Abstract
Hypertension is a major global health problem, but prevalence rates vary widely among regions. To determine prevalence, treatment, and control rates of hypertension, we measured conventional blood pressure (BP) and 24-hour ambulatory BP in 6546 subjects, aged 40 to 79 years, recruited from 10 community-dwelling cohorts on 3 continents. We determined how between-cohort differences in risk factors and socioeconomic factors influence hypertension rates. The overall prevalence was 49.3% (range between cohorts, 40.0%–86.8%) for conventional hypertension (conventional BP ≥140/90 mm Hg) and 48.7% (35.2%–66.5%) for ambulatory hypertension (ambulatory BP ≥130/80 mm Hg). Treatment and control rates for conventional hypertension were 48.0% (33.5%–74.1%) and 38.6% (10.1%–55.3%) respectively. The corresponding rates for ambulatory hypertension were 48.6% (30.5%–71.9%) and 45.6% (18.6%–64.2%). Among 1677 untreated subjects with conventional hypertension, 35.7% had white coat hypertension (23.5%–56.2%). Masked hypertension (conventional BP <140/90 mm Hg and ambulatory BP ≥130/80 mm Hg) occurred in 16.9% (8.8%–30.5%) of 3320 untreated subjects who were normotensive on conventional measurement. Exclusion of participants with diabetes mellitus, obesity, hypercholesterolemia, or history of cardiovascular complications resulted in a <9% reduction in the conventional and 24-hour ambulatory hypertension rates. Higher social and economic development, measured by the Human Development Index, was associated with lower rates of conventional and ambulatory hypertension. In conclusion, high rates of hypertension in all cohorts examined demonstrate the need for improvements in prevention, treatment, and control. Strategies for the management of hypertension should continue to not only focus on preventable and modifiable risk factors but also consider societal issues.
Keywords: blood pressure, diabetes mellitus, hypertension, prevalence, special populations
Hypertension, a noncommunicable disease, is a major risk factor for cardiovascular disease.1 According to the Global Burden of Disease, heart disease was the leading cause of death in 2010, responsible for ≈232 million disability-adjusted life years worldwide.2 The number of cardiovascular deaths is expected to double by 2030.3 The global cost of cardiovascular diseases was US$863 billion in 2010 and ≈45% of the total cost is because of loss of productivity from disability or premature death, or loss of work time because of illness or the need to seek care.4 Consequently, many studies have concluded that reducing cardiovascular risk on a global basis, through control of hypertension, is critical to world health.5
Prevalence rates of hypertension are usually based on the conventional blood pressure (BP). This excludes a substantial number of individuals who have masked hypertension that has been shown to confer cardiovascular risk similar to that of sustained hypertension.6 However, prevalence rates based on the conventional BP include a considerable number of subjects with white coat hypertension. Recently, we showed that cardiovascular risk in most subjects with white coat hypertension is comparable to that of age- and risk-matched normotensive subjects.7
The main goal of this study was to compare prevalence, treatment, and control rates of conventional and ambulatory hypertension among cohorts of the International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO). However, as efforts to control hypertension have also focused on reducing the prevalence of cardiovascular risk factors8 and hypertension rates vary among regions, probably because demographic, social, and economic differences influence lifestyle and risk factors,9,10 we determined how differences in modifiable risk factors among countries influence hypertension rates. To assess the influence of socioeconomic factors, we used the Human Development Index (HDI), a statistic developed by the United Nations.11,12 This strategy might inform the prioritization of allocation of resources for hypertension prevention in different countries, considering traditional risk factors and socioeconomic factors.
Methods
Study Population
The IDACO database13 currently includes 12 725 participants, representing 12 randomly recruited population cohorts.14–22 Studies qualified for inclusion if they involved a random population sample, if baseline information was available on the conventional and ambulatory BPs and cardiovascular risk factors, and if subsequent follow-up included both fatal and nonfatal outcomes. All studies received ethical approval, and participants gave written informed consent.
Because disregarding treated subjects and women could affect our results, we excluded 2 IDACO cohorts as they did not include subjects taking antihypertensive drugs (n=981)23 or recruited only 70-year-old men (n=1143).17 Because the age range largely differed among cohorts and the prevalence rates of hypertension strongly depend on age, we selected 7843 subjects aged 40 to 80 years, an age range that was covered by all the cohorts. In addition, we applied the following exclusion criteria: (1) conventional BP unavailable (n=208), (2) nighttime BP not recorded (n=598),16 and (3) ambulatory BP recordings including <10 daytime readings (n=95) or <5 nighttime readings (n=396).13 Thus, the number of subjects included in our analyses was 6546.
BP Measurement
Trained observers measured the conventional BP with a manual mercury sphygmomanometer14,16,19–21, an automated device based on the Korotkoff sound technique (USM-700F; UEDA Electronic Works, Tokyo, Japan),15 or automated oscillometric devices (OMRON HEM-705CP, Omron Healthcare, Kyoto, Japan and Dinamap 8100, Critikon Inc, Tampa, FL),18,22 using the appropriate cuff size, with the subjects in the sitting position. Conventional BP was the average of 214–21 or 322 consecutive readings obtained either at the participants’ homes16,18–21 or at an examination center.14,15,22 Terminal digit preference was limited, suggesting accurate BP measurements (Table S1 in the online-only Data Supplement).
We programmed portable monitors to obtain ambulatory BP readings at 30-minute intervals throughout the entire day or at intervals ranging from 15 to 30 minutes during daytime and from 20 to 45 minutes at night (Table S2). The monitors used an oscillometric technique (SpaceLabs 90202 and 90207; SpaceLabs Inc, Redmond, WA) in Noorderkempen,16 EPOGH (European Project on Genes in Hypertension),20,21 Montevideo,18 Maracaibo,22 and JingNing.19 Takeda TM-2421 recorders (A&D, Tokyo, Japan) and the ABPM-630 devices (Nippon Colin, Komaki, Japan), used in Copenhagen14 and Ohasama,15 respectively, implemented both oscillometric and auscultatory techniques, but we analyzed only the oscillometric data. An SAS macro was used to process all ambulatory recordings that remained unedited. Only the Ohasama recordings were sparsely edited according to previously published criteria.24 Within-subject means of the ambulatory BP were weighted by the time interval between successive readings.
