Abstract
Background
Birth asphyxia is still one of the primary causes of newborn mortality worldwide. Similarly, the risk of newborn asphyxia in Ethiopia remains unacceptably high. Thus, studies on the incidence and predictors of mortality among newborns admitted with birth asphyxia are crucial to addressing this problem. As a result, the purpose of this study was to assess the incidence and predictors of mortality among neonates admitted with birth asphyxia to the neonatal intensive care units (NICUs) of West Shewa Zone Public Hospitals in Central Ethiopia.
Methods
An institution-based retrospective cohort study was conducted among 760 asphyxiated neonates admitted to the NICUs of West Shewa Zone Public Hospitals between 30 March 2021 and 30 April 2023. The data were collected using CSEntry and analysed bu using Stata V.17. Bivariate and multivariate Cox proportional hazard regression analyses were carried out, and significant predictors were found using a 95% CI and a p<0.05.
Results
A total of 760 asphyxiated neonates were followed for a total of 6880 neonatal days. At the end of follow-up, 263 (34.6%) of the neonates died (95% CI 31.3% to 38.1%), which resulted in a mortality incidence of 10.6/100 person-days of observation. Chewing khat (adjusted HR, AHR 2.21; 95% CI 1.13 to 4.31), home delivery (AHR 1.45, 95% CI 1.1 to 1.9), lack of antenatal care follow-up (AHR 1.44, 95% CI 1.08 to 1.89), hypothermia (AHR 1.56, 95% CI 1.12 to 2.17), hypoglycaemia (AHR 2.23, 95% CI 1.91 to 2.25) and obstructed labour (AHR 1.4, 95% CI 1.02 to 1.91) were found to be the significant predictors of neonatal mortality among asphyxiated neonates at a p≤0.05.
Conclusion and recommendation
The magnitude of neonatal mortality among asphyxiated neonates in the study area was high. Therefore, in order to significantly reduce the risks of birth asphyxia and subsequent newborn death, all interested stakeholders should take these predictors into consideration.
Keywords: Mortality, Neonatology
WHAT IS ALREADY KNOWN ON THIS TOPIC
Birth asphyxia significantly contributes to the high neonatal mortality rate in Ethiopia.
In Ethiopia, the neonatal mortality rate increased from 29 deaths per 1000 live births in 2016 to 33 in 2019.
WHAT THIS STUDY ADDS
This study uses Cox proportional hazard regression to provide greater statistical power to identify predictors of mortality due to birth asphyxia.
A mortality incidence due to birth asphyxia was found to be 10.6/100 person-days of observation.
Chewing khat, home delivery, lack of antenatal care follow-up, hypoglycaemia and obstructed labour were found to be the significant predictors of neonatal mortality among asphyxiated neonates.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
HRs make the results clearly understandable, improving the accessibility of the data for non-statisticians and healthcare professionals.
This finding is crucial for improving clinical care, informing policy decisions and ultimately reducing the burden of neonatal mortality associated with birth asphyxia.
Background
Birth asphyxia is defined by the WHO as a failure to initiate and sustain breathing at birth.1 It happens when the blood flow to or from the fetus is cut-off or when gas exchange is compromised before, during or after childbirth. Birth asphyxia can cause multisystem organ failure, severe metabolic acidosis, hypercarbia, progressive hypoxaemia, newborn encephalopathy and possibly death.2 Based on the appearance, pulse, grimace, activity and respiration (APGAR) score in the 1st, 5th and 10th min of life, birth asphyxia can be categorised as mild, moderate or severe.2
In the first month of life, 2.4 million children worldwide died in 2020. Approximately 6700 newborns die per day, which accounts for 47% of all children under the age of 5 who pass away, up from 40% in 1990. With 27 deaths per 1000 live births, sub-Saharan Africa had the highest newborn mortality rate in 2020.1
Birth asphyxia, along with severe infections and preterm birth, is one of the primary causes of neonatal fatalities worldwide, accounting for an estimated 900 000 deaths each year.3 4 It is also estimated to account for approximately 23% of all newborn deaths globally.4 With mortality rates of 26.7% for newborns and 11.3% for children under the age of 5, respectively, birth asphyxia is the second-leading cause of newborn mortality in Ethiopia.5
The Sustainable Development Goals were adopted by the United Nations in 2015, with the goal of lowering newborn mortality to less than 12 per 1000 live births by 2030.6 The Ethiopian government has also undertaken multiple strategies to achieve this target, including promoting the development of emergency obstetric and newborn care services with the goal of improving neonatal and maternal health.7 However, newborn deaths continue to be a major public health concern.
