Abstract
Background
This study aimed at documenting the levels of stress, depression, anxiety and participation in care among mothers versus fathers of newborns hospitalised in a third-level neonatal intensive care unit (NICU) in Northern Italy.
Methods
Parental stress, depression and anxiety were assessed by the Parental Stressor Scale in NICU (PSS:NICU), the Edinburgh Postnatal Depression Scale (EPDS) and the State-Trait Anxiety Inventory (STAI). Participation in care was evaluated with the Index of Parental Participation. Differences between mothers and fathers were assessed with the Mood’s median test and z-test, respectively for continuous and discrete variables. Multivariate analyses controlling for potential confounders were performed to confirm gender differences.
Results
191 parents (112 mothers and 79 fathers) were enrolled. Mothers reported significantly higher median scores for stress (2.9 vs 2.2, p<0.001) and trait anxiety (37 vs 32, p=0.004) and higher depression rates (EPDS ≥12: 43.8% vs 19.0%, p<0.001). ‘High stress’ (PSS:NICU ≥3) was reported by 45.5% of mothers compared with 24.1% of fathers (p=0.004). The frequency of the three conditions simultaneously was significantly higher among mothers (20.0% vs 3.8%, p=0.016), with the vast majority of mothers (76.0%) suffering from at least one condition compared with less than half of fathers (45.3%, p<0.001). Participation in care was more frequent in mothers (median score: 19 vs 15, p<0.001), with the exception of activities related to advocacy (median 5 vs 4, p=0.053). In a multivariate analysis, gender differences in mental health outcomes did not change.
Conclusions
Routine screening of mental distress among parents of infants in NICU is warranted, and gender differences need to be acknowledged in order to deliver tailored support and to promote collaboration with the family of vulnerable newborns. Knowledge and skills on how to prevent and cope with mental distress of parents should be part of the core curriculum of staff working in NICU.
Keywords: neonatology, caregivers
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Having a baby hospitalised in a neonatal intensive care unit (NICU) is a distressing experience for parents. Most studies on NICU parental mental health focused on mothers. Little is known on the level of parents’ participation in newborn care in most NICU settings.
WHAT THIS STUDY ADDS
In our study setting, mothers were more likely to suffer from stress, depression and anxiety, with the vast majority of them (76.0%) suffering from at least one condition compared with less than half (45.3%) of fathers. Mothers had a significantly higher participation in care than fathers. These differences were not explained by neonatal conditions.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Both mothers and fathers of infants in NICU can be advantaged by being routinely screened for mental distress. Awareness of gender differences in their mental distress is fundamental for NICU staff in delivering more tailored support.
Introduction
Having a baby hospitalised in a neonatal intensive care unit (NICU) is a distressing and traumatic experience for parents.1–6 A growing body of literature shows that, compared with parents of well babies, parents of infants hospitalised in the NICU are at higher risk to suffer from several mood and mental disorders, ranging from post-traumatic stress disorder, acute-stress disorder, depression and anxiety.1–6 When parents in the NICU are distressed or depressed, their interactions with their infants may be less sensitive and attuned to their infant’s needs. This in turn may interfere with the social, emotional, cognitive and physical development of these already vulnerable infants.5
However, several gaps exist on the current evidence on the mental health and well-being of parents of infants hospitalised in the NICU. For a long time, most of the studies on psychological indicators of parents of newborns in NICU focused exclusively on mothers.2 7 It is only in recent years that a few authors raised attention to the essential role of fathers in the NICU and to their specific needs.8–10 Studies comparing mental health and well-being of mothers versus fathers while assessing multiple indicators are still limited.3 4 11–13 In general, in the existing studies which explored this topic, NICU mothers were reported to be more stressed than fathers,4 11–13 although this difference was not always consistent.3
Awareness of parental psychological distress is a first essential step in order to promote parental well-being. A routine screening of mood and anxiety disorders for parents in the NICU has been proposed by several authors.4 7 8 14 15 Yet this is not implemented in most neonatal units, limiting staff awareness on the problem as well as actions to contain such distress. Gender differences need to be acknowledged in order to deliver tailored support for fathers and mothers, and to promote collaboration with the family of vulnerable newborns.8
In parallel, evidence showed that family-centred care and support to parents’ participation in newborn care can be effective not only to promote parental well-being but also to help NICU hospitalised babies to better thrive and develop.16–18 However, little is known on the level of parents’ participation in newborn care in most NICU settings.
Given these gaps in the literature, our study aimed at comparing the levels of stress, anxiety, depression and participation in care among mothers and fathers of infants in the NICU of an Italian tertiary hospital.
Methods
Study design and setting
This is a cross-sectional study, and it is reported according to the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) Statement.19 The STROBE Checklist is provided as online supplemental table 1.
bmjpo-2023-002429supp001.pdf (285KB, pdf)
The study was part of the baseline assessment of an ongoing multicentre intervention project called ‘Empowering Parents in NICU’ (EPiNICU), aiming at increasing parental participation in NICU in different settings, including Italy (as a model for a high-income country), Brazil (upper middle income) and Tanzania (lower middle income).
The study was conducted in the NICU of the Institute for Maternal and Child Health IRCSS ‘Burlo Garofolo’, a referral maternal and child hospital and research centre in the North-East of Italy. This is an open bay NICU with 24 cots of which 10 are in the intensive care unit, 12 in the semi-intensive care unit and 2 in an isolated negative-pressure room. It handles an average of 260 NICU admissions/year. A total of 9 neonatologists, 24 nurses, 2 psychologists were in service during the study period. Since the 1980s, the NICU has been a 24/7 open ward for both parents. During the COVID-19 pandemic, however, some visiting restrictions to parents were applied though these were implemented together with other organisational changes in order to ensure parents’ prolonged presence and psychological support as detailed elsewhere.20
Study participants
We enrolled prospectively mothers and fathers of newborns admitted to NICU or semi-intensive care for at least 48 hours, with an age of at least 18 years and fluent in Italian. Parents with a newborn bereavement, or a previous diagnosed psychological/mental disorder or refusing consent were excluded. All participants provided a written consent before answering to the study questionnaires.
