Introduction
In 2020, nearly 10 million U.S. adolescents (1.6 million 12 to 17 years of age and 8.2 million 18 to 25 years of age) met the diagnostic criteria for a substance use disorder (SUD; e.g., alcohol, tobacco, cannabis, and other drugs), and the majority were untreated.1 In the United States, more than 90% of adults with SUDs began their substance use in adolescence.2,3 Adolescents with SUDs have poorer functional outcomes across multiple domains (education/employment, family/social, and health) and are at greater lifetime risk for experiencing an array of adverse outcomes, including sexually transmitted diseases, poor family planning, justice system involvement, school-related challenges, neurocognitive impairments, and increased mental health burden.4,5 Adolescent substance use is associated with the leading causes of death in this age group: unintentional injury, suicide, and violence.6 Identifying SUDs during adolescence, and intervening, can mitigate an enormous burden on individuals, families, and communities.
Adolescence
Adolescence is a phase of life that bridges childhood and adulthood, a period that involves neurobiological, physiological, psychological, and social maturation, including engagement in risky behaviors such as consuming substances.7 Given the societal and legislative changes in the United States over the past 50 years, the transition period between childhood and adulthood has become protracted. In 2020, the average age at first marriage, often considered a sign of adulthood in the United States, was 30 years for men and 28 years for women, compared with 23 years and 21 years, respectively, in 1972.8 Legislatively, the passage of the Patient Protection and Affordable Care Act in 2010 afforded dependents the legal means to remain on their parents’ health insurance plan until 26 years of age.9 Thus, rather than 10 to 19 years of age, an expanded and more inclusive range of 10 to 25 years of age is essential for developmentally appropriate treatment and corresponds more closely to the current understanding of this life phase.10
Neurobiologic Development
Evolving understanding of neurodevelopment has illuminated why adolescence is such a period of risk for initiating substance use and developing SUDs.11 Brain development is characterized by uneven maturation, with the limbic structures involved in emotional responsivity and reward maturing earlier than the cortical areas involved in judgment, decision-making, and impulse control.2 Dopamine release in the nucleus accumbens (sometimes called the pleasure or reward center) is the final common pathway for all psychoactive substance use.12 Adolescents have more dopamine receptors than adults, resulting in a heightened response to substance use.13 At the same time, the brain regions that control executive functioning (e.g., logical reasoning, planning, and complicated decision-making), including the prefrontal cortex and the cerebellum, remain immature as they undergo a dynamic choreography of synaptic pruning into the mid-20s.14 This neuronal orchestration results in an expected delay of behavioral inhibition maturation relative to neural reward systems and gives rise to greater reward-seeking and risk-taking behaviors in adolescents than in adults.11 The hazards are compounded by the fact that the adolescent brain is more vulnerable to the lasting effects of substance use, including an increased risk of addiction because it is not fully mature.15 Heavy substance use during adolescence is associated with neurocognitive deficits and may further alter the development of neural systems regulating reward and inhibitory behavior, delay social maturation, and disrupt academic achievement.16,17
Definition of Adolescent SUDs
When a clinician encounters adolescents suspected of or known to have a substance use problem, it is essential to integrate the assessment process with potential treatment decisions. The assessment phase involves identifying any substance use and related issues, psychiatric comorbidities, or social problems that are clinically significant. The SUD is determined by whether the adolescent meets the SUDs criteria in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
In 2013, the DSM-5 ushered physicians toward unifying diagnostic criteria for abuse and dependence into a singular SUD, eliminating the “legal problems” criteria and adding a criterion about craving and a strong desire to use.18 The diagnostic criterion for SUDs includes 11 maladaptive behaviors and symptoms across four domains (social problems, loss of control, risky behaviors, and physiological changes) within the past 12 months. Depending on the number of criteria endorsed, severity may be mild (2 to 3), moderate (4 to 5), or severe (>6).18
Several limitations exist when attempting to apply the DSM-5 SUDs criteria in a developmentally considerate manner to adolescents. Kaminer and Winters19 have noted that the DSM-5 criteria for SUDs have questionable validity when applied to adolescents. An accurate and developmentally specific measurement of adolescent substance use is essential to providing a precise understanding of the nature and extent of an adolescent’s use pattern and determining their treatment needs. The current limitations of using the DSM-5 diagnostic criteria for SUDs in adolescents should serve as fertile ground for future investigation into better characterizing symptoms in adolescents.
