Highlights
-
•
Integration of Advanced Practice Radiation Therapists (APRTs) within the multi-professional team enhances service delivery in radiation therapy (RT).
-
•
APRT goes beyond task shifting, using unique skills and innovation to enhance patient care.
-
•
Future APRT roles should be based on the level of practice, not the technology or an individual.
-
•
There is a need for standardisation of APRT through consensus, including education frameworks, levels of practice and career progression.
-
•
Challenges may be overcome through international collaboration and practice sharing across jurisdictions.
Keywords: Advanced practice, Radiation therapist, Radiation therapy, Role development
Abstract
The radiation therapy (RT) landscape is continuously evolving, necessitating adaptation in roles and responsibilities of radiation therapists (RTTs). Advanced Practice Radiation Therapists (APRTs) have taken on a proactive role in expanding services and assuming responsibilities within multi-professional teams.
A European Society for Radiotherapy and Oncology (ESTRO) brought geographically diverse and experienced RTTs together, to discuss how advanced practice (AP) in the RTT profession should be future-proofed and create a global platform for collaboration. Challenges in achieving consensus and standardisation of APRT was identified across jurisdictions, emphasising the importance of international collaboration.
Whilst highlighting the pivotal role of APRTs in driving innovation, improving patient care, and navigating the complexities of modern RT practice, this position paper presents outcomes and recommendations from the workshop. Discussions highlighted the need for standardised role definitions, education frameworks, regulatory support, and career development pathways to enable the advancement of APRT effectively. Increasing networks and collaboration is recommended to ensure APRTs can shape the future of RT.
Abstract
The radiation therapy (RT) landscape is continuously evolving, necessitating adaptation in roles and responsibilities of radiation therapists (RTTs). Advanced Practice Radiation Therapists (APRTs) have taken on a proactive role in expanding services and assuming responsibilities within multi-professional teams.
A European Society for Radiotherapy and Oncology (ESTRO) brought geographically diverse and experienced RTTs together, to discuss how advanced practice (AP) in the RTT profession should be future-proofed and create a global platform for collaboration. Challenges in achieving consensus and standardisation of APRT was identified across jurisdictions, emphasising the importance of international collaboration.
Whilst highlighting the pivotal role of APRTs in driving innovation, improving patient care, and navigating the complexities of modern RT practice, this position paper presents outcomes and recommendations from the workshop. Discussions highlighted the need for standardised role definitions, education frameworks, regulatory support, and career development pathways to enable the advancement of APRT effectively. Increasing networks and collaboration is recommended to ensure APRTs can shape the future of RT.
Background
Radiation Therapy (RT) is rapidly evolving and has become increasingly complex. Integration of novel techniques and advanced technology into clinical practice requires healthcare professionals to adapt their roles and responsibilities [1]. In the past decade, roles within RT have evolved from a clinician-led model to a multi-professional team (MPT) approach [2], [3].
The Advanced Practice Radiation Therapist (APRT) is an autonomous professional within the MPT who acts beyond the traditionally defined radiation therapist (RTT) scope of practice (SOP) [4], [5], [6], [7]. APRTs work safely within an advanced, extended, but defined SOP, routinely involved in all aspects of the pathway. APRT actively develop services and adopt tasks traditionally fulfilled by other members of the oncology MPT. This task-shifting approach has been conceptualised under the implementation of APRT to meet service demands, addressing perceived or known gaps in the RT pathway [2].
In 2019, the European Society for Radiotherapy and Oncology (ESTRO) Radiation Therapist committee (RTTC) presented an overview of the evidence for APRT and delivered the ESTRO RTTC position on the future of advanced practice (AP) for the RTT profession [4]. Although similar APRT roles can be identified, many APRT positions are unique and developed in response to a specific service need [8], [9]. The visibility of the overt and hidden impacts of these roles should be promoted and showcased, to drive RT service delivery [2], [3], [4], [7], [8], [9], ensuring stakeholder support which is essential for sustainability.
