Summary
Cavernous hemangioma, currently known as “cavernous venous malformation,” is a common, benign, non-infiltrative, slowly progressive vascular malformation of the orbit presenting in adults. We report the case of a 9-year-old girl who presented with a painless palpable mass over the right upper eyelid of 7 years’ duration. A computed tomography scan of the orbits revealed a heterogeneously enhancing, well-circumscribed mass in the right upper eyelid with no orbital extension. A transcutaneous excisional biopsy with histopathology disclosed cavernous venous malformation. The majority of cavernous venous malformations are intraconal and present in the fourth to fifth decade of life.
Introduction
Cavernous venous malformation is a slow-flow vascular anomaly according to the International Society for the Study of Vascular Anomalies (ISSVA). It accounts for 5%–7% of all orbital masses and is the most prevalent vascular lesion of the orbit in adults.1 It is a hamartoma that usually presents in middle-aged adults, more often in females.2 Almost 80% of orbital cavernous venous malformations are located within the muscle cone lateral to the optic nerve, and -thus presenting as gradually increasing, painless, axial proptosis.3 Rarely, cavernous venous malformations can be painful, with multiple lesions, and develop in the extraconal space, resulting in nonaxial proptosis. Cavernous venous malformation primarily involving the eyelid without orbital extension is very rare. To our knowledge, this is the first reported case of isolated cavernous hemangioma of the eyelid occurring in the first decade of life.
Case Report
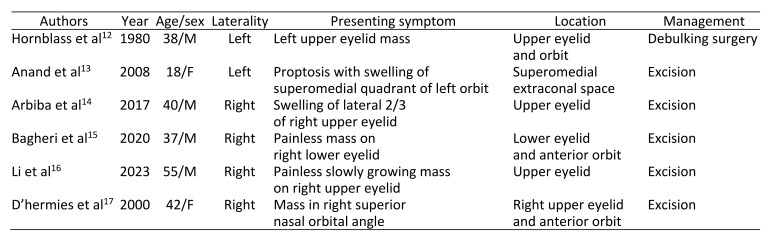
A 9-year-old girl presented at Eye OPD of Postgraduate Institute of Medical Education and Research, Chandigarh, India with a chief complaint of a right upper eyelid mass for 7 years. The mass was initially small in size showing gradual, painless enlargement over the years. There was no prior evidence of vision loss, proptosis, ocular deviation, or diplopia. There was no previous history of similar swelling in either eyelid or in other parts of the body. The systemic examination was normal. Her best-corrected visual acuity was 6/6 in each eye. Extraocular movements, intraocular pressure, and the anterior and posterior segments were normal. The mass, located within the right upper eyelid, was soft and measured 2 × 1 cm. It was globular in shape, with a lobulated surface extending from the lateral canthus up to lateral to midline of the upper eyelid with preserved eyelashes (Figure 1).
Figure 1.
A, Clinical image showing firm, globular, lobulated right upper eyelid mass (arrow). B, Postoperative photograph showing improved eyelid contour.
On palpation, the mass was firm, well-circumscribed, not fixed to the overlying skin, and comparatively mobile. Finger insinuation was possible below the supraorbital rim. The mass was nonreducible and nonpulsatile. On auscultation, no bruit was heard. It did not increase in dimension with the Valsalva maneuver. No proptosis was noted.
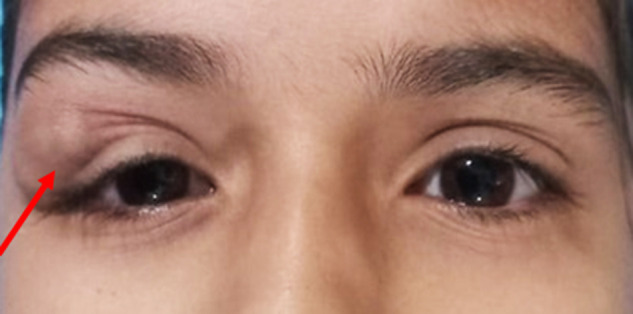
Computed tomography (CT) of the orbits revealed a heterogeneously enhancing mass lesion measuring 1.8 × 2.1 × 1.3 cm in the superolateral aspect of the right upper eyelid, anterior to the septum, with no orbital extension (Figure 2).
Figure 2.
Axial computed tomography scan of the orbits revealing heterogeneously enhancing mass lesion in the lateral aspect of the right upper eyelid with no orbital extension.
