Abstract
Purpose:
This article describes effective interventions to promote regular physical activity and reduce sedentary behavior that were identified as part of the 2018 Physical Activity Guidelines Advisory Committee Scientific Report.
Methods:
A comprehensive literature search was conducted of eligible systematic reviews, meta-analyses, and relevant governmental reports published between 2011 and 2016. For the physical activity promotion question, articles were first sorted by four social ecological levels of impact (i.e., individual, community, communication environment, and physical environment and policy levels) and then further sorted into more specific categories that emerged during the review process. For the sedentary behavior reduction question, the literature was sorted directly into emergent categories (i.e., youth, adult, and worksite interventions).
Results:
Effective physical activity promotion strategies were identified at each level of impact, including those based on behavior change theories and those occurring at different settings throughout the community. Effective interventions also included those delivered in person by trained staff or peer volunteers and through different information and communication technologies, such as by phone, Web or Internet, and computer-tailored print. A range of built environment features were associated with more transit-based and recreational physical activity in children and adults. Effective sedentary reduction interventions were found for youth and in the workplace.
Conclusions:
A promising number of interventions with demonstrated effectiveness were identified. Future recommendations for research include investigating the most useful methods for disseminating them to real-world settings; incorporating more diverse population subgroups, including vulnerable and underrepresented subgroups; collecting cost data to inform cost-effectiveness comparisons; and testing strategies across different levels of impact to determine which combinations achieve the greatest effects on different modes of physical activity across the week.
Keywords: PHYSICAL ACTIVITY, INTERVENTION, SYSTEMATIC REVIEW, SOCIAL ECOLOGICAL MODEL, PAGAC
Other articles in this issue describe a broad spectrum of evidence-based health benefits associated with regular physical activity and lower levels of sedentary behavior over the life course. The evidence clearly shows that physical activity provides a wide array of benefits—from reducing feelings of anxiety and depression and improving sleep and quality of life to lowering the risk of developing diabetes, heart disease, and many cancers. A large proportion of Americans, however, are not receiving the substantial benefits a physically active lifestyle can offer. In 2015, only about one half of US adults and one quarter of high school students and children in the United States reported meeting the age-specific federal guidelines for aerobic physical activity (1–3). Nearly one third of adults and one quarter of older adults (65+ yr of age) reported being inactive during their leisure time (1,4). These findings reflect the large burden of physical inactivity in the United States, which has been reported to be even higher when device-based measurement has been used (5). Furthermore, a large burden is found in a growing number of countries throughout the world (6). For individuals who are not yet participating in regular physical activity, there are a number of effective intervention strategies that individuals and communities can use to increase physical activity and reduce sedentary behavior.
The major goal of this article is to highlight the current evidence-based strategies and approaches for increasing regular physical activity and reducing sedentary behavior. This area was deemed of particular interest for the 2018 Physical Activity Guidelines Advisory Committee given it was not reviewed as part of the 2008 Physical Activity Guidelines Advisory Committee Report (7). In light of the variety of intervention strategies and approaches used, the evidence for the current review was organized by level of impact using an adapted version of a social ecological framework (8) (see Fig. 1). Using this framework, the evidence was divided into four broad levels—individual, community, the communication environment (i.e., interventions delivered through information and communication technologies [ICT]), and physical environments and policy. The potential public health impacts of the described intervention strategies and approaches are also discussed, along with recommendations for future research and practice in physical activity promotion. Because the aim of the 2018 Physical Activity Guidelines Advisory Committee Report was to evaluate the physical activity evidence as it pertains to population health, intervention-based clinical health impacts/ clinical meaningfulness were not evaluated. Additionally, such clinical health impacts typically were not the focus of the reviews that were part of the evidence search.
FIGURE 1—
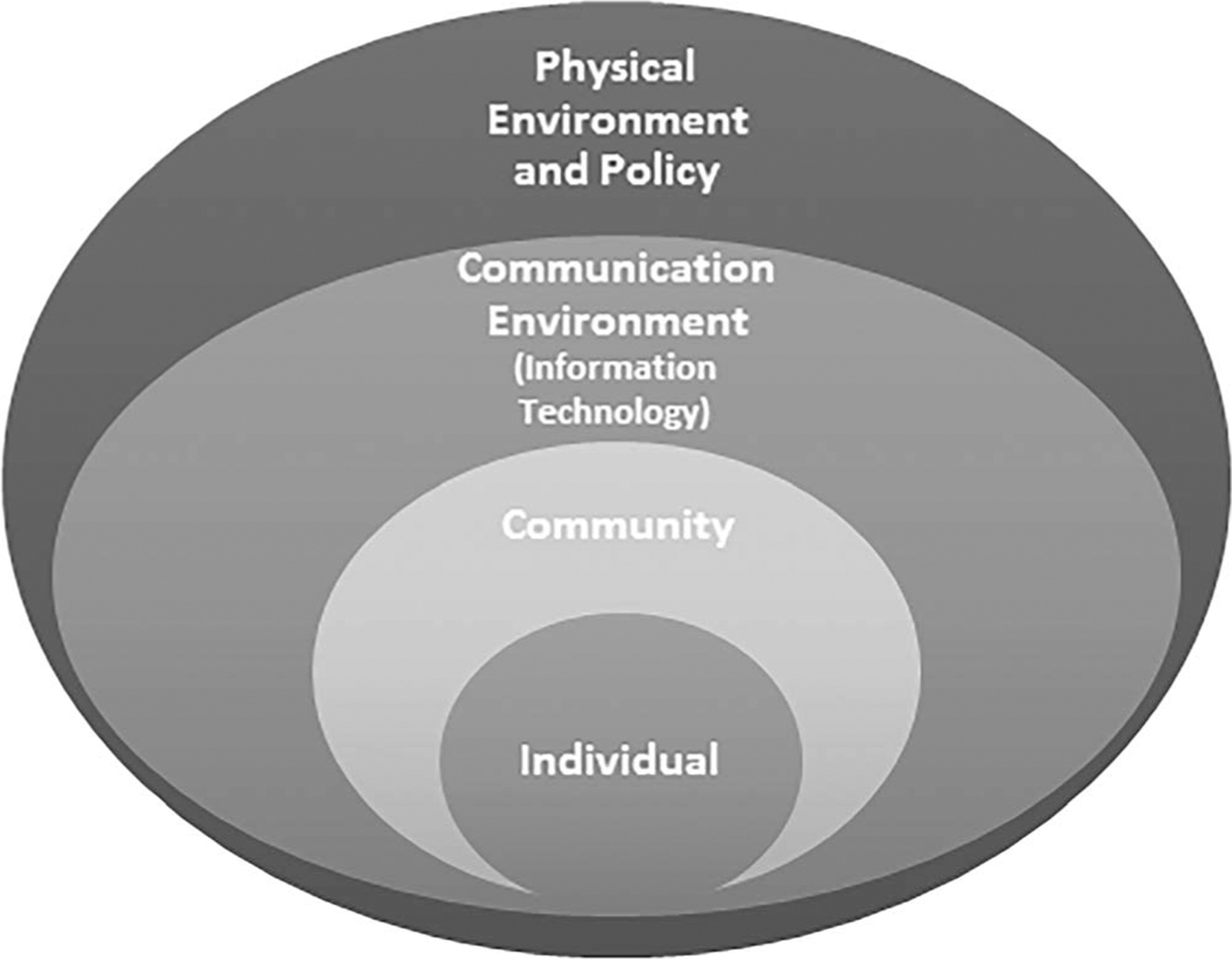
Social ecological framework.
METHODS
Questions of interest.
The Physical Activity Promotion Subcommittee of the Physical Activity Guidelines Advisory Committee focused on two central questions to examine in the physical activity intervention area, as follows: 1) What interventions are effective for increasing physical activity at different levels of impact? 2) What interventions are effective for reducing sedentary behavior? The Committee also sought to determine whether intervention effectiveness varied by age, sex, race/ethnicity, or socioeconomic status, when such information was available. Thus, the Subcommittee charge was to identify those intervention areas for which effective interventions were available, as opposed to searching for any intervention areas for which the evidence did not support effectiveness.
Evidence review process.