Epidemiology
The U.S. federal government relies on national surveys to estimate the prevalence of adolescent substance use, including Monitoring the Future (MTF), the National Survey on Drug Use and Health (NSDUH), and the Youth Risk Behavior Surveillance System, among others. The NSDUH and the MTF go back to 1971 and 1975, respectively. The MTF collects substance use trends and related attitudes annually from students in grades 8, 10, and 12, and the NSDUH collects annual data on substance use and SUDs from persons 12 years of age and older.20
Gender Differences in Substance Use and SUDs
Historically, adolescent males have had higher rates of substance use than females.21 The gender gap has narrowed, with females at times equaling males in the prevalence of use.22 In 2019, females 12 to 20 years of age reported higher rates of past-month alcohol consumption (19.9% vs. 17.2%) and binge drinking (11.8% vs. 10.4%) than their male peers; however, they reported comparatively equal rates of heavy alcohol consumption (2.1% vs. 2.3% for males and females, respectively).23
The 2020 NSDUH indicates rates of past-year DSM-5 SUD among 12- to 17-year-old males and females (5.5% and 7.2%), again pointing to a narrowing and an inversion of the gender gap, particularly among adolescents.24 In the group 18 years of age and older, the historical trends returned, with 17.7% of males and 13.2% of females meeting the criteria for an SUD.24 Evidence suggests that many preventive and therapeutic interventions may have different effects on males and females25; exploring these differences is a high-priority area for future research and is consistent with the emphasis on precision medicine.
Racial and Ethnic Disparities in Substance Use, SUDs, and Consequences
Adolescents are prone to taking risks, chasing excitement, acting impulsively, and succumbing to peer pressure, regardless of race, class, and ethnicity. Forty years of adolescent self-report on national surveys confirm that youth of all races and ethnicities indicate involvement in risky, irresponsible, and even dangerous behaviors, including substance use. Nothing in the data collection suggests that Black or Latinx (used to describe a person of Latin American descent, unless a particular data source uses the term Hispanic) adolescents are inherently more reckless, impulsive, or dangerous than White youth. In fact, notwithstanding some differences in the type of substances, White youth report substance use (and other risky behaviors) at rates similar to — and sometimes higher than — Black and Latinx youth.
Although Black adolescents tend to report using marijuana (cannabis) more often and at earlier ages than White youth, White adolescents are more likely to report using many other drugs by the eighth through twelfth grades.26 Hallucinogens, synthetic marijuana, and all forms of prescription drugs, such as amphetamines, narcotics (oxycodone, hydrocodone/acetaminophen), and tranquilizers obtained without a doctors’ prescription, are just a few of the substances that are more popular among White adolescents than Black adolescents.26 White adolescents are also more likely than Black adolescents to have tried or used an electronic nicotine delivery system (ENDS; e.g., e-cigarettes, vaping).27 White adolescents outpace Black adolescents in all forms of alcohol use, including one-time experiences, binge drinking, getting drunk, and driving while intoxicated.26 Historically, this results in White and Latinx adolescents having higher prevalence rates of past-year SUDs than their same-age Black peers.24
Substance use behaviors arise from the same impulsive, shortsighted features shared among adolescents. Yet society does not treat all adolescents the same. Black youth who experiment with substances are likely to be considered more dangerous than White youth exhibiting the same behaviors.28 Educators flooded with negative images and false narratives about Black youth, regardless of socioeconomic status, are less likely to tolerate adolescent substance use–related misconduct and more likely to respond in ways that jeopardize a youth’s future.29,30 Police officers vulnerable to racial bias and stereotypes in fast-paced and stressful encounters with adolescents make snap judgments and racialized assumptions about what they see and how they respond.31–33 As a result, there is an overrepresentation of Black youth in drug cases referred to U.S. juvenile courts.34
The ramifications of social injustice in the societal response to and treatment of adolescent SUDs are profound and have resulted in decades of devastation to individuals, families, and communities. Guided by a scientific understanding of adolescent SUDs and the painful public health effects of criminalizing substance use, physicians and legislators have the opportunity — and the responsibility — to shift societal perception and, in turn, to shape policy and law.
Risk Factors
Understanding the common adolescent SUD risk factors and associated implications is critical for the primary care provider because early identification of risk factors allows for potential mitigation and close monitoring for early signs of substance use. Risk factors associated with substance use are complex and begin long before an individual has a first drink or first smoke or tries an illicit substance (Fig. 1).35 Stressful environments in early life have been vividly shown in both animal and human research to increase the later-life propensity to mental illness and increase the likelihood of SUDs.36 Most adolescent substance use will decrease as individuals reach adulthood. However, the younger an adolescent initiates substance use, the greater the risk of developing an SUD37; for this group, frequent heavy substance use typically persists.
Figure 1. Risk Factors Associated with Substance Use.