Birth asphyxia has a wide spectrum of complications that can damage the newborn’s motor, sensory, cognitive and psychosocial development.8 9 Even though the vast majority of newborns suffering from birth asphyxia recover quickly, a small number may develop hypoxic-ischaemic encephalopathy (HIE).10 Around 20%–30% of HIE infants die in the neonatal period, and 33%–50% of survivors have permanent neurodevelopmental problems such as cerebral palsy and mental retardation.11 12
There are various factors that increase the chance of death in newborns who have asphyxia. Risk factors for HIE include prematurity, maternal fever, multiple pregnancies, maternal anaemia, neonates who require resuscitation, neonates who have convulsions, prolonged capillary refill time, stage of HIE, low APGAR score (0–3), coma, prolonged seizures that are resistant to treatment, end-organ dysfunction and congenital brain malformation.13–16
Identifying predictors of mortality in asphyxiated newborns is critical for developing effective therapies and implementing critical measures on time. However, factors influencing death in asphyxiated newborns in Ethiopia have not been thoroughly studied. Moreover, the majority of previous research used logistic regression analysis, but in the current study, Cox proportional hazard regression analysis was used. This choice was made because the Cox model offers advantages over logistic regression in time-to-event data and survival analysis. It handles time-to-event variables, provides more statistical power and offers interpretability through easily understandable HRs, making the results more accessible to clinicians and non-statisticians. Therefore, this study was aimed at determining the incidence and predictors of mortality among newborns suffering from birth asphyxia in selected hospitals in West Shewa Zone, central Ethiopia.
Methods
Study setting, design and period
A facility-based retrospective cohort study was conducted among asphyxiated neonates admitted to the neonatal intensive care unit (NICU) of selected hospitals in West Shewa Zone, central Ethiopia, from 30 March 2020 to 30 April 2023. The zone is located in the Oromia Regional State, west of Addis Ababa, Ethiopia’s capital city. Ambo, the capital of the West Shewa Zone, is 114 km from Addis Ababa. According to the West Shewa Zonal Health Office, the zone’s overall population in 2021 is predicted to be 2 381 079, with 1 214 350 women. In the zone, there are 9 government hospitals, 96 health centres and 529 health posts.
Population
All neonates admitted to the NICU of public hospitals in the West Shewa Zone, Ethiopia, with the diagnosis of birth asphyxia were considered the source population, while all neonates admitted to the NICU of selected hospitals in the West Shewa Zone with similar diagnoses were the study population. However, asphyxiated neonates with an unknown date of admission or discharge date were excluded from the study.
Sample size determination and sampling procedure
Four of the nine public hospitals in the West Shewa Zone were chosen at random. The study participants were recruited from the NICU registration logbook. A total of 828 asphyxia cases were recorded in the NICU admission logbooks of the participating hospitals between 30 March 2020 and 30 April 2023. Using their medical record number, asphyxiated infants’ medical records were accessed from the card room. 19 of the 830 neonate cards with birth asphyxia had a different diagnosis, and 49 cards had considerable missing data. Finally, the study included 760 cards that fulfilled the eligibility criteria.
Operational definition
Birth asphyxia is considered when the 5th min APGAR score is less than 7.2
Event: Death of asphyxiated neonates at a specific time (day) within the 28 days of follow-up as evidenced by physician confirmation.17
Censored: Newborns with birth asphyxia who did not develop the outcome of interest (death) until the end of the follow-up period, recovered from illness, discharged against medical advice or transferred out to other health institutions without knowing the outcome.15
Survival time: The time in days from admission to the development of the outcome variable (death) within 28 days follows up time.17
Data collection tools and quality control
By evaluating similar types of literature, the data collection instrument was modified to assess survival status and predictors of mortality among newborns admitted with asphyxia.15–18 The survey was created in CSPRO V.7.3 software and exported to CSEntry for Android for electronic data collection. Data were collected by eight neonatal nurses, with four master’s holders supervising the process.
Data quality was ensured by data collection training, continuous supervision and timely feedback. The data extraction tool was pretested on 5% (38 cards) of the sample size, and any necessary adjustments were performed prior to data collection. The Cronbach alpha value was 0.81, which was used to examine the tool’s internal consistency.
Patient and public involvement
No patient or the public was directly involved in developing the research questions, the design, protocol, data collection tools, results and dissemination plan of the study.
Data processing and analysis
The data were collected using the CS-Entry Android app and then exported to Stata V.17 for analysis. Descriptive statistics were used and provided in tables, figures and text. The study participants’ survival status was described using Kaplan-Meier survival curves. The proportional hazard assumption was tested using global goodness of fit based on Schoenfeld residual before running the Cox proportional hazard regression model, and variables with a p>0.05 were regarded as meeting the assumption. The overall p value for the global test was 0.18, and each predictor variable had a p>0.05. Variables with a p≤0.2 in bivariate Cox regression were further analysed using multivariate Cox regression. As a measure of association, the multivariate Cox regression’s adjusted HR (AHR) with a 95% CI was used. Variables having a p value of 0.5 were regarded as statistically significant predictors.
Results
Sociodemographic characteristics
For this study, 760 newborn charts were analysed, with 433 (57%) of them being male. Almost all, 750 (98.7%) of the asphyxiated neonate’s mothers were married. The majority of respondents, 344 (45.3%), were protestant religious followers, and more than two-thirds, 533 (70.1), were rural residents. In the study, 19.3% of the neonate’s mothers and 17.6% of the neonate’s fathers attended education above college. The majority of the neonate’s mothers, 746 (98.2%), have no history of chewing khat during their current pregnancy (table 1).
Table 1.
