Abstract
The risk of maternal death in the United States is higher than peer nations and is rising and varies dramatically by the race and place of residence of the woman. Critical efforts to reduce maternal mortality include patient risk stratification and system-level quality improvement efforts targeting specific aspects of clinical care. These efforts are important for addressing the causes of an individual’s risk, but research to date suggests that individual risk factors alone do not adequately explain between-group disparities in pregnancy-related death by race, ethnicity, or geography. The holistic review and multidisciplinary makeup of maternal mortality review committees make them well positioned to fill knowledge gaps about the drivers of racial and geographic inequity in maternal death. However, committees may lack the conceptual framework, contextual data, and evidence base needed to identify community-based contributing factors to death and, when appropriate, to make recommendations for future action. By incorporating a multileveled, theory-grounded framework for causes of health inequity, along with indicators of the community vital signs, the social and community context in which women live, work, and seek health care, maternal mortality review committees may identify novel underlying factors at the community level that enhance understanding of racial and geographic inequity in maternal mortality. By considering evidence-informed community and regional resources and policies for addressing these factors, novel prevention recommendations, including recommendations that extend outside the realm of the formal health care system, may emerge.
Keywords: maternal death, maternal mortality, maternal mortality review committees, quality improvement
Population patterns of maternal mortality
Each maternal death is a tragic loss for families and communities. At a population level, maternal mortality rates may reveal critical flaws and shortcomings in health systems, communities, and society at large where prevention opportunities were missed. The US pregnancy-related mortality ratio increased 140% from 7.2 deaths per 100,000 live births in 1987 to 17.3 in 2013.1
While a portion of this increase is due to enhanced record-linkage activities, the adoption of the International Classification of Diseases, 10th revision, and the introduction of checkboxes to indicate pregnancy status on death certificates,2,3 maternal mortality has increased beyond what can be explained by improved case ascertainment alone.3 The United States. has one of the highest pregnancy-related mortality ratio among high-income countries, and the United States alone experienced recent increases rather than decreases in maternal mortality.4
The burden of maternal mortality is unequally shared, with some groups faring worse and worsening faster. Compared with non-Hispanic white women in the United States, American Indian/Alaska Native women experience 150% higher relative risk of pregnancy-related death, and black women experience 233% times the risk (Figure 1). Black women not only experience the highest mortality rate, but between 2008 and 2014, their rates increased by 9.6 (from 46.7 to 56.3) deaths per 100,000 live births compared with an increase of 4.4 (from 15.9 to 20.3) per 100,000 for white women.5
FIGURE 1. US Pregnancy-related mortality ratios, United States, by race and Hispanic ethnicity, 2006–2013.
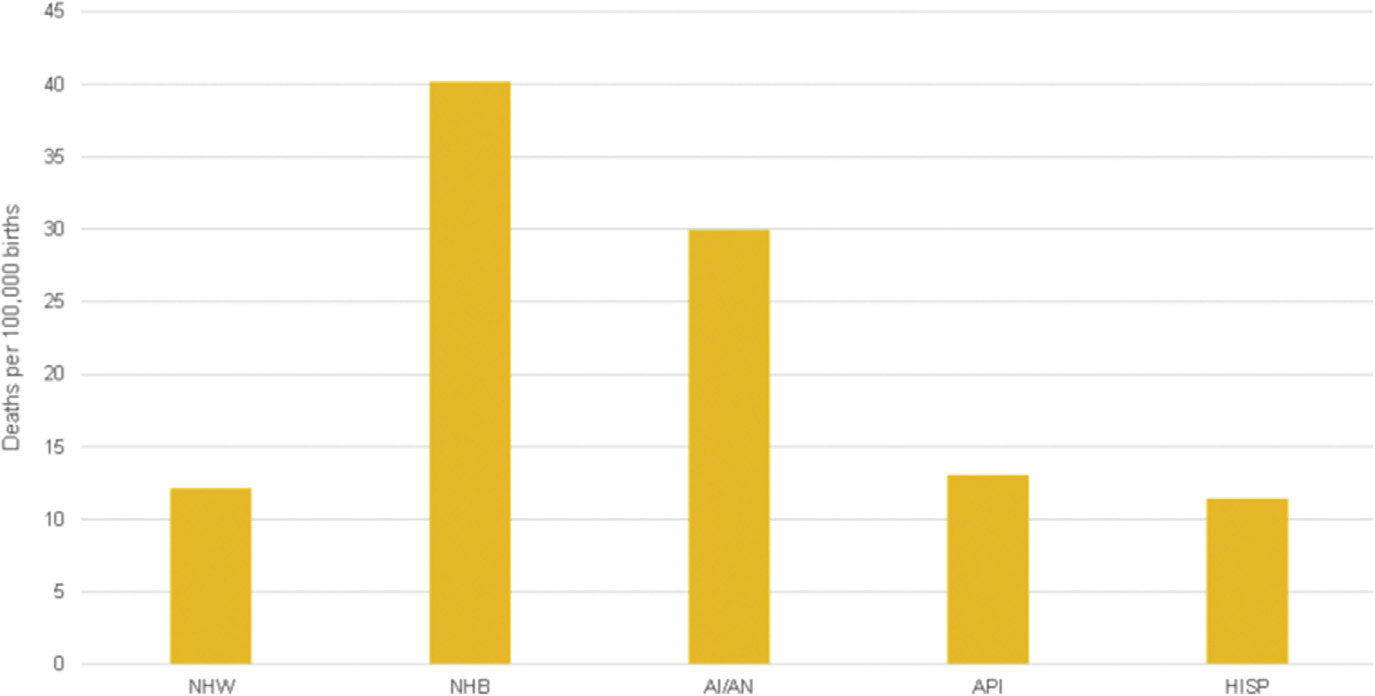
Pregnancy-related mortality ratios, United States, by race and Hispanic ethnicity, 2006–2013 Reproduced from Pregnancy Mortality Surveillance System, Centers for Disease Control and Prevention.
