Abstract
Purpose
To improve understanding of podcast use in medical education by examining current research on descriptive attributes and educational outcomes, highlighting implications of the current evidence base for educational practices, and identifying research gaps to guide future investigation.
Method
The authors conducted a scoping review, searching PubMed and Embase databases in June–July 2020 for English-language studies of audio-only medical education podcast use in undergraduate, graduate, and continuing medical education. The authors excluded studies without original data or with nonphysician data that could not be separated from physician data. From included studies, the authors extracted data regarding descriptive outcomes (e.g., podcast use, content areas, structure) and educational outcomes (classified using Kirkpatrick’s 4 levels of evaluation).
Results
Of 491 unique articles, 62 met inclusion criteria. Descriptive outcomes were reported in 44 studies. Analysis of these studies revealed podcast use has increased over time, podcasts are a top resource for resident education, and podcasts are being incorporated into formal medical curricula. Educational outcomes were reported in 38 studies. The 29 studies that assessed learner reaction and attitudes to podcasts (Kirkpatrick level 1) showed learners value podcasts for their portability, efficiency, and combined educational and entertainment value. The 10 studies that assessed knowledge retention (Kirkpatrick level 2) showed podcasts to be noninferior to traditional teaching methods. The 11 studies that assessed behavior change (Kirkpatrick level 3) showed improved documentation skills in medical students and self-reported practice change in residents and practicing physicians after listening to podcasts. None of the studies reported system change or patient outcomes (Kirkpatrick level 4).
Conclusions
Future research should focus on the optimal structure of podcasts for learning, higher-level outcomes of podcasts, and the implementation of podcasts into formal curricula. Podcasts may prove to be essential tools for disseminating and implementing the most current, evidence-based practices.
Podcasts are playing an increasing role in medical education. U.S.-based internal medicine podcasts are consumed in 192 countries, with high uptake among medical students, residents, and practicing physicians. 1,2 Indeed, for emergency medicine residents, podcasts are the most used form of asynchronous education, 3 and internal medicine residents find podcasts more helpful than textbooks or journals. 4 Podcasts are available in almost every specialty, including anesthesia, dermatology, OB/ GYN, pediatrics, and radiology. 5
Podcasts can have widespread impact, particularly compared with traditional forms of didactic medical education such as classroom lectures, noon conferences, and grand rounds. For example, the internal medicine podcast The Curbsiders averages over 40,000 downloads per episode. 2 Podcasts also help foster “virtual communities” to support learning, 6 a feature that has become especially relevant during an era of physical distancing due to the COVID-19 pandemic.
U.S. medical schools and residency programs have begun to integrate podcasts into their formal medical curricula. The Accreditation Council for Graduate Medical Education allows emergency medicine residents to use podcasts with question sets for 1 of every 5 hours of education. 7 Residencies are creating curricula that involve teaching through the podcast medium (e.g., the internal medicine residency at Beth Israel Deaconess Medical Center’s Innovations in Media and Education Delivery [iMED] track). 8
Medical podcasts, along with other forms of digital education, may enable “a paradigm shift in medical education,” 3 but despite their rapid growth and adoption, research around this educational approach is limited and many uncertainties exist about its integration into medical education. In this scoping review, we sought to improve understanding of podcast use in medical education by examining the current research on their descriptive attributes and educational outcomes, as structured within the Kirkpatrick evaluative framework. 9 In this way, we aimed to highlight the implications of the current evidence base for educational practices and to identify research gaps to guide future investigation into podcast use in medical education.
Method
We performed a scoping review based on current best practices, including the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR). 10,11 In June–July 2020, we conducted a systematic search for peer-reviewed, published, English-language literature on the use of audio-only podcasts in undergraduate, graduate, and continuing medical education (CME). We focused on medical education podcasts, which we defined as podcasts whose primary focus is learning for physicians and physicians-in-training. We searched PubMed from inception through June 10, 2020, using key words medical education, clinical clerkship, medical students, interns, residents, trainee, or physician, and podcasts or podcasting. We searched Embase from inception through July 15, 2020, using similar key words. The full search strategies are provided in Supplemental Digital Appendix 1 at http://links.lww.com/ACADMED/B218.
We collated and reviewed all citations using Covidence systematic review software (Covidence, Melbourne, Australia). Screening by abstract and title was performed independently by 2 reviewers (J.M.K. and J.B.). Covidence flagged conflicts in exclusion screening, and the 2 reviewers resolved the conflicts. Exclusion criteria included: review articles with no original data; video medium or “vodcasts”; non–English-language studies; articles that curated existing podcasts; studies with visual aids, such as PowerPoint presentations; studies of multiple instructional modalities in addition to podcasts; commentary articles; studies of quality indicators in podcasts; and “how to create a podcast” articles without preliminary data. We also excluded studies that included nonphysicians where we could not separate physician data from other practitioner data.
Two authors (J.M.K. and J.B.) reviewed full texts. We identified 2 categories of reported results for data abstraction: descriptive outcomes and educational outcomes. Data regarding descriptive outcomes related to availability and accessibility (e.g., podcast use, learner levels, content areas, length, structure, barriers to uptake) were abstracted from each article. Educational outcomes were classified using Kirkpatrick’s 4 levels of evaluation, which are commonly used in medical education research to assess the effects of a program on trainees, patients, and populations. 9,12 Based on Kirkpatrick’s framework, data regarding learner reaction and attitudes, knowledge retention, behavior change, system change, and patient outcomes were abstracted from each study.
