Abstract
Introduction:
The use of weight-inclusive programming within a workplace wellness context remains understudied.
Methods:
The present study is a pilot/feasibility study of a 3-month, virtual, weight-inclusive, intuitive eating-based workplace wellness program. Program participants (n = 114), who were all employees at a large public university in the Midwest, received weekly emails with a link to an instructional video related to intuitive eating and were encouraged to meet virtually with their health coach. Participants provided self-report data on behavioral and psychological outcomes including intuitive eating, internalized weight stigma, eating disorder symptoms, and diet quality at baseline, post-intervention (3 months from baseline), and follow-up (6 months from baseline). Changes in behavioral and psychological outcomes from baseline to post-intervention and follow-up were examined using paired t-tests, with Cohen’s d effect sizes reported. Generalized linear models were used to examine whether participant characteristics and program engagement were associated with program outcomes.
Results:
Increases in intuitive eating and decreases in internalized weight stigma and eating disorder symptoms were seen from baseline to post-intervention (Cohen’s d = 1.02, −0.47, and −0.63, respectively) and follow-up (Cohen’s d = 0.86, −0.31, and −0.60). No changes in dietary quality were seen at post-intervention, but a significant reduction in intake of added sugars, fast food, and sugar sweetened beverages were observed at follow-up (Cohen’s d = −0.35, −0.23, −0.25).
Conclusions:
This study provide preliminary support for the acceptability and potential impact of a weight-inclusive workplace wellness program that should be tested in a rigorous randomized trial.
Keywords: Workplace wellness, Intuitive eating, Weight-inclusive, Disordered eating, Weight stigma
1. Introduction
Approximately half of employers within the United States offer wellness programming to employees, with the goal of promoting engagement in health-enhancing behaviors and preventing disease (Mattke, Liu, Caloyeras, et al., 2013). The most commonly offered programs are those focused on nutrition and/or weight management (Mattke et al., 2013). Participation in these programs is often restricted to employees with high body weights and enrollment among eligible employees is low (Mattke et al., 2013). Effect sizes of dietary changes across studies of workplace nutrition and/or weight management programs have generally been small and variable (Ni Mhurchu, Aston, & Jebb, 2010), and changes in BMI have been modest with limited evidence of sustainable effects in the long term (Anderson, Quinn, Glanz, et al., 2009; Mattke et al., 2013). Further, recent research identifies workplace health promotion programs, particularly those that focus on weight reduction, as potential catalysts of weight stigma (Täuber, Mulder, & Flint, 2018a), which could diminish the potential health benefits of such programs. Taken together, existing nutrition-focused workplace wellness programming in the US may not be adequately addressing the full spectrum of nutrition-related health needs of employees who enroll (Jinnett et al., 2019; Miller & Jacob, 2001).
Weight-inclusive approaches to health promotion have been proposed as an alternative to weight-focused interventions (Tylka, Annunziato, Burgard, et al., 2014). These approaches do not focus on weight as an intervention target or weight loss as a program goal, but rather on behavioral and psychological targets such as intuitive eating (i.e., internally-regulated eating that is devoid of dieting behavior) and body acceptance (i.e., promoting positive body image, rejecting societal body ideals) (Mensinger, Calogero, Stranges, & Tylka, 2016; Tylka, 2006). This shift in focus away from weight as a primary indicator of health seen in weight-inclusive approaches is based on the recognition that health and well-being are multifaceted (Tylka et al., 2014). While weight-inclusive interventions are understudied to date, systematic reviews of weight-inclusive interventions have found that this approach is associated with positive changes in many domains of health, from physical to psychological, including blood lipids, blood pressure, depression, diet quality, disordered eating, and physical activity, independent of weight loss (Bacon & Aphramor, 2011; Clifford et al., 2015; Schaefer & Magnuson, 2014). An additional potential benefit of weight-inclusive programs in a workplace context is that they are accessible to employees of all body sizes, including anyone for whom a weight-focused program would be contraindicated.
Little research to date has examined who may be most likely to seek out weight-inclusive programming and for whom it may be most beneficial. However, weight-inclusive approaches that include intuitive eating are thought to be particularly well suited for individuals with a history of chronic dieting, weight cycling, and disordered eating, risk factors which are more common in higher weight individuals (Duncan, Ziobrowski, & Nicol, 2017; Nagata, Garber, Tabler, Murray, & Bibbins-Domingo, 2018; Täuber, Mulder, & Flint, 2018b; Tylka et al., 2014). Higher intuitive eating is consistently associated with fewer body image disturbances and lower disordered eating (Linardon, Tylka, & Fuller-Tyszkiewicz, 2021). For those with current or past disordered eating, intuitive eating may be beneficial in healing relationships with food and maintaining recovery (Koller, Thompson, Miller, Walsh, & Bardone-Cone, 2020). Indeed, intuitive eating has been proposed as a protective factor in the association between internalized weight stigma and behavioral sequelae such as lower engagement in physical activity and greater eating disorder pathology including binge eating (Braun, Unick, Abrantes, et al., 2022; Puhl & Suh, 2015). Those with a history of weight cycling may also benefit from weight-inclusive, intuitive eating-based approaches to nutrition, as intuitive eating has been linked to weight stability in a community sample (Tylka, Calogero, & Daníelsdóttir, 2020).
Given the limitations of existing nutrition-focused workplace wellness programs, the present pilot/feasibility study provides a unique opportunity to examine the potential impact of a weight-inclusive, intuitive eating-based workplace wellness program on behavioral and psychological outcomes. Specifically, we sought to examine changes in intuitive eating, internalized weight stigma, eating disorder symptoms, and diet quality among employees enrolled in a weight-inclusive, intuitive eating-based workplace wellness program. We further examined whether participant characteristics were associated with study retention, program satisfaction, and program engagement. Finally, we examined whether participant characteristics and program engagement were associated with changes in behaviors and psychological outcomes from baseline to post-intervention and follow-up. We hypothesized that program participants would experience an increase in intuitive eating, a decrease in both internalized weight stigma and eating disorder symptoms, and an improvement in diet quality while participating in our program. We expected that these changes would be greatest for the participants with higher levels of self-reported engagement in the program. We further hypothesized that program satisfaction would be higher among participants with a history of disordered eating and frequent dieting.
2. Methods
2.1. MHealthy nourish your whole self program
The University of Michigan offers employees workplace wellness programs, including nutrition programming, through its health and well-being initiative, MHealthy. A needs assessment was conducted in the summer of 2020 among past participants in MHealthy-sponsored nutrition programming, which revealed that weight cycling, chronic dieting, and disordered eating were common among past program participants (Sonneville et al., 2021). Based on the results of the needs assessment, MHealthy developed a new, weight-inclusive, intuitive eating-based program for employees. This program was created by a team of four registered dietitians at MHealthy and a dietetic intern. Content for this program was based on the 4th/current edition of Intuitive Eating, the Intuitive Eating Workbook, and the Intuitive Eating ProSkills training (Tribole, 2020; Tribole & Resch, 2017). The team created 11 modules for the program. The first module provided a general introduction to intuitive eating. The remaining 10 modules corresponded to the 10 principles of intuitive eating outlined in the 4th edition of Intuitive Eating: 1) Reject the Diet Mentality; 2) Honor Your Hunger, 3) Make Peace with Food; 4) Challenge the Food Police; 5) Discover the Satisfaction Factor; 6) Feel Your Fullness; 7) Cope with Your Emotions with Kindness; 8) Respect Your Body; 9) Movement—Feel the Difference; and 10) Honor Your Health with Gentle Nutrition (Tribole, 2020; Tribole & Resch, 2017). Each module included a 15-min instructional video, an accompanying slide deck, and activity handouts, as well as a list of intuitive eating resources. The content was designed to be delivered virtually and to allow for flexibility and autonomy regarding program components/engagement.
MHealthy began offering this weight-inclusive, intuitive eating-based program, Nourish Your Whole Self, in January 2021. Nourish Your Whole Self (NYWS) is a 3-month program led by MHealthy health coaches who have completed the Intuitive Eating PRO Skills Training and receive weekly supervision related to delivering an intuitive eating intervention. NYWS participants received weekly emails with a link to the instructional video corresponding to that week’s module, a copy of the slides, a PDF copy of any lesson materials/handouts, and their coach’s contact information. Participants were encouraged to meet virtually with their assigned coach weekly to discuss the current topic or any other dietary-related concerns, but were not required to do so. Outside of the optional coaching meetings, the program was delivered asynchronously. No group meetings were offered at the time of this study.
2.2. Study participants and procedures
The present study is a pilot/feasibility study funded by the Michigan Nutrition and Obesity Research Center (MNORC) conducted among University of Michigan employees enrolled in the MHealthy NYWS program. Study recruitment emails were sent to 350 employees who enrolled in the NYWS program between February 2021 and August 2021. Of the 350 program participants, 209 responded (response rate = 59.7 %) and were assessed for eligibility via a brief screener. Exclusion criteria for the study included current pregnancy, not being an employee of the University of Michigan, enrollment in a weight management program within 6 months prior to starting NYWS, and being under 18 years of age. Of the 209 employees who responded, 154 were deemed eligible, 53 were deemed ineligible, one did not complete the screener and one declined to participate. Of the 53 that were deemed ineligible, 46 had been enrolled in weight management programs in the past 6 months, 6 were not currently employees of the University of Michigan, and one was pregnant. After completing the screener, those eligible were sent an invitation to participate in the study. Of the 154 who were invited, 119 responded and consented to participate. Of the 119 individuals who provided consent, 114 participants completed all sections of the baseline survey and received $15 for completing the survey. Unique links to the follow-up surveys were automatically sent to each participant who completed the baseline survey at post-intervention (3.5 months from baseline) and follow-up (6.5 months from baseline). Participants who completed the post-intervention and follow-up survey received $25 and $35 incentives, respectively. No incentives were offered for completing NYWS program activities (e.g., watching a video, scheduling a coaching session).
A description of the sample size for each step of the study is shown in Fig. 1. All surveys were administered via the University’s REDCap database (Michigan Institute for Clinical & Health Research: UL1TR002240) (Harris, Taylor, Minor, et al., 2019). This study was approved by the University of Michigan Institutional Review Board (HUM00189600).
Fig. 1.
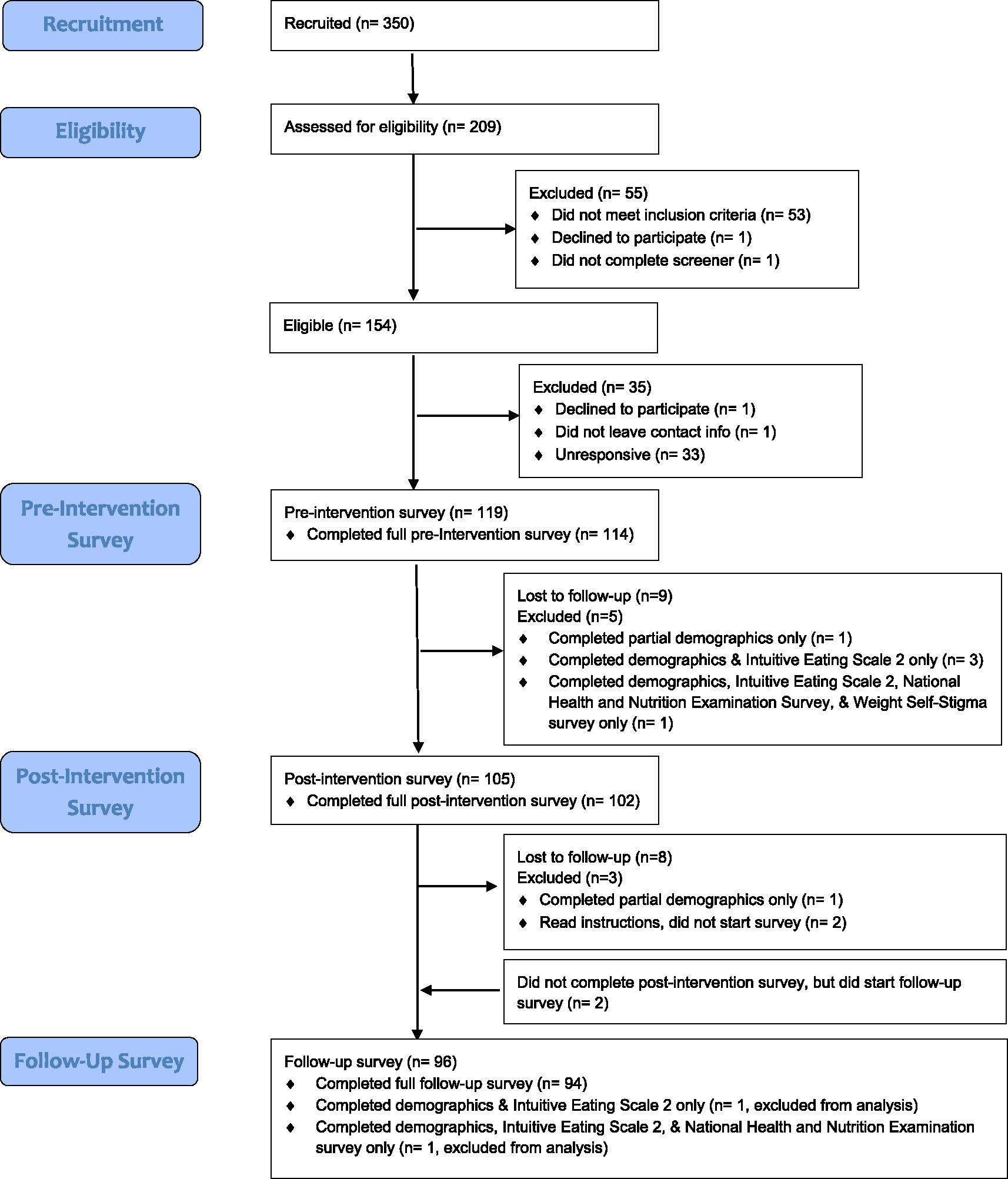
Consort diagram.
2.3. Measures
2.3.1. Participant characteristics
At baseline, study participants provided demographic data including age, gender identity, race/ethnicity, height, weight, highest educational attainment, and subjective social status. Subjective social status was assessed using MacArthur Scale of Subjective Social Status, where participants were asked to place themselves on a ladder with 10 rungs representing where they stand relative to other people in the United States (Adler, Epel, Castellazzo, & Ickovics, 2000; Cundiff, Smith, Uchino, & Berg, 2013). To create roughly equal size groups representing lower versus higher subjective social status, responses were dichotomized at the scale’s midpoint (1–5 vs 6–10). Self-reported height and weight were used to calculate each participant’s body mass index (BMI). Individuals with a BMI ≥ 30 were classified as having a larger body size.
Frequency of dieting and weight cycling was assessed using two items from the Brownell Weight Cycling Questionnaire (Foreyt et al., 1995). Frequency of dieting was assessed using the item, “How often are you dieting?” with the response options: never, rarely, often, always. This variable was categorized into frequent (“often” or “always” response) or infrequent (“rarely” or “never” response). Weight cycling was assessed using the item, “How many times in your life would you estimate you have lost more than 10 pounds?” with response options: 0, 1–5, 6–10, 11–15, 16–20, 21–25, 26 or more. While there is no standard of definition of what constitutes weight cycling, one previous study characterized 1–4 cycles as a “low number” of weight cycles (Stevens, Jacobs, Sun, et al., 2012). Accordingly, we categorized these into a binary variable representing participants with a history of weight cycling (>10 pound weight loss, 6 or more times) and those with low/no history of weight cycling (>10 pound loss, 0–5 times).
Self-reported eating disorder history was assessed with a single item from the Eating Disorder Screen for Primary Care (ESP) (Cotton, Ball, & Robinson, 2003) “Do you currently suffer with or have you ever suffered in the past with an eating disorder?” with response options: yes, no.
2.3.2. Study outcomes
At baseline, post-intervention, and follow-up, participants completed a series of questionnaires summarized below corresponding to the primary outcomes.
Current eating disorder symptoms were assessed using the Eating Disorder Examination Questionnaire-Short (EDE-QS), which is a 12-item version of the Eating Disorder Examination-Questionnaire (EDE-Q) that asks about eating disorder symptoms occurring over the past 7 days (Gideon et al., 2016). The EDE-QS uses a 4-point response scale, with a higher score indicating higher symptom levels. The continuous mean EDE-QS score was used to examine change in eating disorder symptoms from baseline to post-intervention and follow-up. In a sample of mostly young adult women, Prnjak et al. identified that a mean EDE-QS score of 1.2 (total score of 15) ensured the best trade-off between sensitivity (0.83) and specificity (0.85) (Prnjak, Mitchison, Griffiths, et al., 2020). Thus, we used a mean EDE-QS score of ≥1.2 to characterize high risk for an eating disorder at baseline.
Internalized weight stigma was assessed using the 12-item Weight Self-Stigma Questionnaire (WSSQ). Strong internal consistency (0.88), as well as acceptable test-retest reliability (0.79) of this questionnaire have been demonstrated in samples of high-weight adults (Lillis, Luoma, Levin, & Hayes, 2010). WSSQ scores were calculated as the sum of the 12 items.
Intuitive eating was assessed using the 23-item Intuitive Eating Scale-2 (IES-2). The IES-2 has been shown to be reliable and valid in college women and men (Tylka & Kroon Van Diest, 2013). Higher scores indicate higher levels of intuitive eating. IES-2 scores were calculated as the mean of all items (response options ranged from 1: strongly disagree to 5: strongly agree).
Dietary quality was assessed using the National Health and Nutrition Examination Survey (NHANES) Dietary Screener Questionnaire (DSQ) (Thompson, Midthune, Kahle, & Dodd, 2017). DSQ items were used to estimate intake of fruits, vegetables, dairy, added sugars, whole grains, fiber, calcium, and sugar sweetened beverages. An additional item was added to capture intake of plant-based milks such as oat milk, soy milk, and almond milk; intake of these products was included in the calculation of calcium intake. An additional item was also added to estimate intake of fast food (“During the past month, how many times did you buy food at a restaurant where food is ordered at a counter or at a drive-through window (there is no waiter/waitress)?”).
2.3.3. Study retention, program satisfaction, and program engagement
Study retention was defined as completion of the post-intervention survey, regardless of their level of participation in NYWS. On the post-intervention survey, participants who indicated any participation in NYWS were asked to report the number of videos they watched (0–10+) and the number of coaching sessions they attended (0–12+) while participating in the program. Items assessing program satisfaction and self-reported program engagement were also included in the post-intervention survey. Program satisfaction was assessed using a 1–10 scale (“with 1 being no satisfaction and 10 being full satisfaction”). Based on the distribution of responses, satisfaction was categorized as higher (response of 8 or higher) and lower (response of 7 or lower). Self-reported program engagement was also assessed using a 1–10 scale with a ≥8 versus ≤7 categorization.
2.4. Analysis
We examined means and frequencies for demographic data (age, race/ethnicity, gender identity, subjective social status, and educational attainment) and other baseline characteristics (BMI, self-reported eating disorder history, high eating disorder risk [mean EDE-QS score ≥ 1.2], weight cycling history [loss of 10 lbs 6+ times], frequent dieting [“often” or “always” dieting], and larger body size [BMI ≥ 30]). We report mean scores for intuitive eating (IES-2 scores), disordered eating (EDE-QS scores), internalized weight stigma (WSSQ scores), and measures of diet quality (intake of fruits, vegetables, dairy, added sugars, whole grains, fiber, calcium, fast food, and sugar sweetened beverages) from the baseline, post-intervention, and follow-up survey and examined changes in each of these measures using paired t-tests and Cohen’s d effect sizes.
We examined metrics of feasibility and acceptability including completion of the post-intervention survey (i.e., study retention), as well as program satisfaction (higher vs lower) and self-reported program engagement (higher vs lower) as assessed on the post-intervention survey. Chi-square or Fisher’s exact tests were used to determine whether study retention, program satisfaction, and program engagement were associated with participant characteristics including self-reported eating disorder history, high eating disorder risk, weight cycling history, frequent dieting, body size, subjective social status, and educational attainment. Generalized linear models were used to examine whether participant characteristics and program engagement were associated with study outcomes at follow-up. Analyses were performed using SAS version 9.4.
3. Results
3.1. Baseline characteristics
The study sample included 114 individuals who completed the informed consent and all sections on the baseline questionnaire (see Fig. 1). Demographic data and baseline characteristics of interest are shown in Table 1. Participants were given a “prefer not to answer” response option for all survey questions, which resulted in a small number of missing values. At baseline, scores on the IES-2, EDE-QS, and WSSQ ranged from 1.65 to 4.13, 0–2.17, and 12–59, respectively. The Cronbach’s alpha of the IES-2, EDE-QS, and WSSQ at baseline were 0.85, 0.77, and 0.89, respectively.
Table 1.
Baseline characteristics of study participants (n = 114).
| Mean (standard deviation) | ||
|---|---|---|
|
| ||
| Age (years) (n = 112) | 47.0 (12.6) | |
| BMI (kg/m2) (n = 113) | 30.7 (6.5) | |
|
| ||
| N (%) | ||
|
| ||
| Race/ethnicity | ||
| White | 91 (79.8 %) | |
| Black or African American | 7 (6.1 %) | |
| Asian | 4 (3.5 %) | |
| Hispanic, Latino, or Spanish origin | 2 (1.8 %) | |
| Middle Eastern or North African | 2 (1.8 %) | |
| American Indian or Alaska Native | 0 (0.0 %) | |
| Multiple races/ethnicities or other | 5 (4.4 %) | |
| Prefer not to answer | 3 (2.6 %) | |
| Gender identity | ||
| Cisgender female | 104 (91.2 %) | |
| Cisgender male | 4 (3.5 %) | |
| Non-binary or genderqueer | 1 (0.9 %) | |
| Prefer not to answer | 5 (4.4 %) | |
| Self-reported eating disorder history (n = 112) | 17 (15.2 %) | |
| High eating disorder risk | 45 (39.5 %) | |
| Weight cycling history | 39 (34.2 %) | |
| Frequent dieting | 55 (48.2 %) | |
| Larger body size (n = 113) | 51 (45.1 %) | |
| Higher subjective social status (n = 112) | 62 (55.4 %) | |
| Higher educational attainment | 52 (45.6 %) | |
High eating disorder risk: Eating Disorder Examination-Question Short score ≥ 1.2).
Weight cycling history: loss of 10 lbs 6+ times.
Frequent dieting: “often” or “always” (versus “rarely” or “never”).
Larger body size: body mass index ≥30.
Higher subjective social status: 6–10 rating on the Mac MacArthur Scale of Subjective Social Status (versus 1–5).
Higher educational attainment: advanced degree (versus less than an advanced degree).
3.2. Behavioral and psychological outcomes
Changes in intuitive eating, internalized weight stigma, current eating disorder symptoms, and measures of dietary quality among study participants from baseline to post-intervention and follow-up are shown in Table 2. Between baseline and post-intervention, study participants’ mean IES-2 scores increased, their WSSQ scores decreased, and their EDE-QS scores decreased. Their IES-2, WSSQ, and EDE-QS scores remained significantly different from baseline at follow-up, albeit attenuated relative to post-intervention for all three measures.
Table 2.
Change (unadjusted) in intuitive eating, internalized weight stigma, eating disorder symptoms, and measures of diet quality from baseline to post-intervention (n = 102) and follow-up (n = 94).
| Measure | Mean (standard deviation) | Mean difference in change from baseline (95 % confidence interval) | p-Value | Cohen’s d |
|---|---|---|---|---|
|
| ||||
| Intuitive eating | ||||
| Baseline | 2.80 (0.50) | |||
| Post-intervention | 3.35 (0.60) | 0.57 (0.45, 0.68) | <0.0001 | 1.02 |
| Follow-up | 3.28 (0.65) | 0.50 (0.38, 0.61) | <0.0001 | 0.86 |
| Internalized weight stigma | ||||
| Baseline | 36.28 (10.27) | |||
| Post-intervention | 31.67 (9.94) | −4.73 (−6.09, −3.37) | <0.0001 | −0.47 |
| Follow-up | 32.84 (11.05) | −3.28 (−4.89, −1.67) | <0.0001 | −0.31 |
| Eating disorder symptoms | ||||
| Baseline | 1.07 (0.47) | |||
| Post-intervention | 0.75 (0.49) | −0.30 (−0.38, −0.22) | <0.0001 | −0.63 |
| Follow-up | 0.78 (0.50) | −0.29 (−0.37, −0.20) | <0.0001 | −0.60 |
| Fruits (cup equivalents) | ||||
| Baseline | 0.97 (0.37) | |||
| Post-intervention | 0.99 (0.37) | 0.02 (−0.04, 0.08) | 0.48 | 0.06 |
| Follow-up | 0.95 (0.38) | −0.01 (−0.07, 0.06) | 0.86 | −0.02 |
| Vegetables (cup equivalents) | ||||
| Baseline | 1.50 (0.40) | |||
| Post-intervention | 1.57 (0.44) | 0.05 (−0.03, 0.13) | 0.19 | 0.12 |
| Follow-up | 1.55 (0.41) | 0.02 (−0.06, 0.10) | 0.63 | 0.05 |
| Dairy (cup equivalents) | ||||
| Baseline | 1.49 (0.39) | |||
| Post-intervention | 1.53 (0.61) | 0.04 (−0.07, 0.16) | 0.45 | 0.08 |
| Follow-up | 1.46 (0.42) | −0.04 (−0.11, 0.03) | 0.27 | −0.10 |
| Added sugars (teaspoon equivalents) | ||||
| Baseline | 14.24 (3.91) | |||
| Post-intervention | 13.54 (2.87) | −0.58 (−1.21, 0.04) | 0.067 | −0.17 |
| Follow-up | 12.95 (2.61) | −1.21 (−1.88, −0.54) | <0.001 | −0.35 |
| Whole grains (ounce equivalents) | ||||
| Baseline | 0.73 (0.29) | |||
| Post-intervention | 0.73 (0.29) | −0.003 (−0.05, 0.05) | 0.92 | −0.01 |
| Follow-up | 0.73 (0.29) | −0.00006 (−0.06, 0.06) | 0.99 | 0.00 |
| Fiber (grams) | ||||
| Baseline | 16.43 (2.89) | |||
| Post-intervention | 16.55 (2.80) | 0.03 (−0.38, 0.44) | 0.88 | 0.01 |
| Follow-up | 16.32 (2.84) | −0.16 (−0.62, 0.29) | 0.48 | −0.06 |
| Calcium (milligrams) | ||||
| Baseline | 917.79 (138.44) | |||
| Post-intervention | 932.02 (190.02) | 13.55 (−20.66, 47.76) | 0.43 | 0.08 |
| Follow-up | 910.04 (145.53) | −10.97 (−32.91, 10.98) | 0.32 | −0.08 |
| Sugar sweetened beverages (servings/week) | ||||
| Baseline | 4.59 (2.33) | |||
| Post-intervention | 4.42 (1.92) | −0.14 (−0.54, 0.26) | 0.49 | −0.06 |
| Follow-up | 4.16 (1.06) | −0.47 (−0.92, −0.03) | 0.037 | −0.25 |
| Fast food (servings/week) | ||||
| Baseline | 0.68 (0.83) | |||
| Post-intervention | 0.57 (0.64) | −0.05 (−0.16, 0.07) | 0.44 | −0.07 |
| Follow-up | 0.48 (0.41) | −0.13 (−0.26, −0.001) | 0.048 | −0.23 |
Between baseline and post-intervention, no significant changes in dietary quality (i.e., intake of fruits, vegetables, dairy, added sugars, whole grains, fiber, calcium, fast food, and sugar sweetened beverages) were observed. At follow-up only, a significant decrease in intake of added sugars, sugar sweetened beverages, and fast food from baseline was observed. No changes were observed in intake of fruits, vegetables, dairy, whole grains, fiber, or calcium at follow-up.
Changes in study outcomes between baseline and follow-up did not vary by participants’ baseline characteristics, with one exception. Participants at low eating disorder risk at baseline had greater improvements in intuitive eating scores from baseline to follow-up relative to those at high eating disorder risk at baseline.
3.3. Study retention, program satisfaction, and program engagement
Program participants who indicated any participation in NYWS (96/102) at post-intervention reported watching a mean (SD) of 6.64 (3.23) videos, with 35 % watching 10+ videos, and reported attending an average of 5.97 (3.28) coaching sessions. As shown in Table 3, most participant characteristics were not associated with study retention, program satisfaction, or self-reported program engagement. Participants with larger body sizes were less likely to be retained in the study at post-intervention. Among those who completed the post-intervention survey, however, higher satisfaction was somewhat more common among those with larger body sizes, though not statistically significant at the 0.05 level. Higher self-reported program engagement was associated with greater increases in intuitive eating (p < 0.001) and reductions in internalized weight stigma (p < 0.01), added sugars (p = 0.02), and sugar sweetened beverages (p = 0.03).
Table 3.
Association (unadjusted) between baseline characteristics of study participants and study retention, program satisfaction, and program engagement.