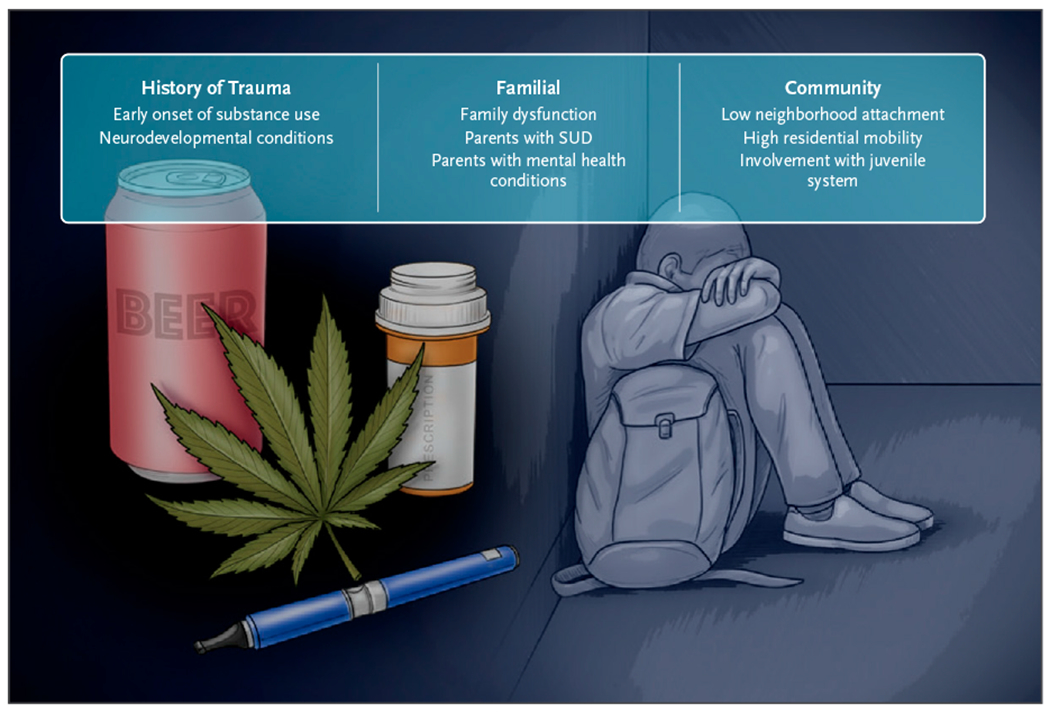
Risk factors are complex and begin long before an individual first tries an illicit substance.35 Risk factors have been identified at the individual, familial, and community levels. SUD denotes substance use disorder.
Longitudinal studies that monitor substance use progression over time have identified several individual-level (e.g., genetic predisposition) and environmental (e.g., community, family, and school, or a history of bullying) factors that increase the likelihood of progressing from sporadic use to disorder.38,39
Individual-level factors include temperament, positive attitude toward substance use (or low perception of risk related to substance use), selection of friends who engage in regular substance use, and early onset of substance use.2
The greatest risk is in those who engage in substance use before 14 years of age — they have a 34% prevalence rate of lifetime SUD.2 People with neurodevelopmental conditions, such as autism spectrum disorder or attention-deficient/hyperactivity disorder (ADHD), are at a higher than average risk for developing an SUD.40 Multiple factors at the community level, including low neighborhood attachment, availability of substances, and high residential mobility, also increase risk.41 Youth involved in the juvenile justice system are at exceptionally high risk.42 Familial factors include parents with SUDs or mental health conditions and family dysfunction.43 In addition, vulnerability for developing an SUD is higher among people with a family history of SUD,44 for whom genetic and environmental risks are compounded.
SCREENING TOOLS
Per the U.S. Preventive Services Task Force (USPSTF), evidence to support screening adolescents for unhealthy drug use is insufficient, in part because there is inadequate evidence to estimate the magnitude of harms associated with screening — namely, associated stigma, labeling, breach of confidentiality, or medico-legal consequences of documenting substance use.45
Whereas the USPSTF requires more evidence to recommend routine screening of adolescents for substance use, professional medical societies, including the American Academy of Pediatrics and the American Academy of Child and Adolescent Psychiatry, recommend screening adolescents for substance use annually.46,47 About 50% to 86% of pediatricians report routinely screening for substance use, and most screen using their clinical impressions rather than a validated screening tool.47 The ideal screening tool is brief, easy to use, sensitive, specific, and validated for identifying SUDs in order to guide subsequent assessment and intervention as appropriate (Table 1).
Table 1.
Brief Description of Selected Adolescence Substance Use Screening Tools.*
| Tool | No. of Questions | Description | Cutoff | Psychometrics |
|
|---|---|---|---|---|---|
| Sensitivity | Specificity | ||||
| CRAFFT 2.1 | 4 to 9 | Asks no. of days of use of alcohol, marijuana, and other drugs in past 12 mo, and asks about problems associated with use | ≥2 yes responses on six CRAFFT items | 0.91 | 0.93 |
|
| |||||
| NIAAA | 2 | Alcohol only: screens for friends’ use and for days of personal use in past 12 mo among children and adolescents (9 to 18 yr of age) | ≤15 yr of age: ≥1 d in past 12 mo (middle school) | 0.89 | 0.91 |
| 16 to 17 yr of age: ≥6 d in past 12 mo (high school) ≥18 yr of age: ≥12 d in past 12 mo |
0.88 | 0.81 | |||
|
| |||||
| S2BI | 3 to 7 | Asks frequency of use in past year of tobacco, alcohol, marijuana, and other drugs | Monthly and single past-year frequency question from the S2BI was sensitive and specific for discriminating among four categories of substance use experience (no past-year use, use without an SUD, mild or moderate SUD, and severe SUD) for each substance | 1.00 | 0.94 |
|
| |||||
| BSTAD | 6 to 36 | Asks no. of days of tobacco, alcohol, marijuana or other substance use by person and their friends in past 12 mo | Tobacco ≥6 d | 0.95 | 0.97 |
| Alcohol ≥2 d | 0.96 | 0.85 | |||
| Marijuana ≥2 d | 0.80 | 0.93 | |||
BSTAD denotes Brief Screening for Alcohol, Tobacco, and other Drugs; CRAFFT Car, Relax, Alone, Friends/Family, Forget, Trouble; NIAA National Institute of Alcohol Abuse and Alcoholism; S2BI Screening to Brief Intervention; and SUD substance use disorder.