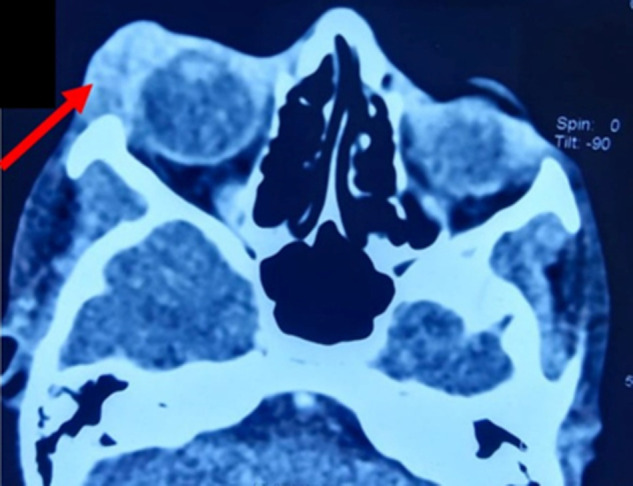
Under general anesthesia, the patient underwent surgical excision of the lesion via a transcutaneous approach, with an incision over the mass. A multilobulated, well-encapsulated mass of reddish-pink color measuring 2.5 × 1 cm was excised (Figure 3). The mass was sparsely adherent to surrounding tissue and could be easily delivered through the wound. No significant bleeding was present, and no feeding vessel was identified. Minimal oozing from the surgical field was managed. The surgical incision was closed in two layers after the excision of redundant skin. Histopathological examination of the excised mass revealed a well-encapsulated lesion composed of dilated, thin-walled vascular channels lined by a single layer of endothelium with no atypia, mitosis, or necrosis. The findings were suggestive of cavernous venous malformation (Figure 4).
Figure 3.
Gross specimen showing multilobulated reddish-pink mass.
Figure 4.
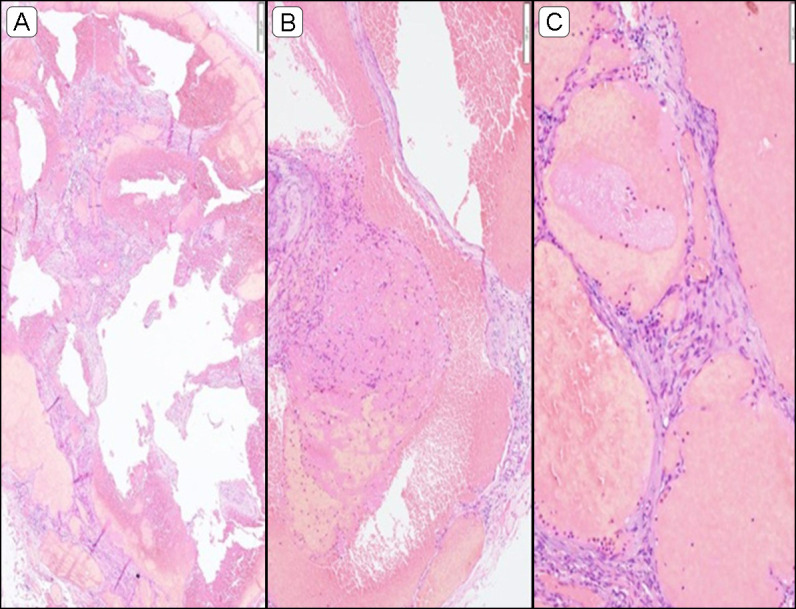
Histopathological examination of the eyelid mass with hematoxylin-eosin (H&E) stain A, Low magnification depicting circumscribed lesion composed of dilated thin-walled vascular channels (scale bar = 200 µm). B, Occasional vessels shows fibrin thrombi within its lumen (scale bar = 100 µm). C, High magnification depicting flattened endothelial cells (scale bar = 50 µm).
Postoperatively, the patient showed marked improvement in eyelid contour. The reconstructive outcome was good (Figure 1B), as was functional outcome during 8 months of follow-up.
Discussion
The most frequent vascular lesion of the orbit in adults is cavernous venous malformation, commonly known as cavernous hemangioma. It is considered a congenital anomaly. Cavernous venous malformation is most frequently located in the lateral aspect of the retrobulbar muscle cone.2 Cavernous venous malformations in the orbit can cause various symptoms, depending on their location. They may result in painless proptosis if involving the muscle cone, diplopia if affecting the extraocular muscles, decreased vision if compressing the optic nerve, ptosis and a palpable mass in the eyelid, or a visible mass underneath the skin if located superficially. Orbital cavernous venous malformations typically present in individuals during their fourth to fifth decade of life, making their occurrence in individuals under the age of 20 years rare.4,5
There are two types of cavernous venous malformation of the eyelid: hypodermal and dermal. Hypodermal lesions are relatively superficial, well-circumscribed, and dark blue in color due to dilatation and engorgement of blood vessels, whereas the dermal lesions are more deeply situated and are more infiltrating, with no change in color of the overlying skin.6 Ours was a case a hypodermal cavernous venous malformation of the eyelid.