| Characteristic | Study retention (n = 114) | p-Value | Program satisfaction (n = 95) | p-Value | Program engagement (n = 96) | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Yes n = 102 (89.5 %) |
No n = 12 (10.5 %) |
Higher satisfaction n = 64 (67.4 %) |
Lower satisfaction n = 31 (32.6 %) |
Higher self-reported engagement N = 49 (51.0 %) |
Lower self-reported engagement n = 47 (49.0 %) |
||||
|
| |||||||||
| Self-reported eating disorder history | 1.0 | 1.0 | 0.53 | ||||||
| Yes | 15 (88.2) | 2 (11.8) | 9 (64.3 %) | 5 (35.7 %) | 6 (42.9 %) | 8 (57.1 %) | |||
| No | 85 (89.5) | 10 (10.5) | 54 (67.5 %) | 26 (32.5 %) | 42 (51.9 %) | 39 (48.2 %) | |||
| High eating disorder risk | 1.0 | 0.47 | 0.32 | ||||||
| Yes | 40 (88.9) | 5 (11.1) | 22 (62.9 %) | 13 (37.1 %) | 16 (44.4 %) | 20 (55.6 %) | |||
| No | 62 (89.9) | 7 (10.1) | 42 (70.0 %) | 18 (30.0 %) | 33 (55.0 %) | 27 (45.0 %) | |||
| Weight cycling history | 0.75 | 0.19 | 0.94 | ||||||
| Yes | 36 (92.3) | 3 (7.7) | 23 (76.7 %) | 7 (23.3 %) | 16 (51.6 %) | 15 (48.4 %) | |||
| No | 66 (88.0) | 9 (12.0) | 41 (63.1 %) | 24 (36.9 %) | 33 (50.8 %) | 32 (49.2 %) | |||
| Frequent dieting | 0.63 | 0.88 | 0.54 | ||||||
| Yes | 50 (90.9) | 5 (9.1) | 32 (68.1 %) | 15 (31.9 %) | 23 (47.9 %) | 25 (52.1 %) | |||
| No | 52 (88.1) | 7 (11.9) | 32 (66.7 %) | 16 (33.3 %) | 26 (54.2 %) | 22 (45.8 %) | |||
| Body size | 0.03 | 0.06 | 0.90 | ||||||
| Larger | 42 (82.4) | 9 (17.7) | 30 (79.0 %) | 8 (21.1 %) | 20 (51.3 %) | 19 (48.7 %) | |||
| Smaller | 59 (95.2) | 3 (4.8) | 34 (60.7 %) | 22 (39.3 %) | 28 (50.0 %) | 28 (50.0 %) | |||
| Subjective social status | 1.0 | 0.11 | 0.32 | ||||||
| Higher | 56 (90.3) | 6 (9.7) | 40 (74.1) | 14 (25.9) | 30 (55.6) | 24 (44.4) | |||
| Lower | 46 (92.0) | 4 (8.0) | 24 (58.5) | 17 (41.5) | 19 (45.2) | 23 (54.8) | |||
| Educational attainment | 0.06 | 1.0 | 0.84 | ||||||
| Higher | 50 (96.2) | 2 (3.9) | 31 (67.4) | 15 (32.6) | 23 (50.0) | 23 (50.0) | |||
| Lower | 52 (83.9) | 10 (16.1) | 33 (67.4) | 16 (32.7) | 26 (52.0) | 24 (48.0) | |||
High eating disorder risk (yes): Eating Disorder Examination-Question Short score ≥ 1.2).
Weight cycling history (yes): loss of 10 lbs 6+ times.
Frequent dieting (yes): “often” or “always” (versus “rarely” or “never”).
Larger body size: body mass index ≥30.
Higher subjective social status: 6–10 rating on the Mac MacArthur Scale of Subjective Social Status (versus 1–5).
Higher educational attainment: advanced degree (versus less than an advanced degree).
4. Discussion
In this pilot/feasibility study, we sought to examine changes in intuitive eating, internalized weight stigma, eating disorder symptoms, and diet quality among employees enrolled in a weight-inclusive, intuitive eating-based workplace wellness program. Individuals enrolled in the program experienced increases in intuitive eating and decreases in internalized weight stigma and eating disorder symptoms after participating in the program. These improvements were maintained at follow-up, approximately 3 months after completing the program, at which time they also reported lower intakes of added sugars, sugar sweetened beverages, and fast food relative to baseline. Improvements in intuitive eating and reductions in internalized weight stigma, added sugar intake, and sugar sweetened beverage intake were greatest in those who self-reported a higher level of engagement in the program. Program satisfaction generally did not vary by participants’ sociodemographic characteristics, disordered eating risk, or level of internalized weight stigma.
Findings from our study align with those of another nonrandomized observational study of an intuitive eating and mindfulness-based workplace wellness program at another large Midwestern university, in which participants experienced improvements in intuitive eating and body appreciation (Bush, Rossy, Mintz, & Schopp, 2014). Our findings also align with review articles of intuitive eating-based programs, which show improvement in psychological and dietary outcomes, as well as high levels of program satisfaction (Bacon & Aphramor, 2011; Clifford et al., 2015; Schaefer & Magnuson, 2014). To our knowledge, our study was the first weight-inclusive, intuitive eating-based program to be offered virtually. We observed significant reductions in intake of added sugars, sugar sweetened beverages, and fast food at follow-up. These findings align with two previous randomized controlled trials conducted among adult women which found reductions in consumption of ultra-processed (Dimitrov Ulian, Pinto, de Morais, et al., 2018)/high-fat/high-sugar (Carbonneau, Bégin, Lemieux, et al., 2017) foods among participants receiving a weight-inclusive, intuitive eating-based intervention relative to controls. The dietary changes observed in our study were not present at post-intervention but emerged in the follow-up period. This finding may reflect the fact that behavior change, particularly in the context of a low-intensity or “small change” intervention, is a slow and gradual process, but that changes may be more durable over time (Graham, Madigan, & Daley, 2022; Ory, Lee Smith, Mier, & Wernicke, 2010; Prochaska & Velicer, 1997). This may also be a function of the intuitive eating principles included in the intervention, in which “gentle nutrition” is the final principle covered in the intervention. This approach differed from the nutrition intervention used in the other two trials which appeared to include more directive nutrition advice (both programs included lectures on national eating guidelines) relative to our program. This difference may explain why no increases in nutrient-dense foods such as fruits and vegetables from baseline to post-intervention or follow-up were seen in our study, but increases in fruit and vegetable intake were observed in the other trials (Carbonneau et al., 2017; Dimitrov Ulian et al., 2018).
While the literature suggests that weight-inclusive, intuitive eating programs could be particularly well-suited for those with histories of weight cycling or frequent/chronic dieting, these characteristics were not associated with program engagement or satisfaction in the present study, suggesting the potential for widespread appeal of weight-inclusive workplace wellness offerings relative to these risk factors. Although improvements in eating disorder symptoms were seen for participants irrespective of baseline eating disorder risk and eating disorder history, individuals at high eating disorder risk showed smaller improvements in intuitive eating scores. This finding may indicate the need for more intensive therapeutic interventions for these individuals. High program satisfaction was somewhat more common among individuals with larger bodies relative to those with smaller bodies (difference not significant) and no differences in self-reported program engagement were seen according to body size.
