Abstract
Background: Asia hosts the second-largest international migrant population in the world. In Southeast Asia (SEA), key types of migration are labour migration, forced migration, and environmental migration. This scoping review seeks to identify key themes and gaps in current research on the ethics of healthcare for mobile and marginalised populations in SEA, and the ethics of research involving these populations.
Methods: We performed a scoping review using three broad concepts: population (stateless population, migrants, refugees, asylum seekers, internally displaced people), issues (healthcare and ethics), and context (11 countries in SEA). Three databases (PubMed, CINAHL, and Web of Science) were searched from 2000 until May 2023 over a period of four months (February 2023 to May 2023). Other relevant publications were identified through citation searches, and six bioethics journals were hand searched. All searches were conducted in English, and relevant publications were screened against the inclusion and exclusion criteria. Data were subsequently imported into NVivo 14, and thematic analysis was conducted.
Results: We identified 18 papers with substantial bioethical analysis. Ethical concepts that guide the analysis were ‘capability, agency, dignity’, ‘vulnerability’, ‘precarity, complicity, and structural violence’ (n=7). Ethical issues were discussed from the perspective of research ethics (n=9), clinical ethics (n=1) and public health ethics (n=1). All publications are from researchers based in Singapore, Thailand, and Malaysia. Research gaps identified include the need for more research involving migrant children, research from migrant-sending countries, studies on quality of migrant healthcare, participatory health research, and research with internal migrants.
Conclusions: More empirical research is necessary to better understand the ethical issues that exist in the domains of research, clinical care, and public health. Critical examination of the interplay between migration, health and ethics with consideration of the diverse factors and contexts involved is crucial for the advancement of migration health ethics in SEA.
Keywords: Bioethics, Southeast Asia, Research Ethics, Clinical Ethics, Public Health Ethics, Migration Health, Migrants, Refugees
Introduction
This scoping review commissioned by the Southeast Asia Bioethics Network, 1 seeks to identify research gaps in the ethics of healthcare for and research with marginalised migrant populations within Southeast Asia (SEA). The first phase of this research is to identify key themes in bioethics-related research within the SEA region, and thus serve as a reference to those with an interest in the ethics of migration health, including but not limited to researchers, policymakers, healthcare practitioners, and members or representatives of migrant communities. For the purpose of this paper, the word ‘migrant’ will include asylum seekers, refugees, internally displaced persons, stateless persons, and economic or labour migrants in regular or irregular situations, but exclude professional migrants, marriage migrants, international students and tourists. While we acknowledge that there are important ethical considerations related to the migration and health of the excluded migrant groups, it is beyond the scope of this paper to address these issues.
This paper begins with a brief overview of the migration landscape in SEA, with focus on the main reasons prompting migration in this region, followed by a discussion on why migration is a complex determinant of health. It then provides an outline of the role of bioethics in advancing migration health. Then, using a scoping review methodology, literature related to the ethics of migration health was analysed thematically and presented in the results section. Engagement with regional stakeholders of migration health was also undertaken to attain a more holistic overview of the research priorities in advancing regional migration health. In the discussion section, the value of conceptual and empirical bioethics research is discussed, and key research gaps identified by the scoping review are highlighted. The paper concludes by summarising the potential roles of the SEA Bioethics Network in advancing migration health ethics in this region.
Migration: A Southeast Asian context
The term ‘migrant’ is an umbrella term not defined under international law but is defined by the International Organization for Migration (IOM) as “a person who moves away from his or her place of usual residence, whether within a country or across an international border, temporarily or permanently, and for a variety of reasons” ( Sironi et al., 2019, p.132). Over the span of the last few decades, the number of migrants has increased exponentially across the globe ( McAuliffe & Triandafyllidou, 2021). Due to an intensification of intercontinental connectivity and mobility, the IOM estimates that there were around 281 million international migrants worldwide in 2020, which equates to 3.6% of the global population ( McAuliffe & Triandafyllidou, 2021). Europe with 87 million migrants (30.9% of the international migrant population) is currently the largest destination for international migrants, followed closely by the 86 million international migrants living in Asia (30.5%) ( McAuliffe & Triandafyllidou, 2021). Data on international migrants does not reflect immigration status or policy categories, and includes migrant workers, refugees or any other category of international migrants ( Migration Factsheet No. 2, n.d.). Another important point to note is that the majority of migratory movement is within countries and not across international borders, and hence the actual total number of migrants globally is far larger than estimated. 2 Table 1 summarises the definition of various groups of migrants relevant to this background paper.
Table 1. Definitions of different groups of migrants ( Sironi et al., 2019).
| Term | Definition |
|---|---|
| Asylum Seeker | “An individual who is seeking international protection. In countries with individualized procedures, an asylum
seeker is someone whose claim has not yet been finally decided on by the country in which he or she has submitted it. Not every asylum seeker will ultimately be recognized as a refugee, but every recognized refugee is initially an asylum seeker” (p14) |
| Refugee | “A person who, owing to a well-founded fear of persecution for reasons of race, religion, nationality, membership
of a particular social group or political opinion, is outside the country of his nationality and is unable or, owing to such fear, is unwilling to avail himself of the protection of that country; or who, not having a nationality and being outside the country of his former habitual residence as a result of such events, is unable or, owing to such fear, is unwilling to return to it.” (p175) |
| Migrant in an
irregular situation |
“A person who moves or has moved across an international border and is not authorized to enter or to stay in a
State pursuant to the law of that State and to international agreements to which that State is a party.” (p133) |
| Migrant in a
regular situation |
“A person who moves or has moved across an international border and is authorized to enter or to stay in a State
pursuant to the law of that State and to international agreements to which that State is a party.” (p134) |
| Internally
displaced persons |
“Persons or groups of persons who have been forced or obliged to flee or to leave their homes or places of
habitual residence, in particular as a result of or in order to avoid the effects of armed conflict, situations of generalized violence, violations of human rights or natural or human-made disasters, and who have not crossed an internationally recognized State border.” (p109) |
| Stateless person | “A person who is not considered as a national by any State under the operation of its law.” (p207) |
The SEA which includes 11 countries, i.e., Lao People’s Democratic Republic (PDR), Vietnam, Cambodia, Myanmar, Thailand, Malaysia, Singapore, Brunei, Philippines, Timor-Leste, and Indonesia, has a long history of population movement ( Migration Data Portal, 2022). With bilateral agreements and national labour-export programs, labour migration continued to increase over the years. Forced migration movements are also significant, with over a million Rohingyas fleeing Myanmar in successive waves since the early 1990s. Today, migration in SEA continues to increase due to conflict, enhanced mobility infrastructure, and employment-related issues. While North America, Europe and Western Asia are important regions of destination, the majority of the 23.6 million migrants from SEA do not migrate out of the region ( Migration Data Portal, 2022).
Owing to disparate socioeconomic development, civil unrest and natural disasters, many from the SEA region migrate in search of better living conditions and livelihood opportunities. Besides that, irregular migration, including the smuggling and trafficking of persons, is also an issue of regional importance ( IOM Thailand, n.d.). The key drivers for migration in SEA can be broadly categorised into labour migration, forced migration driven by regional conflict and violence, and environmental migration.
i) Labour migration
Regional economic disparities within and amongst SEA countries have led to a high number of labour migrants, and has resulted in the region experiencing one of the highest rates of population mobility in the world ( König et al., 2022). “According to the World Bank, the Association of Southeast Asian Nations (ASEAN) region accounts for 8% of the world’s migrants and hosts 4% of the world’s migrants”, with the majority of migrant workers working in lower-skilled occupations in the region ( ASEAN Secretariat, 2022). Cambodia, Indonesia, Lao PDR, Myanmar, the Philippines, and Vietnam are net-sending countries, while Brunei, Malaysia, Singapore, and Thailand are net-receiving countries of labour migration ( Pasadilla, 2011).
As of December 2022, the foreign workforce in Singapore numbered 1.4 million ( Ministry of Manpower Singapore, n.d.). Thailand, a major migrant-receiving country, has 2.49 million documented migrant workers as of March 2023 ( ILO Triangle in ASEAN, 2023). Conversely, the Philippines has nearly 11% of its total population living or working outside of the country, a value followed closely by Vietnam ( McAuliffe & Triandafyllidou, 2021). Vietnam is predominantly a migrant-sending nation, but recent census data shows an increasing trend of internal rural-urban migration ( IOM, 2020). Rural poverty, decline in agriculture and increased demand for labour in urban centers has resulted in significant internal rural-urban migration in SEA, particularly in countries such as Cambodia, Timor-Leste, and Vietnam ( UNESCO, 2018). Notwithstanding formal labour migration, there are irregular migrant workers in SEA who also contribute to the labour workforce, but this data is not reflected in official statistics ( ILO Regional Office for Asia and Pacific, 2022).
Conventionally, labour migration benefits migrant-receiving countries as it helps catalyse economic growth dependent on foreign labour, while migrant-sending countries stand to gain from a reduction in the rate of unemployment and increased income via foreign remittances ( Elmhirst, 2013). Nonetheless, it has been documented that many labour migrants particularly those in informal sectors are exposed to a multitude of abuses and mistreatment, including but not limited to forced labour ( McAuliffe & Triandafyllidou, 2021). Recent figures from the International Labour Organisation (ILO) indicated that more than 11 million people in Asia Pacific are victims of forced labour, 3 accounting for well over half of the global estimated number of 21 million victims, most of whom are involved in the sectors of agriculture, construction, manufacturing, entertainment and domestic work ( ILO, 2018).
ii) Forced migration driven by conflict and violence
The Rohingya people are the world’s largest stateless population, a circumstance contributed in part by their systematic exclusion from Myanmar citizenship since 1982 ( USA for UNHCR, n.d.). Being stateless, the Rohingya are denied basic rights and are exposed to various forms of abuse and exploitation ( UNHCR, 2022). Heightened violence against the Rohingyas in Rakhine State in 2017 and the subsequent military coup of February 2021 have caused massive displacements and the forced migration of the Rohingya regionally and internationally. As a result of the February 2021 military takeover, more than one million remained internally displaced from their homes, and at least 70,000 have fled Myanmar, adding to millions of Myanmar migrants with irregular status in the region ( McAuliffe & Triandafyllidou, 2021). As of December 2022, the refugee camps in Bangladesh’s Cox’s Bazaar are reported to host close to one million Rohingyas (UNHCR Operational Data Portal, n.d.). Overcrowding, poor sanitation ( English, 2018), devastating fires ( de la Portilla, 2022), heavy rain and landslides ( Relief Web, 2021), and violent criminal activities ( Aziz, 2022) have all given rise to increasingly dire humanitarian crises in refugee camps, pushing the Rohingyas into a constant state of forced displacement. Data from UNHCR in January 2023 revealed a 360% increase in Rohingya refugees attempting perilous sea journeys in search of protection, security, family reunification, and improved livelihoods in other countries within SEA ( UNHCR Flash Update, 2023).