Results
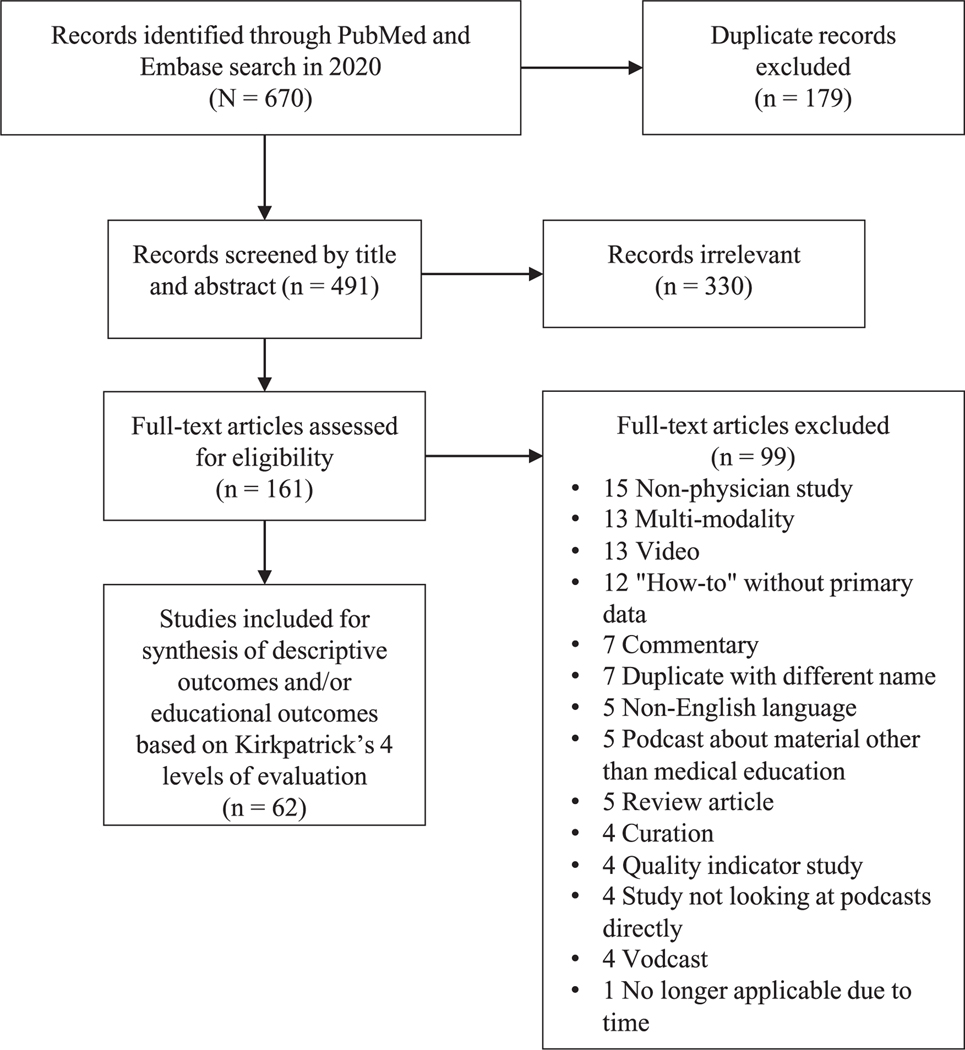
Of the 670 articles identified in the searches, 179 were duplicates and removed, leaving 491 unique articles. Of these, 330 articles were deemed irrelevant by title and abstract screening. We assessed 161 full-text articles for eligibility and excluded 99 (see Figure 1). A total of 62 articles met inclusion criteria, 2,3,5,6,13–70 the earliest of which was published in 2007. 52 A summary of the outcomes of each of the included articles is available in Supplemental Digital Appendix 2 at http://links.lww.com/ACADMED/B218.
Figure 1.
PRISMA 10 flowchart for scoping review of the literature on podcast use in medical education, conducted June–July 2020.
The majority of included studies (n = 44) described the use, availability, and accessibility of podcasts (e.g., number of residents who listen to podcasts, incorporation into medical curricula, ideal podcast length). 2,3,5,6,13,16,17,19,22,24,25,27,29–31,33–36,38–41,43–45,48–50,52–62,65,66,68,69 Many included studies (n = 38) assessed educational outcomes (e.g., learner reactions, knowledge retention, behavior change). 3,6,13–15,17,18,20,21,23–26,28,32,33,36–38,40–42,44–48,51,53,54,57,60,63–65,67,68,70 Some studies reported only descriptive outcomes (n = 24), 2,5,16,19,22,27,29–31,34,35,39,43,49,50,52,55, 56,58,59,61,62,66,69 or only educational outcomes (n = 18). 14,15,18,20,21,23,26,28,32,37,42,46,47,51,63,64,67,70
Descriptive outcomes
Usage over time.
The use and acceptability of podcasts in medical education have evolved over time. For example, in a 2007 study, 60% of medical students and physicians felt podcasts had no role in professional development, 52 and in a 2012 study, only 2% of pediatric anesthesia residents identified podcasts as their favorite learning method. 69 Emergency medicine trainees were early adopters of podcasts for medical education. One 2015 study found 90% of Canadian emergency medicine residents used podcasts, and podcasts were in the “top 3 resources most contributing to a resident’s education.” 44 Podcasts are increasing in popularity in other specialties: A 2019 study of residents from various training programs reported that 71% of residents supported the utility of podcasts. 43
International use.