As a professional group, it is essential for APRTs to be equipped with critical thinking skills [5], allowing the adaption of APRT roles in response to ongoing changes in the scientific landscape, technology, and service needs. Task shifting through APRT roles is not the replacement of medical colleagues alone. Rather it maximises the potential for the APRT to use their specialised training and expertise, enhancing efficiency and effectiveness in performing tasks. For the profession, it presents opportunities for career development, professional progression, and recruitment and retention, especially when there is thoughtful and deliberate adoption of the APRT framework, in conjunction with intentionality [2], [10], [11].
Against this background, a need to bring together RTTs working across a wide spectrum of practice and geographical variance were identified to discuss how the RTT profession should be future-proofed and create a global platform for collaboration. This resulted in the ESTRO 2022 RTT workshops entitled, “RTT advanced practice and how it can change the future of radiotherapy”. This paper aims to present outcomes from these workshops. The objective was to establish recommendations and investigate potential enablers to facilitate APRT progression.
Workshop process & participant selection
ESTRO 2022 RTT workshops were designed to facilitate scientific collaborations and professional networking within the RTT community. Workshops were advertised on the ESTRO webpage and promoted on social media, inviting applications accompanied by a motivational statement. The workshop co-chairs (AD, HMcN, NH and YT) selected participants to form an APRT expert reference group (ERG), based on their motivational statements and the below RTT selection criteria:
-
•
Managers, APRTs and educators
-
•
Highly motivated to define the future of the RTT profession and underpinning education programmes.
-
•Interested in:
-
oextending the RTT scope of practice
-
odeveloping leadership, management, teaching and research skills
-
oan education and training framework for APRT
-
o
-
•
Greater than three years clinical experience was recommended.
The ESTRO 2022 RTT workshops were composed of two 2-hour virtual meetings held in November 2022 and February 2023 (Fig. 1). Prior to the launch of workshops, the APRT ERG members were provided with useful resources on APRT and asked to consider some questions and topics listed in Table 1.
Fig. 1.
Description of planned workshops.
Table 1.
Questions and statements asked of participants in preparation for the workshop.
| Questions & statements |
|---|
| a) Prepare 3–4 words to describe APRT. |
| b) In your opinion, should APRT be interpreted as the scope of practice of an individual or a level of practice? |
| c) In your experience, is it clear that AP is usually defined by role or technology? |
| d) Ideally, should APRT role development be driven by technology? |
| e) Post a question you have on unsolved APRT issues. |
| f) Insert 3–4 examples of future developments that AP roles are key to their success. |
Workshop part 1 (W1)
Attendees were APRT ERG members, with co-chairs acting as facilitators. It commenced with APRT ERG members responding to questions on an online polling platform (Table 1). Responses were anonymous, real-time and could be viewed by all APRT ERG members. This initiated live discussion and using the chat function. The APRT ERG was then split into 2 smaller subgroups to promote further in-depth discussion and collaboration with co-chairs.
After W1, a recording of the meeting and the chat discussion were accessed by individual co-chairs. Following familiarisation with the data, common, repetitive themes were extracted firstly by an individual approach, then agreed using a team consensus (Table 2).
Table 2.
Thematic framework regarding the description of APRT.
| Themes | Keywords | Supporting Quotes |
|---|---|---|
| Clinical Expertise |
- Autonomy - Specialisation - Competence |
“Need to not focus on specific areas, but look at levels of autonomy and levels of working across all 4 pillars” |
| “we need to describe the current AP roles in terms of transversal capabilities & specific competencies to work across all pillars of AP” | ||
| Decision-Making |
- Critical Thinking - Complex Decision-Making - Problem-Solver |
“Other than AI, ART and automation, what else will shape the future of RT for the RTT. Answer: Clinical Decision Making ” |
| “APRT you must do original work - new ways of working, new ways of thinking” | ||
| Leadership |
- Influence - Innovative Leadership - Agent of Positive Change |
“Assisting other setups of AP roles” |
| “Ensure adhere to 4 pillars including research and leadership as key components” | ||
| Innovation | - Resourceful | “Research, development and education should be built into APRT role” |
| - Multi-disciplinary | “Through the practice of the 4 pillars of AP. Research will create new knowledge” | |
| - Proactive and continuous | “Collaborative initiatives with own profession, and other professionals” |
To ensure consistency and coherence, all APRT ERG members were contacted, detailing a summary of W1, and themes. This allowed opportunity for discussion, revisions and refinement before virtual workshop part 2 (W2), reducing unconscious bias of the co-chairs.