The issue of forced migration is not limited to the Rohingya. SEA is also host to refugees and asylum seekers from other parts of the world, including but not limited to Pakistan, Yemen, Afghanistan, Palestine, Somalia and Iraq. At the time of writing, there are significant numbers of refugees and asylum seekers in Malaysia (183,790 registered refugees, with a majority of them from Myanmar) ( UNHCR Malaysia, 2023), Thailand (90,630 in refugee camps, 5000 urban refugees, 480,00 stateless persons) ( UNHCR Thailand, 2023), followed by Indonesia (12,706 persons of concern) ( UNHCR Indonesia, 2023).
iii) Environmental migration
The IOM defines environmental migrants as “persons or groups of persons who, for compelling reasons of sudden or progressive changes in the environment that adversely affect their lives or living conditions, are obliged to leave their habitual homes, or choose to do so, either temporarily or permanently, and who move either within their country or abroad” ( Kälin & Weerasinghe, 2017, p. 1) SEA, which is home to more than 640 million people, is vulnerable to extreme weather events and rising sea levels associated with climate change ( Prakash, 2018). In 2020, as a result of the Mount Taal volcanic eruption, cyclones, storms and flooding, the Philippines, Vietnam and Indonesia recorded more than six million displacements combined ( McAuliffe & Triandafyllidou, 2021). Periodic major environmental disasters aside, in the Mekong Delta, seasonal migration towards urban centres for work during the high flood season is a common practice, especially amongst rice farmers dependent on agriculture for livelihood ( Dun, 2011). Similarly, Timor-Leste's geographical attributes mean that it is also particularly susceptible to natural hazards, such as droughts, floods and landslides ( IOM Timor-Leste, n.d.).
Beyond these three major drivers of migration, there are also other diverse reasons for migration within and across countries ( Migration Data Portal, 2022). Migration is a global reality, and although the majority of global migration occurs within low- and middle-income countries (LMICs), migration from LMICs to high-income countries (HICs) forms the most prominent dialogue ( Abubakar et al., 2018). The discourse on migration is dominated by debates on immigration and border control, with gaps in understanding the relationship between migration and health. The health of migrants remains at the margins of policy making in countries at all income levels, and responses have generally revolved around disease control programmes such as immigration health assessments, health screening for fitness to work or travel, and border quarantine ( Wickramage et al., 2019).
Migration as a complex determinant of health
Health is defined as “a state of complete physical, mental and social well-being” ( WHO, 1948). Migration is a complex multi-directional process: it can be short-term, permanent, circular or result in a return to the country of origin, and it can be regular or irregular ( ASEAN Migration Outlook, 2022). At different phases of migration, migrants’ interactions with determinants of health will determine their health before, during or after their migration journey. For example, migration can potentially lead to poorer health due to precarious working conditions and poor access to healthcare or improve health by reducing the risks of encountering violence in the home country or by having better healthcare access in destination countries ( Vearey et al., 2020). Table 2 summarises the determinants of health for migrants at different phases of migration.
Table 2. Determinants of health at different phases of migration ( Legido-Quigley et al., 2020; Vearey et al., 2020).
| Pre-migration phase |
|---|
| ▪ Genetic and biological characteristics.
▪ Epidemiological profiles at origin (e.g. endemicity, infectious and chronic disease patterns). ▪ Exposures to trauma from protracted conflicts, human rights violations and interpersonal violence. ▪ Baseline health status, access to basic health services and nutrition in the country of origin. |
| Movement phase |
| ▪ Duration, circumstances and condition of journey. Overcrowded and unsafe living conditions, inadequate shelter, poor
sanitation, insufficient food and water. ▪ Experiencing or witnessing violence, exploitation and other abuses. |
| Interception phase |
| ▪ Injuries due to abuse, sexual violence and difficult journey.
▪ Starvation and nutritional deficits. ▪ Mental trauma. ▪ Infectious diseases and untreated chronic conditions. |
| Arrival and integration phase |
| ▪ Domestic migration policies and legal framework govern migrants’ access to health services (based on their legal status).
Barriers to health services including financial, legal, structural, physical and social determinants. ▪ Overcrowded living conditions upon arrival leading to various skin and respiratory infections. ▪ Limited health services in detention centres. ▪ Health risks behaviours and vulnerabilities among migrants and families. ▪ Language and cultural values - linguistically and culturally sensitive health service provision. ▪ Racism, social exclusion, discrimination, exploitation. ▪ Family/partner separation and stress. |
| Return/Resettlement |
| ▪ Duration of absence.
▪ Reintegration with family, household, and community at origin. ▪ Migrants may return to households that have benefitted from remittance flows and promote positive health trajectories, or maybe worse-off physically and psychologically with the cumulative tolls of their migration journeys. ▪ Delay in establishing/seeking healthcare as a result of long resettlement process. |
Across all migration phases, gender, age and socio-economic status are also determinants of migrant health ( Vearey et al., 2020). Beyond personal health, migration also impacts the health of family members left behind. The term ‘migration health’ is used because the process of migration impacts not only the health of migrants themselves but also their family members and the community at large ( Onarheim et al., 2021). In the Philippines, where approximately 12% of all Filipino households currently have or had a family member who is a migrant working overseas ( Mapa, 2020), left-behind children have been shown to suffer a vast range of poor physical and mental health outcomes ( Dominguez & Hall, 2022). Besides children, grandparents in Cambodian skip-generation households who look after left-behind children often face difficult ethical trade-offs and tend to prioritise their grandchildren's health and nutrition over their own ( Schneiders et al., 2021).
Different countries in SEA provide different forms of healthcare entitlements to migrants, and the accessibility and quality of healthcare are often linked to their legal and socioeconomic status ( de Smalen et al., 2021; König et al., 2022). Furthermore, in SEA, only the Philippines, Cambodia, and Timor-Leste have ratified the 1951 Refugee Convention or its 1967 Protocol ( UNHCR Global Appeal 2012–2013, n.d.). As a result, there are no legal safeguards, particularly in healthcare for refugees in countries such as Malaysia, Thailand and Indonesia, all of which host significant numbers of refugees. With the escalation of anti-immigration rhetoric and policies around the world, previously popular resettlement destinations such as the United States have limited refugee inflow ( Wroughton, 2018), leading to refugees having to stay for protracted periods in transit countries in SEA.
Irregular migrants who rely on informal economic sectors for their livelihoods often experience significant negative impacts on their health. These individuals face increased health risks due to their engagement in dirty, dangerous, and demanding jobs that may be degrading or demeaning ( Hargreaves et al., 2019). Additionally, they are susceptible to violence and have limited access, if any, to quality healthcare and social protection services. Being a migrant places individuals in sometimes hostile relationships with the state and can limit behavioural choices, such as nutrition and health services utilisation, which has knockdown effects on health ( Castañeda et al., 2015). Besides that, the World Migration Report in 2022 indicated that 75% of victims of trafficking for labour and sexual exploitation within Asia originate from SEA ( McAuliffe & Triandafyllidou, 2021). A study involving a large sample of men, women, and child survivors of trafficking in Cambodia, Vietnam and Thailand revealed a high prevalence of violence and unsafe working conditions, causing severe physical and psychological morbidity with increased need for healthcare ( Kiss et al., 2015).
From a public health perspective, migrant health and well-being are also integrally linked to the health and well-being of the populations in their countries of origin, transit and destination ( WHO, 2022b). Health concerns such as the transmission of infectious diseases can arise during all phases of the migration, and migrants originating from countries with severely compromised healthcare services may experience interruptions in vaccination schedules and poor baseline health ( Vearey et al., 2020). Such instances have potentially negative public health implications for migrants and host communities. Moreover, the geographical location and climate conditions of SEA make vector-borne diseases such as malaria a common problem. For instance, due to high levels of mobility, migrants face difficulties in accessing consistent care, which increases the risk of developing drug-resistant malaria ( IOM, 2020). Without access to timely testing and treatment, chances for onward transmission of diseases would correspondingly increase, potentially incurring higher costs to migrants and the host healthcare system ( Vearey et al., 2020).
The UN 2030 Agenda for Sustainable Development acknowledges that health is a fundamental precondition for migrants to work productively and contribute to the development of communities of origin and destination, and thus coordinated efforts are needed to ensure that the health of migrants is addressed throughout all migration phases ( IOM Migration Health Division, n.d.). Migration is thus a complex determinant of health with dynamic interactions with legal, social, economic and public health considerations.
The role of bioethics in SEA migration health
Bioethics is concerned with ethical issues relating to health and life sciences ( Dawson et al., 2018). It is an “interdisciplinary field populated by scholars, teachers, and clinical practitioners from a wide variety of traditional disciplines, such as philosophy, religious studies, law, medicine, nursing, social work, public health, the medical humanities (literature and history), and social sciences (politics, sociology, economics, anthropology)” ( University of Virginia, 2023). Onarheim et al. (2021) highlighted myriad ethical dilemmas faced by key stakeholders in migration health, which include health workers, regional and international policymakers, data managers and researchers, and migrants themselves, which suggests that bioethics is inextricably linked to almost all aspects of migration health. There are various ethical normative questions that can arise in migration health - questions such as “To what extent is the responsibility of receiving countries in providing healthcare for migrants?” “Are policies limiting healthcare to migrants morally acceptable?”, and “Should there be a difference in healthcare coverage for different groups of migrants?” ( Wild, 2012). In the context of resource-limited settings, is it ethically justifiable for (undocumented) migrants to receive similar health coverage as citizens?
While ethical concerns are pertinent for all research participants, research involving migrant populations produces a more complex set of ethical conundrums ( Parker, 2012). Research with migrants requires special consideration of issues surrounding potential exploitation, informed consent, and respect for participant autonomy ( Lott, 2005). The necessity and utility of research with marginalised migrant populations should be thoroughly assessed to ensure that the research seeks to provide new information that is of social value to the study population ( Global Forum of Bioethics in Research Meeting Report, 2017). Migration health researchers should also be cognisant of the fact that power inequalities experienced in research can leave specific members of a society (including migrants) dependent on the decisions of others, and that ethics of research is not limited to ethics board approval ( Pottie & Gabriel, 2014).
One important way in which bioethics can contribute to migration health is through advocacy research 4 , especially on behalf of others who are marginalised and systematically deprived of the ability to act in their own interests ( Dawson et al., 2018). Bioethicists hold a unique position to analyse ways in which migrants’ right to health is undermined and ways to redress breaches of human rights and equity ( Zion, 2019). Therefore, in response to policies violating human rights and health equity, there is a significant role for bioethicists (and all involved parties) to act individually and collectively as a community to bring forth constructive differences to practice and policy ( Dawson et al., 2018). Research on migrant health ethics can also be transformative – bringing disempowered voices into focus and providing a platform that offers solutions to pertinent issues surrounding migrant health ( Zion, 2019). It is imperative to not only recognise ethical challenges in migration health, but also to document the issues while systematically formulating sustainable ethical solutions to research, clinical practice and policymaking on migration health ( Onarheim et al., 2021).
