Abstract
This cohort study characterizes heterogeneity in cardiac function prior to sepsis and describes associations with hospitalization outcomes and mortality.
Between 2009 and 2014, 21% of US adults with sepsis did not survive.1 Guidelines recommend urgent resuscitation of patients with sepsis, although the ideal treatment regimen is not clear2 and challenges to resuscitation, including the management of sepsis-related cardiac dysfunction, remain.3 How preexisting cardiac disease is associated with outcomes is poorly understood. This study characterizes heterogeneity in cardiac function prior to sepsis and describes associations with hospitalization outcomes and mortality.
Methods
Unique patients hospitalized from January 2013 to December 2014 at 12 community and academic hospitals affiliated with UPMC were included in this cohort study, with follow-up through December 31, 2019. We identified patients with sepsis using the Third International Consensus Definitions in the first 6 hours of presentation.4 Transthoracic echocardiography (TTE) findings were linked to patient data for up to 12 months prior to the sepsis episode. Clinical data were abstracted and included demographics and comorbidities before sepsis.
Preexisting cardiac abnormalities were categorized as none, right ventricular (RV), left ventricular (LV), or biventricular (BV) dysfunction based on the presence of either moderate or severe impairment of ventricular function on the TTE (<40%). Characteristics of patients with vs without TTE were compared to assess selection bias. Among patients who underwent TTE, acute illness severity, maximum values of biomarkers of organ dysfunction in the first 6 hours, provision of organ support, intensive care unit (ICU) admission, ICU and hospital length of stay, and mortality at 28 days, 365 days, and 3 and 5 years were compared by type of preexisting cardiac dysfunction. Descriptive data were compared using analysis of variance, the Kruskal-Wallis test, and the χ2 test with a Bonferroni-adjusted (2-sided) significance level of P < .05, as appropriate. Mortality was evaluated with Kaplan-Meier curves, log-rank tests, and multivariable logistic regression adjusted for age and sex. All analyses used Stata, version 18.0 (StataCorp LLC). The University of Pittsburgh institutional review board approved this minimal risk study with a waiver of informed consent.
Results
Of 513 281 patients, 31 052 met sepsis criteria, of whom 4599 (15.0%) had TTE data (mean [SD] age, 68 [5] years; 2277 [49.50%] male; 3871 [84.2%] White) (Table). Patients with TTE data were not meaningfully different in demographics or sepsis presentation compared with those without TTE data.
Table. Characteristics Before and During Hospitalization for Sepsis and Mortality.
| Variable | No TTE performed | TTE performed | TTE performed in the 12 mo prior to sepsis | P valuea | |||
|---|---|---|---|---|---|---|---|
| No dysfunction | RV dysfunction alone | LV dysfunction alone | BV dysfunction | ||||