In W2, common themes identified from W1 were presented to the APRT ERG. A panel discussion was conducted regarding potential enablers for driving forward APRT that go beyond pre-defined roles. The APRT ERG used workshop outcomes in the development of this paper, with a draft manuscript written and co-authored by the co-chairs and APRT ERG members who expressed interest in joining the writing group. This resulted in a fully collaborative approach, approved by all authors.
Workshop outcomes
Nineteen RTTs submitted applications, of which 17 were selected to participate based on meeting the defined criteria. The APRT ERG was composed of 21 RTTs from the United Kingdom (6), Canada (4), Australia (3), Ireland (2), the Netherlands (2), Switzerland (2), Portugal (1) and Malta (1).
Workshop part 1 (W1)
Clarification of APRT
Themes and keywords summarised by the co-chairs are described in Table 2. Answers emphasised 4 key themes: clinical expertise, decision-making, leadership, and innovation.
Of 17 respondents, 11 indicated that in their experience APRT roles had been developed according to level of practice, and not determined by any individual RTT scope of practice or tasks. They agreed this should be recommended for future APRT roles, expressing strong agreement that by formalising the role itself (and levels), would ensure improved sustainability. 20/21 (95 %) participants suggested that APRT role development should not be driven by a particular technology but related to the increased levels of responsibility and autonomy that extends their SOP.
Standardisation of APRT
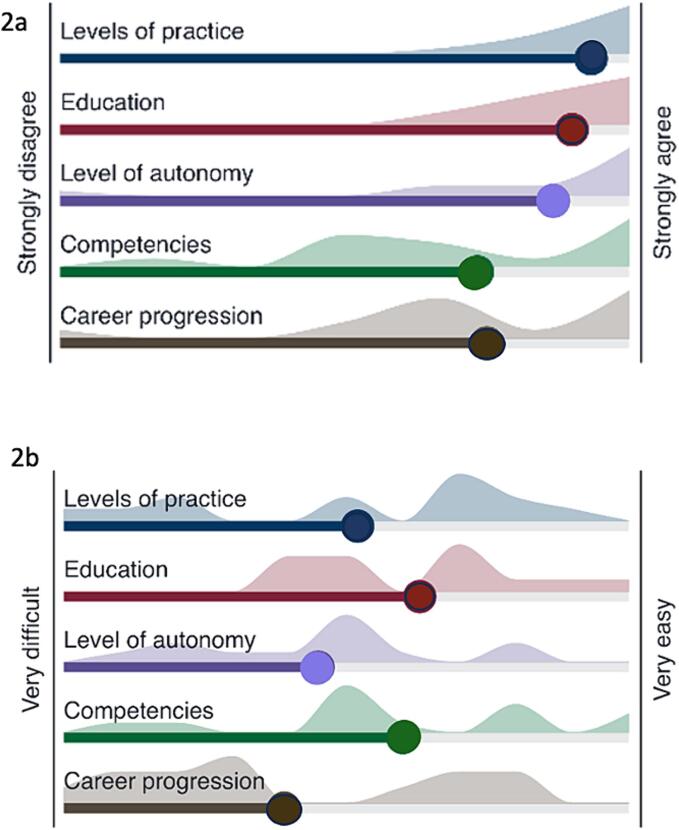
Participants level of agreement (on a scale from 1 (strongly disagree) to 7 (strongly agree) of which aspects of APRT need to be standardised, and which ones may be difficult to standardised are demonstrated in Fig. 2a and 2b. Issues related to standardising APRT, are described in Table 3.
Fig. 2.
a-b. Average agreement on what aspects need to be standardised (a), and level of how easy/difficult to standardise (b). Shading represents variation in answers.
Table 3.