Sociodemographic characteristics of a pregnant mother who had admitted asphyxiated babies at NICUs at West Shewa Public Hospitals, Central Ethiopia (N=760)
| Covariates | Categories | Total number (%) | Status | |
| Died (%) | Censored (%) | |||
| Maternal age | <25 | 230 (30.3) | 48 (20.9) | 182 (79.1) |
| 25–34 | 221 (29.1) | 63 (28.5) | 158 (71.5) | |
| ≥35 | 309 (40.6) | 152 (49.2) | 157 (50.8) | |
| Mothers’ educational status | Can’t read and write | 114 (15) | 37 (32.5) | 77 (67.5) |
| Can read and write | 160 (21.1) | 48 (30) | 112 (70) | |
| Primary1–8 | 167 (22) | 61 (36.5) | 106 (63.5) | |
| Secondary9–12 | 172 (22.6) | 83 (48.3) | 89 (51.7) | |
| College and above | 147 (19.3) | 34 (23.1) | 113 (76.9) | |
| Religion | Orthodox | 268 (35.3) | 93 (34.7) | 175 (65.3) |
| Protestant | 344 (45.3) | 148 (43) | 196 (57) | |
| Muslim | 70 (9.2) | 11 (15.7) | 59 (84.3) | |
| Wakefana | 78 (10.3) | 11 (14.1) | 67 (85.9) | |
| Mothers’ occupation | Housewife | 454 (59.8) | 178 (39.2) | 276 (60.8) |
| Private business | 23 (3) | 0 (0) | 23 (100) | |
| Daily labourer | 38 (5) | 5 (13.2) | 33 (86.8) | |
| Family size | <4 | 262 (34.5) | 83 (31.7) | 179 (68.3) |
| 4-5 | 326 (42.9) | 113 (34.7) | 213 (65.3) | |
| ≥6 | 172 (22.6) | 67 (39) | 105 (61) | |
| Distance from health facilities | <10 km | 260 (34.2) | 87 (33.5) | 173 (66.5) |
| ≥10 km | 500 (65.8) | 176 (35.2) | 324 (64.8) | |
| Alcohol consumption | No | 721 (94.9) | 245 (34) | 476 (66) |
| Yes | 39 (5.1) | 18 (46.2) | 21 (53.8) | |
NICUs, neonatal intensive care units.
Neonates-related characteristics
More than three-quarters (79.2%) of newborns were hospitalised within the first hour following birth. The majority of the neonates, 576 (75.8%), had a normal birth weight with a mean weight of 2.86 kg and an SD of ±0.71 kg. Only about one-fourth, 176 (23.2%), of the neonates cried immediately after birth, and only 14.5% of the neonates had a normal APGAR score (≥7) at the 1st min of life. Nearly one-quarter, 193 (25.4%) of the neonates, were preterm. Neonatal resuscitation procedures were performed for the majority, 535 (70.4%) of the study participants in the delivery room immediately after delivery. About two-thirds, 504 (66.4%), of the neonates were hypothermic, while one-fourth, or 194 (25.5%), of the participants were hypoglycaemic. Regarding the management of birth asphyxia, nearly three-fourths (73.6%) of the neonate’s orders were revised every 12 hours by physicists. More than half, 415 (54.5%) of the neonates, were treated with continuous positive airway pressure. The majority of the participants, 480 (63.2%), were given antibiotics (table 2).
Table 2.
Neonates-related characteristics of asphyxiated babies who were admitted at NICUs of West Shewa Public Hospitals, Central Ethiopia (N=760)
| Covariates | Categories | Total number (%) | Status | |
| Died (%) | Censored (%) | |||
| Birth weight | <2500 g | 184 (24.2) | 72 (39.1) | 112 (60.9) |
| ≥2500 g | 576 (75.8) | 191 (33.2) | 385 (66.8) | |
| Gestational age at delivery | Preterm | 193 (25.4) | 134 (69.4) | 59 (30.6) |
| Term | 487 (64.1) | 108 (22.2) | 379 (77.8) | |
| Post-term | 80 (10.5) | 21 (26.3) | 59 (73.7) | |
| APGAR score at 1 min | 0–3 | 398 (52.4) | 206 (51.8) | 192 (48.2) |
| 4–6 | 252 (33.2) | 29 (11.5) | 223 (88.5) | |
| ≥7 | 110 (14.5) | 28 (25.5) | 82 (74.5) | |
| APGAR score at 5th min | 0–3 | 392 (51.6) | 133 (33.9) | 259 (66.1) |
| 4–6 | 320 (42.1) | 109 (34.1) | 211 (65.9) | |
| ≥7 | 48 (6.3) | 21 (43.8) | 27 (56.2) | |
| Comorbidity | No | 558 (73.4) | 188 (33.7) | 370 (66.3) |
| Yes | 202 (26.6) | 75 (37.1) | 127 (62.9) | |
| Oxygen saturation | 50–69 | 300 (39.5) | 93 (31) | 207 (69) |
| 70–89 | 326 (42.9) | 131 (40.2) | 195 (59.8) | |
| ≥90 | 134 (17.6) | 39 (29.1) | 95 (70.9) | |
| RDS | No | 659 (86.7) | 249 (37.8) | 410 (62.2) |
| Yes | 101 (13.3) | 14 (13.9) | 87 (86.1) | |
| MAS | No | 588 (77.4) | 113 (19.2) | 475 (80.8) |
| Yes | 172 (22.6) | 150 (87.2) | 22 (12.8) | |
| Neonatal sepsis | No | 629 (82.8) | 240 (38.2) | 389 (61.8) |
| Yes | 131 (17.2) | 23 (17.6) | 108 (82.4) | |
| Birth Injury | No | 729 (95.9) | 240 (32.9) | 489 (67.1) |
| Yes | 31 (4.1) | 23 (74.2) | 8 (25.8) | |
.APGAR, appearance, pulse, grimace, activity and respiration; MAS, meconium aspiration syndrome; NICUs, neonatal intensive care units ; RDS, respiratory distress syndrome.