The differential diagnosis, based on history and clinical examination, included cavernous venous malformation, dermoid, neurofibroma, and lymphangioma. Considering the regular surface and margin with absence in direction of bony fusion, dermoid was ruled out.7 The absence of café au lait spots, Lisch nodules, or cutaneous multiple fibromas precluded neurofibroma.8 Lymphangioma is characteristically ill-circumscribed, and in contrast to cavernous venous malformation, it shows an infiltrative growth pattern.9
Evagelidou et al10 reported a case of an infant with orbital cavernous venous malformation and accompanying intracranial lesions. Maheshwari et al11 reported a case of a 4-year-old girl who presented with painless unilateral proptosis, with histopathology suggestive of cavernous venous malformation. Neither of these cases reported the occurrence of cavernous venous malformation specifically in the eyelid without extension into the orbit.
The underlying pathophysiology of cavernous venous malformations consist of hemodynamic changes causing opening of new channels and extension of tumor into interstitium separated by a fibrous capsule from the surrounding normal tissue. Why these lesions tend to occur in the orbit versus eyelid is poorly understood.
Isolated cavernous venous malformation of the eyelid is rare; when present, it is usually accompanied by an orbital lesion. Table 1 summarizes the findings of previous studies that have described eyelid mass as a presenting symptom of cavernous venous malformation; the majority of them had an accompanying orbital lesion.12–17 In an analysis of 214 cases of cavernous vascular malformation of the orbit, 11.7% of lesions presented with eyelid swelling.18 Aymard et al19 and Rootman et al20 reported orbital cavernous venous malformation extending to subcutaneous tissue in 9.3% and 5.1% of patients, respectively. In most cases, the lesion is well-circumscribed. Cavernous venous malformation typically shows sluggish, gradual enlargement but do not regress spontaneously.
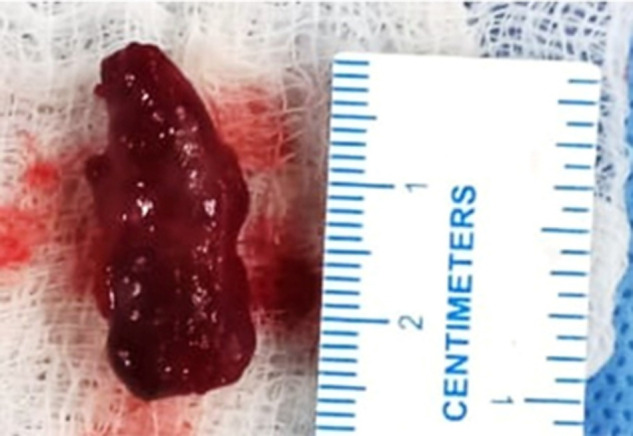
Table 1.
Previous studies describing eyelid mass as a presenting symptom of cavernous venous malformation
Preoperative imaging allows for the accurate diagnosis of 93% of patients.18 Small calcifications or phleboliths may be visible on CT in addition to homogeneous soft tissue density. On dynamic imaging, cavernous venous malformation is characterized by progressive enhancement.
Histopathologically, cavernous venous malformation consists of numerous large, dilated, blood-filled vascular spaces lined by a flat layer of endothelium and enclosed in a pseudocapsule. They do not possess a prominent arterial supply. The lumens may show intralesional thrombosis because of the slow vascular flow and resultant stasis.1
The management of cavernous venous malformation of the eyelid depends on the location along with the rate of growth of the mass. Smaller lesions that do not produce any functional compromise may be observed. Rapidly enlarging lesions causing deprivation, anisometropic amblyopia, or aesthetic impairment warrant treatment.
In conclusion, cavernous venous malformation may occur superficially in the eyelid, and it must be considered in the differential diagnosis for any well-defined eyelid tumor. Other diagnoses should be accurately ruled out by a proper examination of the mass and relevant investigations, including imaging and histopathology. A well-circumscribed cavernous venous malformation of the eyelid can easily be excised and should be followed by a histopathologic analysis to rule out any malignant component.
Literature Search
PubMed was searched in May 2023 for English-language results using the following terms: cavernous hemangioma, eyelid, cavernous venous malformation, child, pediatric, and young age.
