ABSTRACT
Objective:
The aim of this study was to adapt the Prolonged Grief Disorder – Caregiver Form (PG-12), which is used to measure grief symptoms of caregivers providing care to their relatives with a chronic diseases that cause functional disability to Turkish and to investigate its psychometric properties. We also aimed to investigate the prevalence of prolonged grief disorder in the caregiver sample.
Method:
The sample consisted of 120 adult participants (70.8% female) who acted as caregivers. The participants were administered Prolonged Grief Disorder-Caregiver Form, Zarit Caregiver Burden Scale, Beck Depression Inventory and Life Satisfaction Scale.
Results:
The results of confirmatory factor analysis showed that the single-factor structure of PG-12, consistent with the original form, was supported. PG-12 scores showed a positive correlation with depression and caregiver burden scores and a negative correlation with life satisfaction scores. The internal consistency coefficient of the scale was 0.85. The prevalence of prolonged grief disorder calculated using PG-12 was found to be 31.66%.
Conclusion:
The results showed that PG-12 is a valid and reliable tool for assessing the grief symptoms of people who provides care for a relative. In addition, the prevalence of prolonged grief disorder in our study population was high. Additional studies are needed in Turkey to confirm this rate and develop new strategies for caregivers.
Keywords: Prolonged Grief Disorder, Caregiver, Anticipatory Grief, Validity, Reliability
INTRODUCTION
Along with developments in medicine, the pharmaceutical industry, and technology, people’s average life expectancy has increased over time. The period between becoming ill and dying was shorter a few centuries ago, but nowadays people can survive for many years, even when they suffer from various chronic diseases (World Health Association 2011). This increase in survival times for people with chronic diseases has created a need for long-term treatment and care. The diagnosis of a loved one’s life-threatening chronic illness and that person’s need for care can be experienced as traumatic life events (Lai et al. 2017), and many studies have found that prolonged grief, depression, anxiety, and post-traumatic stress are more common in caregivers than in the normal population (Aoun et al. 2020, Schulz et al. 2006, Wadhwa et al. 2013).
The mourning caregivers experience has been emphasized and hotly debated in recent years (Chiambretto et al. 2010, Lichtenthal et al. 2011). Caregivers lose their previous relationships with care recipients, who cease to be the people they used to know and become dependents who cannot meet their own needs and require care (Boss and Yeats 2014). Moreover, providing uninterrupted care can cause caregivers to forfeit social relations, restrict their autonomy, and feel a loss of control over their lives (Boss and Yeats 2014, Coelho and Barbosa 2016). Hence, as a result of these cumulative losses, caregivers of people with severe chronic illnesses may experience grief despite their relatives still being alive. The phenomenon of grief in caregivers may manifest as anticipatory grief (Large and Slinger 2015, Rando 1988), pre-death grief, or pre-loss grief (Nielsen et al. 2016, Treml et al. 2021).
Grief after a loss is normal and expected. After a loss, certain symptoms are likely to occur, but they decrease over time as people adapt to their work and social lives after the loss (Prigerson et al. 2009). Although most people go through this process as expected, some people fail to adapt to daily life even long after the loss; there is no decrease in the severity of their symptoms, and it is as if time has stopped for them. This condition is called prolonged grief disorder (Prigerson et al. 2009). Prolonged grief disorder usually results from the loss of a loved one, but it is also observed in caregivers struggling to care for people with serious illnesses (Jacobsen et al. 2010, Prigerson et al. 2009, Tomarken et al. 2008).
Ignoring caregivers’ grief symptoms may decrease their ability to provide care, as well as cause them to be unsatisfied with life, feel exhausted, and be at risk of psychiatric disorders (Chiambretto et al. 2010, Lichtenthal et al. 2011). Therefore, it is crucial to be able to measure caregivers’ grief symptoms and to provide professional help to people with high symptom severity. In the literature, we found no assessment tool that could measure the prolonged grief symptoms of relatives caring for chronic patients and could be used as an auxiliary tool to detect prolonged grief disorder cases in Turkey. To eliminate this absence, we reviewed international studies and found that the Prolonged Grief Disorder-Caregiver Form (PG-12), developed by Prigerson and Maciejewski (2008), is an internationally accepted measurement and diagnostic tool used for different samples in different countries.
The first 11 items of the PG-12 assess the severity of grief symptoms, such as longing, denial, sadness, sorrow, resentment, avoidance, and diminished sense of self. The last item examines whether these symptoms are causing impaired socio-occupational functioning. Prolonged grief disorder can be diagnosed by evaluating all items of the scale together, and the severity of anticipatory grief symptoms can be evaluated by merely using the first 11 items (Prigerson and Maciejewski 2008). It is well known that one should not make a clinical diagnosis based solely on a self-report measurement tool. Hence, the PG-12 should not be considered a standalone diagnostic measurement tool, but only an auxiliary measurement tool to support physicians’ diagnoses. A diagnosis of prolonged grief disorder made with PG-12 means that the severity of prolonged grief symptoms is higher than the threshold value and may impair the ability to function in important areas of a person’s life (Prigerson et al. 2009).
PG-12 is widely used to measure anticipatory grief symptoms and to diagnose pre-death prolonged grief disorder in many different countries. In a study conducted in Denmark, the prevalence of pre-death prolonged grief disorder (n=2865) was 15.2% in a sample of caregivers of cancer patients (Nielsen et al. 2017a). Another study conducted with caregivers of individuals treated by palliative services in Australia found that the prevalence of pre-death prolonged grief disorder (n=301) was 14.9% (Hudson et al. 2011). Similarly, the prevalence was 33% in a study of caregivers of cancer patients (n=94) in Portugal (Coelho et al. 2017), and 38.5% in a study of caregivers of vegetative patients (n=52) in Italy (Bastianelli et al. 2016). It is clear that PG-12 can be used for diagnostic purposes and to measure caregivers’ prolonged grief symptoms in various countries.