Obstetric characteristics of the mother
In this study, almost three-quarters of the women (73%) were multigravida, and the majority of them, 644 (84.7%), had antenatal care (ANC) follow-up. More than two-thirds of those who attend ANC, 453 (70.3%), had four or more ANC visits. The pregnancy-induced hypertension affected 72 (9.5%) of the women. Anaemia due to iron insufficiency was also detected in 187 (24.6%) of the women. In this study, obstetric haemorrhage information was also sought, and the findings showed that 91 (12%) of the women reported experiencing antepartum haemorrhage, while 65 (8.6%) of the women experienced postpartum haemorrhage (online supplemental table).
bmjpo-2023-002403supp001.pdf (33.1KB, pdf)
Survival status of asphyxiated neonates
A total of 760 neonates were followed for 6880 neonatal days, with a minimum and maximum of 1 and 23 days, respectively. The overall graph of the Kaplan-Meier survivor function showed a decrease in deaths over a period of time. According to this graph, the rate of death was highest during the first and second weeks of life (figure 1). Chewing khat, place of delivery, ANC follow-up (figure 2), hypothermia (figure 3), hypoglycaemia (figure 4) and obstructed labour were all factors that contributed to neonatal death from birth asphyxia.
Figure 1.
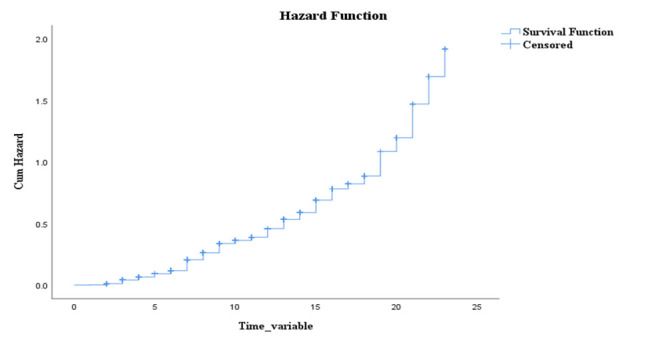
Overall Kaplan-Meier failure estimates of asphyxiated neonates admitted to NICUs of West Shewa Public Hospitals, Central Ethiopia (N=760). NICUs, neonatal intensive care units.
Figure 2.
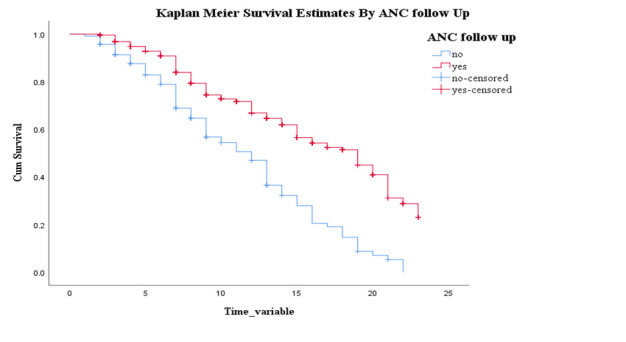
Kaplan-Meier survival curve of neonates with birth asphyxia by ANC follow-up in selected West Shewa Public Hospitals, Central Ethiopia (N=760). ANC, antenatal care.
Figure 3.
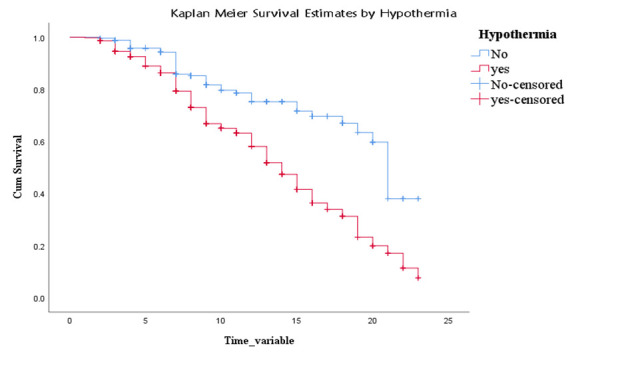
Kaplan-Meier survival curve of neonates with birth asphyxia by hypothermia in selected West Shewa Public Hospitals, Central Ethiopia (N=760).
Figure 4.
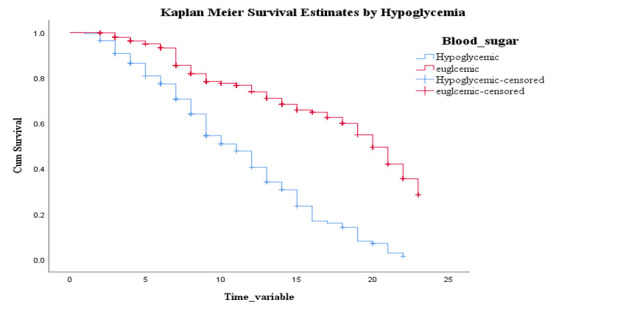
Kaplan-Meier survival curve of neonates with birth asphyxia by neonatal hypoglycaemia in selected West Shewa Public Hospitals, Central Ethiopia (N=760).