| No. of patients | 26 453 | 4599 | 3625 | 136 | 715 | 123 | |
| Age, mean (SD), y | 68 (17) | 68 (15) | 68 (15) | 71 (14) | 70 (15) | 71 (13) | <.001 |
| Sex, No. (%) | |||||||
| Female | 12 707 (48.0) | 2322 (50.5) | 1736 (47.9) | 61 (44.9) | 453 (63.4) | 72 (58.5) | <.001 |
| Male | 13 746 (52.0) | 2277 (49.5) | 1889 (52.1) | 75 (55.1) | 262 (36.6) | 51 (41.5) | |
| Race and ethnicity, No. (%)b | |||||||
| Black | 2752 (10.4) | 595 (12.9) | 462 (12.7) | 12 (8.8) | 106 (14.8) | 15 (12.2) | >.99 |
| White | 22 767 (86.1) | 3871 (84.2) | 3066 (84.6) | 120 (88.2) | 582 (81.4) | 103 (83.7) | |
| Other | 934 (3.5) | 133 (2.9) | 97 (2.7) | 4 (2.9) | 27 (3.8) | 5 (4.1) | |
| Characteristics before sepsis | |||||||
| Elixhauser Comorbidity Index, mean (SD)c | 1.0 (1.1) | 1.6 (1.3) | 1.5 (1.2) | 1.8 (1.3) | 2.0 (1.4) | 2.1 (1.4) | <.001 |
| Time from TTE until sepsis episode, mean (SD), d | NA | 111 (108) | 117 (109) | 104 (106) | 89 (100) | 74 (92) | <.001 |
| Sepsis episode | |||||||
| Surgery during hospitalization, No. (%) | 3521 (13.3) | 628 (13.7) | 492 (13.6) | 12 (8.8) | 100 (14.0) | 24 (19.5) | >.99 |
| SOFA score, median (IQR)d | 3.0 (2.0-4.0) | 4.0 (2.0-5.0) | 4.0 (2.0-5.0) | 4.0 (3.0-6.0) | 4.0 (3.0-5.0) | 4.0 (3.0-6.0) | .054 |
| SIRS criteria, median (IQR)e | 1.0 (0.0-2.0) | 2.0 (1.0-2.0) | 2.0 (1.0-2.0) | 2.0 (1.0-2.5) | 2.0 (1.0-2.0) | 2.0 (1.0-3.0) | .13 |
| Serum lactate, median (IQR), mmol/L | 1.5 (1.0-2.3) | 1.6 (1.1-2.6) | 1.6 (1.1-2.5) | 1.9 (1.2-3.2) | 1.7 (1.1-2.7) | 1.8 (1.1-3.6) | .003 |
| Serum creatinine, median (IQR), mg/dL | 1.2 (0.9-1.9) | 1.4 (0.9-2.5) | 1.4 (0.9-2.4) | 1.5 (0.9-2.3) | 1.6 (1.1-2.8) | 1.6 (1.1-2.5) | <.001 |
| Platelet count, median (IQR), ×103/μL | 193 (137-260) | 193 (132-264) | 194 (132-266) | 184 (127-246) | 191 (134-260) | 185 (132-241) | >.99 |
| INR, median (IQR) | 1.2 (1.1-1.6) | 1.3 (1.1-1.9) | 1.3 (1.1-1.8) | 1.4 (1.2-2.2) | 1.3 (1.1-2.0) | 1.5 (1.2-2.3) | <.001 |
| Total bilirubin, median (IQR), mg/dL | 0.7 (0.4-1.1) | 0.7 (0.4-1.2) | 0.7 (0.4-1.2) | 0.7 (0.5-1.2) | 0.8 (0.5-1.4) | 0.7 (0.5-1.4) | <.001 |
| Organ support during sepsisf | |||||||
| Vasopressors administered during hospital stay, No. (%) | 2280 (8.6) | 1198 (26.0) | 832 (23.0) | 45 (33.1) | 258 (36.1) | 63 (51.2) | <.001 |
| Mechanical ventilation given during hospital stay, No. (%) | 3444 (13.0) | 1483 (32.2) | 1114 (30.7) | 62 (45.6) | 257 (35.9) | 50 (40.7) | .001 |
| Health care use during sepsis | |||||||
| ICU admission during hospital stay, No. (%) | 7214 (27.3) | 3179 (69.1) | 2432 (67.1) | 107 (78.7) | 538 (75.2) | 102 (82.9) | <.001 |
| ICU length of stay, median (IQR), d | 4.0 (2.0-7.0) | 4.0 (3.0-8.0) | 4.0 (3.0-8.0) | 4.0 (3.0-9.0) | 4.0 (3.0-7.0) | 4.0 (3.0-8.0) | >.99 |
| Hospital length of stay, median (IQR), d | 5.0 (4.0-9.0) | 8.0 (5.0-13.0) | 8.0 (5.0-13.0) | 9.0 (6.0-13.5) | 8.0 (5.0-13.0) | 9.0 (6.0-14.0) | >.99 |
| Mortality at 28 d, No. (%) | 2552 (9.6) | 885 (19.2) | 642 (17.7) | 37 (27.2) | 175 (24.5) | 31 (25.2) | <.001 |