Methods
Objectives
Despite the burgeoning academic literature on migration health in SEA, our hypothesis is that there is limited migration-health related normative bioethical analysis (e.g., literature prescribing what practitioners ought to do) and empirical bioethics research (e.g., literature describing what is the ‘experiential landscape’ in which ethical decisions and practices occur, pertaining to current opinions, values and practices etc) ( Rehmann-sutter et al., 2012; Kon, 2019). We also hypothesise that there is currently no comprehensive overview of the literature available on migration health ethics in SEA. This background paper seeks to answer two key research questions:
1. What is the existing literature on migration health ethics in SEA, and what are the key themes?
2. What are the research gaps in migration health ethics?
To answer these questions, we conducted a scoping review based on the Joanna Briggs Institute Manual ( Peters et al., 2020) and supplemented our understanding of the research gaps by engaging regional stakeholders in migration health. The findings would assist in establishing the future research agenda and priorities for scholars and researchers who are interested in research on migration health ethics in the context of SEA.
Search strategy
We conducted a scoping review of the literature relating to three broad concepts: population (i.e. stateless population, migrants, refugees, asylum seekers, internally displaced people), issues (i.e. healthcare and ethics), as well as geographical contexts (i.e., 11 countries in SEA). The search strategy ( Table 3), inclusive of keywords and free text terms, was developed and subsequently used for the following electronic databases: PubMed, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Web of Science. All three databases were searched from 2000 until May 2023 over a period of four months (February 2023 to May 2023). Additional searches for both full-text peer-reviewed articles, book chapters, commentaries, or other relevant policy documents and reports were done through forward and backward citation searches with Google Scholar, the WHO Regional Library (South-East Asia Regional Office), International Organization for Migration (IOM) repositories, and the United Nations High Commissioner for Refugees (UNHCR). Using keywords such as the names of SEA countries, ‘migrants’ and ‘refugees’, six bioethics journals (Journal of Medical Ethics, BMC Medical Ethics, Developing World Bioethics, Bioethics, Public Health Ethics and Asian Bioethics Review) were hand-searched for relevant publications. All searches were conducted in English.
Table 3. Search strategy.
|
Search
strategy |
(asylum* OR migrant OR migration* OR refugee* OR displaced OR foreign* OR stateless OR non-citizen OR noncitizen OR
mobile OR traffick*) AND (health*) AND (Ethic* OR Research ethics OR Biomedical ethics OR Bioethics) |
|
Inclusion
criteria |
1. Studies on the ethics of healthcare for or research with asylum seekers, refugees, internal and international labour
migrants, internally displaced persons, mobile populations who are marginalised and/or vulnerable. 2. Studies conducted in SEA or from SEA perspective, including cross-national studies. 3. Includes primary and secondary research 4. Studies published in the English language from the year 2000-2023, to ensure relevance and accuracy in the interpretation of articles. |
|
Exclusion
criteria |
1. Study population involving international students, international expatriates, tourists, healthcare professional
migrants. 2. Studies on SEA migrants resettled in countries outside of SEA. 3. Studies not based in SEA. 4. Epidemiological and socio-epidemiological studies 5. Did not contain substantial bioethical analysis |
Analysis
SHN independently reviewed the literature and identified relevant articles based on the title and abstract. ZLO and TCV assisted in assessing the articles’ full text to determine whether they fulfilled the inclusion criteria ( Table 3). Data was initially charted by SHN into a table with the following data items: first author, title and DOI, year, country, study area/population, study design, and remarks (brief summary and any key concepts), then were categorised into subdomains of ‘research ethics’, ‘clinical ethics’, ‘public health ethics’, and ‘general (unclassified)’.
The full-text articles were subsequently extracted and imported into NVivo 14 (Version Number: 14.23.0 (13)) to facilitate further thematic analysis using an iterative, inductive-deductive approach. Taguette ( https://www.taguette.org/), a freely accessible software, is also capable of the same analysis used in this study.Starting with preliminary main codes, which comprised the ethics sub-domains, new codes were then added as sub-category codes and new main codes as the analysis progressed. Thematic analysis was conducted as described by Braun and Clarke, where themes were identified and reported using six phases: (1) becoming familiar with the data, (2) generating initial codes, (3) generating initial themes, (4) developing and reviewing themes, (5) defining themes, and (6) producing the report ( Braun & Clarke, 2006).
As the articles retrieved varied in terms of research designs and data outcomes, we adopted a modified narrative synthesis approach, adapted from Deliz et al., 2020. First, each included study was classified into one of the sub-themes derived from thematic analysis. Each study was then summarised in turn, comparing themes within and between studies. Any studies that were especially innovative or largely representative of the sub-theme were highlighted.
Critical appraisal of the sources included was not done as we aimed to map out existing literature in migration health ethics and identify key concepts, gaps in knowledge and/or future research needs, rather than synthesising quantitative or qualitative data ( Peters et al., 2021).
Results
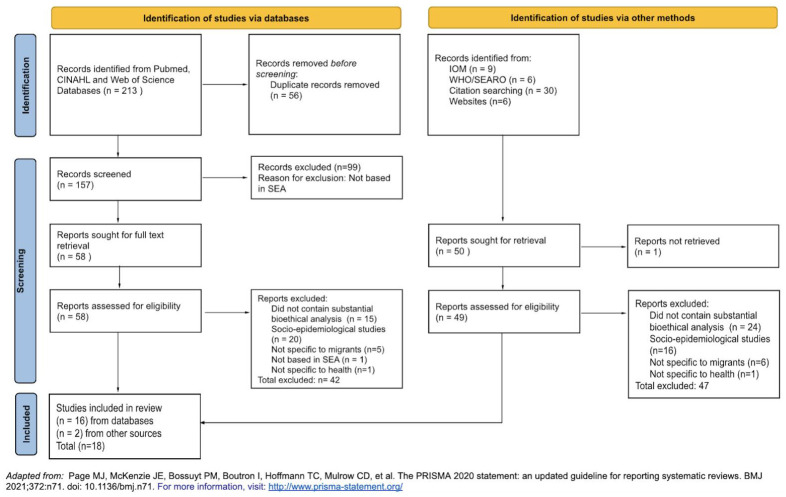
212 potentially relevant journal articles were identified from three separate databases. Records were imported into Zotero ( https://www.zotero.org/) and deduplicated (n=157). These 157 articles were assessed against the exclusion criteria, and 99 articles were excluded as they were not based in SEA. A total of 58 full texts were retrieved and screened, and a further 42 articles were excluded (did not contain substantial bioethical analysis, n=15; socio-epidemiological studies, n=20; not specific to migrants, n=5; not based in SEA, n=1; not specific to health, n=1). Two additional publications were retrieved from citation search. A total of 18 studies were included in the final review (see Figure 1). All publications included are summarised in Table 4.
Figure 1. PRISMA Selection Flowchart.
Table 4. Included studies (in alphabetical order based on first author’s name).
| First Author | Title and DOI | Year | Country | Study Area/Population | Study Design | Remarks | |
|---|---|---|---|---|---|---|---|
| 1. | Adams, P. | Ethical issues in research involving minority populations:
The process and outcomes of protocol review by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University https://doi.org/10.1186/1472-6939-14-33 |
2013 | Thailand | Research with minority
populations including migrants |
Quantitative and
qualitative analysis of submitted research proposals |
Ethical issues in research
with minority population |
| 2. | Cheah, P. Y. | Community engagement on the Thai-Burmese border:
Rationale, experience and lessons learnt. https://doi. org/10.1016/j.inhe.2010.02.001 |
2010 | Thailand | T-CAB at SMRU | Descriptive study | Experience, lessons learnt
and the unique challenges faced working with CAB |
| 3. | Chin, C. | Precarious Work and its Complicit Network: Migrant
Labour in Singapore https://doi.org/10.1080/00472336.2019.1572209 |
2019 | Singapore | Migrant care workers and
construction workers |
Narrative review | Introduced the concept of
precarity and complicity in migrant workers. |
| 4. | Ditton, M. J. | The Control of Foreigners as Researchers in Thailand.
https://doi.org/10.1525/jer.2009.4.3.49 |
2009 | Thailand | Migrants at Thai-
Myanmar border |
Commentary | Challenges faced when
conducting research with migrants. |
| 5. | Dutta, M. J. | COVID-19, Authoritarian Neoliberalism, and Precarious
Migrant Work in Singapore: Structural Violence and Communicative Inequality https://www.frontiersin.org/ articles/10.3389/fcomm.2020.00058 |
2020 | Singapore | South Asian migrant
workers in Singapore |
Qualitative
Research |
Low-wage contract-based
workers perform ‘hyper- precarious’ work, and how a lack of infrastructures for living and communication contributed to structural violence. |
| 6. | Freeman, T | At the limits of “capability”: The sexual and reproductive
health of women migrant workers in Malaysia https://doi. org/10.1111/1467-9566.13323 |
2021 | Malaysia | Women migrant workers
and stakeholders including health-care providers, unions, NGOs, employers and relevant government departments |
Qualitative study | Conceptualisation of
capability approach and application to migrant’s women access to sexual reproductive health. |
| 7. | Jecker, N. S. | Justice and global care chains: Lessons from Singapore.
https://doi.org/10.1111/dewb.12213 |
2019 | Singapore | Migrant care workers | Qualitative study | Utilised the human
capability approach to identify ways the capabilities were not upheld. |
| 8. | Khirikoekkong, N. | Research ethics in context: Understanding the
vulnerabilities, agency and resourcefulness of research participants living along the Thai–Myanmar border. https:// doi.org/10.1093/inthealth/ihaa052 |
2020 | Thailand | Pregnant migrant women
along Thai-Myanmar border |
Qualitative study | Explored vulnerabilities
and agency of clinical trial’s pregnant research participants |
| 9. | Khirikoekkong, N | Culturally responsive research ethics: How the socio-ethical
norms of Arr-nar/Kreng-jai inform research participation at the Thai-Myanmar border. PLOS Global Public Health, 3(5), e0001875. https://doi.org/10.1371/journal.pgph.0001875 |
2023 | Thailand | community advisory
board members, healthcare workers from the same clinic, or researchers st SMRU |
Qualitative study | Identified how socio-
ethical norms of Arr-nar/ Kreng-jai inform research participation at the Thai- Myanmar border |
| 10. | Maung Lwin, K | Motivations and perceptions of community advisory
boards in the ethics of medical research: The case of the Thai-Myanmar border https://doi.org/10.1186/1472-6939-15-12 |
2014 | Thailand | T-CAB at SMRU | Qualitative study | Identified considerations
relevant to the development of an approach to evaluating community engagement in complex research setting |
| 11. | Parker, M. J | Moral and scientific boundaries: Research ethics on the
Thai–Burma border. https://doi.org/10.1136/medethics- 2012-100582 |
2012 | Thailand | Research with migrants at
Thai-Myanmar border |
Commentary | Overview of issues in
research ethics. |
| 12. | Pratt, B | Closing the translation gap for justice requirements in
international research. https://doi.org/10.1136/medethics- 2011-100301 |
2012 | Thailand | Karen and Myanmar
refugees and migrants. |
Case study
qualitative research - in-depth interviews with trial stakeholders, direct observation at trial sites and analysis of trial- related documents |
Empirical bioethics
research to investigate if research at SMRU upholds obligations of justice in international research. |
| 13. | Pratt, B | Linking international clinical research with stateless
populations to justice in global health. https://doi.org/10.1186/1472-6939-15-49 |
2014 | ||||
| 14. | Pratt, B | Exploitation and community engagement: Can Community
Advisory Boards successfully assume a role minimising exploitation in international research? https://doi. org/10.1111/dewb.12031 |
2015 | Thailand | T-CAB at SMRU | Qualitative
research - in- depth interview, direct observation, and document analysis |
Used a case study
approach to determine if members of T-CAB are able to safeguard communities from exploitation from research. |
| 15. | Schaefer, G. O. | Zero COVID and health inequities: Lessons from Singapore.