Incidence density and median time to death among neonates admitted with birth asphyxia
A total of 263 (34.6%) of the neonates died at the end of the follow-up period (95% CI 31.3% to 38.1%), which resulted in a mortality incidence of 10.6/100 person-days of observation (95% CI 9.4 to 11.9). The median survival time was 16 days (95% CI 15 to 17). The majority of neonatal mortality happens during the first 118 (44.9%) and second 96 (36.5%) weeks of life.
The survival probability of an asphyxiated newborn at the end of 7, 14 and 21 days is 80.8% (95% CI 77.4% to 83.8%), 53.7% (95% CI 48.4% to 58.6%) and 20.8% (95% CI 14.2% to 28.2%), respectively.
Predictors of mortality among neonates with birth asphyxia
The bivariate Cox proportional hazard regression analysis showed a p≤0.2 for maternal-related factors such as age, history of chewing khat, ANC follow-up, obstructed labour and place of delivery. Similar results were obtained for the following variables related to neonates: age at admission, having comorbidity, birth injury, APGAR score at first minute, hypothermia, blood sugar and MAS. Further analysis of the above variables in the multivariable Cox proportional hazard regression revealed that chewing khat, place of delivery, ANC follow-up, hypothermia, hypoglycaemia and obstructed labour were found to be the significant predictors of neonatal mortality among asphyxiated neonates at a p≤0.05.
Asphyxiated newborns whose mothers chewed chats had a 2.21-fold increased risk of mortality (AHR 2.21; 95% CI 1.13 to 4.31). Similarly, compared with mothers who gave birth in healthcare facilities, the risk of death was 1.45 times higher for asphyxiated newborns whose mothers gave birth at home (AHR 1.45, 95% CI 1.1 to 1.9). Additionally, the risk of death was 1.44 times higher among asphyxiated neonates whose mothers didn't have ANC compared with their counterparts (AHR 1.44, 95% CI 1.08 to 1.89). Likewise, when compared with their counterparts, asphyxiated neonates that developed hypothermia had a 1.56 times higher risk of mortality (AHR 1.56, 95% CI 1.12 to 2.17). Moreover, the risk of death was 2.23 times higher among neonates with hypoglycaemia (AHR 2.23, 95% CI 1.91 to 2.25). Finally, the risk of mortality was 1.4 times higher among asphyxiated neonates whose mothers developed obstructed labour during delivery (AHR 1.4, 95% CI 1.02 to 1.91) (table 3).
Table 3.
Predictors of mortality among asphyxiated neonates admitted to NICUs of West Shewa Public Hospitals, Central Ethiopia (N=760)
| Covariates | Category | Survival status | CHR (95% CI) | AHR (95% CI) | |
| Died (%) | Censored (%) | ||||
| Maternal age | <25 | 48 (20.9) | 182 (79.1) | 1 | 1 |
| 25–34 | 63 (28.5) | 158 (71.5) | 1.58 (1.08 to 2.29) | 1.42 (0.96 to 2.08) | |
| ≥35 | 152 (49.2) | 157 (50.8) | 2.72 (1.97 to 3.77) | 1.28 (0.88 to 1.87) | |
| Chewing khat | No | 253 (33.9) | 493 (66.1) | 1 | 1 |
| Yes | 10 (71.4) | 4 (28.6) | 1.96 (1.04 to 3.68) | 2.21 (1.13 to 4.31)* | |
| Age of neonate at admission | <30 min | 68 (31.8) | 146 (62.8) | 0.78 (0.57 to 1.07) | 1.79 (0.98 to 3.28) |
| 30–60 min | 110 (28.4) | 278 (71.6) | 0.65 (0.49 to 0.86) | 1.77 (0.97 to 3.26) | |
| >60 min | 85 (53.8) | 73 (46.2) | 1 | 1 | |
| Birth weight | <2500 g | 72 (39.1) | 112 (60.9) | 1.38 (1.05 to 1.81) | 1.26 (0.86 to 1.85) |
| ≥2500 g | 191 (33.2) | 385 (66.8) | 1 | 1 | |
| Place of delivery | Home | 75 (37.1) | 127 (62.9) | 1.48 (1.13 to 1.94) | 1.45 (1.1 to 1.9)* |
| Health facility | 188 (33.7) | 370 (66.3) | 1 | 1 | |
| Birth injury | No | 240 (32.9) | 489 (67.1) | 1 | 1 |
| Yes | 23 (74.2) | 8 (25.8) | 1.93 (1.25 to 2.96) | 1.49 (0.89 to 2.48) | |
| ANC follow-up | No | 83 (71.6) | 33 (28.4) | 2.33 (1.79 to 3.02) | 1.44 (1.08 to 1.89)* |
| Yes | 180 (28) | 464 (72) | 1 | 1 | |
| Comorbidity | Yes | 77 (67.5) | 37 (32.5) | 2.07 (1.59 to 2.71) | 0.68 (0.4 to 1.14) |
| No | 186 (28.8) | 460 (71.2) | 1 | 1 | |
| APGAR score at first minute | 0–3 | 133 (33.9) | 259 (66.1) | 1.79 (1.21 to 2.66) | 1.18 (0.78 to 1.78) |
| 4–6 | 109 (34.1) | 211 (65.9) | 0.47 (0.28 to 0.78) | 0.51 (0.29 to 1.87) | |
| ≥7 | 21 (43.8) | 27 (56.2) | 1 | 1 | |
| Hypothermia | No | 49 (19.1) | 207 (80.9) | 1 | 1 |
| Yes | 214 (42.5) | 290 (57.5) | 2.28 (1.67 to 3.1) | 1.56 (1.12 to 2.17)* | |
| Blood sugar | Hypoglycaemic | 136 (70.1) | 58 (29.9) | 3.08 (2.42 to 3.93) | 2.23 (1.91 to 2.55) |
| Euglycemic | 127 (22.4) | 439 (77.6) | 1 | 1 | |
| MAS | No | 113 (19.2) | 475 (80.8) | 1 | 1 |
| Yes | 150 (87.2) | 22 (12.8) | 4.96 (3.88 to 6.34) | 3.02 (2.23 to 4.08) | |
| Obstructed labour | No | 140 (22.4) | 486 (77.6) | 1 | 1 |
| Yes | 123 (91.8) | 11 (8.2) | 3.62(2.84 to 4.61) | 1.4 (1.02 to 1.91)* | |
1-reference category.
