Duodenal neuroendocrine tumors (D-NETs) are uncommon neoplastic entities 1 . The current guidelines advocate for resection when the lesion is ≤20 mm in size, in the absence of lymph node involvement 2 . However, the utility of endoscopic resection remains unclear, especially due to the risk of incomplete resection 3 . Endoscopic submucosal dissection (ESD) is an attractive technique because it offers the potential to achieve en bloc resection with clear margins. In a previous retrospective study, ESD for D-NETs achieved a 100% en bloc resection rate; however, the R0 resection rate is far from perfect and the perforation rate is not null 4 . The use of a traction device, with double clips and rubber band traction, has been described previously to improve the exposure of the tiny submucosal space 5 .
In this case, we describe the benefits of using an adaptative traction device (A-TRACT; Hospices Civils de Lyon, Lyon, France) during duodenal ESD ( Video 1 ).
Use of an adaptative traction device with endoscopic submucosal dissection for successful removal of a duodenal neuroendocrine tumor.
Video 1
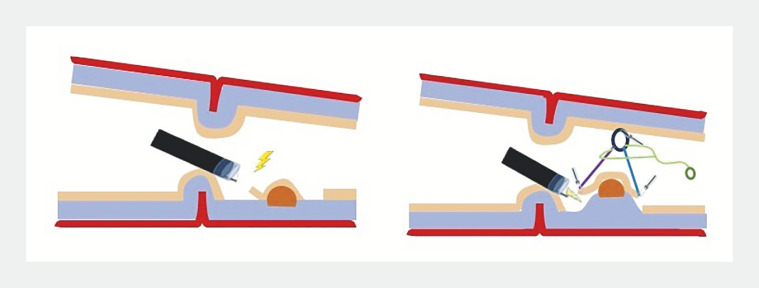
A 76-year-old patient was referred for removal of a D-NET of 8 mm in size, located in the upper part of the duodenal bulb, just behind the pylorus. An ESD was indicated to ensure R0 resection. After circumferential incision and trimming, the two loops of A-TRACT 2 were fixed by two clips to the lesion edges and another clip was used to affix the rubber band to the opposite mucosal wall, allowing exposure of the lesion previously hidden by the pylorus ( Fig. 1 ). The dissection was started with good traction, allowing the cut line to be clearly identified. After half of the lesion had been cut, traction was tightened to optimize visualization, and the dissection was safely completed in 40 minutes without adverse events. The histopathology revealed a G1 NET with lateral free margins but without deep free margins.
Fig. 1.
Schematic representation of the adaptive traction device (A-TRACT 2; Hospices Civils de Lyon, Lyon, France), allowing visualization of the lesion, which was previously hidden by the pylorus, and optimal exposure of the submucosa.
We hypothesize that this traction device could facilitate duodenal ESD, which is known to be technically challenging and with high risk of adverse events.
Endoscopy_UCTN_Code_TTT_1AO_2AG_3AD
Footnotes
Conflict of Interest J. Jacques, M. Pioche, and J. Rivory are co-founders of the ATRACT devices and co. E. De Cristofaro, T. Walter, T. Wallenhorst, and P. Lafeuille declare that they have no conflict of interest.
Endoscopy E-Videos https://eref.thieme.de/e-videos .
E-Videos is an open access online section of the journal Endoscopy , reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high-quality video and are published with a Creative Commons CC-BY license. Endoscopy E-Videos qualify for HINARI discounts and waivers and eligibility is automatically checked during the submission process. We grant 100% waivers to articles whose corresponding authors are based in Group A countries and 50% waivers to those who are based in Group B countries as classified by Research4Life (see: https://www.research4life.org/access/eligibility/ ). This section has its own submission website at https://mc.manuscriptcentral.com/e-videos .
References
- 1.Hoffmann KM, Furukawa M, Jensen RT et al. Duodenal neuroendocrine tumors: classification, functional syndromes, diagnosis and medical treatment. Best Pract Res Clin Gastroenterol. 2005;19:675–697. doi: 10.1016/j.bpg.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Panzuto F, Ramage J, Pritchard DM et al. European Neuroendocrine Tumor Society (ENETS) 2023 guidance paper for gastroduodenal NET G1–G3. J Neuroendocrinol. 2023;35:e13306. doi: 10.1111/jne.13306. [DOI] [PubMed] [Google Scholar]
- 3.Gincul R, Ponchon T, Napoleon B et al. Endoscopic treatment of sporadic small duodenal and ampullary neuroendocrine tumors. Endoscopy. 2016;48:979–986. doi: 10.1055/s-0042-112570. [DOI] [PubMed] [Google Scholar]
- 4.Gupta S, Kumar P, Chacchi R et al. Duodenal neuroendocrine tumors: short-term outcomes of endoscopic submucosal dissection performed in the Western setting. Endosc Int Open. 2023;11:E1099–E1107. doi: 10.1055/a-2181-0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oung B, Walter T, Hervieu V et al. Nonampullary duodenal subepithelial neuroendocrine tumor removed R0 by endoscopic submucosal dissection with double clips and rubber band traction. Gastrointest Endosc. 2019;4:570–573. doi: 10.1016/j.vgie.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]