Confidentiality
Confidentiality plays a vital role in adolescent health care. Evidence suggests that adolescents who receive physician confidentiality assurances are more willing to disclose use to their provider and to seek health care services.48
Adolescent self-report of substance use within a confidential assessment is valid, compares favorably to bioassay results,49 and is appropriate for universal screening. When symptoms are unclear, or when collateral history is missing, the complementary use of a biologic sample (e.g., urinalysis) from a consenting patient may help the provider with additional objective data (e.g., use vs. nonuse or quantifiable level).50 Biologic testing is not supported as a stand-alone screening or monitoring procedure for substance use.51
Managing Screen Results
When screening tools suggest an SUD, further assessment is indicated. Exploring age at first use, current pattern (e.g., quantity and frequency), negative consequences from use (e.g., accidents or injuries), and effects on physical and emotional health, school, and family can help to guide the next steps.
When feasible, a separate parent interview is helpful, although it is worth noting that parents frequently underestimate the severity and intensity of use.52 Results from a subsequent conversation can help direct a brief intervention and follow-up, facilitate connection with behavioral health counselors, and match the appropriate level of specialty care (e.g., outpatient, intensive outpatient, residential, inpatient, etc.) when needed. While the push toward integrated/collaborative care services in primary care may expand the capacity for substance use treatment for many adolescents, those with severe SUDs, particularly those with psychiatric comorbidities, may require more intensive treatment. Intensive treatment varies in length and intensity from intensive outpatient and partial hospitalization programs to residential treatment of variable duration lengths and sustained care (e.g., “recovery high schools”).
The referral to treatment process, coordination, and implementation are understudied within the adolescent substance use research. Familiarity with available substance use treatment programs in the community and understanding the level of care treatment matching parameters can help providers facilitate care for patients with more severe disorders. The American Academy of Pediatrics clinical report on screening, brief intervention, and referral to treatment provides guidance on level of care treatment matching for youth.47
Psychiatric Comorbidity
The majority of adolescents with SUDs will have other co-occurring mental illnesses.53 Evidence suggests that 37% to 80% of adolescents with SUDs have at least one other mental disorder.54 The relationship between psychiatric symptoms and substance use is bidirectional.
Psychiatric conditions, such as ADHD, mood and anxiety disorders, and psychosis, increase adolescent substance use risk.55 Children with ADHD are significantly more likely to try a range of substances during their lifetime compared with their non-ADHD counterparts.56 A recent meta-analysis suggests that adolescent cannabis use is associated with an increased risk of psychosis later in life.57 Co-occurrence of substance use and psychiatric disorders during adolescence is associated with poorer outcomes, including lower treatment retention, increased risk of relapse, worse psychosocial and family functioning, and higher likelihood of persistence of substance use problems into adulthood.
Given these considerations, screening for co-occurring psychiatric disorders and symptoms, including anxiety, ADHD, depression, trauma, eating disorders, nonsuicidal self-injury (e.g., cutting), and suicidal ideation, is recommended in primary care.53,58 There is evidence to suggest that appropriate diagnosis and concurrent treatment of psychiatric and substance use conditions can lead toward improvement in mental health outcomes.53,59
Interventions and Treatment Options
GOALS
The primary goals of adolescent SUD treatment are achieving and maintaining abstinence from substance use. While abstinence should remain the explicit, long-term goal for treatment, a realistic view recognizes both the chronicity of SUDs in some adolescents and the self-limiting nature of substance use in others. Continuous engagement, retention in care, and harm reduction, which aim to reduce the adverse effects of substance use, decrease the severity and frequency of relapses, and improve one or more domains of functioning,60 may be reasonable goals for some adolescents. Despite the controversy of harm reduction, “controlled use” of any substance causing a use disorder should never be an explicit goal in treating adolescents.
PSYCHOSOCIAL INTERVENTIONS
Research and best practices suggest that SUD treatment plans for adolescents include the following: motivational interviewing to enhance a patient’s motivation and engagement; family therapies that improve familial involvement to improve supervision, monitoring, and communication between parents and children (e.g., family behavioral therapy, family systems therapy, multidimensional family therapy); cognitive behavioral therapies that improve problem-solving skills, social skills, and relapse prevention (e.g., the Adolescent Community Reinforcement Approach and dialectical behavioral therapy); interventions that increase prosocial behaviors, peer relationships, and academic functioning; adequate duration of treatment, including provision of follow-up care after acute treatment61; and integrated interventions that simultaneously address comorbid psychiatric disorders through psychosocial therapies and/or medication(s).53
To improve the efficacy and to enhance the implementation of effective treatment programs, there is a need to study how to improve retention and engagement and to determine the optimal duration, dosage, and specificity of interventions for adolescent SUDs.
EVIDENCE FOR PHARMACOTHERAPY
SUDs in adolescents have multifactorial etiologies, and treatment requires integrated and concurrent approaches for substance use and any co-occurring psychiatric disorders. Medications should not be considered a stand-alone treatment for adolescent SUDs. Pharmacotherapy has the potential to complement existing psychosocial interventions and improve outcomes. The literature on pharmacotherapy for adolescent SUDs is limited. However, there is evidence to suggest that pharmacologic interventions may increase the effectiveness of psychosocial interventions for adolescent SUDs and specific psychiatric comorbidities such as ADHD.59,62,63
There are no Food and Drug Administration (FDA)–approved medications for adolescent SUDs other than buprenorphine, which is approved for adolescents 16 years of age or older for opioid use disorder.64 Despite alcohol, cannabis, and nicotine being the most commonly used substances during adolescence, there have been few pharmacologic investigations of youth with alcohol, cannabis, or tobacco (nicotine) use disorders. In addition, treatment strategies for youth vaping are still in their infancy, and no formal recommendations exist for promoting ENDS cessation.
There is evidence that some of the medications approved for adults are beneficial for adolescents, the most promising findings being buprenorphine for opioid use disorder and bupropion (300 mg) and varenicline for tobacco use disorders.65–68 N-acetylcysteine appears to be a promising treatment for cannabis use disorder and potentially alcohol use disorder, but more research is needed.68
Overall, pharmacotherapy has the potential to be an effective way to support psychosocial interventions and increase treatment effects; however, more rigorous research trials, inclusive of randomization, large sample sizes, and broadly diverse patients, are warranted before the FDA approves any of the potential adjunctive medications.
TREATMENT DURATION
There is a need for longitudinal follow-up cohorts of youth who have received SUD treatment to determine the optimal length of treatment. Within the broader field of addiction medicine, a treatment duration of 3 months is often considered a minimum to support a reduction in or cessation of substance use. For adolescents, treatment needs, preferences, and priorities may be particularly dynamic, regularly changing on the basis of motivation for treatment, familial and peer support, and the evolution and episodic nature of symptoms and severity.53 Employing strategic approaches to treatment reengagement can be helpful, as individuals may prematurely terminate their participation in the treatment services offered.69
Future Directions
Achieving health equity for adolescents with SUDs will require targeted interventions to address several disparities (e.g., age, race and ethnicity, gender) and designing a new legislative model that unties youth with SUDs from the legal system and a health care model that resembles a medical home.70 Future research studies should focus on pragmatic trials of interventions (e.g., brief interventions, mobile technology) that improve accessibility, medications, and novel therapeutics (e.g., vaccines to treat opioid disorders).71 There is a need to study aftercare programs that effectively achieve reduced youth substance use.
Footnotes
Disclosures
Author disclosures are available at evidence.nejm.org.
References
- 1.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2020 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2021. HHS publication no. PEP21-07-01-003, NSDUH Series H-56. [Google Scholar]
- 2.Jordan CJ, Andersen SL. Sensitive periods of substance abuse: early risk for the transition to dependence. Dev Cogn Neurosci 2017;25:29–44. DOI: 10.1016/j.dcn.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ignaszewski MJ. The epidemiology of drug abuse. J Clin Pharmacol 2021;61(Suppl 2):S10–S17. DOI: 10.1002/jcph.1937. [DOI] [PubMed] [Google Scholar]
- 4.Yonek JC, Dauria EF, Kemp K, Koinis-Mitchell D, Marshall BDL, Tolou-Shams M. Factors associated with use of mental health and substance use treatment services by justice-involved youths. Psychiatr Serv 2019;70:586–595. DOI: 10.1176/appi.ps.201800322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gakh M, Coughenour C, Assoumou BO, Vanderstelt M. The relationship between school absenteeism and substance use: an integrative literature review. Subst Use Misuse 2020;55:491–502. DOI: 10.1080/10826084.2019.1686021. [DOI] [PubMed] [Google Scholar]
- 6.Petrosky E, Ertl A, Sheats KJ, Wilson R, Betz CJ, Blair JM. Surveillance for violent deaths — National Violent Death Reporting System, 34 states, four California counties, the District of Columbia, and Puerto Rico, 2017. MMWR Surveill Summ 2020;69:1–37. DOI: 10.15585/mmwr.ss6908a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. Elk Grove Village, IL: American Academy of Pediatrics, 2017. [Google Scholar]
- 8.U.S. Census Bureau. Families and households data tables. 2021. (https://www.census.gov/topics/families/families-and-households/data/tables.1972.List_1483115411.html).
- 9.Rangel CB. H.R.3590 — 111th Congress (2009–2010): Patient Protection and Affordable Care Act. 2010. [Google Scholar]
- 10.Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health 2018;2:223–228. DOI: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- 11.Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med 2016;374:363–371. DOI: 10.1056/NEJMra1511480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierce RC, Kumaresan V. The mesolimbic dopamine system: the final common pathway for the reinforcing effect of drugs of abuse? Neurosci Biobehav Rev 2006;30:215–238. DOI: 10.1016/j.neubiorev.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther 2009;122:125–139. DOI: 10.1016/j.pharmthera.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenroot RK, Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev 2006;30:718–729. DOI: 10.1016/j.neubiorev.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci 2009;40:31–38. DOI: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wade NE, Bagot KS, Tapert SF, Gruber SA, Filbey FM, Lisdahl KM. Cognitive functioning related to binge alcohol and cannabis co-use in abstinent adolescents and young adults. J Stud Alcohol Drugs 2020;81:479–483. DOI: 10.15288/jsad.2020.81.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cawkwell PB, Hong DS, Leikauf JE. Neurodevelopmental effects of cannabis use in adolescents and emerging adults with ADHD: a systematic review. Harv Rev Psychiatry 2021;29:251–261. DOI: 10.1097/HRP.0000000000000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry 2013;170:834–851. DOI: 10.1176/appi.ajp.2013.12060782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaminer Y, Winters KC. DSM-5 criteria for youth substance use disorders: lost in translation? J Am Acad Child Adolesc Psychiatry 2015;54:350–351. DOI: 10.1016/j.jaac.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration. Comparing and evaluating youth substance use estimates from the National Survey on Drug Use and Health and other surveys. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2012. HHS publication no. SMA 12-4727, Methodology Series M-9. [PubMed] [Google Scholar]
- 21.National Institute on Drug Abuse. Sex and gender differences in substance use. 2022. (https://www.drugabuse.gov/publications/research-reports/substance-use-in-women/sex-gender-differences-in-substance-use).
- 22.Substance Abuse and Mental Health Services Administration. NSDUH detailed tables. CBHSQ data. 2020. (https://www.samhsa.gov/data/report/2020-nsduh-detailed-tables). [PubMed]
- 23.Lipari RN, Park-Lee E. Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2020. HHS publication no. PEP20-07-01-001, NSDUH Series H-55. [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration. Section 5 PE tables: results from the 2020 National Survey on Drug Use and Health: detailed tables. 2020. (https://www.samhsa.gov/data/sites/default/files/reports/rpt35323/NSDUHDetailedTabs2020/NSDUHDetailedTabs2020/NSDUHDetTabsSect5pe2020.htm).
- 25.Doumas DM, Esp S, Turrisi R, Bond L, Flay B. Efficacy of the eCHECKUP TO GO for high school seniors: sex differences in risk factors, protective behavioral strategies, and alcohol use. J Stud Alcohol Drugs 2020;81:135–143. DOI: 10.15288/jsad.2020.81.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future national survey results on drug use, 1975-2019: Volume I, Secondary school students. Ann Arbor: Institute for Social Research, The University of Michigan, 2020. (http://monitoringthefuture.org/pubs/monographs/mtf-vol1_2019.pdf). [Google Scholar]
- 27.Miech RA, Patrick ME, O’Malley PM, Johnston LD, Bachman JG. Trends in reported marijuana vaping among US adolescents, 2017–2019. JAMA 2020;323:475–476. DOI: 10.1001/jama.2019.20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jordan A, Allsop AS, Collins PY. Decriminalising being Black with mental illness. Lancet Psychiatry 2021;8:8–9. DOI: 10.1016/S2215-0366(20)30519-8. [DOI] [PubMed] [Google Scholar]
- 29.Simon KM. Them and me — the care and treatment of Black boys in America. N Engl J Med 2020;383:1904–1905. DOI: 10.1056/NEJMp2022606. [DOI] [PubMed] [Google Scholar]
- 30.Wooten L, Jordan A, Simon KM, Gold JA. This is us: a case examination on Black men in therapy. Acad Psychiatry 2021;45:763–767. DOI: 10.1007/s40596-021-01528-6. [DOI] [PubMed] [Google Scholar]
- 31.Del Pozo B, Sightes E, Goulka J, et al. Police discretion in encounters with people who use drugs: operationalizing the theory of planned behavior. Harm Reduct J 2021;18:132. DOI: 10.1186/s12954-021-00583-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goff PA, Jackson MC, Di Leone BAL, Culotta CM, DiTomasso NA. The essence of innocence: consequences of dehumanizing Black children. J Pers Soc Psychol 2014;106:526–545. DOI: 10.1037/a0035663. [DOI] [PubMed] [Google Scholar]
- 33.Voigt R, Camp NP, Prabhakaran V, et al. Language from police body camera footage shows racial disparities in officer respect. Proc Natl Acad Sci USA 2017;114:6521–6526. DOI: 10.1073/pnas.1702413114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Office of Juvenile Justice and Delinquency Prevention. Juvenile court statistics. 2018. (https://ojjdp.ojp.gov/library/publications/juvenile-court-statistics-2018).
- 35.Nawi AM, Ismail R, Ibrahim F, et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health 2021;21:2088. DOI: 10.1186/s12889-021-11906-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Compton WM, Jones CM, Baldwin GT, Harding FM, Blanco C, Wargo EM. Targeting youth to prevent later substance use disorder: an underutilized response to the us opioid crisis. Am J Public Health 2019;109(Suppl 3):S185–S189. DOI: 10.2105/AJPH.2019.305020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jester JM, Buu A, Zucker RA. Longitudinal phenotypes for alcoholism: heterogeneity of course, early identifiers, and life course correlates. Dev Psychopathol 2016;28:1531–1546. DOI: 10.1017/S0954579415001157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health 2020;67:354–361. DOI: 10.1016/j.jadohealth.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vrijen C, Wiertsema M, Ackermans MA, van der Ploeg R, Kretschmer T. Childhood and adolescent bullying perpetration and later substance use: a meta-analysis. Pediatrics 2021;147:e2020034751. DOI: 10.1542/peds.2020-034751. [DOI] [PubMed] [Google Scholar]
- 40.McKowen J, Woodward D, Yule AM, et al. Characterizing autistic traits in treatment-seeking young adults with substance use disorders. Am J Addict 2022;31:108–114. DOI: 10.1111/ajad.13247. [DOI] [PubMed] [Google Scholar]
- 41.Beyers JM, Toumbourou JW, Catalano RF, Arthur MW, Hawkins JD. A cross-national comparison of risk and protective factors for adolescent substance use: the United States and Australia. J Adolesc Health 2004;35:3–16. DOI: 10.1016/j.jadohealth.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 42.Siringil Perker S, Chester LEH. The justice system and young adults with substance use disorders. Pediatrics 2021;147(Suppl 2):S249–S258. DOI: 10.1542/peds.2020-023523H. [DOI] [PubMed] [Google Scholar]
- 43.Rusby JC, Light JM, Crowley R, Westling E. Influence of parent-youth relationship, parental monitoring, and parent substance use on adolescent substance use onset. J Fam Psychol 2018; 32:310–320. DOI: 10.1037/fam0000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Acheson A, Vincent AS, Cohoon AJ, Lovallo WR. Defining the phenotype of young adults with family histories of alcohol and other substance use disorders: studies from the Family Health Patterns project. Addict Behav 2018;77:247–254. DOI: 10.1016/j.addbeh.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krist AH, Davidson KW, Mangione CM, et al. Screening for unhealthy drug use: US Preventive Services Task force recommendation statement. JAMA 2020;323:2301–2309. DOI: 10.1001/jama.2020.8020. [DOI] [PubMed] [Google Scholar]
- 46.Bukstein OG, Bernet W, Arnold V, et al. Practice parameter for the assessment and treatment of children and adolescents with substance use disorders. J Am Acad Child Adolesc Psychiatry 2005;44:609–621. DOI: 10.1097/01.chi.0000159135.33706.37. [DOI] [PubMed] [Google Scholar]
- 47.Levy SJL, Williams JF. Substance use screening, brief intervention, and referral to treatment. Pediatrics 2016;138:e20161211. DOI: 10.1542/peds.2016-1211. [DOI] [PubMed] [Google Scholar]
- 48.Croft B, Parish SL. Care integration in the Patient Protection and Affordable Care Act: implications for behavioral health. Adm Policy Ment Health 2013;40:258–263. DOI: 10.1007/s10488-012-0405-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boykan R, Messina CR, Chateau G, Eliscu A, Tolentino J, Goniewicz ML. Self-reported use of tobacco, e-cigarettes, and marijuana versus urinary biomarkers. Pediatrics 2019;143:e20183531. DOI: 10.1542/peds.2018-3531. [DOI] [PubMed] [Google Scholar]
- 50.Grout RW, Cheng ER, Aalsma MC, Downs SM. Let them speak for themselves: improving adolescent self-report rate on pre-visit screening. Acad Pediatr 2019;19:581–588. DOI: 10.1016/j.acap.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 51.Hadland SE, Levy S. Objective testing: urine and other drug tests. Child Adolesc Psychiatr Clin N Am 2016;25:549–565. DOI: 10.1016/j.chc.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simon KM, Harris SK, Shrier LA, Bukstein OG. Measurement-based care in the treatment of adolescents with substance use disorders. Child Adolesc Psychiatr Clin N Am 2020;29:675–690. DOI: 10.1016/j.chc.