NHW, non-Hispanic white; NHB, non-Hispanic black; AI/AN, American Indian/Alaska Native; API, Asian/Pacific Islander.
Kramer. Health equity framework for maternal mortality. Am J Obstet Gynecol 2019.
There is also substantial geographic variation in maternal mortality (Figure 2), with an approximately 3-fold differences between the highest- and lowest-rate states. Geographic disparities in perinatal and maternal health outcomes between states, counties, and neighborhoods, independent of the geography of racial composition, highlight the importance of place as a contextual determinant of women’s health.6–8
FIGURE 2. Interstate variation in pregnancy-related mortality ratio, 2006–2013.
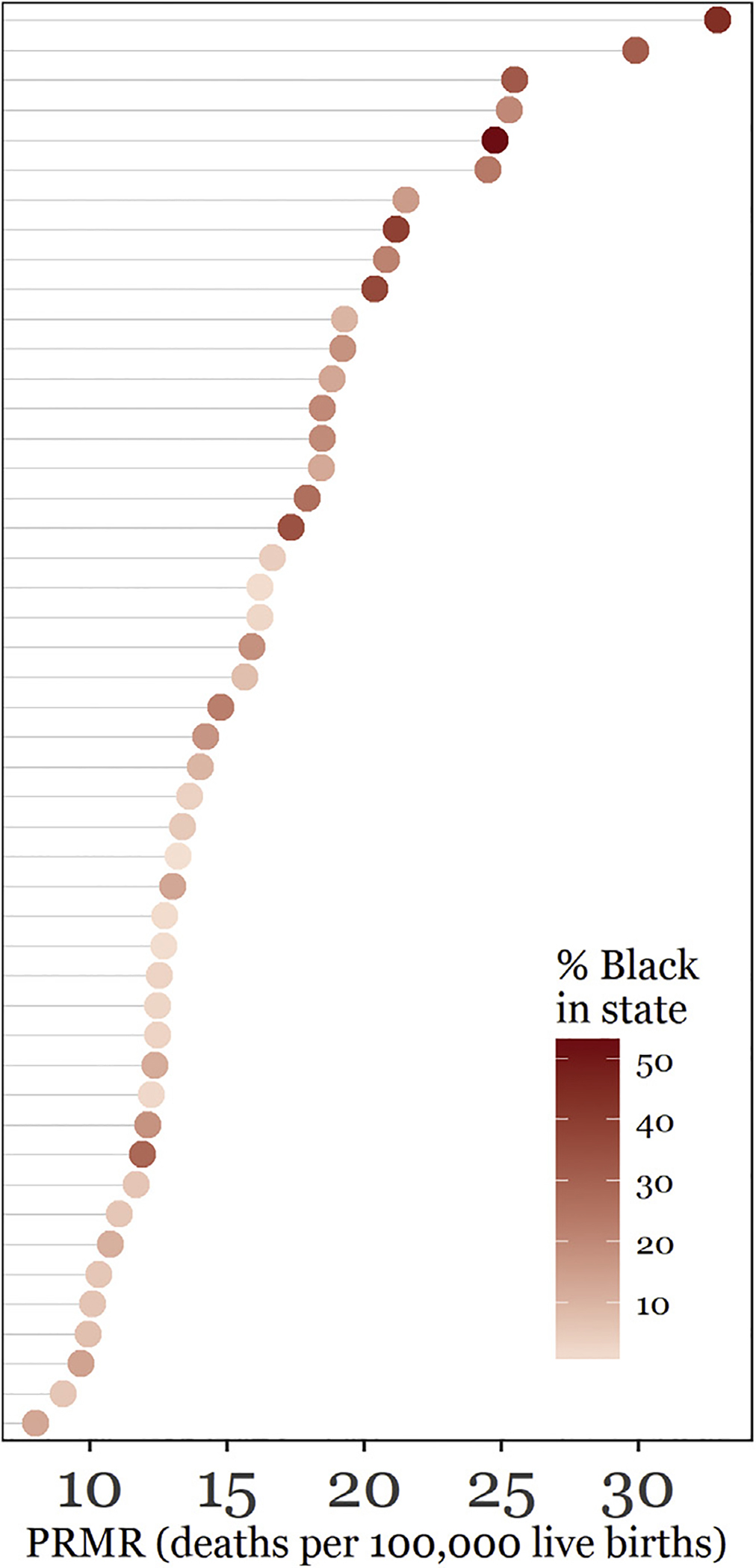
Anonymized state-specific, pregnancy-related mortality ratios for 47 states and the District of Columbia. States with fewer than 10 pregnancy-related deaths between 2006 and 2013 were excluded. State-specific proportion of live births to black mothers is reflected in color gradient of points. Sensitivity analysis restricted to states adopting the pregnancy checkbox on death certificates prior to 2006 produced a similar pattern, with a 2.6-fold difference between highest and lowest state. Pregnancy-related mortality ratio was deaths per 100,000 births. Reproduced from Pregnancy Mortality Surveillance System, Centers for Disease Control and Prevention.