The evidence review process and methods are fully detailed in the 2018 Physical Activity Guidelines Advisory Committee Report (9), and will be briefly described here. The protocol-driven methodology applied was aimed at minimizing bias and maximizing the identification of relevant and high-quality systematic reviews (10). Due to the size of the physical activity promotion evidence base, which spans at least six decades, includes review articles from both the US and non-US regions, and was not formally reviewed in developing the original 2008 US Physical Activity Guidelines (11), the focus of the evidence review was limited, due to pragmatic considerations, to systematic reviews, meta-analyses, and relevant governmental reports published from 2011 through 2016 and deemed of sufficient quality based on the Physical Activity Guidelines Advisory Committee’s eligibility criteria (9). These criteria included publication language (English), publication status (i.e., peer-reviewed, high-quality report), research type (i.e., systematic review, meta-analysis, pooled analysis, relevant report), and study subjects (human) (10). Evidence sources published before or after the 2011 to 2016 period were unable to be included, and thus are not represented in the 2018 Physical Activity Guidelines Advisory Committee Report. Although it is possible that reviewing additional literature through the beginning of 2018 could provide further insights, the nature of the evidence being accumulated in this field makes it less likely than other fields that the current evidence evaluation would have substantively changed. This is because of the broad heterogeneity of the physical activity promotion literature across a variety of factors (e.g., target populations, study designs and methods, physical activity types, intervention content, length and delivery channels). This, in turn, makes it less likely that any one additional study or review would be sufficiently rigorous and comprehensive to substantially change the evidence grades during that additional 16-month period. This point notwithstanding, the constrained period remains a limitation of the review process.
Additionally, studies included within the articles being evaluated typically reflected a mix of physical activity measures (i.e., self-report, device-based assessment), the types of primarily aerobic forms of physical activity being targeted (e.g., walking, moderate-to-vigorous forms of physical activity, aerobic activities combined with strengthening activities), and outcomes (e.g., total volume of activity, duration and/or frequency of moderate-to-vigorous activity, percentage of participants meeting guidelines). The review articles generally did not look at associations between specific types of physical activity measures and intervention outcomes, or how different types of physical activity outcomes were affected.
For efficiency, one comprehensive search was conducted which included global key word terms for both physical activity promotion and sedentary behavior reduction (see Fig. 2). Relevant review articles for each field were then sorted to specifically address each question of interest. For each question of interest (i.e., physical activity promotion, sedentary behavior reduction), eligible articles were next sorted into more specific categories (i.e., topic areas) that emerged as part of the review process. For the physical activity promotion question, articles were first sorted by the four social ecological levels of impact described earlier, and then further grouped into specific categories that emerged in examining each article (e.g., at the Community level, seven categories emerged). In light of the smaller overall evidence base available for the sedentary behavior reduction question, that literature was grouped directly in emergent clusters (as opposed to by level of impact) of youth, adult, and worksite interventions.
FIGURE 2—
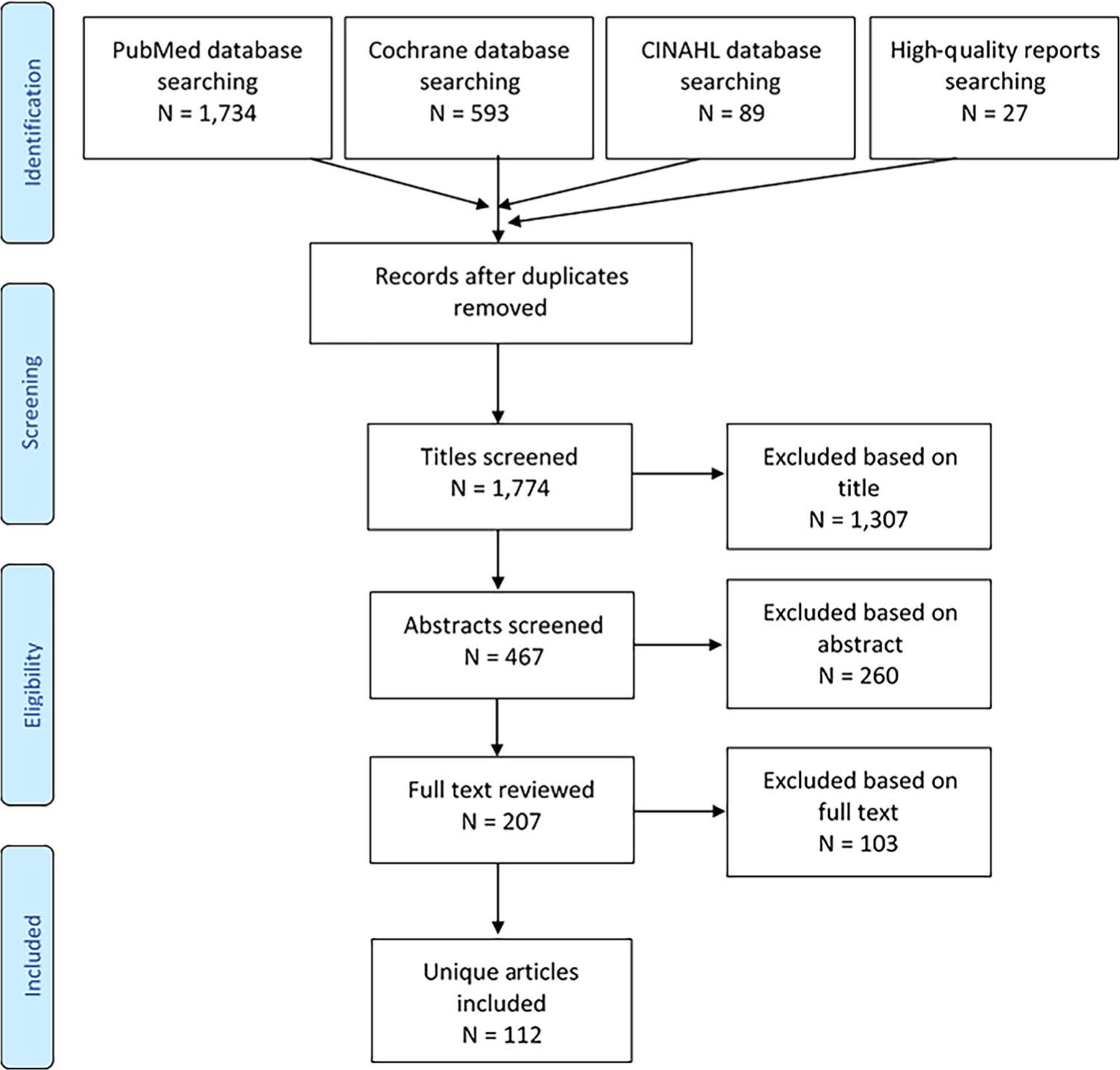
Evidence review flowchart.
When available, information was abstracted from the reviews for between- and within-group comparisons, the magnitude of effect, type and amount of physical activity, and physical activity intensity and frequency. For most systematic reviews, which constituted the majority of articles evaluated, such information, including effect size estimates, was often inadequately described or missing. When effect size estimates were available, we included them in the findings of this article. A standard evidence-grading rubric was utilized across all Committee topic areas which consisted of evidence grades of strong, moderate, limited, and grade not assignable (9). The collective scientific expertise of the Committee members was utilized in making final determinations with respect to applying the rubric in arriving at evidence grades, commensurate with the formal charge of the Committee. The Physical Activity Promotion Subcommittee assigned evidence grades of “Strong” or “Moderate” when the body of systematic evidence was reasonably large (e.g., typically more than one rigorous systematic review or a published meta-analysis, with articles usually including more than 10 studies) and indicated a consistent effect across rigorously designed studies (e.g., experiments). “Strong” was distinguished from “Moderate” based on the larger pool of more rigorously designed studies available (e.g., experimental designs) and typically longer intervention periods (e.g., greater than 6 months) (9). Because both strong and moderate evidence grades reflect sufficiently consistent bodies of literature supporting the use and deployment of the interventions involved, they constitute the focus of this article.
RESULTS
Number of Articles Included in the Review
For both questions, a total of 1778 eligible systematic reviews, meta-analyses, and governmental reports (all referred to as “articles” in this article) were evaluated for relevance in addressing questions 1 and 2. Of this total, 96 articles were deemed relevant to address question 1 related to physical activity promotion, and 18 articles were deemed relevant to address question 2 related to sedentary behavior reduction.
Results of the Evidence Review: Interventions to Promote Physical Activity
Categories for which consistent strong or moderate evidence support was found for physical activity intervention effectiveness are provided in Table 1 and described briefly below by levels of impact. Promising, but currently understudied, strategies within each level are listed within each level of impact but, due to space constraints, are not described in detail. The “Online-Only Supplementary Material” included in the 2018 Physical Activity Guidelines Advisory Committee Report contains detailed information about all articles that were considered by the Committee.
TABLE 1.