Several articles demonstrated the international spread of medical education podcasts, with some podcasts reaching over 100 countries. 57,62 Podcast use may not be consistent across countries. A study of urology trainees found North American urology trainees listened to health care–focused podcasts more often than did trainees from South America, Europe, Asia, Africa, Australia, and New Zealand. 22
Across specialties.
Podcast content is available in multiple specialties. A 2020 study examining podcast content across 19 subspecialties found that neurosurgery was the only subspecialty without an active podcast. 5 In fields where visualization is important, such as dermatology 30 and radiology, 16 the use of podcasts is widespread; for example, there were 41 podcasts focused on radiology in 2020. 16,30 Emergency medicine appears to have the most podcast content, with twice the podcast volume compared with other specialties, although specialties such as internal medicine and pediatrics also have a large volume of content. 5
Learner levels.
Learners at all levels listen to podcasts. The internal medicine podcast The Curbsiders has a broad audience of students, residents, and practitioners. 2 A 2020 review of radiology podcasts found the majority targeted radiology attendings (88%), with few targeted at radiographers and students (7%). 16 The podcast hosts varied, with 37% of podcasts hosted by radiologists and 12% by residents. 16 However, some studies found residents to be more likely than practicing physicians to use podcasts, suggesting younger physicians have more readily adopted podcasts as a form of education. 24,44 In a 2017 study, approximately 80% of medical student applicants to emergency medicine residency programs reported they listen to podcasts to supplement their education. 35 Regarding usage in CME, the internal medicine podcast Annals on Call has thousands of CME credits claimed, demonstrating substantial use by independent physicians. 2
Incorporation into formal education.
Educators are incorporating podcasts into medical curricula. A 2018 study found medical educators in Germany viewed podcasts as useful for teaching and learning. 61 In a 2015 study in the United States, almost all emergency medicine residents (97%) reported their residency program gives them information regarding free open-access medical education, which is a broad term to describe freely available educational resources including blogs and podcasts. 49 Two internal medicine residency programs distributed podcasts with key points from conferences. 13,45
Podcast content.
Listeners select podcast content for various reasons, including just-in-time training and filling knowledge gaps. Residents choose podcasts relevant to their clinical practice, with 80% of surveyed emergency medicine residents reporting they pick topics based on recent clinical encounters. 3 In addition, residents feel podcasts can supplement clinical learning and use them to prepare for new rotations. 34 Anesthesia residents reported using podcasts for routine study (28%), to learn about new topics (38%), to review for an exam (21%), and to prepare for an upcoming case (18%). 39 Podcasts are also used for board exam studying. Of trainees who used a free podcast to prepare for The Royal College of Physicians Postgraduate Membership Examination in the United Kingdom, about three-quarters reported it was good, useful, and novel. 36
Learners prefer content matched to learner level 39 and specialty. 65 For example, in a study of family medicine, neurology, and internal medicine residents, residents in each program identified unique neurology content areas for podcasts to focus on. 65
Podcast length.
Various reports on the optimal length of podcasts appear in the literature. Among medical students who listened to a general surgery podcast with 10- to 15-minute episodes, almost all listeners felt the length and detail were “about right.” 64 In comparison, listeners of a palliative care podcast appreciated episodes with a duration of less than 6 minutes. 41 A 2018 study found that the majority of Canadian medical students listened to podcast episodes in multiple sessions of 15 to 30 minutes. 37 Another study of medical students found that the ideal podcast length is less than 30 minutes. 14 However, ideal podcast length may vary by content. The majority of medical students who listened to podcasts on asthma and toxicology wanted only the asthma podcast to be shorter. 37 Preferred podcast duration also varies by format, with anesthesia residents wanting shorter podcasts about procedure skills, journal article summaries, case presentations, and debates/discussions and longer didactic lecture podcasts. 39
Podcast structure.
Learners value several other aspects of podcast content and production. Learner audiences across specialties believe the incorporation of dialogue—rather than monologue lectures—creates a conversational tone, and personal anecdotes and humor create an enjoyable, engaging, and entertaining educational experience. 6,15,17,18,38,46,51,64 Podcasts were called “edutainment” by a 2019 study. 38 Learners also value podcasts that have credible source material, 18,65 summarize key points at the end, include content quizzes, and explain all acronyms. 18,37,46 Some listeners requested podcasts include the ability to navigate quickly to desired content 65 and to choose a faster listening speed. 18 Lastly, audio quality is important to listeners. 65
Barriers to podcast uptake.
Initially, lack of podcast awareness was a barrier to uptake, with a 2013 study of residents finding that 98% did not use podcasts because they did not know they were available. 39 A more recent study (2017) found that most residents discover new podcasts by word of mouth, 48 suggesting that peer and faculty recommendations may have overcome this barrier as the availability of podcasts has grown. Cost may also be a barrier to podcast use. When a Canadian emergency medicine podcast changed from a pay-for-service model to a free online resource, its downloads increased 4-fold to 45,000 downloads monthly. 68 Further, the inconsistent production schedules of many podcasts may hinder uptake by listeners. 30 In addition, residents identify podcasts as a passive learning process and may unsubscribe from podcasts that are not engaging. 6 Listeners note they can get distracted while listening and sometimes their retention from podcasts is “not great.” 6 Other barriers for some learners include lack of time and podcast length, 14,15,46 as well as difficulty with navigation and concerns about credibility. 58
Educational outcomes
Learner reactions and attitudes (Kirkpatrick level 1).
Twenty-nine studies described learners’ reactions and attitudes to medical education podcasts (n = 29). 3,6,13–15,17,18,21,23–25,32,33,36–38,40,41,45– 47,51,53,57,60,64,65,67,68 While learners generally had positive reactions to podcasts, specific factors caused dissatisfaction, as noted above (see “Barriers to podcast uptake”).
Learner reactions as listening behaviors.
Audiences at all levels of training (medical students, residents, fellows, and independent physicians) appreciate that medical education podcasts offer flexible learning opportunities that they can participate in while engaged in other activities. 6,25,32,38,40,46 Learners also value the autonomy of podcasts, including how podcasts give them freedom to review a desired topic at a time and place that is convenient for them, move at their own pace, and repeat content. 36,39,64 Podcasts offer efficient learning that is “quick and concise” and “straight to the point.” 64 Most pediatric residents (92%) in a 2020 study noted podcasts make it easier for them to find time to study. 40
A common attitudinal change from listening to medical education podcasts is a reported sense of community. Listeners reported that listening to podcasts made them feel more connected to their local practice community 6 as well as more connected to larger national and global professional communities. 6,57 Attending physicians also reported feeling more connected to residents through podcasts. 13
Learner reactions to podcasts compared with other methods of instruction.
For medical students, podcasts seem helpful 21 but are not a replacement for didactics. 19 In a 2019 study, students ranked podcasts lower in importance than small group tutorials, simulation, and large group lectures for a musculoskeletal curriculum. 47 The majority of students on an emergency medicine rotation (60%) felt their oral case skills would be improved with brief instructions during orientation while only one-fifth of them reported a podcast would be helpful. 23
Podcasts appear to be more readily accepted among residents. When family medicine residents were randomized to a formal lecture versus a podcast for learning in a 2015 study, there were no significant differences in satisfaction between the groups, and 100% of those receiving the podcast intervention (n = 24) were either very or somewhat interested in listening to additional podcasts. 67 Another study found that residents rated podcasts higher in enjoyability, maintaining interest, and entertainment compared with written material. 51 In general, residents rate podcasts as more enjoyable and entertaining than other forms of learning such as readings. 46,51,64
Subjective confidence and knowledge attainment.
Four studies commented on listeners’ perceived knowledge improvement and confidence after listening to podcasts. 40,46,60,68 Listening to podcasts appears to improve learners’ self-efficacy and helps them feel more confident managing illnesses. 46,68 Almost all residents (97%) who listened to a pediatrics podcast felt the podcast increased their knowledge and helped them apply knowledge clinically. 40 Similarly, all listeners who submitted CME evaluations for 1 podcast noted learning something new that was clinically applicable. 60
Knowledge retention (Kirkpatrick level 2).
Ten studies objectively assessed knowledge retention by looking at test scores. 14,15,20,28,37,42,51,53,63,67 Some of these studies evaluated changes in medical student knowledge (n = 4) 14,15,37,42 and others evaluated changes in resident and fellow knowledge (n = 6). 20,28,51,53,63,67 Overall, podcasts appear to be noninferior to traditional educational resources for knowledge retention.
After use of a podcast, medical students’ knowledge scores increased posttest compared with pretest in 3 studies without a comparison group. 14,15,42 In another study, medical students had statistically significant increases in posttest knowledge scores when taught with podcasts or blogs, with no significant differences between the podcast and blog groups. 37
Several studies evaluated knowledge retention in residents and fellows, comparing retention after podcasts with retention after traditional educational interventions, such as didactic lectures, 53,67 written curricula, 51 and bulletins. 20 In studies that used a pretest/posttest methodology, there were significant increases in posttest scores in the podcast cohort. 51,67 The four studies that evaluated knowledge retention in residents and fellows all found participants who used podcasts performed as well as or better than participants who learned from other forms of instruction. 20,51,53,67
Another study looked at the use of interpolated questions in podcasts to increase active learning. 63 Residents were randomized to listen to either a regular podcast or that same podcast with interspaced, interpolated questions. There were no significant differences between the 2 groups on the immediate posttest, but the trainees randomized to the podcast with interpolated questions had a significantly higher mean score on the retention test several weeks later. 63
For emergency medicine residents, self-report of listening to the podcast EM Basic and years of residency training were both associated with higher in-training exam scores. 28 However, listening to a different podcast (EM:RAP) was associated with lower in-training exam scores. 28
Behavior change outcomes (Kirkpatrick level 3).
Behavior changes based on listening to medical education podcasts were observed in 11 studies, primarily by participant self-report. 26,32,38,44,45,48,54,60,67,68,70
Medical students.
Two studies looked at behavior changes in medical students. 26,70 In 1 study, the podcast group received a podcast on documentation skills before a clinical rotation while the comparison group did not receive any intervention. 70 Two independent reviewers scored students’ clinical notes, and the podcast group scored significantly higher. In the second study, medical students were assessed on their ability to complete a written clinical assessment including a differential diagnosis for chest pain. 26 Students who received access to a podcast on developing a differential diagnosis scored significantly higher than those who did not.
Residents and independent physicians.
Six included studies measured self-reported change in practice related to podcast use and found that 55% to 90% of listeners reported changing their practice on the basis of what they heard in the podcast. 32,38,45,48,60,68 The highest reported change occurred among emergency medicine physicians. 68
Three studies found 43% to 100% of listeners to medical education podcasts were motivated to spend additional time learning about podcast topics or listening to more podcasts. 45,60,67 Both residents and program directors reported increased use of the primary literature after accessing free online educational resources such as podcasts, wikis, and blogs. 44 One study correlated guideline-concordant care in obstetrics with podcast use and found that physicians who reported using podcasts always or often for continuing education had greater odds of counseling postpartum patients on healthy eating behaviors. 54
System change and patient outcomes (Kirkpatrick level 4).
None of the studies reported evidence of system or care delivery outcomes attributed to medical education podcast interventions. None of the studies measured changes in patient outcomes due to podcast use.
Discussion
Medical education podcasts are increasingly being used as learning tools. Our review of the literature revealed significant gaps in research about their optimal use and effectiveness in medical education. We found that learners value medical education podcasts because they are flexible, fill self-defined learning needs, and provide a sense of community and entertainment. Our findings suggest advanced learners find podcasts valuable, particularly podcasts with high production and audio quality. Medical students appear to have less affinity for the medium than more advanced learners, rating podcasts as less helpful than other educational resources; they may benefit from more targeted podcast development. The literature on podcast use appears to be broadly similar to the literature on other e-learning interventions, especially regarding learner flexibility, the importance of technical skills, and the challenges in integration in heterogenous fields. 71 Podcast research suffers from many of the same limitations as well, with a paucity of controlled studies, heterogenous populations, and poor reporting. 72
We identified several areas for future research. First, research is needed on the best delivery structure for medical education podcasts. It is likely that different types of learners and learning settings may benefit from particular formats and types of podcasts. Podcast use has thrived in visual fields like dermatology 30 and radiology, 16 suggesting that the areas and content best suited to podcasts are not entirely intuitive and are worthy of future research.
Second, research is needed on the formal integration of podcasts as 1 part of a broader curriculum. Medical education podcasts have seen rapid implementation in some fields. 73 In emergency medicine, this may be due to contextual factors related to the traditional emergency medicine educational structure (e.g., the difficulty in getting all learners together at 1 time) as well as approval and flexibility from accrediting bodies at the programmatic level (e.g., the provision for Individualized Interactive Instruction in emergency medicine residencies 74). The success of integrating podcasts into emergency medicine training offers an important observation: learning via podcasts appears to be highly learner-specific and contextual, suggesting that best practices need to consider key aspects of the producer (audio quality, expertise, format), the listener (immediate needs, available time), and the clinical learning environment. In addition, podcast producers should consider the accessibility of their content when considering listener needs. For example, learners with hearing limitations may prefer audio transcripts to accompany podcasts, yet not all podcasts make written summaries available. 37
Third, research is needed on the effects of medical education podcasts on system change and patient outcomes. While research is lacking, there is reason to be optimistic about the impact of medical education podcasts in these areas, particularly in CME, which has the potential to reach the largest audience. Because podcasts have a global spread and the capacity to engage far more people per episode than a typical continuing education conference, medical education podcasts may prove to be essential tools for disseminating innovations and implementing the most current, evidence-based practices into patient care. This potential makes understanding how to make medical education podcasts more effective an imperative for education researchers.
Limitations
There are important limitations to our scoping review. Podcasts and podcast use have changed rapidly, and research published a decade ago describes a considerably different phenomenon from research published in 2020. Medical education podcasts appear noninferior to other educational approaches, but studies often lack comparison groups or active controls. In addition, published studies are heterogenous, incorporating a variety of medical specialties, didactic styles, audiences, and delivery and evaluation methods. Additionally, many medical education podcasts exist that have not been rigorously studied, thus limiting knowledge of the full impact of this medium on learners. The scoping review approach attempts to catalog this heterogeneity to support generalizability; however, the limitations of the included studies limit generalizability overall. This review excluded studies published in languages other than English, limiting our ability to characterize the impact of non–English-language podcasts, although only 5 studies were excluded for this reason. Lastly, this review searched only 2 major databases (PubMed and Embase). These databases were chosen as the foundational sources for reviews in health and biomedical sciences. An informal search of other databases (including PsycInfo, ERIC, and CINAHL) did not yield substantial additional contributions.
Conclusions
Medical education podcast use is an evolving educational approach with evidence of benefit to learners across all levels of training. Medical education podcasts reach a broad audience, and learners value podcasts for their flexibility and relevance to immediate clinical concerns. Podcasts hold the potential to be powerful tools for disseminating innovations and evidence and should be further studied to improve understanding of how to maximize their benefits to learners and patients.
Supplementary Material
Acknowledgments:
The authors would like to acknowledge Kelsey Sawyer, MS, biomedical and life sciences librarian, Brown University, for her help in creating the strategy for the literature search.
Funding/Support:
J. Berk received funding support from the New York Academy of Medicine Jeremiah A. Barondess Fellowship in the Clinical Transaction, the American Board of Medical Specialties Visiting Scholars Program, and internal funding from the Children’s Miracle Network Award (Department of Pediatrics at Hasbro Children’s Hospital).