*p<0.05.
AHR, adjusted HR; ANC, antenatal care; APGAR, appearance, pulse, grimace, activity and respiration; CHR, crude HR; MAS, meconium aspiration syndrome; NICUs, neonatal intensive care units .
Discussion
In resource-constrained countries, including Ethiopia, the mortality rate of newborns remains unacceptably high. A WHO report identifies preterm birth and birth asphyxia as the primary culprits behind most newborn deaths. Encouragingly, Ethiopia witnessed a decline in neonatal mortality from 39 per 1000 live births in 2005 to 29 per 1000 in 2016. However, this progress was short-lived, as the rate rose again to 33 per 1000 births in 2019. In this study, attempts have been made to assess the incidence and predictors of mortality among neonates admitted with birth asphyxia, and results revealed that the overall cumulative incidence of mortality among asphyxiated newborns was 34.6% (95% CI 31.3% to 38.1%). Comparable findings were reported from studies conducted in Dessie Comprehensive Specialised Hospital, Northeast Ethiopia, 32%.15 This is higher than two studies conducted in Ethiopia showing an incidence of 22.5%19 and 31%20 at Jimma Medical Center and Debre Markos Compressive Hospital, respectively. This result is also higher than the findings of research undertaken in other African nations, such as Nigeria, where the incidence was 18%21 and 27,22 and Tanzania, where it was 23%.23 However, it is lower than studies conducted in Ethiopia17 and India13 showing an incidence rate of 42.29% and 40.6%, respectively. This may be the result of differences in hospital environments and resources, improvements in hospital healthcare capabilities, management procedures and study design. It might also be associated with differences in thermal control in the delivery room and NICU and resuscitation skills among healthcare providers.
Khat use during pregnancy has been linked to negative perinatal and maternal outcomes such as low birth weight, congenital defects, early rupture of membranes, perinatal death and lower APGAR scores.24 25 These problems can have an indirect impact on newborn mortality. This study also showed that asphyxiated newborns whose mothers chewed chats had a 2.21-fold increased risk of mortality. This study finding is consistent with the study conducted in pregnant women attending ANC at the AL-Gamhouri Teaching Hospital in Taiz, Republic of Yemen.26
Studies have shown that home delivery is associated with higher neonatal mortality rates than hospital delivery, particularly in low-income and middle-income countries.25 This study also revealed that the risk of death was 1.45 times higher for asphyxiated newborn whose mothers gave birth at home. This implies improving access to healthcare facilities for deliveries, as well as promoting essential newborn care and postnatal care, could potentially help lower neonatal mortality rates.
Proper ANC can contribute to lowering the high mortality rate linked to birth asphyxia.27 28 Similarly, this study showed that the risk of death was 1.44 times higher among asphyxiated neonates whose mothers did not have ANC follow-up. This is due to the fact that ANC provides a framework for critical healthcare such as disease screening, prevention and management of pregnancy-related problems. This improves pregnant women’s health and prevents foetal problems, including perinatal asphyxia.29 30
Numerous studies have shown that neonatal hypothermia increases the risk of newborn mortality.31 32 Asphyxiated neonates that developed hypothermia had a 1.56 times higher risk of mortality. This is because hypothermia increases the risk of hypoglycaemia, metabolic acidosis, hypoxia, chronic lung disease, coagulation defects, intraventricular haemorrhage, sepsis, dehydration, fluid and electrolyte imbalance, and hypotension.27
Hypoglycaemia can have negative effects on infants with perinatal asphyxia.33 The risk of death was 2.23 times higher among neonates with hypoglycaemia in this study too. This is because hypoglycaemia can cause brain injury and worse neurodevelopmental outcomes in infants with HIE.34
Obstructed labour is one of the five major causes of maternal mortality and morbidity in developing countries, accounting for 19.1% of maternal deaths in Ethiopia.35 This study also highlighted that the risk of mortality was 1.4 times higher among asphyxiated neonates whose mothers developed obstructed labour during delivery. The extended interruption of the fetoplacental circulation may be a possible explanation.