According to the World Health Organization (2018) Noncommunicable Diseases Country Profiles report, approximately 89% of deaths in Turkey in 2016 were due to chronic diseases. When the Turkish Statistical Institute (2020) examined the cause-of-death statistics, it found quite similar results. Cancer, circulatory system diseases, nervous system diseases, respiratory system diseases, and metabolic diseases affect hundreds of thousands of people, meaning that the high prevalence of chronic diseases leads to a large number of people assuming the role of caregiver. Caregivers’ grief and impaired psychological well-being can have a significant negative impact on their socio-occupational functioning (Cooper et al. 2007, Goldberg and Rickler 2011, Lim and Zebrack 2004). Therefore, the grief process of hundreds of thousands, or maybe millions, of caregivers has become a serious public mental health concern. Although using PG-12 as a measurement tool in Turkey would not, in itself, provide a holistic solution for caregivers’ grief, it may be an important tool for supporting projects, research, and psychosocial interventions. Therefore, in this study, we aimed to investigate the psychometric properties of PG-12 for a sample of Turkish participants. We also aimed to investigate the prevalence of pre-death prolonged grief disorder among caregivers in Turkey.
METHOD
Participants
Within the scope of the research, we reached out to 120 adults aged between 18–65 who cared for adults with chronic diseases and who were relatives of the people they cared for. Participants were reached by convenience sampling method. Children, even if not ill, are naturally in a care-receiving position, and parents are naturally expected to care for their children. Therefore, it is thought that there may be great differences in psychological burdens of caring for an adult or a child (Raina et al. 2004). For this reason, it was thought that the people who care for an ill child could be the sample of a different study and we excluded people cared for patients under the age of 18 from this study. In addition, Prigerson and Maciejewski (2008) used a sample of adult caregivers in their original study, which developed the PG-12 instrument we adapted in the current study. Information about the participants is presented in Table 1.
Table 1.
Sociodemographic Characteristics of Caregivers and Patients and Information Regarding Diagnosis and Caregiving Process
| Variables | f | % | M | SD | Range |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 85 | 70.8 | |||
| Male | 34 | 28.3 | |||
|
| |||||
| Age | 42.48 | 12.08 | 46.00 | ||
|
| |||||
| Education | |||||
| Primary | 13 | 10.8 | |||
| Middle | 7 | 5.8 | |||
| High School | 37 | 30.8 | |||
| Collage | 49 | 40.8 | |||
| Master’s Degree | 11 | 9.2 | |||
| Doctoral Degree | 3 | 2.5 | |||
|
| |||||
| Marital status | |||||
| Single | 30 | 25 | |||
| Married | 79 | 65.8 | |||
| Divorced | 5 | 4.2 | |||
| Widow | 6 | 5 | |||
|
| |||||
| Economic status | |||||
| Low | 31 | 25.8 | |||
| Middle | 83 | 69.2 | |||
| High | 6 | 5 | |||
|
| |||||
| Employment status | |||||
| Employed | 45 | 37.5 | |||
| Unemployed | 75 | 62.5 | |||
|
| |||||
| Relationship to patient | |||||
| Sibling | 4 | 3.3 | |||
| Spouse | 37 | 30.8 | |||
| Daughter/Son | 67 | 55.8 | |||
| Partner | 1 | 0.8 | |||
| Daughter-in-law/Son-in-law | 6 | 5 | |||
| Grandchild | 5 | 4.2 | |||
|
| |||||
| Patient’s age | 63.13 | 14.7 | 73 | ||
|
| |||||
| Diagnosis | |||||
| Amyotrophic Lateral Sclerosis | 52 | 43.3 | |||
| Cancer | 25 | 20.8 | |||
| Alzheimer’s Disease/Dementia | 12 | 10 | |||
| Cardiovascular diseases | 6 | 5 | |||
| Parkinson’s Disease | 5 | 4.2 | |||
| Respiratory Diseases | 3 | 2.5 | |||
| Kidney Failure | 2 | 1.7 | |||
| Other | 15 | 12.5 | |||
|
| |||||
| Duration of diagnosis (month) | 62.19 | 73.44 | 381.5 | ||
|
| |||||
| Duration of caregiving (month) | 52.29 | 66.75 | 479.5 | ||
|
| |||||
| Weekly caregiving duration (hour) | 72.83 | 62.81 | 167.0 | ||
Instruments
Within the scope of this study, we administered the Sociodemographic Information and Caregiver Form, Prolonged Grief Disorder Scale-Caregiver Form, Zarit Caregiver Burden Scale, Beck Depression Inventory and Life Satisfaction Scale to the participants.
Sociodemographic Information and Caregiver Form: It is an information form prepared by the researchers in which the participant is asked about themselves, the person they care for, and other demographic characteristics in Table 1.
Prolonged Grief Disorder Scale-Caregiver Form (PG-12): PG-12, developed by Prigerson and Maciejewski (2008), evaluates the symptoms of pre-death prolonged grief disorder in caregivers, including separation anxiety, emotions, cognitions, and behaviors. The first 11 items of the 12-item instrument are measured using a five-point Likert-type response scale. The first four items are rated as follows: 1=“Not at all,” 2=“At least once,” 3=“At least once a week,” 4=“At least once a day,” and 5=“Several times a day.” The next 7 items are rated as follows: “1=“Not at all,” 2=“Slightly,” 3=“Somewhat,” 4=“Quite a bit,” and 5=“Overwhelmingly.” The twelfth item of the scale concerns impaired functioning and is answered with “Yes/No”. The total score for the scale is determined by the first 11 items and varies between 11 and 55. An increase in score means an increase in the severity of grief symptoms. The twelfth item evaluates impaired functioning and is required for diagnosis. Although the first 11 items can be used to measure the severity of grief symptoms, the instrument can also be used as an auxiliary tool for diagnosing prolonged grief disorder by including item 12. A diagnosis of pre-death prolonged grief disorder is made if the following criteria are met:
Event Criterion: The person to whom it is applied must be caring for a relative with a serious illness.
Separation Anxiety: The person must experience at least one of the symptoms listed in PG-12 items 1 and 2 (1=longing and yearning, 2=emotional pain, intense sadness, or sorrow) at least once a day.
Cognitive, Emotional, and Behavioral Symptoms: The person must have answered at least five of items 3–11 (3=avoidance, 4=feeling stunned, shocked, or dazed, 5=diminished sense of self, 6=trouble accepting the illness, 7=difficulty in trusting others, 8=feeling bitter, 9=difficulty in moving on, 10=numbness, 11=feeling that life is unfulfilling, empty, or meaningless) with “at least once a day,” “several times a day,” ‘‘quite a bit,’’ or ‘‘overwhelmingly.”
Impairment Criterion: The person must have a significant impairment in social, occupational, or other important areas of life (for example, household responsibilities). In other words, if impairment exists, item 12 will be answered with “Yes.”
In the original study, the internal consistency coefficient for PG-12 was found to be 0.78 (Prigerson and Maciejewski 2008). In the present study, the Cronbach’s alpha value was found to be 0.85.
Zarit Caregiver Burden Scale (ZCBS): This is a five-point Likert-type measurement tool developed by Zarit et al. (1980), consisting of 19 items and is used to measure subjective caregiver burden. The score that can be obtained from the scale is 19–95. An increase in score means an increase in caregivers’ subjective burden. The Cronbach’s alpha coefficient of the original scale was found between 0.87 and 0.94, and the test–retest reliability was 0.71. It was adapted into Turkish by Özlü et al. (2009). The Cronbach’s alpha coefficient of the Turkish version of the scale was 0.83. In this study, the Cronbach’s alpha value of the scale was determined as 0.92.
Beck Depression Inventory (BDI): The BDI, developed by Beck et al. (1961), is a measurement tool that consists of 21 Likert-type items, scored 0–3, which evaluates the cognitive, emotional, and behavioral symptoms of depression. Hisli (1989) adapted the scale for use in Turkey, and in the current study, the Cronbach’s alpha value of the scale was found to be 0.91.
Satisfaction With Life Scale (SWLS): This is a five-point Likert-type measurement tool developed by Diener et al. (1985), consisting of five items that determine individuals’ life satisfaction levels. An increase in the scores obtained from the scale indicates an increase in life satisfaction. The test–retest correlation coefficient of the original scale was 0.82, and the Cronbach’s alpha coefficient was 0.87. The adaptation of the scale for use in Turkey was carried out by Köker (1991), and the test–retest reliability coefficient for the scale was 0.85. In a second adaptation study conducted by Dağlı and Baysal (2016), the Cronbach’s alpha coefficient of the scale was calculated as 0.88. In the current study, the Cronbach’s alpha value of the scale was found to be 0.83.
Procedure
First, a psychologist who had a good level of proficiency in English and Turkish translated the PG-12 instrument into Turkish after obtaining the necessary written permissions for the adaptation study from the PG-12 developers. The Turkish version was translated back to English by three experts (two clinical psychologists and one psychologist) who were fluent in both languages, and the Turkish version was finalized by comparing the translation with the original scale.
Ethical permission to conduct the research (approval date, 27.10.2020; document no., E-12908312-300-00001306011) was obtained from the Hacettepe University Ethical Board. The data collection process took approximately three months, from December 2020 to February 2021. We conducted the study online using Google Forms software. We reached out to participants in various regions of Turkey through welfare associations, support groups for patients’ relatives, and social media. After obtaining written and verbal consent from the administrators of the associations and support groups, we shared the invitation to participate in the research which included the purpose of study and the criteria for being a participant in the communication groups. First, we distributed an informed consent form to the participants, which included the conditions for voluntary participation in the study, the purpose of the study, confidentiality and other similar issues. In the online data collection process, we determined the time it took the participants to complete the questionnaires and whether they had completed the scales multiple times from their computers. We identified no situations that could threaten the study.
Statistical Analysis
We conducted the analyses using IBM® Statistical Package for the Social Sciences® (SPSS) version 24 AMOS 21 program. We examined all items for all the measurement tools to identify missing values, and the missing value rate did not exceed 1% for any item. We then analyzed outliers by calculating the z-values for the total scores of the scales. The z-values for the total scores of all scales were between -3.2 and +3.2. No participant was excluded from the data as an outlier. We examined normality and multivariate normality assumptions in order for confirmatory factor analysis (CFA) to produce robust results. For the analysis carried out using the AMOS program, the critical values for kurtosis and skewness were between -3 and +3, and the multivariate kurtosis value was less than 10. These values showed that the data were appropriate for the analysis.
We conducted CFA to test the construct validity of the PG-12 for the Turkish sample. CFA evaluates Chi-Squared and degrees of freedom ratio Chi-Squared divided by degrees of freedom value (X2/df<3), Comparative Fit Index (CFI>0.90), Goodness of Fit Index (GFI 0>0.90), Adjusted Goodness of Fit Index (AGFI>0.90) and Root Mean Square Residual (RMSA<0.08) criteria (Byrne 2016, Hu and Bentler 1998). To examine convergent and divergent validity, we evaluated the relationships between the PG-12 and ZCBS, BDI, and SWLS instruments using Pearson’s correlation analysis. We used the between-group separation method to evaluate criterion validity, and we conducted t-tests for independent samples to examine the differentiation of the PG-12 total scale score between the groups with low and high BDI and ZCBS scores. We examined the internal consistency coefficient and item-total score correlations to evaluate the reliability of PG-12.
RESULTS
Confirmatory Factor Analysis
To test whether the single-factor measurement model in the original PG-12 form was valid for the Turkish version, we examined the single-factor model using the maximum likelihood method. In the analyses we carried out, the fit indices were X2/df=1.60, p=0.008, CFI=0.95, IFI=0.95, GFI=0.91, AGFI=0.85, and RMSEA=0.07. When we reviewed these indices, we found that the X2/df, CFI, and IFI values for the collected data perfectly overlapped with the theoretical model (Byrne 2016, Hu and Bentler 1998). The RMSEA and AGFI values indicated an acceptable level of conformity (Byrne 2016, Hu and Bentler 1998). When we evaluated all of these indices together, the data collected using PG-12 were compatible with the single-factor 11-item model; that is, the factor structure was confirmed. In addition to the model fit indices, we examined whether the standardized regression coefficients for all 11 Likert-type items in PG-12 were significant. We observed that all items, except for the third item, had factor loadings above 0.40, and all of these loadings were statistically significant (p<0.001). As shown in Figure 1, the standardized regression coefficient for the third item was 0.29, but this value was not statistically significant at the 0.001 level (p=0.02).
Figure 1.
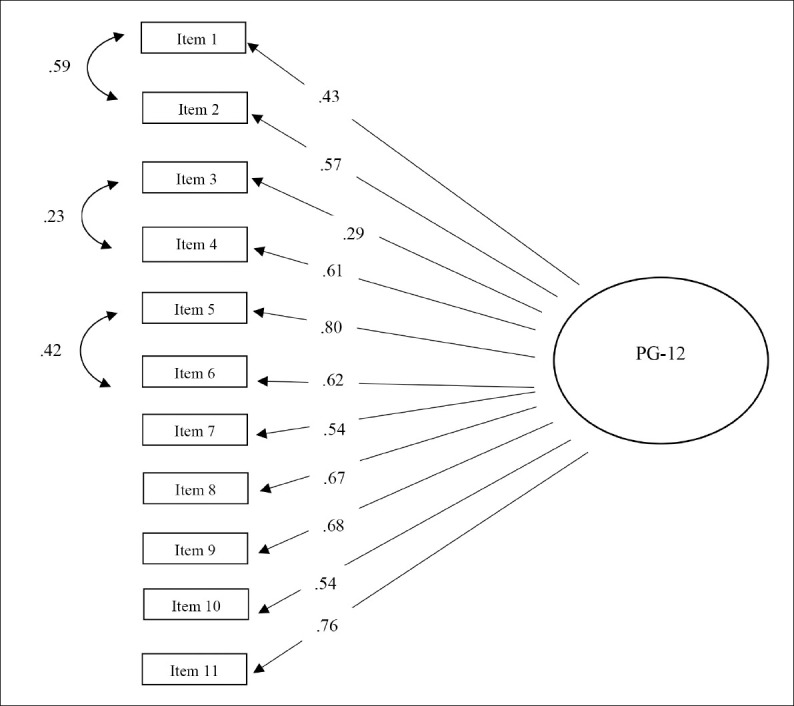
Results of the CFA of the PG-12 Turkish Version
CFA: Confirmatory Factor Analysis, PG-12: Prolonged Grief Disorder Scale-Caregiver Form
Convergent and Divergent Validity
To evaluate the convergent and divergent validity of the PG-12 instrument, we examined the Pearson’s correlation coefficients between PG-12, ZCBS, BDI, and SWLS and found that the coefficients for the relationships between PG-12 and the other scales were statistically significant. The positive correlations of PG-12 with BDI and ZCBS and the negative correlation of PG-12 with SWLS supported convergent and discriminant validity, according to the literature (Holley and Mast 2009, Hudson et al. 2011, Nielsen et al. 2017b, Chan et al. 2017). Table 2 presents Pearson’s correlation coefficients for these variables.
Table 2.
Pearson Correlation Coefficients Between PG-12 and BDI, ZCBS, and SWLS
| 1 | 2 | 3 | 4 | ||
|---|---|---|---|---|---|
| 1.PG-12 | 1 | 0.60** | 0.36** | -0.41** | |
| 2.BDI | 1 | 0.31** | -0.51** | ||
| 3.ZCBS | 1 | -0.19* | |||
| 4.SWLS | 1 | ||||
| *p<0.05 **p<0.01 | |||||
PG-12: Prolonged Grief Disorder Scale-Caregiver Form, BDI: Beck Depression Inventory, ZCBS: Zarit Caregiver Burden Scale, SWLS: Satisfaction with Life Scale.
Criterion Validity
To test the criterion validity of the PG-12 instrument, we used the intergroup differentiation method. For this purpose, we ranked all participants according to their largest to smallest BDI total scores. The participants fell into two separate groups with the highest 25% and the lowest 25% depression scores, and these groups’ scores were compared with each other in terms of PG-12 scores. The same procedure was repeated for the ZCBS scores. T-test findings showed that the participants in the highest 25% quantile of depression scores had statistically significantly higher scores on PG-12 than the group in the lowest quantile. Similarly, participants in the highest 25% quantile in terms of ZCBS scores obtained significantly higher PG-12 scores than those in the lowest 25% quantile. Table 3 presents the t-test findings.
Table 3.
Comparison of Groups with Low and High Caregiver Burden and Depression in terms of PG-12 Scores
| N | M | SD | t | df | p | |
|---|---|---|---|---|---|---|
| Group with Low Depression Score | 30 | 31.83 | 7.25 | -6.92 | 58 | 0.000 |
| Group with High Depression Score | 30 | 45.60 | 8.14 | |||
| Group with Low Caregiver Burden Scores | 30 | 35.03 | 10.27 | -3.13 | 51.14 | 0.003 |
| Group with High Caregiver Burden Scores | 30 | 42.13 | 6.99 |
PG-12: Prolonged Grief Disorder Scale-Caregiver Form,
Reliability
We calculated the Cronbach’s alpha value as an indicator of the internal consistency coefficient to determine the reliability level of PG-12, and this value was α=0.85. George and Mallery (2010) stated that Cronbach’s alpha values above 0.80 indicate a high level of internal consistency. In addition to the internal consistency coefficient, we examined the item-total score correlations of PG-12, and the correlation values ranged between 0.44 and 0.74. Since the item-total test correlation coefficients for all items in PG-12 were over 0.40 and statistically significant (p<0.01), PG-12 is clearly a highly distinctive and reliable measurement tool (Büyüköztürk 2015).
Prevalence of Prolonged Grief Disorder in Caregivers
We investigated the prevalence of prolonged grief disorder in a sample of 120 caregivers who were caring for their relatives with chronic illnesses, considering criteria A, B, C, and D in the PG-12 instructions (see the Methods section). It was evident that 31.66% of the caregivers met the diagnostic criteria for pre-death prolonged grief disorder. The mean age of the participants who met these diagnostic criteria was 41.82 years (SD=12.24), and the mean age of the relatives they cared for was 64.47 years (SD=15.29). Of the participants who met the diagnostic criteria, 68.4% were children of people with chronic diseases. Also, 78.9% of the diagnosed participants were women, 60.5% had a college or postgraduate education, 57.9% were unemployed, and almost all (97.4%) were of low to middle socioeconomic status. The diagnosed participants reported that they spent an average of 82 hours (SD=65.02) per week caring for their relatives, and 50% of the diagnosed participants cared for bedridden relatives.
DISCUSSION
In this study, the Prolonged Grief Disorder Scale-Caregiver Form was adapted for use in Turkey. The analyses showed that the validity and reliability values were close to those for the original form and were statistically significant. The CFA results supported the single-factor model according to the original scale and adaptation studies conducted in various cultures (Chiambretto et al. 2008, Coelho et al. 2017, Prigerson and Maciejewski 2008). The correlation values for convergent and discriminant validity and the t-test results for criterion validity supported construct validity, and the Cronbach’s alpha value was a good indicator of the reliability of the scale for the Turkish sample.
When we examined the standardized regression coefficients using CFA to determine whether they were significant, the factor loadings were above 0.40 for all items except the third item, for which the standardized regression coefficient was.29 (p=0.02). In this case, we evaluated two possibilities. One possibility was that item 3, asking about avoidance, was not understood by the participants, either because they understood something other than what was meant by the avoidance item or did not understand the psychology-related terminology. Another possibility was that because the participants were caregivers who constantly shared the same environments as the people they cared for, avoidance was not an option. In other words, the necessity of constantly being in the same environments as the care recipients and inevitably confronting the reality of the situation may have made it difficult for caregivers to avoid reminders of their relatives’ illnesses. Based on the findings in the CFA that the third item did not work as well as the other items, we had to make a decision about whether to remove this item from the scale. Since the PG-12 instrument has frequently been used in studies published in prominent journals by outstanding researchers in many countries, and it has also been used in cross-cultural comparison studies, we decided to retain the original form and keep the third item in the scale. Another reason for keeping the third item in the scale was that the fit indices were extremely high, and the 11-item version of the scale was compatible with the data.
When we examined the prevalence of prolonged grief disorder in the sample, we found that approximately 32% of caregivers met the diagnostic criteria for prolonged grief disorder. In previous studies that examined the anticipatory grief symptoms of caregivers using PG-12, the prevalence of prolonged grief was 15.2% in Nielsen et al.’s (2017a) study of caregivers of cancer patients (n=2865), 14.9% in Hudson et al.’s (2011) study of caregivers of relatives treated by palliative services (n=301), 33% in Coelho et al.’s (2017) sample of caregivers of cancer patients (n=94), and 38.5% in Bastianelli et al.’s (2016) study of caregivers of patients in a vegetative state (n=52). Although the prevalence of prolonged grief disorder in Italy, Portugal, and Turkey, which are Mediterranean countries, is similar, cultural differences in family ties may explain the lower prevalence of prolonged grief in studies conducted in Australia and Denmark which is Northern European countries. While family ties are less important and more individualistic cultures are predominant in Northern Europe, close family ties are the norm in the Mediterranean region, and the family is prioritized over the individual (Reher 1998). Hence, caregivers in Mediterranean countries may experience more severe effects from relational losses associated with their relatives’ illnesses. Also, they may experience a higher pressure to assume the role of caregiver due to cultural codes, however reluctantly (Mahoney et al. 2005). Identity of caregivers also vary depending on the cultures in which studies are conducted. While 64% of caregivers in Nielsen et al.’s (2017a) study were the spouses of patients, 60% of caregivers in Coelho et al.’s (2017) study were the patients’ children. In the present study, although the caregivers were mostly patients’ children (55.8%), spouses took second place (30.8%). Although a limited number of studies have revealed that caregivers of spouses experience more anticipatory grief than caregivers of parents, the loss of competence of a parent for a caregiver, even if he/she has reached adulthood, and the consequent change in roles may affect the severity of the grieving experience (Ar 2017, Hudson et al. 2011, Nanni et al. 2014).
The caregivers providing care for their relatives with chronic diseases experience an extended period of grief due to the loss of social relations, restriction of their autonomy, loss of control over their lives, suppression of their own emotional and physical needs, and interruption of their future plans as well as their relatives’ struggles with diseases, declining health status of the relatives they care for, the loss of relationships with those relatives, and their relatives’ impending deaths (Boss and Yeats 2014, Coelho and Barbosa 2016). The fact that 31.66% of the participants met the diagnostic criteria for prolonged grief disorder revealed that these individuals experienced severe grief symptoms in terms of emotions, cognitions, behaviors, and separation anxiety in the face of loss, which impaired their functioning in important areas of their lives. Although most patients’ caregivers experience similar losses, a minority of caregivers have symptoms that meet the criteria for prolonged grief. Also, individual differences between caregivers may play a role in their different experiences of prolonged grief disorder. In this study, consistent with the literature, the participants who met the diagnostic criteria for prolonged grief disorder had low income levels and dedicated most of their time (an average of 82 hours per week) to providing care as primary caregivers. Anticipatory grief is likely to occur in people with high relational dependency tendencies, low education levels, low income levels, people who are neurotic, have trouble with intimacy, who have an inability to make sense of loss, and less attachment to spiritual values (Burke et al. 2015, Tomarken et al. 2008). However, assuming the role of primary caregiver and living with the patient are also risk factors (Areia et al. 2019, Hudson et al. 2011). In particular, low levels of social support for caregivers and the grieving process increase the likelihood of anticipatory grief (Burke et al. 2015).
Limitations of the Study
The main limitation of this research was that the measurements were based on self-reports. Self-reports can lead to the possibility of participants not being able to evaluate themselves objectively and/or giving answers they believe to be acceptable to society, potentially biasing the results. Another limitation of the study was the lack of a representative sample. Besides the inclusion in the sample only of individuals who cared for their adult relatives, the participants had particularly high levels of education. These factors could limit the generalizability of the findings. Also, reaching the participants through support groups for patients’ relatives suggests that the sample received social support and therefore did not reflect the experiences of the wider population. Another limitation of the study is that it was cross-sectional. Also, the high ratio of women to men in the sample was compatible with the literature, which may have biased the research findings, since we do not yet know whether there are gender-related differences in the grieving process (Gopalan and Brannon 2006).
Implications for Clinical Practice
Bringing PG-12 into the national literature as a valid and reliable measurement tool for Turkey is of critical importance. The PG-12 instrument, which is internationally recognized and accepted, has been used in many studies of caregivers’ anticipatory grief (Breen et al. 2020, Coelho et al. 2017, Hudson et al. 2011, Lai et al. 2017, Nielsen et al. 2016, Nielsen et al. 2017a, Nielsen et al. 2019, Thomas et al. 2014). Besides being a short and easily applicable measurement tool, the fact that it can be used to both evaluate the severity of anticipatory grief and diagnose pre-death prolonged grief disorder makes PG-12 convenient for clinicians in Turkey. Also, the fact that it is valid and reliable for any serious illness of a loved one expands its applicability compared to similar measurement tools that evaluate anticipatory grief in caregivers. Also, we believe that this scale will help shape psychological support services for caregivers according to their specific needs. Considering the caregiver population in Turkey and the prevalence of bereavement in this population, the necessity and benefits of this measurement tool are obvious.
In summary, the PG-12 is suitable for evaluating the grief symptoms of caregivers in Turkey in terms of its psychometric properties, and we foresee that it will be useful in both research and clinical practice.
Acknowledgement:
This article is a part of the master’s thesis of the first author Gizem Önal, conducted under the supervision of the last author Assoc. Prof. Zeynep Tüzün Gün.
REFERENCES
- 1.Aoun SM, Kissane DW, Cafarella PA, et al. Grief, depression, and anxiety in bereaved caregivers of people with motor neurone disease:a population-based national study. Amyotroph Lateral Scler Frontotemporal Degener. (2020);21:593–605. doi: 10.1080/21678421.2020.1790610. [DOI] [PubMed] [Google Scholar]
- 2.Ar Y. Predictors of depression, anxiety, grief and growth among turkish offspring as caregivers of parents with alzheimer's disease:a multi-method study. Unpublished doctoral thesis, Middle East Technical University Institute of Social Sciences, Ankara, Turkey. (2017) [Google Scholar]
- 3.Areia NP, Fonseca G, Major S, et al. Psychological morbidity in family caregivers of people living with terminal cancer:prevalence and predictors. Palliat Support Care. (2019);17:286–93. doi: 10.1017/S1478951518000044. [DOI] [PubMed] [Google Scholar]
- 4.Bastianelli A, Gius E, Cipolletta S. Changes over time in the quality of life, prolonged grief and family strain of family caregivers of patients in vegetative state:A pilot study. J Health Psychol. (2016);21:844–52. doi: 10.1177/1359105314539533. [DOI] [PubMed] [Google Scholar]
- 5.Beck AT, Ward C, Mendelson M, et al. Beck depression inventory (BDI) Arch Gen Psychiatry. (1961);4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 6.Boss P, Yeats JR. Ambiguous loss:A complicated type of grief when loved ones disappear. Bereavement Care. (2014);33:63–9. [Google Scholar]
- 7.Breen LJ, Aoun SM, O'Connor M, et al. Effect of caregiving at end of life on grief, quality of life and general health:a prospective, longitudinal, comparative study. Palliat Med. (2020);34:145–54. doi: 10.1177/0269216319880766. [DOI] [PubMed] [Google Scholar]
- 8.Burke LA, Clark KA, Ali KS, et al. Risk factors for anticipatory grief in family members of terminally ill veterans receiving palliative care services. J Soc Work End Life Palliat Care. (2015);11:244–66. doi: 10.1080/15524256.2015.1110071. [DOI] [PubMed] [Google Scholar]
- 9.Büyüköztürk Ş. Sosyal bilimler için veri analizi el kitabı. (21st Edition) Ankara: Pegem; (2015). pp. 182–94. [Google Scholar]
- 10.Byrne BM. Structural equation modelling with AMOS:Basic concepts, applications, and programming. (3rd Edition.) New York: Routledge; (2016). pp. 53–95. [Google Scholar]
- 11.Chan WCH, Wong B, Kwok T, et al. Assessing grief of family caregivers of people with dementia:validation of the Chinese version of the Marwit–Meuser caregiver grief inventory. Health Soc Work. (2017);42:151–8. doi: 10.1093/hsw/hlx022. [DOI] [PubMed] [Google Scholar]
- 12.Chiambretto P, Moroni L, Guarnerio C, et al. Italian validation of the prolonged grief disorder questionnaire (PG-12) G Ital Med Lav Ergon. (2008);30:105–10. [PubMed] [Google Scholar]
- 13.Chiambretto P, Moroni L, Guarnerio C, et al. Prolonged grief and depression in caregivers of patients in vegetative state. Brain Inj. (2010);24:581–8. doi: 10.3109/02699051003610490. [DOI] [PubMed] [Google Scholar]
- 14.Coelho A, Barbosa A. Family Anticipatory Grief:An Integrative Literature Review. Am J Hosp Palliat Care. (2016);34:774–85. doi: 10.1177/1049909116647960. [DOI] [PubMed] [Google Scholar]
- 15.Coelho A, Silva C, Barbosa A. Portuguese validation of the Prolonged Grief Disorder Questionnaire–Predeath (PG–12):psychometric properties and correlates. Palliat Support Care. (2017);15:544–53. doi: 10.1017/S1478951516001000. [DOI] [PubMed] [Google Scholar]
- 16.Cooper C, Balamurali TBS, Livingston G. A systematic review of the prevalence and covariates of anxiety in caregivers of people with dementia. Int Psychogeriatr. (2007);19:175–95. doi: 10.1017/S1041610206004297. [DOI] [PubMed] [Google Scholar]
- 17.Dağlı A, Baysal N. Adaptation Of The Satisfaction With Life Scale Into Turkish:The Study Of Validity And Reliability. Electronic Journal of Social Sciences. (2016);15:1250–62. [Google Scholar]
- 18.Diener ED, Emmons RA, Larsen RJ, et al. The satisfaction with life scale. J Pers Assess. (1985);49:71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 19.George D, Mallery P. A simple study guide and reference. (10th Edition) GEN, Boston, MA: Pearson Education, Inc; (2010). SPSS for Windows step by step; pp. 235–46. [Google Scholar]
- 20.Goldberg A, Rickler KS. The role of family caregivers for people with chronic illness. Med Health R I. (2011);94:41–2. [PubMed] [Google Scholar]
- 21.Gopalan N, Brannon LA. Increasing family members'appreciation of family caregiving stress. J Psychol. (2006);140:85–94. doi: 10.3200/JRLP.140.2.85-94. [DOI] [PubMed] [Google Scholar]
- 22.Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji dergisi. (1989);7:3–13. [Google Scholar]
- 23.Holley CK, Mast BT. The impact of anticipatory grief on caregiver burden in dementia caregivers. Gerontologist. (2009);49:388–96. doi: 10.1093/geront/gnp061. [DOI] [PubMed] [Google Scholar]
- 24.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis:Conventional criteria versus new alternatives. Structural Equation Modeling:A Multidisciplinary Journal. (1998);6:1–55. [Google Scholar]
- 25.Hudson PL, Thomas K, Trauer T, et al. Psychological and social profile of family caregivers on commencement of palliative care. J Pain Symptom Manage. (2011);41:522–34. doi: 10.1016/j.jpainsymman.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Jacobsen JC, Zhang B, Block SD, et al. Distinguishing symptoms of grief and depression in a cohort of advanced cancer patients. Death Stud. (2010);34:257–73. doi: 10.1080/07481180903559303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Köker S. Normal ve sorunlu ergenlerin yaşam doyumu düzeyinin karşılaştırılması. Unpublished Master's Thesis, Ankara University Institute of Social Sciences, Ankara. (1991) [Google Scholar]