Kramer. Health equity framework for maternal mortality. Am J Obstet Gynecol 2019.
Causes of individual cases vs the causes of population incidence
Developing effective interventions to reverse increasing trends and growing disparities in maternal mortality requires identification and intervention on the leading causal factors. Conventionally, prevention efforts focused on screening and identifying high-risk women for targeted prevention and intervention resources.
The identification and management of women at high risk to provide appropriate care at the appropriate time remains a critically important goal of obstetric practice, necessary for reducing a woman’s risk of severe morbidity or death. Approaching morbidity and mortality prevention by searching for women with individual risk factors is an example of what Rose9 referred to as seeking the causes of cases.
However, because between-group black-white racial disparities persist, even among women at otherwise low risk,10 focusing on individual-level risk factors alone is inadequate for effectively reducing population-level health disparities. For example, one study found no racial differences in the prevalence of 5 pregnancy complications (preeclampsia, eclampsia, abruption, placenta pre-via, and postpartum hemorrhage), but black women with each condition died at 2–3 times the rate as white women with the same conditions.11
Other studies report persistent, large black-white disparities in maternal mortality, even after stratifying on risk status, socioeconomic status, and demographic factors such as age and marital status.12,13 In each example, individual risk factors for maternal mortality matter, but these markers of high risk alone are inadequate for explaining between-race differences in the rate of pregnancy-related death.
In contrast to the high-risk individual approach, a multileveled framework goes beyond the causes of individual cases of morbidity or mortality, acknowledging what Rose9 refers to as the causes of population incidence rates. As an example, the history of racial and economic residential segregation in the United States means that individual women live, work, and play in sometimes dramatically distinct social and physical environments based on their race or class.14,15
This kind of spatial stratification may mean that, on average, black and white women grow up, emerge into adulthood, and become pregnant with different cumulative trajectories of access to health services and distinct patterns of exposure to both health stressors as well as economic and educational opportunities linked to health status.16 These group-level environmental differences may help explain intergroup differences in health status, health access, and physiological resilience beyond individual-level risk factors.
Proposing a health equity framework for maternal mortality
The 2018 American College of Obstetricians and Gynecologists Committee Opinion on the importance of social determinants of reproductive health17 builds on the rich theoretical and empirical evidence for understanding drivers of population disparities in general18–20 as well as maternal, perinatal, and pediatric health outcomes.21–25 Drawing from this work, we propose a framework that integrates the individual-level biomedical and behavioral causes of maternal death, with the population-level differences in sociocontextual environment, which might be drivers of disparities in rates of death between groups (Figure 3, adapted from elsewhere20).
FIGURE 3. Conceptual model for community determinants of maternal mortality.
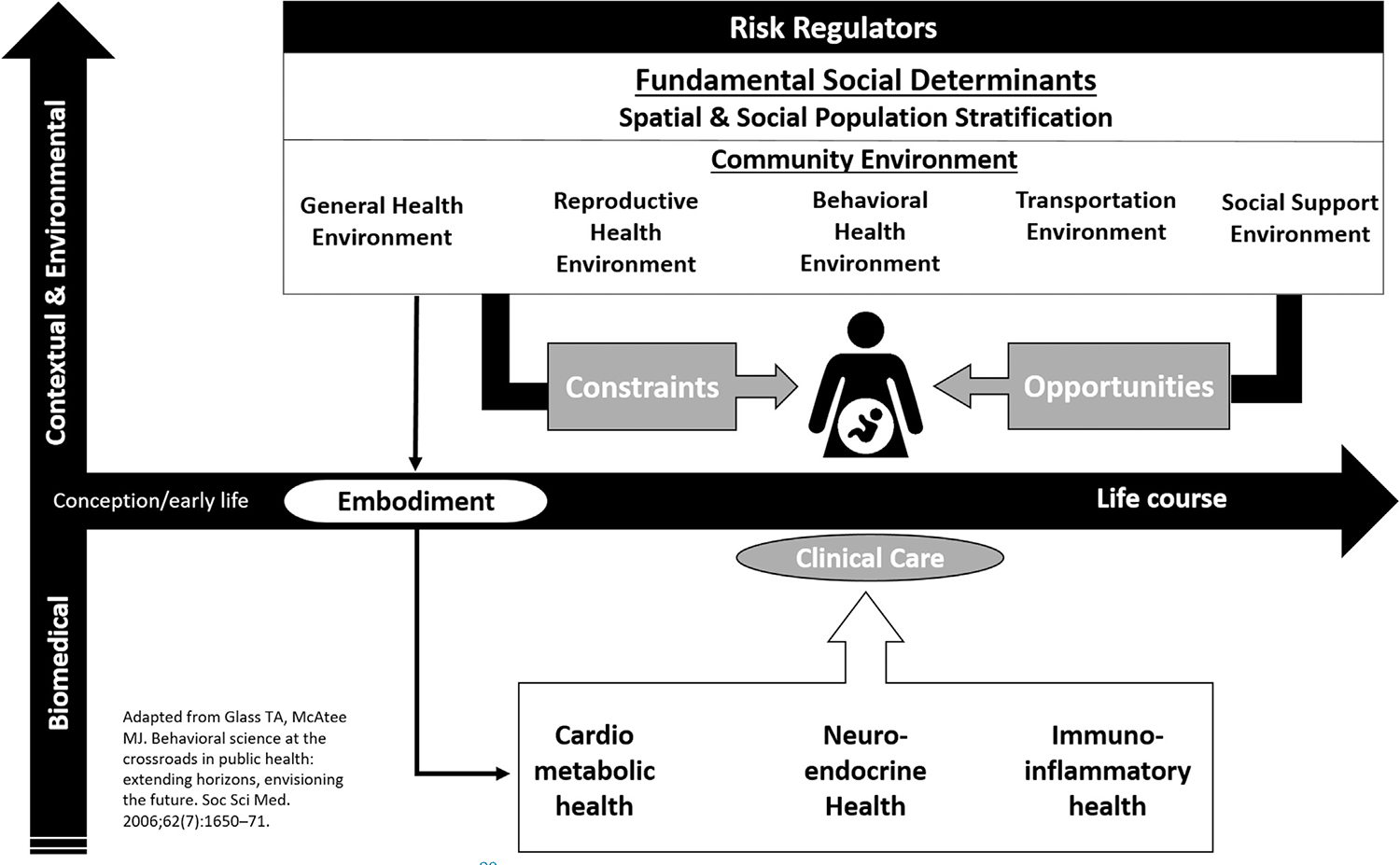
In this framework (adapted from Glass and McAtee20), the pregnant woman is situated at the intersection of 2 dimensions. The horizontal dimension represents her life course social and health trajectory and recognizes that preconceptional health including accumulated and chronic psychosocial stress, prevalent chronic health conditions (such as diabetes, hypertensions, and heart disease), and adequate family planning all contribute to her health at conception, through pregnancy, and postpartum. The vertical dimension represents the multileveled causes of morbidity and mortality, ranging from biomedical conditions (such as cardiometabolic, neuroendocrine, and immune-inflammatory health), which are under the skin, up to the health service, transportation, and social support community environments. These environmental factors represent risk regulators, which constrain