https://doi.org/10.1136/medethics-2022-108205 |
2022 | Singapore | Migrant workers | Commentary | Public health strategy and
ethics |
| 16. | Tam, WJ | 健康是本钱 - Health is my capital: a qualitative study of
access to healthcare by Chinese migrants in Singapore. https://doi.org/10.1186/s12939-017-0567-1 |
2017 | Singapore | Chinese migrant workers | Qualitative study | Descriptive study of
migrants’ vulnerability through their migration journey |
| 17. | Voo, T | Ethical medical repatriation of guest workers: Criteria and
challenges. https://doi.org/10.1111/dewb.12286 |
2021 | Singapore | Migrant worker with non-
work-related injury |
Case study | Normative analysis of ethics
of medical repatriation |
| 18. | Yea, S. | The produced injured: Locating workplace accidents
amongst precarious migrant workmen in Singapore. https://doi.org/10.1016/j.socscimed.2022.114948 |
2022 | Singapore | Migrant workmen men
who were out-of-work due to an injury or salary/labour problems with their employer in Singapore |
Qualitative study | High injury rates are
caused by migrants' structural and economic vulnerabilities. |
We found a number of researchers who have conducted their empirical research or analysis through the lens of these ethical concepts: (i) capability, agency, and dignity (n=2); (ii) vulnerability (n=4); and (iii) precarity, complicity, and structural violence (n=3).
We also found research articles and commentaries which did not rely on specific ethical concepts in their methodological approach or analysis. These articles correspond to subfields in bioethics, namely: (i) research ethics (n=9) which concerns issues in the conduct of research; (ii) clinical ethics (n=1) which concerns issues in healthcare; and (iii) public health ethics (n=1) which pertains to ethical issues in public health ( National Institute of Environmental Health Sciences, n.d.).
Although not specifically analysed in this review, there were significant numbers of publications which focused on health equity or were motivated by inequity in migrant health (n=26) (see Shu, 2023a). These papers typically revealed inequities in health status or determinants between migrant and host populations.
Ethical concepts
The ethical concepts discussed in this section, while presented as distinct entities for the purpose of clarity, are in fact interlinked with many shared features.
Capabilities, agency, and dignity
We found two studies which analysed and applied the ethical concepts of capabilities, agency, and dignity in their research.
Freeman et al. (2021) applied a capability approach (CA) as a conceptual framework to analyse the experience of women migrant workers in Malaysia in meeting sexual and reproductive health (SRH) needs. The CA focuses on expanding the freedoms and opportunities (“capabilities”) available to individuals to live a life they value, including in the pursuance of SRH. The authors also considered “agency freedom” (i.e., “freedom to bring about the achievements one values and which one attempts to produce”) and “agency achievement” (i.e., the realisation of these pursuits) as a requisite to human flourishing ( Sen, 1992, pp.56–57). The CA is deemed influential in informing health policy and practice and has been used as a moral and philosophical justification for a right to health. Using a qualitative approach, the authors found that several capabilities that are critical in the management of SRH include having opportunities to acquire SRH knowledge, freedom to access SRH health care, and the presence of community leaders to act as focal points to share and disseminate SRH information. Through this approach, barriers to accessing SRH were identified, and essential resources such as education programmes, better access to appropriate health care, and social capital were identified to enhance SRH amongst women migrant workers. Public policies that deny access to health resources constrain migrant women's agencies, thus preventing them from realising their capability for SRH.
Similarly, Jecker and Chin (2019) also employed a human capability approach in analysing the plight of women primarily from Indonesia and the Philippines who migrated to Singapore to work as domestic care workers. The authors flesh out the concept of ‘human dignity’ as respect owed to other persons simply by their virtue of being human, and that is independent of our favourable appraisal of a person's merits. Thus, ‘human dignity’ is linked to what being human means (i.e., what humans are capable of doing and being). Jecker’s account of 10 central human capabilities includes being able to “have health, nourishment and shelter” and “to use one’s body to do what one intends to do” ( Jecker & Chin, 2019, p.159). The authors further explain that the lowest levels of capabilities comprised a floor required for human dignity (i.e. reaching a minimum threshold with respect to all the central human capabilities), and the highest levels comprise ‘a pinnacle for human flourishing’( Jecker & Chin, 2019, p.159). The study found that human dignity comes under threat for domestic care migrant workers in Singapore as they lack minimal opportunities for health. Food insecurity, employers’ abusive behaviour, occupational health risks, lack of rest and restricted social connection all reduced their capability for health. Their capability for bodily integrity, which closely relates to privacy, autonomy and agency, was not respected through movement restrictions and mandatory biannual health checks. 5 Using the capability approach, a multifaceted failure to safeguard the dignity of domestic care migrant workers was highlighted, and recommendations to protect their capabilities and dignity were proposed.
Vulnerability
There are four papers which examine ethical issues involving migrants in different contexts using the concept of vulnerability.
In their qualitative study with pregnant migrant women living along the Thai-Myanmar border, Khirikoekkong et al. (2020) uses the definition of vulnerability as a state of being “more susceptible to risks and less able to protect one’s own interests”, where “being in a vulnerable situation shapes obligations for others to help or take special care”, to consider ethical issues with research with this migrant population. The authors suggest that labelling a study population as ‘vulnerable’ (such as ‘pregnant women’, ‘migrants’ or ‘children’) can potentially err in two ways: first, by unfairly excluding individuals who are capable of consenting or assenting (with some support) and depriving them of the potential benefits of research participation, and secondly, by not being protective enough of individuals who do not belong to designated vulnerable groups. The study identified political, economic, social and health vulnerabilities, and found that despite the challenges and vulnerabilities in everyday lives, migrant women were able to exercise resourcefulness and agency to benefit from research participation. Therefore, researchers should be aware of specific contextual and structural vulnerabilities and be responsive to the vulnerabilities by respecting the agency of migrant women, minimising the burden of research participation, and providing adequate compensation.
Although the term ‘vulnerability’ was not specifically defined, Freeman et al. (2021) described women as “more vulnerable [compared] to their male counterparts” because “only women experience pregnancy and childbirth, sexually transmitted infections (STIs)…and women are more likely to be subjected to sexual violence’, and ‘these vulnerabilities are magnified in the context of migration”. Moreover, women migrant workers who are pregnant or have contracted STIs are liable to work permit cancellation and those who stay on become undocumented. They are unable to access antenatal care despite the availability of health care services. Consequently, pregnant women migrant workers may risk their lives inducing abortions for fear of losing their jobs. The risk of deportation following migrant care workers’ pregnancy was also highlighted by Jecker and Chin’s paper which emphasises gender-based vulnerabilities ( Jecker & Chin, 2019). Similarly, Tam et al.,’s research on Chinese migrant workers in Singapore highlighted different points of vulnerability through their migration journey, from existing vulnerabilities during the migration process, through their point of injury or illness and healthcare consultation, to the point of discharge, recovery and repatriation ( Tam et al., 2017).
Precarity, complicity and structural violence
Expanding on the concept of vulnerability, three other studies analysed the concept of precarity, complicity and structural violence with respect to the plight of migrant workers in Singapore.
Chin introduced the concept of precarity and complicity in the management of temporary migrant labour in Singapore ( Chin, 2019). Precarity is defined as a set of vulnerable labour conditions, including “low wages, short fixed-term contracts, numerous intermediaries such as recruitment agencies and sub-contractors, and poor legal and social protections”. Vulnerability in this context is defined as ‘a state of being exposed to the possibility of harm’ by exploitation, abuse and injury. With a focus on male construction workers and female domestic workers in Singapore, Chin provided a framework to identify how migrant workers' management strategies increase social vulnerabilities that constitute precarious work (through diffusing, displacing and disentangling responsibility towards migrant workers). Moreover, migrant workers faced disempowerment, discrimination, and were dependent on employers for food and accommodation, effectively deprived of ‘ordinary means’ to fulfil their well-being. The author also assigned moral responsibility to the complicit network, i.e., the state, employers, agents and others who enable, collaborate and condone social vulnerabilities. The identification of the mechanism that enables and sustains precarious work and assigning responsibilities to the complicit network provides a nuanced perspective of transforming precarity and identifying grounds for redress.
Yea similarly examined how the precarious migrant labour regime in Singapore contributes to heightened vulnerability and increased risks of serious workplace injuries and fatalities among migrant workers ( Yea, 2022). Using qualitative research with South Asian migrant workmen, Yea offered a conceptual framework of the ‘produced injured’ – emphasizing that ‘the political economy of migrant labour increases vulnerability to injury’. The author highlighted that the organisation of migration (including fees/debts and deportability) and fraudulent/deceptive recruitment (including wrongful deployment and substandard living conditions) have contributed to increased risks for injury. It was also difficult for workers to extricate themselves from risky work when they experienced conditions that were not agreed to initially before migration, including having to perform work that they were untrained for. The author provided accounts of migrants’ experiences and concluded that precarity is an ‘organising feature’ in the experience of occupational health and injury amongst migrant workers. Migrants’ vulnerability is embedded in structures and processes beyond the work environment in which injury occurs.
Using migrants’ lived experiences, Dutta described how low-wage contract-based workers perform ‘hyper-precarious’ work – defined by a lack of protection strategies, an absence of systemic infrastructures for workers to address their labour-related needs, and policy oversight that holds the employers accountable ( Dutta, 2020). Structural contexts of poor housing, sanitation infrastructures and food insecurity are framed as a form of ‘structural violence’ that worsens migrant workers' health and well-being, particularly during the COVID-19 pandemic. The fear of being terminated or deported for speaking up and the absence of information or voice infrastructures were deemed a form of ‘communicative and symbolic violence’, leading to migrants’ poor mental health.