Strategies and approaches with evidence of effectiveness for the general population and selected populations.a
| Category | Intervention Approaches | Evidence Type (Number of Studies) | Selected Effect Sizesb |
|---|---|---|---|
| Physical activity promotion interventions Individual Behavior change theories and models | Behavior change theories and techniques (general adult as well as more specific populations) | 1 SR (12) 1 MA (11) | One meta-analysis reported a positive effect of providing lottery and escalating incentives on exercise session attendance when compared with no incentive for short-duration interventions lasting 4 to 26 wk; pooled results showed an increase in exercise attendance of 11.55%; 95% CI, 5.61%–17.50% (12). |
| Interventions specific to older adults | Effective strategies include identifying & problem-solving around age-specific PA barriers, social support, modeling of PA behaviors, rewards linked with PA behavior change | 2 SR (158 and 18) 1 MA (24) | Interventions had a small effect on physical activity d = 0.14 (95% CI, 0.09–0.20, P < 0.001) (13). |
| Interventions specific to youth | Effective strategies include in-person education & experiential strategies (e.g., exercise classes) Above can be enhanced through family inclusion | 2 MA (47 and 58) | 1. Significant effect sizes for interventions targeting individuals only (g = 0.27; 95% Cl, 0.12–0.42), which were further enhanced when individual interventions also included families (g = 0.44; 95% Cl, 0.23–0.66) or school and print or digital media (e.g., newspaper, radio; g = 0.30; 95% Cl, 0.04–0.57) (14). |
| 2. Family-based physical activity interventions found a small but significant effect size favoring the intervention group (SMD, 0.41; 95% Cl, 0.15–0.67) (15). | |||
| Peer-Led | Peer-led behavioral self-management interventions (older adults and individuals with chronic disease) | 1 MA (21) | Moderate effects for increases in physical activity overall among the 17 studies where effects sizes were available (SMD, 0.4; 95% Cl, 0.22–0.55, P< 0.001) (16). |
| Community Community-wide | Community-wide interventions that use intensive contact with the majority of the target population | 2 SR (16 and 33) 1 MA (10) PAGMR | Effect sizes not mentioned in PAGAC chapter. |
| School interventions | Multiple-component programs occurring during school hours aimed at physical activity across the school day in primary school-age (typically ages 5 to 12 yr) and adolescent youth Revising the structure of physical education (PE) classes to increase in-PE physical activity in primary school-age and adolescent youth | 5 SR (range, 8–129) 2 MA (13 and 15) AHA PAGMR | 1. CATCH and SPARK trials: Results showed that vigorous physical activity was significantly higher among intervention students (mean (M) = 58.6 min) compared to controls (M = 46.5 min) (P< 0.003) (17). Students spent more minutes per week being physically active in teacher- and specialist-led classes compared to controls (33 min, 40 min, and 18 min, respectively, P< 0.001), although PA did not increase outside of school (18). |
| 2. Absolute difference of 10.37% (95% Cl, 6.33–14.41) of lesson time spent in moderate-to-vigorous physical activity in favor of the interventions over controls. This estimated difference of 10.37% of lesson time corresponds to 24% more active learning time in the intervention groups compared with the control condition (SMD, 0.62; 95% Cl, 0.39–0.84) (19). | |||
| Communication environment (information and communication technologies) Wearable activity monitors | Wearable activity monitors, including step counters (pedometers) and accelerometers, when used in conjunction with goal-setting and other behavioral strategies (general population of adults and those with type 2 diabetes or with overweight or obesity) | 4 SR (range: 5–14) 3 MA (11 for each) | 1. Accelerometry interventions across 12 trials resulted in a small but significant increase in physical activity levels (SMD, 0.26; 95% Cl, 0.04–0.49). The additional benefit of activity monitors when compared with an active comparison arm (e.g., a physical activity intervention without activity monitors) is less clear (SMD, 0.17; 97% Cl, −1.09 to 1.43) (20). |
| 3. Type 2 diabetes: step-counter use significantly increased physical activity by a mean of 1822 steps per day (7 studies, 861 participants; 95% Cl, 751–2894 steps per day), use of a step-counter in combination with setting a specific physical activity goal resulted in significantly more steps per day compared to control arms (weighted mean difference (WMD) of 3200 steps per day; 95% Cl, 2053–4347 steps per day), whereas step-counter use without a goal did not significantly increase physical activity relative to control arms (WMD of 598 steps per day; 95% Cl, −65 to 1260 steps per day). Use of a step diary or log also was related to a statistically significant increase in physical activity (WMD = 2816 steps per day), whereas when a step diary was not used, physical activity did not increase significantly (WMD = 115 steps per day) (21). | |||
| 4. Overweight/Obesity: a significant positive intervention effect for steps per day was found for behavioral physical activity interventions that included an activity monitor when compared with waitlist or usual care interventions (n = 4) (SMD, 0.90; 95% Cl, 0.61–1.19, P< 0.0001). A similar intervention comparison also found a significant positive effect for total moderate-to-vigorous physical activity minutes per time unit (n = 3) (SMD, 0.50; 95% Cl, 0.11–0.88, P= 0.01). In a meta-analysis of a similar intervention comparison (i.e., the addition of an activity monitor to an existing intervention versus when it was not added) using the mean difference for walking MET-minutes per week as the outcome and involving only two studies (both of which included women only), a statistically significant positive effect was found (mean difference for walking MET-minutes per week = 282; 95% Cl, 103.82–460.18, P= 0.002) (22). | |||
| Telephone-assisted interventions | Telephone-assisted interventions (general adult population, including older adults) | 2 SR (11 and 27) | Effect sizes not mentioned in the PAGAC chapter. |
| “The majority of high-quality studies in this area produced effect sizes indicating a moderate or better intervention effect (i.e., d> 0.5). The evidence indicates that longer-duration interventions (i.e., 12 months or more) are associated with greater effectiveness.” | |||
| Web-based or Internet-delivered interventions | Internet-delivered interventions that include educational components (general adult population) | 3 SR (range: 7–15) 1 MA (34) | 1. Overall effect size estimates indicate a small but positive intervention effect on physical activity in the general adult population (d = 0.14). Studies that initially screened participants and enrolled only those classified as sedentary or insufficiently active produced larger effects (d = 0.37) relative to studies that did not screen participants for physical activity level (d = 0.12). The meta-analysis, which targeted either physical activity only (n = 21) or physical activity and additional health-related behaviors, such as nutrition or weight management behaviors (n = 13), found that the two different types of interventions produced similar effect sizes (23). |
| 2. In a systematic review of nine web-based physical activity interventions in individuals with type 2 diabetes, six studies reported significant short-term increases (less than 6 months, typically) in physical activity when compared with a control arm. The overall magnitude of the physical activity increases reported in this review ranged from 3% to 125% (24). | |||
| 3. In a systematic review of seven self-guided web-based physical activity intervention trials among patients with a range of chronic disease conditions (e.g., multiple sclerosis, heart failure, type 2 diabetes mellitus, physical disabilities, metabolic syndrome), three studies reported significant physical activity improvements relative to controls, while four studies reported nonsignificant differences between groups. Effect sizes ranged from 0.13 to 0.56, with wide variability in physical activity change across studies (25). | |||
| Computer-tailored print interventions | Computer-tailored print interventions that collect user information through mailed surveys that is then used to generate computer-tailored mailings containing personalized physical activity advice and support (general adult population) | 2 SR (11 and 26) | The majority of studies in this area produced effect sizes that were small (i.e., Cohen’s d ranging from 0.12 to 0.35) when compared to minimal or no-intervention control arms. (F11–57) |
| Mobile phone programs | Mobile phone programs consisting of or including text-messaging (general adult population) Use of smartphone applications (children and adolescents) | 5 SR (range: 9–30) 3 MA (range: 11–74) | 1. General adult population: text messaging interventions aimed at general adult populations found significant positive effect sizes, relative to controls, that were on average 0.40 or greater, with a median effect size in one systematic review of 0.50 (26). |
| 2. Smartphone apps - youth: Interventions have been reported to have small to moderate effects in both girls and boys, with one systematic review reporting Cohen’s d coefficients ranging from −0.36 to 0.86. As part of these meta-regression analyses, investigators were able to explain 45 percent of the variability in physical activity effect size among children and 62 percent of the variability in physical activity effect size among adolescents (27). | |||
| Physical environment and policy Point-of-decision prompts to promote stair use | Point-of-decision prompts to use stairs versus escalators or elevators (adults) | 2 SR (6 and 67) AHA | In one systematic review of 67 studies, 77 percent reported increases in stair use. For those studies with significant effects (n = 55 studies), the percent stair use increase ranged from 0.3 percent to 34.7 percent. When odds ratios were reported, they ranged from 1.05 (95% Cl, 1.01–1.10) to 2.90 (95% Cl, 2.55–3.29) (28). |
| Built environment characteristics that support active transport | Built environment characteristics and infrastructure that support active transport to destinations (e.g., Safe Routes to School programs, street connectivity, a mix of residential, commercial, and public land uses) (children, adults, and older adults) | 3 SR (range: 12–42) 1 MA (42) AHA The Guide to Community Preventive Services | 1. RESIDE study: each unit increase in perceived safety from crime was associated with 3.2 min-wk−1 more of transport physical activity. In addition, the association remained similar (3.6 min-wk−1 increases with unit increases in perceived safety from crime) when also controlling for built environmental characteristics such as residential density, streets connectivity, and number of local destinations (29). |