Patient involvement
The data presented in this paper are part of a baseline assessment that parents underwent, therefore patients were not involved in the design, conduct, reporting or dissemination plans of our research. Patient participation was encouraged at later stages of the EPiNICU project. The parent association ‘Scricciolo’ was actively involved in identifying interventions to improve parental empowerment in the NICU.
Data collection and categorisation
The study objectives and methods were introduced to parents either by a neonatologist or a NICU psychologist with a median of 4.5 (IQR 0–10) days before discharge and after a median of 9 (IQR 5.3–20) days from admission. In particular, with a median of 1 (IQR 0–2) day before discharge for newborns who were hospitalised for a period ≤14 days, and a median of 10 (IQR 5–17) days before discharge for newborns who were hospitalised for a period >14 days (note that the range of duration of hospitalisation in this group was 15–150 days). Five self-administrated questionnaires were used, to collect information on parental stress, depression, anxiety, participation in newborn care and parents’ characteristics. Questionnaires for parental stress, depression and anxiety are screening tools for these conditions. Parental stress, which was predefined as the study primary outcome, was measured with the Parental Stressor Scale in NICU (PSS:NICU),21 validated in Italy22 and including 26 statements divided in three sections exploring stress due to Sights and Sounds (6 items), to Infant Behaviour and Appearance (13 items) and to Parental Role Alteration (7 items). Answers for each question were on a Likert scale from 1 (‘no stress’) to 5 (‘extremely stressful’). Total PSS:NICU scores were calculated according to Miles21 using the stress occurrence level (SOL) calculated including only experienced items and focused on parents and real lived experiences.21 In the absence of a clear indication in the existing literature, we defined ‘high stress’ as a median SOL score≥3.
Parental depression was screened with the Edinburgh Postnatal Depression Scale (EPDS), which has been previously validated in Italy.23 The scale includes 10 questions with four possible answers each, and a total score ranging from 0 to 30, exploring the emotional state during the last 7 days. The Italian cut-off value for suggesting a clinical depression is a score ≥12 both for women and men.23 24
Anxiety was measured with the State-Trait Anxiety Inventory (STAI), which include two different scales assessing frequency of feelings in general: (1) the State Anxiety Scale (STAI-Y1) evaluating the current state of anxiety; (2) the Trait Anxiety Scale (STAI-Y2) evaluating anxiety proneness.25 Each scale includes 20 items with a score ranging each from 1 (‘almost never’) to 4 (‘almost always’), thus for each scale, the total score can range from 20 to 80. According to the literature, scores over 40 are considered indicative of ‘any anxiety’, scores in between 41 and 50 indicating ‘mild anxiety’, 51–60 ‘moderate anxiety’ and >60 ‘severe anxiety’.26 27 This questionnaire was used in a subsample of patients (N=130 of a total of 191).
Parental participation was measured with the Index of Parental Participation (IPP), originally developed for children, and slightly modified to describe activities related to newborn care in the last 24 hours. The adaptation was approved and back translated by Dr Melnyk, the author of the instrument.28 The IPP includes 30 dichotomous (yes/no) items, divided in 4 sections: activities related to Daily Living (6 items); Providing Comfort (7 items); Advocating for newborn health (7 items); Technical Tasks (10 items). The total score ranges from 0 to 30, with higher scores indicating higher parental participation in care. The IPP questionnaire is included as online supplemental table 2.
A structured form questionnaire was used to collect key parental characteristics, while data on newborns were collected from the clinical files.
Data were collected before and during the COVID-19 pandemic (from November 2019 to December 2020) based on a preliminary study on a subsample of the current sample (N=151), showing that parental stress, depression and participation in care did not change significantly during the COVID-19 pandemic compared with the prepandemic period,18 and data were not further analysed except for pandemic phases. In the present paper, we report new data compared with the previous publication,20 by comparing study outcomes in mothers versus fathers, and by analysing a larger sample of parents.
Data analysis
A sample of 154 parents (77 for each subgroup) was calculated based on an expected difference of 0.3 points in the PSS:NICU (SOL) total score and an SD of 0.5, using a Wilcoxon-Mann-Whitney test with 95% confidence and a power of 95%.
First, a descriptive analysis of parents and newborn characteristics was conducted. Summary statistics were presented as absolute frequencies and percentages, and medians and IQRs were used for continuous non-normally distributed data.
To evaluate parents’ mental well-being, we tested stress, depression and anxiety scores between mothers and fathers. The four sections of IPP and all items were tested between groups to assess differences in mothers and fathers’ participation in care.
For all scores, the differences between mothers and fathers were analysed by considering the medians and the percentages of observations over the cut-offs presented in the Data Collection section. The median test (also known as Mood’s median test) and the two proportions Z-test were used, respectively.
We also analysed the concurrent presence of stress, depression and anxiety on the subgroup of parents who contributed to the study providing data for all the related scores. For this analysis, we included only those parents with all three scores for mental distress (N=130, 75 mothers and 55 fathers) and we used the STAI state score (STAI-Y1) for anxiety, defining ‘any state anxiety’ by a score>40.
To explore whether differences between mothers and fathers in mental distress outcomes and participation in care did not depend on neonatal variables indicating clinical severity, we first investigated, through a two-sample t-test, the differences between the distributions of PSS:NICU, SOL, EPDS, STAI-Y1, IPP dividing the sample by relevant newborn characteristics. Specifically, we considered: Respiratory Distress Syndrome, any respiratory distress, intubation, outborn, gestational age, birth weight, length of stay, major complications. Given the limited sample size of newborn with some conditions of interest—sepsis, surgery, neurological event, major birth trauma and malformation—to ensure statistical power, we created a composite variable called major complications defined by the presence of any of these conditions.