| Mortality at 365 d, No. (%) | 6954 (26.3) | 2052 (44.6) | 1546 (42.6) | 77 (56.6) | 365 (51.0) | 64 (52.0) | <.001 |
| Mortality at 3-y follow-up, No. (%) | 10 895 (41.2) | 2838 (61.7) | 2157 (59.5) | 102 (75.0) | 494 (69.1) | 85 (69.1) | <.001 |
| Mortality at 5-y follow-up, No. (%) | 12 325 (46.6) | 3084 (67.1) | 2352 (64.9) | 106 (77.9) | 532 (74.4) | 94 (76.4) | <.001 |
| Adjusted OR (95% CI) for mortalityg | |||||||
| At 28 d | NA | NA | 1 [Reference] | 1.63 (1.10-2.41) | 1.45 (1.19-1.76) | 1.50 (0.99-2.28) | NA |
| At 365 d | NA | NA | 1 [Reference] | 1.61 (1.13-2.30) | 1.31 (1.11-1.55) | 1.35 (0.94-1.95) | NA |
| At 3 y | NA | NA | 1 [Reference] | 1.86 (1.24-2.79) | 1.41 (1.19-1.70) | 1.38 (0.93-2.07) | NA |
| At 5 y | NA | NA | 1 [Reference] | 1.71 (1.12-2.62) | 1.47 (1.22-1.78) | 1.59 (1.03-2.46) | NA |
Abbreviations: ICU, intensive care unit; INR, international normalized ratio; NA, not applicable; OR, odds ratio; SIRS, systemic inflammatory response syndrome; SOFA, Sequential Organ Failure Assessment; TTE, transthoracic echocardiography.
SI conversion factors: To convert serum creatinine to micromole per liter, multiply by 88.4; platelet count to ×109/L, multiply by 1.0; and total bilirubin to micromoles per liter, multiply by 17.104.
Bonferroni-adjusted, omnibus P value comparing across 4 groups of patients for whom TTE was performed with no dysfunction as reference group, using analysis of variance, the Kruskal-Wallis test, and the χ2, as appropriate.
Derived from UPMC registration system data using fixed categories similar to the Centers for Medicare & Medicaid Services electronic health record meaningful use dataset. “Other” included American Indian or Alaska Native, Asian, Chinese, Filipino, Hawaiian or Other Pacific Islander, Middle Eastern, Native American, not specified, or Pacific Islander.
An overall measure of comorbidity burden derived from diagnostic codes at hospital discharge.
A measure of acute organ dysfunction, assessed across 6 organs, with scores ranging from 0 to 24, maximum score reached within 6 hours of sepsis episode.
A measure of systemic inflammation, ranging from 0 to 4, maximum score reached within 6 hours of sepsis episode.
At any time during hospitalization.
Adjusted for age and sex in multivariable logistic regression model, with no dysfunction as referent group.
Of patients with TTE data, 974 (21.2%) had preexisting cardiac dysfunction. Of these, 136 (14.0%) had RV dysfunction, 715 (73.4%) had LV dysfunction, and 123 (12.6%) had BV dysfunction. The type of preexisting cardiac dysfunction was not associated with acute sepsis severity (Table). Presenting Sequential Organ Failure Assessment and systemic inflammatory response syndrome criteria were not significantly different. Vasopressor support was more common for patients with RV, LV, or BV dysfunction than no dysfunction (RV, 33.1%; LV, 36.1%; BV, 51.2%; none, 23.0%; P < .001), as was admission to the ICU (RV, 78.7%; LV, 75.2%; BV, 82.9%; none, 67.1%; P < .001). Neither ICU nor hospital length of stay significantly differed.