| 2. Youth: positive associations found between land-use mix and children’s physical activity (OR ranged from 1.8 (95% Cl, 1.05–3.42) to 3.46 (95% Cl, 1.6–7.47)). (AHA Scientific Statement) | |||
| 3. Older adults: A meta-analysis of 42 quantitative studies found significant positive associations among a number of environmental variables and active transport behaviors, including residential density and urbanization, walkability, easy access to building entrances, and access to and availability of services and destinations. A weak, negative association was found between neighborhood disorder (e.g., litter, vandalism and decay) and total walking for transport (30). | |||
| Community design and characteristics that support recreational physical activity | Community design and characteristics that support physical activity, such as having safe and readily usable walking and cycling infrastructure and other favorable built environment elements (children and general adult populations) | 1 SR (600) AHA The Guide to Community Preventive Services | 1. RESIDE study: each unit increase in perceived safety from crime was associated with 13.5 min-wk−1 more of recreational physical activity over a 7-yr follow-up period. This amount of increase remained similar (13.7 min-wk−1) when also controlling for additional built environmental characteristics (i.e., residential density, streets connectivity, and mix of local destinations) (29). |
| 2. Adults: the largely cross-sectional studies reviewed by the AHA Scientific Statement generally indicated a significant relationship between neighborhood aesthetics and leisure-time physical activity, walking, or meeting physical activity recommendations (ORs ranged from 1.13 to 2.6). Absence of heavy traffic was associated with more walking and leisure-time physical activity (OR = 1.22; 95% Cl, 1.08–1.37). (AHA Scientific Statement) | |||
| Access to indoor and/or outdoor recreation facilities or outlets | Having access to indoor (e.g., gyms) and/or outdoor recreation facilities or outlets, including parks, trails, and natural or green spaces (children and general adult populations) | 3 SR (range: 12–90) AHA | Greater access generally was shown to be related to more physical activity among adults (OR 1.20; 95% Cl, 1.06–1.34). (AHA Scientific Statement) |
| Sedentary behavior reduction interventions Youth | Reductions in television viewing and other screen-time behaviors in primarily school-based settings (youth) through school-based counseling, parental involvement, tailored feedback, and use of screen allowance devices at home | 5 SR (range: 10–22) 4 MA (range: 13–34) | 1. As a whole, the studies reviewed showed small but consistent effects on sedentary behavior reduction (e.g., mean difference was −20.44 min-d−1; 95% Cl, −30.69 to −10.20) (31). |
| 2. School-based interventions focused primarily on reducing screen time in children through in-class or after-school curricula, and typically included messages targeting screen time as well as other health behaviors (e.g., exercise, diet). Such interventions had small but consistent effects in reducing sedentary time, particularly for those lasting longer than 6 months (e.g., mean difference was −0.25 h-d−1; 95% Cl, −0.37 to −0.13) (32). | |||
| Worksite | Interventions targeting sedentary behavior in worksites (adults), including physical changes to workstations | 2 SR (15 and 40) 2 MA (8 and 21) | Interventions that focused on providing educational or motivational support showed only small and inconsistent effects on sedentary behavior (e.g., mean difference was −15.52 min per 8-h workday [95% Cl, −22.88 to −8.16]). Interventions that targeted physical changes to work stations (i.e., predominantly the addition of sit-stand workstations, with a few that used treadmill desks or portable pedal machines) had consistently medium to large effects (e.g., mean difference was −72.78 min per 8-h workday [95% Cl, −104.92 to −40.64]). Additionally, these effects were stronger when these types of work station changes were combined with educational and behavioral support (e.g., mean difference was −88.80 min per 8-h workday [95% Cl, −132.69 to −44.61]) (33). |
Intervention categories derived from a comprehensive search of eligible systematic reviews and meta-analyses along with selected governmental reports identified during a 2011–2016 evidence search.
Effect sizes are from articles mentioned in manuscript. Due to space limitations, not all articles included in the Committee Report were captured in the article; however, a full list of all systematic reviews, meta analyses, and effect sizes can be found in 2018 Physical Activity Guidelines Advisory Committee Report.
SR, systematic review; MA, meta-analysis; PAGMR, Physical Activity Guidelines Midcourse Report; AHA, American Heart Association Scientific Statement.
Individual-Level Strategies and Approaches
Much of the original physical activity promotion literature dating back to the mid-twentieth century has been comprised of individual-level interventions consisting of person-to-person or small group-based programs. The literature evaluated as part of the 2011 to 2016 comprehensive evidence review resulted in five individual-level intervention categories, with four of those categories containing a sufficiently consistent and rigorous evidence base to be highlighted here. The fifth category, interventions for postnatal women, was identified as an area with limited evidence from systematic reviews and meta-analyses that warranted further study.
Application of behavioral theories and models to inform interventions.
The current evidence base supports the application of behavioral theories and models (e.g., Social Cognitive Theory, the Transtheoretical Model, Theory of Planned Behavior, Self-Determination Theory) and strategies drawn from such theories in developing effective programs at the individual level as well as at other levels of impact (9). For example, a meta-analysis of 82 randomized controlled trials (RCT) of theory-based interventions in more general adult populations reported an overall average effect size of 0.31 (95% confidence interval [CI], 0.24–0.37) relative to controls (34). Among the most commonly reported behavior change techniques associated with physical activity change were self-monitoring of behavior and intention formation. Several techniques within theory-based behavioral interventions were identified as areas warranting additional study, including providing rewards (conditional and unconditional) for exercise session attendance and understanding the effects of achieving physical activity goals across a variety of age groups.
Interventions specific to youth and older adults.
Notably, the evidence base at the individual level has expanded well beyond the general adult populations constituting the early targets of intervention to important population subgroups, including youth and older adults. Robust evidence exists for individual-level interventions aimed specifically at youth (9). Effective programs often have included in-person education and experiential activities (i.e., exercise classes), which can be enhanced through incorporating the family as part of the intervention (14). Examples of such interventions include in-person and Web-based education, hands on experiential activities (e.g., supervised exercise, dance, or sports and recreational activities), and replacing sedentary behaviors with increased physical activity (14).
Interventions aimed specifically at older adults have been shown to be effective in promoting increased physical activity across intervention periods of a year or more (9). Among the types of strategies that have been reported to be effective among older adult samples are individual or group-based advice and counseling, problem-solving around barriers to physical activity, social support, modeling and similar demonstrations of the physical activities being targeted, and use of rewards linked to behavior change (13).
Extending the Reach of Individual-Level Interventions—Peer-Led Interventions
While in-person individual-level approaches provide a flexible means for tailoring programs to the needs of each person, they often require a level of staff time and support that can be costly and/or infeasible to deliver to larger groups of people or in certain contexts (e.g., under-resourced communities). The growth of information and communication technologies (described in a subsequent section) as well as peer-led programs can provide a level of personalized advice and support in a manner that may reduce costs and enhance reach to a wider and more diverse audience. For example, there is consistent evidence supporting the effectiveness of peer-led behavioral self-management interventions such as the Chronic Disease Self-Management Program in attaining meaningful increases in physical activity among older adults and persons with chronic conditions, particularly over the short-term (e.g., 3 months) (16). Examples of original research supporting the longer-term effectiveness (1 yr or longer) of peer-engaged in-person or phone-delivered physical activity interventions in healthy midlife and older adults also are available (35,36). However, it is also important to further evaluate the impacts of such physical activity programs on important health outcomes of interest, such as physical function, which a recent meta-analysis in this area suggested may be more difficult to attain with such interventions (37).
Community-Level Strategies and Approaches
Community interventions can be aimed at the entire community (i.e., community-wide) or at particular community settings. Among the settings that have been frequently targeted for physical activity intervention are educational, housing, recreational, worksite, primary care, and faith-based settings. They offer potentially convenient locations for reaching diverse groups of people and, depending on the setting or location, provide a means for targeting different age groups using a range of strategies (38).
As noted earlier, the Committee’s evidence review focused on those eligible systematic reviews, meta-analyses, and government reports published between 2011 and 2016. The available evidence during that time frame allowed us to identify robust evidence supporting contact-intensive community-wide interventions and interventions occurring in school settings. Meanwhile, other community setting reviews captured during the 2011 to 2016 review period (i.e., childcare and preschool settings, faith-based interventions, primary care settings, worksites, nurse-delivered interventions in home or other community settings), while promising, presented less rigorous intervention evidence. We present highlights from the two areas (contact-intensive community-wide interventions and school settings) that received particularly rigorous evidence support during the targeted review period.
Community-wide interventions.
Community-wide interventions that use intensive contact with the majority of the target population over time can increase physical activity across the population (9). Although a large number of community-wide interventions that included physical activity promotion have occurred throughout the world, a relatively smaller number have been able to report sufficiently intensive contact with the majority of community members over time to produce significant physical activity increases across the target population. One example is a study conducted in China (39) that reported a significant increase in community-wide physical activity levels in three urban areas of Hangzhou city. The types of intervention strategies that were used included door-to-door distribution of instructions and information, identification and support of community members at increased chronic disease risk, and health counselor advising. The effectiveness of this type of community-wide intervention has been supported by a recent 5-yr cluster-randomized trial evaluating the effects of a community-wide intervention on population-level physical activity among midlife and older adults in Japan (40). The percent of adults achieving recommended levels of regular physical activity in the communities randomized to the social marketing-based intervention (n = 9) increased by 4.6 percentage points over 5 yr relative to the control communities (n = 3). The intervention, which consisted of targeted educational outreach, information delivery through different media channels, and different types of social support, was effective in promoting aerobic, muscle strengthening, and flexibility activities in those communities in which these different physical activity types were specifically targeted. Of note, however, in the intervention community in which all three types of physical activity were targeted simultaneously, less positive change occurred relative to those communities targeting fewer physical activity types (40). Although promising evidence for positive physical activity changes in some portions of the community has been reported in other studies in the United States and elsewhere, it remains a challenge to reach broad segments of communities with sufficient intervention duration and intensity to produce sustainable changes, particularly when interventions often include strategies to improve other risk factors beyond physical activity (9).
Overall, there is an extensive literature evaluating community-wide as well as setting-specific community interventions for physical activity promotion (9,41). The robustness of the evidence overall could be improved by using more rigorous study designs and assessment strategies, longer intervention time frames, and consistent applications of intervention fidelity processes and procedures (9).
School interventions.
Among the most robust literature available in the physical activity promotion field is that aimed at promoting physical activity in school settings (41). Effective multicomponent school-based interventions, such as CATCH (17) and SPARK (18), include structural changes in physical education (PE) classes, classroom activity breaks, activity sessions occurring before and after school, active transport to and from school, behavioral skill-building to promote physical activity participation, and the provision of after-school spaces and equipment for physical activity (17,18). Such interventions have been found to significantly increase physical activity during school hours relative to controls in primary school and adolescent youth (9). A number of studies also have shown that implementing a well-designed PE curriculum with appropriately trained teachers can improve amounts of within-class moderate-to-vigorous physical activity. For example, a meta-analysis in this area (19) reported a 24% increase in active learning time during PE in the intervention groups relative to controls irrespective of age, sex, and intervention duration (standard mean difference [SMD], 0.62; 95% CI, 0.39–0.84).
Communication Environment-Level Strategies and Approaches
The communication environment includes a large and growing group of ICT that have been used increasingly to promote regular physical activity. The ICT strategies are typically tested with individuals but can be deployed widely within a larger communication and technology environment, thus having the potential for broad reach. Given this observation along with the unique delivery channels represented in this emerging field, we chose to treat ICT interventions as a distinct level of impact (8). Such interventions have the potential for providing more dynamic intervention delivery (e.g., “just-in-time” strategies) than those accessed in the more traditional in-person interventions found at the individual level. Typical delivery channels used include technologies such as wearable activity monitors, cell or smart phones, and the Internet. Among the advantages of ICT intervention approaches are their ability, similar to the individual-level approaches highlighted earlier, to personalize information, behavior change strategies, and support to the varying contexts and needs of individual users while providing a means for readily documenting the information delivered and responses received. For example, the passive sensing capabilities of smartphones and similar mobile devices can provide near continuous, lower burden physical activity tracking abilities, as well as a means for capturing social and environmental contextual information that allow delivery of “just in time” personalized advice and support (42). In addition, in light of accelerating smartphone ownership (69%) in the US population and other developed countries (43), as well as in a growing number of developing economies worldwide (46% own smartphones) (43), the population reach of mobile device-based interventions can potentially rival or eclipse community interventions.
The evidence evaluated during the 2011 to 2016 comprehensive review that focused on ICT interventions was organized into seven categories, with five of those categories containing a sufficiently consistent and rigorous evidence base to be highlighted here. The two categories not included, which represent areas needing further systematic study, were active video games promoting active play or exercise and interventions delivered via social media. A recent meta-analysis of 18 RCT of active video games focusing on healthy, community-dwelling older adults suggested that use of such games can promote short-term mobility and balance gains in healthy populations (44). However, their impacts in older adults with balance or mobility limitations are less clear. In addition, while program adherence rates were reported overall to be reasonably high, intervention durations in this area remain brief (i.e., from 3 to 20 wk) (44). With respect to social media, a recent systematic review of physical activity interventions using a specific social media platform—Facebook—found that only two of eight interventions reviewed resulted in significant physical activity increases relative to controls (45). As represented in this review, this nascent intervention field continues to suffer from weak designs, lack of theory-based content, small sample sizes, and short follow-up periods (45).
Wearable activity monitors.
The evidence reviewed supports the use of wearable activity monitors, such as step-counters and accelerometers, when used jointly with specific behavioral strategies such as goal-setting, behavioral coaching, and/or group-based support for increasing regular physical activity in general adult populations as well as some specific adult subgroups. In general adult populations, a meta-analysis of 12 trials using activity monitors reported a significant, albeit small, increase in physical activity levels relative to minimal-attention or usual care controls (SMD, 0.25; 95% CI, 0.04–0.49) (20). In this review, setting a specific physical activity goal appeared to enhance physical activity outcomes irrespective of whether it was a self-chosen goal versus a goal specified by the intervention team (e.g., a 10,000-step goal) (20). The importance of setting a specific physical activity goal in combination with an activity monitor was also supported in a meta-analysis of patients with type 2 diabetes (21). In this meta-analysis, setting a specific physical activity goal resulted in a significant mean increase of 3200 steps per day relative to controls, whereas step-counter use without a goal did not increase physical activity significantly relative to control. Use of a step diary also was efficacious in increasing physical activity (21). Significant positive effects of behavioral interventions that included activity monitors in comparison with waitlist or usual care interventions were also found in a meta-analysis of adults with overweight or obesity (22).
Among some of the challenges accompanying wearable activity monitor use are the timing of their use in physical activity programs (e.g., during the adoption vs maintenance phases of behavior change) (46), and methods for extending the duration of use.
Telephone-assisted interventions.
Decades of physical activity intervention work have supported the use of physical activity advice and support delivered by phone for general adult as well as older adult populations, with effect sizes in the moderate range or stronger (i.e., d > 0.5) (47). Longer-term interventions (i.e., 12 months or longer) have been associated with greater effectiveness, and at least two large-scale dissemination studies targeting diverse groups of midlife and older adults and including trained community staff as well as volunteers have reported physical activity increases of a magnitude similar to those obtained in RCT (47–49). Of interest, a review of a small number of trials that combined physical activity and dietary interventions in general adult and older adult populations suggested that including a dietary intervention might at times hamper physical activity change (47). This finding was supported in a subsequent RCT in which the timing of the introduction of these two health behavior interventions was manipulated systematically (i.e., sequential or simultaneous ordering) (50). Greater increases in physical activity occurred when the physical activity intervention was initiated from the beginning, as opposed to when it was added following initiation of a dietary intervention (50).
Web-based or Internet-delivered interventions.
Systematic reviews and meta-analyses of interventions delivered remotely over a web page or the Internet and that include educational components have reported small but positive intervention effects in general adult populations (6); for example, one meta-analysis found a d = 0.14 when comparing such interventions with control arms (23). Larger effect sizes have been reported for studies which screened out already active individuals (d = 0.37) (23), while targeting physical activity alone or in combination with other health behaviors (i.e., dietary behaviors, weight management behaviors) produced similar effect sizes (23). Web-based or Internet interventions may also result in significant short-term physical activity increases (i.e., typically less than 6 months) in persons with type 2 diabetes when compared with controls (24), although this literature is less well developed and more variable than the literature for general adult populations.
Computer-tailored print interventions.
These programs collect user information via mailed surveys, which is then used to develop computer-tailored mailings that include personalized physical activity advice and support (51). Current evidence indicates that, in general adult populations, such interventions have a positive, albeit small effect (d = 0.12 to 0.35) on physical activity levels, particularly in the short-term (i.e., 6 months or less) (51). Commonly used tailoring variables upon which to personalize the mailed advice were psychosocial and behavioral variables (e.g., perceived barriers to activity; motivational readiness to change) (51).
Mobile phone interventions.
In generally healthy adult populations, the relatively small number of mobile phone interventions that include or focus primarily on text-messaging have reported significant positive effects, relative to controls, on physical activity levels (9). Some of the effect sizes reported in the available reviews have been notable (i.e., an average of 0.40 or greater) (26). In a number of studies, text-messaging was used primarily to provide simple cues or messages related to becoming more active (9).
While no reviews of text-messaging interventions in youth were found during the 2011 to 2016 search period, reviews were identified evaluating the efficacy of physical activity smartphone apps in youth. Occurring in school and other community settings and across diverse countries, the evidence indicates small to moderate effects on physical activity levels in boys and girls, although at least one systematic review reported Cohen’s d coefficients of 0.36 to 0.86 (27). When types and combinations of behavioral strategies were evaluated systematically, differences were found in children relative to adolescents. For example, while general encouragement, modeling and instruction predicted positive physical activity effects in children (27), providing teens with specific instruction tended to reduce the effects of the intervention (27).
While no systematic reviews were found during the search period evaluating smartphone apps in adults, a recent systematic review and meta-analysis of 18 RCT in this area indicated some promising results for adults, with small to moderate increases in device-based physical activity when measured in minutes per day (SMD, 0.43; 95% CI, 0.03–0.82) (52). However, most studies included additional intervention components (e.g., counseling sessions), which could result in larger effects than if the smartphone app was offered alone (53).
Physical Environment and Policy-Level Strategies and Approaches
Physical environment-level approaches can be defined broadly as the evaluation and targeting of features in the built environment that may affect physical activity levels, including pedestrian or bicycling infrastructure, ready access to stairs, and access to indoor and outdoor recreational facilities, including parks, trails, and gyms (9). Policy-level approaches, meanwhile, include local ordinances and laws, as well as organizational policies and practices that can influence physical activity (9). Over the last several decades there has been an increase in research worldwide evaluating the associations between physical environment factors and levels of physical activity (38). In addition to the large number of cross-sectional observational designs that have been used in this field, more rigorous longitudinal and natural experimental designs have been added more recently to the literature (29,38). Environmental and policy-level evidence can set the stage for intervention approaches that can span large portions of the population, therefore having a potentially larger impact and “reach” than interventions at other levels of impact (e.g., the individual-level). However, environmental and policy approaches are also, by their often complex and multifactorial nature, constrained by the real-world challenges that can make it difficult to implement as well as evaluate them. These challenges notwithstanding, four approaches at this level, described below, have achieved consistent evidence support and are important public health strategies to consider in the physical activity area.
Point-of-decision prompts promoting stair use.
Systematic reviews of short-term point-of-decision studies (typically ranging from 4 to 12 wk) conducted in a variety of community settings (e.g., shopping malls, transit hubs, worksites) have reported increases in stair use in the majority of studies evaluated (e.g., 77% of 67 studies reviewed) (28). Most of the studies reviewed used quasi-experimental designs (e.g., interrupted time series, controlled before-and-after studies) (28). Percent stair use increases have ranged from 0.3% to 34.7% (28). Some studies suggest that responses to the prompts may vary by age, sex, and weight status (9).
Built environment characteristics that support active transport to destinations.
The evidence reviewed reported that street connectivity, a mix of commercial, residential and public land uses, and similar types of characteristics, along with Safe Routes to School programs, are positively associated with greater walking and cycling for transport among adults, older adults, and children relative to environments lacking such elements (9,38). For instance, the results of a large natural experiment (RESIDE) (29) found increases across a 7-yr period in active transport among residents moving to neighborhoods that they perceived as safer for walking and bicycling relative to those who did not move to such neighborhoods. The importance of walkability and similar environmental features for active transport and other forms of physical activity additionally has been supported by a recent large-scale study of US smartphone app users (42). This study showed that women may be particularly sensitive to the effects of walkability features in terms of their daily physical activity levels.
Community design and characteristics that support recreational physical activity.
Readily usable and safe walking and cycling infrastructure and related built environment features (e.g., sidewalks, street connectivity, absence of heavy traffic) are also positively associated with greater amounts of recreational physical activity among both children and adults relative to environments without such infrastructure. For example, one meta-analysis reported that absence of heavy traffic was associated with significantly more walking and leisure-time physical activity in adults (odds ratio, 1.22; 95% CI, 1.08–1.37) (54).
Access to indoor and/or outdoor recreation facilities or outlets.
The evidence review additionally showed that access to indoor (e.g., gyms or fitness centers) or outdoor recreational facilities (e.g., parks, trails, open streets programs which temporarily reduce motor vehicle access in specified locations) is positively associated with greater physical activity among both children and adults compared to environments without such facilities or outlets (9). For example, a meta-analysis reported that greater access to such facilities among adults was related to more physical activity, with an odds ratio of 1.20 (95% CI, 1.06–1.34) (54). In addition, some intervention studies have shown that combining a built environment approach (e.g., building a new footpath) with a public education or skills-building program has resulted in increased physical activity levels (55).
Policy-specific approaches to physical activity promotion.
In contrast to the built environment arena, little evidence was found during the 2011 to 2016 evidence search period evaluating the impacts of specific policies related to land use, urban sprawl, and similar environmental design factors on physical activity levels. Only one review was found during this search period that focused specifically on policy approaches for physical activity programs (56), and this review was primarily descriptive in nature. It identified land use policies and school physical activity policies as among the most promising types of policies that have been studied to date. In a review that included five studies of urban sprawl and physical activity, 80% found a relationship between less sprawl and more physical activity of different types (e.g., active transport, recreational, total physical activity) (38), and one prospective study reported positive impacts over time of urban sprawl mitigation policies on physical activity (57).
SUMMARY OF KEY INTERVENTION COMPONENTS FOR PHYSICAL ACTIVITY PROMOTION AT EACH LEVEL
For investigators designing and implementing physical activity interventions, a number of key intervention components were highlighted above. At the individual level, self-monitoring of behavior and intention formation are commonly related to increased physical activity. At the community level, door-to-door distribution of instructions and information, identification and support of community members at increased chronic disease risk, and health counselor advising can be important components, as can well-structured PE classes and environmental changes in school settings. At the communication environment level, goal setting was found to be particularly important, and assessing perceived barriers to activity and motivational readiness to change are useful. At the physical environment/policy level, street connectivity, a mix of commercial, residential, and public land uses and similar types of built environment characteristics, along with Safe Routes to School programs, are positively associated with greater walking and cycling for transport among adults, older adults, and children relative to environments lacking such elements.
RESULTS OF THE EVIDENCE REVIEW: INTERVENTIONS TO REDUCE SEDENTARY BEHAVIOR
A summary of the intervention categories for which sufficiently consistent evidence was found supporting sedentary behavior reduction among youth and in worksites is summarized in Table 1 and briefly described below. Interventions to reduce sedentary behavior among adults were identified as an area warranting further study. Given the relative newness of this area, the size of the evidence base was smaller than that for physical activity interventions (9). However, the evidence available tended toward more rigorous methods (i.e., meta-analyses of RCT).
Youth interventions.
The 2011 to 2016 evidence review found support for sedentary behavior interventions in youth which typically were delivered in school settings, generally lasted at least 6 months, and targeted primarily reductions in television viewing and other screen-time activities (9). Combinations of strategies were often used in these studies consisting of school-based counseling, parental involvement, tailored feedback regarding screen-time activities, and the use of screen allowance devices to limit TV and video game viewing time. Taken together, the reviews indicated small but consistent self-reported sedentary behavior reduction effects (e.g., a mean reduction of about 20 min·d−1) irrespective of whether the intervention was delivered alone or as part of a multiple behavior change program (31). A more recent review of 0- to 5-yr-old children showed similar reductions in sedentary time (i.e., mean difference of 18.91 fewer sedentary minutes per day relative to control; 95% CI, −33.31 to −4.51) (58). It was unclear from the evidence reviewed whether such consistent reductions in sedentary behavior would be sufficiently large to produce positive health effects in this age group.
Worksite interventions.
We found consistent evidence supporting the effectiveness of sedentary reduction interventions with worksite populations that performed their work duties typically while seated (9). This was particularly the case for interventions that targeted physical changes to work stations (e.g., sit-stand workstations), which reported medium to large effect sizes based on device-measured sedentary behaviour (i.e., mean difference of 72.78 fewer sedentary minutes per 8-h workday relative to control, 95% CI, −104.92 to −40.64) (33). Such effects were strengthened when the workstation changes were combined with educational (e.g., e-newsletters), social (e.g., workgroup contests), and other environmental (e.g., managerial support, signage) support strategies (e.g., mean difference of −88.80 min per 8-h workday relative to control) (33). Evidence of efficacy in the meta-analyses also appeared to be somewhat diminished when walking workstations and cycle ergometers were used (59).