Additionally, to confirm potential gender differences, we conducted univariate and multivariate logistic regression, considering the presence of mental health conditions under analysis (ie, high stress, clinical depression, any anxiety) as binary outcome variables and parental role as well as newborn characteristics (twin, newborn sex) and the clinical characteristics listed above as explanatory variables. For these analyses, for the dependent variables, we used the cut-offs suggested by literature and used also for the descriptive analyses. We categorised the independent continuous variables according to their distribution. Potential confounders and parental role were included in the multivariate models. Frequencies, ORs and adjusted ORs (adjOR) were calculated, with 95% CIs and p values of significance.
Statistical analyses were performed using R V.4.2.2. All tests performed were two-tailed and a p value of less than 0.05 was considered statistically significant.
Results
Sample characteristics
Of the 272 newborns admitted to our Neonatal Unit during the study period, 188 met the inclusion criteria. Among these, 65 (34%) were not enrolled, with only very few refusals to participate (online supplemental figure 1). Overall, we included 123 newborns and 191 parents (112 mothers, 79 fathers).
Characteristics of parents are summarised in table 1, with the only statistical differences between groups being the working status, despite being high in both mothers (87%) and fathers (97%, p<0.0001) and the median age of parents with mothers being younger than fathers (36 vs 39 years, p=0.003).
Table 1.
Characteristics of mothers and fathers
| Overall N=191 |
Mothers N=112 |
Fathers N=79 |
P value | ||||
| N | % | N | % | N | % | ||
| Age, median (IQR) | 37 | (34, 41) | 36 | (32, 39) | 39 | (36, 43.5) | 0.003 |
| Education* | |||||||
| Primary education | 24 | 12.57 | 10 | 8.93 | 14 | 17.72 | 0.113 |
| Lower secondary education | 80 | 41.88 | 45 | 40.18 | 35 | 44.30 | 0.674 |
| Upper secondary education | 4 | 2.09 | 4 | 3.57 | 0 | 0 | 0.236 |
| Bachelor’s or more | 81 | 42.41 | 52 | 46.43 | 29 | 36.71 | 0.234 |
| Missing | 2 | 1.05 | 1 | 0.89 | 1 | 1.27 | -† |
| Working status | |||||||
| Working | 167 | 87.43 | 90 | 80.36 | 77 | 97.47 | 0.001 |
| Unemployed | 20 | 10.47 | 19 | 16.96 | 1 | 1.27 | 0.001 |
| Missing | 4 | 2.09 | 3 | 2.68 | 1 | 1.27 | -† |
| Marital status | |||||||
| Married | 186 | 97.38 | 108 | 96.43 | 78 | 98.73 | 0.601 |
| Unmarried | 5 | 2.62 | 4 | 3.57 | 1 | 1.27 | -† |
| Parity (only women) | |||||||
| 1 | – | – | 63 | 56.25 | – | – | – |
| 2 | – | – | 28 | 25 | – | – | – |
| >2 | – | – | 20 | 17.86 | – | – | – |
| Missing | – | – | 1 | 0.89 | – | – | – |
*ISCED (International Standard Classification of Education) classification: primary education—ISCED 1; lower secondary education—ISCED 2; upper secondary education—ISCED 3; bachelor’s or equivalent—ISCED 6.38
†Impossible to run a test because there are too few observations.
Characteristics of newborns are detailed in table 2. Overall, the newborn population was heterogeneous in all clinical characteristics. About half of them were admitted to the intensive unit while the other half to the semi-intensive one.
Table 2.
Newborn characteristics
| N | % | |
| Sex | ||
| Female | 63 | 51.22 |
| Male | 60 | 48.78 |
| Gestational age, weeks | ||
| ≤27 | 6 | 4.88 |
| 28–33 | 29 | 23.58 |
| 34–36 | 41 | 33.33 |
| 37–41 | 47 | 38.21 |
| Birth weight | ||
| <1000 g | 7 | 5.69 |
| 1000–1499 g | 13 | 10.57 |
| 1500–2499 g | 47 | 38.21 |
| ≥2500 g | 56 | 45.53 |
| Outborn | 24 | 19.51 |
| Apgar at 5 min<7 | 3 | 2.44 |
| Ventilation at birth | 28 | 22.76 |
| Intubation | 24 | 19.51 |
| Respiratory distress syndrome (RDS) | 21 | 17.07 |
| Any respiratory distress | 58 | 47.15 |
| Sepsis | 16 | 13.01 |
| Surgery | 12 | 9.76 |
| Neurological event * | 5 | 4.07 |
| Major birth trauma † | 1 | 0.81 |
| Major malformation ‡ | 8 | 6.50 |
| Admission to | ||
| Newborn intensive care unit§ | 60 | 48.78 |
| Semi-intensive care unit¶ | 63 | 51.22 |
| Median | IQR | |
| Length of stay—days | 15 | 8.5, 26 |
Among the 123 newborns under analysis, 23 are twins.
*Defined as convulsions, intraventricular haemorrhage, periventricular leukomalacia.
†Defined as fractured clavicle or humerus or fracture at any other site; brachial plexus paralysis and subgaleal haematoma.
‡Defined for head and craniofacial structures: anencephaly, encephalocele, holoprosencephaly, hydrocephaly, microphthalmia, anophthalmia, colobomas, microtia, cleft lip, cleft palate, severe micrognathia, macro and macroglossia. Neck: cystic hygroma. Chest: pectus excavatum, absent or hypoplastic clavicles. Back: meningomyelocele, spina bifida. Abdomen: omphalocele, gastroschisis. Genitalia: ambiguous genitalia. Extremities: absent or limb deficiencies, polydactyly, complete syndactyly, polysyndactyly, absent digits, ectrodactyly. Cardiovascular and great vessels: tetralogy of Fallot, truncus arteriosus, hypoplastic left heart, ventricular or atrial septal defect, transposition of the great vessels, interrupted aortic arch type B, total anomaly of pulmonary venous return, hypoplasia or coarctation of the aorta.
§Criteria for the admission to the neonatal intensive-care area of our III level unit include to be an ELBW (extremely low birth weight) or a VLBW (very low birth weight), or to be a newborn with surgical, metabolic or any other condition which require either a ventilatory, a cardiocirculatory support, or a central catheter or hypothermia.
¶Criteria for the admission in the semi-intensive area of our NICU include infants weighing more than 1500 g and being stable either with no need for respiratory support or with only nasal high flow therapy, and with a peripheral access and/or a naso-gastric tube for enteral nutrition.
NICU, neonatal intensive care unit.
Stress, depression and anxiety
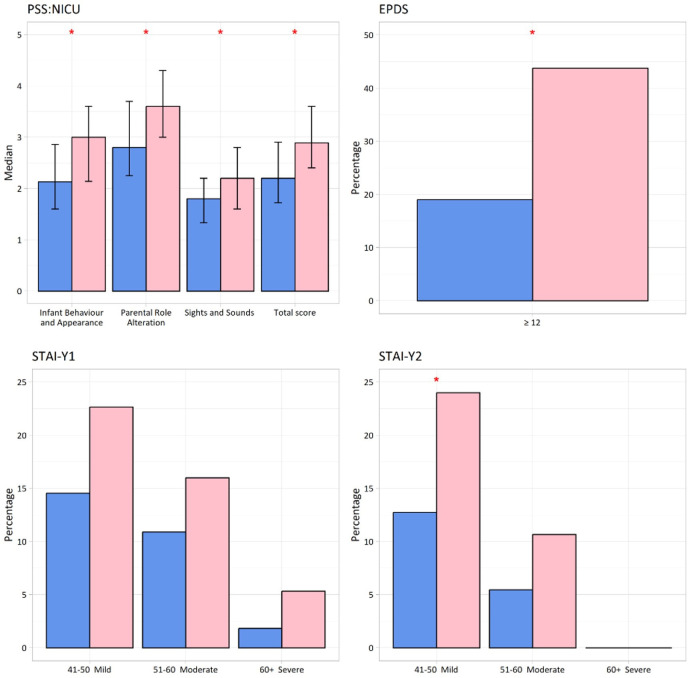
As shown by figure 1 and online supplemental tables 3 and 4, mothers compared with fathers showed significantly higher median scores for stress and depression, and higher frequency of both state and trait anxiety, though a statistically significant difference was identified only for mild trait anxiety.
Figure 1.
Stress (median SOL scores), depression (EPDS≥12) and anxiety levels (mild, moderate, severe) among mothers and fathers. Sample size=191 (130 for STAI). Red asterisk=significant difference between mothers and fathers (p<0.05). EPDS, Edinburgh Postnatal Depression Scale; PSS:NICU, Parental Stressor Scale in NICU; SOL, stress occurrence level; STAI-Y1, State Anxiety Scale; STAI-Y2, Trait Anxiety Scale.
Specifically, PSS:NICU median scores were 2.9 (IQR 2.4–3.6) in mothers compared with 2.2 (IQR 1.7–2.9) in fathers (p<0.001), with all subscores for stress being significantly higher in mothers. Parental role alteration was the highest source of stress for both mothers (3.6, IQR 3.0–4.3) and fathers (2.8, IQR 2.3–3.7) (online supplemental table 3). ‘High stress’ was present in 45.54% of mothers compared with 24.05% of fathers (p=0.004).
Median EPDS scores were 10 (IQR 6.5–15) in mothers compared with 7 (IQR 3–10) in fathers (p<0.001) (online supplemental table 3). Almost half of mothers had an EPDS suggestive of clinical depression, compared with one father out of five (respectively, 43.75% vs 18.99%, p<0.001) (online supplemental table 4).
No significant differences between mothers and fathers were found in state anxiety median scores (STAI-Y1), while mothers were more likely to have a higher score for trait anxiety (STAI-Y2) (median score 37 vs 32, p=0.004) (online supplemental table 3).
When analysed by frequency, state and trait anxiety were more frequent among mothers versus fathers though the differences were not statistically significant (44% vs 27.27%, p=0.076; 34.67% vs 18.18%, p=0.061) with mild trait anxiety being significantly more frequent in mothers compared with fathers (24% vs 12.73%, p=0.042) (online supplemental table 4, figure 1).
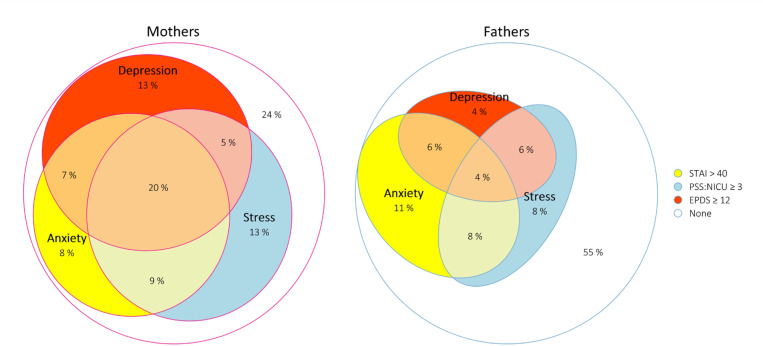
When investigating whether mothers and fathers suffered from more than one condition among stress, depression and anxiety, mothers were suffering from all three conditions more frequently than fathers (20% vs 3.8%, p=0.016), with the vast majority of mothers (76%) suffering from at least one condition compared with less than half of fathers (45.3%, p<0.001). Patterns of overlap among conditions varied from mothers and fathers were relatively similar (figure 2).
Figure 2.
Differences in pattern of overlaps among conditions between mothers and fathers. For anxiety, STAI state score was considered. Sample size=75 (mothers), 55 (fathers). EPDS, Edinburgh Postnatal Depression Scale; PSS:NICU, Parental Stressor Scale in NICU; STAI, State Anxiety Scale-Y1.