Thematic framework concerning the standardisation of APRT.
| Themes | Issues | Relevance |
|---|---|---|
| Role Definitions |
How to standardise APRT roles? | Establishing clear and well-defined roles for APRT is a recurring theme. This clarity is seen as a crucial step in advancing the profession and ensuring that APRT roles are understood and recognized. |
| How to define advanced practice tasks? | ||
| How to concretely define APRT competencies? | ||
| How to differentiate enhanced practice from advanced practice? | ||
| What counts as advanced practice? | ||
| Training and Education |
What is the most effective framework for training and establishing APRT roles? | The importance of addressing issues related to training and education is emphasised. These include standardising education requirements, recognising different levels of APRT, demonstrating ways to develop these roles, and providing guidance to employers and colleagues. |
| How to determine effective training frameworks for establishing and growing APRT roles? | ||
| How to determine the optimal blend of clinical and academic components in APRT training? | ||
| Regulatory and Funding Challenges |
How to overcome regulatory barriers that hinder APRT? | This theme displays the identification of solutions to barriers and the exploration of future roles within APRT. This involves considering the needs and aspirations of various stakeholders. |
| How to get buy-in from multi-professional team and management teams to support and develop APRT roles? | ||
| How to secure funding for specific APRT roles and national practice agreements? | ||
| Succession and Career Development | How to address the importance of APRT succession planning? | It highlights the need to address APRT career progression within a standardised framework. Research should be significantly embedded in APRT roles, with a focus on its integration, dissemination, collaboration, and impact on patient care and service improvement. |
| How to address career development beyond APRT? |
Workshop part 2 - enablers for driving forward APRT
Role definitions
Challenges in defining and understanding APRT were consolidated, including the lack of consensus on the APRT definition, the need for clarity in levels of practice, and the importance of advocacy and education to clarify its meaning and value within the profession. Particular emphasis was on the importance of having a consistent understanding of APRT and achieving some level of consensus within the RT community. It was proposed that developing consensus guidelines and establishing defined pillars of APRT e.g. a “European APRT framework” detailing progression pathways would be advantageous.
Training and education
The ERG agreed that APRT have a crucial role in adding to the body of knowledge, with suggestions that research is built into APRT roles, focussing on patient care, experience, and the impact of roles. Innovation (“original ideas”), providing education (“sharing work and knowledge”, “presentation and publication”) and collaboration (“building online communities”, “initiatives with our own profession and other MDT colleagues”) were cited as essential in ensuring APRT roles advance.
Regulatory and funding Challenges
The APRT ERG recommended there was a need for careful planning, adequate funding, governance, and support to integrate and sustain APRT roles effectively. Proactive planning, recognition, and evidence-based practices were identified to ensure the long-term success of these APRT roles with measurable impact. This theme incorporates various elements, including financial support and the professional integration, both crucial for advancing AP. These are intrinsically linked to the needs and aspirations of various stakeholders.
Succession and career development
Suggestions for succession planning of the APRT role referenced the necessity of the wider organisational support (“government and executive recognition”), “workforce planning”, and recommending integration of APRT into service-design as prospective opposed to “reactive”, i.e. “future-proofing” needs to be strategically embedded into service plans with clear expectations, be evidence-based, and have appropriate governance. There was group agreement that development of AP roles could improve retention.
Other than artificial intelligence or advanced radiotherapy, research and clinical trials; individualised and combined cancer treatment (“precision medicine in RT value-based healthcare”); and patient care (“survivorship”, “prehabilitation and late effects”) were suggested as potential APRT developments. On further discussion, the ERG recognised that the future of APRT should progress with a multifaceted picture of cancer care, defining research as an essential component. Future developments should optimise potential impact on patient-centred approaches, survivorship, multimodal treatments, precision medicine, community-based care, equity, whilst considering the evolving landscape of cancer treatment.
Discussion
This paper aligns with the ESTRO RTTC position paper, advocating for APRT adoption and acknowledging its positive impact on patient care throughout Europe [4]. Despite two decades or more of implementation (in some jurisdictions), workshops revealed ongoing variation in definitions and expectations, with no global consensus [2], [7]. This reflects the complexity of AP, which has been well described within nursing as “dynamic, complex, and situational”, with international efforts to enhance the understanding of AP roles ongoing [12]. Workshops outcomes, whilst highlighting challenges, can act as an incentive for the RTT profession to advance APRT. To aid this effort, recommendations are summarised in Table 4.
Table 4.
Summary of recommendations from workshop outcomes.
| Role Definitions: |
|
|
|
| Training and Education: |
|
|
| Regulatory and Funding Challenges: |
|
|
| Succession and Career Development: |
|
|
|
Contradictions in many jurisdictions stem from a lack of conceptual understanding of the APRT role, often leading to its adoption based on operational demand, rather than from a strategic priority. While APRTs frequently fulfil workforce deficits in a clinical area of practice, they also contribute additional skills at an advanced level of practice. APRTs bring new ways of thinking and innovative approaches to service delivery across clinical practice, education, leadership, and research [13]. However, challenges arise due to healthcare funding being attached to clinical provision, presenting regulatory challenges when expanding responsibilities beyond initial registration, impacting implementation.
Personalised RT is becoming the standard of care, with a progressive shift away from generalised protocols. RTTs evaluate the clinical and technical aspects of patient care prior to and during RT, making informed decisions on appropriate courses of action [5], [14], [15]. They play an irreplaceable role in the MPT, and comprehensive education and training must underpin their development, allowing delivery of safe, high-quality care [13]. APRTs rely on complex critical thinking and autonomous decision-making, essential in providing timely and accurate treatment delivery e.g. in stereotactic body RT and adaptive RT, where patient specific adaptations may be time sensitive [16].
The workshop determined that APRT development should focus on levels of responsibility, rather than specific technology, or individuals. APRT utilise expert knowledge, including academic education, clinical experience, and leadership skills, to lead the MPT [17]. They can lead research and quality initiatives, enabling broader professional insights and facilitate practice change [6], moving from a ‘task shifting’ mindset to one based on a ‘level of practice’ [9]. While England, has already incorporated this approach into advanced clinical practice framework [18], other countries across Europe are still in their infancy of formalising similar frameworks [8]. Contradictions in role expectation and lack of clarity of the role indicate that further guidance is necessary.
In addition to defining roles clearly, the APRT ERG considered standardised expectations in relation to education, career pathways, regulation and funding were important for the development of APRT. Although challenging to achieve, it is important to recognise the significance of standardisation for ensuring transparency of expectations and future growth [2], [3]. Previous discussions have outlined educational expectations for AP [19].
It was recognised that APRT is a higher level of practice demanding expert knowledge and experience, but the level of education required to achieve the APRT title was not clearly defined internationally [19]. As a consequence, implementation is often standalone rather than with a universal approach, creating difficulty in envisioning standardised roles.
Global funding and regulation is challenging due to cultural and economic diversity. Through international innovation and collaboration, impactful research provides the evidence base for APRT role requirements [20], [21]. Culture change within a service necessitates evidence showcasing the benefit of APRTs. However, APRTs need to be enabled to undertake research, and as discussed, this should be part of the APRT role, supported by job plans. Research is often the weakest aspect due to lack of skills and confidence; therefore, entities such as the collaborative Advanced Practice Radiation Therapy International Community of Practice (APRT ICoP) group are important enablers. Currently, the APRT ICoP has more than 70 members from 17 different countries. Working with stakeholders to affirm and promote APRT role identity, it aims to influence increasing APRT utilisation in cancer care systems; and provides an accessible mechanism for APRTs to share knowledge and provide mentorship. Collaborative groups allow a supportive environment for research development, allowing co-design and co-elevation of ideas, bringing them to fruition and motivating APRTs to undertake and disseminate impactful research.
Conclusions
Fundamentally, implementing APRT is complex and nuanced. Although earlier position papers have made explicit the definition for APRT and education expectations [4], [19], there remains uncertainty in effectively operationalising APRT within a service, while remaining agile to the changing practice landscape. Acknowledging that some uncertainties are difficult to overcome, there is clear evidence demonstrating positive impact. The profession must work together internationally to advocate for APRT, embracing the complexities and collaborating for maximum impact.
Given the fluid development of APRTs globally, recommendations from this paper should be enablers for change. Implementation of the ICoP represents a positive step, with opportunities for individuals to collaborate, and address research. Work on impact should go beyond patient metrics and consider the educational, leadership and research benefits on the service. Empowering current APRTs as trailblazers, supported by the wider community, a cultural shift can enable APRTs to reach their full potential internationally, positively impacting the lives of patients.
Author contributions
Conceptualization: Aileen Duffton, Yatman Tsang, Helen McNair, Nicole Harnett. Methodology: Aileen Duffton, Yatman Tsang, Helen McNair, Nicole Harnett. Validation: Aileen Duffton, Yat Tsang, Nicole Harnett, Helen A McNair, Erica Bennett, Melanie Clarkson, Jose Guilherme Couto, Gavin Lawler, Kristie Matthews, Celeste Oliveira, Natalie Rozanec, Rita Simões. Formal analysis: Aileen Duffton, Yat Tsang, Celeste Oliveira, Gavin Lawler. Investigation: Aileen Duffton, Yat Tsang. Resources: Aileen Duffton, Yat Tsang. Data curation: Aileen Duffton, Yat Tsang. Writing – original draft: Aileen Duffton, Yat Tsang. Writing – review & editing: Aileen Duffton, Yat Tsang, Nicole Harnett, Helen A McNair, Erica Bennett, Melanie Clarkson, Jose Guilherme Couto, Gavin Lawler, Kristie Matthews, Celeste Oliveira, Natalie Rozanec, Rita Simões. Visualization: Aileen Duffton, Yat Tsang, Nicole Harnett, Helen A McNair, Erica Bennett, Melanie Clarkson, Jose Guilherme Couto, Gavin Lawler, Kristie Matthews, Celeste Oliveira, Natalie Rozanec, Rita Simões. Supervision: Aileen Duffton, Yatman Tsang. Project administration: Aileen Duffton, Yatman Tsang, Celine De Champs. Funding acquisition: ESTRO.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank all workshop participants for their contributions Kaj Bailey, Shazad Ahmed Bhutto, Lucy Buckley, Mairead Daly, Rebecca Height, Jenneke Jacobs, Elizabeth Joyce, Shanna Roosenthaler, Eva Van Weerd. Participation was voluntary and consent was implied through the application to participate. Personal data enabled communication and participation and were accessible to the group to allow professional discussion. Each workshop was recorded with permission from all participants.
Aileen Duffton is supported by the Beatson Cancer Charity and CRUK RadNet Glasgow. Rita Simões is a clinical doctoral research fellow funded by Higher Education England (HEE) and the National Institute for Health and Care Research (NIHR), award number CDR-2018-04-ST2-004.
References
- 1.Vandewinckele L., Claessens M., Dinkla A., Brouwer C., Crijns W., Verellen D., et al. Overview of artificial intelligence-based applications in radiotherapy: recommendations for implementation and quality assurance. Radiother Oncol. 2020;153:55–66. doi: 10.1016/j.radonc.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Tsang Y., Harnett N. Advanced practice in radiotherapy: how to move to the next level? Technical Innovations & Patient Support in Radiation Oncology. 2021;1(17):57–58. doi: 10.1016/j.tipsro.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matthews K., Duchesne G., Baird M. Navigating uncertainty: the implementation of australian radiation therapy advanced practitioners. Technical Innovations & Patient Support in Radiation Oncology. 2021;1(17):82–88. doi: 10.1016/j.tipsro.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duffton A., Devlin L., Tsang Y., Mast M., Leech M. Advanced practice: an ESTRO RTTC position paper. Tech Innov Patient Support Radiat Oncol. 2019;10:16–19. doi: 10.1016/j.tipsro.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lavergne C., Rozanec N., Harnett N. The palliative clinical specialist radiation therapist: a CAMRT white paper. Journal of Medical Imaging and Radiation Sciences. 2021;52(4):636–649. doi: 10.1016/j.jmir.2021.08.016. [DOI] [PubMed] [Google Scholar]