Methodological constraints included small sample sizes and short-term intervention durations (3 to 6 months) (59). However, these constraints have been addressed in recent trials using cluster-randomized designs that demonstrated similar effect sizes to those observed in the meta-analyses (60,61). In addition, a recently published cluster-randomized trial resulted in reductions in body fat percentage at the end of the multicomponent intervention (62).
DISCUSSION AND FUTURE RECOMMENDATIONS
The above highlights from the 2018 Physical Activity Guidelines Advisory Committee Scientific Report underscore the range of effective interventions for promoting regular physical activity at different life stages. Of particular note are the promising number of technology-based approaches that can effectively promote short-term physical activity increases. An ongoing challenge for the field as a whole is to identify the best methods for promoting sustained physical activity for different population groups within different environmental and cultural contexts as well as life stages. One way to increase sustained physical activity is to target several levels of the social ecological framework within the same intervention. Unfortunately, such multilevel interventions have not been commonplace to date. In addition, while the type and nature of the physical activity (e.g., intensity, duration, frequency, its enjoyability and related factors) can influence the effectiveness of an intervention for different population groups, few of the reviews, meta-analyses, and reports that were evaluated presented systematic information on the associations of such program factors with intervention success. The field as a whole would benefit from further research in this area.
The evidence also supports the effectiveness of those sedentary behavior reduction approaches that have received systematic study to date. Such evidence notwithstanding, there remains much that we need to know about how to most efficiently and effectively promote these key health behaviors among the significant proportion of the population who are substantially sedentary or insufficiently active on a regular basis. Among other important areas for further systematic investigation are the following:
Incorporate more diverse population subgroups, including broader age groups, men as well as women, diverse racial/ethnic groups, and vulnerable and underrepresented population groups (e.g., lower-income residents, patient subgroups).
Develop efficient methods for collecting cost data on all interventions being tested to inform cost-benefit and cost-effectiveness comparisons across the field as a whole (63).
Study the most effective methods for disseminating to real-world settings those physical activity interventions that work, a number of which have been highlighted in this review. As part of this dissemination process, it is critical that specific efforts are made to reach traditionally underserved segments with interventions adapted to their needs. Doing this can help to ensure that all population groups can benefit from interventions shown to be effective. Additionally, it will be important to systematically evaluate such dissemination efforts to better capture actual intervention effects when delivered in the community (48).
As a complement to dissemination approaches, conduct implementation research as a means of identifying methods for enhancing the uptake and implementation of programs shown to be effective to ensure that they maintain their effectiveness when delivered at scale.
Test strategies across different levels of impact, as has been done in school settings, to determine which combinations achieve the greatest effects on different modes of physical activity across the week and in different population groups.
Test methods for sustaining physical activity increases over time and across different contexts, given that inactivity is most appropriately conceptualized as a “chronic condition,” as opposed to an acute condition that can be “cured” with a finite intervention without targeting maintenance.
Continue the systematic work aimed at increasing our understanding of the most effective strategies and mechanisms of action underlying physical activity interventions. An example of such an approach, based on international scientific consensus-building and evidence review and analysis, aims to build a taxonomy of behavior change techniques for physical activity and other health behaviors (64). Such a taxonomy can serve as the starting point to identify the most effective strategies and mechanisms for behavior change for different population groups, contexts, and outcomes.
Finally, although this article highlights those interventions reviewed for which the evidence supported intervention effectiveness, many such interventions were noted to have small to moderate effects in increasing physical activity. Among the aims of the future recommendations described above are to help facilitate the development of increasingly robust multicomponent and multiple-level interventions that can strengthen intervention effects among different population segments. This point notwithstanding, it has been noted that even small effects of an intervention can translate into meaningful public health impacts when the intervention is disseminated effectively across a large segment of the population (65,66). This observation underscores our call for an increased focus on broad dissemination of the group of interventions that show effectiveness, even if an intervention might alone produce a reasonably small individual-level effect. With careful attention to ensuring that all groups benefit from the knowledge that has been gained in the physical activity promotion field, the untapped promise for the nation’s health offered through a physically active lifestyle can be more fully realized.
Acknowledgments
The authors gratefully acknowledge the members of the 2018 Physical Activity Guidelines Advisory Committee for their advice and input. The authors thank Benjamin Chrisinger, PhD, Eric Hyde, MPH, and Kyle R. Sprow, MPH in supporting the activities of the Physical Activity Promotion Subcommittee of the 2018 Physical Activity Guidelines Advisory Committee.
Conflict-of-Interest and Disclosure of Funding statements: The authors report no conflicts of interest. The findings and conclusion of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. No funding was received for this work.
Footnotes
This article is being published as an official pronouncement of the American College of Sports Medicine. This pronouncement was reviewed for the American College of Sports Medicine by members-at-large and the Pronouncements Committee. Disclaimer: Care has been taken to confirm the accuracy of the information present and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this publication and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. Application of this information in a particular situation remains the professional responsibility of the practitioner; the clinical treatments described and recommended may not be considered absolute and universal recommendations.
REFERENCES
- 1.U.S. Department of Health & Human Services. Physical activity. Healthy people 2020 objective data search website 2018. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/physical-activity/objectives.
- 2.Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. [DOI] [PubMed] [Google Scholar]
- 3.The Child & Adolescent Health Measurement Initiative (CAHMI). 2016 National Survey of Children’s Health. Washington, DC: Data Resource Center for Child and Adolescent Health; 2016. [Google Scholar]
- 4.Watson KB, Carlson SA, Gunn JP, et al. Physical inactivity among adults aged 50 years and older—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(36):954–8. [DOI] [PubMed] [Google Scholar]
- 5.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. [DOI] [PubMed] [Google Scholar]
- 6.Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012; 380(9838):247–57. [DOI] [PubMed] [Google Scholar]
- 7.Physical Activity Guidelines Advisory Committee. Report of the Physical Activity Guidelines Advisory Committee, 2008. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 8.Napolitano MA, Lewis B, Whiteley JA, Ives A, Marcus B. Theoretical Foundations of Physical Activity Behavior Change. ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription. 7th ed. New York, NY: Lippincott, Williams & Wilkins; 2013. pp. 730–44. [Google Scholar]
- 9.Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services; 2018. p. 2018. [Google Scholar]
- 10.Torres A, Tennant B, Ribeiro-Lucas I, Vaux-Bjerke A, Piercy K, Bloodgood B. Umbrella and systematic review methodology to support the 2018 physical activity guidelines advisory committee. J Phys Act Health. 2018;15(11):805–10. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 12.Mitchell MS, Goodman JM, Alter DA, et al. Financial incentives for exercise adherence in adults: systematic review and meta-analysis. Am J Prev Med. 2013;45(5):658–67. [DOI] [PubMed] [Google Scholar]
- 13.French DP, Olander EK, Chisholm A, Mc Sharry J. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Ann Behav Med. 2014;48(2):225–34. [DOI] [PubMed] [Google Scholar]
- 14.Cushing CC, Brannon EE, Suorsa KI, Wilson DK. Systematic review and meta-analysis of health promotion interventions for children and adolescents using an ecological framework. J Pediatr Psychol. 2014; 39(8):949–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown HE, Atkin AJ, Panter J, Wong G, Chinapaw MJ, van Sluijs EM. Family-based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev. 2016;17(4):345–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Best KL, Miller WC, Eng JJ, Routhier F. Systematic review and meta-analysis of peer-led self-management programs for increasing physical activity. Int J Behav Med. 2016;23(5):527–38. [DOI] [PubMed] [Google Scholar]
- 17.Luepker RV, Perry CL, McKinlay SM, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The child and adolescent trial for cardiovascular health. CATCH collaborative group. JAMA. 1996;275(10):768–76. [DOI] [PubMed] [Google Scholar]