Participation in care
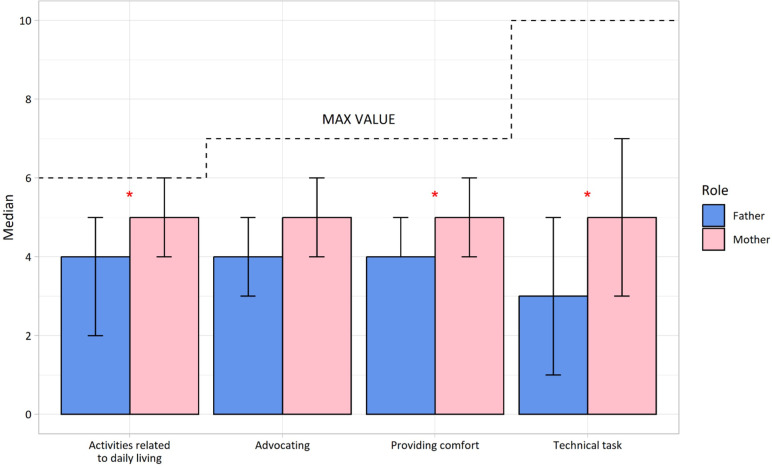
With regard to participation in care, mothers showed significantly higher median subscores in all areas of participation investigated (5 vs 4 for fathers for activities related to daily living and providing comfort, 5 vs 3 for fathers for technical tasks, all p values <0.01) except for activities related to the advocacy for their baby (5 vs 4 for fathers, p=0.053) (figure 3, online supplemental table 3).
Figure 3.
IPP median subscores in mothers and fathers. Red asterisk=significant difference between mothers and fathers (p<0.05). Sample size=191. IPP, Index of Parental Participation.
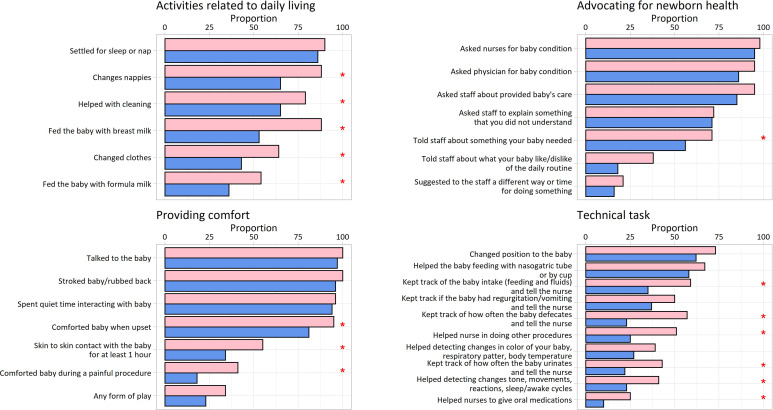
When single IPP items were analysed (figure 4), the only advocacy activity that was reported more frequently among mothers was to have actively told staff what her newborn needed (37.5% mothers vs 17.7% fathers, p=0.005). Mothers were more likely than fathers to comfort their newborns when upset or during painful procedures (94.6% vs 79.7%, p=0.003) and to do skin-to-skin for at least 1 hour (55.4% vs 34.2%, p=0.006).
Figure 4.
Single items in IPP questionnaire in mothers and fathers. Red asterisk=significant difference between mothers and fathers (p<0.05). Sample size=191. IPP, Index of Parental Participation.
Participation in the area of technical tasks showed the lower scores for both mothers and fathers, though it was higher among mothers who helped staff in keeping track of some clinical parameters (42.0% vs 21.5%, p=0.005, for urine and 56.2% vs 22.8%, p<0.001, for faeces) and in helping to give oral medication (25.0% vs 10.1%, p=0.016).
Univariate and multivariate analyses
Checking the differences between the distributions of the scores dividing the sample by relevant newborn characteristics, only four comparisons were statistically significant (online supplemental table 5). We found significantly higher scores for SOL in parents of hospitalised newborns with major complications (medians 2.96, IQR 2.26–3.52, vs 2.52, IQR 1.94–3.13, p=0.024) and for EPDS in parents of babies older than 34 weeks compared with younger babies (medians 10, IQR 6–13, vs 7, IQR 3–10.5, p=0.002). Anxiety was not associated with any neonatal condition. Participation in care was significantly higher for parents both of babies weighing more than 1500 g compared with very low birth weight (18, IQR 15–23, vs 15, IQR 10–21, p=0.013) and outborn compared with inborn babies (20, IQR 18–24, vs 18, IQR 13–21.5, p=0.003).
In the univariate and multivariate analysis, when correcting for potential confounders, gender differences in stress and depression did not change (online supplemental table 6). Mothers were two times more likely to suffer from ‘high stress’ than fathers (adjOR 2.16, 95% CI 1.11 to 4.35, p=0.026), and almost four times more likely to have a positive screening for depression (adjOR 3.89, 95% CI 1.88 to 8.57, p<0.001). We found no significant gender differences in ‘any state anxiety’ and this result was confirmed in the multivariate analysis (adjOR 1.72, 95% CI 0.80 to 3.77, p=0.171).
Discussion
This is one of the few studies exploring more than one mental health indicators in mothers versus fathers of newborns in the NICU, and, to the best of our knowledge, the only study exploring multiple indicators of mental health together with a measure of participation in care.
In the NICU where this study was conducted, we found that self-reported stress, depression symptoms and mild trait anxiety were very frequent, confirming previous studies,1–5 13 and significantly higher in mothers compared with fathers. Gender differences in mental distress did not change when controlling for neonatal characteristics.
In line with our study, a recent systematic review found that in the NICU setting, the pooled prevalence of stress, anxiety and depression is significantly higher among mothers than fathers.13 Overall, our findings suggest that more attention should be given to the mental health of parents of infants hospitalised in the NICU, particularly to mothers, who are more directly involved in newborn care. This includes the need for more studies, to better describe differences in mental health indicators and participation in care among mothers and fathers in different settings and to describe tailored interventions, both in support of parents and staff.