Research ethics
Nine articles pertaining to ethical issues with migrant health research in Thailand were included in this review. This section could be broken down into the sub-themes of (i) general commentary (n=2), (ii) research ethics committee (n=1), (iii) community engagement (n=3), (iv) cultural responsiveness in research (n=1), and (v) research and global health justice (n=2).
General commentary
Drawing on the experience of malaria research at the Thai-Myanmar border, Parker provided a snippet of the complex cluster of challenges in research ethics ( Parker, 2012). Researchers are often faced with conflicting forms of guidance, with challenges in establishing good practice and effective solutions in research. The diversity in languages, values, beliefs and education levels of participants poses challenges to the informed consent process including the development of consent-related materials. While effective and inclusive community engagement is essential, it can be challenging when taking into account factors such as religious, political, linguistic, and ethnic diversity. There can also be concerns about the scope of the responsibilities of researchers before, during and after research, alongside difficulties in navigating the competing interests of research stakeholders such as government agencies and research funders.
Based on their research experience, Ditton and Lehane highlighted the need to understand the complexity of the political environment, cultural nuances and the roles of various stakeholders in chronic humanitarian crises involving migrants ( Ditton & Lehane, 2009). The authors have also documented the process of obtaining approval from the government for research to be conducted with migrants along the Thai-Myanmar border, as well as ethical and legal considerations for working with all stakeholders.
Research ethics committee
Adams et al.,’s (2013) paper provides an overview of the common research ethics issues encountered by a research ethics committee. Specifically, it analysed research proposals involving minority populations (including migrants) submitted to the institutional ethics committee of the Faculty of Tropical Medicine, Mahidol University, Thailand, and found that the majority of proposals submitted required revision or deferrals to ensure that there is no exploitation and undue negative legal implications, that the research methodology is well understood, and that appropriate compensation was provided to research participants ( Adams et al., 2013). The authors suggested the establishment of a community advisory board consisting of relevant community members in the early planning phase to ensure that research activities achieve acceptable ethical standards.
Community engagement
In safeguarding migrant communities’ interests, the Shoklo Malaria Research Unit (SMRU) at the Thai-Myanmar border facilitated the set-up of the Tak Province Community Ethics Advisory Board (T-CAB) in 2009 ( Cheah et al., 2010). Extensive training was provided to committee members consisting of Burmese or Thai nationals from the Karen ethnic group to undertake the tasks of vetting through research proposals. The T-CAB serves as an independent research advisory committee and acts as a bridge between researchers and community members, ensuring that local cultural sensitivities are taken into consideration. Despite the challenges in setting up a community advisory board, there were significant benefits through engagement with a wide range of community members. Besides advising on the ethical and operational aspects of research, such as informed consent procedures, confidentiality issues, and risks and benefits, the advisory board also serves as a platform for multilateral communication between researchers, research participants and other community members, and has an influence on research aims and impact. Further research has been done to investigate whether such an advisory board is reciprocally beneficial for the T-CAB members ( Maung Lwin et al., 2014). Despite practical challenges in navigating communication amongst board members of different cultural and linguistic backgrounds, evidence suggests that the T-CAB members saw positives in being active participants of research as they were able to serve as gatekeepers and empower the community by ensuring that research responds to the communities’ genuine needs ( Maung Lwin et al., 2014).
Two years after the establishment of the T-CAB, Pratt et al. investigated if the members could effectively safeguard research communities against exploitation ( Pratt et al., 2015). It has been proposed that the role of reducing exploitation should be formalised, and training needs to be provided for the members to develop critical appraisal skills and an understanding of what constitutes ‘exploitation’ and ‘health priority’. At the time of the study, the T-CAB members did not feel that they had the authority to take action if their recommendations were not adhered to. In recognition of the inherent power imbalances and resource limitations in such research settings, the study found that a considerable amount of time and training is needed to develop core competencies and capacities in protecting research communities against potential exploitation.
Cultural responsiveness in research
In recognition of the lack of practical research ethics guidance which takes into account moral perspectives in diverse cultural contexts, an empirical sociocultural analysis was performed using a qualitative approach at the Thai-Myanmar border ( Khirikoekkong et al., 2023). The research specifically analysed how sociocultural-moral norms pervasive in all aspects of the lives of local communities, known as Arr-nar (in Burmese and Karen) or Kreng-jai (in Thai), influence multiple aspects of research ethics, including “voluntary participation, provision of fair benefits, and understanding of research risks and burdens”. The study detailed the inherent complexities in the direct translation of ethical concepts into local languages, and the various steps taken to ensure the accuracy of the interpretation of the research data. The study also incorporated a creative use of participatory visual methods (PVM) using drawings and stories to confirm themes emerged from the qualitative data. The complex socio-ethical norms of Arr-nar/Kreng-jai not only inform ethical responsibilities, such as ensuring understanding, voluntariness, or duty of care, it also informs moral feelings, such as trust, appreciation, guilt or concern. Arr-nar/Kreng-jai impacted the motivations behind research participation, the commitment to maintaining research participation, and was implicated in the assessment of voluntariness, understanding and refusals. The research indicated that a greater sensitivity to local moral and social norms can be central to ensuring the ethical conduct of international research, and offered practical ethical guidance for researchers working in SEA.
Research and global health justice
‘Justice’, in the context of research ethics, often refers to the fair selection and recruitment of research participants, as well as equitable distribution of burdens and benefits ( Benatar, 2002). In global health research, this means ensuring that the research burden and risks should not fall disproportionately on participants in resource-poor context, and correspondingly research benefits should not be conferred disproportionately on those residing in the ‘global north’ where research funders and research institutions concentrate. The ethical framework of ‘research for health justice’ describes how international clinical research should be organized to advance the ends of global justice ( Pratt et al., 2014). Pratt et al., detailed the main requirements of achieving justice in international clinical trials, and laid out the obligations of governments, funders, sponsors, researchers and global health institutions. Clinical research in low and middle-income research settings commonly includes an obligation to:
-
i)
respond to local health needs and priorities
-
ii)
ensuring the provision of ancillary healthcare
-
iii)
provide access to post-trial benefits such as treatment or practices developed by the research
-
iv)
strengthen research capacity in host countries and communities.
Using a case study approach at SMRU, in-depth interviews (with investigators, T-CAB members, trial participants and research funding representatives), direct observation of T-CAB meetings and trial sites, and analysis of trial-related documents were conducted to measure whether and how obligations of justice are translated into international research practice ( Pratt et al., 2012). This methodology enabled the acquisition of authentic insights from diverse stakeholders and examined adherence to ethical requirements and contextual factors underlying the centre's research model. The study found that external research actors from high-income countries were partially able to uphold global health justice obligations. Challenges included the difficulties for external researchers to keep up with the changing disease burdens of host communities and adjust the focus of their research agendas accordingly. Moreover, in research involving the stateless population, the building of long-term, sustainable research capacity amongst mobile populations was not feasible due to regular staff turnover as a result of resettlement or migration. Therefore, it may not be reasonable to expect research capacity to be built to a level of independent proficiency when working with stateless populations who lack access to secondary and tertiary education opportunities. The study also highlighted difficulties in the provision of post-trial benefits when the population is not able to access state health systems.
Clinical ethics
Voo et al., performed a normative analysis of ethical issues concerning the medical repatriation of documented migrant workers in Singapore who sustained non-work-related health conditions ( Voo et al., 2021). The legal and policy regime in Singapore creates a landscape where migrant workers who suffer serious non-work-related medical conditions are vulnerable to repatriation. By adapting Kuczewski's ethical criteria for medical repatriation of undocumented migrants in the US ( Kuczewski, 2012) and applying them to a case study, critical aspects of the professional and ethical duties of medical professionals were discussed. In a context where migrant healthcare is largely dependent on ‘employer’s responsibility’, medical professionals should nonetheless avoid acquiescing to an employer’s decision which is against the best interests of the migrant worker qua patient. Instead, they should propose treatment plans that could be borne by employers or ensure the continuity of appropriate care following medical repatriation. The research highlighted that the ethics of medical repatriation involves more than medical professionals' ethical conduct, as country-specific policies in migration and healthcare can pose significant challenges. The authors have also listed a set of assessment questions to assist medical professionals in adhering to ethical standards in medical repatriation to avoid ‘patient-dumping’ in migrant-sending countries.
Public health ethics
Schaefer commented that the zero COVID policy as a public health strategy in Singapore exacerbated existing health inequalities for migrant workers in Singapore ( Schaefer, 2022). Restrictive policies curtailed their ability to earn a living and forced them to remain in cramped living spaces for extended periods of time. Despite being vaccinated, migrant workers’ movement remained limited even as restrictions were eased for the general population, raising doubt if public health strategy is truly prioritizing and promoting health equity within its broad framework.
Discussion
Whilst the health of migrants has been studied to varying degrees in SEA, our research on the ethical aspects of migration health highlights a gap in research capacity and output, especially in empirical bioethics research and normative analysis. In the process of conducting this review, we found a significant number of epidemiological and socio-epidemiological studies that seek to identify differences in health and health care for different groups of migrants ( Kim et al., 2023; Pham et al., 2019; Rajaraman et al., 2020). A key motivation for doing epidemiological studies, which often seeks to identify disparities in different groups, is often an ethical one with aims to bring about greater health equity between host and migrant communities ( Wild & Dawson, 2018). Socio-epidemiological studies are also useful in examining the interaction between socio-structural factors, distribution of health and disease, as well as how these influence individual and population health ( von dem Knesebeck, 2015). Nonetheless, we noticed an underapplication of ethical theories or frameworks, or conceptual analysis.
Utility of bioethics research
By utilising conceptual tools, ethical issues experienced in practice by the stakeholders involved can be better articulated, and consequently, could more reliably encourage and support responsible ethical conduct ( Beauchemin et al., 2022). Ethical concepts such as agency, vulnerability, precarity, and complicity identified from this review allow stakeholders in migrant health to identify and understand complex ethical issues in migrant health policy and research. For instance, the research by Chin and Yea has shown that the conceptualisation of the ethical issues faced by migrants may provide grounds for assigning responsibilities, reform and redress ( Chin, 2019; Yea, 2022). The research by Jecker and Chin (2019) and Freeman et al. (2021) similarly provided evidence of ways in which human capabilities were not upheld for migrant women in Singapore and Malaysia respectively. This knowledge may then be used for further analysis of policies and development of practices that promote well-being and dignity ( Molenaar & Van Praag, 2022).
Using the concept of vulnerability as an example, migrants are considered to be vulnerable due to poverty or low socioeconomic status, precarity, poor access to healthcare, and discrimination. The use of such terms can be useful in describing the practical difficulties migrants face, but the widespread generalisation in the use of ‘vulnerability’ as a fixed descriptor for migrants without clear understanding of how they are or are not vulnerable may have potentially negative implications ( Molenaar & Van Praag, 2022). This approach often fails to consider the perspectives and experiences of the migrants themselves, resulting in their marginalisation or exclusion from discussions on their health and health access. The presumed inherent vulnerability could also disproportionately redirect focus on migrants’ perceived deficit and weakness, and draw attention away from the structural causes of vulnerability which could be remedied ( Molenaar & Van Praag, 2022). It may even affect migrants themselves – some may refrain from engaging in positive, constructive activities, consciously limiting their abilities in a bid to portray themselves as vulnerable ( Mohammadi & Askary, 2022). In research, it could unfairly exclude their participation or could undermine their agency, denying migrants the opportunity to be involved in beneficial health research ( Khirikoekkong et al., 2020).
The theorisation of migration health ethics may also help us to understand the reasonings behind actions (or inactions) and could form the basis of why we should care enough about migrant health and act on it. Empirical bioethics research with an aim to describe policies and practices would assist in the identification of ethical issues and how they are experienced in practice. As evidenced by the publications included in this review, empirical research allows for an insight into how ethics is being carried out and whether or not a research or an intervention is upholding ethical standards ( Cheah et al., 2010; Pratt et al., 2014). Pratt et al., have provided evidence that bioethics empirical work is necessary to inform the obligations of justice in international clinical research and in the development of guidance to facilitate adherence and implementation of ethical guidelines ( Pratt et al., 2014). These play a crucial role in promoting justice in global health because only by having empirical evidence of the real and potential problems of putting ethics into practice can we then seek to address the issues identified and work towards improvement. Research detailing the actual experience of the implementation of a CAB, its challenges and benefits including from the perspective of community members themselves can also benefit other researchers in the region seeking to implement CAB to ethically enhance the way in which they conduct research ( Cheah et al., 2010).
Countries in Southeast Asia may share geographical proximity, but each country is rich with its own ethnic, religious, linguistic and cultural traditions and norms ( Arphattananon, 2021). Even within the same national territory, there may be a divergence in socio-cultural norms and values. As evidenced by the research on cultural responsiveness by Khirikoekkong et al. (2023) empirical ethics research on sociocultural and ethical norms can foster a nuanced comprehension of local customs and practices, and how these cultural factors impact the realm of research ethics. Knowledge from research as such may then aid in the development of research ethics support that is more responsive to local and regional ethical norms.
On the other hand, normative ethics analysis, such as the study by Voo et al. (2021) allows for discussion of ethical concepts, their implications, and identification of what ‘should be’ done in potentially ethically challenging circumstances in migrant’s medical management. Based on other research done in SEA, medical professionals are often faced with ethical dilemmas such as being forced to make clinical decisions based on migrants’ ability to pay ( Loganathan et al., 2019), having to navigate a dissonance between laws and professional codes including but not limited to the obligation to report undocumented migrants to the police ( Chuah et al., 2019) and being compelled to restrict the issuance of medical certificates ( Loganathan et al., 2019; Voo et al., 2021). Ethical guidance in migrant health delivery could be useful in assisting medical professionals in confronting multifaceted ethical dilemmas.
The health and well-being of migrants are impacted by a complex range of global and local factors, both within and beyond the health sector. Therefore, an ethical approach to policy making, research and clinical practice can provide means to identify ethical issues, frameworks for systematising information and catalyse the formulation of ethically acceptable solutions ( Onarheim et al., 2021). The systematic unpacking of dilemmas, values, and conflicts of interest equips decision-makers in migration health with analytic tools and guidance in dealing with challenges in policy making and practice. Ethical scrutiny and procedural guidance can also assist in highlighting policies and practices that are at variance with fundamental principles of medical ethics, public health and human rights ( Onarheim et al., 2021).
Research gaps identified
A bibliographic analysis of global migration health research from 2000 to 2016 has shown that most of the published academic literature represents the perspectives of high-income migrant destination countries, with a focus on communicable health diseases and mental health ( Sweileh et al., 2018). Despite the fact that Asia has one of the largest numbers of international migrants, research output from Asia is relatively low in comparison to other parts of the world ( Sweileh et al., 2018). Based on the limited number of studies identified and included in this review, there is a need to increase funding, human resources and research output in migration health ethics in this region. We found that the majority of bioethics research included in this review was done in Thailand, Singapore and Malaysia, which are major migrant destination countries in SEA. There is a paucity of migration health ethics research found in other parts of SEA, which is indicative of the need for future research and collaborative work.
We engaged with regional stakeholders in migration health to supplement our understanding of the research gaps identified from this review, which are detailed below:
i) Research involving migrant children
As most migration health research was undertaken in high income countries, issues relating to migrant children in developing countries remain largely unexplored ( Sweileh et al., 2018). This review has similarly identified a dearth of research in ethics relating to migrant children. There are millions of child migrants who travel across borders with or without their parents or were born to migrant parents in host countries ( ILO, 2015). Children who are unaccompanied or undocumented can be at increased risk of exploitation with limited access to basic social services such as education, housing and healthcare ( ILO, 2015). Considering the multifaceted realities of migrant children, more research could also be done to contextualise the practical difficulties in conducting health research and providing health care for migrant children in SEA. Such documentation is crucial in the formulation of responsive and pragmatic ethical guidelines to support future research that seeks to advance migrant children's health and well-being.
ii) Research from migrant-sending countries
The discourse about migration health ethics has focused on issues related to barriers to accessing health care, with a handful of studies focused on individual migrants’ well-being and dignity in destination countries. In predominantly migrant-sending countries such as Indonesia, Cambodia, and the Philippines, more research could be done to document migrants' experiences or challenges in destination countries or on return to their home countries.
iii) Quality of migrant healthcare
In investigating the ethical aspects of health service delivery, further research could focus on the quality of health care – from the perspective of service providers and migrants. Such studies can be useful for quality improvement and could serve as a baseline for subsequent monitoring and evaluation initiatives. Analysis of culturally competent, migrant-inclusive health systems is crucial so that different policy options can be considered to realise “migrant-inclusive universal health coverage” systems regionally ( Pocock et al., 2020). Studies on policy implementation, such as research from Thailand ( Suphanchaimat et al., 2019) which investigates the divergence between intention and implementation of health policies for migrants may be useful in the improvement of health services for migrants.
iv) Participatory health research
Participatory health research with an aim to shift the research paradigm from “research on people” to “research with people” is gaining international recognition and traction ( WHO, 2022a). One expression of participation is community engagement across the different phases of research, especially in advising on research ethics, and not just tokenistic involvement of migrants in health research, where migrants’ participation is limited to initial consultations to support recruitment or for dissemination of information at the end of research cycles ( WHO, 2022b). The CAB in Tak Province, Thailand, is a notable example of good practice that promotes the participation of migrant community members in research advisory boards, advocating for a shift away from solely researcher-directed projects and outcomes ( Cheah et al., 2010). There could also be a greater imperative to involve community members not just as ancillary support (for example, in participant recruitment and interpretation services) but to formally embed their roles in the ethics committee and be involved as researchers themselves.
v) Research with internal migrants
The vast majority of individuals do not move across national borders; instead, a significantly higher number migrate within their own countries. In 2009, approximately 740 million people were internal migrants, which is over three times the number of international migrants. ( McAuliffe & Triandafyllidou, 2021). However, most studies have focused on the ethics of the health of international migrants, indicative of a potential need to also focus on the ethical challenges stakeholders face in the health and healthcare for internal migrants.
Strengths and limitations
This scoping review – the first of its kind for Southeast Asia – aims to map out and signpost existing bioethics research in migration health for the region. Given the paucity of bioethics research in this area, the findings of this review are ameliorated and complemented by engagement with key regional stakeholders and experts in migration health in SEA. As bioethics is a relatively new field in SEA, this review showcases the range and utility of bioethics research on migration health, and demonstrates some ways in which it could contribute to the advancement of migration health regionally.
However, this study also possesses several limitations. Firstly, in terms of search strategy, the selected search terms were broad and might not have captured all relevant keywords in bioethics, leading to the potential exclusion of important bioethics research in SEA. Due to limitations in language interpretation, non-English publications were not included in this review. Secondly, this review does not differentiate between distinct migrant groups in different countries. Migrants are not a homogeneous group, and thus specific contextual factors, such as geography, socio-politics, and legal considerations, should be considered when examining their health outcomes, structural vulnerabilities and ethical issues in research and health practices involving migrants. Thirdly, there is a lack of capacity to perform quality appraisals of publications. Future work needs to be done to identify and analyse a broader body of research, and to identify further research gaps and priorities.
Conclusion
More robust research is required to understand the multidimensional ethical aspects of migration health in SEA. Based on our review and engagement with regional experts, we conclude that bioethics scholarships have an undeniably crucial role in synthesizing the content and extent of the ethical obligations of different stakeholders in migration health and in the construction of context-specific ethical guidelines to safeguard and support all stakeholders in healthcare and research. Clarity in ethical concepts is critical for migrant health by providing insights into the moral dimensions of the issues and challenges and is a cornerstone in the development of ethical frameworks for practice. In generating ethical solutions to issues relating to migration health in the SEA context, it is crucial for new knowledge to be generated through research grounded in migrants’ realities, with emphasis given to regional and temporal contexts ( WHO, 2022a).
The convergence of migration policy with ethics and health created a growing imperative for policy-makers, scholars, and practitioners in SEA to engage in cross-sector dialogue to align priorities and address the complexities of migrants’ health ( Kapilashrami et al., 2020). It is of paramount importance that ethics, in consideration of relevant regional values and belief systems, is central to research, policies, interventions, healthcare delivery and community engagement systems. As such, it would require regional expertise and meaningful collaboration to develop research agendas that ultimately aim to improve long-term health outcomes for migrants. The Southeast Asia Bioethics Network aims to cultivate the development of a vital interdisciplinary research community with a diverse range of skills and expertise, and position itself as a platform to engage and connect various stakeholders in migration health ethics and research. Ultimately, it aims to advance the health of migrants in the region through the promotion of ethical considerations in policy development, research, and health practices.
Acknowledgements
We would like to extend our deepest appreciation to the following experts for their time and insights on research gaps and priorities in migration health:
1. Dr Charles Hui, Chief of Infectious Diseases, Immunology and Allergy, Professor of Pediatrics, Faculty of Medicine, University of Ottawa
2. Dr Kolitha Wickramage, IOM
3. Dr Susheela Balasundaram, UNHCR Malaysia
4. Dr Tharani Loganathan, University Malaya
5. Dr Natarajan Rajaraman, Maluk Timor
6. Napat Khirikoekkong, Mahidol Oxford Tropical Medicine Research Unit (MORU)
7. Dr Melati Nungsari, Asia School of Business
8. Dr Phang Khean Chang, University Malaya
9. Watinee Kunpeuk, International Health Policy Program (IHPP), Ministry of Public Health, Thailand.
10. Anne Baltazar, founder of ANAK, a Malaysian non-governmental organisation for stateless children in Sabah.
The authors would also like to thank individuals who contributed to the completion of this background paper.
1. Professor Angus Dawson for his thoughtful feedback and constructive suggestions, especially on the early drafts of this paper.
2. Mrs. Adida Mohd Amin and Dr Ranita Hisham from Universiti Malaya Library for their help refining the search strategy.
Funding Statement
This research was supported by Wellcome Trust, ID: 222870/Z/21/Z. PYC’s research is supported by Wellcome (ID 220211/Z/20/Z). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; peer review: 2 approved with reservations]
Footnotes
1 The Southeast Asia Bioethics Network is a collaborative network consisting of the Faculty of Law, University Malaya, the Centre for Biomedical Ethics, National University of Singapore and the Mahidol Oxford Tropical Medicine Research Unit, University of Oxford funded by a Wellcome Trust five-year research grant.
2 The most recent estimate was 740 million internal migrants globally in 2009 as cited in Yilmaz Esmer, Gary Fields, Metin Heper, Cevat Karatas, Frederic Shorter. 2009. Human Development Report 2009: Overcoming barriers: Human mobility and development. New York. Available at: https://hdr.undp.org/content/human-development-report-2009
3 Forced Labour in Asia and the Pacific. (2018, April 2). http://www.ilo.org/asia/areas/forced-labour/WCMS_634534/lang--en/index.htm. The ILO defines forced labour as "all work or service which is exacted from any person under the threat of a penalty and for which the person has not offered himself or herself voluntarily."
4 “Studies seeking to measure social problems with a view to heightening public awareness of them and providing a catalyst to policy proposals and other action to ameliorate the problem in question”, ( Oxford Reference, n.d.)
5 Results from health checks were not shared confidentially, but were instead sent to employers and employees simultaneously.
Data availability
Underlying data
Zenodo: Publications with focus on health equity. https://doi.org/10.5281/zenodo.8202416. ( Shu, 2023a).
This project contains the following underlying data:
Appendix 1 Publications which focus on health equity, or were motivated by inequity in migrant health but were not included in analysis.docx.
Reporting guidelines
Zenodo: PRISMA-ScR checklist and flow chart for ‘Migration Health Ethics in Southeast Asia: A Scoping Review. https://doi.org/10.5281/zenodo.8226767. ( Shu, 2023b).
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
References
- Abubakar I, Aldridge RW, Devakumar D, et al. : The UCL- Lancet Commission on Migration and Health: The health of a world on the move. Lancet. 2018;392(10164):2606–2654. 10.1016/S0140-6736(18)32114-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams P, Wongwit W, Pengsaa K, et al. : Ethical issues in research involving minority populations: The process and outcomes of protocol review by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Thailand. BMC Med Ethics. 2013;14(1): 33. 10.1186/1472-6939-14-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Advocacy research. Oxford Reference. (n.d.). Reference Source [Google Scholar]
- Arphattananon T: Multi-Lingual and Multicultural Education in Globalizing Southeast Asia. Advances in Southeast Asian Studies. Article 2,2021;14(2). 10.14764/10.ASEAS-0064 [DOI] [Google Scholar]
- ASEAN Migration Outlook. July, 2022. Reference Source
- Aziz A: Rohingya crisis: 115 murders reported in camps in 5 years. August 25, 2022. Reference Source
- Beauchemin É, Côté LP, Drolet MJ, et al. : Conceptualising Ethical Issues in the Conduct of Research: Results from a Critical and Systematic Literature Review. J Acad Ethics. 2022;20(3):335–358. 10.1007/s10805-021-09411-7 [DOI] [Google Scholar]
- Benatar SR: Reflections and recommendations on research ethics in developing countries. Soc Sci Med. 2002;54(7):1131–1141. 10.1016/s0277-9536(01)00327-6 [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V: Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Castañeda H, Holmes SM, Madrigal DS, et al. : Immigration as a Social Determinant of Health. Annu Rev Public Health. 2015;36(1):375–392. 10.1146/annurev-publhealth-032013-182419 [DOI] [PubMed] [Google Scholar]
- Cheah PY, Lwin KM, Phaiphun L, et al. : Community engagement on the Thai-Burmese border: Rationale, experience and lessons learnt. Int Health. 2010;2(2):123–9. 10.1016/j.inhe.2010.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin C: Precarious Work and its Complicit Network: Migrant Labour in Singapore. J Contemp Asia. 2019;49(4):528–551. 10.1080/00472336.2019.1572209 [DOI] [Google Scholar]
- Chuah FLH, Tan ST, Yeo J, et al. : Health System Responses to the Health Needs of Refugees and Asylum-seekers in Malaysia: A Qualitative Study. Int J Environ Res Public Health. 2019;16(9):1584. 10.3390/ijerph16091584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson A, Jordens CFC, Macneill P, et al. : Bioethics and the Myth of Neutrality. J Bioeth Inq. 2018;15(4):483–486. 10.1007/s11673-018-9885-2 [DOI] [PubMed] [Google Scholar]
- de la Portilla R: Rebuilding from the ashes in Cox’s Bazar. 26 January, 2022. Reference Source
- de Smalen AW, Chan ZX, Lopes CA, et al. : Developing an evidence assessment framework and appraising the academic literature on migrant health in Malaysia: A scoping review. BMJ Open. 2021;11(1): e041379. 10.1136/bmjopen-2020-041379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deliz JR, Fears FF, Jones KE, et al. : Cultural Competency Interventions During Medical School: A Scoping Review and Narrative Synthesis. J Gen Intern Med. 2020;35(2):568–577. 10.1007/s11606-019-05417-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditton MJ, Lehane L: The Control of Foreigners as Researchers in Thailand. J Empir Res Hum Res Ethics. 2009;4(3):49–57. 10.1525/jer.2009.4.3.49 [DOI] [PubMed] [Google Scholar]
- Dominguez GB, Hall BJ: The health status and related interventions for children left behind due to parental migration in the Philippines: A scoping review. Lancet Reg Health West Pac. 2022;28: 100566. 10.1016/j.lanwpc.2022.100566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dun O: Migration and Displacement Triggered by Floods in the Mekong Delta. International Migration. 2011;49(s1):e200–e223. 10.1111/j.1468-2435.2010.00646.x [DOI] [Google Scholar]
- Dutta MJ: COVID-19, Authoritarian Neoliberalism, and Precarious Migrant Work in Singapore: Structural Violence and Communicative Inequality. Front Commun. 2020;5. 10.3389/fcomm.2020.00058 [DOI] [Google Scholar]
- Elmhirst R: Conceptualizing and researching flooding and migration in ASEAN.In: Chantavanich, S., C. Middleton and M. Ito (eds.). On the Move: Critical Migration Themes in ASEAN.Bangkok, International Organization for Migration and Chulalongkorn University-Asian Research Center for Migration,2013;67–94. Reference Source [Google Scholar]
- English J: Half a Million Rohingya Refugee Children at Risk in Overcrowded Camps in Bangladesh with Cyclone and Monsoon Season on Horizon. 16 thJanuary, 2018. Reference Source
- Freeman T, Miles L, Ying K, et al. : At the limits of “capability”: The sexual and reproductive health of women migrant workers in Malaysia. Sociol Health Illn. 2023;45(5):947–970. 10.1111/1467-9566.13323 [DOI] [PubMed] [Google Scholar]
- Global Forum on Bioethics in Research Meeting Report: The ethics of research with refugee and migrant populations. 2017. Reference Source
- Hargreaves S, Rustage K, Nellums LB, et al. : Occupational health outcomes among international migrant workers: A systematic review and meta-analysis. Lancet Glob Health. 2019;7(7):e872–e882. 10.1016/S2214-109X(19)30204-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ILO: Forced Labour in Asia and the Pacific. April 2,2018. Reference Source
- ILO: Migration and children: An outline of international standards, regional trends and good practices.2015.