Cross-Classification Based on Conventional and Ambulatory BPs
Conventional hypertension was a BP of ≥140 mm Hg systolic or ≥90 mm Hg diastolic or use of antihypertensive drugs.25 Ambulatory hypertension was a 24-hour ambulatory BP ≥130 mm Hg systolic or ≥80 mm Hg diastolic or use of antihypertensive drugs25; for the daytime BP, these thresholds were 135 and 85 mm Hg, and for the nighttime BP, these thresholds were 120 and 70 mm Hg, respectively. When systolic BP and diastolic BP fell in different categories (ie, normotensive versus hypertensive), we considered the participant as hypertensive. We cross-classified untreated subjects based on their conventional and 24-hour ambulatory BPs into sustained normotensives, sustained hypertensives, white coat hypertensives, and masked hypertensives. Sustained normotension and sustained hypertension were consistently normal or elevated BP on both conventional and ambulatory measurements. White coat hypertension was conventional hypertension in the presence of a normal ambulatory BP. Masked hypertension was ambulatory hypertension in participants with a normal untreated conventional BP.
Other Clinical Data
We used questionnaires administered at enrollment to each participant to obtain information on medical history and smoking and drinking habits. Body mass index was body weight in kilograms divided by height in meters squared. We measured serum cholesterol and blood glucose by automated enzymatic methods. Diabetes mellitus was the use of antidiabetic drugs, a fasting glucose of ≥7.0 mmol/L, a random glucose of ≥11.1 mmol/L, a self-reported diagnosis, or diabetes mellitus documented in practice or hospital records.
Definition of Cardiovascular Risk Factors
We identified the following cardiovascular risk factors, based on the European Society of Hypertension and the European Society of Cardiology guidelines25: (1) obesity, defined as body mass index ≥30 kg/m2, (2) diabetes mellitus, (3) current smoking, (4) dyslipidemia, defined as total cholesterol ≥6.2 mmol/L, and (5) history of cardiovascular complications.
We used the inequality-adjusted HDI at the time of recruitment to rate the social and economic developments of a country.12 The HDI summarizes the average achievement in 3 key dimensions of human development: a long and healthy life, access to knowledge, and a decent standard of living. The HDI measures longevity by life expectancy at birth. Access to knowledge is rated by a combination of mean years of schooling and the expected years of schooling. Standard of living is based on the gross national income per capita. The HDI ranks all countries on a scale from 0 to 1, with higher scores indicating greater human development.
Statistical Analyses
We used SAS software, version 9.4 (SAS Institute, Cary, NC), for database management and statistical analyses. Among-cohort comparisons of means and proportions were tested using ANOVA and Fischer exact test, respectively. After stratification for cohort and sex, we interpolated missing values of body mass index (n=3) and total serum cholesterol (n=86) from their regression slope on age. For each cohort, we calculated prevalence, treatment, and control rates of hypertension in all subjects combined and separately in men and women and in 2 age groups (middle age 40–59 years and older age 60–79 years). We calculated crude rates and rates standardized to sex and age by the direct method. We computed 95% confidence intervals of rates as R±1.96×√(R/N), where R and N are the rate and the number of individuals used to calculate the rate. To determine the influence of the various risk factors, we calculated prevalence rates in each cohort, first including all participants, then excluding participants with ≥1 risk factors. We compared hypertension prevalence rates in subjects with and without risk factors using logistic regression analysis stratified for cohort. We assessed the association between the prevalence rates of hypertension and the HDI using meta-regression analysis with cohort entered as a random-effect.
Results
Characteristics of Participants
The total number of subjects included in our analyses was 6546: 2142 from Copenhagen, Denmark (enrollment 1993–1997)14; 1275 from Ohasama, Japan (1988–1994)15; 943 from Noorderkempen, Belgium (1985–2008)16; 962 from Montevideo, Uruguay (1995–1998)18; 189 from the JingNing county, China (2003–2004)19; 115 from Novosibirsk, Russia (1999–2001)20; 76 from Pilsen, Czech Republic (2000–2001)21; 161 from Padua, Italy(1999–2001)21; 139 from Kraków, Poland (1999–2000)21; and 544 from Maracaibo,22 Venezuela (1998–2007). Participants recruited in Kraków, Novosibirsk, Pilsen, and Padova took part in the EPOGH.21
Overall, the 10 cohorts included 2936 (44.9%) women, 1879 (28.8%) smokers, 577 (8.8%) diabetic patients, 1051 (16.1%) obese subjects, 5040 (77.0%) participants with dyslipidemia, and 539 (8.2%) patients with previous cardiovascular disease (Table S3). Mean age (±SD) was 57.8±10.2 years. Conventional systolic and diastolic BPs averaged 134.9±23.6 and 81.1±12.1 mm Hg, respectively. The corresponding values for the 24-hour ambulatory systolic and diastolic BPs were 125.2±13.9 and 74.6±8.7 mm Hg, respectively.
Prevalence, Treatment, and Control Rates of Conventional Hypertension
In the total study population, 3226 of the 6546 participants (49.3%) had conventional hypertension (Table 1). Prevalence rates were consistently higher in older subjects (60–79 years) than in middle-aged participants (40–59 years; Table S4). In Copenhagen, Ohasama, Montevideo, and Maracaibo, conventional hypertension tended to be more prevalent in men than in women, whereas opposite tendencies were observed in Noorderkempen, EPOGH, and JingNing. The sex- and age-standardized prevalence rates of conventional hypertension ranged from 43.0% in Copenhagen to 84.7% in Maracaibo.
Table 1.
Crude and Sex- and Age-Standardized Prevalence of Conventional and Ambulatory Hypertension by Cohort in 6546 Participants Aged 40 to 80 Years
| Conventional Hypertension | Ambulatory Hypertension | ||||||
|---|---|---|---|---|---|---|---|
| Cases | Crude Rate | Standardized Rate* | Cases | Crude Rate | Standardized Rate* | ||
| Copenhagen | 2142 | 952 | 44.4 (42.3–46.5) | 43.0 (41.9–44.6) | 1045 | 48.8 (46.7–50.9) | 47.3 (46.1–48.9) |
| Ohasama | 1275 | 591 | 46.4 (43.6–49.1) | 44.9 (42.1–48.0) | 609 | 47.8 (45.0–50.5) | 46.9 (44.2–50.1) |
| Noorderkempen | 943 | 377 | 40.0 (36.9–43.1) | 44.7 (41.6–48.3) | 332 | 35.2 (32.2–38.3) | 38.9 (35.8–42.5) |
| Montevideo | 962 | 488 | 50.7 (47.6–53.9) | 52.2 (49.1–55.6) | 471 | 49.0 (45.8–52.1) | 50.0 (46.8–53.4) |
| JingNing | 189 | 94 | 49.7 (42.6–56.9) | 51.2 (44.4–58.7) | 111 | 58.7 (51.7–65.7) | 59.7 (53.0–67.1) |
| EPOGH | 491 | 252 | 51.3 (46.9–55.7) | 54.5 (46.7–63.2) | 259 | 52.7 (48.3–57.2) | 56.4 (48.6–65.1) |
| Maracaibo | 544 | 472 | 86.8 (83.9–89.6) | 84.7 (80.4–89.4) | 362 | 66.5 (62.6–70.5) | 64.0 (58.6–70.0) |
| All | 6546 | 3226 | 49.3 (48.1–50.5) | … | 3189 | 48.7 (47.5–49.9) | … |
Conventional hypertension was a conventional blood pressure of ≥140 mm Hg systolic or ≥90 mm Hg diastolic or use of antihypertensive drugs. Ambulatory hypertension was a 24-hour blood pressure ≥130 mm Hg systolic or ≥80 mm Hg diastolic or use of antihypertensive drugs. EPOGH indicates European Project on Genes in Hypertension.
Rates were standardized to the distribution of sex and age in the whole study population (55.2% women, 53.9% between 40 and 60 years).
Of the 3226 hypertensive subjects in the total study population, 1549 (48.0%) received antihypertensive treatment. Treatment rates ranged from 33.5% in Copenhagen to 74.1% in Ohasama (Table 2; Figure S1). Conventional BP was controlled in 598 (38.6%) of the treated hypertensive participants. Control rates varied from 10.1% in Maracaibo to 55.3% in Ohasama.
Table 2.
Treatment and Control Rates of Conventional and Ambulatory Hypertension by Cohort
| Conventional Hypertension | Ambulatory Hypertension | |||||||
|---|---|---|---|---|---|---|---|---|
| All HT | Treated and Controlled | Treated and Not Controlled | Not Treated | All HT | Treated and Controlled | Treated and Not Controlled | Not Treated | |
| Copenhagen | 952 | 105 (11.0) | 214 (22.5) | 633 (66.5) | 1045 | 108 (10.3) | 211 (20.2) | 726 (69.5) |
| Ohasama | 591 | 242 (40.9) | 196 (33.2) | 153 (25.9) | 609 | 261 (42.8) | 177 (29.1) | 171 (28.1) |
| Noorderkempen | 377 | 98 (26.0) | 95 (25.2) | 184 (48.8) | 332 | 124 (37.4) | 69 (20.8) | 139 (41.9) |
| Montevideo | 488 | 66 (13.5) | 162 (33.2) | 260 (53.3) | 471 | 73 (15.5) | 155 (32.9) | 243 (51.6) |
| JingNing | 94 | 9 (9.6) | 34 (36.2) | 51 (54.3) | 111 | 8 (7.2) | 35 (31.5) | 68 (61.3) |
| EPOGH | 252 | 61 (24.2) | 99 (39.3) | 92 (36.5) | 259 | 63 (24.3) | 97 (37.5) | 99 (38.2) |
| Maracaibo | 472 | 17 (3.6) | 151 (32.0) | 304 (64.4) | 362 | 69 (19.1) | 99 (27.3) | 194 (53.6) |
| All | 3226 | 598 (18.5) | 951 (29.5) | 1677 (52.0) | 3189 | 706 (22.1) | 843 (26.5) | 1640 (51.4) |
Values are n (percentage). Treatment and control rates were assessed among those with hypertension. Conventional hypertension was a conventional blood pressure ≥140 mm Hg systolic or ≥90 mm Hg diastolic or use of antihypertensive drugs. Ambulatory hypertension was a 24-hour systolic blood pressure ≥130 mm Hg systolic or ≥80 mm Hg diastolic or use of antihypertensive drugs. EPOGH indicates European Project on Genes in Hypertension; and HT, hypertension.
Prevalence, Treatment, and Control Rates of Ambulatory Hypertension
The number of participants with 24-hour ambulatory hypertension totaled 3189 (48.7%; Table 1). In each cohort, 24-hour ambulatory hypertension tended to be more prevalent in men than in women and in older subjects than in middle-aged subjects (Table S5). The sex- and age-standardized prevalence rates ranged from 38.9% in Noorderkempen to 64.0% in Maracaibo. Diagnoses of hypertension based on conventional and 24-hour ambulatory BPs were concordant in 82.2% of the participants, ranging from 73.9% in Maracaibo to 85.1% in Ohasama.
Among the participants with ambulatory hypertension, 1549 (48.6%) received antihypertensive treatment. Treatment rates ranged from 30.5% in Copenhagen to 71.9% in Ohasama (Table 2; Figure S2). The ambulatory BP was controlled in 706 (45.6%) of the treated hypertensive participants. Control rates varied from 18.6% in JingNing to 64.2% in Ohasama.
The prevalence, treatment, and control rates for daytime and nighttime hypertension are provided in Tables S6 and S7. Diagnoses of hypertension based on daytime and nighttime ambulatory BPs were concordant in 81.9% of the participants, ranging from 77.9% in Copenhagen to 86.5% in Ohasama.
Prevalence of White Coat, Masked, and Sustained Hypertensions
Of the 3320 untreated subjects who were classified as normotensive based on the conventional BP, 561 (16.9%) had masked hypertension, that is, they were hypertensive based on the 24-hour ambulatory BP. The prevalence of masked hypertension among conventionally normotensive subjects ranged from 8.8% in Noorderkempen to 30.5% in JingNing. Of the 1677 untreated participants who were classified as hypertensive based on the conventional BP, 598 (35.7%) had white coat hypertension, that is, they were normotensive based on 24-hour ambulatory BP. The prevalence of white coat hypertension among conventionally hypertensive subjects varied from 23.5% in JingNing to 56.2% in Ohasama (Table 3). Of the 4997 untreated subjects, 1079 (21.6%) had sustained hypertension. The Maracaibo cohort reported the highest rate of sustained hypertension with 47.3% whereas Ohasama had the lowest rate (8.0%).
Table 3.
Prevalence of White Coat and Masked Hypertensions Among 4997 Untreated Participants
| Conventional Normotension | Conventional Hypertension | Conventional and Ambulatory Hypertension | |||
|---|---|---|---|---|---|
| All | Masked HT | All | White Coat HT | Sustained HT | |
| Copenhagen | 1190 | 249 (20.9) | 633 | 156 (24.6) | 477 (26.2) |
| Ohasama | 684 | 104 (15.2) | 153 | 86 (56.2) | 67 (8.0) |
| Noorderkempen | 566 | 50 (8.8) | 184 | 95 (51.6) | 89 (11.9) |
| Montevideo | 474 | 74 (15.6) | 260 | 91 (35.0) | 169 (23.0) |
| JingNing | 95 | 29 (30.5) | 51 | 12 (23.5) | 39 (26.7) |
| EPOGH | 239 | 39 (16.3) | 92 | 32 (34.8) | 60 (18.1) |
| Maracaibo | 72 | 16 (22.2) | 304 | 126 (41.4) | 178 (47.3) |
| All | 3320 | 561 (16.9) | 1677 | 598 (35.7) | 1079 (21.6) |
Values are number of participants (percentage). This analysis included untreated participants only. White coat hypertension was conventional hypertension in the presence of a normal ambulatory blood pressure. Masked hypertension was ambulatory hypertension in participants with a normal conventional blood pressure. Sustained hypertension was hypertension on both conventional and ambulatory measurements. EPOGH indicates European Project on Genes in Hypertension; and HT, hypertension.