References
- 1.Calandriello L, Grimaldi G, Petrone G, et al. Cavernous venous malformation (cavernous hemangioma) of the orbit: current concepts and a review of the literature. Surv Ophthalmol. 2017;62:393–403. doi: 10.1016/j.survophthal.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Ansari SA, Mafee MF. Orbital cavernous hemangioma: role of imaging. Neuroimaging Clin N Am. 2005;15:137–58. doi: 10.1016/j.nic.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Louisraj S, Ponnudurai T, Rodriguez D, Thomas PA, Nelson Jesudasan CA. Cavernous hemangioma of the orbit: an unusual acute presentation. Int Med Case Rep J. 2017;10:255–9. doi: 10.2147/IMCRJ.S133284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acciarri N, Giulioni M, Padovani R, Gaist G, Pozzati E, Acciarri R. Orbital cavernous angiomas: surgical experience on a series of 13 cases. J Neurosurg Sci. 1995;39:203–9. [PubMed] [Google Scholar]
- 5.Orcuitt JC, Wulc AE, Mills RP, Smith CH. Asymptomatic orbital cavernous hemangiomas. Ophthalmology. 1991;98:1257–60. doi: 10.1016/s0161-6420(91)32146-8. [DOI] [PubMed] [Google Scholar]
- 6.Margileth AM, Museles M. Current concepts in diagnosis and management of congenital cutaneous hemangiomas. Pediatrics. 1965;36:410–6. [PubMed] [Google Scholar]
- 7.Sezenoz AS, Arat YO, Tepeoglu M. An unusual eyelid mass: tarsal dermoid cyst. Saudi J Ophthalmol. 2015;29:312–4. doi: 10.1016/j.sjopt.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pe’er J. Pathology of eyelid tumors. Indian J Ophthalmol. 2016;64:177–90. doi: 10.4103/0301-4738.181752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pang P, Jakobiec FA, Iwamoto T, Hornblass A. Small lymphangiomas of the eyelids. Ophthalmology. 1984;91:1278–84. doi: 10.1016/s0161-6420(84)34158-6. [DOI] [PubMed] [Google Scholar]
- 10.Evagelidou E, Tsanou E, Asproudis I, et al. Orbital cavernous hemangioma in an infant with intracranial lesions: a case report. Cases J. 2009;2:6912. doi: 10.4076/1757-1626-2-6912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maheshwari R, Thool A. Orbital cavernous hemangioma of childhood. Indian J Ophthalmol. 2007;55:313–5. doi: 10.4103/0301-4738.33052. [DOI] [PubMed] [Google Scholar]
- 12.Hornblass A, Sabates WI. Eyelid and orbital cavernous hemangioma associated with keratoconus. Am J Ophthalmol. 1980;89:396–400. doi: 10.1016/0002-9394(80)90010-0. [DOI] [PubMed] [Google Scholar]
- 13.Anand R, Deria K, Sharma P, Narula M, Garg R. Extraconal cavernous hemangioma of orbit: a case report. Indian J Radiol Imaging. 2008;18:310–2. doi: 10.4103/0971-3026.43849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aribaba OT, Idowu OO, Olowoyeye AO, Amusan OO. Ocular adnexa carvenous hemagioma: case report. Adv Ophthalmol Vis Syst. 2017;7:426–7. [Google Scholar]
- 15.Bagheri A, Feizi M, Tavakoli M. Unusual subcutaneous presentation of cavernous hemangioma in the lower eyelid. J Ophthalmic Vis Res. 2020;15:236–9. doi: 10.18502/jovr.v15i2.6741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li R, Ren M, Liu L. Infrequent giant cutaneous cavernous hemangioma of the eyelid. Ophthalmology. 2023;130:654. doi: 10.1016/j.ophtha.2022.08.001. [DOI] [PubMed] [Google Scholar]
- 17.D’hermies F, Cherif N, Hurbli T, et al. Unusual preseptal location of an orbital cavernous hemangioma in African patient [in French] J Fr Ophtalmol. 2000;23:631–4. [PubMed] [Google Scholar]
- 18.Yan J, Wu Z. Cavernous hemangioma of the orbit: analysis of 214 cases. Orbit. 2004;23:33–40. doi: 10.1076/orbi.23.1.33.28992. [DOI] [PubMed] [Google Scholar]
- 19.Aymard PA, Langlois B, Putterman M, Jacomet PV, Morax S, Galatoire O. Management of orbital cavernous hemangioma—evaluation of surgical approaches: report of 43 cases [in French] J Fr Ophtalmol. 2013;36:820–9. doi: 10.1016/j.jfo.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Rootman DB, Heran MK, Rootman J, White VA, Luemsamran P, Yucel YH. Cavernous venous malformations of the orbit (so-called cavernous haemangioma): a comprehensive evaluation of their clinical, imaging and histologic nature. Br J Ophthalmol. 2014;98:880–8. doi: 10.1136/bjophthalmol-2013-304460. [DOI] [PubMed] [Google Scholar]