A major limitation of this pilot/feasibility study is the lack of a comparison condition. Given the results of the study, this intervention should be tested using a randomized, controlled design. An additional limitation of the study is its short duration. The 3-month duration may not elicit meaningful and/or long-lasting changes relative to programs of longer duration, highlighting the need for longer-term studies of intuitive eating interventions. The study population was only made up of University of Michigan employees and was homogeneous with respect to gender and race/ethnicity and had high representation from individuals with advanced degrees. Further, we were unable to examine whether those who elected to participate differed from those who were invited but did not participate. While subjective social status is expected to be correlated with food insecurity (Willis, 2021), a potential barrier to intuitive eating, we were unable to examine how food insecurity (current or past) may have impacted study outcomes. In light of important criticisms of intuitive eating-based interventions related to the privilege required to implement the principles of intuitive eating and the lack of a trauma-informed perspective in the approach (Burnette et al., 2023; Wilson & Trotter, 2021), the lack of diversity of our sample is a critical issue that should be addressed in future studies of weight-inclusive workplace interventions.. Future studies should aim to recruit participants who are diverse in terms of body size, gender, racial/ethnic background, socioeconomic status, and other identities.
While our findings may not be widely generalizable, the feasibility demonstrated in the present study likely translates to other large-scale workplace wellness programs at institutions similar to the University of Michigan. We used validated scales to assess out outcomes of interest, however, the lack of objective health data and rigorous assessment of dietary intake is a limitation of the current study that should be incorporated in future trials. Another key limitation of the study is the lack of objective data about engagement in components of the program.
5. Conclusion
The present study provided a unique opportunity to assess the feasibility, acceptability, and potential impact of a weight-inclusive, intuitive eating-based workplace wellness program, as well as to examine for whom these programs may be best suited. Results indicate significant improvements in behavioral and psychological outcomes during participation, with greater improvements in outcomes for those with higher levels of self-reported program engagement. Many nutrition-focused workplace wellness programs restrict program enrollment to only those above a particular body weight/BMI, excluding those at lower weights who are seeking assistance with nutrition habits. The results of this study support the notion that this type of nutrition programming may be beneficial for employees with a range of body sizes and may improve the health of employees through increased intuitive eating, decreased internalized weight stigma, decreased eating disorder symptoms, and improvements in diet quality. Future research should examine the effects of weight-inclusive, intuitive eating-based workplace wellness programming in a rigorous, randomized trial.
Acknowledgements
We would like to express special thanks to the Nourish Your Whole Self team that delivered the program: Stacy Knasiak, Diana Rose, and Holly Scherer.
Role of funding sources
Michigan Nutrition & Obesity Research Center (MNORC) Pilot/Feasibility Grant Program; P30 DK089503.
Footnotes
Declaration of competing interest
All authors have no conflicts of interest to disclose.
CRediT authorship contribution statement
Jane Schmid: Formal analysis, Investigation, Writing – original draft. Ashley Linxwiler: Conceptualization, Data curation, Investigation, Supervision, Writing – review & editing. Erica Owen: Conceptualization, Investigation, Supervision, Writing – review & editing. Heather Caplan: Investigation, Supervision, Writing – review & editing. Kristi Rahrig Jenkins: Conceptualization, Investigation, Writing – review & editing. Katherine W. Bauer: Methodology, Supervision, Writing – review & editing. Matthew Zawistowski: Methodology, Supervision, Writing – review & editing. Heidi M. Weeks: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing. Kendrin Sonneville: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Data availability
Data will be made available on request.
References
- Adler NE, Epel ES, Castellazzo G, & Ickovics JR (2000). Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychology, 19(6), 586–592. [DOI] [PubMed] [Google Scholar]
- Anderson LM, Quinn TA, Glanz K, et al. (2009). The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. American Journal of Preventive Medicine, 37(4), 340–357. [DOI] [PubMed] [Google Scholar]
- Bacon L, & Aphramor L (2011). Weight science: Evaluating the evidence for a paradigm shift. Nutrition Journal, 10, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun TD, Unick JL, Abrantes AM, et al. (2022). Intuitive eating buffers the link between internalized weight stigma and body mass index in stressed adults. Appetite, 169, Article 105810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CB, Hazzard VM, Larson N, Hahn SA, Eisenberg ME, & Neumark-Sztainer D (2023). Is intuitive eating a privileged approach? Cross-sectional and longitudinal associations between food insecurity and intuitive eating. Public Health Nutrition, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush HE, Rossy L, Mintz LB, & Schopp L (2014). Eat for life: A work site feasibility study of a novel mindfulness-based intuitive eating intervention. American Journal of Health Promotion, 28(6), 380–388. [DOI] [PubMed] [Google Scholar]
- Carbonneau E, Bégin C, Lemieux S, et al. (2017). A Health at Every Size intervention improves intuitive eating and diet quality in Canadian women. Clinical Nutrition, 36 (3), 747–754. [DOI] [PubMed] [Google Scholar]
- Clifford D, Ozier A, Bundros J, Moore J, Kreiser A, & Morris MN (2015). Impact of non-diet approaches on attitudes, behaviors, and health outcomes: A systematic review. Journal of Nutrition Education and Behavior, 47(2), 143–155.e141. [DOI] [PubMed] [Google Scholar]
- Cotton MA, Ball C, & Robinson P (2003). Four simple questions can help screen for eating disorders. Journal of General Internal Medicine, 18(1), 53–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cundiff JM, Smith TW, Uchino BN, & Berg CA (2013). Subjective social status: Construct validity and associations with psychosocial vulnerability and self-rated health. International Journal of Behavioral Medicine, 20(1), 148–158. [DOI] [PubMed] [Google Scholar]