- 6.Linden K., Renaud J., Zohr R., Gaudet M., Haddad A., Pantarotto J., et al. Clinical specialist radiation therapist in palliative radiation therapy: report of an orientation, training, and support program. Journal of Medical Imaging and Radiation Sciences. 2019;50(4):543–550. doi: 10.1016/j.jmir.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira C., Barbosa B., Couto J.G., Bravo I., Khine R., McNair H. Advanced practice roles of therapeutic radiographers/radiation therapists: a systematic literature review. Radiography (Lond) 2022;28(3):605–619. doi: 10.1016/j.radi.2022.04.009. [DOI] [PubMed] [Google Scholar]
- 8.Oliveira C., Barbosa B., Couto J.G., Bravo I., Hughes C., McFadden S., et al. Advanced practice roles amongst therapeutic radiographers/radiation therapists: a european survey. Radiography. 2023;29(2):261–273. doi: 10.1016/j.radi.2022.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Rozanec N., Lavergne C., Harnett N. A Canadian experience of palliative advanced practice radiation therapy TIPS: training, implementation, practice and sustainability. Tech Innov Patient Support Radiat Oncol. 2021;18(17):89–96. doi: 10.1016/j.tipsro.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hooks C., Walker S. An exploration of the role of advanced clinical practitioners in the east of England. Br J Nurs. 2020;29(15):864–869. doi: 10.12968/bjon.2020.29.15.864. [DOI] [PubMed] [Google Scholar]
- 11.Wood E., King R., Robertson S., Senek M., Tod A., Ryan T. Sources of satisfaction, dissatisfaction and well-being for UK advanced practice nurses: a qualitative study. J Nurs Manag. 2021 Jul 1;29(5):1073–1080. doi: 10.1111/jonm.13245. [DOI] [PubMed] [Google Scholar]
- 12.Brykczynski C.L. Role development of the advanced practice nurse. Hamric & Hanson's Advanced Practice Nursing-E-Book: Hamric & Hanson's Advanced Practice Nursing-E-Book. 2022 Aug;5:98. [Google Scholar]
- 13.Khine R.N.M., Stewart-Lord A. An examination of advanced clinical Practice: qualitative insights from therapeutic radiography advanced and consultant practitioners based in England. Technical Innovations & Patient Support in Radiation Oncology. 2021;17 doi: 10.1016/j.tipsro.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coffey M., Leech M., Poortmans P. Benchmarking radiation TherapisT (RTT) education for safe practice: the time is now. Radiother Oncol. 2016;119(1):12–13. doi: 10.1016/j.radonc.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 15.Tsang Y.M., Routsis D.S. Adapting for adaptive radiotherapy (ART): the need to evolve our roles as therapeutic radiographers. Radiography. 2021 doi: 10.1016/j.radi.2021.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Erler D. CSRT in SBRT: who am I and what exactly do I do? Journal of Medical Imaging and Radiation Sciences. 2013;44(1):55. [Google Scholar]
- 17.Harnett N., Bak K., Zychla L., Gutierrez E., Warde P. Defining advanced practice in radiation therapy: a feasibility assessment of a new healthcare provider role in Ontario, Canada. Radiography. 2019;25(3):241–249. doi: 10.1016/j.radi.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 18.Health Education England (HEE). (2017). Multi professional framework for advanced clinical practice in England. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf.
- 19.Coffey M., Leech M. Introduction to the ESTRO european qualifications framework (EQF) 7 and 8: benchmarking radiation therapist (RTT) advanced education. Technical innovations & patient support in radiation oncology. 2018;1(8):19–21. doi: 10.1016/j.tipsro.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDonagh D., Tonning K.L., Freeman B., Birring E.J., Dimopoulos M., Harnett N., et al. An environmental scan of advanced practice radiation therapy in the United States: a PESTEL analysis. International Journal of Radiation Oncology* Biology* Physics. 2023;117(1):11–21. doi: 10.1016/j.ijrobp.2023.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Harnett N., Bak K., Lockhart E., Ang M., Zychla L., Gutierrez E., et al. The clinical specialist radiation therapist (CSRT): a case study exploring the effectiveness of a new advanced practice role in Canada. J Med Radiat Sci. 2018;65(2):86–96. doi: 10.1002/jmrs.281. [DOI] [PMC free article] [PubMed] [Google Scholar]