Footnotes
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Jessica M. Kelly, Division of Emergency Medicine, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania..
Andrea Perseghin, VCU Health, Richmond, Virginia..
Alan W. Dow, Department of Medicine, Virginia Commonwealth University School of Medicine, Richmond, Virginia..
Shreya P. Trivedi, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts..
Adam Rodman, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts..
Justin Berk, Departments of Medicine and Pediatrics, Warren Alpert Medical School, Brown University, Providence, Rhode Island.
References
- 1.Rodman A, Abrams HR, Watto M, et al. Medical Podcasting in low- and middle-income countries: A needs assessment and vision for the future. Teach Learn Med. 2021;33:416–422. [DOI] [PubMed] [Google Scholar]
- 2.Berk J, Trivedi SP, Watto M, Williams P, Centor R. Medical education podcasts: Where we are and questions unanswered. J Gen Intern Med. 2020;35:2176–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mallin M, Schlein S, Doctor S, Stroud S, Dawson M, Fix M. A survey of the current utilization of asynchronous education among emergency medicine residents in the United States. Acad Med. 2014;89:598–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernstein E, Bhardwaj N, Pfoh ER, Yudelevich E. A nationwide survey of educational resource utilization and perception among internal medicine residents. J Gen Intern Med. 2021;36:1598–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Little A, Hampton Z, Gronowski T, Meyer C, Kalnow A. Podcasting in medicine: A review of the current content by specialty. Cureus. 2020;12:e6726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riddell J, Robins L, Brown A, Sherbino J, Lin M, Ilgen JS. Independent and interwoven: A qualitative exploration of residents’ experiences with educational podcasts. Acad Med. 2020;95:89–96. [DOI] [PubMed] [Google Scholar]
- 7.Estes M, Gopal P, Siegelman JN, Bailitz J, Gottlieb M. Individualized interactive instruction: A guide to best practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2019;20:363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvard Medical School. Digital education: Twitter, podcasts, visuals, and beyond. https://cmeregistration.hms.harvard.edu/events/digital-education-twitter-podcastsvisuals-and-beyond/event-summary-eb029f12d6ec43d5a48a8ef7d47c876b.aspx?dvce=1. Accessed November 4, 2021.
- 9.Dzara K, Gooding H. A guide to educational pyramids commonly used in medical education programs. Acad Med. 2022;97:313. [DOI] [PubMed] [Google Scholar]
- 10.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- 11.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–146. [DOI] [PubMed] [Google Scholar]
- 12.Kirkpatrick D. Evaluating Training Programs. Madison, WI: American Society for Training and Development; 1975. [Google Scholar]
- 13.Childers RE, Dattalo M, Christmas C. Podcast pearls in residency training. Ann Intern Med. 2014;160:70. [DOI] [PubMed] [Google Scholar]
- 14.Chin A, Helman A, Chan TM. Extracurricular podcast use behaviour and effect on knowledge retention in undergraduate medical students. CJEM. 2016;18(suppl 1):S86. [Google Scholar]
- 15.Chin A, Helman A, Chan TM. Podcast use in undergraduate medical education. Cureus. 2017;9:e1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clarke CGD, Nnajiuba U, Howie J, Khan M, Pinto Dos Santos D, Ranschaert E. Giving radiologists a voice: A review of podcasts in radiology. Insights Imaging. 2020;11:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cosimini MJ, Espinoza J. Telephone management training by podcast—Length and content considerations. Acad Pediatr. 2017;17:e9–e10. [Google Scholar]
- 18.Cosimini MJ, Cho D, Liley F, Espinoza J. Podcasting in medical education: How long should an educational podcast be? J Grad Med Educ. 2017;9:388–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coughlin TA, Jones KI, Lund JN, Clement RG, Longman CL, Jones K. The uptake of podcasting and portable media players amongst UK medical students. Med Teach. 2011;33:85. [DOI] [PubMed] [Google Scholar]
- 20.De Los Reyes S, Cholakian D, Chau D, Forde B, Johnson C, Bienstock J. Education on the go: Studying the use of podcasts in resident education. Obstet Gynecol. 2017;130(suppl 1):47S. [Google Scholar]
- 21.Dryden A, Hilner J, Forgie S. Teaching and reviewing bacteriology with short, innovative podcasts. Int J Antimicrob Agents. 2009;34(suppl 2):S123–S124. [Google Scholar]
- 22.Dubin JM, Greer AB, Patel P, et al. International comparative study of the roles and attitudes towards social media in urology trainees. Eur Urol Open Sci. 2020;19(suppl 2):e2000–e2001. [Google Scholar]
- 23.Duong D, Oyama L, Smith J, Spector J, Narang A. Attitudes of medical students on their instruction of the emergency medicine oral case presentation. SAEM Abstracts, Plenary Session. Acad Emerg Med. 2011;18(suppl 1):S52. [Google Scholar]
- 24.Freed NA, Langlois BK, Mitchell PM, Schechter-Perkins EM, Eliseo LJ. Use of free open access medical education among EM residents and attendings at Boston Medical Center. Abstracts of the SAEM 2014 Annual Meeting. Acad Emerg Med. 2014;21(suppl 5):S69. [Google Scholar]
- 25.Friedman MA, Adjei N, Wenstrom K. Modern learning: How today’s obstetrics and gynecology residents gain knowledge. Obstet Gynecol. 2017;129:93S. [Google Scholar]
- 26.Fu D, Shepherd L, Chahine S. Podcasting can improve clinical clerks’ ability to generate differential diagnosis for an ED patient presentation. Can J Emerg Med. 2015;17(suppl 2):S10. [Google Scholar]
- 27.Gallagher J, Kenwright D, Abels P, Gallagher P. Is obstetrics and gynaecology going the distance? Clin Teach. 2012;9: 243–247. [DOI] [PubMed] [Google Scholar]
- 28.Grace PM, Aust Z, Belcher C, Desai S. Residents in emergency medicine comparative survey on technology. Abstracts of the SAEM 2017 Annual Meeting. Acad Emerg Med. 2017;24(suppl 1):S186. [Google Scholar]
- 29.Gutmann J, Kühbeck F, Berberat P, Fischer M, Engelhardt S, Sarikas A. How do “digital natives” learn pharmacology? A mixed-methods study on the use of learning media by undergraduate medical students. Naunyn Schmiedebergs Arch Pharmacol. 2014;387:S45. [Google Scholar]
- 30.Henley J, Amir M, Sampson B, Tamai JM, Dellavalle RP. Dermatology podcasting: An untapped resource for continuing education. J Am Acad Dermatol. 2013;68:513–515. [DOI] [PubMed] [Google Scholar]
- 31.Herrmann FE, Lenski M, Steffen J, et al. A survey study on student preferences regarding pathology teaching in Germany: A call for curricular modernization. BMC Med Educ. 2015;15:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson AP, Rich NC, Kniery K, et al. Audible bleeding, the vascular surgery podcast: Affecting the practice of vascular surgery. J Vasc Surg. 2020;72:e57. [Google Scholar]
- 33.Ko P, Sarsfield M, Welch K, Grant W. Introducing FOAM (free open access medical education) to fourth-year medical students: A self-directed learning and critical reflection project. Acad Emerg Med. 2015;22(suppl 1):S448. [Google Scholar]
- 34.Kuhlmann E, Simpson K. What is the internal medicine resident’s perspective on using podcasts to enhance critical care medicine education? Am J Respir Crit Care Med. 2013;187:A2819. [Google Scholar]
- 35.Lee T, Rosen C. Curricular and co-curricular social media-based learning during medical school. West J Emerg Med. 2017;18:S9. [Google Scholar]
- 36.Levy JB, Braude P. Are podcasts useful in postgraduate medical education? Med Educ. 2011;45(suppl 2):19. [Google Scholar]
- 37.Lien K, Chin A, Helman A, Chan TM. A randomized comparative trial of the knowledge retention and usage conditions in undergraduate medical students using podcasts and blog posts. Cureus. 2018;10:e2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malecki SL, Quinn KL, Zilbert N, et al. Understanding the use and perceived impact of a medical podcast: Qualitative study. JMIR Med Educ. 2019;5:e12901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matava CT, Rosen D, Siu E, Bould DM. eLearning among Canadian anesthesia residents: A survey of podcast use and content needs. BMC Med Educ. 2013;13:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCarthy J, Porada K. Serving up Peds Soup: Podcast-based paediatric resident education. Med Educ. 2020;54:456–457. [DOI] [PubMed] [Google Scholar]
- 41.Nwosu AC, Monnery D, Reid VL, Chapman L. Use of podcast technology to facilitate education, communication and dissemination in palliative care: The development of the AmiPal podcast. BMJ Support Palliat Care. 2017;7:212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Neill E, Power A, Stevens N, Humphreys H. Effectiveness of podcasts as an adjunct learning strategy in teaching clinical microbiology among medical students. J Hosp Infect. 2010;75:83–84. [DOI] [PubMed] [Google Scholar]
- 43.Block J, Lerwick P. 1064: Educational preferences among residents in the ICU. Crit Care Med. 2019;47:509. [Google Scholar]
- 44.Purdy E, Thoma B, Bednarczyk J, Migneault D, Sherbino J. The use of free online educational resources by Canadian emergency medicine residents and program directors. CJEM. 2015;17:101–106. [DOI] [PubMed] [Google Scholar]
- 45.Qian ET, Leverenz DL, McPherson JA, Kroop SF. An Internal medicine residency podcast: Impact on the educational experience and care practices of medical residents. J Gen Intern Med. 2021;36:1457–1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reid Burks A, Nicklas D, Owens J, Lockspeiser TM, Soranno D. Urinary tract infections: Pediatric primary care curriculum podcast. MedEdPORTAL. 2016;12:10434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reynolds TD, Marshall RW. Learning from our students: An exploration of student and teacher experiences in undergraduate rheumatology. Rheumatology. 2019;58(suppl 3):iii51–iii52. [Google Scholar]
- 48.Riddell J, Swaminathan A, Lee M, Mohamed A, Rogers R, Rezaie SR. A survey of emergency medicine residents’ use of educational podcasts. West J Emerg Med. 2017;18:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rodenberg C, Brewer K. Emergency medicine residents and attendings are using more non-traditional learning methods including podcasts, blogs, online videos and reading via computers or tablets. Acad Emerg Med. 2015;22(suppl 1):S361. [Google Scholar]