- Dimitrov Ulian M, Pinto AJ, de Morais SP, et al. (2018). Effects of a new intervention based on the health at every size approach for the management of obesity: The “health and wellness in obesity” study. PLoS One, 13(7), Article e0198401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan AE, Ziobrowski HN, & Nicol G (2017). The prevalence of past 12-month and lifetime DSM-IV eating disorders by BMI category in US men and women. European Eating Disorders Review, 25(3), 165–171. [DOI] [PubMed] [Google Scholar]
- Foreyt JP, Brunner RL, Goodrick GK, Cutter G, Brownell KD, & St Jeor ST (1995). Psychological correlates of weight fluctuation. The International Journal of Eating Disorders, 17(3), 263–275. [DOI] [PubMed] [Google Scholar]
- Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, & Serpell L (2016). Development and psychometric validation of the EDE-QS, a 12 item short form of the Eating Disorder Examination Questionnaire (EDE-Q). PLoS One, 11(5), Article e0152744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham HE, Madigan CD, & Daley AJ (2022). Is a small change approach for weight management effective? A systematic review and meta-analysis of randomized controlled trials. Obesity Reviews, 23(2), Article e13357. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, et al. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, Article 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinnett K, Kyle T, Parry T, Stevenin B, Ramasamy A, & ACTION Steering Group. (2019). Insights into the role of employers supporting obesity management in people with obesity: Results of the national ACTION study. Population Health Management, 22(4), 308–314. [DOI] [PubMed] [Google Scholar]
- Koller KA, Thompson KA, Miller AJ, Walsh EC, & Bardone-Cone AM (2020). Body appreciation and intuitive eating in eating disorder recovery. The International Journal of Eating Disorders, 53(8), 1261–1269. [DOI] [PubMed] [Google Scholar]
- Lillis J, Luoma JB, Levin ME, & Hayes SC (2010). Measuring weight self-stigma: The weight self-stigma questionnaire. Obesity (Silver Spring), 18(5), 971–976. [DOI] [PubMed] [Google Scholar]
- Linardon J, Tylka TL, & Fuller-Tyszkiewicz M (2021). Intuitive eating and its psychological correlates: A meta-analysis. International Journal of Eating Disorders, 54(7), 1073–1098. [DOI] [PubMed] [Google Scholar]
- Mattke S, Liu H, Caloyeras J, et al. (2013). Workplace wellness programs study: Final report. Rand Health Quarterly, 3(2), 7. [PMC free article] [PubMed] [Google Scholar]
- Mensinger JL, Calogero RM, Stranges S, & Tylka TL (2016). A weight-neutral versus weight-loss approach for health promotion in women with high BMI: A randomized-controlled trial. Appetite, 105, 364–374. [DOI] [PubMed] [Google Scholar]
- Miller WC, & Jacob AV (2001). The health at any size paradigm for obesity treatment: The scientific evidence. Obesity Reviews, 2(1), 37–45. [DOI] [PubMed] [Google Scholar]
- Nagata JM, Garber AK, Tabler JL, Murray SB, & Bibbins-Domingo K (2018). Prevalence and correlates of disordered eating behaviors among young adults with overweight or obesity. Journal of General Internal Medicine, 33(8), 1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni Mhurchu C, Aston LM, & Jebb SA (2010). Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health, 10, 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ory MG, Lee Smith M, Mier N, & Wernicke MM (2010). The science of sustaining health behavior change: The health maintenance consortium. American Journal of Health Behavior, 34(6), 647–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prnjak K, Mitchison D, Griffiths S, et al. (2020). Further development of the 12-item EDE-QS: Identifying a cut-off for screening purposes. BMC Psychiatry, 20(1), 146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, & Velicer WF (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38–48. [DOI] [PubMed] [Google Scholar]
- Puhl R, & Suh Y (2015). Health consequences of weight stigma: Implications for obesity prevention and treatment. Current Obesity Reports, 4(2), 182–190. [DOI] [PubMed] [Google Scholar]
- Schaefer JT, & Magnuson AB (2014). A review of interventions that promote eating by internal cues. Journal of the Academy of Nutrition and Dietetics, 114(5), 734–760. [DOI] [PubMed] [Google Scholar]
- Sonneville KR, et al. (2021). Chronic dieting and disordered eating among higher weight employees participating in workplace weight management programming. In International conference on eating disorders (virtual). [Google Scholar]
- Stevens VL, Jacobs EJ, Sun J, et al. (2012). Weight cycling and mortality in a large prospective US study. American Journal of Epidemiology, 175(8), 785–792. [DOI] [PubMed] [Google Scholar]
- Täuber S, Mulder LB, & Flint SW (2018a). The impact of workplace health promotion programs emphasizing individual responsibility on weight stigma and discrimination. Frontiers in Psychology, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Täuber S, Mulder LB, & Flint SW (2018b). The impact of workplace health promotion programs emphasizing individual responsibility on weight stigma and discrimination. Frontiers in Psychology, 9, 2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson FE, Midthune D, Kahle L, & Dodd KW (2017). Development and evaluation of the National Cancer Institute’s dietary screener questionnaire scoring algorithms. The Journal of Nutrition, 147(6), 1226–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tribole E (2020). Intuitive eating: A revolutionary anti-diet approach (4th edition). St. Martin’s Press. [Google Scholar]
- Tribole E, & Resch E (2017). The intuitive eating workbook: Principles for nourishing a healthy relationship with food. Oakland, CA: New Harbinger Publications, Inc. [Google Scholar]
- Tylka T (2006). Development and psychometric evaluation of a measure of intuitive eating. Journal of Counseling Psychology: American Psychological Association, 53, 226–240. [Google Scholar]
- Tylka TL, & Kroon Van Diest AM (2013). The Intuitive Eating Scale-2: Item refinement and psychometric evaluation with college women and men. Journal of Counseling Psychology, 60(1), 137–153. [DOI] [PubMed] [Google Scholar]
- Tylka TL, Annunziato RA, Burgard D, et al. (2014). The weight-inclusive versus weight-normative approach to health: Evaluating the evidence for prioritizing well-being over weight loss. Journal of Obesity, 2014, Article 983495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylka TL, Calogero RM, & Daníelsdóttir S (2020). Intuitive eating is connected to self-reported weight stability in community women and men. Eating Disorders, 28(3), 256–264. [DOI] [PubMed] [Google Scholar]
- Willis DE (2021). Feeding inequality: Food insecurity, social status and college student health. Sociology of Health & Illness, 43(1), 220–237. [DOI] [PubMed] [Google Scholar]
- Wilson J, & Trotter W (2021). How whiteness shows up in your work and what to do about it. In EDRDPRO webinar. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.