or influence individual behaviors, health access, exposures, and experiences. Overlaying these community environments are the fundamental social determinants of health including structural racism, segregation, and poverty concentration, which systematically determine differences between racial and economic subpopulations in life-course opportunities and exposures. Together these community and social environments may influence individual behaviors, and they may also be biologically embodied as suggested by the weathering hypothesis, which seeks to explain disparities in reproductive health as a function of the premature physiological aging of neuroendocrine and immune systems as a result of chronic and repetitive stress.
Kramer. Health equity framework for maternal mortality. Am J Obstet Gynecol 2019.
This framework situates the pregnant woman at the intersection of 2 dimensions. The horizontal dimension represents her life course social and health trajectory, recognizing that preconception health, including accumulated chronic psychosocial stress, chronic health conditions (such as diabetes, hypertensions, and heart disease), and adequate family planning, all contribute to her health at conception, through pregnancy, and postpartum.26–28
The vertical dimension represents multileveled causes of reproductive health. Acting under the skin are the proximate biomedical conditions (such as cardiometabolic, neuroendocrine, and immune-inflammatory health), which are often the previously mentioned causes of cases of maternal morbidity and mortality. These biomedical processes are influenced in part by the timing, quality, and quantity of clinical care as well as health behaviors, which themselves are influenced by constraints and opportunities contained in the community environment.
Acting above the skin, we conceive of the community environment as the intersection of domains of resources and experiences. The general health, reproductive health, and behavioral health environments constitute local health service quality and quantity contributing to women’s health before, during, and after pregnancy.29–31 The transportation environment is necessary to link women to these services,32 and the social support environment reflects familial and community social networks and social capital necessary for psychosocial resilience.33,34 For example, women with lower social support and accessibility and quality of health services may experience increased unintended pregnancy and be more likely to enter pregnancy with prevalent or uncontrolled physical and behavioral health comorbidities that heighten the risk for poor outcomes.21,34,35 Together these environmental factors represent risk regulators, which constrain or influence individual behaviors, health access, comorbidities, exposures, and experiences.20
Overlaying these community resources are the fundamental social determinants of health, which refer to broader sociohistorical processes influencing and patterning socioeconomic opportunities, built environments, and exposure to chronic stressors.36 Disparities in maternal morbidity or mortality by race, class, and geography may be produced when fundamental social and economic factors (eg, structural racism, residential segregation, transgenerational poverty) produce average between-group differences in exposures and opportunities across women’s life course.
The final component of the framework is the link from the social and community environment back to individual physiological processes known as embodiment.19,37 One example of the biological embodiment of social experience is evidence that chronic stress related to discrimination or socioeconomic instability results in dysregulation of inflammatory and neuroendocrine processes during pregnancy.38–40
Just as practitioners use laboratory tests to inform a patient’s prescribed course of action in clinical settings, investigators can use geographically referenced indicators to identify community vital signs related to social determinants of health for mothers.23,41 The Table lists illustrative community-based indicators for each domain in the conceptual framework. Indicators were chosen if they met the following criteria: (1) previously used to measure the desired domain or indicators of sociospatial environments in health; (2) publicly available at a substate level of aggregation (eg, census tract or county), and (3) available for all US areas, making them applicable to MMRC data from any locale.
Finding a path forward: integrating the health equity framework into surveillance activities
Current population-based surveillance of maternal mortality in the United States relies on International Classification of Diseases, 10th revision, coding in National Vital Statistics System death files or on the more robust Pregnancy Mortality Surveillance System, which uses linked death and birth or fetal death certificates reviewed by medical epidemiologists to adjudicate whether death was related to pregnancy.42
These 2 systems provide important information about patterns of mortality over time and by race. Death certificates primarily document the fact of death and in many instances the proximate medical cause of death. However, they cannot characterize the underlying contributing causes leading to a pregnancy-associated death or the opportunities for prevention.
Maternal mortality review committees provide a complementary approach to systematically understanding proximate and distal contributing causes of maternal mortality by convening multidisciplinary teams of experts to review details of each maternal death and make recommendations for systems-level interventions to reduce risk.43
MMRCs have demonstrated wide-ranging estimates of the preventability of maternal deaths, with the variation attributable in part to the disciplinary diversity on the committee and the range of data available for review.12,44,45 For example, committees reliant solely on medical record review characterized only 28% of maternal deaths as preventable,46 while MMRCs conducting more holistic reviews engaged at the perinatal region level and state level reported 40% and 70% of maternal deaths as preventable, respectively.45,47
By viewing women not only as isolated patients but also as members of a larger environment replete with exposures and opportunities, then upstream health service, social, and environmental determinants of health may be conceived of as underlying contributors to a biomedical cascade of events ending in a tragic death. The higher attribution of preventability by state review committees is due in part to the more multidisciplinary mix of review committee members representing a broader view of the levels of causal contribution to maternal death: estimation of preventability depends on one’s view of modifiable causes.45
Given the positioning of MMRCs to conduct comprehensive evaluation of the complex reasons for a given clinical outcome, we believe our equity framework for maternal mortality can be readily incorporated into the MMRC case review process. Community-based indicators such as the examples presented in the Table can be linked to each maternal death using geocoded residential and clinical locations. In this way, a richer case narrative is possible in which individual behaviors, conditions, and processes are contextualized within a physical and social environment of opportunity and constraint while maintaining confidentiality. For instance, knowing a woman lived in a community without public transportation and where few residents own a car can be important when assessing why a woman did not make it to a specialist appointment. With this information, MMRCs can better understand the lived experience of the woman and make informed recommendations for preventive action.
One possible barrier to MMRC consideration of community-based contributors to preventable maternal mortality is the concern that social determinants of health arise outside the formal health care system and are thus perceived by members of MMRCs as unmodifiable. To begin to address this concern, we conducted a systematic web-based narrative review of the academic literature and publicly available information on existing policy and programmatic interventions addressing the identified community risk factors48 (Table).
TABLE.
Health equity domains, indicators, and possible policy and programmatic interventions
| Proposed sociospatial indicators | Data source | Illustrative interventions for this domain |
|---|---|---|
| General health environment | ||
| Primary care provider availability | Area health resources file | • Telemedicine (direct service provision and provider continuing education) • State Medicaid reimbursement policies that incen- tivize telemedicine • Training and loan repayment programs to incentivize clinician location • Mobile health units • State administrative and reimbursement policies that incentivize providers to accept MedicaidI • Interventions to increase availability of healthier foods and beverages in schools • Creating or improving places for physical activity |
| % Medicaid eligible | American community survey | |
| % Uninsured | American community survey | |
| Obesity prevalence | County health rankings | |
| % Poor/fair self-rated health | County health rankings | |
| Reproductive health environment | ||
| Obstetrician availability | Area health resources file | • Telemedicine (direct service provision and provider collaboration/continuing education) • State Medicaid reimbursement policies that incentivize telemedicine • Collaboration around integration of care and safe transfers during birth • Mobile health units • Family Medicine rotations and residency with a focus on obstetric services • Reduce barriers to independent practice for advanced practice registered nurses • State Medicaid patient reimbursement for contraception and education in clinical settings • Training of primary care physicians on contraceptive methods • Reimbursement of postpartum long-acting reversible contraception • Coordination of prenatal and delivery care and safe transfer to higher-level care |
| Certified nurse midwife availability | Area health resources file | |
| Family planning needs | Guttmacher Institute | |
| Newborn bed/bassinet availability | Area health resources file | |
| Infant mortality rate | County health rankings | |
| Low birthweight prevalence | County health rankings | |
| Behavioral health environment | ||
| Mental health provider availability | Area health resources file | • Telemedicine (direct service provision and provider collaboration/continuing education) • Medicaid reimbursement for maternal depression screening during well-child screening • Provider training on integrating maternal mental health services into the clinical setting • Increased collaboration between medical and behavioral health providers • Public education to reduce stigma among medical professionals • Provision of priority access for maternal drug treatment programs • Access to medication-assisted treatment for pregnant women |
| Poor mental health days | County health rankings | |
| Frequent mental distress | County health rankings | |
| Drug overdose deaths | County health rankings | |
| Nonmedical opioid use | SAMHSA/NSDUH | |
| Any mental illness | SAMHSA/NSDUH | |
| Unmet substance abuse treatment need | SAMHSA/NSDUH | |
| Prevalence of serious thoughts of suicide | SAMHSA/NSDUH | |
| Transportation environment | ||
| Rural/urban composition | American Community Survey | • State Medicaid reimbursement for nonemergency transportation • Public transportation grants and initiatives • Ride hailing partnerships |
| Car ownership | American Community Survey | |
| Long commute driving alone | County health rankings | |
| Public transit availability | EPA Smart Location Database | |
| Social support environment | ||
| % Single parent–headed households | American Community Survey | • Integrated referrals to social service supports in clinical models • Group prenatal care • Nurse family partnership • Video or telephone medical interpretation • State certification for medical interpreters |
| Social Capital Index | County health rankings | |
| % English speaking | American Community Survey | |
| Fundamental social determinants | ||
| Current poverty and persistent poverty | American Community Survey | • Integrated referrals to social service supports in clinical models • Group prenatal care • Increased screening and counseling for intimate partner violence • Medicaid reimbursement for language services |
| Violent crime rate | FBI uniform crime reporting | |
| Income inequality | American Community Survey | |
| Educational attainment | American Community Survey | |
| Food insecurity | Community Health Rankings | |
| Severe housing problems | County health rankings | |
| Racial and economic segregation | American Community Survey | |
Websites for each resource include the following: Area Resource Health File: https://datawarehouse.hrsa.gov/data/datadownload.aspx; American Community Service: https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t; County Health Ranking: http://www.countyhealthrankings.org/; EPA Smart Location Database: https://www.epa.gov/smartgrowth/smart-location-mapping#SLD; FBI UCR crime data: https://www.ucrdatatool.gov/; and SAMHSA/NSDUH: https://www.samhsa.gov/data/population-data-nsduh/reports?tab=38.