- 28.Lai C, Luciani M, Galli F, et al. Persistent complex bereavement disorder in caregivers of terminally ill patients undergoing supportive-expressive treatment:a pilot study. J Ment Health. (2017);26:111–8. doi: 10.3109/09638237.2016.1167855. [DOI] [PubMed] [Google Scholar]
- 29.Large S, Slinger R. Grief in caregivers of persons with Alzheimer's disease and related dementia:A qualitative synthesis. Dementia. (2015);14:164–83. doi: 10.1177/1471301213494511. [DOI] [PubMed] [Google Scholar]
- 30.Lichtenthal WG, Nilsson M, Kissane DW, et al. Underutilization of mental health services among bereaved caregivers with prolonged grief disorder. Psychiatr Serv. (2011);62:1225–9. doi: 10.1176/appi.ps.62.10.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lim JW, Zebrack B. Caring for family members with chronic physical illness:a critical review of caregiver literature. Health Qual Life Outcomes. (2004);2:1–9. doi: 10.1186/1477-7525-2-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mahoney DF, Cloutterbuck J, Neary S, et al. African American, Chinese, and Latino family caregivers'impressions of the onset and diagnosis of dementia:cross-cultural similarities and differences. Gerontologist. (2005);45:783–92. doi: 10.1093/geront/45.6.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nanni MG, Biancosino B, Grassi L. Pre-loss symptoms related to risk of complicated grief in caregivers of terminally ill cancer patients. J Affect Disord. (2014);160:87–91. doi: 10.1016/j.jad.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 34.Nielsen MK, Neergaard MA, Jensen AB, et al. Do we need to change our understanding of anticipatory grief in caregivers?A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin Psychol Rev. (2016);44:75–93. doi: 10.1016/j.cpr.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Nielsen MK, Neergaard MA, Jensen AB, et al. Preloss grief in family caregivers during end?of?life cancer care:A nationwide population?based cohort study. Psychooncology. (2017);26:2048–56. doi: 10.1002/pon.4416. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen MK, Neergaard MA, Jensen AB, et al. Predictors of complicated grief and depression in bereaved caregivers:a nationwide prospective cohort study. J Pain Symptom Manage. (2017);53:540–50. doi: 10.1016/j.jpainsymman.2016.09.013. [DOI] [PubMed] [Google Scholar]
- 37.Nielsen MK, Carlsen AH, Neergaard MA, et al. Looking beyond the mean in grief trajectories:A prospective, population-based cohort study. Soc Sci Med. (2019);232:460–9. doi: 10.1016/j.socscimed.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 38.Özlü A, Yıldız M, Aker T. A Reliability and Validity Study on the Zarit Caregiver Burden Scale. Noro Psikiyatr Ars. (2009);46:38–42. [Google Scholar]
- 39.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder:Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS medicine. (2009);6:1000–121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prigerson HG, Maciejewski PK. Prolonged Grief Disorder Inventory (PG-12) Unpublished Measurement Tool. (2008) [Google Scholar]
- 41.Raina P, O'Donnell M, Schwellnus H, et al. Caregiving process and caregiver burden:conceptual models to guide research and practice. BMC pediatrics. (2004);4:1. doi: 10.1186/1471-2431-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rando TA. Anticipatory grief:The term is a misnomer but the phenomenon exists. J Palliat Care. (1988);4:70–3. [PubMed] [Google Scholar]
- 43.Reher D. Family Ties in Western Europe:Persistent Contrasts. Population and Development Review. (1998);24:203. [Google Scholar]
- 44.Schulz R, Boerner K, Shear K, et al. Predictors of complicated grief among dementia caregivers:a prospective study of bereavement. Am J Geriatr Psychiatry. (2006);14:650–8. doi: 10.1097/01.JGP.0000203178.44894.db. [DOI] [PubMed] [Google Scholar]
- 45.Thomas K, Hudson P, Trauer T, et al. Risk factors for developing prolonged grief during bereavement in family carers of cancer patients in palliative care:a longitudinal study. J Pain Symptom Manage. (2014);47:531–41. doi: 10.1016/j.jpainsymman.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 46.Tomarken A, Holland J, Schachter S, et al. Factors of complicated grief pre?death in caregivers of cancer patients. Psychooncology. (2008);17:105–11. doi: 10.1002/pon.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Treml J, Schmidt V, Nagl M, et al. Pre-loss grief and preparedness for death among caregivers of terminally ill cancer patients:A systematic review. Soc Sci Med. (2021);284:114240. doi: 10.1016/j.socscimed.2021.114240. [DOI] [PubMed] [Google Scholar]
- 48.Turkish Statistical Institute (2020 June) Death and Cause of Death Statistics 2019 [Press release] Retrived from https://data.tuik.gov.tr/Bulten/Index?p=Olum-ve-Olum-Nedeni-Istatistikleri-2019-33710 on 1 October, 2021 .
- 49.Wadhwa D, Burman D, Swami N, et al. Quality of life and mental health in caregivers of outpatients with advanced cancer. Psychooncology. (2013);22:403–10. doi: 10.1002/pon.2104. [DOI] [PubMed] [Google Scholar]
- 50.World Health Organization. Global status report on noncommunicable diseases 2010. (2011). Retrived from http://www.who.int/nmh/publications/ncd_report2010/en/ on 3 October, 2021 .
- 51.World Health Organization. International classification of diseases for mortality and morbidity statistics (11th Revision) (2018). Retrived from https://icd.who.int/browse11/l-m/en on 1 October, 2021 .
- 52.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly:correlates of feelings of burden. Gerontologist. (1980);20:649–55. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]