Prevalence of Hypertension in Relation to Risk Factors
Overall, the prevalence of hypertension, defined either by conventional BP or by 24-hour ambulatory monitoring, was significantly higher in diabetics than in nondiabetics, in obese as compared with nonobese subjects, in dyslipidemic compared with normolipidemic participants, and in subjects with a history of cardiovascular disease as compared with those without such history. By contrast, conventional and ambulatory hypertension were less prevalent in smokers than in nonsmokers (Table 4).
Table 4.
Odds Ratios of Having Hypertension According to the Presence of Other Cardiovascular Risk Factors
| Conventional Hypertension | Ambulatory Hypertension | |||
|---|---|---|---|---|
| Odds Ratio | PValue | Odds Ratio | PValue | |
| Diabetes mellitus | 1.95 (1.60–2.36) | <0.0001 | 2.19 (1.81–2.64) | <0.0001 |
| Obesity | 2.59 (2.23–3.01) | <0.0001 | 2.51 (2.18–2.90) | <0.0001 |
| Dyslipidemia | 1.44 (1.29–1.61) | <0.0001 | 1.34 (1.20–1.49) | <0.0001 |
| Previous cardiovascular disease | 3.50 (2.84–4.30) | <0.0001 | 3.11 (2.54–3.79) | <0.0001 |
| Smoking | 0.60 (0.54–0.68) | <0.0001 | 0.81 (0.72–0.90) | 0.0002 |
Odds ratios (95% confidence interval) are obtained from univariate logistic regression analysis stratified for cohort. Conventional hypertension was a conventional blood pressure ≥140 mm Hg systolic or ≥90 mm Hg diastolic or use of antihypertensive drugs. Ambulatory hypertension was a 24-hour systolic blood pressure ≥130 mm Hg systolic or ≥80 mm Hg diastolic or use of antihypertensive drugs. Diabetes mellitus was the use of antidiabetic drugs, a fasting glucose ≥7.0 mmol/L, a random glucose ≥11.1 mmol/L, a self-reported diagnosis, or diabetes mellitus documented in practice or hospital records. Obesity was a body mass index ≥30 kg/m2. Dyslipidemia was a total cholesterol ≥6.2 mmol/L.
Tables 5 and 6 illustrate the impact of the risk factors on the prevalence of conventional and ambulatory hypertension in the general population cohorts. Overall, the prevalence of hypertension tended to decrease when subjects with diabetes mellitus, obesity, hypercholesterolemia, or history of cardiovascular disease were excluded from analysis but tended to increase when smokers were excluded. These tendencies were consistent across cohorts with 2 exceptions: the prevalence rates in the Ohasama cohort tended to decrease when smokers were excluded (from 46.4% to 45.7% for conventional hypertension and from 47.8% to 46.7% for ambulatory hypertension) and the ambulatory hypertension rate in Montevideo remained largely unchanged by exclusion of hypercholesterolemic participants (from 49.0% to 49.3%).
Table 5.
Prevalence Rates of Conventional Hypertension After Exclusion of Subjects With Risk Factors
| Participants Free of | |||||||
|---|---|---|---|---|---|---|---|
| Smoking | Diabetes Mellitus | Obesity | Cholesterol ≥6.2 mmol/L | History of CVD | All Risk Factors | ||
| Copenhagen | 952/2142 (44.4) | 633/1208 (52.4) | 901/2069 (43.5) | 732/1812 (40.4) | 439/1128 (38.9) | 865/2013 (43.0) | 186/489 (38.0) |
| Ohasama | 591/1275 (46.4) | 476/1042 (45.7) | 472/1052 (44.9) | 568/1243 (45.7) | 535/1175 (45.5) | 534/1209 (44.2) | 314/760 (41.3) |
| Noorderkempen | 377/943 (40.0) | 293/678 (43.2) | 348/906 (38.4) | 282/791 (35.7) | 226/608 (37.2) | 298/835 (35.7) | 98/321 (30.5) |
| Montevideo | 488/962 (50.7) | 412/769 (53.6) | 441/887 (49.7) | 321/717 (44.8) | 292/604 (48.3) | 432/881 (49.0) | 137/321 (42.7) |
| JingNing | 94/189 (49.7) | 69/128 (53.9) | 94/189 (49.7) | 91/185 (49.2) | 82/170 (48.2) | 87/181 (48.1) | 52/103 (50.5) |
| EPOGH | 252/491 (51.3) | 196/373 (52.5) | 226/453 (49.9) | 163/353 (46.2) | 171/341 (50.1) | 196/407 (48.2) | 59/144 (41.0) |
| Maracaibo | 472/544 (86.8) | 405/457 (88.6) | 348/410 (84.9) | 342/394 (86.8) | 378/436 (86.7) | 408/480 (85.0) | 157/184 (85.3) |
| All | 3226/6546 (49.3) | 2484/4655 (53.4) | 2830/5966 (47.4) | 2499/5495 (45.5) | 2123/4462 (47.6) | 2820/6006 (45.7) | 1003/2322 (43.2) |
Values are the number of hypertensive participants and the total number of participants not having the corresponding risk factor. The number between brackets is the percentage hypertensive subjects. Diabetes mellitus was the use of antidiabetic drugs, a fasting glucose ≥7.0 mmol/L, a random glucose ≥11.1 mmol/L, a self-reported diagnosis, or diabetes mellitus documented in practice or hospital records. Obesity was a body mass index ≥30 kg/m2. CVD indicates cardiovascular disease; and EPOGH, European Project on Genes in Hypertension.
Table 6.