- ILO Regional Office for Asia and Pacific. Migration Statistics. AP Migration.2022; Retrieved 3 March 2023. Reference Source
- ILO: Triangle in ASEAN: Quarterly Briefing Note Thailand.2023. Reference Source
- IOM Migration Health Division: Migration health in the sustainable development goals: ‘leave no one behind’ in an increasingly mobile society. n.d. Reference Source
- IOM: Situation Analysis of Migrant Health in Viet Nam.2020. Reference Source [Google Scholar]
- IOM Thailand: Migration Context. (n.d.); Retrieved 1 stMarch 2023. Reference Source
- IOM: Timor-Leste. (n.d.). Reference Source
- Jecker NS, Chin JJ: Justice and global care chains: Lessons from Singapore. Dev World Bioeth. 2019;19(3):155–168. 10.1111/dewb.12213 [DOI] [PubMed] [Google Scholar]
- Kälin W, Weerasinghe S: Environmental Migrants and Global Governance: Facts, Policies and Practices. In: McAuliffe, M. and M. Klein Solomon (Conveners) (2017) Ideas to Inform International Cooperation on Safe, Orderly and Regular Migration. IOM: Geneva.IOM.2017. Reference Source [Google Scholar]
- Kapilashrami A, Wickramage K, Asgari-Jirhandeh N, et al. : Migration health research and policy in south and south-east Asia: Mapping the gaps and advancing a collaborative agenda. WHO South-East Asia Journal of Public Health. 2020;9(2):107–110. 10.4103/2224-3151.294303 [DOI] [PubMed] [Google Scholar]
- Khirikoekkong N, Asarath S, Nosten S, et al. : Culturally responsive research ethics: How the socio-ethical norms of Arr-nar/Kreng-jai inform research participation at the Thai-Myanmar border. PLOS Global Public Health. 2023;3(5): e0001875. 10.1371/journal.pgph.0001875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khirikoekkong N, Jatupornpimol N, Nosten S, et al. : Research ethics in context: Understanding the vulnerabilities, agency and resourcefulness of research participants living along the Thai-Myanmar border. Int Health. 2020;12(6):551–559. 10.1093/inthealth/ihaa052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim EE, Alemi Q, Stempel C, et al. : Health disparities among Burmese diaspora: An integrative review. Lancet Reg Health Southeast Asia. 2023;8: 100083. 10.1016/j.lansea.2022.100083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiss L, Pocock NS, Naisanguansri V, et al. : Health of men, women, and children in post-trafficking services in Cambodia, Thailand, and Vietnam: An observational cross-sectional study. Lancet Glob Health. 2015;3(3):e154–e161. 10.1016/S2214-109X(15)70016-1 [DOI] [PubMed] [Google Scholar]
- Kon AA: The role of empirical research in bioethics. Am J Bioeth. 2009;9(6–7):59–65. 10.1080/15265160902874320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- König A, Nabieva J, Manssouri A, et al. : A Systematic Scoping Review on Migrant Health Coverage in Thailand. Trop Med Infect Dis. 2022;7(8):166. 10.3390/tropicalmed7080166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczewski M: Can Medical Repatriation Be Ethical? Establishing Best Practices. Am J Bioeth. 2012;12(9):1–5. 10.1080/15265161.2012.692433 [DOI] [PubMed] [Google Scholar]
- Legido-Quigley H, Leh Hoon Chuah F, Howard N: Southeast Asian health system challenges and responses to the ‘Andaman Sea refugee crisis’: A qualitative study of health-sector perspectives from Indonesia, Malaysia, Myanmar, and Thailand. PLoS Med. 2020;17(11): e1003143. 10.1371/journal.pmed.1003143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loganathan T, Rui D, Ng CW, et al. : Breaking down the barriers: Understanding migrant workers’ access to healthcare in Malaysia. PLoS One. 2019;14(7): e0218669. 10.1371/journal.pone.0218669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lott JP: Module Three: Vulnerable/Special Participant Populations. Dev World Bioeth. 2005;5(1):30–54. 10.1111/j.1471-8847.2005.00101.x [DOI] [PubMed] [Google Scholar]
- Mapa DS: 12 percent of Filipino households have an OFW member (results from the 2018 national migration survey). Philippine Statistics Authority.2020. [Google Scholar]
- Maung Lwin K, Cheah PY, Cheah PK, et al. : Motivations and perceptions of community advisory boards in the ethics of medical research: The case of the Thai-Myanmar border. BMC Med Ethics. 2014;15(1): 12. 10.1186/1472-6939-15-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuliffe M, Triandafyllidou A, (eds.): World Migration Report 2022. International Organization for Migration (IOM), Geneva,2021. Reference Source
- Migration Factsheet No.2. Migrants. (n.d). Reference Source [Google Scholar]
- Migration Data Portal. 2022. Reference Source
- Ministry of Manpower Singapore: Foreign workforce numbers. (n.d.). Retrieved 30 March 2023. Reference Source
- Mohammadi S, Askary S: Refugees live in destitution in Indonesia: Years of limbo and suffering lead refugees to protests for many weeks now for resettlement. Indonesia ReliefWeb, January 11,2022. Reference Source
- Molenaar J, Van Praag L: Migrants as ‘vulnerable groups’ in the COVID-19 pandemic: A critical discourse analysis of a taken-for-granted label in academic literature. SSM Qual Res Health. 2022;2: 100076. 10.1016/j.ssmqr.2022.100076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Environmental Health Sciences: Bioethics. Reference Source
- Onarheim KH, Wickramage K, Ingleby D, et al. : Adopting an ethical approach to migration health policy, practice and research. BMJ Glob Health. 2021;6(7): e006425. 10.1136/bmjgh-2021-006425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MJ: Moral and scientific boundaries: Research ethics on the Thai-Burma border. J Med Ethics. 2012;38(9):559–560. 10.1136/medethics-2012-100582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasadilla G: Social security and labor migration in ASEAN (Issue 34). Asian Development Bank,2011. Reference Source [Google Scholar]
- Peters MDJ, Godfrey C, McInerney P, et al. : Scoping Reviews (2020 version). In: E, A. and Z, M. (eds) Joanna Briggs Institute Reviewer’s Manual. JBI,2020. 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- Peters MDJ, Marnie C, Colquhoun H, et al. : Scoping reviews: Reinforcing and advancing the methodology and application. Syst Rev. 2021;10(1):263. 10.1186/s13643-021-01821-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham KTH, Nguyen LH, Vuong QH, et al. : Health Inequality between Migrant and Non-Migrant Workers in an Industrial Zone of Vietnam. Int J Environ Res Public Health. 2019;16(9): 1502. 10.3390/ijerph16091502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pocock NS, Chan Z, Loganathan T, et al. : Moving towards culturally competent health systems for migrants? Applying systems thinking in a qualitative study in Malaysia and Thailand. PLoS One. 2020;15(4): e0231154. 10.1371/journal.pone.0231154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pottie K, Gabriel P: Ethical Issues across the Spectrum of Migration and Health Research. In: M. B. Schenker, X. Castaneda, & A. RodriguezLainz (Eds.), Migration and Health: A Research Methods Handbook. Univ California Press,2014;345–360. 10.1525/9780520958494-019 [DOI] [Google Scholar]
- Prakash A: Boiling Point. International Monetary Fund, September,2018. Reference Source
- Pratt B, Maung Lwin K, Zion D, et al. : Exploitation and community engagement: Can Community Advisory Boards successfully assume a role minimising exploitation in international research? Dev World Bioeth. 2015;15(1):18–26. 10.1111/dewb.12031 [DOI] [PubMed] [Google Scholar]
- Pratt B, Zion D, Maung Lwin K, et al. : Linking international clinical research with stateless populations to justice in global health. BMC Med Ethics. 2014;15: 49. 10.1186/1472-6939-15-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt B, Zion D, Maung Lwin K, et al. : Closing the translation gap for justice requirements in international research. J Med Ethics. 2012;38(9):552–558. 10.1136/medethics-2011-100301 [DOI] [PubMed] [Google Scholar]
- Rajaraman N, Yip TW, Kuan BYH, et al. : Exclusion of Migrant Workers from National UHC Systems—Perspectives from HealthServe, a Non-profit Organisation in Singapore. Asian Bioeth Rev. 2020;12(3):363–374. 10.1007/s41649-020-00138-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehmann-Sutter C, Porz R, Scully JL: How to Relate the Empirical to the Normative: Toward a Phenomenologically Informed Hermeneutic Approach to Bioethics. Camb Q Healthc Ethics. 2012;21(4):436–447. 10.1017/S0963180112000217 [DOI] [PubMed] [Google Scholar]
- Relief Web: Heavy rains and floods in Cox’s Bazar.2021; accessed on 6 thFebruary 2023. Reference Source
- Schaefer GO: Zero COVID and health inequities: Lessons from Singapore. J Med Ethics. 2022;48(3):174. 10.1136/medethics-2022-108205 [DOI] [PubMed] [Google Scholar]
- Schneiders ML, Phou M, Tun V, et al. : Grandparent caregiving in Cambodian skip-generation households: Roles and impact on child nutrition. Matern Child Nutr. 2021;17 Suppl 1(Suppl 1): e13169. 10.1111/mcn.13169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen A: Inequality re-examined.Harvard University Press,1992. Reference Source [Google Scholar]
- Shu HN: Publications with focus on health equity. Zenodo.Dataset,2023a. 10.5281/zenodo.8202416 [DOI]
- Shu HN: PRISMA-ScR Checklist. Dataset,2023b. 10.5281/zenodo.8226767 [DOI]
- Sironi A, Bauloz C, Emmanuel M, (eds.): Glossary on Migration. International Migration Law No. 34.International Organization for Migration (IOM), Geneva,2019. Reference Source
- Suphanchaimat R, Pudpong N, Prakongsai P, et al. : The Devil Is in the Detail—Understanding Divergence between Intention and Implementation of Health Policy for Undocumented Migrants in Thailand. Int J Environ Res Public Health. 2019;16(6): 1016. 10.3390/ijerph16061016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweileh WM, Wickramage K, Pottie K, et al. : Bibliometric analysis of global migration health research in peer-reviewed literature (2000-2016). BMC Public Health. 2018;18(1): 777. 10.1186/s12889-018-5689-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam WJ, Goh WL, Chua J, et al. : 健康是本钱 - Health is my capital: A qualitative study of access to healthcare by Chinese migrants in Singapore. Int J Equity Health. 2017;16(1): 102. 10.1186/s12939-017-0567-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNESCO: Policy Briefs on Internal Migration in Southeast Asia .24 Jan, 2018; accessed 6th June 2023. Reference Source
- UNHCR Flash Update: Protection at Sea in South-East Asia - 2022 in Review. January, 2023. Reference Source
- UNHCR Global Appeal 2012-2013: Southeast Asia. (n.d.) Reference Source
- UNHCR Indonesia: Factsheet Indonesia. accessed on 1 stMarch 2023. Reference Source
- UNHCR Malaysia: Figure at A Glance.2023; accessed 1st March 2023. Reference Source
- UNHCR Operational Data Portal: Refugee Situation - Bangladesh. Reference Source
- UNHCR Thailand.2023; accessed on 1st March 2023. Reference Source
- UNHCR: Forced returns to Myanmar must stop immediately, says Türk. 26 October,2022. Reference Source
- University of Virginia: Health, Ethics and Society Program. 2023. Reference Source
- USA for UNHCR: Rohingya Refugee Crisis Explained. (n.d.); Retrieved 6 thFebruary 2023. Reference Source
- Vearey J, Hui C, Wickramage K: 7 Migration and health: Current issues, governance and knowledge gaps. World Migration Report. 2020;2020(1): e00017. 10.1002/wom3.17 [DOI] [Google Scholar]
- von dem Knesebeck O: Concepts of social epidemiology in health services research. BMC Health Serv Res. 2015;15: 357. 10.1186/s12913-015-1020-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voo TC, Kaur S, Rajaraman N: Ethical medical repatriation of guest workers: Criteria and challenges. Dev World Bioeth. 2021;21(4):227–236. 10.1111/dewb.12286 [DOI] [PubMed] [Google Scholar]
- World Health Organization: Constitution of the World Health Organization. Geneva: World Health Organization,1948.
- WHO: Participatory health research with migrants: a country implementation guide. 2022a. Reference Source
- WHO: World report on the health of refugees and migrants. Geneva,2022b. Reference Source
- Wickramage K, Simpson PJ, Abbasi K: Improving the health of migrants. BMJ. 2019;366: l5324. 10.1136/bmj.l5324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild V: Migration and Health: Discovering New Territory for Bioethics. Am J Bioeth. 2012;12(9):11–13. 10.1080/15265161.2012.692439 [DOI] [PubMed] [Google Scholar]
- Wild V, Dawson A: Migration: A core public health ethics issue. Public Health. 2018;158:66–70. 10.1016/j.puhe.2018.02.023 [DOI] [PubMed] [Google Scholar]
- Wroughton L: U.S. to Sharply Limit Refugee Flows to 30,000 in 2019. Reuters,2018. Reference Source
- Yea S: The produced injured: Locating workplace accidents amongst precarious migrant workmen in Singapore. Soc Sci Med. 2022;301: 114948. 10.1016/j.socscimed.2022.114948 [DOI] [PubMed] [Google Scholar]
- Zion D: On beginning with justice: Bioethics, advocacy and the rights of asylum seekers. Bioethics. 2019;33(8):890–895. 10.1111/bioe.12660 [DOI] [PubMed] [Google Scholar]