EPA, Environmental Protection Agency; NSDUH, National Survey on Drug Use and Health; SAMHSA, Substance Abuse and Mental Health Services Administration.
Kramer. Health equity framework for maternal mortality. Am J Obstet Gynecol 2019.
Committees need not feel limited to the interventions listed in the Table but can use them to inform community-level interventions most suited to mothers in their jurisdiction. Community partnerships are effective strategies for addressing social determinants of health49 and could be used to achieve many of the Table interventions, such as partnering with local health care systems to provide prenatal care in a group setting or via mobile health units. Partnership with a state Perinatal Quality Collaborative50 may also facilitate organizational relationships for patient referrals to necessary social services. State-administered Medicaid or public health programs have enormous potential to use innovative strategies for improving maternal health,51 including strategies that address maternal depression and access to interconception care as well as language and transportation services.
The proposed framework, along with the proposed indicators, can help MMRCs describe contributors to inequity, of which geographic, income, and racial disparities in pregnancy-related mortality are a symptom. However, data for potentially important indicators are not always available at community levels. For instance, indicators describe a community’s access to care, but not the quality of care provided. We can measure a community’s level of segregation, but we do not have universal indicators for the stress of associated discrimination experienced by individual women as a result.
We also lack standard measures for less tangible but positive influences on maternal health outcomes, such as the presence of supportive motherhood groups and other faith- and community-based outreach organizations. Some limitations of the proposed environmental measures could be at least partially addressed by incorporating information from family interviews, similar to those conducted in fetal-infant mortality reviews, into the maternal death review process.52
Just as the current list of community indicators is incomplete, our review of evidence-based, community-level interventions for each domain highlights important gaps, evidenced by a relatively sparse menu of prevention activities. As programmatic, policy, and systems-level interventions are evaluated, these can be incorporated into the framework. Acknowledging these limitations, we present a framework to advance incorporation of health equity into MMRC discussions and recommendations.
Conclusion
Increasing maternal mortality rates in the United States have raised national attention and calls for action. These trends, paired with the stark racial inequity in risk for death, have been framed not only as a public health emergency but as a human rights failure.53 Awareness of this urgency has grown in recent years, thanks in part to effective descriptive epidemiology of temporal trends, geographic variation, and racial disparities. But describing the problem is only the first step; effective clinical, public health, and community actions to meaningfully prevent maternal deaths and eliminate racial disparities require richer understanding of the multileveled causes of risk and incidence and development of evidence-based interventions within health systems but also in the broader community.
Obstetricians have led the charge in identifying provider, facility, and health-system factors contributing to maternal death.29,54,55 The continued advance of risk stratification, quality improvement practices, and standardization of clinical care are essential to address the problem. However, clinicians need not shoulder the responsibility alone. As evidence grows for the role of national, state, and local policies, programs, and processes in shaping population health, we need a richer evidence base for understanding the modifiable social and environmental determinants of health and health inequities.
Incorporation of an equity framework into maternal mortality surveillance could provide insight in several ways. First, by contextualizing each case in MMRC review, women are seen not as isolated individuals but as part of a wider community fabric influencing their health trajectories. Second, by incorporating community-based indicators into the review process, the power of the aggregated data will contribute to enhanced descriptive and etiologic evidence base, clarifying which factors matter more or less for population risk. Finally, by empowering MMRCs and other stakeholders with measures of community context and initial sets of possible policy or program recommendations, we can avoid the feeling that the social determinants of health are fixed and unchangeable.
These efforts are early steps in expanding our understanding of community-based drivers of maternal mortality. Given the limited evidence base for how community-based indicators relate to maternal mortality in the United States, future quantitative and qualitative work is needed to determine which domains and sociospatial indicators have the most meaningful impact on maternal health. It is clear that we cannot fully understand the reasons for both within- and between-population differences in maternal mortality unless we adopt approaches to systematically identify and evaluate them.
THE PROBLEM:
Maternal mortality in the United States has increased in recent years, and racial and geographic disparities are unacceptably large. Conventional clinical risk factors for maternal mortality are important for risk stratification of individuals but do not adequately explain maternal mortality rate differences between racial and geographic populations. This knowledge gap limits implementation of effective efforts to eliminate inequity in maternal mortality.
A SOLUTION:
Maternal mortality review committees (MMRC) holistic and multidisciplinary approach make them well positioned to fill these knowledge gaps. However, MMRCs may currently lack the tools to examine underlying social determinants of maternal mortality. We propose a literature- and theory-grounded framework for social determinants of maternal health, sociospatial measures of community context to potentially incorporate into individual maternal death review narratives, and illustrative policy and programmatic interventions that map community-based factors to possible MMRC recommendations for prevention.
Acknowledgments
This work was supported by an award agreement between the Centers for Disease Control and Prevention Foundation and the Merck for Mothers Program.
Footnotes
The authors report no conflict of interest.
The views expressed herein are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Michael R. Kramer, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, GA.
Andrea E. Strahan, Department of Health Policy and Management, Rollins School of Public Health, Emory University, Atlanta, GA.
Jessica Preslar, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, GA.
Julie Zaharatos, CDC Foundation, Atlanta, GA.
Amy St Pierre, CDC Foundation, Atlanta, GA.
Jacqueline E. Grant, Department of Obstetrics and Gynecology, School of Medicine, University of North Carolina, Durham, NC.
Nicole L. Davis, Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
David A. Goodman, Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
William M. Callaghan, Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
REFERENCES
- 1.Division of Reproductive Health. Pregnancy Mortality Surveillance System [Internet]. National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. 2017. Available at: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html. Accessed January 1, 2017. [Google Scholar]
- 2.Davis NL, Hoyert DL, Goodman DA, Hirai AH, Callaghan WM. Contribution of maternal age and pregnancy checkbox on maternal mortality ratios in the United States, 1978–2012. Am J Obstet Gynecol 2017;352.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacDorman MF, Declercq E, Cabral H, Morton C. Recent Increases in the US maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol 2016;128:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global Burden of Disease 2015 Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England) 2016;388:1775–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDorman MF, Declercq E, Thoma ME. Trends in maternal mortality by sociodemographic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol 2017;129:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callaghan WM. Geographic variation of reproductive health indicators and outcomes in the United States: place matters. Am J Obstet Gynecol 2014;211:278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kramer MR, Hogue CR. Place matters: variation in the black/white very preterm birth rate across US metropolitan areas, 2002–2004. Public Health Rep 2008;123:576–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brantley MD, Davis NL, Goodman DA, Callaghan WM, Barfield WD. Perinatal regionalization: a geospatial view of perinatal critical care, United States, 2010–2013. Am J Obstet Gynecol 2017;216:185.e1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose G Sick individuals and sick populations. Int J Epidemiol 2001;30:427–32. [DOI] [PubMed] [Google Scholar]
- 10.Saftlas AF, Koonin LM, Atrash HK. Racial disparity in pregnancy-related mortality associated with livebirth: can established risk factors explain it? Am J Epidemiol 2000;152:413–9. [DOI] [PubMed] [Google Scholar]
- 11.Tucker MJ, Berg CJ, Callaghan WM, Hsia J. The black-white disparity in pregnancy-related mortality from 5 conditions: differences in prevalence and case-fatality rates. Am J Public Health 2007;97:247–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberg D, Geller SE, Studee L, Cox SM. Disparities in mortality among high risk pregnant women in Illinois: a population based study. Ann Epidemiol 2006;16:26–32. [DOI] [PubMed] [Google Scholar]
- 13.Harper MA, Espeland MA, Dugan E, Meyer R, Lane K, Williams S. Racial disparity in pregnancy-related mortality following a live birth outcome. Ann Epidemiol 2004;14:274–9. [DOI] [PubMed] [Google Scholar]
- 14.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001;116:404–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kramer MR. Residential segregation and health. In: Duncan DT, Kawachi I, eds. Neighborhoods and health, 2nd ed. New York: Oxford University Press; 2018. p. 321–56. [Google Scholar]
- 16.Kramer MR. Race, place, and space: ecosocial theory and spatiotemporal patterns of pregnancy outcomes. In: Howell FM, Porter JR, Matthews SA, eds. Recapturing space: new middle-range theory in spatial demography. Cham, Switzerland: Springer International Publishing; 2016. p. 275–99. [Google Scholar]
- 17.American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women. Summary: importance of social determinants of health and cultural awareness in the delivery of reproductive health care. ACOG Committee Opinion No. 729. Obstet Gynecol 2018;131:198–9.29266073 [Google Scholar]
- 18.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- 19.Krieger N Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 2001;30:668–77. [DOI] [PubMed] [Google Scholar]
- 20.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med 2006;62:1650–71. [DOI] [PubMed] [Google Scholar]
- 21.Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med 2010;39:263–72. [DOI] [PubMed] [Google Scholar]
- 22.Kramer MR, Schneider EB, Kane JB, et al. Getting under the skin: children’s health disparities as embodiment of social class. Popul Res Policy Rev 2017;36:671–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping neighborhood health geomarkers to clinical care decisions to promote equity in child health. Health Aff (Millwood) 2017;36:999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Louis JM, Menard MK, Gee RE. Racial and ethnic disparities in maternal morbidity and mortality. Obstet Gynecol 2015;125:690–4. [DOI] [PubMed] [Google Scholar]