Prevalence Rates of Ambulatory Hypertension After Exclusion of Subjects With Risk Factors
| Participants Free of | |||||||
|---|---|---|---|---|---|---|---|
| Smoking | Diabetes Mellitus | Obesity | Cholesterol ≥6.2 mmol/L | History of CVD | All Risk Factors | ||
| Copenhagen | 1045/2142 (48.8) | 629/1208 (52.1) | 992/2069 (47.9) | 812/1812 (44.8) | 501/1128 (44.4) | 953/2013 (47.3) | 201/489 (41.1) |
| Ohasama | 609/1275 (47.8) | 487/1042 (46.7) | 487/1052 (46.3) | 588/1243 (47.3) | 550/1175 (46.8) | 552/1209 (45.7) | 325/760 (42.8) |
| Noorderkempen | 332/943 (35.2) | 252/678 (37.2) | 303/906 (33.4) | 238/791 (30.1) | 194/608 (31.9) | 258/835 (30.9) | 74/321 (23.1) |
| Montevideo | 471/962 (49.0) | 390/769 (50.7) | 422/887 (47.6) | 316/717 (44.1) | 298/604 (49.3) | 424/881 (48.1) | 140/321 (43.6) |
| JingNing | 111/189 (58.7) | 77/128 (60.2) | 111/189 (58.7) | 107/185 (57.8) | 96/170 (56.5) | 103/181 (56.9) | 56/103 (54.4) |
| EPOGH | 259/491 (52.7) | 200/373 (53.6) | 229/453 (50.6) | 169/353 (47.9) | 176/341 (51.6) | 202/407 (49.6) | 59/144 (41.0) |
| Maracaibo | 362/544 (66.5) | 309/457 (67.6) | 253/410 (61.7) | 253/394 (64.2) | 286/436 (65.6) | 308/480 (64.2) | 108/184 (58.7) |
| All | 3189/6546 (48.7) | 2344/4655 (50.4) | 2797/5966 (46.9) | 2483/5495 (45.2) | 2101/4462 (47.1) | 2800/6006 (46.6) | 963/2322 (41.5) |
Values are the number of hypertensive participants and the total number of participants not having the corresponding risk factor. The number between brackets is the percentage hypertensive subjects. Diabetes mellitus was the use of antidiabetic drugs, a fasting glucose ≥7.0 mmol/L, a random glucose ≥11.1 mmol/L, a self-reported diagnosis, or diabetes mellitus documented in practice or hospital records. Obesity was a body mass index ≥30 kg/m2. CVD indicates cardiovascular disease; and EPOGH, European Project on Genes in Hypertension.
Hypertension Prevalence Rates in Relation to the HDI
Results of random-effects meta-regression analysis showed that the sex- and age-adjusted prevalence rates of both conventional and ambulatory hypertension in different cohorts were inversely related to the HDI (Figure). A 0.1 higher HDI was associated with a 15.7% (95% confidence interval, 1.2–30.3; P=0.034) lower prevalence rate of conventional hypertension and a 11.0% (confidence interval, 3.7–18.3; P=0.003) lower prevalence rate of ambulatory hypertension. The prevalence of the cardiovascular risk factors was, however, not significantly correlated with HDI.
Figure.
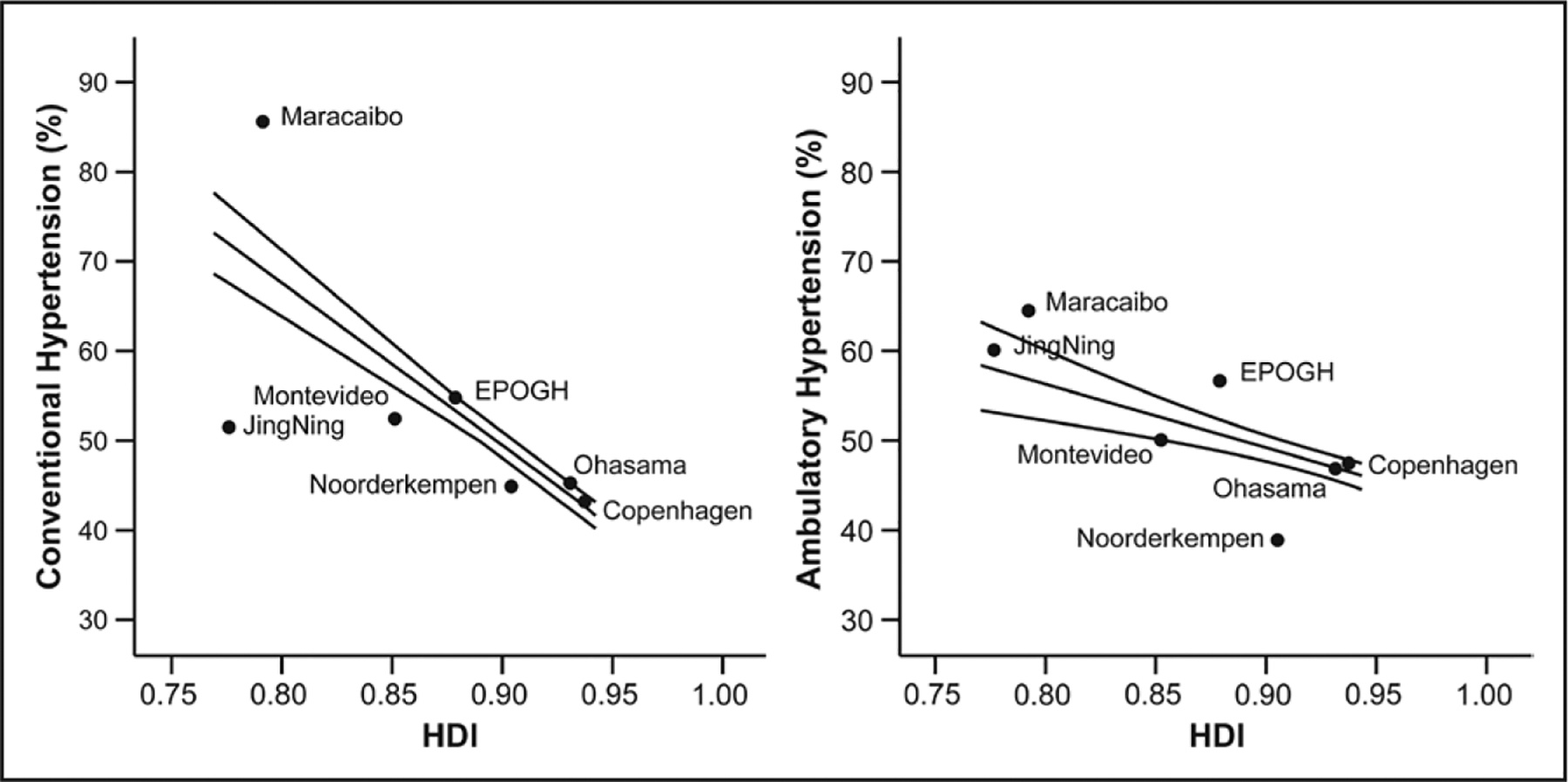
Meta-regression analysis relating the sex- and age-adjusted prevalence rates of conventional (left) and ambulatory (right) hypertensions to the Human Development Index (HDI). EPOGH indicates European Project on Genes in Hypertension.