Limitation of the study
Some sociodemographic and clinical characteristics of mothers and neonates were overlooked due to the nature of the study design. Likewise, long-term consequences among survivors were not addressed, and this conclusion cannot be extrapolated to the broader population.
Conclusion
The magnitude of neonatal mortality among asphyxiated neonates in the study area was found to be high. Chewing khat, place of delivery, ANC follow-up, hypothermia, hypoglycaemia and obstructed labour were found to be the significant predictors of neonatal mortality among asphyxiated neonates. As a result, healthcare practitioners and concerned stakeholders should take these factors into account in order to reduce the risks of birth asphyxia and neonatal mortality associated with it.
Supplementary Material
Acknowledgments
We are grateful to the staff members of the NICU and the card rooms of the included hospitals for their cooperation and provision of important information. Also, we would like to extend our special thanks to both data collectors and supervisors.
Footnotes
Contributors: GGB and EYR developed the proposal, analysis and write up of the results and discussion. DNG and GMG reviewed the manuscript for critical input, supervised all data analysis, manuscript writing and provided critical input to the manuscript. All other authors critically revised the manuscript and approved the final version. GGB accepts full responsibilities for the work or the conduct of study, had access to the data and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Full data for this research are available through the first author on request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and the research review committee of the College of Medicine and Health Sciences of Ambo University granted ethical approval with reference number AURH/M197/6/5/2015. Obtaining consent from the study participants was not possible as it is a secondary data collection.
References
- 1. World Health Organization . Newborn mortality fact sheet. 2022. Available: https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021
- 2. Geme JWS. Nelson textbook of pediatrics. Elsevier, 2020. [Google Scholar]
- 3. Weiner GM, Hooper SB, Davis PG, et al. Respiratory and cardiovascular support in the delivery room. The Newborn Lung: Elsevier, 2019:173–95. [Google Scholar]
- 4. Grady SC, Frake AN, Zhang Q, et al. Neonatal mortality in East Africa and West Africa: a geographic analysis of district-level demographic and health survey data. Geospat Health 2017;12:501. 10.4081/gh.2017.501 [DOI] [PubMed] [Google Scholar]
- 5. Mekonnen W, Assefa N, Asnake W, et al. Under five causes of death in Ethiopia between 1990 and 2016: systematic review with meta-analysis. Ethiopian Journal of Health Development 2020;34. [Google Scholar]
- 6. Manandhar M, Hawkes S, Buse K, et al. Gender, health and the 2030 agenda for sustainable development. Bull World Health Organ 2018;96:644–53. 10.2471/BLT.18.211607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. (FMoH) FMoH . Health sector transformation plan II (HSTP II); 2020/21-2024/25. 2021. [Google Scholar]
- 8. González de Dios J, Moya Benavent M, Izura Azanza V, et al. Electrophysiological studies in the follow-up of children with perinatal asphyxia history. An Esp Pediatr 1997;46:597–602. [PubMed] [Google Scholar]
- 9. Mendler MR, Mendler I, Hassan MA, et al. Predictive value of Thompson-score for long-term neurological and cognitive outcome in term newborns with perinatal asphyxia and hypoxic-ischemic encephalopathy undergoing controlled hypothermia treatment. Neonatology 2018;114:341–7. 10.1159/000490721 [DOI] [PubMed] [Google Scholar]
- 10. Efstathiou N, Theodoridis G, Sarafidis K. Understanding neonatal hypoxic-ischemic encephalopathy with metabolomics. Hippokratia 2017;21:115–23. [PMC free article] [PubMed] [Google Scholar]
- 11. Bouiller J-P, Dreyfus M, Mortamet G, et al. Intrapartum asphyxia: risk factors and short-term consequences. J Gynecol Obstet Biol Reprod (Paris) 2016;45:626–32. 10.1016/j.jgyn.2015.06.022 [DOI] [PubMed] [Google Scholar]
- 12. Bruckmann EK, Velaphi S. Intrapartum asphyxia and hypoxic ischaemic encephalopathy in a public hospital: incidence and predictors of poor outcome. S Afr Med J 2015;105:298–303. 10.7196/samj.9140 [DOI] [PubMed] [Google Scholar]
- 13. Meshram RM, Bokade CM. Risk factors for mortality in birth asphyxia of outborn neonates: a prospective observational study. Sri Lanka J Child Health 2019;48:26. 10.4038/sljch.v48i1.8648 [DOI] [Google Scholar]
- 14. Lee ACC, Mullany LC, Tielsch JM, et al. Risk factors for neonatal mortality due to birth asphyxia in Southern Nepal: a prospective, community-based cohort study. Pediatrics 2008;121:e1381–90. 10.1542/peds.2007-1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yitayew YA, Yalew ZM. Survival status and predictors of mortality among asphyxiated neonates admitted to the NICU of Dessie comprehensive specialized hospital. PLoS One 2022;17:e0279451. 10.1371/journal.pone.0279451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tolossa T, Wakuma B, Mengist B, et al. Survival status and predictors of neonatal mortality among neonates admitted to neonatal intensive care unit (NICU) of Wollega University referral hospital (WURH) and Nekemte specialized hospital, Western Ethiopia: a prospective cohort study. PLoS One 2022;17:e0268744. 10.1371/journal.pone.0268744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ketema DB, Aragaw FM, Wagnew F, et al. Birth asphyxia related mortality in Northwest Ethiopia: a multi-centre cohort study. PLoS One 2023;18:e0281656. 10.1371/journal.pone.0281656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Getaneh FB, Sebsbie G, Adimasu M, et al. Survival and predictors of asphyxia among neonates admitted in neonatal intensive care units of public hospitals of Addis Ababa, Ethiopia, 2021: a retrospective follow-up study. BMC Pediatr 2022;22:262. 10.1186/s12887-022-03238-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kajela L, Berhanu S, Kune G, et al. Time to death and its predictors among asphyxiated neonates admitted to Jimma University medical center, Ethiopia: a retrospective cohort study. In Review [Preprint] 2023. 10.21203/rs.3.rs-2416790/v1 [DOI]
- 20. Shibabaw AT, Belay GM, Desta BK, et al. Incidence and predictors of mortality among neonates with perinatal asphyxia, Northwest Ethiopia, 2021: an institution based retrospective cohort study. In Review [Preprint] 2021. 10.21203/rs.3.rs-1013476/v1 [DOI]
- 21. Ekwochi U, Asinobi NI, Osuorah CD, et al. Incidence and predictors of mortality among newborns with perinatal asphyxia: A 4-year prospective study of newborns delivered in health care facilities in Enugu, South-East Nigeria. Clin Med Insights Pediatr 2017;11:1179556517746646. 10.1177/1179556517746646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Adebami OJ. Maternal and fetal determinants of mortality in babies with birth asphyxia at Osogbo, Southwestern Nigeria. Glo Adv Res J Med Med Sci 2015;4:270–6. [Google Scholar]
- 23. Cavallin F, Menga A, Brasili L, et al. Factors associated with mortality among asphyxiated newborns in a low-resource setting. J Matern Fetal Neonatal Med 2022;35:1178–83. 10.1080/14767058.2020.1743670 [DOI] [PubMed] [Google Scholar]
- 24. Yelamali B, Panigatti P, Pol R, et al. Outcome of newborn with birth asphyxia in tertiary care hospital-a retrospective study. Medica Innovatica 2014;3:59–64. [Google Scholar]
- 25. Yitayih Y, Vanderplasschen W, Vandewalle S, et al. The effects of Khat use during pregnancy on perinatal and maternal outcomes: a meta-analysis. Arch Womens Ment Health 2023;26:11–27. 10.1007/s00737-023-01293-5 [DOI] [PubMed] [Google Scholar]
- 26. Abdel-Aleem MA, Department of Obstetrics and Gynecology, Assiut University, Egypt, Department of Obstetrics and Gynecology, Assiut University, Egypt . Khat chewing during pregnancy: an insight on an ancient problem. Impact of chewing Khat on maternal and fetal outcome among Yemeni pregnant women. JGNB 2015;1:1–4. 10.15436/2380-5595.15.004 [DOI] [Google Scholar]
- 27. Nauman Kiyani A, Khushdil A, Ehsan A. Perinatal factors leading to birth asphyxia among term newborns in a tertiary care hospital. Iran J Pediatr 2014;24:637–42. [PMC free article] [PubMed] [Google Scholar]
- 28. Mamo SA, Teshome GS, Tesfaye T, et al. Perinatal asphyxia and associated factors among neonates admitted to a specialized public hospital in South central Ethiopia: a retrospective cross-sectional study. PLoS One 2022;17:e0262619. 10.1371/journal.pone.0262619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wondemagegn AT, Alebel A, Tesema C, et al. The effect of Antenatal care follow-up on neonatal health outcomes: a systematic review and meta-analysis. Public Health Rev 2018;39:33. 10.1186/s40985-018-0110-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. World Health Organization . WHO recommendations on antenatal care for a positive pregnancy experience. 2016. [PubMed] [Google Scholar]
- 31. Ajaari J, Masanja H, Weiner R, et al. Impact of place of delivery on neonatal mortality in rural Tanzania. Int J MCH AIDS 2012;1:49–59. 10.21106/ijma.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Das U, Chaplot B, Azamathulla HM. The role of place of delivery in preventing neonatal and infant mortality rate in India. Geographies 2021;1:47–62. 10.3390/geographies1010004 [DOI] [Google Scholar]
- 33. Parmentier CEJ, de Vries LS, van der Aa NE, et al. Hypoglycemia in infants with hypoxic-ischemic encephalopathy is associated with additional brain injury and worse neurodevelopmental outcome. J Pediatr 2022;245:30–8. 10.1016/j.jpeds.2022.01.051 [DOI] [PubMed] [Google Scholar]
- 34. De Angelis LC, Brigati G, Polleri G, et al. Neonatal hypoglycemia and brain vulnerability. Front Endocrinol (Lausanne) 2021;12:634305. 10.3389/fendo.2021.634305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yeshitila YG, Daniel B, Desta M, et al. Obstructed labor and its effect on adverse maternal and fetal outcomes in Ethiopia: a systematic review and meta-analysis. PLoS One 2022;17:e0275400. 10.1371/journal.pone.0275400 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2023-002403supp001.pdf (33.1KB, pdf)
Data Availability Statement
Data are available on reasonable request. Full data for this research are available through the first author on request.