Our study adds on the existing literature, which mainly focused on parental stress, showing that, generally, though not consistently so, mothers and fathers differ in terms of their reactions to having a NICU hospitalised infant.3 4 11 A 2013 metanalysis of 38 studies describing parents of preterm and low birth weight infants found that differences in stress between mothers and fathers were clinically negligible.3 Conversely, in line with our results, an updated 2020 metanalysis of 53 studies focused on parental stress measured by PSS:NICU, found that mothers are significantly more stressed than fathers, with parental role alteration being the greatest source of stress for both NICU mothers and fathers.4 In our setting, we found that this difference was relevant with almost one in two mothers suffering from high stress compared with one in five fathers. These prevalences are in line with Shetty et al systematic review that found in the NICU setting a pooled prevalence of stress of 41% among mothers versus 22% in fathers.13
When looking at depression and anxiety, results of our study showed that both conditions were more frequent in mothers, though significantly so for depression and trait anxiety. These results are to a large extent aligned with previous studies, although again literature is not fully consistent. Garfield et al studied the trajectories in self-rated depression evaluated with EPDS in a Chicago NICU, showing that at admission and at discharge mothers were significantly more likely to be depressed than fathers but, interestingly, while mothers showed a reduction over time in their EPDS scores, fathers essentially remained the same.29 In a study in New Zealand, where parents in the NICU were compared with parents of full-term infants not requiring admission to the NICU, using the Hospital Anxiety and Depression Rating Scale, anxiety and depression scores were higher among mothers than fathers in both groups of parents.30 However, in a prospective study of parents of newborns born less than 30 weeks of gestational age based in an Australian NICU, Pace et al found that fathers had a frequency of clinically significant symptoms of depression and anxiety comparable with those of mothers, and in both populations, these symptoms declined over time with a similar pattern.31 Shetty et al found in a meta-analysis of 40 studies, that pooled prevalence of both depression and anxiety were higher among mothers than fathers.13
While it is plausible that differences among fathers and mothers are to some extent setting specific and, therefore, need to be estimated for each setting, gender differences in psychological distress as well as the role of father in newborn care need to be acknowledged by all NICU staff and taken into account during daily clinical work. Although in our study, fathers experienced less frequently stress, anxiety and depressive symptoms, they were far to be immune from them. It is only in recent years that awareness on paternal psychological suffering in the NICU context has been raised.8–10 Taking care of the psychological needs of fathers appears pivotal, as fathers play an essential role in promoting the early father–baby attachment relationship, in having positive effects on the psychological and somatic development of the newborn, and on the health of the mother and whole family.8–10
Many scientific societies and authors are calling for a routine screening of mood and anxiety disorders for parents in the NICU,4 7 8 14 15 as their psychological suffering may have short-term and long-term negative effects not only on their health but also on the future health of their babies. It is critical to consider both mothers and fathers, and, when appropriate, other caregivers, when implementing these recommendations. Understanding parental emotions and experiences of a NICU hospitalisation together with their coping mechanisms,32 33 taking care of caregivers’ mental health together with the promotion and support of a parent responsive and attuned care are among those fundamental ‘nurturing care’ practices, which are advocated by the WHO and by several paediatric societies, as they actively reduce ‘toxic stress’, buffer adversity and help infants to flourish.34 35
We found limited data to compare our findings on differences in participation in care in the NICU between mothers and fathers. As in our study, in a Canadian NICU, caregiver involvement was higher among mothers than fathers.36 In our setting, this may be due to the fact that a high percentage of fathers in our study population (97%) were employed. However, also a very high percentage of mothers in our study were employed (87%), thus suggesting that family support policies such as parental leave, together with local culture, may actually play a bigger role than employment status itself in affecting who is acting as primary caregiver for the newborn. In Italy, parental leave is different between mothers and fathers, with a recognised paid paternity leave of 10 days.37 This difference is confirmed by our clinical real-life experience as mothers are usually present in our NICU for longer time compared with fathers, giving them more opportunities to actively participate in care of their newborns. However, in the advocacy area, these differences were not so evident, showing similar participation between fathers and mothers. Again, this finding emphasises the key role that fathers play in the NICU. Importantly, since data were self-reported, they may also mirror self-perception of mothers and fathers, who may be another relevant area for further research.
Several limitations of our study need to be acknowledged. First, its cross-sectional nature cannot test any causal relationships among different study variables. However, it gives a valuable picture on differences among mothers’ and fathers’ psychological distress and participation in care. This new evidence is fundamental to start a quality improvement process to better take care of parental mental health and to empower parents in the NICU, as the EPiNICU study aims at. Second, frequency of parental mental distress may have been overestimated as study data were mainly collected during COVID-19 pandemic. However, a previous analysis on a smaller sample of parents across different time periods (pre-pandemic, low and high COVID-19 incidence) showed that prevalence of stress and depression did not change significantly in our setting with COVID-19 compared with the prepandemic period.20 Third, differences in mental distress between mothers and fathers might have been influenced by the clinical severity of their hospitalised newborn. In our study, we could not use a standardised neonatal severity score but when controlling for neonatal characteristics we found that differences between mothers and fathers did not change. Fourth, the intrinsic limitations of the questionnaires need to be taken into account. The collected data are based on self-assessment and not on clinical interviews, hence giving a picture of self-perceptions and of the risks for the conditions rather than representing a clinical diagnosis. The IPP questionnaire focuses on activities in the last 24 hours and does not capture parental satisfaction during participation in newborn care. Nevertheless, these questionnaires are validated and widely used in the existing literature.4 14 Fifth, as anticipated, findings of this study are not directly generalisable to other settings; however, they contribute to fill a gap in evidence and highlight the need to replicate similar studies in different settings.
In conclusion, our study confirmed that in parents of infants hospitalised in the NICU stress, depression and anxiety were very frequent, and significantly more frequent in mothers, though mothers participated in care more than fathers did. Routine screening of mental distress among parents in the NICU is warranted, while capacities of staff to cope with NICU challenging environment, hence effectively supporting parents without risking burn-out, need to be strengthened and be part of NICU staff curriculum. More studies are warranted in order to explore how parental participation in care is associated with parental mental distress in different contexts.
Supplementary Material
Acknowledgments
We would like to thank all collaborators to the EPiNICU Study Group: for Italy: Barbara Albertacci, Prof Egidio Barbi, Dr Stefano Bembich, Dr Livia Bicego, Luisa Bulzis, Dr Domenica Squillaci, Francesca Marrazzo, Dr Silvia Nider, Dr Cristina Tuminelli, Dr Cecilia Vuillard; for Tanzania: Dr Gaetano Azzimonti, Dr Martina Borrellini, Emmanuel Ndile, Dr Giovanni Putoto, Dr Giovanni Torelli; for Brazil: Dr Emanuelle Pessa Valente, Dr Geisy Maria de Souza Lima, Dr Dafne Barcala, Dr Juliana Barradas, Dr Waldemar Brandão Neto, Dr Giselle Paiva, Dr Walkyria Campos, Dr Vivian Farias, Dr Lorena Freitas, Renata Araújo, Núbia Dantas, Maria Eduarda Fraga; for Sri Lanka: Dr Mohamed Rishard, Dr Hemantha Senanayake, Nalin Gamaathige. We thank all parents who took their time to respond to the questionnaires. We thank Dr Bernadette J. Mazurek Melnyk, PhD, APRN-CNP, FAANP, FNAP, FAAN for the authorised modified version of IPP/HC-AA in the NICU setting (Adapted from Dr Melnyk’s instrument). We thank Dr Margaret S. Miles for the authorised Italian version (PSS: NICU version 3.0 (19/01/06)) edited by R. Montirosso and B. Premoli (IRCCS 'E.Medea'—Associazione 'La Nostra Famiglia', Bosisio Parini (LC), Italia). A special thanks to the parent association 'Scricciolo' supporting parents of Burlo Garofolo’s NICU. This work was supported by the Italian Ministry of Health, through the contribution given to the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste—Italy.
Footnotes
Contributors: Conception of the EPINICU study: ML. Conception of the paper: JB, ML, IM, MG. Collection of data: JB, MG, ME, MU, SP. Data entry: MG. Analysis and interpretation of the data: PD, IM, JB, ML. Drafting of the article: JB, ML. Critical revision of the article for important intellectual content and final approval of the article: JB, PD, IM, MG, LT, ME, UM, SP, LT, ML. Guarantor author: JB.
Funding: The study was supported by 'Chiesi Foundation Research Grant 2019 in Neonatology' to our Institute of Research. As per the contract undersigned among parties, 'The Grant does not constitute, directly or indirectly, a fee for services provided or to be provided in favour of the Foundation'.
Competing interests: No, there are no competing interests.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Ethical Committee of Friuli Venezia Giulia Region, Italy (Prot.31633, 22 October 2019). Participants gave informed consent to participate in the study before taking part.
References
- 1. Roque ATF, Lasiuk GC, Radünz V, et al. Scoping review of the mental health of parents of infants in the NICU. J Obstet Gynecol Neonatal Nurs 2017;46:576–87. 10.1016/j.jogn.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 2. Woodward LJ, Bora S, Clark CAC, et al. Very Preterm birth: maternal experiences of the neonatal intensive care environment. J Perinatol 2014;34:555–61. 10.1038/jp.2014.43 Available: MID:24651730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schappin R, Wijnroks L, Uniken Venema MMAT, et al. Rethinking stress in parents of Preterm infants: a meta-analysis. PLoS One 2013;8:e54992. 10.1371/journal.pone.0054992 Available: MID:2340510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Caporali C, Pisoni C, Gasparini L, et al. A global perspective on parental stress in the neonatal intensive care unit: a meta-analytic study. J Perinatol 2020;40:1739–52. 10.1038/s41372-020-00798-6 [DOI] [PubMed] [Google Scholar]
- 5. Johnson Rolfes J, Paulsen M. Protecting the infant-parent relationship: special emphasis on perinatal mood and anxiety disorder screening and treatment in neonatal intensive care unit parents. J Perinatol 2022;42:815–8. 10.1038/s41372-021-01256-7 Available: MID:34711936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McKeown L, Burke K, Cobham VE, et al. The prevalence of PTSD of mothers and fathers of high-risk infants admitted to NICU: A systematic review. Clin Child Fam Psychol Rev 2023;26:33–49. 10.1007/s10567-022-00421-4 [DOI] [PubMed] [Google Scholar]
- 7. Staver MA, Moore TA, Hanna KM. An integrative review of maternal distress during neonatal intensive care hospitalization. Arch Womens Ment Health 2021;24:217–29. 10.1007/s00737-020-01063-7 [DOI] [PubMed] [Google Scholar]
- 8. Baldoni F, Ancora G, Latour JM. Being the father of a Preterm-born child: contemporary research and recommendations for NICU staff. Front Pediatr 2021;9:724992. 10.3389/fped.2021.724992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Merritt L, Maxwell J, Urbanosky C. The needs of NICU fathers in their own words: A qualitative descriptive study. Adv Neonatal Care 2022;22:E94–101. 10.1097/ANC.0000000000000934 [DOI] [PubMed] [Google Scholar]
- 10. Holm KG, Aagaard H, Maastrup R, et al. How to support fathers of Preterm infants in early Parenthood - an integrative review. J Pediatr Nurs 2022;67:e38–47. 10.1016/j.pedn.2022.10.001 [DOI] [PubMed] [Google Scholar]
- 11. Matricardi S, Agostino R, Fedeli C, et al. Mothers are not fathers: differences between parents in the reduction of stress levels after a parental intervention in a NICU. Acta Paediatr 2013;102:8–14. 10.1111/apa.12058 [DOI] [PubMed] [Google Scholar]
- 12. Ionio C, Colombo C, Brazzoduro V, et al. Mothers and fathers in NICU: the impact of Preterm birth on parental distress. Eur J Psychol 2016;12:604–21. 10.5964/ejop.v12i4.1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shetty AP, Halemani K, Issac A, et al. Prevalence of anxiety, depression, and stress among parents of neonates admitted to neonatal intensive care unit: a systematic review and meta-analysis. Clin Exp Pediatr 2024;67:104–15. 10.3345/cep.2023.00486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. ACOG committee opinion No.757: screening for perinatal depression. Obstet Gynecol 2018;132:e208–12. 10.1097/AOG.0000000000002927 [DOI] [PubMed] [Google Scholar]