- 18.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, play and active recreation for kids. Am J Public Health. 1997; 87(8):1328–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lonsdale C, Rosenkranz RR, Peralta LR, Bennie A, Fahey P, Lubans DR. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev Med. 2013;56(2):152–61. [DOI] [PubMed] [Google Scholar]
- 20.Goode AP, Hall KS, Batch BC, et al. The impact of interventions that integrate accelerometers on physical activity and weight loss: a systematic review. Ann Behav Med. 2017;51(1):79–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qiu S, Cai X, Chen X, Yang B, Sun Z. Step counter use in type 2 diabetes: a meta-analysis of randomized controlled trials. BMC Med. 2014;12(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Vries HJ, Kooiman TJ, van Ittersum MW, van Brussel M, de Groot M. Do activity monitors increase physical activity in adults with overweight or obesity? A systematic review and meta-analysis. Obesity (Silver Spring). 2016;24(10):2078–91. [DOI] [PubMed] [Google Scholar]
- 23.Davies CA, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int J Behav Nutr Phys Act. 2012;9:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Connelly J, Kirk A, Masthoff J, MacRury S. The use of technology to promote physical activity in type 2 diabetes management: a systematic review. Diabet Med. 2013;30(12):1420–32. [DOI] [PubMed] [Google Scholar]
- 25.Bossen D, Veenhof C, Dekker J, de Bakker D. The effectiveness of self-guided web-based physical activity interventions among patients with a chronic disease: a systematic review. J Phys Act Health. 2014; 11(3):665–77. [DOI] [PubMed] [Google Scholar]
- 26.Buchholz SW, Wilbur J, Ingram D, Fogg L. Physical activity text messaging interventions in adults: a systematic review. Worldviews Evid-Based Nurs. 2013;10(3):163–73. [DOI] [PubMed] [Google Scholar]
- 27.Brannon EE, Cushing CC. A systematic review: is there an app for that? Translational science of pediatric behavior change for physical activity and dietary interventions. J Pediatr Psychol. 2015;40(4): 373–84. [DOI] [PubMed] [Google Scholar]
- 28.Jennings CA, Yun L, Loitz CC, Lee EY, Mummery WK. A systematic review of interventions to increase stair use. Am J Prev Med. 2017;52(1):106–14. [DOI] [PubMed] [Google Scholar]
- 29.Giles-Corti B, Bull F, Knuiman M, et al. The influence of urban design on neighbourhood walking following residential relocation: longitudinal results from the RESIDE study. Soc Sci Med. 2013;77:20–30. [DOI] [PubMed] [Google Scholar]
- 30.Cerin E, Nathan A, van Cauwenberg J, Barnett DW. The neighbourhood physical environment and active travel in older adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Grieken A, Ezendam NP, Paulis WD, van der Wouden JC, Raat H. Primary prevention of overweight in children and adolescents: a meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int J Behav Nutr Phys Act. 2012;9(2):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friedrich RR, Polet JP, Schuch I, Wagner MB. Effect of intervention programs in schools to reduce screen time: a meta-analysis. J Pediatr (Rio J). 2014;90(3):232–41. [DOI] [PubMed] [Google Scholar]
- 33.Chu AH, Ng SH, Tan CS, Win AM, Koh D, Müller-Riemenschneider F. A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers. Obes Rev. 2016;17(5):467–81. [DOI] [PubMed] [Google Scholar]
- 34.Gourlan M, Bernard P, Bortolon C, et al. Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomised controlled trials. Health Psychol Rev. 2016;10:50–66. [DOI] [PubMed] [Google Scholar]
- 35.Buman MP, Giacobbi PR Jr, Dzierzewski JM, et al. Peer volunteers improve long-term maintenance of physical activity with older adults: a randomized controlled trial. J Phys Act Health. 2011;8(2 Suppl):S257–66. [PMC free article] [PubMed] [Google Scholar]
- 36.Castro CM, Pruitt LA, Buman MP, King AC. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychol. 2011;30(3):285–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burton E, Farrier K, Hill KD, Codde J, Airey P, Hill AM. Effectiveness of peers in delivering programs or motivating older people to increase their participation in physical activity: systematic review and meta-analysis. J Sports Sci. 2018;36(6):666–78. [DOI] [PubMed] [Google Scholar]
- 38.Community Preventive Services Taskforce. The Community Guide on Physical Activity: Built Environment Approaches Combining Transportation System Interventions with Land Use and Environmental Design. Atlanta, GA: Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 39.Gao F, Liu QM, Ren YJ, He PP, LV J, Li LM. Assessment on the short-term impact regarding the community-based interventions to improve physical activities in three urban areas of Hangzhou city. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34(6):582–5. [PubMed] [Google Scholar]
- 40.Kamada M, Kitayuguchi J, Abe T, et al. Community-wide intervention and population-level physical activity: a 5-year cluster randomized trial. Int J Epidemiol. 2018;47(2):642–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Physical Activity Guidelines for Americans Midcourse Report Subcommittee of the President’s Council on Fitness SN. Physical Activity Guidelines for Americans Midcourse Report: Strategies to Increase Physical Activity Among Youth. Washington, DC: U.S. Department of Health and Human Services; 2012. [Google Scholar]
- 42.Althoff T, Sosic R, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547(7663):336–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ericsson.com. Ericsson Mobility Report 2017. [July 23, 2017]. Available from: https://www.ericsson.com/en/mobility-report.
- 44.Taylor LM, Kerse N, Frakking T, Maddison R. Active video games for improving physical performance measures in older people: a meta-analysis. J Geriatr Phys Ther. 2018;41(2):108–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferrer DA, Ellis R. A review of physical activity interventions delivered via Facebook. J Phys Act Health. 2017;14(10):823–33. [DOI] [PubMed] [Google Scholar]
- 46.Jakicic JM, Davis KK, Rogers RJ, et al. Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: the IDEA randomized clinical trial. JAMA. 2016;316(11):1161–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med. 2012;42(1):81–8. [DOI] [PubMed] [Google Scholar]
- 48.Wilcox S, Dowda M, Leviton LC, et al. Active for life: final results from the translation of two physical activity programs. Am J Prev Med. 2008;35(4):340–51. [DOI] [PubMed] [Google Scholar]
- 49.Hooker SP, Seavey W, Weidmer CE, et al. The California active aging community grant program: translating science into practice to promote physical activity in older adults. Ann Behav Med. 2005; 29(3):155–65. [DOI] [PubMed] [Google Scholar]
- 50.King AC, Castro CM, Buman MP, Hekler EB, Urizar GG Jr, Ahn DG. Behavioral impacts of sequentially versus simultaneously delivered dietary plus physical activity interventions: the CALM trial. Ann Behav Med. 2013;46(2):157–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Short CE, James EL, Plotnikoff RC, Girgis A. Efficacy of tailored-print interventions to promote physical activity: a systematic review of randomised trials. Int J Behav Nutr Phys Act. 2011;8:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gal R, May AM, van Overmeeren EJ, Simons M, Monninkhof EM. The effect of physical activity interventions comprising wearables and smartphone applications on physical activity: a systematic review and meta-analysis. Sports Med Open. 2018;4(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duncan MJ, Spence JC, Mummery WK. Perceived environment and physical activity: a meta-analysis of selected environmental characteristics. Int J Behav Nutr Phys Act. 2005;2:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hunter RF, Christian H, Veitch J, Astell-Burt T, Hipp JA, Schipperijn J. The impact of interventions to promote physical activity in urban green space: a systematic review and recommendations for future research. Soc Sci Med. 2015;124:246–56. [DOI] [PubMed] [Google Scholar]
- 56.Brennan LK, Brownson RC, Orleans CT. Childhood obesity policy research and practice: evidence for policy and environmental strategies. Am J Prev Med. 2014;46(1):e1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aytur SA, Rodriguez DA, Evenson KR, Catellier DJ. Urban containment policies and physical activity. A time-series analysis of metropolitan areas, 1990–2002. Am J Prev Med. 2008;34(4):320–32. [DOI] [PubMed] [Google Scholar]
- 58.Downing KL, Hnatiuk JA, Hinkley T, Salmon J, Hesketh KD. Interventions to reduce sedentary behaviour in 0–5-year-olds: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2018;52(5):314–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shrestha N, Ijaz S, Kukkonen-Harjula KT, Kumar S, Nwankwo CP. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev. 2015;1:Cd010912. [DOI] [PubMed] [Google Scholar]
- 60.Healy GN, Eakin EG, Owen N, et al. A cluster randomized controlled trial to reduce office workers’ sitting time: effect on activity outcomes. Med Sci Sports Exerc. 2016;48(9):1787–97. [DOI] [PubMed] [Google Scholar]
- 61.Edwardson CL, Yates T, Biddle SJH, et al. Effectiveness of the stand more AT (SMArT) work intervention: cluster randomised controlled trial. BMJ. 2018;363:k3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Danquah IH, Kloster S, Holtermann A, et al. Take a stand!—a multi-component intervention aimed at reducing sitting time among office workers-a cluster randomized trial. Int J Epidemiol. 2017; 46(1):128–40. [DOI] [PubMed] [Google Scholar]
- 63.Rose T, Barker M, Maria Jacob C, et al. A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J Adolesc Health. 2017;61(6):669–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26(11):1479–98. [DOI] [PubMed] [Google Scholar]
- 65.Rose G Sick individuals and sick populations. Int J Epidemiol. 2001; 30(3):427–32. [DOI] [PubMed] [Google Scholar]
- 66.Abrams DB, Orleans CT, Niaura RS, Goldstein MG, Prochaska JO, Velicer W. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: a combined stepped-care and matching model. Ann Behav Med. 1996; 18(4):290–304. [DOI] [PubMed] [Google Scholar]