- 25.Peck MG, Sappenfield WM, Skala J. Perinatal periods of risk: a community approach for using data to improve women and infants’ health. Matern Child Health J 2010;14:864–74. [DOI] [PubMed] [Google Scholar]
- 26.Geronimus AT, Hicken MT, Pearson J, Seashols SJ, Brown KL, Cruz TD. Do US black women experience stress-related accelerated biological aging? A novel theory and first population-based test of black-white differences in telomere length. Hum Nat 2010;21:19–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q 2002;80:433–79, iii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the black-white gap in birth outcomes: a life-course approach. Ethn Dis 2010;20(1 Suppl 2):62–76. [PMC free article] [PubMed] [Google Scholar]
- 29.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol 2016;215:143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howell EA, Zeitlin J. Improving hospital quality to reduce disparities in severe maternal morbidity and mortality. Semin Perinatol 2017;41:266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levin BL, Becker MA. A public health perspective of women’s mental health. In: Levin BL, Becker MA, eds. New York, NY: Springer New York; 2010. [Google Scholar]
- 32.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38:976–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kane JB, Margerison-Zilko C. Theoretical insights into preconception social conditions and perinatal health: the role of place and social relationships. Popul Res Policy Rev 2017;36:639–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Appleton AA, Kiley K, Holdsworth EA, Schell LM. Social support during pregnancy modifies the association between maternal adverse childhood experiences and infant birth size. Matern Child Health J 2019;23:408–15. [DOI] [PubMed] [Google Scholar]
- 35.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–63. [DOI] [PubMed] [Google Scholar]
- 36.Gadson A, Akpovi E, Mehta PK. Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome. Semin Perinatol 2017;41:308–17. [DOI] [PubMed] [Google Scholar]
- 37.Krieger N Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health 2012;102:936–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hobel CJ, Goldstein A, Barrett ES. Psychosocial stress and pregnancy outcome. Clin Obstet Gynecol 2008;51:333–48. [DOI] [PubMed] [Google Scholar]
- 39.Wadhwa PD, Culhane JF, Rauh V, et al. Stress, infection and preterm birth: a bio-behavioural perspective. Paediatr Perinat Epidemiol 2001;15(Suppl 2):17–29. [DOI] [PubMed] [Google Scholar]
- 40.Hogue CJR, Bremner JD. Stress model for research into preterm delivery among black women. Am J Obstet Gynecol 2005;192(Suppl 5):S47–55. [DOI] [PubMed] [Google Scholar]
- 41.Bazemore AW, Cottrell EK, Gold R, et al. “Community vital signs”: incorporating geocoded social determinants into electronic records to promote patient and population health. J Am Med Informatics Assoc 2016;23:407–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.St Pierre A, Zaharatos J, Goodman D, Callaghan WM. Challenges and opportunities in identifying, reviewing, and preventing maternal deaths. Obstet Gynecol 2017;0(0):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodman D, Stampfel C, Creanga A, et al. Revival of a core public health function: state- and urban-based maternal death review processes. J Women’s Health 2013;22:395–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berg CJ, Harper MA, Atkinson SM, et al. Preventability of pregnancy-related deaths: results of a state-wide review. Obstet Gynecol 2005;106:1228–34. [DOI] [PubMed] [Google Scholar]
- 45.Geller SE, Koch AR, Martin NJ, Prentice P, Rosenberg D. Comparing two review processes for determination of preventability of maternal mortality in Illinois. Matern Child Health J 2015;19:2621–6. [DOI] [PubMed] [Google Scholar]
- 46.Clark SL, Belfort MA, Dildy GA, Herbst MA, Meyers JA, Hankins GD. Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery. Am J Obstet Gynecol 2008;199:36.e1–5; discussion 91–2. e7–11. [DOI] [PubMed] [Google Scholar]
- 47.Building US Capacity to Review and Prevent Maternal Death. Report from nine maternal mortality review committees. Atlanta, GA; 2018. Available at:. https://www.cdcfoundation.org/building-us-capacity-review-and-prevent-maternal-deaths. Accessed October 22, 2019.
- 48.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10(Suppl 1):6–20. [DOI] [PubMed] [Google Scholar]
- 49.Henize AW, Beck AF, Klein MD, Adams M, Kahn RS. A road map to address the social determinants of health through community collaboration. Pediatrics 2015;136:e993–1001. [DOI] [PubMed] [Google Scholar]
- 50.Henderson ZT, Suchdev DB, Abe K, Johnston EO, Callaghan WM. Perinatal quality collaboratives: improving care for mothers and infants. J Womens Health (Larchmt) 2014;23:368–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Applegate M, Gee RE, Martin JN. Improving maternal and infant health outcomes in Medicaid and the Children’s Health Insurance Program. Obstet Gynecol 2014;124:143–9. [DOI] [PubMed] [Google Scholar]
- 52.Shaefer J, Abdulahi H. Fetal and infant mortality review programs improve community systems. 2016. Available at: www.NFIMR.org.
- 53.Bingham D, Strauss N, Coeytaux F. Maternal mortality in the United States: a human rights failure. Contraception 2011;83:189–93. [DOI] [PubMed] [Google Scholar]
- 54.DʼAlton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol 2014;123:973–7. [DOI] [PubMed] [Google Scholar]
- 55.Bernstein PS, Martin JN, Barton JR, et al. National Partnership for Maternal Safety: consensus bundle on severe hypertension during pregnancy and the postpartum period. Anesth Analg 2017;125:540–7. [DOI] [PubMed] [Google Scholar]