Discussion
In this study, we examined prevalence, treatment, and control rates of conventional and ambulatory hypertension in 6546 subjects, aged 40 to 79 years, from 10 population-based cohorts in 3 continents. We determined how between-cohort differences in risk factors and socioeconomic aspects influence hypertension rates. Our key findings were that (1) the number of people with hypertension is high in all 10 cohorts, with estimates ranging from 40.0% to 86.8% for conventional hypertension and from 35.2% to 66.5% for 24-hour ambulatory hypertension; (2) only 33.5% to 74.1% of the subjects with conventional hypertension and 30.5% to 71.9% of the participants with ambulatory hypertension received antihypertensive drugs; (3) of those treated, BP was controlled in 10.1% to 55.3% of the subjects with conventional hypertension and in 18.6% to 64.2% of the participants with ambulatory hypertension; (4) after removing subjects with ≥1 traditional risk factors, the conventional (30.5%–77.7%) and ambulatory (23.1%–54.4%) hypertension prevalence rates remained high and the risk factors could not explain differences in prevalence rates among cohorts; and (5) the prevalence rates of both conventional and ambulatory hypertension were inversely related to the HDI, a marker for the social and economic developments of a country.
The prevalence of conventional hypertension in the whole IDACO population was 49.3%, which is higher than reported by previous multicountry studies (26.4% and 42.4%).5,26 The overall ambulatory prevalence rate of hypertension in our study was 48.7%. Few previous studies reported hypertension rates based on ambulatory BP monitoring. We estimated the overall prevalence of ambulatory hypertension from 3 multicountry studies by adding individuals with sustained and masked hypertension and individuals treated with antihypertensive drugs. The results showed rates of 35.3%,27 33.4%,28 and 33.3%.29 Our higher rate might be because of the older age of our subjects (40–79 years).
Yusuf et al26 showed that the risk factor burden, as assessed by the INTERHEART risk score (A Study of Risk Factors for First Myocardial Infarction in 52 Countries and Over 27 000 Subjects), is higher in high-income countries than in low-income countries. However, the rates of major cardiovascular disease and death were substantially higher in low-income countries than in high-income countries.26 Similarly, in our study, lower social and economic developments, as assessed by the HDI, were associated with higher prevalence of both conventional and ambulatory hypertension. This could not be attributed to the higher prevalence of cardiovascular risk factors in countries with lower social and economic developments because the HDI was not significantly related to the prevalence of cardiovascular risk factors. In addition, excluding individuals with cardiovascular risk factors did not remove differences in hypertension prevalence rates between cohorts. Thus, socioeconomic factors did explain some of the variation among IDACO cohorts. Populations in developing countries generally have fewer years of education than populations in developed countries,30 and lower education levels have been shown to be correlated with higher rates of hypertension.31,32 Unfortunately, we could not assess the relationship between education and hypertension because we did not have that information from all participating cohorts. We expressed that hypertension remains to be a problem worldwide, being associated with developed or developing conditions of regions.
Overall, fewer than half of all hypertensive subjects in this study received treatment and had BP in the normal range, consistent with results of previous studies.33 Hypertension treatment and control rates varied among IDACO cohorts, but the reasons for this are unclear. Treatment and control rates were not related to socioeconomic measures. Furthermore, previous studies found similar rates of hypertension treatment and control in developed and developing countries.34 The alarming rates of poor treatment and control of hypertension, highly correlated with morbidity and mortality because of cardiovascular disease,35,36 demand immediate and significant changes in public health actions and medical education.37 This reinforces the notion that prevention and adequate treatment of hypertension are urgently needed.38
Among IDACO cohorts, there were large variations in the prevalence of white coat, masked, and sustained hypertensions. We consider that this might be because of differences in age, sex ratio, risk factors distributions, and in the methodology and setting for conventional and ambulatory measurements (devices implemented and place where conventional BP was recorded).
Results for the Maracaibo population stood out among the overall results. The highest prevalence of hypertension among IDACO cohorts was found in Maracaibo. This is consistent with findings of the CARMELA study (Cardiovascular Risk Factor Multiple Evaluation in Latin America), where the highest prevalence for men and the second highest for women were in Venezuela, compared with 7 other Latin American countries.39 The Maracaibo cohort had the highest rate of sustained hypertension (47.3% among untreated subjects) compared with the next highest (26.7%) in the IDACO cohorts. Longitudinal studies have shown that subjects with sustained hypertension are at higher risk of cardiovascular mortality than subjects with masked or white coat hypertension.29 The outlying results for Maracaibo can be at least partly attributed to lifestyle. The typical diet in Maracaibo is rich in carbohydrates, salt, and fats.40,41 Outdoor recreational activities are scarce, and high temperatures limit the hours in which residents can perform physical activities.42 A sedentary lifestyle is prevalent.42,43 However, we cannot rule out the possible influence of other factors, such as gene–environment interactions and high levels of violence-related stress, on hypertension rates.
This study had several strengths: the use of multiple cohorts from both developed and developing countries; the population-based design of data collection for all cohorts; the use of both conventional BP measurements and ambulatory BP monitoring; the availability of individual subject data allowing us to assess the relationship between risk factors and the hypertension prevalence rates; and the use of the HDI as a socioeconomic indicator. However, our study also had some limitations. Some cohorts had a small sample size and conventional and ambulatory BP measurements were not standardized among the cohorts although day and night periods were homogeneous.13 The conventional BP in our study was the average of 2 readings obtained at a single examination. Participants using antihypertensive drugs were classified as hypertensive. This might have caused an overestimation of our prevalence rates of ambulatory hypertension by the inclusion of white coat hypertensive subjects treated based on their conventional BP. Finally, our data were collected between 1985 and 2008. Hypertension prevalence rates might have changed during this time period.44 Unfortunately, the IDACO database does not include follow-up BP measurements preventing us from assessing time trends in hypertension prevalence, treatment, and control rates. Overall, the study provides a large-scale, multinational view of hypertension, treatment, and control.
Perspectives
Hypertension affected almost half of our study population, which represented 12 countries and, therefore, is a major public health problem. Population-specific differences in hypertension rates were at least partly explained by differences in the ages of the participants and differences in socioeconomic conditions. Regional variation in rates of cardiovascular risk factors did not explain differences in hypertension rates among cohorts and were not related to variation in the HDI. However, exclusion of subjects with traditional risk factors from analysis reduced hypertension rates by 8% to 9%, implying that there are other important factors that need to be targeted to reduce hypertension rates at global scale. All cohorts had low rates of treatment and control, indicating that immediate and significant changes are needed in public health actions and medical education.37,38 Strategies for reducing rates of hypertension should continue to focus on preventable and modifiable risk factors but should also consider local socioeconomic factors as target for hypertension prevention.
