic and musculoskeletal diseases (RMDs): systematic reviews informing the 2021 EULAR recommendations for lifestyle improvements in people with RMDs. RMD Open 2022;8:e002170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.