- 15. Murthy S, Haeusslein L, Bent S, et al. Feasibility of universal screening for postpartum mood and anxiety disorders among Caregivers of infants hospitalized in Nicus: a systematic review. J Perinatol 2021;41:1811–24. 10.1038/s41372-021-01005-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. North K, Whelan R, Folger LV, et al. Family involvement in the routine care of hospitalized Preterm or low birth weight infants: A systematic review and meta-analysis. Pediatrics 2022;150:e2022057092O. 10.1542/peds.2022-057092O [DOI] [PubMed] [Google Scholar]
- 17. Gooding JS, Cooper LG, Blaine AI, et al. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol 2011;35:20–8. 10.1053/j.semperi.2010.10.004 [DOI] [PubMed] [Google Scholar]
- 18. Committee on Hospital Care and Institute For Patient- and Family-Centered Care . Patient- and family-centered care and the Pediatrician’s role. Pediatrics 2012;129:394–404. 10.1542/peds.2011-3084 [DOI] [PubMed] [Google Scholar]
- 19. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bua J, Mariani I, Girardelli M, et al. Parental stress, depression, and participation in care before and during the COVID-19 pandemic: A prospective observational study in an Italian neonatal intensive care unit. Front Pediatr 2021;9:737089. 10.3389/fped.2021.737089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miles MS, Funk SG, Carlson J. Parental stressors scale: neonatal intensive care unit. Nurs Res 1993;42:148–52. [PubMed] [Google Scholar]
- 22. Montirosso R, Provenzi L, Calciolari G, et al. Measuring maternal stress and perceived support in 25 Italian Nicus. Acta Paediatr 2012;101:136–42. 10.1111/j.1651-2227.2011.02440.x [DOI] [PubMed] [Google Scholar]
- 23. Benvenuti P, Ferrara M, Niccolai C, et al. The Edinburgh postnatal depression scale: validation for an Italian sample. J Affect Disord 1999;53:137–41. 10.1016/s0165-0327(98)00102-5 [DOI] [PubMed] [Google Scholar]
- 24. Loscalzo Y, Giannini M, Contena B, et al. The Edinburgh postnatal depression scale for fathers: A contribution to the validation for an Italian sample. Gen Hosp Psychiatry 2015;37:251–6. 10.1016/j.genhosppsych.2015.02.002 [DOI] [PubMed] [Google Scholar]
- 25. Pedrabissi L, Santinello M. Inventario per L’ansia di Stato e di Tratto: Nuova versione Italiana Dello STAI-forma Y [Manual for the State-Trait Anxiety Inventory: New Italian Version of the STAY-Y form. Firenze: Organizzazioni Speciali, 1989. [Google Scholar]
- 26. Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res (Hoboken) 2011;63:S467–72. 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Polloni L, Cavallin F, Lolli E, et al. Psychological wellbeing of parents with infants admitted to the neonatal intensive care unit during SARS-Cov-2 pandemic. Children (Basel) 2021;8:755. 10.3390/children8090755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Melnyk BM. Coping with unplanned childhood hospitalization: effects of informational interventions on mothers and children. Nurs Res 1994;43:50–5. [PubMed] [Google Scholar]
- 29. Garfield CF, Lee YS, Warner-Shifflett L, et al. Maternal and paternal depression symptoms during NICU stay and transition home. Pediatrics 2021;148:e2020042747. 10.1542/peds.2020-042747 [DOI] [PubMed] [Google Scholar]
- 30. Carter JD, Mulder RT, Bartram AF, et al. Infants in a neonatal intensive care unit: parental response. Arch Dis Child Fetal Neonatal Ed 2005;90:F109–13. 10.1136/adc.2003.031641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pace CC, Spittle AJ, Molesworth CM-L, et al. Evolution of depression and anxiety symptoms in parents of very Preterm infants during the newborn period. JAMA Pediatr 2016;170:863–70. 10.1001/jamapediatrics.2016.0810 [DOI] [PubMed] [Google Scholar]
- 32. Loewenstein K, Barroso J, Phillips S. The experiences of parents in the neonatal intensive care unit: an integrative review of qualitative studies within the Transactional model of stress and coping. J Perinat Neonatal Nurs 2019;33:340–9. 10.1097/JPN.0000000000000436 [DOI] [PubMed] [Google Scholar]
- 33. Al Maghaireh DF, Abdullah KL, Chan CM, et al. Systematic review of qualitative studies exploring parental experiences in the neonatal intensive care unit. J Clin Nurs 2016;25:2745–56. 10.1111/jocn.13259 [DOI] [PubMed] [Google Scholar]
- 34. Garner A, Yogman M, CHILD COPAO, et al. Preventing childhood toxic stress: Partnering with families and communities to promote relational health. Pediatrics 2021;148:e2021052582. 10.1542/peds.2021-052582 [DOI] [PubMed] [Google Scholar]
- 35. Nurturing care for early childhood development. 2018. Available: https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/child-health/nurturing-care
- 36. Kim THM, Campbell-Yeo M, Disher T, et al. Caregiver presence and involvement in a Canadian neonatal intensive care unit: an observational cohort study. J Pediatr Nurs 2021;60:123–9. 10.1016/j.pedn.2021.04.023 [DOI] [PubMed] [Google Scholar]
- 37. Italy - Maternity and paternity leave allowance, Available: https://ec.europa.eu/social/main.jsp?catId=1116&langId=en&intPageId=4618
- 38. UNESCO Institute for Statistics . International standard classification of education: ISCED 2011. 2012.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2023-002429supp001.pdf (285KB, pdf)
Data Availability Statement
Data are available upon reasonable request.