Given that ≈23% of the population was affected either by white coat or masked hypertension, cost-effectiveness studies are needed to assess whether implementing 24-hour ambulatory BP monitoring in the detection, diagnosis, and treatment of hypertension in resource-poor settings should be recommended. Without those studies at hand, it seems intuitive to consider that regions with limited resources should focus on identifying people with hypertension who still do not receive treatment and that the treatment provided is able to effectively control high BP. However, in populations where white coat hypertension reaches a third of those with untreated conventional hypertension (eg, Maracaibo) or masked hypertension reaches a third of the conventional normotensive subjects (eg, JingNing) that assumption might be challenged. If ambulatory BP measurement is deemed too costly, home BP monitoring might provide an appropriate and cheap alternative.
Supplementary Material
Novelty and Significance.
What Is New?
Data on the prevalence of ambulatory hypertension are scarce. We compared prevalence, treatment, and control rates of conventional and ambulatory hypertension among 10 population-based cohorts in 3 continents. We examined how between-cohort differences in risk factors influence hypertension rates. We are the first to assess the impact of socioeconomic factors on conventional and ambulatory hypertension.
What Is Relevant?
Overall, the prevalence of hypertension was 49.6% for the conventional blood pressure and 48.7% for the ambulatory blood pressure. Less than half of individuals with hypertension received antihypertensive treatment, and of those, less than half had their blood pressure controlled.
Hypertension risk factors explained ≈9% of the total hypertension rates.
Lower social and economic developments was associated with higher prevalence rates of both conventional and ambulatory hypertension.
Summary
Our study highlights the high prevalence rates of hypertension among all cohorts and the poor treatment and control rates, even when ambulatory blood pressure measurement is used to define hypertension. The impact of traditional risk factors and socioeconomic aspects on the hypertension prevalence rates underscores that strategies for reducing rates of hypertension should continue focusing on preventable and modifiable risk factors but should also consider local socioeconomic factors.
Acknowledgments
We gratefully acknowledge the expert clerical assistance of Vera De Leebeeck and Renilde Wolfs (Studies Coordinating Centre, Leuven, Belgium). Thanks also go to Edvin Jaimes for processing professionally all the illustrated figures.
Sources of Funding
Maracaibo Aging Study was supported by the grant 1-R01AG036469 A1 from the National Institute of Aging and Fogarty International Center, grant G-97000726 from FONACIT, and grant LOCTI/008-2008 from FundaConCiencia. The European Union (grants IC15-CT98-0329-EPOGH, LSHM-CT-2006-037093 InGenious HyperCare, HEALTH-F4-2007-201550 HyperGenes, HEALTH-F7-249-EU MASCARA, HEALTH-F7-305507-HOMAGE, and the European Research Council Advanced Research Grant 294713 EPLORE) and the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0734.09, G.0881.13, and G.0880.13N) supported the Studies Coordinating Centre (Leuven, Belgium). The European Union (grants LSHM-CT-2006-037093 and HEALTH-F4-2007-201550) also supported the research groups in Shanghai, Kraków, Padova, and Novosibirsk. The Ohasama study received support via a Grant-in-Aid for Scientific Research (23249036, 23390171, 24390084, 24591060, 24790654, 25253059, 25461083, 25461205, 25860156, 26282200, 26860093, 16H05243, 16K09472, 16K11850, and 16K15359) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; a Grant-in-Aid from the Japan Society for the Promotion of Science (JSPS) fellows (25*7756, 25*9328, 26*857, and 27*656); the Japan Arteriosclerosis Prevention Fund; an Intramural Research Fund (22-4-5) for Cardiovascular Diseases of National Cerebral and Cardiovascular Center; and a Health Labor Sciences Research Grant (H26-Junkankitou [Seisaku]-Ippan-001) from the Ministry of Health, Labor, and Welfare, Japan. The Asociación Española Primera en Salud (AEPS) supported the research group in Montevideo. The Danish Heart Foundation (grant 01-2-9-9A-22914) and the Lundbeck Fonden (grant R32-A2740) supported the studies in Copenhagen. The National Natural Science Foundation of China (grants 81170245, 81270373, 81470533, and 91639203), the Ministry of Science and Technology (2013CB530700 and a grant for China-European Union collaborations [1012]), Beijing, China, and the Shanghai Commissions of Science and Technology (grants 14ZR1436200 and 15XD1503200) and Education (Gaofeng Clinical Medicine Grant Support 20152503) supported the JingNing study in China. The research in Czech Republic was supported by the Charles University Research Fund (project number P36).
Footnotes
Disclosures
None.
The online-only Data Supplement is available with this article at http://hyper.ahajournals.org/lookup/suppl/doi:10.1161/HYPERTENSIONAHA.117.09188/-/DC1.
References
- 1.Kannel WB. Framingham study insights into hypertensive risk of cardiovascular disease. Hypertens Res. 1995;18:181–196. [DOI] [PubMed] [Google Scholar]
- 2.Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, Murray CJ. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–1678. doi: 10.1161/CIRCULATIONAHA.114.008720. [DOI] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bloom DE, Cafiero ET, Jané-Lopis E, Abrahams-Gessel S, Bloom LR, Fathima S, Feigl AB, Gaziano T, Mowafi M, Pandya A, Prettner K, Rosenberg L, Seligman B, Stein AZ, Weinstein C. The Global Economic Burden of Noncommunicable Diseases. Geneva, Switzerland: World Economic Forum; 2011. [Google Scholar]
- 5.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 6.Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA; IDACO Investigators. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007;25:1554–1564. doi: 10.1097/HJH.0b013e3281c49da5. [DOI] [PubMed] [Google Scholar]
- 7.Franklin SS, Thijs L, Asayama K, et al. ; IDACO Investigators. The cardiovascular risk of white-coat hypertension. J Am Coll Cardiol. 2016;68:2033–2043. doi: 10.1016/j.jacc.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 8.Wong ND. Epidemiological studies of CHD and the evolution of preventive cardiology. Nat Rev Cardiol. 2014;11:276–289. doi: 10.1038/nrcardio.2014.26. [DOI] [PubMed] [Google Scholar]
- 9.Irala-Estévez JD, Groth M, Johansson L, Oltersdorf U, Prättälä R, Martínez-González MA. A systematic review of socio-economic differences in food habits in Europe: consumption of fruit and vegetables. Eur J Clin Nutr. 2000;54:706–714. [DOI] [PubMed] [Google Scholar]