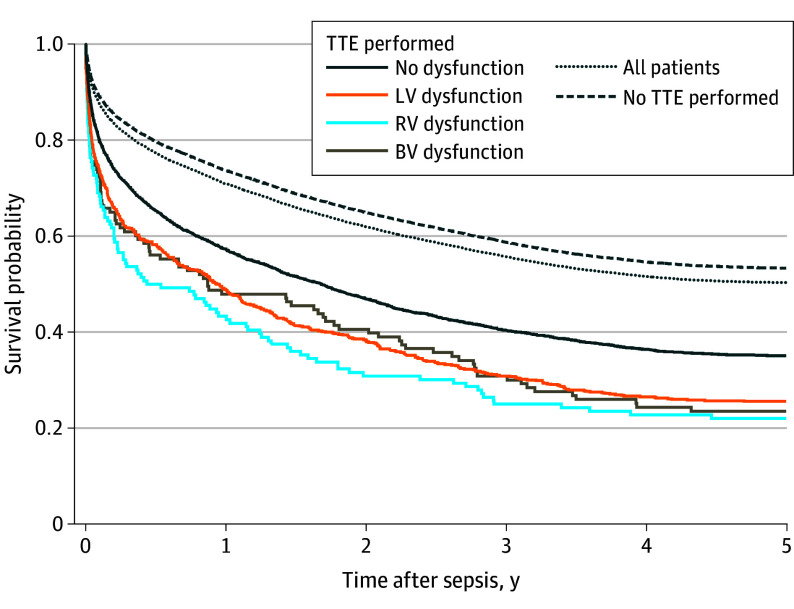
All-cause 28-day mortality was 9.6% for patients without TTE data and 19.2% for those with TTE data. Among those with TTE data, mortality was highest for patients with RV dysfunction (27.2%) and lowest for patients with no dysfunction (17.7%) (Figure). After controlling for age and sex, RV dysfunction (odds ratio [OR], 1.63; 95% CI, 1.10-2.41) and LV dysfunction (OR, 1.45; 95% CI, 1.19-1.76), but not BV dysfunction (OR, 1.50; 95% CI, 0.99-2.28), were associated with 28-day mortality (Table). Results were consistent at 365 days, 3 years, and 5 years, except for BV dysfunction, which became significant at 5 years.
Figure. Mortality Stratified by Type of Preexisting Cardiac Dysfunction During 5 Years After Sepsis Hospitalization.
Log-rank P < .001 for comparison across groups among whom TTE was performed. BV indicates biventricular; LV, left ventricular; RV, right ventricular; and TTE, transthoracic echocardiography.
Discussion
Despite similar clinical presentations and sepsis-related organ dysfunction, patients with preexisting cardiac dysfunction required greater organ support and admission to intensive care. Patients with LV or RV dysfunction had both higher short-term mortality and higher long-term mortality than patients with no cardiac dysfunction before sepsis.
Study limitations include that baseline TTE was not performed for all sepsis patients, leading to a potentially biased cohort due to selection. Results do not apply to cardiac dysfunction during the sepsis episode. Patients were enrolled a decade ago, but the interpretation of TTE data and sepsis care with early recognition and prompt antibiotics have not substantially changed. These data suggest that heterogeneity in cardiac function before sepsis may be associated with resuscitation and outcomes.
Section Editors: Kristin Walter, MD, and Jody W. Zylke, MD, Deputy Editors; Karen Lasser, MD, Senior Editor.
Data Sharing Statement
References
- 1.Rhee C, Dantes R, Epstein L, et al. ; CDC Prevention Epicenter Program . Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009-2014. JAMA. 2017;318(13):1241-1249. doi: 10.1001/jama.2017.13836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yealy DM, Kellum JA, Huang DT, et al. ; ProCESS Investigators . A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683-1693. doi: 10.1056/NEJMoa1401602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parker MM, Shelhamer JH, Bacharach SL, et al. Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med. 1984;100(4):483-490. doi: 10.7326/0003-4819-100-4-483 [DOI] [PubMed] [Google Scholar]
- 4.Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):762-774. doi: 10.1001/jama.2016.0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement