Abstract
Ticks are well-known vectors for transmitting disease and cause a variety of cutaneous manifestations to their afflicted host. Tick bite alopecia serves as a lesser-known illustration of this phenomenon, as few cases are documented in the literature. Scarring and nonscarring forms of tick-induced alopecia are described, with the latter being more common. This case highlights an adult female patient who developed a localized oval zone of midparietal scalp hair loss two months after the detection and removal of several ticks on her scalp. The chronicled events, clinical findings, and histopathology results further confirm a particular pattern of manifestation for tick bite alopecia. This case illustrates the importance of recognizing and considering tick bites as a possible cause of focal hair loss, given a similar presentation and historical account.
Keywords: Tick bite, alopecia, cutaneous arthropod bite reaction
Introduction
Cutaneous reactions to arthropod bites can manifest in a variety of ways. Tick bites can cause localized alopecia, with documented cases in the English literature dating back to the 1950s.1 The reported cases since that time are limited and mostly described among pediatric patients.2 We present the case of an adult female patient who developed localized alopecia on her scalp following a tick bite.
Case Report
A 72-year-old female patient with skin phototype II presented to our outpatient dermatology clinic with a seven-month history of an isolated patch of hair loss to her midparietal scalp. The patient reported finding multiple ticks on her body after being outdoors approximately two months prior to the advent of her hair loss. Ticks were removed with forceps within one day after they were initially detected. She denied fever, headache, rash, or any systemic symptoms. She did develop a small, raised, mildly itchy bump at the site of the scalp tick removal. One day following the bite, she initiated treatment of a 10-day course of doxycycline. The patient’s past medical history was significant for rheumatoid arthritis, Type 2 diabetes mellitus, hypertension, hypercholesterolemia, and some food allergies. The patient did not develop any systemic side effects or worsening of her comorbidities after the tick bite.
Physical examination revealed an alopecic plaque, measuring 5x4.5cm of the posterior midparietal scalp (Figure 1). A 4mm punch biopsy was performed within the plaque, and a second 4mm punch biopsy was obtained at the periphery. Pathological findings showed a noticeable loss of follicles within the specimen, with a marked decrease in sebaceous glands and shift toward catagen/telogen hairs. Vertical and horizontal sections of the scalp were examined, showing an unremarkable epidermis, spongiosis of the follicular epithelium, and focal miniaturization of hairs. Dense lymphocytic infiltrate with eosinophils appeared within the dermis (Figure 2). The section of the subcutis showed complete loss of bulbs. Immunohistochemical stains depicted a mixture of CD20-postive B cells and CD3-positive T cells. Lyme and spirochete immunostains were negative.
FIGURE 1.

A 5x4.5cm oval area of hair loss to the posterior midparietal scalp depicting a centrally located plaque with overlying scale and erythematous peripheral border.
FIGURE 2.
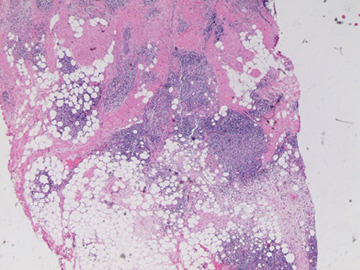
Hematoxylin and eosin (H&E) staining with 200x magnification shows dense infiltrate of lymphocytes with eosinophils, with the infiltrate forming germinal center-like aggregates.
The patient returned to the clinic one week later for suture removal, and an additional 4mm punch biopsy was performed within the area of hair loss of the right superior parietal scalp. The epidermis showed irregular acantholysis, with a small focus of epidermal disruption. The dermis depicted dense superficial and deep lymphoplasmacytic infiltrates with focal nodular aggregate (Figure 3).
FIGURE 3.
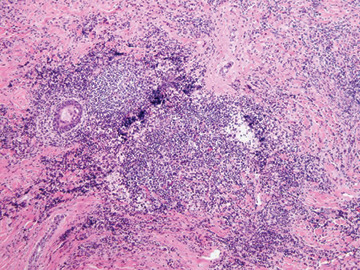
Hematoxylin and eosin (H&E) staining with 100x magnification shows dense superficial and deep lymphoplasmacytic infiltrate with eosinophils.
At the time of writing, the patient received a series of two intralesional triamcinolone injections administered six weeks apart. The triamcinolone concentration was 20mg/cc, and 3cc was dispersed into multiple sites within the area of hair loss at each visit. The patient also applied 5% topical minoxidil foam twice daily to her alopecic plaque and has experienced more than 50 percent hair regrowth to date.
Discussion and Conclusion
Ticks are well-known vectors in transmitting disease and are second only to mosquitoes in spreading infectious human disease across the world.4 Ticks can cause numerous cutaneous manifestations, including papular urticaria, diffuse dermatitis, skin hemorrhages, nodules, nodulopustules, erythema migrans-like rash, and patchy alopecia.5,6 Differentiating cutaneous processes associated with a tick bite from other arthropod or insect bites can prove challenging, as they often have similar clinical and histological features.5 Tick bite-related alopecia does, however, typically present in a particular pattern, which can help differentiate it from other probable causes of focal hair loss. A localized oval zone of alopecia, often resembling a moth-eaten appearance, with erythema and centralized scale or eschar is common, as described in our case, as well as in the published literature.2,8,9 The hair density tends to normalize at the periphery of the lesion, with a return of normalized skin pigment to that of the surrounding scalp.8
Scarring and nonscarring forms of tick-induced alopecia are documented in the literature.2 The nonscarring form is more commonly described, with hair regrowth typically occurring within the first three months of the initial bite.1,5,7 However, Lynch et al2 cited reports of alopecia that persisted for five years after the tick bite-induced localized reaction had healed. Although not fully understood, early detection and treatment might prove critical in reducing the duration of significant hair loss and optimizing the areas of alopecia for substantial hair regrowth. The cause of tick- and other known arthropod-induced alopecia is thought to be associated with the anticoagulants and immunomodulatory chemicals injected within the saliva, which in turn causes a robust inflammatory immune response from the host.2
Tick-associated nonscarring alopecia leads to transient alterations of hair growth, with an increase in catagen and telogen follicles as is similarly seen in alopecia areata.9 There is limited actual destruction of the hair follicles, thus leading to hair regrowth, as described in previous studies.1,7 The scarring form of tick bite alopecia is less frequently observed; when seen, it typically presents with a centralized eschar formation to the area of hair loss that progresses to patches of cicatricial alopecia.2
Classic histological findings of nonscarring tick bite alopecia follow the pattern seen in our case, which showed a dense lymphocytic infiltrate with increased eosinophils and an increased catagen and telogen hair count with miniaturization and partial-to-complete loss of hair follicles.9 The scarring form of tick-induced alopecia will typically present with an eosinophilic or granulomatous infiltrate, inflammation and fibrosis, and a more complete loss of hair follicles, compared to the nonscarring form.2 The recognition of the clinical and histopathological manifestation of tick bite alopecia is paramount for a timely and accurate diagnosis, and, if tick bite alopecia is deemed to be more commonly seen than is currently reported, this might lead to a more standardized and improved treatment approach. Our report describes a case of tick bite alopecia in an adult female patient that will hopefully instill a greater degree of recognition and consideration for similar presentations encountered by practitioners in the primary care and dermatology settings.
REFERENCES
- Ross MS, Friede H. Alopecia due to tick bite. Arch Dermatol. 1955;71(4):524–525. doi: 10.1001/archderm.1955.01540280100026. [DOI] [PubMed] [Google Scholar]
- Lynch MC, Milchak MA, Parnes H, Ioffreda MD. Tick bite alopecia: a report and review. Am J Dermatopathol. 2016;38(11):e150–e153. doi: 10.1097/DAD.0000000000000598. [DOI] [PubMed] [Google Scholar]
- Parola P, Raoult D. Ticks and tickborne bacterial disease in humans: an emerging infectious threat. Clin Infect Dis. 2001;32(6):897–928. doi: 10.1086/319347. [DOI] [PubMed] [Google Scholar]
- Fisher EJ, Mo J, Lucky AW. Multiple pruritic papules from lone star tick larvae bites. Arch Dermatol. 2006;142(4):491–494. doi: 10.1001/archderm.142.4.491. [DOI] [PubMed] [Google Scholar]
- Krinsky WL. Dermatoses associated with the bites of mites and ticks (Arthropoda: Acari). Int J Dermatol. 1983;22(2):75–91. doi: 10.1111/j.1365-4362.1983.tb03319.x. [DOI] [PubMed] [Google Scholar]
- Yesudian P, Thambiah AS. Persisent papules after tick-bites. Dermatologica. 1973;147(3):214–218. doi: 10.1159/000251873. [DOI] [PubMed] [Google Scholar]
- Heyl T. Tick bite alopecia. Clin Exp Dermatol. 1982;7(5):537–542. doi: 10.1111/j.1365-2230.1982.tb02472.x. [DOI] [PubMed] [Google Scholar]
- Sperling LC, Sutton E, Wilke MS. What’s eating you? Tick bite alopecia. Cutis. 2016;98(2):88–90. [PubMed] [Google Scholar]
- Castelli E, Caputo V, Morello V, Tomasino RM. Local reactions to tick bites. Am J Dermatopathol. 2008;30(3):241–248. doi: 10.1097/DAD.0b013e3181676b60. [DOI] [PubMed] [Google Scholar]