- 10.Wang X, Bots ML, Yang F, Hoes AW, Vaartjes I. Prevalence of hypertension in China: a systematic review and meta-regression analysis of trends and regional differences. J Hypertens. 2014;32:1919–1927; discussion 1927. doi: 10.1097/HJH.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 11.Klugman J Human Development Report 2010: The Real Wealth of Nations: Pathways to Human Development. New York, NY: Palgrave Macmillan; 2010. [Google Scholar]
- 12.Noorbakhsh F A modified human development index. World Dev. 1998;26:517–528. [Google Scholar]
- 13.Thijs L, Hansen TW, Kikuya M, et al. ; IDACO Investigators. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. [DOI] [PubMed] [Google Scholar]
- 14.Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 15.Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–2189. [DOI] [PubMed] [Google Scholar]
- 16.Staessen JA, Bieniaszewski L, O’Brien ET, Imai Y, Fagard R. An epidemiological approach to ambulatory blood pressure monitoring:the Belgian Population Study. Blood Press Monit. 1996;1:13–26. [PubMed] [Google Scholar]
- 17.Ingelsson E, Björklund-Bodegård K, Lind L, Arnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–2866. doi: 10.1001/jama.295.24.2859. [DOI] [PubMed] [Google Scholar]
- 18.Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H. Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension. 1999;34(4 pt 2):818–825. [DOI] [PubMed] [Google Scholar]
- 19.Li Y, Wang JG, Gao P, Guo H, Nawrot T, Wang G, Qian Y, Staessen JA, Zhu D. Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population study. Blood Press Monit. 2005;10:125–134. [DOI] [PubMed] [Google Scholar]
- 20.Kuznetsova T, Malyutina S, Pello E, Thijs L, Nikitin Y, Staessen JA. Ambulatory blood pressure of adults in Novosibirsk, Russia: interim report on a population study. Blood Press Monit. 2000;5:291–296. [DOI] [PubMed] [Google Scholar]
- 21.Kuznetsova T, Staessen JA, Kawecka-Jaszcz K, Babeanu S, Casiglia E, Filipovsky J, Nachev C, Nikitin Y, Peleskã J, O’Brien E. Quality control of the blood pressure phenotype in the European Project on Genes in Hypertension. Blood Press Monit. 2002;7:215–224. [DOI] [PubMed] [Google Scholar]
- 22.Maestre GE, Pino-Ramírez G, Molero AE, Silva ER, Zambrano R, Falque L, Gamero MP, Sulbarán TA. The Maracaibo Aging Study: population and methodological issues. Neuroepidemiology. 2002;21:194–201. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. [DOI] [PubMed] [Google Scholar]
- 24.Ohkubo T, Imai Y, Tsuji I, Nagai K, Ito S, Satoh H, Hisamichi S. Reference values for 24-hour ambulatory blood pressure monitoring based on a prognostic criterion: the Ohasama Study. Hypertension. 1998;32:255–259. [DOI] [PubMed] [Google Scholar]
- 25.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 26.Yusuf S, Rangarajan S, Teo K, et al. ; PURE Investigators. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371:818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- 27.Gorostidi M, Sobrino J, Segura J, Sierra C, de la Sierra A, Hernández del Rey R, Vinyoles E, Galcerán JM, López-Eady MD, Marín R, Banegas JR, Sarría A, Coca A, Ruilope LM; Spanish Society of Hypertension ABPM Registry Investigators. Ambulatory blood pressure monitoring in hypertensive patients with high cardiovascular risk: a cross-sectional analysis of a 20,000-patient database in Spain. J Hypertens. 2007;25:977–984. doi: 10.1097/HJH.0b013e32809874a2. [DOI] [PubMed] [Google Scholar]
- 28.Gosse P, Dauphinot V, Roche F, Pichot V, Celle S, Barthelemy JC. Prevalence of clinical and ambulatory hypertension in a population of 65-year-olds: the PROOF study. J Clin Hypertens (Greenwich). 2010;12:160–165. doi: 10.1111/j.1751-7176.2009.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–515. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 30.Barro RJ, Lee JVV. A new data set of educational attainment in the world, 1950–2010. J Dev Econ. 2013;104:184–198. [Google Scholar]
- 31.de Gaudemaris R, Lang T, Chatellier G, Larabi L, Lauwers-Cancès V, Maître A, Diène E. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension. 2002;39:1119–1125. [DOI] [PubMed] [Google Scholar]
- 32.Grotto I, Huerta M, Sharabi Y. Hypertension and socioeconomic status. Curr Opin Cardiol. 2008;23:335–339. doi: 10.1097/HCO.0b013e3283021c70. [DOI] [PubMed] [Google Scholar]
- 33.Chow CK, Teo KK, Rangarajan S, et al. ; PURE (Prospective Urban Rural Epidemiology) Study Investigators. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 34.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–619. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 35.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 36.Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350:757–764. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 38.The Lancet. Hypertension: an urgent need for global control and prevention. Lancet. 2014;383:1861. [DOI] [PubMed] [Google Scholar]
- 39.Hernández-Hernández R, Silva H, Velasco M, Pellegrini F, Macchia A, Escobedo J, Vinueza R, Schargrodsky H, Champagne B, Pramparo P, Wilson E; CARMELA Study Investigators. Hypertension in seven Latin American cities: the Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA) study. J Hypertens. 2010;28:24–34. doi: 10.1097/HJH.0b013e328332c353. [DOI] [PubMed] [Google Scholar]
- 40.Souki-Rincón A, Sandoval M, Sánchez P, Andrade U, García-Rondon D, Cano-Ponce C, Medina M, Almarza J, Urdaneta Y, Gonzáles C. Ingesta de ácidos grasos saturados y sensibilidad a la insulina en adultos jóvenes obesos de Maracaibo. Rev Latinoam Hiperte. 2008;3:159–165. [Google Scholar]
- 41.Araujo MG, Fereira MS, Sulbarán T, Silva E, Calmón G, Campos G. Factores nutricionales y metabólicos como riesgo de enfermedades cardiovasculares en una población adulta de la ciudad de Maracaibo, Estado Zulia, Venezuela. Invest Clin. 2001;42:23–42. [PubMed] [Google Scholar]
- 42.Avila MIM. Factors That Influence the Social Life and Vitality of Public Open Spaces in Maracaibo-Venezuela. Case Study: Plaza de la Madre and Plaza de la República. PhD Thesis. Blacksburg, VA: Virginia Polytechnic Institute and State University; 2001. [Google Scholar]
- 43.Bermúdez VJ, Rojas JJ, Córdova EB, Añez R, Toledo A, Aguirre MA, Cano C, Arraiz N, Velasco M, López-Miranda J. International physical activity questionnaire overestimation is ameliorated by individual analysis of the scores. Am J Ther. 2013;20:448–458. doi: 10.1097/MJT.0b013e318235f1f2. [DOI] [PubMed] [Google Scholar]
- 44.Miura K, Nagai M, Ohkubo T. Epidemiology of hypertension in Japan: where are we now? Circ J. 2013;77:2226–2231. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