- 50.Rosen D, Matava C, Siu E, Bould D. Podcast educational needs assessment survey of Canadian anaesthesia residents. Anaesth Intensive Care. 2011;39:966. [Google Scholar]
- 51.Roth J, Chang A, Ricci B, Hall M, Mehta N. Why not a podcast? Assessing narrative audio and written curricula in obstetrical neurology. J Grad Med Educ. 2020;12:86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sandars J, Schroter S. Web 2.0 technologies for undergraduate and postgraduate medical education: An online survey. Postgrad Med J. 2007;83:759–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shekarchi A, Gordon B, Liu J. Using podcasts in place of clinic talks for graduate medical education at a multi-site residency program. Pediatrics. 2018;142:620. [Google Scholar]
- 54.Boothe-LaRoche A, Belay B, Sharma AJ. Pregnancy and postpartum related weight counseling practices of U.S. obstetrician-gynecologists: Results from the Doc Styles survey, 2010. J Womens Health Care. 2014;3:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sherbino J, Upadhye S, Worster A. Self-reported priorities and resources of academic emergency physicians for the maintenance of clinical competence: A pilot study. CJEM. 2009;11:230–234. [DOI] [PubMed] [Google Scholar]
- 56.Tamas MJ, Mcintosh AC, Carbonara A, Weinman SA. Longitudinal preferences in the format of continuing medical education (CME) activities in diabetes, 2006–2011. Diabetes. 2013;62(S1):A623. [Google Scholar]
- 57.Tarchichi TR, Szymusiak J. Continuing medical education in an on-demand world: Is podcasting the Netflix of medical education? Hosp Pediatr. 2019;9:818–819. [DOI] [PubMed] [Google Scholar]
- 58.Thurtle N, Banks C, Cox M, Pain T, Furyk J. Free open access medical education resource knowledge and utilisation amongst emergency medicine trainees: A survey in four countries. Afr J Emerg Med. 2016;6:12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Twigg V, Carr S, Harrison L, Quaraishi MS. A survey of continuing medical education amongst otolaryngologists in the UK. Int J Surg. 2016;36(suppl 1):S97. [Google Scholar]
- 60.Verma A, Naveed H, Razak F. Developing and evaluating The Rounds Table podcast for continuing medical education in general adult medicine. J Gen Intern Med. 2015;30(S2):S491. [Google Scholar]
- 61.Vogelsang M, Rockenbauch K, Wrigge H, Heinke W, Hempel G. Medical education for “Generation Z”: Everything online?!—An analysis of Internet-based media use by teachers in medicine. GMS J Med Educ. 2018;35:Doc21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Walkinshaw E. Medical podcasts going viral. CMAJ. 2011;183:1577–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Weinstock M, Pallaci M, Aluisio AR, et al. Effect of interpolated questions on podcast knowledge acquisition and retention: A double-blind, multicenter, randomized controlled trial. Ann Emerg Med. 2020;76:353–361. [DOI] [PubMed] [Google Scholar]
- 64.White JS, Sharma N, Boora P. Surgery 101: Evaluating the use of podcasting in a general surgery clerkship. Med Teach. 2011;33:941–943. [DOI] [PubMed] [Google Scholar]
- 65.Brust T, Yeung M. Clinical neuroscience podcasts for family medicine, internal medicine, and neurology residents: A needs assessment study. Neurology. 2014;82(suppl 10):P1.312. [Google Scholar]
- 66.Young KJ, Kim JJ, Yeung G, Sit C, Tobe SW. Physician preferences for accredited online continuing medical education. J Contin Educ Health Prof. 2011;31:241–246. [DOI] [PubMed] [Google Scholar]
- 67.Brust T, Cooke L, Yeung M. A randomized-controlled trial comparing efficacy and user satisfaction of audio podcasts versus a traditional lecture on multiple sclerosis in family medicine resident education. Neurology. 2015;84(suppl 14):P4.195. [Google Scholar]
- 68.Chartier LB, Helman AD. Development of a Canadian emergency medicine open-access podcast: The emergency medicine cases experience. Can J Emerg Med. 2015;17(suppl 2):S29–S30. [Google Scholar]
- 69.Chau D, Bowe E, Brown R, DiLorenzo A. Implementation of a comprehensive but simple method to manage and track resident knowledge and skill acquisition during pediatric anesthesia training: Impact on its first graduating class. Anesth Analg. 2012;114(suppl 5):S236. [Google Scholar]
- 70.Bragg D, Voll J, Maxwell-Armstrong C. Teaching medical documentation skills—An innovative method to improve patient care. Int J Surg. 2013;11:699. [Google Scholar]
- 71.Regmi K, Jones L. A systematic review of the factors—enablers and barriers—affecting e-learning in health sciences education. BMC Med Educ. 2020;20:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vaona A, Banzi R, Kwag KH, et al. E-learning for health professionals. Cochrane Database Syst Rev. 2018;1:CD011736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cadogan M, Thoma B, Chan TM, Lin M. Free Open Access Meducation (FOAM): The rise of emergency medicine and critical care blogs and podcasts (2002–2013). Emerg Med J. 2014;31:e76–e77. [DOI] [PubMed] [Google Scholar]
- 74.Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in emergency medicine. https://www.acgme.org/globalassets/pfassets/programrequirements/110_emergencymedicine_2021.pdf. Updated July 1, 2021. Accessed November 10, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.