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 53.Spencer AE, Valentine SE, Sikov J, et al. Principles of care for young adults with co-occurring psychiatric and substance use disorders. Pediatrics 2021;147(Suppl 2):229–239. DOI: 10.1542/peds.2020-023523F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Heradstveit O, Skogen JC, Hetland J, Stewart R, Hysing M. Psychiatric diagnoses differ considerably in their associations with alcohol/drug-related problems among adolescents. A Norwegian population-based survey linked with national patient registry data. Front Psychol 2019;10:1003. DOI: 10.3389/fpsyg.2019.01003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gray KM, Squeglia LM. Research Review: what have we learned about adolescent substance use? J Child Psychol Psychiatry 2018; 59:618–627. DOI: 10.1111/jcpp.12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harstad E, Levy S. Attention-deficit/hyperactivity disorder and substance abuse. Pediatrics 2014;134:e293–e301. DOI: 10.1542/peds2014-0992. [DOI] [PubMed] [Google Scholar]
- 57.Kiburi SK, Molebatsi K, Ntlantsana V, Lynskey MT. Cannabis use in adolescence and risk of psychosis: Are there factors that moderate this relationship? A systematic review and meta-analysis. Subst Abus 2021;42:527–542. DOI: 10.1080/08897077.2021.1876200. [DOI] [PubMed] [Google Scholar]
- 58.Sellers CM, Díaz-Valdés A, Oliver MM, Simon KM, O’Brien KHM. The relationship between alcohol and cannabis use with nonsuicidal self-injury among adolescent inpatients: examining the 90 days prior to psychiatric hospitalization. Addict Behav 2021;114:106759. DOI: 10.1016/j.addbeh.2020.106759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kast KA, Rao V, Wilens TE. Pharmacotherapy for attention-deficit/hyperactivity disorder and retention in outpatient substance use disorder treatment: a retrospective cohort study. J Clin Psychiatry 2021;82:20m13598. DOI: 10.4088/JCP.20m13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Noyes E, Yeo E, Yerton M, et al. Harm reduction for adolescents and young adults during the COVID-19 pandemic: a case study of community care in reach. Public Health Rep 2021;136:301–308. DOI: 10.1177/0033354921999396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Effective Health Care Program. Interventions for substance use disorders in adolescents: a systematic review. 2018. (https://effectivehealthcare.ahrq.gov/products/substance-use-disorders-adolescents/protocol).
- 62.Squeglia LM, Fadus MC, McClure EA, Tomko RL, Gray KM. Pharmacological treatment of youth substance use disorders. J Child Adolesc Psychopharmacol 2019;29:559–572. DOI: 10.1089/cap.2019.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fadus MC, Squeglia LM, Valadez EA, Tomko RL, Bryant BE, Gray KM. Adolescent substance use disorder treatment: an update on evidence-based strategies. Curr Psychiatry Rep 2019;21:96. DOI: 10.1007/s11920-019-1086-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Borodovsky JT, Levy S, Fishman M, Marsch LA. Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J Addict Med 2018;12:170–183. DOI: 10.1097/ADM.0000000000000388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marsch LA, Bickel WK, Badger GJ, et al. Comparison of pharmacological treatments for opioid-dependent adolescents: a randomized controlled trial. Arch Gen Psychiatry 2005;62:1157–1164. DOI: 10.1001/archpsyc.62.10.1157. [DOI] [PubMed] [Google Scholar]
- 66.Woody GE, Poole SA, Subramaniam G, et al. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. JAMA 2008;300:2003–2011. DOI: 10.1001/jama.2008.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Muramoto ML, Leischow SJ, Sherrill D, Matthews E, Strayer LJ. Randomized, double-blind, placebo-controlled trial of 2 dosages of sustained-release bupropion for adolescent smoking cessation. Arch Pediatr Adolesc Med 2007;161:1068–1074. DOI: 10.1001/archpedi.161.11.1068. [DOI] [PubMed] [Google Scholar]
- 68.Gray KM, Carpenter MJ, Baker NL, et al. A double-blind randomized controlled trial of N-acetylcysteine in cannabis-dependent adolescents. Am J Psychiatry 2012;169:805–812. DOI: 10.1176/appi.ajp.2012.12010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jordan A, Mathis ML, Isom J. Achieving mental health equity: addictions. Psychiatr Clin North Am 2020;43:487–500. DOI: 10.1016/j.psc.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 70.Levy S, Botticelli M. Moving to a medical model of substance use treatment of youth. Pediatrics 2021;147:Suppl 2:S262–S264. DOI: 10.1542/peds.2020-023523J. [DOI] [PubMed] [Google Scholar]
- 71.Kazemi DM, Li S, Levine MJ, Auten B, Granson M. Systematic review of smartphone apps as a mHealth intervention to address substance abuse in adolescents and adults. J Addict Nurs 2021;32:180–187. DOI: 10.1097/JAN.0000000000000416. [DOI] [PubMed] [Google Scholar]


